Abstract
The clinical success of trastuzumab in breast cancer taught us that appropriate tumor evaluation is mandatory for the correct identification of patients eligible for targeted therapies. Although HER2 protein expression by immunohistochemistry (IHC) and gene amplification by fluorescence in situ hybridization (FISH) assays are routinely used to select patients to receive trastuzumab, both assays only partially predict response to the drug. In the case of epidermal growth factor receptor (EGFR), the link between the presence of the receptor or its amplification and response to anti-EGFR therapies could not be demonstrated. Even less is known for HER3 and HER4, mainly due to lack of robust and validated assays detecting these proteins. It is becoming evident that, besides FISH and IHC, we need better assays to quantify HER receptors and categorize the patients for individualized treatments. Here, we present the current available methodologies to measure HER family receptors and discuss the clinical implications of target quantification.
Similar content being viewed by others
Introduction
The HER family (also called ErbB or epidermal growth factor receptor (EGFR) family) comprises four transmembrane receptor tyrosine kinases, EGFR (or HER1), HER2, HER3, and HER4. These receptors signal through homo- and heterodimerization and promote cell proliferation, motility, and invasion [1]. Dysregulated expression and activity of HER family members is frequent in breast cancer. Overexpression of EGFR1, HER2 and HER3 is generally associated with poor prognosis whereas high expression of HER4 is associated with a better outcome [2-7]. Up to 25% of breast carcinomas overexpress HER2. High levels of this oncogene, almost invariably as a consequence of genomic amplification of a region of chromosome 17 (17q21) including the HER2 locus, drives aggressive disease and is an important therapeutic target.
Monoclonal antibodies (that is, trastuzumab, pertuzumab, T-DM1) and small molecule kinase inhibitors (that is, lapatinib, neratinib and afatinib) are the main strategies to target HER2 in breast cancer. Trastuzumab, in combination with chemotherapy, has significantly increased both progression-free survival (PFS) and overall survival in patients with advanced disease [8,9] as well as in the early (adjuvant) setting [10,11]. Lapatinib, given in combination with capecitabine, has shown clinical activity in HER2-positive breast cancer patients that became refractory to trastuzumab-based therapy [12]. Moreover, measurable clinical benefit is observed also when lapatinib is administered as a single agent or in combination with paclitaxel as first-line treatment [13,14]. Recently, the antitumor activity of dual HER2 blockade (trastuzumab in combination with either lapatinib or pertuzumab) was proven to be significantly superior to single agents in a neoadjuvant setting [15-17].
EGFR has been shown to be highly expressed in triple-negative breast cancer (TNBC), both in cell lines and in patients [18]. Moreover, preclinical studies have demonstrated that the inhibition of EGFR affects growth in TNBC cell lines [19]. These findings provided the rationale to test the efficacy of anti-EGFR agents, such as the antibodies cetuximab and panitumumab, in TNBC patients. In the metastatic setting, cetuximab in combination with chemotherapy showed some promising activity [20-22]. Nevertheless, no substantial improvements in either PFS or overall survival were achieved in these patients. A small pilot study testing the efficacy of panitumumab in combination with standard chemotherapy in TNBC patients in the neoadjuvant setting showed a pathological complete response rate of 46.8% [23]. However, the relevance of these findings will be assessed only when PFS and/or overall survival data are available.
There are several unanswered questions about which patients with breast cancer are most likely to benefit from one or another form of anti-HER targeted therapy and which type of determination methodology is most appropriate.
DNA-based, RNA-based, and protein-based assays have been developed to determine the HER status of breast tumors. To date, exploitation of the overexpression of HER2 is part of the management of a breast cancer patient whereas EGFR, HER3, and HER4 determinations are still exploratory and not used in clinical practice. As a matter of fact, to be eligible for anti-HER therapy such as trastuzumab, specimens have to be HER2-positive as determined by immunohistochemistry (IHC) analysis or harbor HER2/neu gene amplification by fluorescence in situ hybridization (FISH). Although these tests have become the benchmarks for defining tumors as HER2-positive, considerable controversy still exists regarding the accuracy, reliability, and inter-observer variability of these assay methods. It is estimated that up to 20% of HER2 testing performed in the field may be inaccurate when validated against central or 'expert' laboratories [24,25]. A recent round-robin study conducted to evaluate current HER2 testing methods and their potential impact on clinical outcomes showed that interpretation issues (especially when dealing with IHC or FISH equivocal results as defined by the American Society of Clinical Oncologists (ASCO)/College of American Pathologists (CAP) guidelines) and/or HER2 tumor heterogeneity may play a significant role in discordant results [26].
In an effort to improve the accuracy and consistency of HER2 testing, a joint task force of ASCO and CAP proposed guideline recommendations for HER2 testing using either IHC or FISH [27]. Among ‘HER2-positive’ tumors (defined by consensus criteria), there is a wide range of variability in terms of HER2-gene amplification and protein expression measured by conventional semi-quantitative methods such as the HercepTest®. The possibility that a quantitative analysis of HER family protein expression could improve the prediction of HER-targeting drugs has led to the evaluation of alternative and more quantitative tests. Despite that, the 2013 ASCO/CAP Update Committee concluded that there was insufficient evidence to warrant inclusion of these new assays to determine HER2 status in unselected patients due to lack of a consistent body of evidence on their analytical validity, clinical validity, and clinical utility [27].
In this review we address these issues by evaluating the current methodologies used for HER family status determination and discussing the clinical implications of HER family quantification on response to anti-HER treatment. In Additional file 1 we list the Food and Drug Administration (FDA) approved/Clinical Laboratory Improvement Amendments certified diagnostic tests available to measure HER receptors in the clinic.
Methodologies
HER status assessment at the protein level
Immunohistochemistry
IHC is the primary technique used to determine protein expression status in a patient sample. It is a simple, fast, easy to implement and relatively inexpensive method for protein detection. Slides are incubated with an antibody directed against the HER receptor protein, labeled, and finally made visible with a chromogen, resulting in a staining localized in the cellular compartment where the protein target is expressed (membrane, cytosol, nucleus). The more the protein is present, the stronger the staining will be. Traditionally, assessment of protein expression is done by visual estimation of staining intensity and is reported as binary (positive versus negative), four-tiered (0, 1+, 2+, and 3+), or semiquantitative continuous variable as for the H score ((% at 0) × 0 + (% at 1+) × 1 + (% at 2+) × 2 + (% at 3+) × 3; range = 0 to 300) results [28].
For companion diagnostic tests, guidelines are generally issued to guide pathologists in the interpretation and scoring of the staining. The HER2 scoring guidelines recommended by ASCO/CAP classified HER2 expression as 0 (no staining or faint incomplete membrane staining observed in ≤10% of tumor cells), 1+ (faint/barely perceptible incomplete membrane staining in >10% of tumor cells), 2+ (circumferential membrane staining that is incomplete and/or weak/moderate and within >10% of tumor cells or complete and circumferential membrane staining that is intense and within ≤10% of tumor cells) or 3+ (circumferential membrane staining that is complete, intense, and within >10% of tumor cells). Tumors with scores 0 and 1+ were considered negative; 2+ was considered equivocal and required FISH reflex testing; 3+ was considered positive and eligible for trastuzumab [29].
Despite the effort to standardize HER2 status determination, current guidelines do not restrict the type and characteristics of IHC assay to be used for HER2 protein expression. The use of FDA approved tests such as HercepTest® (DAKO, Carpinteria, CA, USA), PATHWAY anti-HER-2/neu (Ventana Medical systems, Roche, Tuscon, AZ, USA), InSite™ Her-2/neu (Biogenex, Freemont, CA, USA) as well as fully automated staining systems such as Ventana Benchmark (Ventana Medical systems, Roche, Tuscon, AZ, USA) and Leica Microsystems Bondmax (Leica, Newcastle, UK) may certainly minimize process variability and improve assay repeatability and reproducibility. Nevertheless, many laboratories developed tests with different antibodies directed against other HER2 epitopes (intracellular versus extracellular), which may show non-overlapping specificities and be differently influenced by preanalytical factors [30-32].
Interpretation of membrane staining can be optimized using quantitative image analysis such as the automated quantitative analysis (AQUA) system [33]. AQUA is a fluorescence IHC-based method that provides objective and continuous protein expression scores for tissues by using automated fluorescence microscopy and advanced image analysis algorithms. It is important to note, however, that there are as yet no clinical data related to AQUA’s predictive ability.
Other software applications include Aperio Scanscope (Aperio Technologies; Vista, CA, USA), Definiens (Carlsbad, CA, USA) and Vysis AutoVysion (Abbott Molecular, Des Plaines, IL, USA) among others. These applications can reduce the subjectivity of a traditional scoring system and provide a more reproducible protein expression score [34,35].
Enzyme-linked immunosorbent assay
HER2 receptor protein extracellular domain (ECD, p105) is released into the circulation after cleavage by matrix metalloproteinases and its levels can be measured in the serum using an enzyme-linked immunosorbent assay approved by the FDA (Siemens Healthcare, Erlangen, Germany). Elevated levels of serum HER2 ECD have been shown to be both prognostic and predictive of response to trastuzumab in HER2-positive tumors [36,37]. Serum ECD values have been suggested, therefore, as an alternative technique for determining HER2 status, although available results are controversial. First, not all patients with HER2-positive tumors appear to have elevated serum ECD values and patients with HER2-negative tumors can also have elevated ECD values. Second, the reported data come from studies including a limited number of patients, thus making current evidences still insufficient to consider basing treatment decisions on ECD levels in routine clinical practice. A large meta-analysis study [38] has combined the data of four trastuzumab trials in metastatic breast cancer and showed that, from the combined dataset (N = 322 patients), there was no correlation between baseline ECD value and tumor response. ECD values decreased upon initiation of combination therapy irrespective of treatment and tumor response. Furthermore, disease progression was not reliably predicted by an increase in ECD levels. Therefore, the use of ECD values in treatment decision making was not recommended.
VeraTag™ proximity-based assay
The VeraTag™ proximity-based assay (HERmark® Breast Cancer Assay; Monogram Biosciences, Inc., South San Francisco, CA, USA) enables precise quantitative measurements of total HER-2 expression and HER2 homodimers in formalin-fixed, paraffin-embedded (FFPE) tissue specimens [39,40]. The HERmark assay was developed based on a proprietary proximity-based technology platform that enables accurate quantification of proteins and protein-protein complexes through the release of a fluorescent tag (VeraTag reporter, Monogram Biosciences) conjugated to a pair of monoclonal antibodies directed to unique epitopes on the HER2 receptor in molecular proximity [40]. The continuous total HER-2 expression results are grouped as HERmark negative, HERmark equivocal, and HERmark positive. The threshold for a positive HERmark test is based on the comparison with HER2 tests performed in 1,090 breast tumor reference samples (central IHC and central in situ hybridization) from three different study cohorts. The HERmark assay can detect HER2 at amounts of 2,500 up to more than 1 million receptors per cell, and is thus said to be 7 to 10 times more sensitive than IHC. The assay has been validated according to the specifications prescribed by the Clinical Laboratory Improvement Amendments and is performed only in the CAP-certified clinical reference laboratory at Monogram Biosciences (US). VeraTag™ proximity-based assays have been developed also to measure total EGFR, EGFR-EGFR homodimers and EGFR-HER2 heterodimers [40-42], p95 [43], total HER3, HER3-HER3 homodimers and HER3-phosphoinositide 3-kinase (PI3K) complex heterodimers [44] and the phosphorylated forms of EGFR, HER2, and HER3.
Protein interaction measurements
Clinical application of protein-protein interactions has uncovered many potential targets for novel drug development or drug resistance mechanisms [45], with the MDM2-p53 interaction [46,47] and B-Raf inhibition being examples of recent successes [48]. More recently, incorporation of protein interaction data was shown to also improve the predictive performance of prognostic gene expression signatures [49,50]. Despite the importance of adjunct information supplied by the protein interactome configuration to improve the existing prognostic signatures for predicting patient outcome [50], this protein interaction information has rarely been incorporated in diagnostic/prognostic assays.
Fluorescence lifetime imaging microscopy (FLIM) is based on quantifying the non-radiative transfer of energy between the donor and acceptor fluorophores and can only occur when the two molecules are no further apart than 10 nm, consistent with being in molecular contact [51-53]. Various automated imaging platforms, including ours, measure Förster resonance energy transfer (FRET) - the decrease in donor lifetime, the gold standard for FRET measurements (reviewed recently in [54]) - to directly monitor validated protein-protein interactions [55-61] and post-translational modifications, including conformational changes, in cultured cells [58,62-66]. A two antibody FRET/FLIM approach was originally applied, by ourselves and others, to human cancer tissues to detect the nano-proximity between a donor fluorophore-conjugated anti-protein kinase C or anti-EGFR antibody, and an acceptor fluorophore-labeled phospho-specific antibody, providing highly specific quantification of phosphorylation [67,68]. Detailed methodology for sample preparation and instrumentation can be found elsewhere [69,70]. We have now extended this method to measure endogenous protein-protein interactions in archived pathological material [71]. The presence of autofluorescence in stromal and epithelial components may cause difficulties in accurately determining the fluorescence lifetime of fluorophores in FFPE tissue samples [72]. By circumventing the autofluorescence issue using a new analysis algorithm [73], we have recently described the first clinical utilization of this refined FLIM assay (using Alexa546 and Cy5 as donor and acceptor fluorophores, respectively) to quantify the level of HER1-HER3 dimer formation in FFPE tissues from basal-like breast cancer patients who were treated with a neoadjuvant anti-EGFR treatment (cetuximab or panitumumab) [74]. Moreover, we have demonstrated the existence of EGFR-HER4 dimers in breast cancer cells and how these dimers are important for cell motility [75].
Liquid chromatography-tandem mass spectrometry-based proteomics has emerged as the most effective method to study complex proteomes. In this approach, the proteins representing a proteome are analyzed after enzymatic digestion by liquid chromatography coupled to mass spectrometry (MS). Although this approach is a powerful tool to identify proteins in complex biological samples [76,77], it is not optimal for systematic quantification of these proteins because of the stochastic nature and the limited sensitivity of the approach. During the past few years, targeted proteomics has been shown to be complementary to the more widely used discovery proteomic methods. In targeted proteomics, only pre-determined peptide ions are selected for detection and quantification in a sample. The main MS approach supporting targeted proteomics is selected reaction monitoring (SRM), where specific MS assays are generated a priori and used to selectively detect and quantify proteins of interest in a sample. This approach can provide objective quantification and multiplex capabilities with high sensitivity and in an antibody-free setting [78-80]. SRM methods have long been used to quantify low-abundance protein targets in plasma [81] but application of these techniques to FFPE tissue samples has, until recently, been hindered by incomplete solubilization of samples [82,83]. The Liquid Tissue-(SRM) diagnostic technology platform is a newly developed proteomic method that overcomes this limitation, allowing for precise protein quantification in FFPE tissues. Microdissected FFPE tumor tissues are subjected to Liquid Tissue processing to reverse formalin crosslinks. This is followed by trypsinization to completely solubilize all of the protein in the sample. This tryptic peptide mixture is then subjected to SRM analysis using stable isotope-labeled control peptides for accurate quantification [83-85]. Multiple reports have demonstrated that comparable results may be obtained between formalin fixed and matching frozen tissue [84,86]. The reliability of this approach for analysis of proteins in any biological sample including FFPE patient tumor tissue has been demonstrated [87-91], thus widening the application of MS to patient-derived tissue with a consequent profound impact on patient stratification and targeted cancer therapeutics.
Reverse phase protein array (RPPA) and collaborative enzyme enhanced reactive-immunoassay (CEER) are nano-scaled dot blot platforms allowing the detection of multiple proteins (both total and phosphorylated) in many samples simultaneously. They do not require large amounts of sample but are not suitable for FFPE tissue. For RPPA protein lysates are immobilized onto microarrays and then probed with the primary antibodies of choice. Detection is performed by quantification of the labels (fluorescent, colorimetric or other kinds) bound to either the primary or, more often, the secondary antibody added to amplify the signal. RPPA allows testing hundreds of samples at the same time and multiplexing is performed by analyzing multiple arrays spotted with the same protein lysates with different antibodies [92].
CEER takes advantage of the immunocomplexes formed between antibodies printed on a nitrocellulose microarray surface with the target molecules in cell lysates. Once the complexes are formed, two detector antibodies (one conjugated to glucose oxidase and another conjugated to horse radish peroxidase (HRP)) are added. Target detection (expressed as computational units (CU)) requires the presence of both detector antibodies, and the enzyme channeling event between glucose oxidase and HRP will not occur unless both antibodies are in close proximity [93]. The main difference with RPPA is that, instead of protein lysate, antibodies are immobilized in cellulose arrays. This means that, contrary to RPPA, CEER is capable of measuring the expression of dozens of targets simultaneously in the same sample.
Further studies are needed to prove the clinical relevance of the above described methods.
HER status assessment at the DNA level
In situ hybridization
FISH is considered the gold standard method for gene amplification status determination. FISH uses fluorescently labeled probes (usually red) that are complementary to a part of the target gene. After hybridization to the complementary DNA on the slide, the probes can be visualized with a fluorescence microscope. A second probe labeled with a different fluorochrome (usually green) directed against the centromeric region of the chromosome containing the target gene is generally used as control for polysomy. The number of copies of the target gene and centromere probe can be estimated and the ratio determined.
CISH (chromogenic in situ hybridization) is an alternative for FISH. It uses an immunoperoxidase reaction to visualize the target gene probe, which allows scoring with a conventional light microscope. CISH has several advantages over FISH: signal does not fade and the slides can be kept permanently and allows better preservation of morphology. One of the main limitations of CISH is that most of the available assays are still monoprobe assays, meaning that there is no correction with a centromere control probe and only the absolute gene copy number is scored.
Similar to CISH, silver in situ hybridization (SISH) technology uses a non-fluorescent method where the HRP bound to the probe catalyses the reduction of silver acetate to produce a black signal. Several studies showed a good correlation between FISH, CISH, SISH, and IHC for HER2 status determination [94-100].
Recently released ASCO/CAP guidelines recommended that HER2 must be considered in situ hybridization (ISH)-positive based on a single-probe average HER2 copy number ≥6.0 signals/cell or dual-probe HER2/CEP17 ratio ≥2.0 or dual-probe HER2/CEP17 ratio <2.0 with an average HER2 copy number ≥6.0 signals/cell [27]. Whether the centromere control probes for polysomy 17 are really necessary is a matter of debate given that it has been proven by several studies that true polysomy 17 is very rare in breast carcinomas [101]. Concurrent evaluation of several chromosome 17 genes using multiple-probe FISH or multiplex ligation-dependent probe amplification showed that focal amplifications encompassing the centromere - and not true polysomy - are the most common explanation for increases in CEP17 signals [102,103]. These results suggest that CEP17 copy number assessment by standard ISH is not a useful surrogate for polysomy 17. Compared with IHC, ISH assays, in which the target gene copy number is counted, are considered to be more quantitative analytically. However, ISH is not a direct measurement of the protein and just because a change in gene copy number is observed does not necessarily mean that it is expressed. In addition, the procedure is time consuming and new 'fast' FISH assays are under development to reduce the turnaround time [104].
PCR-based techniques
PCR-based techniques such as multiplex ligation-dependent probe amplification [105] have several advantages over ISH-based assays. First, they are more quantitative and results are easier to interpret. Second, they require only small amounts of DNA and are not affected by DNA degradation, thus performing well with FFPE samples. Third, they can be multiplexed, allowing simultaneous interrogation of multiple genes or different parts of genes, representing an ideal and low cost prescreening tool. Head-to-head comparisons between IHC, FISH, and CISH have shown good correlation among technologies [106-109]. The main weaknesses of PCR-based assays are that they do not preserve tissue morphology, may require sample macro- or microdissection to enrich for tumor content, heterogeneity can be missed and contamination with normal or ductal carcinoma in situ may lead to both false-negative and false-positive results.
HER status assessment at the RNA level
Due to multiplexing capability, RNA-based tests are usually used to generate global gene expression signatures rather than single gene measurements. All these signatures work using proprietary algorithms that generate a score based on the expression levels of the genes measured that can determine risk factors, incidence, prognoses and responses to systemic therapies. Clinically validated gene expression tests that include one or more HER family members in their gene lists are discussed below.
The Oncotype DX assay (Genomic Health, Redwood City, CA, USA) uses RT-PCR as a primary technique and work on RNA extracted from FFPE samples. The assay measures the expression of a panel of 21 genes (only HER2 is included among the HER family genes) and the results are provided as a recurrence score. Although the assay was approved as a prognostic test predictive of breast cancer recurrence in women with newly diagnosed, early stage breast cancer, it also assesses the benefit from certain types of chemotherapy [110]. Recently, Genomic Health started reporting estrogen receptor (ER), progesterone receptor (PR), and HER2 results separately in addition to the recurrence score. Although high overall concordance (greater than 91%) between HER2 by IHC or FISH assay and quantitative RT-PCR using the Oncotype DX test has been reported [111,112], an independent study showed a false-negative rate for Oncotype DX RT-PCR for HER2 of >50% [113].
TargetPrint™ (Agendia, Irvine, CA, USA/Amsterdam, The Netherlands) is a microarray-based gene expression test that allows quantitative assessment of ER, PR and HER2 at the RNA level in breast cancer. Compared with IHC results, HER2 gene expression levels provided by TargetPrint™ have been shown to be more reproducible and truly quantitative. Results were validated against IHC and showed an overall concordance greater that 95% [114-116]. Its use is currently proposed in case of equivocal or unreliable IHC results, discordance between two separate tests, discordance of test results and clinicopathologic features or technical failure of IHC/FISH/CISH.
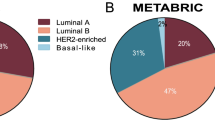
The NanoString Prosigna™ (NanoString Technologies, Seattle, WA, USA) assay measures the expression levels of 50 target genes (including HER2) plus eight constitutively expressed normalization genes (PAM50) to classify a tumor as one of four intrinsic subtypes (luminal A, luminal B, HER2-enriched, and basal-like), which have been shown to be prognostic [117,118]. In addition to identifying a tumor’s intrinsic subtype, the PAM50 signature generates an individualized score estimating a patient’s probability of disease recurrence by weighting the molecular subtype correlations, a subset of proliferation genes, and pathologic tumor size [118,119]. Based on these data, the FDA-cleared and CE-marked Prosigna™ assay, based on the PAM50 gene expression signature, has recently been shown to predict the risk of distant recurrence in women with hormone receptor-positive early stage breast cancer treated with 5 years of endocrine therapy [120-122]. The Nanostring nCounter system uses color-coded probes that bind directly to the RNA transcript without reverse transcription and PCR amplification [123] and work in frozen or FFPE tissues with equivalent ease and efficiency [124]. Assay controls are included to ensure that test samples and the test process meet pre-defined quality thresholds.
The PAM50 gene signature may be run also by classic quantitative PCR and can also provide quantitative and qualitative gene expression scores for the standard biomarkers usually measured semi-quantitatively by IHC - ER, PR and HER2. Using the quantitative PCR cutoff for ERBB2 expression, a study found high specificity (609/624 samples that were low ERBB2 were also HER2-negative by IHC/CISH), while 53% (109/190) of tumors with intermediate-high ERBB2 expression were HER2-positive [125]. This same study and the MA.5 trial [126] found that only about two-thirds of clinically HER2-positive tumors are classified as HER2-enriched. Thus, only a subset of the IHC-defined groups overlap with PAM50 subtype classification.
Although some literature shows an overall high concordance between standard techniques such as IHC and FISH assays and quantitative RT-PCR [111,127-129], there are several practical issues that should be considered when conducting RNA-based analyses. First, the presence of normal tissue within the tumor sample is a major source of subtype misclassification [130]. Therefore, identification of the region of viable invasive breast carcinoma by a pathologist is critical before any RNA extraction is performed. Second, RNA shows greater instability compared with DNA and proteins and thus the selection of technologies that may prevent/overcome RNA degradation is important.
Clinical implications
The fundamental principle of targeted therapy is to specifically harm tumor cells that depend on a definite target for proliferation and survival, sparing non-tumor cells from damage. In many cases, the target is a protein with activating mutations that is present only in tumor cells, facilitating the specificity of the therapy (for example, Braf-mutant melanomas, EGFR-mutant lung cancer), allowing profound inhibition of the target before the emergence of side effects. In the case of HER receptors in breast cancer the target is a protein that, although not carrying any activating alterations, is present in much higher amounts in tumor cells compared with normal cells. In these cases one would guess that the higher is the difference in target expression between normal and tumor cells, the wider is the therapeutic window. However, only the presence of the target or its semiquantitative expression (and not the absolute levels) is currently taken into consideration in clinical practice.
There is an increasing body of evidence indicating that the levels of HER2 in HER2-positive tumors can influence the response to HER2-targeted therapy, converging to the common conclusion that 'more HER2, more response' [131-137]. Quantitative HER2 expression or homodimer levels determined by the HERmark assay correlated with clinical outcome of trastuzumab therapy better than IHC or central FISH studies in patients with metastatic breast cancer. Interestingly, patients with HER2 gene amplification by FISH but low HER2 protein expression or homodimer levels as measured by HERmark responded poorly to trastuzumab-containing therapy, suggesting that not all gene-amplified tumors overexpress the target of trastuzumab [135]. Similarly, absolute HER2 quantification in an homogeneous group of HER2-positive breast cancer (IHC 3+) using triple quadrupole MS was predictive of a better response to trastuzumab in both adjuvant and metastatic settings [136].
But perhaps this is valid until a certain limit. First, the link between the level of HER2 amplification and outcome in patients treated with trastuzumab has been proven only in the neoadjuvant setting [138], whereas other studies failed to demonstrate this association [139,140]. Second, although the clinical benefit from HER2 blockade increases with the level of the target, there may be tumors with extraordinarily high levels of HER2 that are actually more resistant to the therapeutic pressure [141-144]. It is unclear whether this is due to insufficient engagement of the receptor by the targeted agents. In any case, validation of these findings in a larger cohort of patients is necessary. Third, the intriguing observation from B-31 and N9831 studies that tumors that failed to be confirmed as HER2-positive after central laboratory testing may still derive benefit from trastuzumab [145,146] and the complex relationship between HER2, ER, and trastuzumab sensitivity outlined by the study suggest that quantitative HER2 measure alone may not be sufficient, and combination with other markers may be more predictive of trastuzumab response [147].
Since dual HER2 blockade (trastuzumab combined with either pertuzumab or lapatinib) is proving to be more effective than single agent treatment, it will be interesting to investigate whether HER2 absolute levels predict response in this setting as well. In the neoadjuvant setting, this seems to be the case. HER2 levels were measured by HERmark in the primary tumors of patients enrolled in the NeoALTTO trial, testing the activity of trastuzumab in combination with lapatinib compared with single agent treatments, and a positive correlation was found between constitutive HER2 expression and benefit from dual blockade [148].
One of the mechanisms proposed for the synergy observed when combining lapatinib and trastuzumab (at least in preclinical models) is the stabilization and membrane accumulation of HER2 as a consequence of receptor kinase inhibition [149]. One may wonder, therefore, whether lapatinib could sensitize tumors with relatively low levels of HER2 to the antitumor activity of trastuzumab. Testing this possibility, however, is not as easy as it sounds. First, a threshold above which tumors benefit from anti-HER2 therapy (but are still considered 'low expressing tumors') needs to be defined by quantitative methodology. Then, other therapeutic options should be considered to exclude the possibility that these patients can achieve better response from other agents. Genomic analysis of the tumors would be very helpful in these cases as the identification of actionable genetic alterations may guide the choice of therapy. Finally, HER-targeted therapeutic agents such as lapatinib have been shown to stabilize/enhance the HER2-HER3 dimer in preclinical cell models [149]. The quantification of this dimer (as described above), which is believed to be the most potent of all HER dimers with regard to driving cellular proliferation [150,151], will provide important and non-redundant information to that provided by HER protein expression to help clinicians to understand and/or predict the heterogeneity in clinical response.
The quantification of HER3 in response to lapatinib-containing therapies may also be of relevance. In fact, compensatory upregulation of HER3 upon lapatinib treatment has been described both in preclinical models and in patients with HER2-positive breast cancer [152]. The addition of compounds blocking HER3 or the downstream PI3K/AKT pathway significantly potentiates the antitumor effects of lapatinib, underscoring the importance of this occurrence. Because of the mechanistic relationship between EGFR and HER2, EGFR measurement may provide a method for personalizing treatment in breast cancer, beyond the single assay for HER2. Patients with high EGFR using the EGFR antibody D38B1 did not appear to benefit from concurrent trastuzumab in the N9831 trial using the fluorescence-based AQUA quantitative platform [153]. Based on these results, it may be hypothesized that the subset of tumors with high EGFR expression may better respond to lapatinib or dual HER blockade compared with trastuzumab alone.
The absolute levels of EGFR may be predictive for response to anti-EGFR therapy in TNBC patients. We recently showed that patients with tumors expressing high levels of EGFR were more likely to achieve pathological complete response following panitumumab-based therapy [74]. Furthermore, we found that EGFR levels tended to decrease in the residual tumors collected at surgery compared with the primary tumor before the commencement of therapy, indicating that the levels of EGFR may be influenced by the therapeutic pressure. It remains to be defined whether this is a global downregulation of EGFR in all tumor cells or is a positive selection of cells with lower EGFR expression.
As a matter of fact, the acquired loss of expression of HER receptors may be an obvious mechanism of resistance to targeted therapy according to the simple paradigm 'no target, no response'. This has also been described in HER2-positive breast cancer patients upon treatment with trastuzumab-based therapy [154]. Therefore, measuring the levels of HER receptors at the time of progression to targeted therapy should be encouraged to avoid persevering with similar targeted approaches.
Conclusion and perspectives
It is becoming evident that the 'simple detection' of the HER receptors in breast cancer is not sufficient to predict the benefit that patients will achieve from anti-HER therapy. The example of HER2 is archetypal. We know that HER2-positive patients benefit from anti-HER2 therapy, but now we also know that 15 to 20% of these patients express levels of the receptors that are almost comparable with HER2-negative tumors. And, more importantly, these patients do not achieve the same benefit from anti-HER2 therapy as do patients with high HER2 expression. This is especially true in the neoadjuvant setting in patients undergoing dual HER2 blockade [148].
Let’s make an example of how relevant these findings can be. The disease-free survival data from the ALTTO adjuvant trial (comparing patients that received lapatinib, trastuzumab or the combination of the two agents) were recently released [155]. The take home message was that the combination was not significantly superior to trastuzumab single agent in preventing relapses to therapy. These findings were somehow surprising since the NeoALTTO trial clearly demonstrated that dual HER2 blockade is more effective than monotherapy in the neoadjuvant setting. But if we dissect the data we realize that many variables could have influenced this outcome. First, the number of PFS events taken into consideration was lower than the one needed for the planned statistical analysis. Second, a significant percentage of patients enrolled in the combination arm were not treated with a full dose of lapatinib (for toxicity reasons). In a study where the 'control arm' (trastuzumab-based therapy) is known to cure more than 80% of patients, these factors may have diluted the possible improvement in PFS. Thus, it is not so surprising that the difference observed in the ALTTO trial was not significant. It would be interesting to quantify the levels of HER2 in these samples and correlate them with clinical response. Perhaps we will identify a subset of patients with high HER2 expression that is more sensitive to dual HER2 blockade and shows significant clinical benefit in the long term. Fortunately, these samples are available for future biomarker analyses, including HER2 quantification.
For EGFR things are far behind. The basis for testing anti-EGFR therapy in TNBC was the knowledge that overexpression of EGFR occurs in up to 50% of cases [156]. But a real stratification based on how much EGFR these tumors express has never been made. Now we have evidence that, the higher the levels of EGFR, the higher the probability to achieve pathological complete response from cetuximab- or panitumumab-based therapy in the neoadjuvant setting [74]. Again, one would wonder whether the reported activity of anti-EGFR therapy in TNBC (or even in head and neck and colon cancers) would be different if stratification based on the EGFR levels had been done in these clinical trials.
Conclusion
In conclusion, HER receptor quantification may be more tedious than FISH or IHC but it can help in stratifying and selecting patients for anti-HER therapy. Measuring the levels of the targets in patients undergoing 'targeted' therapy sounds like a good idea.
Abbreviations
- AQUA:
-
Automated quantitative analysis
- ASCO:
-
American Society of Clinical Oncologists
- CAP:
-
College of American Pathologists
- CEER:
-
Collaborative enzyme enhanced reactive-immunoassay
- CISH:
-
Chromogenic in situ hybridization
- ECD:
-
Extracellular domain
- EGFR:
-
Epidermal growth factor receptor
- ER:
-
Estrogen receptor
- FDA:
-
Food and Drug Administration
- FFPE:
-
Formalin-fixed, paraffin-embedded
- FISH:
-
Fluorescence in situ hybridization
- FLIM:
-
Fluorescence lifetime imaging microscopy
- FRET:
-
Förster resonance energy transfer
- HRP:
-
Horse radish peroxidase
- IHC:
-
Immunohistochemistry
- ISH:
-
In situ hybridization
- MS:
-
Mass spectrometry
- PFS:
-
Progression-free survival
- PI3K:
-
Phosphoinositide 3-kinase
- PR:
-
Progesterone receptor
- RPPA:
-
Reverse phase protein array
- SISH:
-
Silver in situ hybridization
- SRM:
-
Selected reaction monitoring
- TNBC:
-
Triple-negative breast cancer
References
Holbro T, Beerli RR, Maurer F, Koziczak M, Barbas 3rd CF, Hynes NE. The ErbB2/ErbB3 heterodimer functions as an oncogenic unit: ErbB2 requires ErbB3 to drive breast tumor cell proliferation. Proc Natl Acad Sci U S A. 2003;100:8933–8.
Naidu R, Yadav M, Nair S, Kutty MK. Expression of c-erbB3 protein in primary breast carcinomas. Br J Cancer. 1998;78:1385–90.
Pawlowski V, Revillion F, Hebbar M, Hornez L, Peyrat JP. Prognostic value of the type I growth factor receptors in a large series of human primary breast cancers quantified with a real-time reverse transcription-polymerase chain reaction assay. Clin Cancer Res. 2000;6:4217–25.
Suo Z, Berner HS, Risberg B, Karlsson MG, Nesland JM. Estrogen receptor-alpha and C-ERBB-4 expression in breast carcinomas. Virchows Arch. 2001;439:62–9.
Suo Z, Risberg B, Kalsson MG, Willman K, Tierens A, Skovlund E, et al. EGFR family expression in breast carcinomas. c-erbB-2 and c-erbB-4 receptors have different effects on survival. J Pathol. 2002;196:17–25.
Tovey SM, Witton CJ, Bartlett JM, Stanton PD, Reeves JR, Cooke TG. Outcome and human epidermal growth factor receptor (HER) 1–4 status in invasive breast carcinomas with proliferation indices evaluated by bromodeoxyuridine labelling. Breast Cancer Res. 2004;6:R246–51.
Witton CJ, Reeves JR, Going JJ, Cooke TG, Bartlett JM. Expression of the HER1-4 family of receptor tyrosine kinases in breast cancer. J Pathol. 2003;200:290–7.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–92.
Hudis CA. Trastuzumab - mechanism of action and use in clinical practice. N Engl J Med. 2007;357:39–51.
Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005;353:1659–72.
Smith I, Procter M, Gelber RD, Guillaume S, Feyereislova A, Dowsett M, et al. 2-year follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer: a randomised controlled trial. Lancet. 2007;369:29–36.
Geyer CE, Forster J, Lindquist D, Chan S, Romieu CG, Pienkowski T, et al. Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med. 2006;355:2733–43.
Gomez HL, Doval DC, Chavez MA, Ang PC, Aziz Z, Nag S, et al. Efficacy and safety of lapatinib as first-line therapy for ErbB2-amplified locally advanced or metastatic breast cancer. J Clin Oncol. 2008;26:2999–3005.
Di Leo A, Gomez HL, Aziz Z, Zvirbule Z, Bines J, Arbushites MC, et al. Phase III, double-blind, randomized study comparing lapatinib plus paclitaxel with placebo plus paclitaxel as first-line treatment for metastatic breast cancer. J Clin Oncol. 2008;26:5544–52.
Baselga J, Bradbury I, Eidtmann H, Di Cosimo S, de Azambuja E, Aura C, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012;379:633–40.
Baselga J, Cortes J, Kim SB, Im SA, Hegg R, Im YH, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366:109–19.
Gianni L, Pienkowski T, Im YH, Roman L, Tseng LM, Liu MC, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13:25–32.
Nielsen TO, Hsu FD, Jensen K, Cheang M, Karaca G, Hu Z, et al. Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res. 2004;10:5367–74.
Hoadley KA, Weigman VJ, Fan C, Sawyer LR, He X, Troester MA, et al. EGFR associated expression profiles vary with breast tumor subtype. BMC Genomics. 2007;8:258.
Baselga J, Gomez P, Greil R, Braga S, Climent MA, Wardley AM, et al. Randomized phase II study of the anti-epidermal growth factor receptor monoclonal antibody cetuximab with cisplatin versus cisplatin alone in patients with metastatic triple-negative breast cancer. J Clin Oncol. 2013;31:2586–92.
Carey LA, Rugo HS, Marcom PK, Mayer EL, Esteva FJ, Ma CX, et al. TBCRC 001: randomized phase II study of cetuximab in combination with carboplatin in stage IV triple-negative breast cancer. J Clin Oncol. 2012;30:2615–23.
O'Shaughnessy J, Weckstein DJ, Vukelja SJ, McIntyre K, Krekow L, Holmes FA, et al. Preliminary results of a randomized phase II study of weekly irinotecan/carboplatin with or without cetuximab in patients with metastatic breast cancer. Breast Cancer Res Treat. 2007;106:S32. Abstract 308.
Nabholtz JM, Abrial C, Mouret-Reynier MA, Dauplat MM, Weber B, Gligorov J, et al. Multicentric neoadjuvant phase II study of panitumumab combined with an anthracycline/taxane-based chemotherapy in operable triple-negative breast cancer: identification of biologically defined signatures predicting treatment impact. Ann Oncol. 2014;25:1570–7.
Perez EA, Suman VJ, Davidson NE, Martino S, Kaufman PA, Lingle WL, et al. HER2 testing by local, central, and reference laboratories in specimens from the North Central Cancer Treatment Group N9831 intergroup adjuvant trial. J Clin Oncol. 2006;24:3032–8.
McCullough AE, Dell'orto P, Reinholz MM, Gelber RD, Dueck AC, Russo L, et al. Central pathology laboratory review of HER2 and ER in early breast cancer: an ALTTO trial [BIG 2-06/NCCTG N063D (Alliance)] ring study. Breast Cancer Res Treat. 2014;143:485–92.
Perez EA, Press MF, Dueck AC, Jenkins RB, Kim C, Chen B, et al. Immunohistochemistry and fluorescence in situ hybridization assessment of HER2 in clinical trials of adjuvant therapy for breast cancer (NCCTG N9831, BCIRG 006, and BCIRG 005). Breast Cancer Res Treat. 2013;138:99–108.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. Arch Pathol Lab Med. 2014;138:241–56.
Taylor CR, Levenson RM. Quantification of immunohistochemistry - issues concerning methods, utility and semiquantitative assessment II. Histopathology. 2006;49:411–24.
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–45.
Engel KB, Moore HM. Effects of preanalytical variables on the detection of proteins by immunohistochemistry in formalin-fixed, paraffin-embedded tissue. Arch Pathol Lab Med. 2011;135:537–43.
Khoury T. Delay to formalin fixation alters morphology and immunohistochemistry for breast carcinoma. Appl Immunohistochem Mol Morphol. 2012;20:531–42.
Portier BP, Wang Z, Downs-Kelly E, Rowe JJ, Patil D, Lanigan C, et al. Delay to formalin fixation 'cold ischemia time': effect on ERBB2 detection by in-situ hybridization and immunohistochemistry. Mod Pathol. 2013;26:1–9.
Camp RL, Chung GG, Rimm DL. Automated subcellular localization and quantification of protein expression in tissue microarrays. Nat Med. 2002;8:1323–7.
Gustavson MD, Bourke-Martin B, Reilly D, Cregger M, Williams C, Mayotte J, et al. Standardization of HER2 immunohistochemistry in breast cancer by automated quantitative analysis. Arch Pathol Laboratory Med. 2009;133:1413–9.
McCabe A, Dolled-Filhart M, Camp RL, Rimm DL. Automated quantitative analysis (AQUA) of in situ protein expression, antibody concentration, and prognosis. J Natl Cancer Inst. 2005;97:1808–15.
Colomer R, Llombart-Cussac A, Lluch A, Barnadas A, Ojeda B, Caranana V, et al. Biweekly paclitaxel plus gemcitabine in advanced breast cancer: phase II trial and predictive value of HER2 extracellular domain. Ann Oncol. 2004;15:201–6.
Kostler WJ, Steger GG, Soleiman A, Schwab B, Singer CF, Tomek S, et al. Monitoring of serum Her-2/neu predicts histopathological response to neoadjuvant trastuzumab-based therapy for breast cancer. Anticancer Res. 2004;24(2C):1127–30.
Lennon S, Barton C, Banken L, Gianni L, Marty M, Baselga J, et al. Utility of serum HER2 extracellular domain assessment in clinical decision making: pooled analysis of four trials of trastuzumab in metastatic breast cancer. J Clin Oncol. 2009;27:1685–93.
Huang W, Reinholz M, Weidler J, Yolanda L, Paquet A, Whitcomb J, et al. Comparison of central HER2 testing with quantitative total HER2 expression and HER2 homodimer measurements using a novel proximity-based assay. Am J Clin Pathol. 2010;134:303–11.
Shi Y, Huang W, Tan Y, Jin X, Dua R, Penuel E, et al. A novel proximity assay for the detection of proteins and protein complexes: quantitation of HER1 and HER2 total protein expression and homodimerization in formalin-fixed, paraffin-embedded cell lines and breast cancer tissue. Diagn Mol Pathol. 2009;18:11–21.
DeFazio-Eli L, Strommen K, Dao-Pick T, Parry G, Goodman L, Winslow J. Quantitative assays for the measurement of HER1-HER2 heterodimerization and phosphorylation in cell lines and breast tumors: applications for diagnostics and targeted drug mechanism of action. Breast Cancer Res. 2011;13:R44.
Dua R, Zhang J, Nhonthachit P, Penuel E, Petropoulos C, Parry G. EGFR over-expression and activation in high HER2, ER negative breast cancer cell line induces trastuzumab resistance. Breast Cancer Res Treat. 2010;122:685–97.
Sperinde J, Jin X, Banerjee J, Penuel E, Saha A, Diedrich G, et al. Quantitation of p95HER2 in paraffin sections by using a p95-specific antibody and correlation with outcome in a cohort of trastuzumab-treated breast cancer patients. Clin Cancer Res. 2010;16:4226–35.
Mukherjee A, Badal Y, Nguyen XT, Miller J, Chenna A, Tahir H, et al. Profiling the HER3/PI3K pathway in breast tumors using proximity-directed assays identifies correlations between protein complexes and phosphoproteins. PLoS One. 2011;6:e16443.
Arkin MR, Wells JA. Small-molecule inhibitors of protein-protein interactions: progressing towards the dream. Nat Rev Drug Discov. 2004;3:301–17.
Tovar C, Rosinski J, Filipovic Z, Higgins B, Kolinsky K, Hilton H, et al. From the Cover: Small-molecule MDM2 antagonists reveal aberrant p53 signaling in cancer: implications for therapy. Proc Natl Acad Sci U S A. 2006;103:1888–93.
Vassilev LT, Vu BT, Graves B, Carvajal D, Podlaski F, Filipovic Z, et al. In vivo activation of the p53 pathway by small-molecule antagonists of MDM2. Science. 2004;303:844–8.
Solit DB, Rosen N. Resistance to BRAF inhibition in melanomas. N Engl J Med. 2011;364:772–4.
Chuang HY, Lee E, Liu YT, Lee D, Ideker T. Network-based classification of breast cancer metastasis. Mol Syst Biol. 2007;3:140.
Taylor IW, Linding R, Warde-Farley D, Liu Y, Pesquita C, Faria D, et al. Dynamic modularity in protein interaction networks predicts breast cancer outcome. Nat Biotechnol. 2009;27:199–204.
Peter M, Ameer-Beg SM, Hughes MK, Keppler MD, Prag S, Marsh M, et al. Multiphoton-FLIM quantification of the EGFP-mRFP1 FRET pair for localization of membrane receptor-kinase interactions. Biophys J. 2005;88:1224–37.
Barber PR, Ameer-Beg SM, Gilbey J, Carlin LM, Keppler M, Ng TC, et al. Multiphoton time-domain fluorescence lifetime imaging microscopy: practical application to protein-protein interactions using global analysis. J R Soc Interface. 2008;6:S93–S105.
Kelleher MT, Fruhwirth G, Patel G, Ofo E, Festy F, Barber PR, et al. The potential of optical proteomic technologies to individualize prognosis and guide rational treatment for cancer patients. Target Oncol. 2009;4:235–52.
Fruhwirth GO, Fernandes LP, Weitsman G, Patel G, Kelleher M, Lawler K, et al. How Forster resonance energy transfer imaging improves the understanding of protein interaction networks in cancer biology. Chemphyschem. 2011;12:442–61.
Anilkumar N, Parsons M, Monk R, Ng T, Adams JC. Interaction of fascin and protein kinase Calpha: a novel intersection in cell adhesion and motility. EMBO J. 2003;22:5390–402.
Legg JW, Lewis CA, Parsons M, Ng T, Isacke CM. A novel PKC-regulated mechanism controls CD44 ezrin association and directional cell motility. Nat Cell Biol. 2002;4:399–407.
Ng T, Parsons M, Hughes WE, Monypenny J, Zicha D, Gautreau A, et al. Ezrin is a downstream effector of trafficking PKC-integrin complexes involved in the control of cell motility. EMBO J. 2001;20:2723–41.
Ng T, Squire A, Hansra G, Bornancin F, Prevostel C, Hanby A, et al. Imaging protein kinase Calpha activation in cells. Science. 1999;283:2085–9.
Parsons M, Keppler MD, Kline A, Messent A, Humphries MJ, Gilchrist R, et al. Site-directed perturbation of protein kinase C-integrin interaction blocks carcinoma cell chemotaxis. Mol Cell Biol. 2002;22:5897–911.
Parsons M, Monypenny J, Ameer-Beg SM, Millard TH, Machesky LM, Peter M, et al. Spatially distinct binding of Cdc42 to PAK1 and N-WASP in breast carcinoma cells. Mol Cell Biol. 2005;25:1680–95.
Prag S, Parsons M, Keppler MD, Ameer-Beg SM, Barber P, Hunt J, et al. Activated ezrin promotes cell migration through recruitment of the GEF Dbl to lipid rafts and preferential downstream activation of Cdc42. Mol Biol Cell. 2007;18:2935–48.
Ganesan S, Ameer-Beg SM, Ng TT, Vojnovic B, Wouters FS. A dark yellow fluorescent protein (YFP)-based Resonance Energy-Accepting Chromoprotein (REACh) for Forster resonance energy transfer with GFP. Proc Natl Acad Sci U S A. 2006;103:4089–94.
Dadke S, Cotteret S, Yip SC, Jaffer ZM, Haj F, Ivanov A, et al. Regulation of protein tyrosine phosphatase 1B by sumoylation. Nat Cell Biol. 2007;9:80–5.
Makrogianneli K, Carlin LM, Keppler MD, Matthews DR, Ofo E, Coolen A, et al. Integrating receptor signal inputs that influence small Rho GTPase activation dynamics at the immunological synapse. Mol Cell Biol. 2009;29:2997–3006.
Morris JR, Boutell C, Keppler M, Densham R, Weekes D, Alamshah A, et al. The SUMO modification pathway is involved in the BRCA1 response to genotoxic stress. Nature. 2009;462:886–90.
Carlin LM, Evans R, Milewicz H, Fernandes L, Matthews DR, Perani M, et al. A targeted siRNA screen identifies regulators of Cdc42 activity at the natural killer cell immunological synapse. Sci Signal. 2011;4:ra81.
Keese M, Magdeburg RJ, Herzog T, Hasenberg T, Offterdinger M, Pepperkok R, et al. Imaging epidermal growth factor receptor phosphorylation in human colorectal cancer cells and human tissues. J Biol Chem. 2005;280:27826–31.
Kong A, Leboucher P, Leek R, Calleja V, Winter S, Harris A, et al. Prognostic value of an activation state marker for epidermal growth factor receptor in tissue microarrays of head and neck cancer. Cancer Res. 2006;66:2834–43.
Parsons M, Ng T. Intracellular coupling of adhesion receptors: molecular proximity measurements. Methods Cell Biol. 2002;69:261–78.
Barber PR, Tullis ID, Pierce GP, Newman RG, Prentice J, Rowley MI, et al. The Gray Institute 'open' high-content, fluorescence lifetime microscopes. J Microsc. 2013;251:154–67.
Weitsman G, Lawler K, Kelleher M, Barrett J, Barber PR, Shamil E, et al. Imaging tumour heterogeneity of the consequence of a PKC-substrate interaction in breast cancer patients. Biochem Soc Trans. 2014;in press.
Berezin MY, Achilefu S. Fluorescence lifetime measurements and biological imaging. Chem Rev. 2010;110:2641–84.
Barber PR, Tullis IDC, Rowley MI, Martins CD, Weitsman G, Lawler K, et al. The Gray Institute open microscopes applied to radiobiology and protein interaction studies. In: Brown TG, Cogswell CJ, Wilson T, editors. SPIE Proceedings. Volume 8949. Three-Dimensional and Multidimensional Microscopy: Image Acquisition and Processing XXI. 2014;in press.
Tao J, Castel P, Radosevic-Robin N, Elkabets M, Auricchio N, Aceto N, et al. Blockade of EGFR and HER3 enhances PI3K/Akt anti-tumor activity in triple negative breast cancer. Sci Signal. 2014;7:ra29.
Kiuchi T, Ortiz-Zapater E, Monypenny J, Matthews DR, Nguyen LK, Barbeau J, et al. The ErbB4 CYT2 variant protects EGFR from ligand-induced degradation to enhance cancer cell motility. Sci Signal. 2014;7:ra78.
Aebersold R, Mann M. Mass spectrometry-based proteomics. Nature. 2003;422:198–207.
Domon B, Aebersold R. Mass spectrometry and protein analysis. Science. 2006;312:212–7.
Addona TA, Abbatiello SE, Schilling B, Skates SJ, Mani DR, Bunk DM, et al. Multi-site assessment of the precision and reproducibility of multiple reaction monitoring-based measurements of proteins in plasma. Nat Biotechnol. 2009;27:633–41.
Nilsson T, Mann M, Aebersold R, Yates 3rd JR, Bairoch A, Bergeron JJ. Mass spectrometry in high-throughput proteomics: ready for the big time. Nat Methods. 2010;7:681–5.
Rudnick PA, Clauser KR, Kilpatrick LE, Tchekhovskoi DV, Neta P, Blonder N, et al. Performance metrics for liquid chromatography-tandem mass spectrometry systems in proteomics analyses. Mol Cell Proteomics. 2010;9:225–41.
Keshishian H, Addona T, Burgess M, Kuhn E, Carr SA. Quantitative, multiplexed assays for low abundance proteins in plasma by targeted mass spectrometry and stable isotope dilution. Mol Cell Proteomics. 2007;6:2212–29.
Bateman NW, Sun M, Bhargava R, Hood BL, Darfler MM, Kovatich AJ, et al. Differential proteomic analysis of late-stage and recurrent breast cancer from formalin-fixed paraffin-embedded tissues. J Proteome Res. 2011;10:1323–32.
Prieto DA, Hood BL, Darfler MM, Guiel TG, Lucas DA, Conrads TP, et al. Liquid Tissue: proteomic profiling of formalin-fixed tissues. Biotechniques. 2005;Suppl:32–5.
Hood BL, Darfler MM, Guiel TG, Furusato B, Lucas DA, Ringeisen BR, et al. Proteomic analysis of formalin-fixed prostate cancer tissue. Mol Cell Proteomics. 2005;4:1741–53.
Hembrough T, Thyparambil S, Liao WL, Darfler MM, Abdo J, Bengali KM, et al. Application of selected reaction monitoring for multiplex quantification of clinically validated biomarkers in formalin-fixed, paraffin-embedded tumor tissue. J Mol Diagn. 2013;15:454–65.
Huang SK, Darfler MM, Nicholl MB, You J, Bemis KG, Tegeler TJ, et al. LC/MS-based quantitative proteomic analysis of paraffin-embedded archival melanomas reveals potential proteomic biomarkers associated with metastasis. PLoS One. 2009;4:e4430.
Bateman NW, Sun M, Hood BL, Flint MS, Conrads TP. Defining central themes in breast cancer biology by differential proteomics: conserved regulation of cell spreading and focal adhesion kinase. J Proteome Res. 2010;9:5311–24.
Cheung W, Darfler MM, Alvarez H, Hood BL, Conrads TP, Habbe N, et al. Application of a global proteomic approach to archival precursor lesions: deleted in malignant brain tumors 1 and tissue transglutaminase 2 are upregulated in pancreatic cancer precursors. Pancreatology. 2008;8:608–16.
DeSouza LV, Krakovska O, Darfler MM, Krizman DB, Romaschin AD, Colgan TJ, et al. mTRAQ-based quantification of potential endometrial carcinoma biomarkers from archived formalin-fixed paraffin-embedded tissues. Proteomics. 2010;10:3108–16.
Hembrough T, Thyparambil S, Liao WL, Darfler MM, Abdo J, Bengali KM, et al. Selected reaction monitoring (SRM) analysis of epidermal growth factor receptor (EGFR) in formalin fixed tumor tissue. Clin Proteomics. 2012;9:5.
Patel BN, Sharma N, Sanyal M, Shrivastav PS. High throughput and sensitive determination of trazodone and its primary metabolite, m-chlorophenylpiperazine, in human plasma by liquid chromatography-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2008;871:44–54.
Spurrier B, Ramalingam S, Nishizuka S. Reverse-phase protein lysate microarrays for cell signaling analysis. Nat Protocols. 2008;3:1796–808.
Kim P, Liu X, Lee T, Liu L, Barham R, Kirkland R, et al. Highly sensitive proximity mediated immunoassay reveals HER2 status conversion in the circulating tumor cells of metastatic breast cancer patients. Proc Natl Acad Sci U S A. 2011;9:75.
Arnould L, Denoux Y, MacGrogan G, Penault-Llorca F, Fiche M, Treilleux I, et al. Agreement between chromogenic in situ hybridisation (CISH) and FISH in the determination of HER2 status in breast cancer. Br J Cancer. 2003;88:1587–91.
Bartlett JM, Campbell FM, Ibrahim M, Wencyk P, Ellis I, Kay E, et al. Chromogenic in situ hybridization: a multicenter study comparing silver in situ hybridization with FISH. Am J Clin Pathol. 2009;132:514–20.
Francis GD, Jones MA, Beadle GF, Stein SR. Bright-field in situ hybridization for HER2 gene amplification in breast cancer using tissue microarrays: correlation between chromogenic (CISH) and automated silver-enhanced (SISH) methods with patient outcome. Diagn Mol Pathol. 2009;18:88–95.
Hanna WM, Kwok K. Chromogenic in-situ hybridization: a viable alternative to fluorescence in-situ hybridization in the HER2 testing algorithm. Modern Pathol. 2006;19:481–7.
Lebeau A, Deimling D, Kaltz C, Sendelhofert A, Iff A, Luthardt B, et al. Her-2/neu analysis in archival tissue samples of human breast cancer: comparison of immunohistochemistry and fluorescence in situ hybridization. J Clin Oncol. 2001;19:354–63.
Pauletti G, Dandekar S, Rong H, Ramos L, Peng H, Seshadri R, et al. Assessment of methods for tissue-based detection of the HER-2/neu alteration in human breast cancer: a direct comparison of fluorescence in situ hybridization and immunohistochemistry. J Clin Oncol. 2000;18:3651–64.
Brugmann A, Lelkaitis G, Nielsen S, Jensen KG, Jensen V. Testing HER2 in breast cancer: a comparative study on BRISH, FISH, and IHC. Appl Immunohistochem Mol Morphol. 2011;19:203–11.
Hanna WM, Ruschoff J, Bilous M, Coudry RA, Dowsett M, Osamura RY, et al. HER2 in situ hybridization in breast cancer: clinical implications of polysomy 17 and genetic heterogeneity. Mod Pathol. 2014;27:4–18.
Moelans CB, de Weger RA, van Diest PJ. Absence of chromosome 17 polysomy in breast cancer: analysis by CEP17 chromogenic in situ hybridization and multiplex ligation-dependent probe amplification. Breast Cancer Res Treat. 2010;120:1–7.
Yeh IT, Martin MA, Robetorye RS, Bolla AR, McCaskill C, Shah RK, et al. Clinical validation of an array CGH test for HER2 status in breast cancer reveals that polysomy 17 is a rare event. Modern Pathol. 2009;22:1169–75.
Franchet C, Filleron T, Cayre A, Mounie E, Penault-Llorca F, Jacquemier J, et al. Instant-quality fluorescence in-situ hybridization as a new tool for HER2 testing in breast cancer: a comparative study. Histopathology. 2014;64:274–83.
Schouten JP, McElgunn CJ, Waaijer R, Zwijnenburg D, Diepvens F, Pals G. Relative quantification of 40 nucleic acid sequences by multiplex ligation-dependent probe amplification. Nucleic Acids Res. 2002;30:e57.
Moerland E, van Hezik RL, van der Aa TC, van Beek MW, van den Brule AJ. Detection of HER2 amplification in breast carcinomas: comparison of multiplex ligation-dependent probe amplification (MLPA) and fluorescence in situ hybridization (FISH) combined with automated spot counting. Cell Oncol. 2006;28:151–9.
Moelans CB, de Weger RA, Ezendam C, van Diest PJ. HER-2/neu amplification testing in breast cancer by multiplex ligation-dependent probe amplification: influence of manual- and laser microdissection. BMC Cancer. 2009;9:4.
Moelans CB, de Weger RA, van Blokland MT, van der Wall E, van Diest PJ. Simultaneous detection of TOP2A and HER2 gene amplification by multiplex ligation-dependent probe amplification in breast cancer. Modern Pathol. 2010;23:62–70.
Kuijpers CC, Moelans CB, van Slooten HJ, Horstman A, Hinrichs JW, Al-Janabi S, et al. Added value of HER-2 amplification testing by multiplex ligation-dependent probe amplification in invasive breast cancer. PLoS One. 2013;8:e82018.
Jackisch C, Untch M. Systemic therapy for women with ErbB2-positive breast cancer: new options, new challenges. Breast Care (Basel). 2010;5(s1):1–2.
Baehner FL, Achacoso N, Maddala T, Shak S, Quesenberry Jr CP, Goldstein LC, et al. Human epidermal growth factor receptor 2 assessment in a case–control study: comparison of fluorescence in situ hybridization and quantitative reverse transcription polymerase chain reaction performed by central laboratories. J Clin Oncol. 2010;28:4300–6.
Perez E, Butler S, Dueck A, Baehner F, Cherbavaz D, Thompson E, et al. The relationship between quantitative HER2 gene expression by the 21-gene RT-PCR assay and adjuvant trastuzumab (H) benefit in NCCTG (Alliance) N9831. J Clin Oncol. 2013;31:520.
Dabbs DJ, Klein ME, Mohsin SK, Tubbs RR, Shuai Y, Bhargava R. High false-negative rate of HER2 quantitative reverse transcription polymerase chain reaction of the Oncotype DX test: an independent quality assurance study. J Clin Oncol. 2011;29:4279–85.
Ach RA, Floore A, Curry B, Lazar V, Glas AM, Pover R, et al. Robust interlaboratory reproducibility of a gene expression signature measurement consistent with the needs of a new generation of diagnostic tools. BMC Genomics. 2007;8:148.
Glas AM, Floore A, Delahaye LJ, Witteveen AT, Pover RC, Bakx N, et al. Converting a breast cancer microarray signature into a high-throughput diagnostic test. BMC Genomics. 2006;7:278.
Roepman P, Horlings HM, Krijgsman O, Kok M, Bueno-de-Mesquita JM, Bender R, et al. Microarray-based determination of estrogen receptor, progesterone receptor, and HER2 receptor status in breast cancer. Clin Cancer Res. 2009;15:7003–11.
Majidzadeh AK, Esmaeili R, Abdoli N. TFRC and ACTB as the best reference genes to quantify Urokinase Plasminogen Activator in breast cancer. BMC Res Notes. 2011;4:215.
Parker JS, Mullins M, Cheang MC, Leung S, Voduc D, Vickery T, et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol. 2009;27:1160–7.
Nielsen TO, Parker JS, Leung S, Voduc D, Ebbert M, Vickery T, et al. A comparison of PAM50 intrinsic subtyping with immunohistochemistry and clinical prognostic factors in tamoxifen-treated estrogen receptor-positive breast cancer. Clin Cancer Res. 2010;16:5222–32.
Dowsett M, Sestak I, Lopez-Knowles E, Sidhu K, Dunbier AK, Cowens JW, et al. Comparison of PAM50 risk of recurrence score with oncotype DX and IHC4 for predicting risk of distant recurrence after endocrine therapy. J Clin Oncol. 2013;31:2783–90.
Filipits M, Nielsen TO, Rudas M, Greil R, Stoger H, Jakesz R, et al. The PAM50 risk-of-recurrence score predicts risk for late distant recurrence after endocrine therapy in postmenopausal women with endocrine-responsive early breast cancer. Clin Cancer Res. 2014;20:1298–305.
Gnant M, Filipits M, Greil R, Stoeger H, Rudas M, Bago-Horvath Z, et al. Predicting distant recurrence in receptor-positive breast cancer patients with limited clinicopathological risk: using the PAM50 Risk of Recurrence score in 1478 postmenopausal patients of the ABCSG-8 trial treated with adjuvant endocrine therapy alone. Ann Oncol. 2014;25:339–45.
Geiss GK, Bumgarner RE, Birditt B, Dahl T, Dowidar N, Dunaway DL, et al. Direct multiplexed measurement of gene expression with color-coded probe pairs. Nat Biotechnol. 2008;26:317–25.
Reis PP, Waldron L, Goswami RS, Xu W, Xuan Y, Perez-Ordonez B, et al. mRNA transcript quantification in archival samples using multiplexed, color-coded probes. BMC Biotechnol. 2011;11:46.
Bastien RR, Rodriguez-Lescure A, Ebbert MT, Prat A, Munarriz B, Rowe L, et al. PAM50 breast cancer subtyping by RT-qPCR and concordance with standard clinical molecular markers. BMC Med Genomics. 2012;5:44.
Cheang MC, Voduc KD, Tu D, Jiang S, Leung S, Chia SK, et al. Responsiveness of intrinsic subtypes to adjuvant anthracycline substitution in the NCIC.CTG MA.5 randomized trial. Clin Cancer Res. 2012;18:2402–12.
Benohr P, Henkel V, Speer R, Vogel U, Sotlar K, Aydeniz B, et al. Her-2/neu expression in breast cancer - a comparison of different diagnostic methods. Anticancer Res. 2005;25(3B):1895–900.
Gjerdrum LM, Sorensen BS, Kjeldsen E, Sorensen FB, Nexo E, Hamilton-Dutoit S. Real-time quantitative PCR of microdissected paraffin-embedded breast carcinoma: an alternative method for HER-2/neu analysis. J Mol Diagn. 2004;6:42–51.
Christopherson C, Chang M, Eberhard DA, Sninsky JJ, Anderson SM, Wang AM, et al. Comparison of immunohistochemistry (IHC) and quantitative RT-PCR: ER, PR, and HER2 receptor status. J Clin Oncol. 2012;30:abstr 47.
Elloumi F, Hu Z, Li Y, Parker JS, Gulley ML, Amos KD, et al. Systematic bias in genomic classification due to contaminating non-neoplastic tissue in breast tumor samples. BMC Med Genomics. 2011;4:54.
Toi M, Sperinde J, Huang W, Saji S, Winslow J, Jin X, et al. Differential survival following trastuzumab treatment based on quantitative HER2 expression and HER2 homodimers in a clinic-based cohort of patients with metastatic breast cancer. BMC Cancer. 2010;10:56.
Cheng H, Bai YL, Sikov W, Sinclair N, Bossuyt V, Abu-Khalaf MM, et al. Quantitative measurements of HER2 and phospho-HER2 expression: correlation with pathologic response to neoadjuvant chemotherapy and trastuzumab. BMC Cancer. 2014;14:326.
Montemurro F, Prat A, Rossi V, Valabrega G, Sperinde J, Peraldo-Neia C, et al. Potential biomarkers of long-term benefit from single-agent trastuzumab or lapatinib in HER2-positive metastatic breast cancer. Mol Oncol. 2014;8:20–6.
Duchnowska R, Biernat W, Szostakiewicz B, Sperinde J, Piette F, Haddad M, et al. Correlation between quantitative HER-2 protein expression and risk for brain metastases in HER-2+ advanced breast cancer patients receiving trastuzumab-containing therapy. Oncologist. 2012;17:26–35.
Lipton A, Kostler WJ, Leitzel K, Ali SM, Sperinde J, Weidler J, et al. Quantitative HER2 protein levels predict outcome in fluorescence in situ hybridization-positive patients with metastatic breast cancer treated with trastuzumab. Cancer. 2010;116:5168–78.
Nuciforo P, Thyparambil S, Garrido-Castro A, Peg V, Prudkin L, Jimenez J, et al. Correlation of high levels of HER2 measured by multiplex mass spectrometry with increased overall survival in patients treated with anti-HER2-based therapy. J Clin Oncol. 2014;32:649.
Christiansen J, Barakat N, Murphy D, Rimm D, Dabbas B, Nerenberg M, et al. Her2 expression measured by AQUA analysis on BCIRG-005 and BCIRG-006 predicts the benefit of Herceptin therapy. Cancer Res. 2012;72:PD02-01.
Guiu S, Gauthier M, Coudert B, Bonnetain F, Favier L, Ladoire S, et al. Pathological complete response and survival according to the level of HER-2 amplification after trastuzumab-based neoadjuvant therapy for breast cancer. Br J Cancer. 2010;103:1335–42.
Perez EA, Reinholz MM, Hillman DW, Tenner KS, Schroeder MJ, Davidson NE, et al. HER2 and chromosome 17 effect on patient outcome in the N9831 adjuvant trastuzumab trial. J Clin Oncol. 2010;28:4307–15.
Press MF, Finn RS, Cameron D, Di Leo A, Geyer CE, Villalobos IE, et al. HER-2 gene amplification, HER-2 and epidermal growth factor receptor mRNA and protein expression, and lapatinib efficacy in women with metastatic breast cancer. Clin Cancer Res. 2008;14:7861–70.
Bates M, Sperinde J, Kostler WJ, Ali SM, Leitzel K, Fuchs EM, et al. Identification of a subpopulation of metastatic breast cancer patients with very high HER2 expression levels and possible resistance to trastuzumab. Ann Oncol. 2011;22:2014–20.
Joensuu H, Sperinde J, Leinonen M, Huang W, Weidler J, Bono P, et al. Very high quantitative tumor HER2 content and outcome in early breast cancer. Ann Oncol. 2011;22:2007–13.
Gullo G, Bettio D, Torri V, Masci G, Salvini P, Santoro A. Level of HER2/neu gene amplification as a predictive factor of response to trastuzumab-based therapy in patients with HER2-positive metastatic breast cancer. Invest New Drugs. 2009;27:179–83.
Dowsett M, Procter M, McCaskill-Stevens W, de Azambuja E, Dafni U, Rueschoff J, et al. Disease-free survival according to degree of HER2 amplification for patients treated with adjuvant chemotherapy with or without 1 year of trastuzumab: the HERA Trial. J Clin Oncol. 2009;27:2962–9.
Paik S, Kim C, Wolmark N. HER2 status and benefit from adjuvant trastuzumab in breast cancer. N Engl J Med. 2008;358:1409–11.
Romond EH, Perez EA, Bryant J, Suman VJ, Geyer Jr CE, Davidson NE, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005;353:1673–84.
Pogue-Geile KL, Kim C, Jeong JH, Tanaka N, Bandos H, Gavin PG, et al. Predicting Degree of Benefit From Adjuvant Trastuzumab in NSABP Trial B-31. J Natl Cancer Inst. 2013;105:1782–8.
Scaltriti M, Nuciforo P, Bradbury I, Sperinde J, Agbor-Tarh D, Campbell C, et al. High HER2 expression correlates with response to the combination of lapatinib and trastuzumab. Clin Cancer Res. 2015;21:569–76.
Scaltriti M, Verma C, Guzman M, Jimenez J, Parra JL, Pedersen K, et al. Lapatinib, a HER2 tyrosine kinase inhibitor, induces stabilization and accumulation of HER2 and potentiates trastuzumab-dependent cell cytotoxicity. Oncogene. 2009;28:803–14.
Jura N, Shan Y, Cao X, Shaw DE, Kuriyan J. Structural analysis of the catalytically inactive kinase domain of the human EGF receptor 3. Proc Natl Acad Sci U S A. 2009;106:21608–13.
Aertgeerts K, Skene R, Yano J, Sang BC, Zou H, Snell G, et al. Structural analysis of the mechanism of inhibition and allosteric activation of the kinase domain of HER2 protein. J Biol Chem. 2011;286:18756–65.
Garrett JT, Olivares MG, Rinehart C, Granja-Ingram ND, Sanchez V, Chakrabarty A, et al. Transcriptional and posttranslational up-regulation of HER3 (ErbB3) compensates for inhibition of the HER2 tyrosine kinase. Proc Natl Acad Sci U S A. 2011;108:5021–6.
Cheng H, Ballman K, Vassilakopoulou M, Dueck AC, Reinholz MM, Tenner K, et al. EGFR expression is associated with decreased benefit from trastuzumab in the NCCTG N9831 (Alliance) trial. Br J Cancer. 2014;111:1065–71.
Mittendorf EA, Wu Y, Scaltriti M, Meric-Bernstam F, Hunt KK, Dawood S, et al. Loss of HER2 amplification following trastuzumab-based neoadjuvant systemic therapy and survival outcomes. Clin Cancer Res. 2009;15:7381–8.
Piccart-Gebhart M, Holmes A, Baselga J, De Azambuja E, Dueck A, Viale G, et al. First results from the phase III ALTTO trial (BIG 2–06; NCCTG [Alliance] N063D) comparing one year of anti-HER2 therapy with lapatinib alone (L), trastuzumab alone (T), their sequence (T→L), or their combination (T+L) in the adjuvant treatment of HER2-positive early breast cancer (EBC). J Clin Oncol. 2014;32:LBA2.
Carey L, Winer E, Viale G, Cameron D, Gianni L. Triple-negative breast cancer: disease entity or title of convenience? Nat Rev Clin Oncol. 2010;7:683–92.
Acknowledgments
We want to acknowledge the support from the Tumor Biomarkers Research Program funded by the Banco Bilbao Vizcaya Argentaria (BBVA) Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Additional file
Additional file 1:
A table listing laboratory diagnostic tests cleared by the Food and Drug Administration or offered by central laboratories under Clinical Laboratory Improvement Amendments measuring HER receptors in the clinic. *Epidermal growth factor (EGFR), HER2 and HER3. #Approved for colorectal cancer. LDT, laboratory developed test; Q, quantitative; QL, qualitative; SQ, semiquantitative.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Nuciforo, P., Radosevic-Robin, N., Ng, T. et al. Quantification of HER family receptors in breast cancer. Breast Cancer Res 17, 53 (2015). https://doi.org/10.1186/s13058-015-0561-8
Published:
DOI: https://doi.org/10.1186/s13058-015-0561-8