Abstract
Sepsis is a potentially fatal condition caused by dysregulation of the body's immune response to an infection. Sepsis-induced liver injury is considered a strong independent prognosticator of death in the critical care unit, and there is anatomic and accumulating epidemiologic evidence that demonstrates intimate cross talk between the gut and the liver. Intestinal barrier disruption and gut microbiota dysbiosis during sepsis result in translocation of intestinal pathogen-associated molecular patterns and damage-associated molecular patterns into the liver and systemic circulation. The liver is essential for regulating immune defense during systemic infections via mechanisms such as bacterial clearance, lipopolysaccharide detoxification, cytokine and acute-phase protein release, and inflammation metabolic regulation. When an inappropriate immune response or overwhelming inflammation occurs in the liver, the impaired capacity for pathogen clearance and hepatic metabolic disturbance can result in further impairment of the intestinal barrier and increased disruption of the composition and diversity of the gut microbiota. Therefore, interaction between the gut and liver is a potential therapeutic target. This review outlines the intimate gut–liver cross talk (gut–liver axis) in sepsis.
Similar content being viewed by others
Introduction
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection, with high morbidity and mortality worldwide [1]. Indeed, 2.8 million deaths per year are attributable to sepsis in high-income countries [2]. Sepsis can progress to multiple organ dysfunction syndrome (MODS) [3]. Liver dysfunction in MODS patients is typically associated with significant morbidity, though its exact prevalence remains unknown.
The gut microbiota is recognized as a powerful indicator of disease-related morbidity and progression [4]. For instance, Lachnospiraceae contributes to protecting the intestinal mucosal barrier and offers a microbe-mediated survival advantage in a murine model of sepsis [5]. Bifidobacterium, Muribaculaceae, Parabacteroides distasonis, and Alloprevotella are involved in protection against sepsis-related liver injury in rats [6]. The gut microbiota is key to the development and regulation of the immune system, impacting host susceptibility and response to infection [7]. Intestinal dysbiosis and increased intestinal permeability promote pathogenic microbial overgrowth and translocation of intestinal pathogen-associated molecular patterns (PAMPs) to the lymphatic and portal systems, impairing the body’s defense against infection or injury and aggravating organ damage [8]. Cross talk between the gut and liver is widely acknowledged, as the gut and liver communicate bidirectionally via biliary, portal, and systemic circulation [9]. Moreover, intestinal mucosa and vascular barriers serve as a communication hub between the gut and liver. The liver is crucial for modifying the host defense and controlling inflammation in infection [10]. However, under pathological situations, dysregulated translocation of microbial products initiates inflammation that impairs the function and detoxification capacity of hepatocytes. In general, liver dysfunction, decreased bacterial clearance, and metabolic disorders cause increased dysregulation of the gut microbiota and further breakdown of the intestinal barrier, leading to MODS. Hence, improved knowledge of the gut–liver interaction during sepsis-induced liver damage might contribute to elucidating these complicated disorders and provide insight into novel treatment approaches for sepsis that target underlying mechanisms.
Intestinal barrier
Physical barrier
The presence of intestinal epithelial cells (IECs) and mucus components serves as a first line of defense to maintain the intestinal barrier. The epithelial and intestinal vascular barrier just below the mucus is composed of a monolayer of cells [11], and this epithelium monolayer acts as a protective barrier, restricting pathogens, toxins, and antigens of the gut lumen from passing into the mesenteric lymph and circulation [12, 13]. Although the epithelium monolayer serves as a primary physical barrier, the paracellular gap is regulated by several intercellular connections, including apical tight junctions (TJs), lower adherens junctions, and desmosomes [14, 15]. Of note, the TJ structure is critical in providing a physical barrier to prevent luminal inflammatory molecules from entering the circulation [16].
Mucus covers the entire intestinal surface, which is composed of goblet cell-derived mucins (MUCs). The small intestine is covered with a single mucus layer, whereas the large intestine contains two major mucus layers, with the inner dense mucus layer working mainly as a protective shield for the gut owing to its impermeability to luminal bacteria [17, 18]. Mucus supplies carbohydrates for commensal bacteria, inhibits epithelial apoptosis, and increases release of immune cell components by acting as a viscous trap for antimicrobial peptides and immunoglobulins [19,20,21]. MUC2 is a key element of intestinal mucus layers. Muc2 in mice deficiency exacerbates sublethal doses of lipopolysaccharide (LPS)-induced intestinal bacterial translocation to the liver and increases mortality [22].
Furthermore, the intestinal epithelium generates large amounts of antimicrobial peptides (AMPs) and intestinal alkaline phosphatases (IAPs) [23, 24]. AMPs rapidly kill or inactivate bacteria by secreting lysozyme, regulating downstream innate immune responses, and interfering with bacterial cell wall synthesis, among others, which is a method of immune defense that has evolved over time [23].
IAPs can prevent the follow-up toxicity of newly released LPS [24], regulate HCO3– secretion [25], and promote growth of gut commensal bacteria [26]. Notably, IAPs also prevent LPS from triggering toll-like receptor (TLR)-4/myeloid differentiation factor 88 (MyD88)-mediated inflammatory cascades [27, 28]. Recent research indicates that IAPs induce autophagy in IECs and macrophages to exert anti-inflammatory effects in mice [29].
Immune barrier
The immune cells in the gut form a second line of defense to maintain the intestinal barrier (Table 1). Anatomically, the intestinal canal wall is divided into four layers, including the mucosa, submucosa, muscularis, and serosal layer from the lumen inside to outside. Rich lymphatic follicles are present in the propria layer of the mucosal and submucosal tissues, including isolated and aggregated lymphatic follicles [30, 31]. Considering their distribution in the intestinal wall, gut immune cells mainly include intestinal lymph follicles, interepithelial lymphocytes, and lymphocytes in the propria layer of the mucosa [30, 32, 33]. The intestinal epithelial barrier is protected by local interepithelial lymphocytes, which rapidly activate T helper 1 (Th1) cell cytokine responses aimed at an infected or stressed epithelium [34, 35]. Interestingly, dendritic cells (DCs) inserted into the gut epithelium in vitro can open TJs between IECs and directly take up luminal microorganisms. Furthermore, DCs express TJ proteins to preserve epithelial barrier integrity [36]. The propria layer of the mucosa includes plasmacytoid DCs, innate lymphoid cells, mucosa-associated invariant T cells, and T cells to attack pathogens [34, 37, 38]. Secretory immunoglobulin A (IgA) plays a critical role in the adaptive immunity mediated by lamina-intrinsic plasma cells: It regulates gut microbiota composition, protects the intestinal epithelium from pathogenic microbes, and assists in immune system development [39, 40]. By presenting pathogen antigens to intestinal immune cells, IECs contribute to intestinal adaptive immunity [41].
Membranous cells are specialized epithelial antigen-presenting cells dispersed throughout the follicle-associated epithelium and are critical for antigen-specific IgA production. These gut-associated immune mechanisms protect the systemic circulation from the harmful effects of intestinal pathogens.
Commensal microbiota in intestines
Human microorganisms are diverse, with an estimated 100 trillion microorganisms composed of between 500 and 1000 distinct bacterial species [42, 43]. The majority have been verified to be composed of five phyla, mainly Firmicutes (79.4%) and Bacteroidetes (16.9%) [44]. Normally, the commensal microbiota influences the intestinal environment, limiting the growth of invasive pathogens. For instance, microbial-derived metabolites inhibit the growth of Escherichia coli O157 in vitro [45]. Commensal bacteria also produce bacteriocins that are mainly produced by Firmicutes to fight against invading pathogens [46]. Other bacteria, including Proteobacteria, Bacteroidetes, and Actinobacteria, also encode various bacteriocins. Furthermore, several bacteriocin-producing commensal bacteria (Bifidobacterium and Lactobacillus), known as probiotics, are used to promote gut health [47]. The distribution, adaptability, and function of the microbial community throughout the gastrointestinal tract are matched with different hospitable environmental conditions, allowing mutual benefits between the host and commensal microbiota.
The stomach of healthy adults has the fewest bacteria, namely Lactobacillus and Helicobacter species [48], whereas the duodenal microbiota is dominated by Firmicutes and Actinobacteria [49]. Firmicutes continues to dominate (43%) in the ileum and colon, but the abundance of Proteobacteria and Bacteroides steadily rises in the ileum and colon [50]. Compared to the small intestine, the large intestine shows greater microbial variety, though the colon tends to be occupied by two significant phyla (Bacteroidetes at 50% and Firmicutes at 45%) [51]. The gut microbial community contributes to health by reinforcing the intestinal barrier [52], and commensal bacteria protect against pathogens by competing for nutrients and space [23]. For instance, commensal Enterobacteriaceae fight against Salmonella colonization by competing for oxygen in mice [53]. Furthermore, commensal bacteria activate host pattern recognition receptors to enhance production of AMPs and MUCs [18, 23]. They also induce IgA secretion by providing modest levels of immunological stimulation, therefore establishing a basic immune adaptation that plays a crucial role in enabling the host and microbial community to live in homeostasis. Gut microbiota-generated short-chain fatty acids serve as an energy source for commensal bacteria and defend against LPS-induced intestinal barrier disturbance [54]. Overall, microbiota dysbiosis is considered a major contributor to various diseases [52].
The gut–liver axis
The physiological “gut–liver axis”
The liver is the largest gland, secreting bile acids that are ultimately discharged into the small intestine [55], and is supplied by both arterial and venous blood that mix and bathe the various liver structures and cells [56]. The oxygen-rich arterial blood enters the liver via the hepatic artery, but it is a minor blood supply for this organ. Instead, the portal vein, entering the liver with rich nutrients and pathogen-derived molecules such as LPS, is the major blood supply for the liver [57]. Normally, the liver communicates with the gut and its microbiota through the biliary system and systemic circulation (Fig. 1). The bidirectional association of the gut and its microbiota with the liver is well known as the physiological “gut–liver axis” [58].
During sepsis, several mechanisms contribute to disruption of the gut barrier, including IEC apoptosis, alteration of the mucus layer, and disruption of intercellular junctions, resulting in translocation of intestinal PAMPs into the liver via the lymphatic vessels, portal circulation, or biliary tract. The liver is essential to the regulation of immune defense, with effector cells such as LSECs, macrophages, stellate cells, and hepatocytes immediately identifying and engaging pathogens, clearing bacteria, and releasing cytokines. When an inappropriate immune response or overwhelming inflammation occurs with high levels of DAMPs and proinflammatory cytokine production in the liver, the normal structure of the hepatic sinus is disrupted, and such cells are damaged through apoptosis and autophagy, leading to bacterial clearance dysfunction and metabolic disorders. As a result, the gut barrier is further damaged, gut microbiota dysbiosis is exacerbated, and distal organs are injured due to the spread of PAMPs and DAMPs and systemic inflammation. IECs, intestinal epithelial cells; DAMPs, damage-associated molecular patterns; LSECs, liver sinusoidal endothelium; PAMPs, pathogen-associated molecular patterns
Immunological defense of the liver
The liver is also a key immune tissue, with liver sinusoidal endothelial cells (LSECs), macrophages, stellate cells, lymphocytes, and biliary cells comprising the majority of nonparenchymal cells [59,60,61,62]. LSECs constitute the inner layer of the hepatic sinus vascular or capillary bed, where nutrient-rich hepatic portal vein blood and oxygen-rich hepatic artery blood mix, contributing to immune surveillance by detecting and capturing pathogens and possibly even presenting antigens and removing macromolecular waste products from the blood [63].
Kupffer cells (KCs) constitute the majority of hepatic macrophages in a healthy liver. The yolk sac-derived colony-stimulating factor 1 receptor-positive erythro-myeloid progenitors and bone marrow-derived monocytes are both sources of KCs [64, 65]. The human liver contains two distinct macrophage subtypes: CD68+ macrophage receptor with collagen structure (MARCO)+ macrophages, which contribute to the maintenance of immunological tolerance and inflammation suppression, and CD68+ MARCO– macrophages, which are more proinflammatory [66, 67].
Effects of sepsis on the intestinal barrier and microbiota
Inflammation significantly contributes to the pathogenesis of intestinal damage in sepsis [68]. Sepsis affects expression of claudins, junctional adhesion molecule A, occludin, and zonula occludens-1 and activates myosin light-chain kinase, modulating intestinal permeability [69,70,71]. Owing to activation of TLR4 expressed on intestinal stem cells induced by PAMPs, such as LPS, sepsis may directly affect intestinal stem cell growth and apoptotic death [72, 73]. Intestinal hyperpermeability is strongly associated with dysregulated IEC apoptosis [74], causing changes to the mucus layer, such as decreased thickness, reduced luminal coverage, and poor adhesion [75]. Similarly, decreased villous length is associated with an increase in intestinal permeability and IEC apoptosis [76]. Overexpression of Bcl-2 improves survival by TJ alterations in transgenic mice with the occurrence of hyperpermeability following sepsis [77].
Disruption of intestinal physiology is followed by microbiota dysbiosis in septic patients [78]. In critically ill patients with sepsis, the diversity of the intestinal microbiota declines, and its composition becomes dominated by multidrug-resistant bacteria [79]. Broad-spectrum antibiotic treatment can significantly alter the gut microbiota of severely ill patients [80, 81]. For example, fluoroquinolones increase Lactococcus and Pediococcus but decrease Escherichia/Shigella and Desulfovibrio in critically ill patients [82].
The gut–liver axis in sepsis
Specific role of lipopolysaccharides
The human gut is a reservoir of ≥ 1 g of LPS from an estimated 100 trillion microorganisms, and endotoxin can be detected even in healthy human plasma [83]. Depending on its size, an LPS molecule passes through multiple alternative paths while crossing the small intestine, which include the paracellular pathway, clathrin-mediated endocytosis [84], micropinocytosis and lipid raft-mediated endocytosis [85], goblet cell-associated antigen passages [86], and the chylomicron pathway [87]. In the colon, LPS can be transported by clathrin-mediated or vesicle-mediated protein transport pathways [88]. When the components of the gut barrier are impacted by inflammation in sepsis, as noted in dysregulated IEC apoptosis, these defense luminal mechanisms that help prevent a large number of LPS transfers to the systemic circulation gradually fail [40], causing transmigration of LPS to multiple organs and triggering uncontrolled immunoinflammatory responses [89].
Typically, intestinal LPS passing through the portal vein is processed and detoxified by the liver. Detoxification of LPS, which is phagocytosed by scavenger receptor (SR)-mediated uptake in the liver, is carried out by acylhydrolase (AOAH) and alkaline phosphatase [90, 91]. AOAH selectively removes secondary fatty acyl chains attached to the primary chain in the lipid A fraction, playing an important role in controlling LPS toxicity [92].
Additionally, plasma contains some LPS-binding proteins with varying affinities, including LPS-binding protein (LBP), CD14, bactericidal/permeability-increasing protein (BPI), and lipoproteins engaged in LPS detoxification. LBP is primarily produced by IECs and hepatocytes in the acute phase of sepsis in mice [93]. It binds specifically to lipid A of LPS, forming the LPS-LBP complex; this facilitates LPS transfer and binding with membrane CD14 on the surface of monocytes/macrophages and neutrophils, which is finally recognized by TLR4 and myeloid differentiation-2, promoting an inflammatory response cascade [94]. Activation of TLR4 signaling, classified as MyD88 dependent, MyD88-independent, and Toll/IL-1R domain-containing adaptor-inducing interferon (IFN)-β-dependent pathways, leads to markedly increased cytokines and cell damage [95, 96] (Fig. 2). However, high plasma concentrations of LBP and soluble CD14 may help limit deleterious systemic responses to LPS [97]. BPI is expressed in the intestinal epithelium, and changes in potassium levels in damaged cells can act as damage-associated molecular patterns (DAMPs) to promote BPI expression in murine intestinal epithelium [98].
An overview of the signaling pathway of TLR4 activated by LPS. LPS recognition, as facilitated by LBP and CD14, is mediated by TLR4 and the MD-2 receptor complex. Activation of TLR4 signaling, classified into MyD88 dependent, MyD88-independent, and TRIF-dependent pathways, mediates activation of proinflammatory cytokines (TNF-α, IL-6, etc.) and type I interferon genes. IL, interleukin; LBP, LPS-binding protein; LPS, lipopolysaccharide; MD-2, myeloid differentiation-2; MyD88, myeloid differentiation factor 88; TLR4, toll-like receptor 4; TRIF, Toll/IL-1R domain-containing adaptor-inducing IFN-β; TNF, tumor necrosis factor
Effects of gut dysfunction on the liver
After sepsis along with gut dysfunction, PAMPs and DAMPs from the intestine travel through the portal circulation or biliary tract to the liver [58]. In the hepatic vasculature, effector cells immediately engage circulating pathogens or identify PAMPs, forming a network of immunological sentinels [99,100,101,102,103]. Furthermore, TLRs on macrophages and other cell types in the liver are activated by endogenous components from dying host cells, known as DAMPs [95, 102, 104]. NLRs and the RNA-helicase family also recognize pathogens in the cell cytoplasm [102, 105,106,107]. Gut-derived PAMPs and DAMPs may be a key trigger [108], leading to an inappropriate immune response or overwhelming inflammation, impaired clearance of hepatic pathogenic bacteria, and metabolic disorders [109, 110] (Table 2).
Liver sinusoidal endothelial cells
Because LSECs lack a basal lamina or septum underneath the endothelium, they provide communication areas known as fenestrae between sinusoidal blood and the subendothelial space, facilitating interchange of substrates between the blood and nearby stellate cells and hepatocytes and regulating lipoprotein traffic in the latter [63, 111]. Blood pressure and toxin levels affect the diameter of LSEC fenestrae in mice [112, 113]. Adhesion molecules of the LSEC immunoglobulin superfamily play crucial roles in leukocyte migration to inflammatory sites [114, 115]. Normal LSECs very faintly express vascular cell adhesion molecule-1, but its expression increases markedly under inflammatory stimulation in rats [116].
LSECs have an extremely high endocytotic capacity that is facilitated by SRs and lysosomal activity, which aids internalization and catabolism of several waste substances and small colloidal particles [117,118,119]. For instance, SR-A type 1/1.1 binds to various macromolecules, such as LPS and lipoteichoic acid (LTA), in mice [120, 121]. Seven TLRs are now being studied in LSECs [122]. TLR-9 expressed on murine LSECs recognizes and binds unmethylated CpG motifs that are abundant in bacterial DNA to activate nuclear factor kappa-B (NF-κB) and stimulates production of IL-1β and IL-6 [123]. In addition, LSECs initiate antiviral and proinflammatory responses via TLR3 and adaptive responses via TLR1, TLR6, and TLR8 [124]. Hence, LSECs form an anatomical sieve in the liver, continually monitoring antigens such as PAMPs and DAMPs, with proper tolerance, to maintain hepatic immune homeostasis.
Macrophages
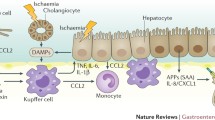
Macrophages exhibit variable phenotypes, including M1-like macrophages that are conventionally triggered by TLR ligands and IFN-γ and M2-like macrophages activated by IL-4/IL-13 in addition to various states in between [125,126,127]. Proinflammatory cytokines are markedly produced by the M1 phenotype, which also generates reactive nitrogen and oxygen intermediates, promotes the Th1 immune response, and plays a significant role in microbicidal and tumoricidal activities [125, 128]. Th2-biased responses are linked to the M2 phenotype, which is typically associated with production of IL-10 and IL-1 receptor antagonists [129, 130]. When macrophages are exposed to bacterial products from the gut in septic mice, they become polarized to the M1 phenotype and participate in the immunoinflammatory response [131]. Sepsis-induced acute liver injury in rats is attenuated by M2-like macrophages, presumably via upregulation of IL-10 expression and suppression of TNF production [132]. Both enhancement of M2-like macrophage polarization and suppression of M1-like macrophage polarization protect the liver from excessive inflammation-induced injury [133, 134] (Fig. 3). Lethal sepsis in mice can be ameliorated by neochromine S5, particularly due to its modulation of M1-like macrophages [135].
When gut-derived PAMPs are exposed to hepatic macrophages, the macrophages are polarized and form large numbers of M1-like macrophages that mainly produce proinflammatory cytokines such as IL-1β, TNF, and IL-6; some M2-like macrophages typically produce IL-10 and play a role in anti-inflammatory reactions. Inflammasomes are activated in hepatic macrophages and in response to pathogen infections and tissue injury. Moreover, neutrophils are attracted to the liver by chemotactic factors, such as CXCL1 and CXCL2 derived from KCs, and released NETs participate in removal of pathogens and toxins. Platelet recruitment is also critical for limiting bacterial infection, and platelets that interact with KCs play a crucial role in fighting against bacterial infection. However, when an inappropriate immune response or overwhelming inflammation occurs with high levels of DAMP formation and proinflammatory cytokine production in the liver, notable hepatocyte injury, macrophage autophagy, and apoptosis occur. Hepatic macrophages are supplemented by KC proliferation and circulating monocyte recruitment and differentiation. CXCL, chemokine (C-X-C motif) ligand; DAMPs, damage-associated molecular patterns; IL, interleukin; KCs, Kupffer cells; NETs, neutrophil extracellular traps; PAMPs, pathogen-associated molecular patterns; TNF, tumor necrosis factor
Moreover, there are some special roles of KCs in defense against pathogens. For one, complement receptor of the immunoglobulin superfamily (CRIg), expressed on subsets of resident macrophages in various tissues and especially on liver KCs, recognizes activated forms of the complement component C3, playing a significant role in removing additional particles and large complexes from the circulation and in effectively clearing opsonized infectious pathogens [136,137,138]. CRIg gene deficiency in mice markedly lowers KC uptake of Staphylococcus aureus and Listeria monocytogenes [136]. CRIg is also involved in direct capture of gram-positive bacteria from the circulation by binding to LTA in mice [139]. Bacteria such as Bacillus cereus and methicillin-resistant Staphylococcus aureus are rapidly captured by KCs in mice and trigger platelets to change their adhesion mode to sustain glycoprotein IIb-mediated adhesion on the KC surface to encapsulate microorganisms, preventing pathogen-induced endothelial permeability and liver damage [140]. However, when addressing macrophage-platelet interactions, it is important to consider immunological repercussions and potential complications such as thrombosis [141, 142]
Neutrophils, NK cells, and natural killer T (NKT) cells
Buildup of activated neutrophils in the liver microcirculation may lead to immune-mediated damage [143]. Neutrophil extracellular traps (NETs) are released by neutrophils during sepsis when they migrate to liver sinusoids [144, 145]. LPS or sepsis triggers intravascular NET development mediated by β2-integrin-dependent platelet–neutrophil interactions inside sinusoids in mice [146]. Furthermore, the neutrophil–endothelium interaction and NETs induce microthrombosis and vascular leakage in a rat model of sepsis [147].
NK cells are much more abundant in the liver than in the circulation; NKT cells with several distinct subsets contribute to antibacterial defense and are influenced by the intestinal microbiota. Both NK and NKT cells contribute to the pathophysiology of liver damage [148, 149]. For example, after injection of poly I:C and D-galactosamine in a murine fulminant hepatitis model, NK cells interact with KCs via NK Group 2 member D/ligand recognition, causing severe liver injury [150]. Moreover, when ischemia or toxin-induced injury occurs in the liver, the activated NKT cells predominantly secrete IFN-γ, leading to accumulation of neutrophils and macrophages and the promotion of liver damage in mice [151]. Another study revealed that activation of NKT can kill hepatocytes directly via Fas/FasL pathways in a murine model [152].
Therapy
Epithelial barrier-targeting therapy
Due to the role of claudin-2 in gated paracellular channel formation and TJ channel modulation, it may be an ideal therapeutic target for regulating the epithelial barrier [153]. In fact, regulation of TJ channel gating kinetics and protein intermolecular interactions may have therapeutic value in inflammation-associated barrier failure, such as occludin S408 dephosphorylation. However, more studies are needed to identify pharmacological means of modulating gating activity for therapeutic purposes. Moreover, microRNA-155 alleviates inflammation and intestinal barrier dysfunction in septic mice, with a decrease in TNF-α and IL-6 levels via inactivation of NF-κB signaling [154].
Targeting the gut microbiome
Probiotics are living nonpathogenic microorganisms that help preserve the intestinal barrier, inhibit pathogen spread, minimize bacterial displacement, and prevent infection [155]. Nevertheless, genomic analysis in an epidemiological investigation detected six independent incidences of probiotic transfer from the capsule to the blood in ICU patients, resulting in bacteremia [156].
Prebiotics are indigestible dietary components, most of which comprise indigestible oligosaccharides that may specifically encourage the development and metabolism of beneficial gut microbiota, improving the balance of the intestinal flora and benefiting human health [157]. Cellulose supplementation has been associated with partly decreased systemic inflammation in mouse sepsis models, suggesting a survival benefit conferred by microbes [158].
Fecal microbial transplantation (FMT) can save mice from lethal sepsis caused by pathogens isolated from a septic patient, which is associated with spread of butyrate-producing Bacteroidetes, improvement in pathogen clearance, and restoration of host immunity via interferon regulatory factor 3 [159]. FMT may be an option for treating sepsis; however, donor screening is necessary to prevent spread of bacteria that may cause unfavorable infection. Moreover, it is important to consider the advantages and hazards of FMT in diverse patient groups.
An entirely different strategy is the use of absorbent materials to prevent enterogenic toxins and bacterial products from entering the blood circulation and the liver. Indeed, cation-exchange resin targeting hyperkalemia and hyperphosphatemia has shown efficacy [160]. Nonabsorbable nanopore carbon reduced portal vein pressure and liver biochemical markers in rats that underwent bile duct ligation, resulting in decreased endotoxin-induced KC stimulation [161, 162]. Therefore, by targeting the gut–liver axis, adsorbent materials is a possible treatment strategy for sepsis.
High-density lipoprotein (HDL) as a potential therapy
One study revealed that HDL is able to neutralize LPS and accelerate LPS clearance via SR-BI-mediated LPS uptake in mice [163]. Numerous apolipoproteins (Apo) on HDL particles play crucial roles in clearing endotoxins to prevent infection.
For instance, the inflammatory response to LPS is inhibited when LPS binds to Apo AI or Apo E [164,165,166], but Apo AII and Apo CI bind to LPS, enhancing inflammation [167, 168]. In a study of 63 severe septic patients, HDL levels < 20 mg/dL and Apo AI < 100 mg/dL on day 1 were associated with an increase in overall and sepsis-attributable 30-day mortality rates, prolonged intensive care unit stay and hospital-acquired infection [169].
Moreover, reconstituted HDL infusion reduces endotoxin-induced histological tissue injury in the lung, liver, and intestines of rats [170]. In addition, 111-indium bacterial labeling in mice highlights the possibility of potential hepatic bacterial clearance promoted by HDL uptake [171]. Thus, HDL may be an important target for future sepsis prevention and therapy.
Conclusions
During sepsis, gradual damage to gut barrier components due to inflammation causes increased intestinal permeability and intestinal dysbiosis, including pathogenic microbial overgrowth and translocation of abundant PAMPs and DAMPs to the liver via the portal circulation or biliary tract. Because of its physical proximity to the gut, the liver, a first-line immune organ acting as a gatekeeper between the gut and systemic circulation, can be rapidly shifted from immune hyporeactivity to produce a potent inflammatory response and effective adaptive immunity. However, an inappropriate immune response or overwhelming inflammation can be triggered by intestinal hyperpermeability and gut-derived PAMPs and DAMPs after sepsis, resulting in impaired hepatic clearance of pathogenic bacteria and metabolic disorder and contributing to MODS. Therefore, a better understanding of the gut–liver interaction in sepsis may help prevent and limit sepsis-induced liver damage and improve the prognosis of patients with sepsis.
Availability of data and materials
Not applicable.
Abbreviations
- AMPs:
-
Antimicrobial peptides
- AOAH:
-
Acylhydrolase
- Apo:
-
Apolipoprotein
- BPI:
-
Bactericidal/permeability-increasing protein
- CRIg:
-
Complement receptor of the immunoglobulin superfamily
- DAMPs:
-
Damage-associated molecular patterns
- FMT:
-
Fecal microbial transplantation
- HDL:
-
High-density lipoprotein
- IAPs:
-
Intestinal alkaline phosphatase
- IECs:
-
Intestinal epithelial cells
- IFN:
-
Interferon
- IL:
-
Interleukin
- KCs:
-
Kupffer cells
- LBP:
-
LPS-binding protein
- LPS:
-
Lipopolysaccharide
- LSECs:
-
Liver sinusoidal endothelial cells
- LTA:
-
Lipoteichoic acid
- MARCO:
-
Macrophage receptor with collagen structure
- MODS:
-
Multiple organ dysfunction syndrome
- MUCs:
-
Mucins
- MyD88:
-
Myeloid differentiation factor 88
- NETs:
-
Neutrophil extracellular traps
- NF-κB:
-
Nuclear factor kappa-B
- NK:
-
Natural killer
- NKT:
-
Natural killer T
- PAMPs:
-
Pathogen-associated molecular patterns
- Th1:
-
T helper 1
- TJs:
-
Tight junctions
- TLR:
-
Toll-like receptor
- TNF:
-
Tumor necrosis factor
References
Singer M, Deutschman CS, Martin GS, Poll T. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10. https://doi.org/10.1001/jama.2016.0287.
Cecconi M, Evans L, Levy M, Rhodes A. Sepsis and septic shock. Lancet. 2018;392:75–87. https://doi.org/10.1016/S0140-6736(18)30696-2.
Fujishima S. Organ dysfunction as a new standard for defining sepsis. Inflamm Regen. 2016;36:24. https://doi.org/10.1186/s41232-016-0029-y.
Gilbert JA, Quinn RA, Debelius J, Xu ZZ, Morton J, Garg N, et al. Microbiome-wide association studies link dynamic microbial consortia to disease. Nature. 2016;535:94–103. https://doi.org/10.1038/nature18850.
Arthur JC, Perez-Chanona E, Mühlbauer M, Tomkovich S, Uronis JM, Fan T, et al. Intestinal inflammation targets cancer-inducing activity of the microbiota. Science. 2012;338:120–3. https://doi.org/10.1126/science.1224820.
Quinn RA, Phelan VV, Whiteson KL, Garg N, Bailey BA, Lim YW, et al. Microbial, host and xenobiotic diversity in the cystic fibrosis sputum metabolome. ISME J. 2016;10:1483–98. https://doi.org/10.1038/ismej.2015.207.
Jia W, Xie G, Jia W. Bile acid–microbiota crosstalk in gastrointestinal inflammation and carcinogenesis. Nat Rev Gastroenterol Hepatol. 2018;15:111–28. https://doi.org/10.1038/nrgastro.2017.119.
Beyaert R, Libert C. How good roommates can protect against microbial sepsis. Cell Host Microbe. 2018;23:283–5. https://doi.org/10.1016/j.chom.2018.02.007.
Schnabl B, Brenner DA. Interactions between the intestinal microbiome and liver diseases. Gastroenterology. 2014;146:1513–24. https://doi.org/10.1053/j.gastro.2014.01.020.
Nesseler N, Launey Y, Aninat C, Morel F, Mallédant Y, Seguin P. Clinical review: the liver in sepsis. Crit Care. 2012;16:235. https://doi.org/10.1186/cc11381.
Kurashima Y, Kiyono H. Mucosal ecological network of epithelium and immune cells for gut homeostasis and tissue healing. Annu Rev Immunol. 2017;35:119–47. https://doi.org/10.1146/annurev-immunol-051116-052424.
Odenwald MA, Turner JR. Intestinal permeability defects: is it time to treat? Clin Gastroenterol Hepatol. 2013;11:1075–83. https://doi.org/10.1016/j.cgh.2013.07.001.
Turner JR. Intestinal mucosal barrier function in health and disease. Nat Rev Immunol. 2009;9:799–809. https://doi.org/10.1038/nri2653.
Farquhar MG, Palade GE. Junctional complexes in various epithelia. J Cell Biol. 1963;17:375–412. https://doi.org/10.1083/jcb.17.2.375.
Bischoff SC, Barbara G, Buurman W, Ockhuizen T, Schulzke JD, Serino M, et al. Intestinal permeability—a new target for disease prevention and therapy. BMC Gastroenterol. 2014;14:189. https://doi.org/10.1186/s12876-014-0189-7.
Suzuki T. Regulation of the intestinal barrier by nutrients: the role of tight junctions. Anim Sci J. 2020;91: e13357. https://doi.org/10.1111/asj.13357.
Johansson MEV, Ambort D, Pelaseyed T, Schütte A, Gustafsson JK, Ermund A, et al. Composition and functional role of the mucus layers in the intestine. Cell Mol Life Sci. 2011;68:3635–41. https://doi.org/10.1007/s00018-011-0822-3.
Cornick S, Tawiah A, Chadee K. Roles and regulation of the mucus barrier in the gut. Tissue Barriers. 2015;3: e982426. https://doi.org/10.4161/21688370.2014.982426.
Schroeder BO. Fight them or feed them: how the intestinal mucus layer manages the gut microbiota. Gastroenterol Rep (Oxf). 2019;7:3–12. https://doi.org/10.1093/gastro/goy052.
Sicard J, Le Bihan G, Vogeleer P, Jacques M, Harel J. Interactions of intestinal bacteria with components of the intestinal mucus. Front Cell Infect Microbiol. 2017;7:387. https://doi.org/10.3389/fcimb.2017.00387.
Faderl M, Noti M, Corazza N, Mueller C. Keeping bugs in check: the mucus layer as a critical component in maintaining intestinal homeostasis. IUBMB Life. 2015;67:275–85. https://doi.org/10.1002/iub.1374.
Kumar M, Leon Coria A, Cornick S, Petri B, Mayengbam S, Jijon HB, et al. Increased intestinal permeability exacerbates sepsis through reduced hepatic SCD-1 activity and dysregulated iron recycling. Nat Commun. 2020;11:483. https://doi.org/10.1038/s41467-019-14182-2.
Mukherjee S, Hooper LV. Antimicrobial defense of the intestine. Immunity. 2015;42:28–39. https://doi.org/10.1016/j.immuni.2014.12.028.
Beumer C, Wulferink M, Raaben W, Fiechter D, Brands R, Seinen W. Calf intestinal alkaline phosphatase, a novel therapeutic drug for lipopolysaccharide (LPS)-mediated diseases, attenuates LPS toxicity in mice and piglets. J Pharmacol Exp Ther. 2003;307:737–44. https://doi.org/10.1124/jpet.103.056606.
Akiba Y, Mizumori M, Guth PH, Engel E, Kaunitz JD. Duodenal brush border intestinal alkaline phosphatase activity affects bicarbonate secretion in rats. Am J Physiol Gastrointest Liver Physiol. 2007;293:G1223–33. https://doi.org/10.1152/ajpgi.00313.2007.
Malo MS, Moaven O, Muhammad N, Biswas B, Alam SN, Economopoulos KP, et al. Intestinal alkaline phosphatase promotes gut bacterial growth by reducing the concentration of luminal nucleotide triphosphates. Am J Physiol Gastrointest Liver Physiol. 2014;306:G826–38. https://doi.org/10.1152/ajpgi.00357.2013.
Goldberg RF, Austen WJ, Zhang X, Munene G, Mostafa G, Biswas S, et al. Intestinal alkaline phosphatase is a gut mucosal defense factor maintained by enteral nutrition. Proc Natl Acad Sci USA. 2008;105:3551–6. https://doi.org/10.1073/pnas.0712140105.
Lallès J. Intestinal alkaline phosphatase: novel functions and protective effects. Nutr Rev. 2014;72:82–94. https://doi.org/10.1111/nure.12082.
Singh SB, Carroll-Portillo A, Coffman C, Ritz NL, Lin HC. Intestinal alkaline phosphatase exerts anti-inflammatory effects against lipopolysaccharide by inducing autophagy. Sci Rep. 2020;10:3107. https://doi.org/10.1038/s41598-020-59474-6.
Doe WF. The intestinal immune system. Gut. 1989;30:1679–85. https://doi.org/10.1136/gut.30.12.1679.
Neutra MR, Mantis NJ, Kraehenbuhl JP. Collaboration of epithelial cells with organized mucosal lymphoid tissues. Nat Immunol. 2001;2:1004–9. https://doi.org/10.1038/ni1101-1004.
Spahn TW. Modulating the intestinal immune system: the role of lymphotoxin and GALT organs. Gut. 2004;53:456–65. https://doi.org/10.1136/gut.2003.023671.
Viola MF, Boeckxstaens G. Niche-specific functional heterogeneity of intestinal resident macrophages. Gut. 2021;70:1383–95. https://doi.org/10.1136/gutjnl-2020-323121.
Mowat AM, Agace WW. Regional specialization within the intestinal immune system. Nat Rev Immunol. 2014;14:667–85. https://doi.org/10.1038/nri3738.
McDonald BD, Jabri B, Bendelac A. Diverse developmental pathways of intestinal intraepithelial lymphocytes. Nat Rev Immunol. 2018;18:514–25. https://doi.org/10.1038/s41577-018-0013-7.
Rescigno M, Urbano M, Valzasina B, Francolini M, Rotta G, Bonasio R, et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001;2:361–7. https://doi.org/10.1038/86373.
Chen VL, Kasper DL. Interactions between the intestinal microbiota and innate lymphoid cells. Gut Microbes. 2014;5:129–40. https://doi.org/10.4161/gmic.27289.
Thaiss CA, Zmora N, Levy M, Elinav E. The microbiome and innate immunity. Nature. 2016;535:65–74. https://doi.org/10.1038/nature18847.
Inamine T, Schnabl B. Immunoglobulin A and liver diseases. J Gastroenterol. 2018;53:691–700. https://doi.org/10.1007/s00535-017-1400-8.
Peterson LW, Artis D. Intestinal epithelial cells: regulators of barrier function and immune homeostasis. Nat Rev Immunol. 2014;14:141–53. https://doi.org/10.1038/nri3608.
Okumura R, Takeda K. Roles of intestinal epithelial cells in the maintenance of gut homeostasis. Exp Mol Med. 2017;49: e338. https://doi.org/10.1038/emm.2017.20.
Kamada N, Seo S, Chen GY, Núñez G. Role of the gut microbiota in immunity and inflammatory disease. Nat Rev Immunol. 2013;13:321–35. https://doi.org/10.1038/nri3430.
McKenney ES, Kendall MM. Microbiota and pathogen “pas de deux”: setting up and breaking down barriers to intestinal infection. Pathog Dis. 2016;74:ftw051. https://doi.org/10.1093/femspd/ftw051.
Tap J, Mondot S, Levenez F, Pelletier E, Caron C, Furet J, et al. Towards the human intestinal microbiota phylogenetic core. Environ Microbiol. 2009;11:2574–84. https://doi.org/10.1111/j.1462-2920.2009.01982.x.
Shin R, Suzuki M, Morishita Y. Influence of intestinal anaerobes and organic acids on the growth of enterohaemorrhagic Escherichia coli O157:H7. J Med Microbiol. 2002;51:201–6. https://doi.org/10.1099/0022-1317-51-3-201.
Cotter PD, Hill C, Ross RP. Bacteriocins: developing innate immunity for food. Nat Rev Microbiol. 2005;3:777–88. https://doi.org/10.1038/nrmicro1273.
Drissi F, Buffet S, Raoult D, Merhej V. Common occurrence of antibacterial agents in human intestinal microbiota. Front Microbiol. 2015;6:441. https://doi.org/10.3389/fmicb.2015.00441.
Bockler R, Meyer H, Schlag P. An experimental study on bacterial colonization, nitrite and nitrosamine production in the operated stomach. J Cancer Res Clin Oncol. 1983;105:62–6. https://doi.org/10.1007/BF00391833.
Chung CS, Chang PF, Liao CH, Lee TH, Chen Y, Lee YC, et al. Differences of microbiota in small bowel and faeces between irritable bowel syndrome patients and healthy subjects. Scand J Gastroenterol. 2016;51:410–9. https://doi.org/10.3109/00365521.2015.1116107.
Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci USA. 2007;104:13780–5. https://doi.org/10.1073/pnas.0706625104.
Kamada N, Chen GY, Inohara N, Núñez G. Control of pathogens and pathobionts by the gut microbiota. Nat Immunol. 2013;14:685–90. https://doi.org/10.1038/ni.2608.
Adak A, Khan MR. An insight into gut microbiota and its functionalities. Cell Mol Life Sci. 2019;76:473–93. https://doi.org/10.1007/s00018-018-2943-4.
Litvak Y, Mon KKZ, Nguyen H, Chanthavixay G, Liou M, Velazquez EM, et al. Commensal enterobacteriaceae protect against salmonella colonization through oxygen competition. Cell Host Microbe. 2019;25:128–39. https://doi.org/10.1016/j.chom.2018.12.003.
Feng Y, Wang Y, Wang P, Huang Y, Wang F. Short-chain fatty acids manifest stimulative and protective effects on intestinal barrier function through the inhibition of NLRP3 inflammasome and autophagy. Cell Physiol Biochem. 2018;49:190–205. https://doi.org/10.1159/000492853.
Tripathi A, Debelius J, Brenner DA, Karin M, Loomba R, Schnabl B, et al. The gut–liver axis and the intersection with the microbiome. Nat Rev Gastroenterol Hepatol. 2018;15:397–411. https://doi.org/10.1038/s41575-018-0011-z.
Bismuth H. Revisiting liver anatomy and terminology of hepatectomies. Ann Surg. 2013;257:383–6. https://doi.org/10.1097/SLA.0b013e31827f171f.
Adams DH, Eksteen B, Curbishley SM. Immunology of the gut and liver: a love/hate relationship. Gut. 2008;57:838–48. https://doi.org/10.1136/gut.2007.122168.
Albillos A, de Gottardi A, Rescigno M. The gut–liver axis in liver disease: pathophysiological basis for therapy. J Hepatol. 2020;72:558–77. https://doi.org/10.1016/j.jhep.2019.10.003.
Rehermann VRAB. The liver as an immunological organ. Hepatology. 2006;43:S54-62. https://doi.org/10.1002/hep.21060.
Fonseca RC, Bassi GS, Brito CC, Rosa LB, David BA, Araújo AM, et al. Vagus nerve regulates the phagocytic and secretory activity of resident macrophages in the liver. Brain Behav Immun. 2019;81:444–54. https://doi.org/10.1016/j.bbi.2019.06.041.
Pavlov VA, Tracey KJ. Neural regulation of immunity: molecular mechanisms and clinical translation. Nat Neurosci. 2017;20:156–66. https://doi.org/10.1038/nn.4477.
de Jonge WJ, van der Zanden EP, The FO, Bijlsma MF, van Westerloo DJ, Bennink RJ, et al. Stimulation of the vagus nerve attenuates macrophage activation by activating the Jak2-STAT3 signaling pathway. Nat Immunol. 2005;6:844–51. https://doi.org/10.1038/ni1229.
Shetty S, Lalor PF, Adams DH. Liver sinusoidal endothelial cells—gatekeepers of hepatic immunity. Nat Rev Gastroenterol Hepatol. 2018;15:555–67. https://doi.org/10.1038/s41575-018-0020-y.
Perdiguero EG, Klapproth K, Schulz C, Busch K, Azzoni E, Crozet L, et al. Tissue-resident macrophages originate from yolk sac-derived erythro-myeloid progenitors. Exp Hematol. 2015;43:S64. https://doi.org/10.1038/nature13989.
Beattie L, Sawtell A, Mann J, Frame TCM, Teal B, de Labastida RF, et al. Liver macrophage function is guided by micro-environment rather than origin. J Hepatol. 2016;65:758–68. https://doi.org/10.1016/j.jhep.2016.05.037.
MacParland SA, Liu JC, Ma X, Innes BT, Bartczak AM, Gage BK, et al. Single cell RNA sequencing of human liver reveals distinct intrahepatic macrophage populations. Nat Commun. 2018;9:4321–83. https://doi.org/10.1038/s41467-018-06318-7.
Zhao J, Zhang S, Liu Y, He X, Qu M, Xu G, et al. Single-cell RNA sequencing reveals the heterogeneity of liver-resident immune cells in human. Cell Discov. 2020;6:22. https://doi.org/10.1038/s41421-020-0157-z.
Habes QLM, Ede LV, Gerretsen J, Kox M, Pickkers P. Norepinephrine contributes to enterocyte damage in septic shock patients: a prospective cohort study. Shock. 2018;49:137–43. https://doi.org/10.1097/SHK.0000000000000955.
Yoseph BP, Klingensmith NJ, Liang Z, Breed ER, Burd EM, Mittal R, et al. Mechanisms of intestinal barrier dysfunction in sepsis. Shock. 2016;46:52–9. https://doi.org/10.1097/SHK.0000000000000565.
Zahs A, Bird MD, Ramirez L, Turner JR, Choudhry MA, Kovacs EJ. Inhibition of long myosin light-chain kinase activation alleviates intestinal damage after binge ethanol exposure and burn injury. Am J Physiol Gastrointest Liver Physiol. 2012;303:G705–12. https://doi.org/10.1152/ajpgi.00157.2012.
Cunningham KE, Turner JR. Myosin light chain kinase: pulling the strings of epithelial tight junction function. Ann N Y Acad Sci. 2012;1258:34–42. https://doi.org/10.1111/j.1749-6632.2012.06526.x.
Neal MD, Sodhi CP, Jia H, Dyer M, Egan CE, Yazji I, et al. Toll-like receptor 4 Is expressed on intestinal stem cells and regulates their proliferation and apoptosis via the p53 up-regulated modulator of apoptosis. J Biol Chem. 2012;287:37296–308. https://doi.org/10.1074/jbc.M112.375881.
Neal MD, Sodhi CP, Dyer M, Craig BT, Good M, Jia H, et al. A critical role for toll-like receptor-4 induction of autophagy in the regulation of enterocyte migration and the pathogenesis of necrotizing enterocolitis. J Immunol. 2013;190:3541–51. https://doi.org/10.4049/jimmunol.1202264.
Armacki M, Trugenberger AK, Ellwanger AK, Eiseler T, Schwerdt C, Bettac L, et al. Thirty-eight-negative kinase 1 mediates trauma-induced intestinal injury and multi-organ failure. J Clin Invest. 2018;128:5056–72. https://doi.org/10.1172/JCI97912.
Chang M, Alsaigh T, Kistler EB, Schmid-Schönbein GW, Heimesaat MM. Breakdown of mucin as barrier to digestive enzymes in the ischemic rat small intestine. PLoS ONE. 2012;7: e40087. https://doi.org/10.1371/journal.pone.0040087.
Yang JM, Radulescu AMP, Chen CP, Zhang HM, James IOM, Besner GEM. Heparin-binding epidermal growth factor-like growth factor improves intestinal barrier function and reduces mortality in a murine model of peritonitis. Surgery. 2013;153:52–62. https://doi.org/10.1016/j.surg.2012.04.002.
Otani S, Oami T, Yoseph BP, Klingensmith NJ, Chen C, Liang Z, et al. Overexpression of BCL-2 in the intestinal epithelium prevents sepsis-induced gut barrier dysfunction via altering tight junction protein expression. Shock. 2020;54:330–6. https://doi.org/10.1097/SHK.0000000000001463.
Defazio J, Fleming ID, Shakhsheer B, Zaborina O, Alverdy JC. The opposing forces of the intestinal microbiome and the emerging pathobiome. Surg Clin North Am. 2014;94:1151–61. https://doi.org/10.1016/j.suc.2014.08.002.
Krezalek MA, DeFazio J, Zaborina O, Zaborin A, Alverdy JC. The shift of an intestinal “microbiome” to a “pathobiome” governs the course and outcome of sepsis following surgical injury. Shock. 2016;45:475–82. https://doi.org/10.1097/SHK.0000000000000534.
Lankelma JM, van Vught LA, Belzer C, Schultz MJ, van der Poll T, de Vos WM, et al. Critically ill patients demonstrate large interpersonal variation in intestinal microbiota dysregulation: a pilot study. Intensive Care Med. 2017;43:59–68. https://doi.org/10.1007/s00134-016-4613-z.
McDonald D, Ackermann G, Khailova L, Baird C, Heyland D, Kozar R, et al. Extreme dysbiosis of the microbiome in critical illness. mSphere. 2016;1:e00199-e216. https://doi.org/10.1128/mSphere.00199-16.
Haak BW, Argelaguet R, Kinsella CM, Kullberg R, Lankelma JM, Deijs M, et al. Integrative transkingdom analysis of the gut microbiome in antibiotic perturbation and critical illness. mSystems. 2021;6:e01148-e1220. https://doi.org/10.1128/mSystems.01148-20.
Erridge CATSC. A high-fat meal induces low-grade endotoxemia: evidence of a novel mechanism of postprandial inflammation. Am J Clin Nutr. 2007;5:1286–92. https://doi.org/10.1093/ajcn/86.5.1286.
Racine R, Mark E. Hyaluronan endocytosis: mechanisms of uptake and biological functions. In: Ceresa B, editor. Molecular regulation of endocytosis. London: BoD–Books on Demand; 2012. p. 377–90.
Fackler SRAO. Viruses, lipid rafts and signal transduction. Signal Transduct. 2006;7:53–63. https://doi.org/10.1002/sita.200600113.
Knoop KA, McDonald KG, McCrate S, McDole JR, Newberry RD. Microbial sensing by goblet cells controls immune surveillance of luminal antigens in the colon. Mucosal Immunol. 2015;8:198–210. https://doi.org/10.1038/mi.2014.58.
Laugerette F, Vors C, Géloën A, Chauvin M, Soulage C, Lambert-Porcheron S, et al. Emulsified lipids increase endotoxemia: possible role in early postprandial low-grade inflammation. J Nutr Biochem. 2011;22:53–9. https://doi.org/10.1016/j.jnutbio.2009.11.011.
Howe SE, Lickteig DJ, Plunkett KN, Ryerse JS, Konjufca V, Bereswill S. The uptake of soluble and particulate antigens by epithelial cells in the mouse small intestine. PLoS ONE. 2014;9: e86656. https://doi.org/10.1371/journal.pone.0086656.
Osamu Takeuchi SA. Pattern recognition receptors and inflammation. Cell. 2010;140:805–20. https://doi.org/10.1016/j.cell.2010.01.022.
Shao B, Lu M, Katz SC, Varley AW, Hardwick J, Rogers TE, et al. A host lipase detoxifies bacterial lipopolysaccharides in the liver and spleen. J Biol Chem. 2007;282:13726–35. https://doi.org/10.1074/jbc.M609462200.
Tuin A, Huizinga-Van DVA, van Loenen-Weemaes AM, Meijer DK, Poelstra K. On the role and fate of LPS-dephosphorylating activity in the rat liver. Am J Physiol Gastrointest Liver Physiol. 2006;290:G377–85. https://doi.org/10.1152/ajpgi.00147.2005.
Lu M, Zhang M, Takashima A, Weiss J, Apicella MA, Li XH, et al. Lipopolysaccharide deacylation by an endogenous lipase controls innate antibody responses to gram-negative bacteria. Nat Immunol. 2005;6:989–94. https://doi.org/10.1038/ni1246.
Vreugdenhil AC, Snoek AM, Greve JW, Buurman WA. Lipopolysaccharide-binding protein is vectorially secreted and transported by cultured intestinal epithelial cells and is present in the intestinal mucus of mice. J Immunol. 2000;165:4561–6. https://doi.org/10.4049/jimmunol.165.8.4561.
Finlay BB, Hancock REW. Can innate immunity be enhanced to treat microbial infections? Nat Rev Microbiol. 2004;2:497–504. https://doi.org/10.1038/nrmicro908.
Guo J, Friedman SL. Toll-like receptor 4 signaling in liver injury and hepatic fibrogenesis. Fibrogenesis Tissue Repair. 2010;3:21. https://doi.org/10.1186/1755-1536-3-21.
Leventhal JS, Schröppel B. Toll-like receptors in transplantation: sensing and reacting to injury. Kidney Int. 2012;81:826–32. https://doi.org/10.1038/ki.2011.498.
Kitchens RL, Thompson PA. Modulatory effects of sCD14 and LBP on LPS-host cell interactions. J Endotoxin Res. 2005;11:225–9. https://doi.org/10.1179/096805105X46565.
Balakrishnan A, Chakravortty D. Epithelial cell damage activates bactericidal/permeability increasing-protein (BPI) expression in intestinal epithelium. Front Microbiol. 2017;8:1567. https://doi.org/10.3389/fmicb.2017.01567.
Schnabl B. Interactions between the intestinal microbiome and liver diseases. Gastroenterology. 2014;146:1513–24. https://doi.org/10.1053/j.gastro.2014.01.020.
Lalazar G, Ilyas G, Malik SA, Liu K, Zhao E, Amir M, et al. Autophagy confers resistance to lipopolysaccharide-induced mouse hepatocyte injury. Am J Physiol Gastrointest Liver Physiol. 2016;311:G377–86. https://doi.org/10.1152/ajpgi.00124.2016.
Ogura Y, Sutterwala FS, Flavell RA. The inflammasome: first line of the immune response to cell stress. Cell. 2006;126:659–62. https://doi.org/10.1016/j.cell.2006.08.002.
Kim HY, Kim SJ, Lee SM. Activation of NLRP3 and AIM2 inflammasomes in Kupffer cells in hepatic ischemia/reperfusion. FEBS J. 2015;282:259–70. https://doi.org/10.1111/febs.13123.
Oami T, Watanabe E, Hatano M, Teratake Y, Fujimura L, Sakamoto A, et al. Blocking liver autophagy accelerates apoptosis and mitochondrial injury in hepatocytes and reduces time to mortality in a murine sepsis model. Shock. 2018;50:427–34. https://doi.org/10.1097/SHK.0000000000001040.
Sutterwala FS, Ogura Y, Flavell RA. The inflammasome in pathogen recognition and inflammation. J Leukoc Biol. 2007;82:259–64. https://doi.org/10.1189/jlb.1206755.
Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464:1357–61. https://doi.org/10.1038/nature08938.
Szabo G, Dolganiuc A, Mandrekar P. Pattern recognition receptors: a contemporary view on liver diseases. Hepatology. 2006;44:287–98. https://doi.org/10.1002/hep.21308.
Yang J, Zhao Y, Shao F. Non-canonical activation of inflammatory caspases by cytosolic LPS in innate immunity. Curr Opin Immunol. 2015;32:78–83. https://doi.org/10.1016/j.coi.2015.01.007.
Alaish SM, Smith AD, Timmons J, Greenspon J, Eyvazzadeh D, Murphy E, et al. Gut microbiota, tight junction protein expression, intestinal resistance, bacterial translocation and mortality following cholestasis depend on the genetic background of the host. Gut Microbes. 2013;4:292–305. https://doi.org/10.4161/gmic.24706.
Bhogal HK, Sanyal AJ. The molecular pathogenesis of cholestasis in sepsis. Front Biosci (Elite Ed). 2013;5:87–96. https://doi.org/10.2741/e598.
Kalhan SC, Guo L, Edmison J, Dasarathy S, McCullough AJ, Hanson RW, et al. Plasma metabolomic profile in nonalcoholic fatty liver disease. Metabolism. 2011;60:404–13. https://doi.org/10.1016/j.metabol.2010.03.006.
Braet F, Wisse E. Structural and functional aspects of liver sinusoidal endothelial cell fenestrae: a review. Comp Hepatol. 2002;1:1. https://doi.org/10.1186/1476-5926-1-1.
Zapotoczny B, Szafranska K, Kus E, Braet F, Wisse E, Chlopicki S, et al. Tracking fenestrae dynamics in live murine liver sinusoidal endothelial cells. Hepatology. 2019;69:876–88. https://doi.org/10.1002/hep.30232.
Monkemoller V, Oie C, Hubner W, Huser T, McCourt P. Multimodal super-resolution optical microscopy visualizes the close connection between membrane and the cytoskeleton in liver sinusoidal endothelial cell fenestrations. Sci Rep. 2015;5:16279. https://doi.org/10.1038/srep16279.
Gulubova MV. Expression of cell adhesion molecules and their β1 and β2 integrin ligands in human liver peliosis. Pathol Res Pract. 2005;201:503–11. https://doi.org/10.1016/j.prp.2005.05.006.
Steinhoff G. Expression patterns of leukocyte adhesion ligand molecules on human liver endothelia. Lack of ELAM-1 and CD62 inducibility on sinusoidal endothelia and distinct distribution of VCAM-1, ICAM-1, ICAM-2, and LFA-3. Am J Pathol. 1993;142:481–8.
Oudar O, Moreau A, Feldmann G, Scoazec J. Expression and regulation of intercellular adhesion molecule-1 (ICAM-1) in organotypic cultures of rat liver tissue. J Hepatol. 1998;29:901–9. https://doi.org/10.1016/s0168-8278(98)80117-7.
Kzhyshkowska J, Gratchev A, Goerdt S. Stabilin-1, a homeostatic scavenger receptor with multiple functions. J Cell Mol Med. 2006;10:635–49. https://doi.org/10.1111/j.1582-4934.2006.tb00425.x.
Ganesan LP, Mates JM, Cheplowitz AM, Avila CL, Zimmerer JM, Yao Z, et al. Scavenger receptor B1, the HDL receptor, is expressed abundantly in liver sinusoidal endothelial cells. Sci Rep. 2016;6:20646. https://doi.org/10.1038/srep20646.
Godoy B, Murgas P, Tichauer J, Von Bernhardi R. Scavenger receptor class A ligands induce secretion of IL1β and exert a modulatory effect on the inflammatory activation of astrocytes in culture. J Neuroimmunol. 2012;251:6–13. https://doi.org/10.1016/j.jneuroim.2012.06.004.
Hampton RY, Golenbock DT, Penman M, Krieger M, Raetz CRH. Recognition and plasma clearance of endotoxin by scavenger receptors. Nature. 1991;352:342–4. https://doi.org/10.1038/352342a0.
Dunne DW, Resnick D, Greenberg J, Krieger M, Joiner KA. The type I macrophage scavenger receptor binds to gram-positive bacteria and recognizes lipoteichoic acid. Proc Natl Acad Sci USA. 1994;91:1863–7. https://doi.org/10.1073/pnas.91.5.1863.
Kawai TKA. Toll-like receptor signaling pathways. Front Immunol. 2014;5:461.
Dalpke A, Frank J, Peter M, Heeg K. Activation of toll-like receptor 9 by DNA from different bacterial species. Infect Immun. 2006;74:940–6. https://doi.org/10.3389/fimmu.2014.00461.
Wu J, Meng Z, Jiang M, Zhang E, Trippler M, Broering R, et al. Toll-like receptor-induced innate immune responses in non-parenchymal liver cells are cell type-specific. Immunology. 2010;129:363–74. https://doi.org/10.1111/j.1365-2567.2009.03179.x.
Mantovani A, Biswas SK, Galdiero MR, Sica A, Locati M. Macrophage plasticity and polarization in tissue repair and remodelling. J Pathol. 2013;229:176–85. https://doi.org/10.1002/path.4133.
Pu-Ste Liu HWXL, Wan-Chen Cheng CCMV, Massimiliano Mazzone HHSF. a-ketoglutarate orchestrates macrophage activation through metabolic and epigenetic reprogramming. Nat Immunol. 2017;18:985–94. https://doi.org/10.1038/ni.3796.
Lawrence T, Natoli G. Transcriptional regulation of macrophage polarization: enabling diversity with identity. Nat Rev Immunol. 2011;11:750–61. https://doi.org/10.1038/nri3088.
Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. J Clin Invest. 2012;122:787–95. https://doi.org/10.1172/JCI59643.
Satoh T, Kidoya H, Naito H, Yamamoto M, Takemura N, Nakagawa K, et al. Critical role of Trib1 in differentiation of tissue-resident M2-like macrophages. Nature. 2013;495:524–8. https://doi.org/10.1038/nature11930.
Mantovani A, Sozzani S, Locati M, Allavena P, Sica A. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol. 2002;23:549–55. https://doi.org/10.1016/s1471-4906(02)02302-5.
Qin H, Holdbrooks AT, Liu Y, Yanagisawa LL. SOCS3 Deficiency promotes M1 macrophage polarization and inflammation. J Immunol. 2012;189:3439–48. https://doi.org/10.4049/jimmunol.1201168.
Zhang Y, Cheng J, Su Y, Li M, Wen J, Li S. Cordycepin induces M1/M2 macrophage polarization to attenuate the liver and lung damage and immunodeficiency in immature mice with sepsis via NF-κB/p65 inhibition. J Pharm Pharmacol. 2022;74:227–35. https://doi.org/10.1093/jpp/rgab162.
Xie J, Wu X, Zhou Q, Yang Y, Tian Y, Huang C, et al. PICK1 confers anti-inflammatory effects in acute liver injury via suppressing M1 macrophage polarization. Biochimie. 2016;127:121–32. https://doi.org/10.1016/j.biochi.2016.05.002.
Kang JW, Lee SM. Resolvin D1 protects the liver from ischemia/reperfusion injury by enhancing M2 macrophage polarization and efferocytosis. Biochim Biophys Acta. 2016;1861:1025–35. https://doi.org/10.1016/j.bbalip.2016.06.002.
Xu F, Ma Y, Huang W, Gao J, Guo M, Li J, et al. Typically inhibiting USP14 promotes autophagy in M1-like macrophages and alleviates CLP-induced sepsis. Cell Death Dis. 2020;11:666. https://doi.org/10.1038/s41419-020-02898-9.
Helmy KY, Katschke KJ, Gorgani NN, Kljavin NM, Elliott JM, Diehl L, et al. CRIg: a macrophage complement receptor required for phagocytosis of circulating pathogens. Cell. 2006;124:915–27. https://doi.org/10.1016/j.cell.2005.12.039.
Vogt L, Schmitz N, Kurrer MO, Bauer M, Hinton HI, Behnke S, et al. VSIG4, a B7 family-related protein, is a negative regulator of T cell activation. J Clin Invest. 2006;116:2817–26. https://doi.org/10.1172/JCI25673.
Holers VM. Complement and its receptors: new insights into human disease. Annu Rev Immunol. 2014;32:433–59. https://doi.org/10.1146/annurev-immunol-032713-120154.
Zeng Z, Surewaard BGJ, Wong CHY, Geoghegan JA, Jenne CN, Kubes P. CRIg functions as a macrophage pattern recognition receptor to directly bind and capture blood-borne gram-positive bacteria. Cell Host Microbe. 2016;20:99–106. https://doi.org/10.1016/j.chom.2016.06.002.
Wong CH, Jenne CN, Petri B, Chrobok NL, Kubes P. Nucleation of platelets with blood-borne pathogens on Kupffer cells precedes other innate immunity and contributes to bacterial clearance. Nat Immunol. 2013;14:785–92. https://doi.org/10.1038/ni.2631.
Surewaard B, Thanabalasuriar A, Zeng Z, Tkaczyk C, Cohen TS, Bardoel BW, et al. alpha-toxin induces platelet aggregation and liver injury during Staphylococcus aureus sepsis. Cell Host Microbe. 2018;24:271–84. https://doi.org/10.1016/j.chom.2018.06.017.
Hitchcock JR, Cook CN, Bobat S, Ross EA, Flores-Langarica A, Lowe KL, et al. Inflammation drives thrombosis after Salmonella infection via CLEC-2 on platelets. J Clin Invest. 2015;125:4429–46. https://doi.org/10.1172/JCI79070.
Brown KA, Brain SD, Pearson JD, Edgeworth JD, Lewis SM, Treacher DF. Neutrophils in development of multiple organ failure in sepsis. Lancet. 2006;368:157–69. https://doi.org/10.1016/S0140-6736(06)69005-3.
Kolaczkowska E, Jenne CN, Surewaard BGJ, Thanabalasuriar A, Lee W, Sanz M, et al. Molecular mechanisms of NET formation and degradation revealed by intravital imaging in the liver vasculature. Nat Commun. 2015;6:6673. https://doi.org/10.1038/ncomms7673.
Yipp BG, Petri B, Salina D, Jenne CN, Scott BNV, Zbytnuik LD, et al. Infection-induced NETosis is a dynamic process involving neutrophil multitasking in vivo. Nat Med. 2012;18:1386–93. https://doi.org/10.1038/nm.2847.
McDonald B, Urrutia R, Yipp BG, Jenne CN, Kubes P. Intravascular neutrophil extracellular traps capture bacteria from the bloodstream during sepsis. Cell Host Microbe. 2012;12:324–33. https://doi.org/10.1016/j.chom.2012.06.011.
Wu Y, Ren J, Zhou B, Ding C, Chen J, Wang G, et al. Laser speckle contrast imaging for measurement of hepatic microcirculation during the sepsis: a novel tool for early detection of microcirculation dysfunction. Microvasc Res. 2015;97:137–46. https://doi.org/10.1016/j.mvr.2014.10.006.
Protzer U, Maini MK, Knolle PA. Living in the liver: hepatic infections. Nat Rrv Immunol. 2012;12:201–13. https://doi.org/10.1038/nri3169.
Chen J, Wei Y, He J, Cui G, Zhu Y, Lu C, et al. Natural killer T cells play a necessary role in modulating of immune-mediated liver injury by gut microbiota. Sci Rep. 2015;4:7259. https://doi.org/10.1038/srep07259.
Hou X, Zhou R, Wei H, Sun R, Tian Z. NKG2D-retinoic acid early inducible-1 recognition between natural killer cells and kupffer cells in a novel murine natural killer cell-dependent fulminant hepatitis. Hepatology. 2009;49:940–9. https://doi.org/10.1002/hep.22725.
Halder RC, Aguilera C, Maricic I, Kumar V. Type II NKT cell-mediated anergy induction in type I NKT cells prevents inflammatory liver disease. J Clin Invest. 2007;117:2302–12. https://doi.org/10.1172/JCI31602.
Diao H, Kon S, Iwabuchi K, Kimura C, Morimoto J, Ito D, et al. Osteopontin as a mediator of NKT cell function in T cell-mediated liver diseases. Immunity. 2004;21:539–50. https://doi.org/10.1016/j.immuni.2004.08.012.
Weber CR, Liang GH, Wang Y, Das S, Shen L, Yu AS, et al. Claudin-2-dependent paracellular channels are dynamically gated. Elife. 2015;4: e9906. https://doi.org/10.7554/eLife.09906.
Cao Y, Wang Z, Wang Z, Jiang X, Lu W. Inhibition of miR-155 alleviates sepsis-induced inflammation and intestinal barrier dysfunction by inactivating NF-κB signaling. Int Immunopharmacol. 2021;90: 107218. https://doi.org/10.1016/j.intimp.2020.107218.
Manzanares W, Lemieux M, Langlois PL, Wischmeyer PE. Probiotic and synbiotic therapy in critical illness: a systematic review and meta-analysis. Crit Care. 2016;20:262. https://doi.org/10.1186/s13054-016-1434-y.
Yelin I, Flett KB, Merakou C, Mehrotra P, Stam J, Snesrud E, et al. Genomic and epidemiological evidence of bacterial transmission from probiotic capsule to blood in ICU patients. Nat Med. 2019;25:1728–32. https://doi.org/10.1038/s41591-019-0626-9.
Everard A, Lazarevic V, Derrien M, Girard M, Muccioli GG, Neyrinck AM, et al. Responses of gut microbiota and glucose and lipid metabolism to prebiotics in genetic obese and diet-induced leptin-resistant mice. Diabetes. 2011;60:2775–86. https://doi.org/10.2337/db11-0227.
Morowitz MJ, Di Caro V, Pang D, Cummings J, Firek B, Rogers MB, et al. Dietary supplementation with nonfermentable fiber alters the gut microbiota and confers protection in murine models of sepsis. Crit Care Med. 2017;45:e516–23. https://doi.org/10.1097/CCM.0000000000002291.
Kim SM, DeFazio JR, Hyoju SK, Sangani K, Keskey R, Krezalek MA, et al. Fecal microbiota transplant rescues mice from human pathogen mediated sepsis by restoring systemic immunity. Nat Commun. 2020;11:2354. https://doi.org/10.1038/s41467-020-15545-w.
Sterns RH, Grieff M, Bernstein PL. Treatment of hyperkalemia: something old, something new. Kidney Int. 2016;89:546–54. https://doi.org/10.1016/j.kint.2015.11.018.
Macnaughtan J, Soeda J, Mouralidarane A, Sandeman S, Howell C, Kozynchenko O, et al. PMO-127 biological effects of oral nanoporous carbon in bile duct ligated rats. Gut. 2012;61:A124. https://doi.org/10.1136/gutjnl-2012-302514b.127.
Macnaughtan J, Soeda J, Mouralidarane A, Sandeman S, Howell C, Milkhalovsky S, et al. PMO-128 Effects of oral nanoporous carbon therapy in leptin null mice as a model of non-alcoholic steatohepatitis. Gut. 2012;61:A121–5. https://doi.org/10.1136/gutjnl-2012-302514b.128.
Morin EE, Guo L, Schwendeman A, Li X. HDL in sepsis—risk factor and therapeutic approach. Front Pharmacol. 2015;6:244. https://doi.org/10.3389/fphar.2015.00244.
Flegel WA, Baumstark MW, Weinstock C, Berg A, Northoff H. Prevention of endotoxin-induced monokine release by human low- and high-density lipoproteins and by apolipoprotein A-I. Infect Immun. 1993;61:5140–6. https://doi.org/10.1128/iai.61.12.5140-5146.1993.
de Bont N, Netea MG, Demacker PN, Verschueren I, Kullberg BJ, van Dijk KW, et al. Apolipoprotein E knock-out mice are highly susceptible to endotoxemia and Klebsiella pneumoniae infection. J Lipid Res. 1999;40:680–5.
Van Oosten M, Rensen PCN, Van Amersfoort ES, Van Eck M, Van Dam A, Brevé JJP, et al. Apolipoprotein E protects against bacterial lipopolysaccharide-induced lethality. J Biol Chem. 2001;276:8820–4. https://doi.org/10.1074/jbc.M009915200.
Berbee JF, van der Hoogt CC, Kleemann R, Schippers EF, Kitchens RL, van Dissel JT, et al. Apolipoprotein CI stimulates the response to lipopolysaccharide and reduces mortality in gram-negative sepsis. FASEB J. 2006;20:2162–4. https://doi.org/10.1096/fj.05-5639fje.
Thompson PA, Berbee JF, Rensen PC, Kitchens RL. Apolipoprotein A-II augments monocyte responses to LPS by suppressing the inhibitory activity of LPS-binding protein. Innate Immun. 2008;14:365–74. https://doi.org/10.1177/1753425908099171.
Chien J, Jerng J, Yu C, Yang P. Low serum level of high-density lipoprotein cholesterol is a poor prognostic factor for severe sepsis. Crit Care Med. 2005;33:1688–93. https://doi.org/10.1097/01.ccm.0000171183.79525.6b.
McDonald MC, Dhadly P, Cockerill GW, Cuzzocrea S, Mota-Filipe H, Hinds CJ, et al. Reconstituted high-density lipoprotein attenuates organ injury and adhesion molecule expression in a rodent model of endotoxic shock. Shock. 2003;20:551–7. https://doi.org/10.1097/01.shk.0000097249.97298.a3.
Tanaka S, Genève C, Zappella N, Yong-Sang J, Planesse C, Louedec L, et al. Reconstituted high-density lipoprotein therapy improves survival in mouse models of sepsis. Anesthesiology. 2020;132:825–38. https://doi.org/10.1097/ALN.0000000000003155.
Acknowledgements
We thank Amro Abdelgawad (Midyorks NHS Trust, Wakefield, England) for his thoughtful review and comments regarding the manuscript.
Funding
This work was supported by the National Key Research and Development Program of China (2021YFC2501800 [to SYY]), National Natural Science Foundation of China (Grant No. 82071480 [to JCZ]), and Japan Society for the Promotion of Science (Grant: 21H00184 and 21H05612) [to KH]).
Author information
Authors and Affiliations
Contributions
All authors contributed to the literature search and acquisition of data, drafting of the initial manuscript, and critical revision of the final manuscript and approved the final version of the manuscript for publication.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
All authors have provided consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, X., Liu, H., Hashimoto, K. et al. The gut–liver axis in sepsis: interaction mechanisms and therapeutic potential. Crit Care 26, 213 (2022). https://doi.org/10.1186/s13054-022-04090-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04090-1