Abstract
Background
In pre-clinical studies, the anti-tumor activity of T-DM1 was enhanced when combined with taxanes or pertuzumab. This phase 1b/2a study evaluated the safety/tolerability of T-DM1 + paclitaxel ± pertuzumab in HER2-positive advanced breast cancer.
Methods
In phase 1b (n = 60), a 3 + 3 dose-escalation approach was used to determine the maximum tolerated dose (MTD) of T-DM1 + paclitaxel ± pertuzumab. The primary objective of phase 2a was feasibility, with 44 patients randomized to T-DM1 + paclitaxel ± pertuzumab at the MTD identified in phase 1b.
Results
The MTD was T-DM1 3.6 mg/kg every three weeks (q3w) or 2.4 mg/kg weekly + paclitaxel 80 mg/m2 weekly ± pertuzumab 840 mg loading dose followed by 420 mg q3w. Phase 2a patients had received a median of 5.0 (range: 0–10) prior therapies for advanced cancer. In phase 2a, 51.2 % received ≥12 paclitaxel doses within 15 weeks, and 14.0 % received 12 paclitaxel doses by week 12. Common all-grade adverse events (AEs) were peripheral neuropathy (90.9 %) and fatigue (79.5 %). A total of 77.3 % experienced grade ≥3 AEs, most commonly neutropenia (25.0 %) and peripheral neuropathy (18.2 %). Among the 42 phase 2a patients with measurable disease, the objective response rate (ORR) was 50.0 % (95 % confidence interval (CI) 34.6–65.4); the clinical benefit rate (CBR) was 56.8 % (95 % CI 41.6–71.0). No pharmacokinetic interactions were observed between T-DM1 and paclitaxel.
Conclusions
This regimen showed clinical activity. Although there is potential for paclitaxel to be added to T-DM1 ± pertuzumab, peripheral neuropathy was common in this heavily pretreated population.
Trial registration
ClinicalTrials.gov NCT00951665. Registered August 3, 2009.
Similar content being viewed by others
Background
Trastuzumab emtansine (T-DM1) is a human epidermal growth factor receptor 2 (HER2)–targeted antibody–drug conjugate composed of the humanized monoclonal antibody trastuzumab conjugated via a stable linker to the cytotoxic microtubule polymerization inhibitor DM1 [1]. In the phase 3 EMILIA trial of patients with metastatic breast cancer (MBC) previously treated with trastuzumab and a taxane, single-agent T-DM1 was associated with statistically significantly improved progression-free survival (PFS; 9.6 vs. 6.4 months; hazard ratio [HR], 0.65; P < 0.001) and overall survival (OS; 30.9 vs. 25.1 months; HR, 0.68; P < 0.001) relative to lapatinib plus capecitabine [2]. In the phase 3 TH3RESA study of patients with MBC previously administered ≥ 2 HER2-targeted therapies in the advanced disease setting and a taxane in any setting, single-agent T-DM1 led to a statistically significant improvement in PFS vs. treatment of physician’s choice (6.2 vs. 3.3 months; HR, 0.53; P < 0.0001) [3]. In a phase 2 trial of first-line MBC, T-DM1 was associated with significantly longer PFS than trastuzumab + docetaxel (14.2 vs. 9.2 months; HR, 0.59; P = 0.035) [4].
Taxanes are mainstay chemotherapy for the treatment of breast cancer [5], and paclitaxel is used in combination with trastuzumab for HER2-positive MBC. Pertuzumab is a humanized monoclonal antibody that recognizes a binding domain on HER2 distinct from that of trastuzumab [6–10]. In the phase 3 CLEOPATRA trial of HER2-positive MBC, the combination of pertuzumab, trastuzumab, and docetaxel significantly prolonged PFS (median 18.5 vs. 12.4 months; HR, 0.62; P < 0.001) [11] and OS (median 56.5 months vs. 40.8 months: HR, 0.68, P < 0.001) [12] vs. trastuzumab + docetaxel.
In pre-clinical experiments, the antitumor activity of T-DM1 was enhanced when combined with paclitaxel [13] or pertuzumab [14]. Based on these promising pre-clinical data, this open-label, multicenter, phase 1b/2a study (TDM4652g/NCT00951665) was designed to investigate the feasibility of combination treatment with T-DM1 + paclitaxel ± pertuzumab in HER2-positive locally advanced breast cancer (LABC) or MBC.
Here we show that T-DM1 + paclitaxel ± pertuzumab shows marked clinical activity in patients with previously treated HER2-positive LABC or MBC, although peripheral neuropathy was a common adverse event (AE).
Methods
Study design
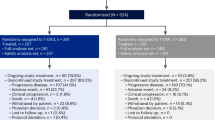
The phase 1b dose-finding portion of this phase 1b/2a study evaluated the efficacy, safety, tolerability, and pharmacokinetics of T-DM1 + paclitaxel ± pertuzumab (Fig. 1a). A traditional 3 + 3 dose-escalation approach was used to explore four regimens. Under regimen 1, intravenous T-DM1 was administered every three weeks (q3w) at 2.0, 2.4, 3.0, or 3.6 mg/kg, and intravenous paclitaxel was administered weekly at 65 mg/m2 or 80 mg/m2. The maximum tolerated dose (MTD) of this combination was utilized in regimen 2, with the addition of intravenous pertuzumab (loading dose of 840 mg on day 1 of cycle 1 followed by 420 mg q3w in subsequent cycles). Under regimen 3, weekly T-DM1 1.2, 1.6, 2.0, or 2.4 mg/kg was administered in combination with weekly paclitaxel 65 mg/m2 or 80 mg/m2. The MTD of this combination was used in regimen 4, with the addition of pertuzumab (dose as above). Patients were followed for a minimum of 22–23 days before additional patients were enrolled to the next dose cohort. Patients were assessed for dose-limiting toxicities (DLTs) during cycle 1 (Additional file 1: Table S1); the minimum DLT observation period was 23 days for regimens 1 and 3, and 22 days for regimens 2 and 4. Based on DLTs observed on-study, DLT criteria were revised to establish a more clinically relevant MTD (Additional file 1: Table S1). Using the MTDs identified in phase 1b, phase 2a patients (Fig. 1b) were randomized (1:1) via an interactive voice response system to T-DM1 3.6 mg/kg q3w + weekly paclitaxel 80 mg/m2 (Group A) or to T-DM1 3.6 mg/kg q3w + weekly paclitaxel 80 mg/m2 + pertuzumab (dose described) (Group B).
Design of (a) phase 1b and (b) phase 2a. aMTD is the highest dose at which 0/3 patients or 1/6 patients experienced a dose-limiting toxicity. bBrain metastases that have required any type of therapy to control symptoms in the 60 days prior to first study treatment. ECOG Eastern Cooperative Oncology Group, HER2 human epidermal growth factor receptor 2, LABC locally advance breast cancer, LD loading dose, MBC metastatic breast cancer, MTD maximum tolerated dose, qw weekly, q3w every three weeks, T-DM1 trastuzumab emtansine
In both study phases, treatment continued until disease progression or unacceptable toxicity. In phase 2a, paclitaxel could be discontinued after 12 doses at the investigator’s discretion for reasons other than disease progression or unacceptable toxicity. Patients who discontinued paclitaxel could continue T-DM1 ± pertuzumab in the absence of disease progression. Dose delays of up to 21 days were allowed for T-DM1, paclitaxel, and pertuzumab.
Patients who developed isolated brain metastases could receive central nervous system radiotherapy and resume study treatment if systemic disease was controlled and ≤1 treatment cycle was missed. An Eastern Cooperative Oncology Group (ECOG) performance status of 0–2 was required to continue therapy. Patients with ongoing clinical benefit, acceptable toxicity, and adequate cardiac function could receive treatment for up to one year. After one year of treatment, patients without disease progression had the option to enroll in an ongoing extension study (TDM4529g/NCT00781612). To allow completion of the present study, phase 2a patients could enroll in TDM4529g 16 weeks after the last patient enrolled in TDM4652g.
This study was reviewed and approved by the relevant institutional review board/ethics committee at each study site (Dana-Farber Cancer Institute Institutional Review Board, Colorado Multiple Institutional Review Board, Western Institutional Review Board Panel 7, Memorial Sloan Kettering Cancer Center Institutional Review Board, Wayne State University Institutional Review Board, or Stanford University Research Compliance Office), and was conducted in accordance with the Declaration of Helsinki, Good Clinical Practice guidelines, and applicable laws. All patients provided written informed consent.
Patients
Eligible patients were aged ≥18 years with an ECOG performance status of 0–2 and measurable or evaluable HER2-positive (immunohistochemistry 3+, fluorescence in situ hybridization–positive, or chromogenic in situ hybridization–positive by local assessment) unresectable LABC or MBC. Phase 1b patients had received prior treatment with trastuzumab in any line, but this was not a requirement for phase 2a. A cardiac ejection fraction ≥50 % by echocardiogram or multigated acquisition (MUGA) scan, adequate hematologic and end-organ function, and life expectancy ≥90 days as assessed by the investigator were also required. Exclusion criteria are described in Additional file 2.
Study objectives
The primary objectives of phase 1b were to determine MTD, identify DLTs, and characterize the safety, tolerability, and pharmacokinetics of T-DM1 (q3w and weekly) + paclitaxel ± pertuzumab. The primary objectives of phase 2a were to further characterize the safety and feasibility of T-DM1 + paclitaxel ± pertuzumab and assess the proportion of patients able to receive 12 doses of T-DM1 + paclitaxel ± pertuzumab. Secondary objectives of both study phases included overall response rate (ORR), clinical benefit rate (CBR), PFS, and duration of response. Biomarkers were an exploratory endpoint.
Assessments
Pharmacokinetic and biomarker analyses were performed, as described in the supplemental materials (Additional file 2). Patients were monitored for AEs and serious AEs throughout the study and for 30 days after last treatment dose. Investigators were instructed to follow unresolved AEs and serious AEs until event resolution/stabilization, patient was lost to follow-up, or study treatment/participation was determined to not be the cause of the event. Echocardiogram or MUGA scans were performed at screening and the end of cycle 2. Scans were repeated every three cycles thereafter throughout phase 1b and every four cycles thereafter throughout phase 2a. Patients who discontinued T-DM1 because of AEs were followed for 30 days for safety and every six weeks for disease progression until the initiation of another anticancer therapy or study withdrawal. AEs were graded according to National Cancer Institute Common Terminology Criteria for AEs v.3.
The feasibility of T-DM1 + paclitaxel ± pertuzumab was assessed by the percentage of patients who completed 12 consecutive weeks of paclitaxel and the percentage who completed ≥12 paclitaxel doses within the first 15 weeks of the study. Patients who discontinued paclitaxel due to disease progression before completing 12 doses were not evaluable for feasibility. The percentage of patients who completed ≥8 paclitaxel doses within the first 12 weeks of the study was analyzed post hoc.
Radiologic tumor assessments, graded according to modified Response Evaluation Criteria in Solid Tumors (RECIST) v1.0 [15], were performed at screening, the end of cycle 2, and every two cycles thereafter throughout phase 1b. For phase 2a, radiologic tumor assessments were performed at baseline and every four cycles (12 weeks) thereafter. Investigator-assessed ORR was based on modified RECIST v1.0; responses were confirmed. CBR was defined as the percentage of patients with investigator-assessed complete response, partial response, or stable disease of ≥6 months duration.
Statistical analyses
All statistical analyses are descriptive (SAS® version 9.2). Patients who received ≥1 dose of study treatment were included in the safety and efficacy analyses. Patients who discontinued treatment due to disease progression before completing 12 doses within 15 weeks were not included in the feasibility assessment. Kaplan–Meier methodology was used to estimate median PFS; corresponding 95 % confidence intervals were determined via the Clopper-Pearson method. The cut-off for these analyses was 15 August 2013, and does not include data from the extension study.
Results
Patients
Sixty patients were enrolled to phase 1b (regimen 1, n = 26; regimen 2, n = 10; regimen 3, n = 21; regimen 4, n = 3) (Fig. 1a), and 44 were randomized to phase 2a (Group A, n = 22; Group B, n = 22). The demographic and baseline characteristics of the phase 1b and 2a populations are shown in Table 1; some imbalances were seen in the cohort of patients randomized to phase 2a. Compared with Group B, fewer patients in Group A were hormone receptor–positive (45.5 % vs. 59.1 %), anthracycline-exposed (59.1 % vs. 77.3 %), and white (72.7 % vs. 90.9 %), while more had been previously administered taxanes (90.9 % vs. 72.7 %).
Forty-one (68.3 %) phase 1b patients withdrew from the study due to disease progression (n = 29), AEs (n = 4), death (n = 3), physician decision (n = 4), and patient decision (n = 1). Nineteen (43.2 %) phase 2a patients discontinued because of disease progression (n = 11), progressive disease (PD)–related death (n = 2), AEs (n = 2), patient decision (n = 2), physician decision (n = 1), and loss to follow up (n = 1).
Maximum tolerated dose
Thirty of the 60 (50.0 %) phase 1b patients were assessed using the original DLT criteria. The following DLTs were observed: neutropenia (n = 3), increased alanine aminotransferase (n = 2), increased aspartate aminotransferase (n = 1), thrombocytopenia (n = 1), and dehydration (n = 1). Following revision of the DLT criteria (Additional file 1: Table S1), no additional DLTs were reported. The MTDs were identified as T-DM1 3.6 mg/kg q3w or weekly 2.4 mg/kg + weekly paclitaxel 80 mg/m2 and pertuzumab 840 mg loading dose followed by 420 mg q3w. The addition of pertuzumab did not alter the MTDs for T-DM1 + paclitaxel.
Safety
Across both study phases, the most common all-grade AEs were peripheral neuropathy (phase 1b, 90.0 %; phase 2a, 90.9 %) and fatigue (phase 1b, 85.0 %; phase 2a, 79.5 %) (Table 2, Additional file 3: Table S2). In phase 1b, 80.0 % (48/60) experienced ≥1 grade ≥3 AE, most commonly peripheral neuropathy (23.3 %), neutropenia (20.0 %), and fatigue (18.3 %) (Additional file 3: Table S2). Of the 44 phase 2a patients, 77.3 % experienced ≥1 grade ≥3 AE, most commonly neutropenia (25.0 %), peripheral neuropathy (18.2 %), and thrombocytopenia (15.9 %) (Table 2). Within the phase 2a cohort the incidence of common all-grade AEs was generally similar without (Group A) or with pertuzumab (Group B); however, rates of all-grade dry eye (27.3 % vs. 54.5 %), alopecia (27.3 % vs. 50.0 %), epistaxis (22.7 % vs. 50.0 %), diarrhea (18.2 % vs. 50.0 %), and rash (13.6 % vs. 40.9 %) were lower among patients receiving T-DM1 + paclitaxel vs. T-DM1 + paclitaxel + pertuzumab.
In phase 1b, 44 patients (73.3 %) discontinued paclitaxel due to AEs, but remained on other study medications. AEs leading to paclitaxel discontinuation in >1 patient were peripheral neuropathy (n = 25), neutropenia (n = 4), fatigue (n = 3), thrombocytopenia (n = 2), dry eye (n = 2), and hypertransaminasemia (n = 2). In phase 2a, 26 patients (59.1 %) discontinued paclitaxel due to AEs. Only peripheral neuropathy (n = 15; fatigue, n = 2) led to paclitaxel discontinuation in >1 patient. There were five deaths (phase 1b, n = 3; phase 2a, n = 2). Two deaths in phase 1b (sudden death and subdural hematoma) were considered treatment-related, while the third (pneumonia) was considered unrelated. Neither death in phase 2a (disease progression) was considered treatment-related.
Feasibility
One phase 2a patient was nonevaluable for feasibility due to PD prior to receiving 12 doses of paclitaxel. Of the remaining 43 patients, 79.1 % (n = 34) received ≥8 paclitaxel doses within 12 weeks, 51.2 % (n = 22) received ≥12 doses within 15 weeks, and 14.0 % (n = 6) received 12 doses by week 12 (Fig. 2).
The median dose intensity of paclitaxel was 82.8 % (range, 52.1–101.3), and the median number of paclitaxel doses administered was 12 (1–48). The overall median treatment duration for paclitaxel in patients in Group A (no pertuzumab) and Group B (with pertuzumab) was 3.04 (range, 0.0–6.9) months and 2.55 (1.0 − 5.8) months, respectively. The median dose intensity of T-DM1 and pertuzumab was 95.9 % (52.2–104.5) and 100 % (67–100), respectively, and the median number of doses administered was 8.5 (1–14) and 8.5 (4–14), respectively.
Efficacy
In phase 1b, 55 of 60 patients had measurable disease. The ORR was 54.5 % (95 % CI 40.6–68.0), and the CBR was 66.7 % (95 % CI 53.5–78.3) (Table 3). In phase 2a, 42 of 44 patients had measurable disease, and the overall ORR was 50.0 % (34.6–65.4) (Table 3). The ORR was 47.6 % (27.6–70.2) in those who did not receive pertuzumab (Group A) and was 52.4 % (29.8–72.4) in patients who did receive pertuzumab (Group B). The overall CBR for phase 2a was 56.8 % (41.6–71.0). The CBR was 54.5 % (32.7–74.0) in patients who did not receive pertuzumab (Group A) and was 59.1 % (38.3–79.3) in patients who did (Group B).
The median duration of follow-up in phase 2a was 6.2 months. Median PFS for patients in Group A was 7.4 months (95 % CI 5.9–not estimable; Fig. 3). Median PFS was not reached in Group B.
Pharmacokinetics
Pharmacokinetic analyses of T-DM1 conjugate, total trastuzumab, DM1, and paclitaxel suggested a low risk of drug − drug interactions between T-DM1 and paclitaxel (Additional file 4: Pharmacokinetics results, Tables S3–S5 and Figure S1).
Biomarkers
Results from the exploratory biomarker analysis of HER2 mRNA are summarized in Additional file 5: Table S6. Due to small subgroup numbers, these data should be interpreted with caution.
Discussion
This phase 1b/2a trial is the first to report on the use of T-DM1 combined with a taxane. Peripheral neuropathy was the most frequent all-grade AE in both study phases and was the main reason for paclitaxel discontinuation. Peripheral neuropathy is associated with taxane use [16, 17] and is less common with single-agent T-DM1 [18]. The rate of all-grade peripheral neuropathy in the present study (90.9 %) was similar to the 78–92 % incidence reported in studies of patients who were largely taxane-naive and administered trastuzumab + weekly paclitaxel 90 mg/m2 [19, 20]. This rate was also comparable to that observed in a phase 2 study of patients with MBC administered trastuzumab + pertuzumab + weekly paclitaxel 80 mg/m2 (82.1 %) [21]. In a phase 3 trial of patients with MBC administered trastuzumab + paclitaxel 175 mg/m2 q3w or 80 mg/m2 weekly, the incidence of grade 3 neuropathy was significantly greater in patients receiving weekly vs. q3w paclitaxel (24 % vs. 12 %, P = 0.0003) [17], further suggesting that this toxicity is largely paclitaxel-related. In the current study, the majority (81.8 %) of patients had received prior taxane treatment, which may have also contributed to the high rate of peripheral neuropathy.
In phase 2a, the incidence of all-grade fatigue in Group A (72.7 %) and Group B (86.4 %) was higher than that observed with single-agent T-DM1 in the phase 3 EMILIA (35.1 %) [2] and TH3RESA studies (25 %) [3], suggesting that this increase is due to the addition of paclitaxel and potentially pertuzumab. Rates of the most common grade ≥3 AEs in phase 2a, neutropenia (25.0 %) and peripheral neuropathy (18.2 %), were higher than reported for single-agent T-DM1 in the EMILIA (neutropenia, 2.0 %; peripheral neuropathy, <2 %) [2] and TH3RESA studies (neutropenia, 2.5 %; peripheral neuropathy, <2 %) [3]. However, the rate of grade ≥3 thrombocytopenia in phase 2a of our study (15.9 %) was similar to the incidence in EMILIA (12.9 %) [2], suggesting that thrombocytopenia was not potentiated by adding paclitaxel ± pertuzumab. In phase 2a of the present study, adding pertuzumab to T-DM1 + paclitaxel did not substantially alter toxicity, although rates of all-grade dry eye, alopecia, epistaxis, diarrhea, and rash were numerically higher in patients also receiving pertuzumab.
Overall, 51.2 % of phase 2a patients received ≥12 doses of weekly paclitaxel 80 mg/m2 within 15 weeks, and 14.0 % received 12 paclitaxel doses by week 12. The feasibility of combining T-DM1 and paclitaxel was lower than that reported in a phase 2 study of the first-line treatment of advanced breast cancer with trastuzumab + paclitaxel: 97 % (33/34) completed ≥12 weeks of treatment with weekly paclitaxel 90 mg/m2 + weekly trastuzumab [20]. This may have been due to the fact that most patients in our cohort had previously received taxane treatment; as mentioned, peripheral neuropathy, which is associated with taxane use [16, 17], was the most common AE leading to paclitaxel discontinuation.
The pharmacokinetics of T-DM1, total trastuzumab, and DM1 in this study were comparable with single-agent T-DM1. Moreover, the pharmacokinetics of paclitaxel were similar in the presence and absence of T-DM1, indicating that the potential for drug–drug interaction between T-DM1 and paclitaxel is low.
In phase 2a of our study, where patients had received a median of 5.0 systemic therapies in the metastatic setting, the ORR was 50.0 %, and the CBR was 56.8 %. Median PFS was not estimable due to limited follow-up of all patients.
The rationale for this study was based on pre-clinical data suggesting that taxanes could enhance the activity of T-DM1. We had assumed that combining T-DM1 with a conventional, non-targeted, cytotoxic agent such as paclitaxel would add to the toxicity of single-agent T-DM1, therefore negating the favorable tolerability profile conferred by the targeted mechanism of action of T-DM1, but the extent of this potentially increased toxicity was unclear. Neurotoxicity is a known treatment-limiting toxicity for weekly paclitaxel [19]. In our study, all-grade neurotoxicity occurred in 90.9 % of patients and grade 3–4 neurotoxicity occurred in 18.2 %; toxicity (predominately peripheral neuropathy) led to 48.8 % of patients being unable to receive ≥12 paclitaxel doses within 15 weeks and 86.0 % being unable to receive 12 paclitaxel doses by week 12. As the majority of patients on this study (phase 1b, 90 %; phase 2a, 82 %) had previously received taxane treatment, the high rate of peripheral neuropathy is not unexpected: taxane retreatment can lead to cumulative toxicities or exacerbation of chronic toxicities such as neuropathy [22]. Thus, it is possible that this regimen may be better tolerated in those who are taxane-naive. In light of the clinical activity of this regimen and given that the primary reason for treatment discontinuation was neuropathy, evaluation of this regimen in patients without prior taxane exposure may be warranted. Alternatively, an intermittent vs. weekly paclitaxel schedule may increase the feasibility of this regimen in those who are taxane-experienced.
Conclusions
With its clinical activity, as demonstrated by an ORR of 50.0 % and a CBR of 56.8 %, these data suggest that there is potential for T-DM1 to be combined with paclitaxel and pertuzumab. However, in this pre-treated population, rates of peripheral neuropathy were high and resulted in frequent and early discontinuation of paclitaxel. It is unclear whether adding pertuzumab or paclitaxel, or the combination of both agents, adds to the substantial clinical activity of single-agent T-DM1 in patients with previously treated advanced breast cancer.
Abbreviations
- AE:
-
Adverse events
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate aminotransferase
- AUC:
-
Area under plasma concentration-time curve
- CBR:
-
Clinical benefit rate
- CI:
-
Confidence interval
- CL:
-
Clearance
- Cmax :
-
Peak plasma concentration
- CR:
-
Complete response
- DLT:
-
Dose-limiting toxicity
- ECOG:
-
Eastern Cooperative Oncology Group
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hazard ratio
- LABC:
-
Locally advanced breast cancer
- LC-MS/MS:
-
Liquid chromatography-tandem mass spectrometry
- LD:
-
Loading dose
- LLOQ:
-
Lower limit of quantitation
- MBC:
-
Metastatic breast cancer
- MQC:
-
Minimum quantifiable concentration
- MTD:
-
Maximum tolerated dose
- MUGA:
-
Multigated acquisition
- NCA:
-
Noncompartmental analysis
- NE:
-
Not estimable
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PFS:
-
Progression-free survival
- PR:
-
Partial response
- PR:
-
Progesterone receptor
- q3w:
-
Every three weeks
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- SD:
-
Stable disease
- t1/2 :
-
Elimination half-life
- T-DM1:
-
Trastuzumab emtansine
- ULN:
-
Upper limit of normal
- Vss :
-
Volume of distribution at steady state
References
Lewis Phillips GD, Li G, Dugger DL, Crocker LM, Parsons KL, Mai E, et al. Targeting HER2-positive breast cancer with trastuzumab-DM1, an antibody-cytotoxic drug conjugate. Cancer Res. 2008;68:9280–90.
Verma S, Miles D, Gianni L, Krop IE, Welslau M, Baselga J, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367:1783–91.
Krop IE, Kim SB, González-Martín A, LoRusso PM, Ferrero JM, Smitt M, et al. Trastuzumab emtansine versus treatment of physician’s choice for pretreated HER2-positive advanced breast cancer (TH3RESA): a randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15:689–99.
Hurvitz SA, Dirix L, Kocsis J, Bianchi GV, Lu J, Vinholes J, et al. Phase II randomized study of trastuzumab emtansine versus trastuzumab plus docetaxel in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer. J Clin Oncol. 2013;31:1157–63.
National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Breast Cancer, version 3, 2012. Available at URL: http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf [accessed 28 Oct 2015].
Adams CW, Allison DE, Flagella K, Presta L, Clarke J, Dybdal N, et al. Humanization of a recombinant monoclonal antibody to produce a therapeutic HER dimerization inhibitor, pertuzumab. Cancer Immunol Immunother. 2006;55:717–27.
Agus DB, Akita RW, Fox WD, Lewis GD, Higgins B, Pisacane PI, et al. Targeting ligand-activated ErbB2 signaling inhibits breast and prostate tumor growth. Cancer Cell. 2002;2:127–37.
Franklin MC, Carey KD, Vajdos FF, Leahy DJ, de Vos AM, Sliwkowski MX. Insights into ErbB signaling from the structure of the ErbB2-pertuzumab complex. Cancer Cell. 2004;5:317–28.
Cho HS, Mason K, Ramyar KX, Stanley AM, Gabelli SB, Denney Jr DW, et al. Structure of the extracellular region of HER2 alone and in complex with the Herceptin Fab. Nature. 2003;421:756–60.
Portera CC, Walshe JM, Rosing DR, Denduluri N, Berman AW, Vatas U, et al. Cardiac toxicity and efficacy of trastuzumab combined with pertuzumab in patients with [corrected] human epidermal growth factor receptor 2-positive metastatic breast cancer. Clin Cancer Res. 2008;14:2710–6.
Baselga J, Cortés J, Kim SB, Im SA, Hegg R, Im YH, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366:109–19.
Swain S, Baselga J, Kim S, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372:724–34.
Krop IE, Modi S, Elias A. A dose-escalation study of trastuzumab-DM1 (T-DM1), paclitaxel (T), and pertuzumab (P) in patients with HER2-positive, locally advanced or metastatic breast cancer (MBC) previously treated with a trastuzumab-containing regimen. Abstract P3-14-10. Cancer Res. 2010;70 Suppl 2:295s.
Phillips GD, Fields CT, Li G, Dowbenko D, Schaefer G, Miller K, et al. Dual targeting of HER2-positive cancer with trastuzumab emtansine and pertuzumab: critical role for neuregulin blockade in antitumor response to combination therapy. Clin Cancer Res. 2014;20:456–68.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors: European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–16.
Seidman AD, Hudis CA, Albanell J, Tong W, Tepler I, Currie V, et al. Dose-dense therapy with weekly 1-hour paclitaxel infusions in the treatment of metastatic breast cancer. J Clin Oncol. 1998;16:3353–61.
Seidman AD, Berry D, Cirrincione C, Harris L, Muss H, Marcom PK, et al. Randomized phase III trial of weekly compared with every-3-weeks paclitaxel for metastatic breast cancer, with trastuzumab for all HER-2 overexpressors and random assignment to trastuzumab or not in HER-2 nonoverexpressors: final results of Cancer and Leukemia Group B protocol 9840. J Clin Oncol. 2008;26:1642–9.
Diéras V, Harbeck N, Budd GT, Greenson JK, Guardino AE, Samant M, et al. Trastuzumab emtansine in human epidermal growth factor receptor 2-positive metastatic breast cancer: an integrated safety analysis. J Clin Oncol. 2014;32:2750–7.
Seidman AD, Fornier MN, Esteva FJ, Tan L, Kaptain S, Bach A, et al. Weekly trastuzumab and paclitaxel therapy for metastatic breast cancer with analysis of efficacy by HER2 immunophenotype and gene amplification. J Clin Oncol. 2001;19:2587–95.
Fountzilas G, Tsavdaridis D, Kalogera-Fountzila A, Christodoulou CH, Timotheadou E, Kalofonos CH, et al. Weekly paclitaxel as first-line chemotherapy and trastuzumab in patients with advanced breast cancer. A Hellenic Cooperative Oncology Group phase II study. Ann Oncol. 2001;12:1545–51.
Dang C, Iyengar N, Datko F, D’Andrea G, Theodoulou M, Dickler M, et al. Phase II study of paclitaxel given once per week along with trastuzumab and pertuzumab in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer. J Clin Oncol. 2015;33:442–7.
Gradishar WJ. Taxanes for the treatment of metastatic breast cancer. Breast Cancer (Auckl). 2012;6:159–71.
Acknowledgements
The authors wish to thank John Ning and David Ipe, MS, who are current and former employees of Genentech, Inc., respectively, for their contributions to this study. Genentech, Inc. sponsored the study and collaborated with the investigators in its design and subsequent data analysis. Third-party writing assistance for this manuscript was provided by CodonMedical, a division of Ashfield Healthcare Communications (a UDG Healthcare plc company), and funded by Genentech, Inc.
This study was presented in part at the American Society of Clinical Oncology, Chicago, Illinois, June 1–5, 2012, and at the San Antonio Breast Cancer Symposium, San Antonio, Texas, December 9–12, 2010, and December 10–14, 2013.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Ian E. Krop and Shanu Modi have received research support from Genentech, Inc. Patricia M. LoRusso has served on speakers’ bureaus and as a consultant for Genentech, Inc. Her institution has received grants for clinical trial research from Genentech, Inc.
Mark Pegram has served as a consultant for Genentech, Inc. His institution received a clinical research contract for the conduct of this study. Ellie Guardino, Betsy Althaus, and Dan Lu are salaried employees of Genentech, Inc. and own stock in F. Hoffmann-La Roche Ltd. Alexander Strasak is a salaried employee of F. Hoffmann-La Roche Ltd. and owns stock in F. Hoffmann-La Roche Ltd.
Anthony Elias has served as a consultant for Genentech, Inc. His institution has received grants for clinical trial research from Genentech, Inc.
Authors’ contributions
All authors participated in trial design and/or data analysis/interpretation, and were involved in all stages of development and finalization of the manuscript. All authors read and approved the final manuscript.
Additional files
Additional file 1: Table S1.
Dose-limiting toxicity criteria. (DOC 136 kb)
Additional file 2:
Supplemental methods. Patient exclusion criteria, pharmacokinetic analysis methods, and biomarker analysis methods. (DOC 138 kb)
Additional file 3: Table S2.
All-grade AEs (occurring in ≥20 %) or grade ≥3 AEs (occurring in >3 %) of the total patient population in phase 1b. (PDF 72 kb)
Additional file 4:
Pharmacokinetics results. Supplemental results for pharmacokinetics analysis. Table S3: Summary of pharmacokinetic exposure of paclitaxel in cycle 1 (absence of T-DM1) and cycle 2 (presence of T-DM1). Table S4: Summary of pharmacokinetic exposure of T-DM1-related analytes (serum T-DM1, serum total trastuzumab and plasma DM1) in cycle 1 following q3w dosing. Table S5: Summary of pharmacokinetic exposure of T-DM1-related analytes (serum T-DM1, serum total trastuzumab and plasma DM1) in cycle 1 following qw dosing. Figure S1: Mean paclitaxel concentration time profiles at (A) a dose of 65 mg/m2 and (B) a dose of 80 mg/m2. (DOC 732 kb)
Additional file 5: Table S6.
Summary of ORR by HER2 mRNA expression level as measured by quantitative reverse transcription polymerase chain reaction. (DOC 138 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Krop, I.E., Modi, S., LoRusso, P.M. et al. Phase 1b/2a study of trastuzumab emtansine (T-DM1), paclitaxel, and pertuzumab in HER2-positive metastatic breast cancer. Breast Cancer Res 18, 34 (2016). https://doi.org/10.1186/s13058-016-0691-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-016-0691-7