Abstract
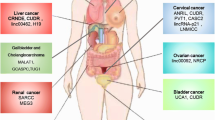
Metabolic reprogramming is commonly recognized as one important hallmark of cancers. Cancer cells present significant alteration of glucose metabolism, oxidative phosphorylation, and lipid metabolism. Recent findings demonstrated that long non-coding RNAs control cancer development and progression by modulating cell metabolism. Here, we give an overview of breast cancer metabolic reprogramming and the role of long non-coding RNAs in driving cancer-specific metabolic alteration.
Similar content being viewed by others
General overview on long non-coding RNAs
LncRNAs are transcripts, longer than 200 nucleotides, that are not translated in proteins [1, 2]. They are classified in several classes based on a very broad definition, that includes enhancer RNA (eRNA), long intergenic transcripts (lincRNAs), transcripts overlapping other non-coding transcripts both in the sense and anti-sense orientation, transcripts overlapping portion of protein-coding transcript. LncRNAs exhibit specific tissue expression and functions, they have been extensively studied as key regulators of cell physiology and pathology [3], and as diagnostic and prognostic markers in different cancers [4, 5]. Despite the very large number of annotated lncRNAs, only a minority of them has been extensively studied at the molecular level, allowing the identification of their mechanism of action. In general, lncRNAs act to regulate gene expression, they can directly affect chromatin remodelling (recruitment of activator and/or repressors) or they can interact with intracellular molecules using different strategies. Indeed, they can act as scaffolds to modulate the activity of other RNAs and proteins, they can sequester miRNAs, RNAs, proteins, they can regulate mRNA stability and splicing, and they can interfere with translation of mRNAs into proteins [6,7,8]. Recently, accumulating evidences suggested that lncRNAs act at different levels in tumours initiation and transformation in several tumours including breast cancer [9,10,11,12,13,14,15,16], also they are involved in metastasis and epithelial-to-mesenchymal transition [17,18,19]. They are also strongly associated to the metabolic reprogramming required for breast tumours development.
Breast cancers and metabolic reprogramming
Cancer cells reprogram their cellular metabolism to sustain cell proliferation by providing appropriate levels of energy in the form of ATP, biosynthetic capacity, and the maintenance of balanced redox status. These metabolic phenotypes are achieved by using glycolysis/ tricarboxylic acid cycle (TCA) intermediates for biosynthesis and NADPH production, increasing demand for nitrogen, requiring of an exogenous supply of glutamine and de novo biosynthesis of lipids [20]. Breast cancer is the leading cause of cancer–related death in women and about 90% of breast cancer deaths are related to the formation of distant metastasis [21]. Breast cancer is a heterogeneous disease that can be classified in several subtypes according to histopathological classes or to the molecular signature [22, 23]. Classically, breast cancer complies with the expression of hormone receptor for estrogen (ER+) and/or for progesterone (PR+) and for the expression of the human epidermal growth factor receptor (HER2) [24,25,26,27]. Therefore, breast cancer has been conventionally classified in five subtypes; luminal A (ER+ /PR+ /HER2−), luminal B, HER2 positive and triple negative (ER−/PR−/HER2−) [28,29,30]. This conventional classification of breast cancer has improved the diagnosis and the targeted therapy in patients, resulting in a better clinical outcome. However, we still need to uncover specific biomarkers that can assist in diagnosis, prognosis and proper treatment for each patient [31, 32]. We have recently shown the involvement of the p53 family [33,34,35,36,37,38] and in particular of p63 via the regulation of Sonic Hedgehog in the control of breast cancer proliferation [39,40,41,42,43,44], its transcriptional target ZNF750 [45, 46], as well as p73 [47]. These molecular mechanisms also showed the involvement of long noncoding RNA uc.63 [48]. Metabolomics research have made a great contribution in understanding specific metabolic pathways that are associated with cancer pathogenesis [49,50,51,52,53,54,55], and it is now largely accepted that metabolic alterations may be used as biomarkers. Thus, here we highlight the current knowledge on the main metabolic alterations that has been described in breast cancer.
Glycolysis
Alteration of the glycolytic pathway in cancer cells (Warburg effect) has been the first metabolic reprogramming to be described [56].
Several experimental evidences in triple negative breast cancer (TNBC) cell line and patient samples have shown an enhanced glycolysis [57, 58]. In agreement, by characterizing glucose consumption, glutamine consumption, and glutamine dependence, it has been shown that ER+ and TNBC cell lines are highly glycolytic [57]. One possible explanation for the glycolytic phenotype of ER+ breast cancer cell lines is that ERα mediates the transcriptional activation of the hypoxia inducible factor-1α (HIF-1α) [59]. HIF-1α has been previously reported to induce a glycolytic signature of metabolic genes [60] and hence, ERα can indirectly activate glycolysis via the activation of HIF-1α. To further support this explanation, HIF-1α is highly expressed in ER+ tumours [61]. Moreover, it has been shown that ER+ cell lines are more glycolytic than ER- cell lines [62]. The increase of glycolysis has been also observed in human tumour samples. Indeed, high levels of glucose transporter 1 (GLUT1) have been observed in TNBC tumours [63]. GLUT1 may also enhance invasion by localizing to the invasive edge of in vivo tumour models [64]. However, more recently has been shown that TNBC cell lines displayed a significant metabolic heterogeneity, being for instance MDA-MB-468 less glycolytic than MDA-MB-231 [65]. Several determinants have been demonstrated to contribute to enhanced glycolysis. For instance, the key enzymes, including hexokinase (HK), phosphofructokinase (PFK) and pyruvate kinase (PK), that play a key role in controlling glycolytic rate have been found upregulated or more enzymatically active in breast cancer tissues [66, 67]. An additional level of regulation of the glycolytic pathway is mediated by the Pyruvate dehydrogenase kinase 1 (PDK1). PDK1 by phosphorylating the enzyme pyruvate dehydrogenase (PDH), results in the inactivation of the PDH enzyme complex that thereby inhibits the conversion of pyruvate to acetyl-coenzyme A, which is then oxidized in the mitochondria to produce energy [68]. Breast cancer stem cells (BCSC) are a small subpopulation of breast tumours, which play a critical role metastasis formation and resistance to treatment [69, 70]. PDK1 has been found highly expressed in BCSC and its expression is required for the metabolic reprogramming toward the glycolysis upon hypoxic conditions [71]. Although the canonical role of glycolysis is to provide ATP and NADH, it should be also mentioned that the glycolytic pathway plays also a key role in providing metabolites for the biosynthesis of fundamental building blocks such as, amino acid and nucleotides. Indeed, the intermediate 3-Phosphoglycerate could be diverted into the serine synthesis [49]. Although serine is a nonessential amino acid, several cancer cells rely on de novo synthesis of serine, which is required for the biosynthesis of lipids, protein, nucleotide, and amino acids [72]. It has been shown that enzymes controlling nucleotides biosynthesis are also responsible for TNBC de-differentiation [73]. The first step of this pathway is the oxidation of 3-Phosphoglycerate to 3-phosphohydroxypyruvate by the enzyme Phosphoglycerate dehydrogenase [74, 75]. Genomic amplification of the Phosphoglycerate dehydrogenase enzyme has been found in 6% of human ER-negative breast cancer [76, 77].
Mitochondrial and OXPHOS
Most of the energy required by the cells is produced in the mitochondria via oxidative phosphorylation (OXPHOS), making mitochondria the powerhouse of the cells [78]. However, beyond producing energy, mitochondria are also involved in many processes including, generation of metabolites, biosynthetic metabolism, production of reactive oxygen species and regulation of cell death; and this is an essential need for cancer cells. Large body of evidence indicates that mitochondria have pleiotropic roles in the pathogenesis of cancer, depending upon genetic, environmental, and tissue-of-origin differences between tumours [79]. Breast cancer displays a significant inter-tumour metabolic heterogeneity [80]. Indeed, the luminal-like MCF-7 (ER+ and PR+) cell line shows a higher mitochondrial respiratory rate compared to the basal-like and highly metastatic MDA-MB-231 (ER− and PR−) cell line [81]. At molecular level, this phenotype was associated to the downregulation in MDA-MB-231 cells of Succinate Dehydrogenase Complex Iron Sulfur Subunit (SDHB), the core catalytic subunit of the mitochondrial heterotetrameric complex II, involved in both the citric acid cycle and electron transport chain. In addition, the expression of the complex I NDUFB8 subunit in MDA-MB-231 cells was lower when compared to MCF-7 cells suggesting that the switch from mitochondrial respiration to glycolysis is required for metastasis formation. This switch is required for cancer cells to evade the excess of ROS that are produced during the detachment from the extracellular matrix during the metastatic process [82, 83]. Therefore, by limiting mitochondrial oxidative metabolism, the glycolysis enables cancer cells to avoid excess ROS generation from mitochondrial respiration and thus gain survival advantage for metastasis. Consistently, the transcription factors HIF promotes metastasis formation by suppressing oxidative metabolism [84, 85]. However, invasive breast cancer cells exploit the transcription coactivator peroxisome proliferator-activated receptor gamma, coactivator 1 alpha (PGC-1α) to enhance oxidative phosphorylation, mitochondrial biogenesis and the oxygen consumption rate. In agreement, in human patients affected by invasive breast cancers has been observed a strong correlation between PGC-1α expression in invasive cancer cells and the formation of distant metastases [86]. In addition, breast cancer cells that metastasize to the lung and bone display an increase of OXPHOS metabolism compared to liver metastatic breast cancer cells, which are more glycolytic [87].
Lipid metabolism
Lipids are a heterogonous group of biomolecules that have a pivotal role in many biological functions including synthesis of biological membranes, working as secondary messenger and as energy source [88]. Cancer cells exhibit increased capacity of producing lipids not only for enabling the formation of lipid bilayers but also changes its composition in order to counteract the oxidative damage of the phospholipids [89]. A comprehensive lipidomics analysis in human breast tissues display an increase in de novo fatty acid synthesis [90]. In particular, the membrane phospholipids, such as palmitate-containing phosphatidylcholines, were increased in tumors when compared with normal breast tissues. Interestingly, ER- breast cancer shows high levels of this lipids and this was associated with cancer progression and patient survival. HER2 is a marker of poor prognosis, which is overexpressed in about 30% of breast cancer [91]. Interestingly, pharmacological inhibition of fatty acid synthase (FAS) suppressed p185HER2 expression suggesting a possible molecular link between FAS and HER2 [92]. Lipid droplets are cytoplasmic organelles that play important roles in lipid metabolism. Recently, several studies have described an increase in intracellular lipid accumulation in different tumours and it has been shown that they are involved in all the steps of the cancer pathogenesis, including initiation, promotion and progression [93]. Accumulation of cholesteryl ester (CE), one of the main components of lipid droplets, was significantly higher in Her2+ and TNBC than in Luminal A tumours, indicating and association between CE content and poor clinical outcome [94]. In addition, lipid accumulation was higher in Her2+ breast cancer, further supporting the involvement of cytoplasmic lipid accumulation in breast cancer development [95,96,97].
To summarizes, breast cancer exhibits metabolic plasticity that allows cancer cells to choose the best metabolic program to sustain tumour progression. Indeed, depending of the genetic and epigenetic alterations and microenvironments conditions (i.e. hypoxia, metastatic site) breast cancer cells fulfil their bioenergetics and biosynthetic needs, choosing between glycolysis, OXPHOS and lipid metabolism. Interestingly, previous, and recent findings, indicate that long non-coding RNA (lncRNAs) affect all these metabolic pathways [57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101]. LncRNAs also modulate hormone sensitivity and resistance in breast cancers [102, 103], see Table 1. Therefore, there are strong evidences indicating that metabolism-associated lncRNAs could be explored as novel therapeutic targets for hormone-refractory breast cancers and breast cancer in general. In this review we provide an overview of the significative findings related to lncRNAs involvement in breast cancer metabolic reprogramming.
LncRNAs and glucose metabolism
Tumor cells preferentially use glycolysis to produce ATP even in aerobic conditions. For this reason, glycolysis-dependent cancer cells will be prone to undergo metabolic reprogramming as they possibly need to compensate for lower energy production efficiency by glycolysis due to high turnover of cell proliferation. Below, we will report examples of relevant lncRNAs involved in the glucose metabolism in breast cancer. A more exhaustive overwiew of lncRNA affecting glucose metabolism is shown in Table 2.
LncRNA BCAR4
BCAR4 (Breast cancer anti-oestrogen resistance 4) is a nuclear lncRNA with oncogenic function that regulates glycolysis. BCAR4 is a YAP target and it required for YAP-dependent regulation of glycolysis. Together with GLI2, BCAR4 promotes the transcription of two enzymes, HK2 and PFKFB3, positive effector of glycolysis in triple negative breast cancer cells. Interesting, if this regulatory axis BCAR4/GLI2-HK2/PFKFB3 is inhibited (using BCAR4 silencing or HK2 and PFKFB3 inhibitors) the YAP-dependent positive effect on glycolysis, and as consequence proliferation and tumorigenesis are suppressed [99] (Fig. 1A). In addition, previous studies have identified BCAR4 as an epigenetic regulator. BCAR4 associates with SNIP1 (Smad nuclear-interacting protein 1) and PPP1R10/PNUTS (serine/threonine-protein phosphatase 1 regulatory subunit 10 to promote the transcription of GLI2 (glioma associated oncogene homolog 2) modulating p300 histone acetyltransferase activity [104]. YAP-BCAR4 axis facilitates glycolysis and breast cancer metastasis. Clinically, BCAR4 and YAP expression are positively correlated in breast cancer and high expression of both BCAR4 and YAP is associated with poor survival of patients with breast cancer [99]. Besides BCAR4, other lncRNAs stimulates glycolysis in breast cancer cells enhancing the transcription of specific enzymes or supporting enzyme catalytic activity (Table 2), for example lncRNA YIYA that promote activation of the PFKFB3 enzyme [105].
LncRNA regulates glycolysis in breast cancer cells. A YAP regulate the expression of the lncRNA BCAR4, which in turn by interacting with GLI2, promotes the transcription of two enzymes, HK2 and PFKFB3, resulting in the upregulation of the glycolytic pathway. B Under hypoxic conditions the LncRNA HIFAL is essential for maintaining HIF-1α transactivation and stimulates glycolysis in breast cancer cells by regulating the expression of glycolytic genes. HK-2: hexokinase 2; PFKB3: 6-Phosphofructo-2-Kinase/Fructose-2,6-Biphosphatase 3; GLUT1: Glucose Transporter 1; LDHA: Lactate Dehydrogenase A; PDK1: Pyruvate Dehydrogenase Kinase 1; GLI2: GLI Family Zinc Finger 2
LncRNA LINK-A
The lncRNA LINK-A (Long Intergenic Non-coding RNA for Kinase Activation, also known as LINC01139) is a cytoplasmic lncRNA with oncogenic function, expressed in triple negative breast cancers. It is the first lncRNA described to interact with phospholipid [100]. LINK-A interacts with AKT and PIP3, to facilitate AKT activation. LINK-A-dependent AKT hyperactivation leads to tumorigenesis and resistance to AKT inhibitors. Clinically, LINK-A overexpression is observed in patients that develop resistance to AKT inhibitors. In addition, LINK-A binds and activates kinases such us breast tumour kinase (BRK) and leucine rich-repeat kinase 2 (LRRK2). HIF1a phosphorylation results in prevention of HIF1a degradation and enhance HIF1a transcriptional activity. These molecular events promote Warburg effects [106].
LncRNA HIFAL
The lncRNA HIFAL (HIF-1α anti-sense lncRNA) is cytoplasmic lncRNA with oncogenic functions. LncRNA HIFAL is essential for maintaining HIF-1α triggered transcription under hypoxia condition and glycolysis in breast cancer cells.
The HIF-1α contributes to the Warburg observed in cancer cells, facilitating the switch from oxidative phosphorylation to glycolysis (4). Indeed, HIF-1 target genes include genes coding glycolytic receptors and enzymes, such us the glucose transporter GLUT1, the hexokinase II (HKII), the lactate dehydrogenase A (LDHA), and the pyruvate dehydrogenase kinase 1 (PDK1) [84, 107,108,109], necessary to switch the tumor cells from oxidative to anaerobic glycolysis in order to adapt to tumor hypoxic condition [110, 111] (Fig. 1B).
HIFAL is an important target of HIF-1 and can serve as a marker of HIF-1 mediated transactivation. HIFAL binds prolyl-hydroxylase 3 (PHD3) to pyruvate kinase 2 (PKM2) to stimulates PKM2/PHD3 complex migration into the nucleus, where interacting with HIF-1α facilitate its transcriptional activity. This is also relevant from a clinical point of view. Indeed, high HIFAL expression is associated with aggressive breast cancer phenotype and poor patient outcome. Furthermore, in vivo studies confirmed that HIFAL overexpression promotes tumor growth, while targeting/inhibiting both HIFAL and HIF-1α significantly reduces cancer growth [98].
Mitochondrial and oxphos lncRNAs
Mitochondrial OXPHOS has been considered as a second line metabolic pathway in cancers, while aerobic glycolysis has been assumed as a major energy resource in cancer. Yet, recent evidence indicated that OXPHOS plays also an important role in cancer energy metabolism [112]. Recently, a big effort has been done to investigate cellular organelle-associated lncRNAs and among them of particular interest played the mitochondria-associated lncRNAs.
LncRNA GAS5
GAS5 is a mitochondria-associated lncRNA very sensitive to cellular glucose levels. Previous studies have shown that it acts as DNA decoy for glucocorticoid receptor upon growth factor treatments. It also regulated insulin receptor transcription and possibly could work as sponge for miRNAs [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114]. GAS5 is found associated to mitochondria. GAS5 reduce the TCA flux. Mechanistically, GAS5 block the association of fumarate hydratase (FH), MDH2 and citrate synthase (CS), by decreasing the MDH2 acetylation (Fig. 2). Clinically, datasets showing high expression of GAS5 with low TCA flux in breast cancer patients is associated with positive clinical outcomes [101]. These results, identifying a lncRNA mitochondria-associated, suggest that organelle-associated lncRNAs might have an important role in controlling cancer development. Furthermore, it gives evidence for a paradigm shift in the current understanding of cancer metabolism, giving importance also to the TCA cycle.
Regulation of mitochondrial activity and lipid metabolism by LncRNA in breast cancer. Energy–stress induces the expression of GAS5, which in turn inhibits the interaction between of FH, MDH2 and CS. This results in the reduction of TCA flux. The lncRNA NEAT stimulate the use of free fatty acids as energy source in breast cancer. NEAT1, sponging miR107, up regulates CPT1A expression in breast cancer cells. Competing with miR34a-5p and miR204-5p NEAT1 also controls the expression of ACSL4. TCA: Tricarboxylic acid; FH: Fumarate hydratase; CS: Citrate synthase; MDH2: Malate dehydrogenase; FAO: Fatty acid oxidation; ACSL4: Acyl-CoA Synthetase Long Chain Family Member 4; CPT1: Carnitine Palmitoyltransferase 1
LncRNAs involved in lipid metabolism
The high-energy demand required for cancer cell proliferation also takes advantage of the lipid utilization. Usually, cancer cells prefer to synthetize lipids using de novo pathways. As matter of facts, usually the expression of upregulated key lipogenic enzymes is up regulated in tumours [84, 92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115]. Interestingly, recent evidences indicated that lncRNAs not only directly interact with lipid (see LINK-A) but also play a role in potentiating lipid biosynthesis using different mechanisms.
LncRNA NEAT1
The lncRNA NEAT1 (Nuclear Enriched Abundant Transcript 1) has been found deregulated in several human cancers including breast cancer. In particular, in breast cancer NEAT1 stimulates the use of free fatty acids as energy source. Indeed, in MDA-MB-231 (TNBC) and MCF7 (ER+/PR+) cancer cell lines NEAT1 by sponging miR-107, upregulates CPT1A expression [116]. CPT1A is a key enzyme for the synthesis of acylcarnitines, which are then transported into the mitochondria and its acyl groups are metabolized in the TCA cycle. In addition, competing with other miRNAs (miR34a-5p, miR204-5p) NEAT1 also controls the expression of ACSL4, essential for ER-negative breast cancer progression [117]; while competing with miR124 it form a positive loop including STAT3 to promote breast cancer progression [118] (Fig. 2). Interestingly, recent studies demonstrate that NEAT1 by sequestering the mRNAs encoding for mitochondria proteins in paraspeckles, also controls mitochondria dynamic and functions [119, 120].
Conclusions
Here, we summarized the functions of cancer metabolism-related lncRNAs, focusing on breast cancer (Tables 1 and 2). LncRNAs involvement in cancer development has opened interesting research area from basic science to clinical research. Several studies support the use of lncRNAs as diagnostic, prognostic and/or predictive biomarkers. Understanding the role of lncRNAs in metabolic reprogramming may be instrumental for their use as monitoring tools and therapeutic targets, leading to improved personalized precision breast cancer medicine.
Availability of data and materials
Available upon requests.
References
Ransohoff JD, Wei Y, Khavari PA. The functions and unique features of long intergenic non-coding RNA. Nat Rev Mol Cell Biol. 2018;19:143–57. https://doi.org/10.1038/nrm.2017.104.
Amelio I, Bernassola F, Candi E. Emerging roles of long non-coding RNAs in breast cancer biology and management. Semin Cancer Biol. 2021;72:36–45. https://doi.org/10.1016/j.semcancer.2020.06.019.
Mercer TR, Dinger ME, Mattick JS. Long non-coding RNAs: insights into functions. Nat Rev Genet. 2009;10:155–9. https://doi.org/10.1038/nrg2521.
Chandra Gupta S, Nandan Tripathi Y. Potential of long non-coding RNAs in cancer patients: from biomarkers to therapeutic targets. Int J Cancer. 2017;140:1955–67. https://doi.org/10.1002/ijc.30546.
Gibb EA, Brown CJ, Lam WL. The functional role of long non-coding RNA in human carcinomas. Mol Cancer. 2011;10:38. https://doi.org/10.1186/1476-4598-10-38.
Rinn JL, Chang HY. Genome regulation by long noncoding RNAs. Annu Rev Biochem. 2012;81:145–66. https://doi.org/10.1146/annurev-biochem-051410-092902.
Wassarman DA, Steitz JA. Interactions of small nuclear RNA’s with precursor messenger RNA during in vitro splicing. Science. 1992;257:1918–25. https://doi.org/10.1126/science.1411506.
Tollervey D, Kiss T. Function and synthesis of small nucleolar RNAs. Curr Opin Cell Biol. 1997;9:337–42. https://doi.org/10.1016/S0955-0674(97)80005-1.
Vidovic D, Huynh TT, Konda P, Dean C, Cruickshank BM, Sultan M, Coyle KM, Gujar S, Marcato P. ALDH1A3-regulated long non-coding RNA NRAD1 is a potential novel target for triple-negative breast tumors and cancer stem cells. Cell Death Differ. 2020;27:363–78. https://doi.org/10.1038/s41418-019-0362-1.
Li Z, Wang D, Lu J, Huang B, Wang Y, Dong M, Fan D, Li H, Gao Y, Hou P, Li M, Liu H, Pan Z-Q, Zheng J, Bai J. Methylation of EZH2 by PRMT1 regulates its stability and promotes breast cancer metastasis. Cell Death Differ. 2020;27:3226–42. https://doi.org/10.1038/s41418-020-00615-9.
Lu J-T, Tan C-C, Wu X-R, He R, Zhang X, Wang Q-S, Li X-Q, Zhang R, Feng Y-M. FOXF2 deficiency accelerates the visceral metastasis of basal-like breast cancer by unrestrictedly increasing TGF-β and miR-182-5p. Cell Death Differ. 2020;27:2973–87. https://doi.org/10.1038/s41418-020-0555-7.
Huang W, Yang Y, Wu J, Niu Y, Yao Y, Zhang J, Huang X, Liang S, Chen R, Chen S, Guo L. Circular RNA cESRP1 sensitises small cell lung cancer cells to chemotherapy by sponging miR-93-5p to inhibit TGF-β signalling. Cell Death Differ. 2020;27:1709–27. https://doi.org/10.1038/s41418-019-0455-x.
Wu N, Yuan Z, Du KY, Fang L, Lyu J, Zhang C, He A, Eshaghi E, Zeng K, Ma J, Du WW, Yang BB. Translation of yes-associated protein (YAP) was antagonized by its circular RNA via suppressing the assembly of the translation initiation machinery. Cell Death Differ. 2019;26:2758–73. https://doi.org/10.1038/s41418-019-0337-2.
Wang X, Li L, Zhao K, Lin Q, Li H, Xue X, Ge W, He H, Liu D, Xie H, Wu Q, Hu Y. A novel LncRNA HITT forms a regulatory loop with HIF-1α to modulate angiogenesis and tumor growth. Cell Death Differ. 2020;27:1431–46. https://doi.org/10.1038/s41418-019-0449-8.
Zhu Y, Gu L, Lin X, Cui K, Liu C, Lu B, Zhou F, Zhao Q, Shen H, Li Y. LINC00265 promotes colorectal tumorigenesis via ZMIZ2 and USP7-mediated stabilization of β-catenin. Cell Death Differ. 2020;27:1316–27. https://doi.org/10.1038/s41418-019-0417-3.
Lee HC, Kang D, Han N, Lee Y, Hwang HJ, Lee S-B, You JS, Min BS, Park HJ, Ko Y-G, Gorospe M, Lee J-S. A novel long noncoding RNA Linc-ASEN represses cellular senescence through multileveled reduction of p21 expression. Cell Death Differ. 2020;27:1844–61. https://doi.org/10.1038/s41418-019-0467-6.
Battistelli C, Sabarese G, Santangelo L, Montaldo C, Gonzalez FJ, Tripodi M, Cicchini C. The lncRNA HOTAIR transcription is controlled by HNF4α-induced chromatin topology modulation. Cell Death Differ. 2019;26:890–901. https://doi.org/10.1038/s41418-018-0170-z.
Wang D, Zhou Z, Wu E, Ouyang C, Wei G, Wang Y, He D, Cui Y, Zhang D, Chen X, Reed SH, Luo J, Chen R. LRIK interacts with the Ku70–Ku80 heterodimer enhancing the efficiency of NHEJ repair. Cell Death Differ. 2020;27:3337–53. https://doi.org/10.1038/s41418-020-0581-5.
Lu L, Chen Z, Lin X, Tian L, Su Q, An P, Li W, Wu Y, Du J, Shan H, Chiang C-M, Wang H. Inhibition of BRD4 suppresses the malignancy of breast cancer cells via regulation of Snail. Cell Death Differ. 2020;27:255–68. https://doi.org/10.1038/s41418-019-0353-2.
Pavlova NN, Thompson CB. The emerging hallmarks of cancer metabolism. Cell Metab. 2016;23:27–47. https://doi.org/10.1016/j.cmet.2015.12.006.
Global Cancer Observatory. (n.d.). https://gco.iarc.fr/.
Viale G. The current state of breast cancer classification. Ann Oncol. 2012;23:x207–10. https://doi.org/10.1093/annonc/mds326.
R. I. Cordo Russo, M. F. Chervo, S. Madera, E. H. Charreau, & P. V. Elizalde, Nuclear ErbB-2: a Novel Therapeutic Target in ErbB-2-Positive Breast Cancer? Hormones and Cancer, 10 (2019) 64–70. https://doi.org/10.1007/s12672-018-0356-3.
Dembinski R, Prasath V, Bohnak C, Siotos C, Sebai ME, Psoter K, Gani F, Canner J, Camp MS, Azizi A, Jacobs L, Habibi M. Estrogen receptor positive and progesterone receptor negative breast cancer: the role of hormone therapy. Horm Cancer. 2020;11:148–54. https://doi.org/10.1007/s12672-020-00387-1.
Pan Y, Wang X, Zhang Y, Qiao J, Sasano H, McNamara K, Zhao B, Zhang D, Fan Y, Liu L, Jia X, Liu M, Song S, Wang L. Estradiol-induced MMP-9 expression via PELP1-mediated membrane-initiated signaling in ERα-positive breast cancer cells. Horm Cancer. 2020;11:87–96. https://doi.org/10.1007/s12672-020-00380-8.
Smart E, Alejo LH, Frasor J. Cytoplasmic ERα and NFκB promote cell survival in mouse mammary cancer cell lines. Horm Cancer. 2020;11:76–86. https://doi.org/10.1007/s12672-020-00378-2.
Fowler AM, Salem K, DeGrave M, Ong IM, Rassman S, Powers GL, Kumar M, Michel CJ, Mahajan AM. Progesterone receptor gene variants in metastatic estrogen receptor positive breast cancer. Horm Cancer. 2020;11:63–75. https://doi.org/10.1007/s12672-020-00377-3.
Madera S, Chervo MF, Chiauzzi VA, Pereyra MG, Venturutti L, Izzo F, Roldán Deamicis A, Guzman P, Dupont A, Roa JC, Cenciarini ME, Barchuk S, Figurelli S, Lopez Della Vecchia D, Levit C, Lebersztein G, Anfuso F, Castiglioni T, Cortese E, Ares S, Deza EG, Gercovich FG, Proietti CJ, Schillaci R, Cordo Russo RI, Elizalde PV. Nuclear PDCD4 expression defines a subset of luminal B-like breast cancers with good prognosis. Horm Cancer. 2020;11:218–39. https://doi.org/10.1007/s12672-020-00392-4.
Lorona NC, Cook LS, Tang M-TC, Hill DA, Wiggins CL, Li CI. Recent use of oral contraceptives and risk of luminal B, triple-negative, and HER2-overexpressing breast cancer. Horm Cancer. 2019;10:71–6. https://doi.org/10.1007/s12672-019-00362-5.
Zhang J, Liu S, Li Q, Shi Y, Wu Y, Liu F, Wang S, Zaky MY, Yousuf W, Sun Q, Guo D, Wang T, Zhang Y, Wang Y, Li M, Liu H. The deubiquitylase USP2 maintains ErbB2 abundance via counteracting endocytic degradation and represents a therapeutic target in ErbB2-positive breast cancer. Cell Death Differ. 2020;27:2710–25. https://doi.org/10.1038/s41418-020-0538-8.
Viedma-Rodríguez R, Martínez-Hernández MG, Martínez-Torres DI, Baiza-Gutman LA. Epithelial mesenchymal transition and progression of breast cancer promoted by diabetes mellitus in mice are associated with increased expression of glycolytic and proteolytic enzymes. Horm Cancer. 2020;11:170–81. https://doi.org/10.1007/s12672-020-00389-z.
Oktay K, Santaliz-Casiano A, Patel M, Marino N, Storniolo AMV, Torun H, Acar B, Madak-Erdogan Z. A computational statistics approach to evaluate blood biomarkers for breast cancer risk stratification. Horm Cancer. 2020;11:17–33. https://doi.org/10.1007/s12672-019-00372-3.
Laurenzi V, Melino G. Evolution of functions within the p53/p63/p73 Family. Ann N Y Acad Sci. 2006;926:90–100. https://doi.org/10.1111/j.1749-6632.2000.tb05602.x.
Candi E, Cipollone R, Rivetti Di Val Cervo P, Gonfloni S, Melino G, Knight R. p63 in epithelial development. Cell Mol Life Sci. 2008;65:3126–33. https://doi.org/10.1007/s00018-008-8119-x.
Candi E, Agostini M, Melino G, Bernassola F. How the TP53 family proteins TP63 and TP73 contribute to tumorigenesis: regulators and effectors. Hum Mutat. 2014;35:702–14. https://doi.org/10.1002/humu.22523.
Bernassola F, Salomoni P, Oberst A, Di Como CJ, Pagano M, Melino G, Pandolfi PP. Ubiquitin-dependent degradation of p73 is inhibited by PML. J Exp Med. 2004;199:1545–57. https://doi.org/10.1084/jem.20031943.
Tomasini R, Tsuchihara K, Mak TW, Lau SK, Wilhelm M, Melino G, Iovanna JL, Tsao M, Jurisicova A, Rufini A, Tsuda C. TAp73 regulates the spindle assembly checkpoint by modulating BubR1 activity. Proc Natl Acad Sci. 2009;106:797–802. https://doi.org/10.1073/pnas.0812096106.
Candi E, Smirnov A, Panatta E, Lena AM, Novelli F, Mancini M, Viticchiè G, Piro MC, Di Daniele N, Annicchiarico-Petruzzelli M, Melino G. Metabolic pathways regulated by p63. Biochem Biophys Res Commun. 2017;482:440–4. https://doi.org/10.1016/j.bbrc.2016.10.094.
Memmi EM, Sanarico AG, Giacobbe A, Peschiaroli A, Frezza V, Cicalese A, Pisati F, Tosoni D, Zhou H, Tonon G, Antonov A, Melino G, Pelicci PG, Bernassola F. p63 sustains self-renewal of mammary cancer stem cells through regulation of Sonic Hedgehog signaling. Proc Natl Acad Sci. 2015;112:3499–504. https://doi.org/10.1073/pnas.1500762112.
Melino G, Memmi EM, Pelicci PG, Bernassola F. Maintaining epithelial stemness with p63. Sci Signal. 2015. https://doi.org/10.1126/scisignal.aaa1033.
Gatti V, Fierro C, Compagnone M, Giangrazi F, Markert EK, Bongiorno-Borbone L, Melino G, Peschiaroli A. ΔNp63 regulates the expression of hyaluronic acid-related genes in breast cancer cells. Oncogenesis. 2018;7:65. https://doi.org/10.1038/s41389-018-0073-3.
Bellomaria A, Barbato G, Melino G, Paci M, Melino S. Recognition of p63 by the E3 ligase ITCH: effect of an ectodermal dysplasia mutant. Cell Cycle. 2010;9:3754–63. https://doi.org/10.4161/cc.9.18.12933.
Viticchiè G, Agostini M, Lena AM, Mancini M, Zhou H, Zolla L, Dinsdale D, Saintigny G, Melino G, Candi E. P63 supports aerobic respiration through hexokinase II. Proceed Nat Acad Sci United States Am. 2015. https://doi.org/10.1073/pnas.1508871112.
Latina A, Viticchiè G, Lena AM, Piro MC, Annicchiarico-Petruzzelli M, Melino G, Candi E. ΔNp63 targets cytoglobin to inhibit oxidative stress-induced apoptosis in keratinocytes and lung cancer. Oncogene. 2016;35:1493–503. https://doi.org/10.1038/onc.2015.222.
Cassandri M, Butera A, Amelio I, Lena AM, Montanaro M, Mauriello A, Anemona L, Candi E, Knight RA, Agostini M, Melino G. ZNF750 represses breast cancer invasion via epigenetic control of prometastatic genes. Oncogene. 2020;39:4331–43. https://doi.org/10.1038/s41388-020-1277-5.
Butera A, Cassandri M, Rugolo F, Agostini M, Melino G. The ZNF750–RAC1 axis as potential prognostic factor for breast cancer. Cell Death Discov. 2020. https://doi.org/10.1038/s41420-020-00371-2.
Vikhreva P, Petrova V, Gokbulut T, Pestlikis I, Mancini M, Di Daniele N, Knight RA, Melino G, Amelio I. TAp73 upregulates IL-1β in cancer cells: Potential biomarker in lung and breast cancer? Biochem Biophys Res Commun. 2017;482:498–505. https://doi.org/10.1016/j.bbrc.2016.10.085.
Marini A, Lena AM, Panatta E, Ivan C, Han L, Liang H, Annicchiarico-Petruzzelli M, Di Daniele N, Calin GA, Candi E, Melino G. Ultraconserved long non-coding RNA uc63 in breast cancer. Oncotarget. 2017;8:35669–80. https://doi.org/10.18632/oncotarget.10572.
Amelio I, Cutruzzolá F, Antonov A, Agostini M, Melino G. Serine and glycine metabolism in cancer. Trends Biochem Sci. 2014;39:191–8. https://doi.org/10.1016/J.TIBS.2014.02.004.
Amelio I, Melino G. The p53 family and the hypoxia-inducible factors (HIFs): determinants of cancer progression. Trends Biochem Sci. 2015;40:425–34. https://doi.org/10.1016/j.tibs.2015.04.007.
Mauretti A, Neri A, Kossover O, Seliktar D, Di Nardo P, Melino S. Design of a novel composite H 2 S-releasing hydrogel for cardiac tissue repair. Macromol Biosci. 2016;16:847–58. https://doi.org/10.1002/mabi.201500430.
Sabelli R, Iorio E, De Martino A, Podo F, Ricci A, Viticchiè G, Rotilio G, Paci M, Melino S. Rhodanese-thioredoxin system and allyl sulfur compounds. FEBS J. 2008;275:3884–99. https://doi.org/10.1111/j.1742-4658.2008.06535.x.
Lamastra FR, De Angelis R, Antonucci A, Salvatori D, Prosposito P, Casalboni M, Congestri R, Melino S. Polymer composite random lasers based on diatom frustules as scatterers. RSC Adv. 2014;4:61809–16.
Cairns RA, Harris IS, Mak TW. Regulation of cancer cell metabolism. Nat Rev Cancer. 2011;11:85–95. https://doi.org/10.1038/nrc2981.
Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the Metabolic requirements of cell proliferation. Science. 2009;324:1029–33. https://doi.org/10.1126/science.1160809.
Liberti MV, Locasale JW. The Warburg effect: how does it benefit cancer cells? Trends Biochem Sci. 2016;41:211–8. https://doi.org/10.1016/j.tibs.2015.12.001.
Du Y, Wei N, Ma R, Jiang S-H, Song D. Long noncoding RNA MIR210HG promotes the Warburg effect and Tumor growth by enhancing HIF-1α translation in triple-negative breast cancer. Front Oncol. 2020. https://doi.org/10.3389/fonc.2020.580176.
Jing Y-Y, Cai F-F, Zhang L, Han J, Yang L, Tang F, Li Y-B, Chang J-F, Sun F, Yang X-M, Sun F-L, Chen S. Epigenetic regulation of the Warburg effect by H2B monoubiquitination. Cell Death Differ. 2020;27:1660–76. https://doi.org/10.1038/s41418-019-0450-2.
Yang J, AlTahan A, Jones DT, Buffa FM, Bridges E, Interiano RB, Qu C, Vogt N, Li JL, Baban D, Ragoussis J, Nicholson R, Davidoff AM, Harris AL. Estrogen receptor-α directly regulates the hypoxiainducible factor 1 pathway associated with antiestrogen response in breast cancer. Proc Natl Acad Sci USA. 2015;112:15172–7. https://doi.org/10.1073/PNAS.1422015112/-/DCSUPPLEMENTAL/PNAS.1422015112.ST01.DOCX.
Semenza GL. HIF-1 mediates metabolic responses to intratumoral hypoxia and oncogenic mutations. J Clin Investig. 2013;123:3664–71. https://doi.org/10.1172/JCI67230.
Pelicano H, Zhang W, Liu J, Hammoudi N, Dai J, Xu R-H, Pusztai L, Huang P. Mitochondrial dysfunction in some triple-negative breast cancer cell lines: role of mTOR pathway and therapeutic potential. Breast Cancer Res. 2014;16:434. https://doi.org/10.1186/s13058-014-0434-6.
Timmerman LA, Holton T, Yuneva M, Louie RJ, Padró M, Daemen A, Hu M, Chan DA, Ethier SP, van’t Veer LJ, Polyak K, McCormick F, Gray JW. Glutamine Sensitivity analysis identifies the xCT Antiporter as a Common triple-negative breast tumor therapeutic target. Cancer Cell. 2013;24:450–65. https://doi.org/10.1016/j.ccr.2013.08.020.
Choi J, Jung W-H, Koo JS. Metabolism-related proteins are differentially expressed according to the molecular subtype of invasive breast cancer defined by surrogate immunohistochemistry. Pathobiology. 2013;80:41–52. https://doi.org/10.1159/000339513.
Estrella V, Chen T, Lloyd M, Wojtkowiak J, Cornnell HH, Ibrahim-Hashim A, Bailey K, Balagurunathan Y, Rothberg JM, Sloane BF, Johnson J, Gatenby RA, Gillies RJ. Acidity generated by the tumor microenvironment drives local invasion. Can Res. 2013;73:1524–35. https://doi.org/10.1158/0008-5472.CAN-12-2796.
Lanning NJ, Castle JP, Singh SJ, Leon AN, Tovar EA, Sanghera A, MacKeigan JP, Filipp FV, Graveel CR. Metabolic profiling of triple-negative breast cancer cells reveals metabolic vulnerabilities. Cancer Metab. 2017;5:6. https://doi.org/10.1186/s40170-017-0168-x.
Wang G, Xu Z, Wang C, Yao F, Li J, Chen C, Sun S. Differential phosphofructokinase-1 isoenzyme patterns associated with glycolytic efficiency in human breast cancer and paracancer tissues. Oncol Lett. 2013;6:1701–6. https://doi.org/10.3892/ol.2013.1599.
Brown RS, Goodman TM, Zasadny KR, Greenson JK, Wahl RL. Expression of hexokinase II and Glut-1 in untreated human breast cancer. Nucl Med Biol. 2002;29:443–53. https://doi.org/10.1016/S0969-8051(02)00288-3.
Saunier E, Benelli C, Bortoli S. The pyruvate dehydrogenase complex in cancer: an old metabolic gatekeeper regulated by new pathways and pharmacological agents. Int J Cancer. 2016;138:809–17. https://doi.org/10.1002/ijc.29564.
Visvader JE, Lindeman GJ. Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat Rev Cancer. 2008;8:755–68. https://doi.org/10.1038/nrc2499.
Yang F, Xu J, Tang L, Guan X. Breast cancer stem cell: the roles and therapeutic implications. Cell Mol Life Sci. 2017;74:951–66. https://doi.org/10.1007/s00018-016-2334-7.
Peng F, Wang J-H, Fan W-J, Meng Y-T, Li M-M, Li T-T, Cui B, Wang H-F, Zhao Y, An F, Guo T, Liu X-F, Zhang L, Lv L, Lv D-K, Xu L-Z, Xie J-J, Lin W-X, Lam EW-F, Xu J, Liu Q. Glycolysis gatekeeper PDK1 reprograms breast cancer stem cells under hypoxia. Oncogene. 2018;37:1062–74. https://doi.org/10.1038/onc.2017.368.
Wang K, Zhang Z, Tsai H, Liu Y, Gao J, Wang M, Song L, Cao X, Xu Z, Chen H, Gong A, Wang D, Cheng F, Zhu H. Branched-chain amino acid aminotransferase 2 regulates ferroptotic cell death in cancer cells. Cell Death Differ. 2021;28:1222–36. https://doi.org/10.1038/s41418-020-00644-4.
Siddiqui A, Gollavilli PN, Schwab A, Vazakidou ME, Ersan PG, Ramakrishnan M, Pluim D, Coggins S, Saatci O, Annaratone L, Schellens JHM, Kim B, Asangani IA, Rasheed SAK, Marchiò C, Sahin O, Ceppi P. Thymidylate synthase maintains the de-differentiated state of triple negative breast cancers. Cell Death Differ. 2019;26:2223–36. https://doi.org/10.1038/s41418-019-0289-6.
Khosla S, Oursler MJ, Monroe DG. Estrogen and the skeleton. Trends Endocrinol Metab. 2012;23:576–81. https://doi.org/10.1016/j.tem.2012.03.008.
Antonov A, Agostini M, Morello M, Minieri M, Melino G, Amelio I. Bioinformatics analysis of the serine and glycine pathway in cancer cells. Oncotarget. 2014;5:11004–13. https://doi.org/10.18632/oncotarget.2668.
Locasale JW, Grassian AR, Melman T, Lyssiotis CA, Mattaini KR, Bass AJ, Heffron G, Metallo CM, Muranen T, Sharfi H, Sasaki AT, Anastasiou D, Mullarky E, Vokes NI, Sasaki M, Beroukhim R, Stephanopoulos G, Ligon AH, Meyerson M, Richardson AL, Chin L, Wagner G, Asara JM, Brugge JS, Cantley LC, Vander Heiden MG. Phosphoglycerate dehydrogenase diverts glycolytic flux and contributes to oncogenesis. Nat Genet. 2011;43:869–74.
Possemato R, Marks KM, Shaul YD, Pacold ME, Kim D, Birsoy K, Sethumadhavan S, Woo H-K, Jang HG, Jha AK, Chen WW, Barrett FG, Stransky N, Tsun Z-Y, Cowley GS, Barretina J, Kalaany NY, Hsu PP, Ottina K, Chan AM, Yuan B, Garraway LA, Root DE, Mino-Kenudson M, Brachtel EF, Driggers EM, Sabatini DM. Functional genomics reveal that the serine synthesis pathway is essential in breast cancer. Nature. 2011;476:346–50. https://doi.org/10.1038/nature10350.
Scheibye-Knudsen M, Fang EF, Croteau DL, Wilson DM, Bohr VA. Protecting the mitochondrial powerhouse. Trends Cell Biol. 2015;25:158–70. https://doi.org/10.1016/j.tcb.2014.11.002.
Vyas S, Zaganjor E, Haigis MC. Mitochondria and Cancer. Cell. 2016;166:555–66. https://doi.org/10.1016/j.cell.2016.07.002.
Avagliano A, Ruocco MR, Aliotta F, Belviso I, Accurso A, Masone S, Montagnani S, Arcucci A. Mitochondrial flexibility of breast cancers: a growth advantage and a therapeutic opportunity. Cells. 2019;8:401. https://doi.org/10.3390/cells8050401.
Lunetti P, Di Giacomo M, Vergara D, De Domenico S, Maffia M, Zara V, Capobianco L, Ferramosca A. Metabolic reprogramming in breast cancer results in distinct mitochondrial bioenergetics between luminal and basal subtypes. FEBS J. 2019;286:688–709. https://doi.org/10.1111/febs.14756.
Kamarajugadda S, Stemboroski L, Cai Q, Simpson NE, Nayak S, Tan M, Lu J. Glucose oxidation modulates anoikis and tumor metastasis. Mol Cell Biol. 2012;32:1893–907. https://doi.org/10.1128/MCB.06248-11.
Elia I, Doglioni G, Fendt S-M. Metabolic hallmarks of metastasis formation. Trends Cell Biol. 2018;28:673–84. https://doi.org/10.1016/j.tcb.2018.04.002.
Luo W, Hu H, Chang R, Zhong J, Knabel M, O’Meally R, Cole RN, Pandey A, Semenza GL. Pyruvate kinase M2 is a PHD3-stimulated coactivator for hypoxia-inducible factor 1. Cell. 2011;145:732–44. https://doi.org/10.1016/j.cell.2011.03.054.
Semenza GL. Defining the role of hypoxia-inducible factor 1 in cancer biology and therapeutics. Oncogene. 2010;29:625–34. https://doi.org/10.1038/onc.2009.441.
LeBleu VS, O’Connell JT, Gonzalez Herrera KN, Wikman H, Pantel K, Haigis MC, de Carvalho FM, Damascena A, Domingos Chinen LT, Rocha RM, Asara JM, Kalluri R. PGC-1α mediates mitochondrial biogenesis and oxidative phosphorylation in cancer cells to promote metastasis. Nature Cell Biology. 2014;16:992–1003. https://doi.org/10.1038/ncb3039.
Andrzejewski S, Klimcakova E, Johnson RM, Tabariès S, Annis MG, McGuirk S, Northey JJ, Chénard V, Sriram U, Papadopoli DJ, Siegel PM, St-Pierre J. PGC-1α promotes breast cancer metastasis and confers bioenergetic flexibility against metabolic drugs. Cell Metab. 2017;26:778-787.e5. https://doi.org/10.1016/j.cmet.2017.09.006.
Zhu M, Wang X, Gu Y, Wang F, Li L, Qiu X. MEG3 overexpression inhibits the tumorigenesis of breast cancer by downregulating miR-21 through the PI3K/Akt pathway. Arch Biochem Biophys. 2019;661:22–30. https://doi.org/10.1016/j.abb.2018.10.021.
Rysman E, Brusselmans K, Scheys K, Timmermans L, Derua R, Munck S, Van Veldhoven PP, Waltregny D, Daniëls VW, Machiels J, Vanderhoydonc F, Smans K, Waelkens E, Verhoeven G, Swinnen JV. De novo lipogenesis protects cancer cells from free radicals and chemotherapeutics by promoting membrane lipid saturation. Can Res. 2010;70:8117–26. https://doi.org/10.1158/0008-5472.CAN-09-3871.
Hilvo M, Denkert C, Lehtinen L, Müller B, Brockmöller S, Seppänen-Laakso T, Budczies J, Bucher E, Yetukuri L, Castillo S, Berg E, Nygren H, Sysi-Aho M, Griffin JL, Fiehn O, Loibl S, Richter-Ehrenstein C, Radke C, Hyötyläinen T, Kallioniemi O, Iljin K, Orešič M. Novel theranostic opportunities offered by characterization of altered membrane lipid metabolism in breast cancer progression. Can Res. 2011;71:3236–45. https://doi.org/10.1158/0008-5472.CAN-10-3894.
Ménard S, Fortis S, Castiglioni F, Agresti R, Balsari A. HER2 as a prognostic factor in breast cancer. Oncology. 2001;61:67–72. https://doi.org/10.1159/000055404.
Menendez JA, Lupu R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat Rev Cancer. 2007;7:763–77. https://doi.org/10.1038/nrc2222.
Cruz ALS, Barreto E de A, Fazolini NPB, Viola JPB, Bozza PT. Lipid droplets: platforms with multiple functions in cancer hallmarks. Cell Death Dis. 2020;11:105. https://doi.org/10.1038/s41419-020-2297-3.
de Gonzalo-Calvo D, López-Vilaró L, Nasarre L, Perez-Olabarria M, Vázquez T, Escuin D, Badimon L, Barnadas A, Lerma E, Llorente-Cortés V. Intratumor cholesteryl ester accumulation is associated with human breast cancer proliferation and aggressive potential: a molecular and clinicopathological study. BMC Cancer. 2015;15:460. https://doi.org/10.1186/s12885-015-1469-5.
Guan B, Wang H, Cao S, Rao Q, Wang Y, Zhu Y, Shi Q, Yin H, Wang X, Zhou X. Lipid-rich carcinoma of the breast clinicopathologic analysis of 17 cases. Ann Diagn Pathol. 2011;15:225–32. https://doi.org/10.1016/j.anndiagpath.2010.10.006.
Mellick AS, Day CJ, Weinstein SR, Griffiths LR, Morrison NA. Differential gene expression in breast cancer cell lines and stroma-tumor differences in microdissected breast cancer biopsies revealed by display array analysis. Int J Cancer. 2002;100:172–80. https://doi.org/10.1002/ijc.10451.
Moritani S, Ichihara S, Hasegawa M, Endo T, Oiwa M, Shiraiwa M, Nishida C, Morita T, Sato Y, Hayashi T, Kato A. Intracytoplasmic lipid accumulation in apocrine carcinoma of the breast evaluated with adipophilin immunoreactivity. Am J Surg Pathol. 2011;35:861–7. https://doi.org/10.1097/PAS.0b013e31821a7f3e.
Zheng F, Chen J, Zhang X, Wang Z, Chen J, Lin X, Huang H, Fu W, Liang J, Wu W, Li B, Yao H, Hu H, Song E. The HIF-1α antisense long non-coding RNA drives a positive feedback loop of HIF-1α mediated transactivation and glycolysis. Nature Commun. 2021. https://doi.org/10.1038/s41467-021-21535-3.
Zheng X, Han H, Liu G, Ma Y, Pan R, Sang L, Li R, Yang L, Marks JR, Wang W, Lin A. Lnc RNA wires up Hippo and Hedgehog signaling to reprogramme glucose metabolism. EMBO J. 2017;36:3325–35. https://doi.org/10.15252/embj.201797609.
Lin A, Hu Q, Li C, Xing Z, Ma G, Wang C, Li J, Ye Y, Yao J, Liang K, Wang S, Park PK, Marks JR, Zhou Y, Zhou J, Hung M-C, Liang H, Hu Z, Shen H, Hawke DH, Han L, Zhou Y, Lin C, Yang L. The LINK-A lncRNA interacts with PtdIns(3,4,5)P3 to hyperactivate AKT and confer resistance to AKT inhibitors. Nat Cell Biol. 2017;19:238–51. https://doi.org/10.1038/ncb3473.
Sang L, Ju H, Yang Z, Ge Q, Zhang Z, Liu F, Yang L, Gong H, Shi C, Qu L, Chen H, Wu M, Chen H, Li R, Zhuang Q, Piao H, Yan Q, Yu W, Wang L, Shao J, Liu J, Wang W, Zhou T, Lin A. Mitochondrial long non-coding RNA GAS5 tunes TCA metabolism in response to nutrient stress. Nat Metab. 2021;3:90–106. https://doi.org/10.1038/s42255-020-00325-z.
Takeiwa T, Ikeda K, Mitobe Y, Horie-Inoue K, Inoue S. Long noncoding RNAs involved in the endocrine therapy resistance of breast cancer. Cancers. 2020;12:1424. https://doi.org/10.3390/cancers12061424.
Mitobe Y, Takayama K, Horie-Inoue K, Inoue S. Prostate cancer-associated lncRNAs. Cancer Lett. 2018;418:159–66. https://doi.org/10.1016/j.canlet.2018.01.012.
Xing Z, Lin A, Li C, Liang K, Wang S, Liu Y, Park PK, Qin L, Wei Y, Hawke DH, Hung M-C, Lin C, Yang L. lncRNA Directs cooperative epigenetic regulation downstream of chemokine signals. Cell. 2014;159:1110–25. https://doi.org/10.1016/j.cell.2014.10.013.
Xing Z, Zhang Y, Liang K, Yan L, Xiang Y, Li C, Hu Q, Jin F, Putluri V, Putluri N, Coarfa C, Sreekumar A, Park PK, Nguyen TK, Wang S, Zhou J, Zhou Y, Marks JR, Hawke DH, Hung M-C, Yang L, Han L, Ying H, Lin C. Expression of long noncoding RNA YIYA promotes glycolysis in breast cancer. Can Res. 2018;78:4524–32. https://doi.org/10.1158/0008-5472.CAN-17-0385.
Lin A, Li C, Xing Z, Hu Q, Liang K, Han L, Wang C, Hawke DH, Wang S, Zhang Y, Wei Y, Ma G, Park PK, Zhou J, Zhou Y, Hu Z, Zhou Y, Marks JR, Liang H, Hung M-C, Lin C, Yang L. The LINK-A lncRNA activates normoxic HIF1α signalling in triple-negative breast cancer. Nat Cell Biol. 2016;18:213–24. https://doi.org/10.1038/ncb3295.
Wheaton WW, Chandel NS. Hypoxia. 2. Hypoxia regulates cellular metabolism. Am J Physiol Cell Physiol. 2011. https://doi.org/10.1152/ajpcell.00485.2010.
Masoud GN, Li W. HIF-1α pathway: role, regulation and intervention for cancer therapy. Acta Pharmaceutica Sinica B. 2015;5:378–89. https://doi.org/10.1016/j.apsb.2015.05.007.
Mathupala SP, Rempel A, Pedersen PL. Glucose catabolism in cancer cells. J Biol Chem. 2001;276:43407–12. https://doi.org/10.1074/jbc.M108181200.
Wheaton WW, Chandel NS. Hypoxia. 2. Hypoxia regulates cellular metabolism. Am J Physiol Cell Physiol. 2011;300:C385–93. https://doi.org/10.1152/ajpcell.00485.2010.
Seagroves TN, Ryan HE, Lu H, Wouters BG, Knapp M, Thibault P, Laderoute K, Johnson RS. Transcription factor HIF-1 is a necessary mediator of the pasteur effect in mammalian cells. Mol Cell Biol. 2001;21:3436–44. https://doi.org/10.1128/MCB.21.10.3436-3444.2001.
Ashton TM, McKenna WG, Kunz-Schughart LA, Higgins GS. Oxidative phosphorylation as an emerging target in cancer therapy. Clin Cancer Res. 2018;24:2482–90. https://doi.org/10.1158/1078-0432.CCR-17-3070.
Kino T, Hurt DE, Ichijo T, Nader N, Chrousos GP. Noncoding RNA Gas5 is a growth arrest– and starvation-associated repressor of the glucocorticoid receptor. Sci Signal. 2010. https://doi.org/10.1126/scisignal.2000568.
Zhao H, Yu H, Zheng J, Ning N, Tang F, Yang Y, Wang Y. Lowly-expressed lncRNA GAS5 facilitates progression of ovarian cancer through targeting miR-196-5p and thereby regulating HOXA5. Gynecol Oncol. 2018;151:345–55. https://doi.org/10.1016/j.ygyno.2018.08.032.
Chavarro JE, Kenfield SA, Stampfer MJ, Loda M, Campos H, Sesso HD, Ma J. Blood levels of saturated and monounsaturated fatty acids as markers of de novo lipogenesis and risk of prostate cancer. Am J Epidemiol. 2013;178:1246–55. https://doi.org/10.1093/aje/kwt136.
Xiong Y, Liu Z, Li Z, Wang S, Shen N, Xin Y, Huang T. Long non-coding RNA nuclear paraspeckle assembly transcript 1 interacts with microRNA-107 to modulate breast cancer growth and metastasis by targeting carnitine palmitoyltransferase-1. Int J Oncol. 2019;55:1125–36. https://doi.org/10.3892/ijo.2019.4869.
Jiang X, Guo S, Zhang Y, Zhao Y, Li X, Jia Y, Xu Y, Ma B. LncRNA NEAT1 promotes docetaxel resistance in prostate cancer by regulating ACSL4 via sponging miR-34a-5p and miR-204-5p. Cell Signal. 2020;65: 109422. https://doi.org/10.1016/j.cellsig.2019.109422.
Pang Y, Wu J, Li X, Wang C, Wang M, Liu J, Yang G. NEAT1/miR-124/STAT3 feedback loop promotes breast cancer progression. Int J Oncol. 2019;55:745–54. https://doi.org/10.3892/ijo.2019.4841.
Alvarez-Paggi D, Hannibal L, Castro MA, Oviedo-Rouco S, Demicheli V, Tórtora V, Tomasina F, Radi R, Murgida DH. Multifunctional cytochrome c: Learning new tricks from an old dog. Chem Rev. 2017;117:13382–460. https://doi.org/10.1021/acs.chemrev.7b00257.
Wang Y, Hu S-B, Wang M-R, Yao R-W, Wu D, Yang L, Chen L-L. Genome-wide screening of NEAT1 regulators reveals cross-regulation between paraspeckles and mitochondria. Nat Cell Biol. 2018;20:1145–58. https://doi.org/10.1038/s41556-018-0204-2.
Godinho M, Meijer D, Setyono-Han B, Dorssers LCJ, Van Agthoven T. Characterization of BCAR4, a novel oncogene causing endocrine resistance in human breast cancer cells. J Cell Physiol. 2011;226:1741–9. https://doi.org/10.1002/jcp.22503.
Xu S, Kong D, Chen Q, Ping Y, Pang D. Oncogenic long noncoding RNA landscape in breast cancer. Mol Cancer. 2017;16:129. https://doi.org/10.1186/s12943-017-0696-6.
Brannan CI, Dees EC, Ingram RS, Tilghman SM. The product of the H19 gene may function as an RNA. Mol Cell Biol. 1990;10:28–36. https://doi.org/10.1128/mcb.10.1.28-36.1990.
Huarte M, Guttman M, Feldser D, Garber M, Koziol MJ, Kenzelmann-Broz D, Khalil AM, Zuk O, Amit I, Rabani M, Attardi LD, Regev A, Lander ES, Jacks T, Rinn JL. A large intergenic noncoding RNA induced by p53 mediates global gene repression in the p53 response. Cell. 2010;142:409–19. https://doi.org/10.1016/j.cell.2010.06.040.
Yang F, Yi F, Zheng Z, Ling Z, Ding J, Guo J, Mao W, Wang X, Wang X, Ding X, Liang Z, Du Q. Characterization of a carcinogenesis-associated long non-coding RNA. RNA Biol. 2012;9:110–6. https://doi.org/10.4161/rna.9.1.18332.
Zhang X, Rice K, Wang Y, Chen W, Zhong Y, Nakayama Y, Zhou Y, Klibanski A. Maternally expressed gene 3 (MEG3) noncoding ribonucleic acid: isoform structure, expression, and functions. Endocrinol. 2010;151:939–47. https://doi.org/10.1210/en.2009-0657.
Srikantan V, Zou Z, Petrovics G, Xu L, Augustus M, Davis L, Livezey JR, Connell T, Sesterhenn IA, Yoshino K, Buzard GS, Mostofi FK, McLeod DG, Moul JW, Srivastava S. PCGEM1, a prostate-specific gene, is overexpressed in prostate cancer. Proc Natl Acad Sci. 2000;97:12216–21. https://doi.org/10.1073/pnas.97.22.12216.
Wang F, Li X, Xie X, Zhao L, Chen W. UCA1, a non-protein-coding RNA up-regulated in bladder carcinoma and embryo, influencing cell growth and promoting invasion. FEBS Lett. 2008;582:1919–27. https://doi.org/10.1016/j.febslet.2008.05.012.
Li Y-H, Hu Y-Q, Wang S-C, Li Y, Chen D-M. LncRNA SNHG5: a new budding star in human cancers. Gene. 2020;749: 144724. https://doi.org/10.1016/j.gene.2020.144724.
Hamilton MJ, Girke T, Martinez E. Global isoform-specific transcript alterations and deregulated networks in clear cell renal cell carcinoma. Oncotarget. 2018;9:23670–80. https://doi.org/10.18632/oncotarget.25330.
Li J, Jiang X, Li Z, Huang L, Zhou Y, Liu Y, Cui Y. Long noncoding RNA GHET1 in human cancer. Clin Chim Acta. 2019;488:111–5. https://doi.org/10.1016/j.cca.2018.11.007.
Zheng F, Chen J, Zhang X, Wang Z, Chen J, Lin X, Huang H, Fu W, Liang J, Wu W, Li B, Yao H, Hu H, Song E. The HIF-1α antisense long non-coding RNA drives a positive feedback loop of HIF-1α mediated transactivation and glycolysis. Nat Commun. 2021;12:1341. https://doi.org/10.1038/s41467-021-21535-3.
Lin J, Zhang X, Xue C, Zhang H, Shashaty MGS, Gosai SJ, Meyer N, Grazioli A, Hinkle C, Caughey J, Li W, Susztak K, Gregory BD, Li M, Reilly MP. The long noncoding RNA landscape in hypoxic and inflammatory renal epithelial injury. Am J Physiol-Renal Physiol. 2015;309:F901–13. https://doi.org/10.1152/ajprenal.00290.2015.
Cui S, Yang X, Zhang L, Zhao Y, Yan W. LncRNA MAFG-AS1 promotes the progression of colorectal cancer by sponging miR-147b and activation of NDUFA4. Biochem Biophys Res Commun. 2018;506:251–8. https://doi.org/10.1016/j.bbrc.2018.10.112.
Zhang J, Fan D, Jian Z, Chen GG, Lai PBS. Cancer specific long noncoding RNAs show differential expression patterns and competing endogenous RNA potential in hepatocellular carcinoma. PLoS One. 2015;10: e0141042. https://doi.org/10.1371/journal.pone.0141042.
Hutchinson JN, Ensminger AW, Clemson CM, Lynch CR, Lawrence JB, Chess A. A screen for nuclear transcripts identifies two linked noncoding RNAs associated with SC35 splicing domains. BMC Genomics. 2007;8:39. https://doi.org/10.1186/1471-2164-8-39.
Liu C, Wu H-T, Zhu N, Shi Y-N, Liu Z, Ao B-X, Liao D-F, Zheng X-L, Qin L. Steroid receptor RNA activator: biologic function and role in disease. Clin Chim Acta. 2016;459:137–46. https://doi.org/10.1016/j.cca.2016.06.004.
Hube F, Guo J, Chooniedass-Kothari S, Cooper C, Hamedani MK, Dibrov AA, Blanchard AAA, Wang X, Deng G, Myal Y, Leygue E. Alternative splicing of the first intron of the steroid receptor RNA activator (SRA) participates in the generation of coding and noncoding RNA isoforms in breast cancer cell lines. DNA Cell Biol. 2006;25:418–28. https://doi.org/10.1089/dna.2006.25.418.
Cheng Y-C, Su L-Y, Chen L-H, Lu T-P, Chuang EY, Tsai M-H, Chuang L-L, Lai L-C. Regulatory mechanisms and functional roles of hypoxia-induced long non-coding RNA MTORT1 in breast cancer cells. Front Oncol. 2021. https://doi.org/10.3389/fonc.2021.663114.
Özgür E, Mert U, Isin M, Okutan M, Dalay N, Gezer U. Differential expression of long non-coding RNAs during genotoxic stress-induced apoptosis in HeLa and MCF-7 cells. Clin Exp Med. 2013;13:119–26. https://doi.org/10.1007/s10238-012-0181-x.
Ma F, Liu X, Zhou S, Li W, Liu C, Chadwick M, Qian C. Long non-coding RNA FGF13-AS1 inhibits glycolysis and stemness properties of breast cancer cells through FGF13-AS1/IGF2BPs/Myc feedback loop. Cancer Lett. 2019;450:63–75. https://doi.org/10.1016/j.canlet.2019.02.008.
Yang F, Zhang H, Mei Y, Wu M. Reciprocal regulation of HIF-1α and LincRNA-p21 modulates the Warburg effect. Mol Cell. 2014;53:88–100. https://doi.org/10.1016/j.molcel.2013.11.004.
Mota MSV, Jackson WP, Bailey SK, Vayalil P, Landar A, Rostas JW, Mulekar MS, Samant RS, Shevde LA. Deficiency of tumor suppressor Merlin facilitates metabolic adaptation by co-operative engagement of SMAD-Hippo signaling in breast cancer. Carcinogenesis. 2018;39:1165–75. https://doi.org/10.1093/carcin/bgy078.
Huang S-L, Huang Z-C, Zhang C-J, Xie J, Lei S-S, Wu Y-Q, Fan P-Z. LncRNA SNHG5 promotes the glycolysis and proliferation of breast cancer cell through regulating BACH1 via targeting miR-299. Breast Cancer. 2021. https://doi.org/10.1007/s12282-021-01281-6.
Fang K, Xu Z-J, Jiang S-X, Tang D-S, Yan C-S, Deng Y-Y, Zhao F-Y. lncRNA FGD5-AS1 promotes breast cancer progression by regulating the hsa-miR-195-5p/NUAK2 axis. Mol Med Rep. 2021;23:460. https://doi.org/10.3892/mmr.2021.12099.
Wang Y, Liu S. LncRNA GHET1 Promotes hypoxia-induced glycolysis, proliferation, and invasion in triple-negative breast cancer through the hippo/YAP Signaling pathway. Front Cell Develop Biol. 2021. https://doi.org/10.3389/fcell.2021.643515.
Ding M, Fu Y, Guo F, Chen H, Fu X, Tan W, Zhang H. Long non-coding RNA MAFG-AS1 knockdown blocks malignant progression in breast cancer cells by inactivating JAK2/STAT3 signaling pathway via MAFG-AS1/miR-3196/TFAP2A axis - PubMed. Int J Clin Exp Pathol. 2020;13(10):2455–73.
Li Y, Li H, Wang W, Yu X, Xu Q. LINC00346 regulates glycolysis by modulation of glucose transporter 1 in breast cancer cells. Mol Cell Probes. 2020;54: 101667. https://doi.org/10.1016/j.mcp.2020.101667.
Acknowledgements
This work has been supported by the Associazione Italiana per la Ricerca contro il Cancro (AIRC) to EC (AIRC IG22206; 2019-2023) and Italian Ministry of Health and IDI-IRCCS (RF-2019-1236888820473) to EC. We apologies with authors if we did not cite their articles, this was due to space limit.
Author information
Authors and Affiliations
Contributions
MA and MM wrote the first draft, EC revised the draft, EC conceived the article. All authors read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Agostini, M., Mancini, M. & Candi, E. Long non-coding RNAs affecting cell metabolism in cancer. Biol Direct 17, 26 (2022). https://doi.org/10.1186/s13062-022-00341-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13062-022-00341-x