Abstract
Background
Chest wall loading has been shown to paradoxically improve respiratory system compliance (CRS) in patients with moderate to severe acute respiratory distress syndrome (ARDS). The most likely, albeit unconfirmed, mechanism is relief of end-tidal overdistension in ‘baby lungs’ of low-capacity. The purpose of this study was to define how small changes of tidal volume (VT) and positive end-expiratory pressure (PEEP) affect CRS (and its associated airway pressures) in patients with ARDS who demonstrate a paradoxical response to chest wall loading. We hypothesized that small reductions of VT or PEEP would alleviate overdistension and favorably affect CRS and conversely, that small increases of VT or PEEP would worsen CRS.
Methods
Prospective, multi-center physiologic study of seventeen patients with moderate to severe ARDS who demonstrated paradoxical responses to chest wall loading. All patients received mechanical ventilation in volume control mode and were passively ventilated. Airway pressures were measured before and after decreasing/increasing VT by 1 ml/kg predicted body weight and decreasing/increasing PEEP by 2.5 cmH2O.
Results
Decreasing either VT or PEEP improved CRS in all patients. Driving pressure (DP) decreased by a mean of 4.9 cmH2O (supine) and by 4.3 cmH2O (prone) after decreasing VT, and by a mean of 2.9 cmH2O (supine) and 2.2 cmH2O (prone) after decreasing PEEP. CRS increased by a mean of 3.1 ml/cmH2O (supine) and by 2.5 ml/cmH2O (prone) after decreasing VT. CRS increased by a mean of 5.2 ml/cmH2O (supine) and 3.6 ml/cmH2O (prone) after decreasing PEEP (P < 0.01 for all). Small increments of either VT or PEEP worsened CRS in the majority of patients.
Conclusion
Patients with a paradoxical response to chest wall loading demonstrate uniform improvement in both DP and CRS following a reduction in either VT or PEEP, findings in keeping with prior evidence suggesting its presence is a sign of end-tidal overdistension. The presence of ‘paradox’ should prompt re-evaluation of modifiable determinants of end-tidal overdistension, including VT, PEEP, and body position.
Similar content being viewed by others
Background
Airway driving pressure (DP) is used routinely to guide ‘lung-protective’ ventilation in acute respiratory distress syndrome (ARDS). The effect of tidal volume (VT) on DP is determined by tidal compliance of the integrated respiratory system (CRS), which is comprised of the lungs and chest wall. For a fixed VT and positive end-expiratory pressure (PEEP), any net change in CRS alters DP in the opposite direction. Because they share a common volume, a decrease in compliance of either the lungs (CL) or the chest wall (CCW) simultaneously decreases CRS unless there is a compensatory improvement in its counterpart.
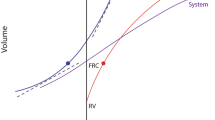
In recent work, reducing lung volume and CCW by external compression, or ‘loading’, has been noted to improve CRS in patients with moderate to severe ARDS [1,2,3,4,5,6]; by immediate implication, loading must therefore result in improved CL and lower transpulmonary pressure in these patients. The most appealing (but as yet unconfirmed) explanation for this counterintuitive mechanical ‘paradox’ (i.e., decreased CCW resulting in improved CRS) is relief of end-tidal overdistension that occurs in the unloaded state.
The purpose of this study was to define how choice of VT and PEEP affect CRS in ARDS patients demonstrating a paradoxical response to chest wall loading. When VT operates in the linear (‘middle’) portion of the pressure–volume relationship, as intended for lung protection, small changes of VT and/or PEEP should leave CRS unaffected [7]. On the other hand, assuming the underlying mechanism of the loading paradox is relief of end-tidal overdistension, we reasoned that ‘paradox positive’ patients would demonstrate a disproportionate reduction in DP (and by extension, increased CRS) following a small decrease of VT or PEEP, both of which alleviate end-tidal overdistension. Conversely, we reasoned that such patients would demonstrate a disproportionate increase in DP (and decreased CRS) following a small increase of VT or PEEP—changes which would exacerbate any end-tidal overdistension.
Methods
This prospective, multi-center physiologic study was performed in two medical intensive care units (Regions Hospital, St. Paul MN, USA and Methodist Hospital, Minneapolis, MN, USA), with all data collected by the same investigative team between December 2021 and March 2022.
Patients
Consecutive patients with ARDS (as defined by the Berlin consensus criteria [8]) who demonstrated no signs of active breathing were enrolled and evaluated. All received invasive mechanical ventilation under controlled conditions, with passive breathing assured by either ongoing administration of neuromuscular blockers or deep sedation sufficient to suppress any evidence of active breathing.
Ventilatory strategy
All patients received mechanical ventilation in volume regulated, control mode (decelerating flow profile) using one of two ventilators: Puritan Bennett 980 (Medtronic; Carlsbad, California, USA) or Maquet Servo-I (Siemens; Bloomfield, Connecticut, USA). Baseline measurements were performed using the VT, PEEP and respiratory rate already prescribed by the clinical team for routine management prior to study enrollment.
Measurements
Measurements were performed in the position of care, either supine or prone, and this was not altered for the purposes of data collection. When possible, study measurements were repeated in the opposite position within 24 h, provided that the criteria for passive breathing were still met.
In the supine orientation, measurements were performed in a semi-recumbent position with the head elevated to 30°; in the prone orientation, measurements were performed with the bed flat (0°). The highest airway pressure during inflation was recorded as the peak pressure. Plateau pressure was measured at least two seconds after performing an end-inspiratory pause. Total PEEP (the sum of set PEEP and auto-PEEP) was measured at least three seconds after performing an end-expiratory pause, assuring that zero flow was achieved.
Measurement of tidal airway pressures were repeated after the following interventions: (1) increasing VT by 1 mL/kg predicted body weight (PBW); (2) decreasing VT by 1 mL/kg PBW; (3) increasing PEEP by 2.5 cmH2O; and (4) decreasing PEEP by 2.5 cmH2O.
Procedure for chest wall loading to detect paradoxical mechanical response
Following baseline measurements (obtained in an unloaded state), manual loading of the chest wall was performed. In the supine position, loading was accomplished by placing a hand over the patient’s umbilicus perpendicular to the axis between the xiphoid process and the pubis; in the prone position, the hand was placed at the approximate mid-point between the inferior costal margin and the iliac crest, perpendicular to the lumbar spine. To gauge load adequacy, an end-inspiratory hold was then performed and manual pressure applied until there was an upward deflection of the pressure–time waveform of ≥ 2 cmH2O, at which point chest wall loading was considered sufficient to influence transpulmonary pressure during tidal breathing. The inspiratory hold on the ventilator was then released, while continuing to apply sustained manual pressure on the abdomen or lumbar region. After five breaths had been delivered, measurements of tidal airway pressure were repeated, and manual pressure was then released.
Statistical analysis
A normality test was performed for all samples to verify a normal distribution. When normality was confirmed, the paired t-test was used to compare mean values of DP and CRS at baseline, during chest wall loading, and following alteration of ventilator parameters as outlined above. In all instances where the normality assumption was not satisfied results were confirmed using the Mann–Whitney test. Differences at the level of a two-tailed P value < 0.05 were considered statistically significant.
Results
Nineteen patients with ARDS were studied, of whom seventeen had ARDS secondary to novel coronavirus (C-ARDS). Seventeen demonstrated a paradoxical response to chest wall loading. Of these, paired measurements were obtained in both the supine and prone positions in eight; in the remaining nine patients, five were evaluated in only the supine position, and four were evaluated in only the prone position. All but one patient had either moderate or severe ARDS, all were ventilated in accordance with lung protective principles for ventilation, and none received extracorporeal support for gas exchange or hemodynamics (Table 1). Mortality at thirty days from the time of data acquisition was 70.6% (12/17). Ventilator settings and gas exchange at baseline are reported in Table 2.
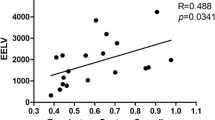
Chest wall loading
Chest wall loading reduced DP by a mean of 3.6 ± 2.3 cmH2O in the supine position and by 2.7 ± 2.3 cmH2O in the prone position (P < 0.01 for both). CRS improved following chest wall loading by a mean of 6.1 ± 3.5 mL/cmH2O in the supine position and 4.1 ± 3.0 mL/cmH2O in the prone position (P ≤ 0.001 for both) (Table 3 and Fig. 1).
Decreasing VT and PEEP in the unloaded state.
Decreasing VT resulted in a reduced DP and an improved CRS in all seventeen patients. DP decreased by a mean of 4.9 ± 2.8 cmH2O in the supine position and 4.3 ± 2.2 cmH2O in the prone position (P ≤ 0.001 for both). CRS improved by a mean of 3.1 ± 2.1 mL/cmH2O in the supine position and 2.5 ± 2.1 mL/cmH2O in the prone position (P ≤ 0.005 for both) (Table 3 and Fig. 2).
Changes in driving pressure by intervention. Individual changes in driving pressure following reduction in PEEP by 2.5 cmH2O (left panel) and tidal volume by 1 ml/kg PBW (right panel). Patients in both the supine (black) and prone (blue dash) positions are represented. Graph is truncated at 5 cmH2O for viewing purposes
Decreasing PEEP similarly resulted in reduced DP and improved CRS in all seventeen patients. DP decreased by a mean of 2.9 ± 1.9 cmH2O in the supine position and 2.2 ± 2.2 cmH2O in the prone position (P ≤ 0.008 for both). CRS improved by a mean of 5.2 ± 3.4 mL/cmH2O in the supine position and 3.6 ± 3.2 mL/cmH2O in the prone position (P ≤ 0.004 for both).
Increasing VT and PEEP
In 6 patients, increasing VT and/or PEEP resulted in an immediate rise of peak airway pressures to above 50 cmH2O; in these cases, attempts to measure airway pressure after 5 tidal breaths had been delivered were not pursued out of concern for patient safety.
VT was increased in twelve patients. An increased DP was observed in eleven of these patients; reduced CRS was observed in eight. In response to the VT increase, DP increased by a mean of 5.5 ± 5.7 cmH2O in the supine position and 3.0 ± 1.3 cmH2O in the prone position (P = 0.03 supine; P < 0.001 prone). CRS deteriorated by a mean of 1.2 ± 4.1 mL/cmH2O in the supine position and 1.1 ± 2.8 mL/cmH2O in the prone position (P = 0.44 supine; P = 0.32 prone) (Additional file 1 Table S1).
Holding VT unchanged, PEEP was increased in fourteen patients; increased DP and reduced CRS were observed in ten of these. In the remaining four, two had no change in DP and CRS, and two had subtle improvements. The PEEP increment caused DP to increase by a mean of 3.4 ± 4.6 cmH2O in the supine position and by 1.0 ± 1.2 cmH2O in the prone position (P = 0.04 supine; P = 0.07 for prone). CRS deteriorated by a mean of 2.2 ± 2.2 mL/cmH2O in the supine position and 1.7 ± 2.4 mL/cmH2O in the prone position (P = 0.01 supine; P = 0.11 prone) (Supplemental Table 1).
Discussion
Among our cohort of patients with moderate-severe ARDS who demonstrated a paradoxical response to manual chest wall loading (17/19), small changes in tidal volume or PEEP exerted strong effects on CRS and DP, despite the intent by their caregivers to follow ‘lung protective’ guidelines to the extent consistent with adequate gas exchange. The presence of mechanical paradox was associated with reduced CRS at baseline; almost all (15/17) paradox positive patients had a baseline CRS < 40 mL/cmH2O, and the majority (11/17) had a baseline CRS ≤ 30 mL/cmH2O. Assuming end-tidal overdistension as the most likely explanation for ‘paradox’, this finding is not unexpected. Because the low compliance state of ARDS reflects primarily the reduced capacity of the ‘baby lung’, as opposed to altered elastic properties of remaining functional lung units [9], the risk of end-tidal overdistension would be expected to rise as compliance declines [10]. The severity of lung disease in our patient sample is also reflected by the CO2 elimination data of Table 2 (PaCO2 and ventilatory ratio).
Interestingly, the presence of paradox itself did not correlate well with duration of mechanical ventilation or hospitalization. While mean duration of hospitalization and of intubation were 16.8 and 11.2 days, respectively, at the time of data collection, over half (9/17) of our patients had been intubated for fewer than six days, and almost one third (5/17) had data collected within one day of intubation.
Consistent with our hypothesis that interventions alleviating end-tidal overdistension would lead to improved mechanics, there was universal improvement in CRS following a minor decrease in either VT or PEEP from the baseline value. Conversely, there was a clear trend toward increased DP and reduced CRS following increases of either machine setting. Indeed, extreme rises in airway pressures in response to small increments of VT or PEEP prevented data from being collected in several patients out of concern for safety; as a result, our data understate the adverse response in our patients with mechanical paradox to increasing either VT or PEEP.
All patients in this study were receiving ventilation with low VT and low to moderate levels of PEEP at baseline; mean VT was 5.6 ± 0.9 mL/kg PBW and mean PEEP was 9.7 ± 3.2 cmH2O. Nonetheless, decreasing VT by 1 mL/kg PBW or PEEP by 2.5 cmH2O resulted in a disproportionate reduction in DP and, therefore, improved CRS. These findings are consistent with those of prior studies demonstrating radiographic evidence of significant hyperinflation in as many as one third of patients treated with a ventilatory strategy targeting 6 mL/kg PBW VT and Pplat < 30 cm H2O [11]; they further demonstrate that no generalized ventilatory strategy, even those generally considered ‘lung-protective,’ can be employed indiscriminately without further concern regarding safety for the individual under care.
The paradoxical response to chest wall loading, in which CRS unexpectedly improves following a decrease in chest wall volume, has been described in several recent reports. In these cases, CRS improved not only in response to direct compression of the chest wall [3, 4, 6], but also in response to interventions that resulted in cephalad displacement of the diaphragm, including abdominal compression [2, 5]; compression of the lumbar region (while prone) [1]; and placement in a less upright position [2, 4, 5]. Considered collectively and in association with the data reported here regarding ventilatory pattern, the most plausible unifying explanation for mechanical paradox is that tidal ventilation infringes on the upper flat portion of the lung’s pressure volume inflation curve. Compression of the chest wall results in a forced volume reduction of lung units otherwise overdistended at end inspiration, leading to descent along the pressure–volume curve to a position more favorable to tidal excursions [12]. Limited data from studies that have used electrical impedance tomography and computed tomography with quantitative density analysis support this hypothesis, even though the precise mechanism remains unconfirmed [4, 6]. An alternative explanation may be that, in the setting of ARDS, heterogeneity gives rise to unaltered lung units that are buttressed by zones of inflammatory debris and edema; as a result, these fortified lung units may be exposed to high transpulmonary pressures without being subjected to injurious strain. In this scenario, volume reduction of such units may still lead to improved CRS, but without the same implications regarding end-tidal overdistension of those embedded individual units.
Limitations
While these findings suggest end-tidal overdistension in patients with mechanical paradox, our study was not designed to be mechanism defining, but rather to focus selectively on the diagnostic value of detecting a paradoxical response to chest wall compression as it pertains to the ventilatory prescription. As such, we did not measure esophageal pressure for the purpose of partitioning CRS into its individual components (CCW and CL). For safety concerns, changes in VT or PEEP were sustained only for brief periods of time and, as noted, in several cases not pursued when small increases were attempted. Although we observed no decreases in oxygen saturation during any loading maneuver or parameter change, the effects of altering the ventilatory prescription on gas exchange or hemodynamics could not be evaluated.
We did not perform interventions in a randomized sequence, primarily because we felt that doing so would compromise the consistency and efficiency of data collection; in each case, however, the duration of alterations was short lived, and the baseline was restored between interventions. As such, we think it is unlikely that randomizing VT and PEEP would have had a significant effect on our findings. Our sample was also drawn primarily from patients affected by C-ARDS, many of whom had been intubated for over a week. Therefore, our results might differ quantitatively (but we suspect not qualitatively) from patients with other forms of severe ARDS. Finally, we emphasize that no conclusions can be drawn regarding the effect of decreasing VT or PEEP on clinical outcomes of paradox positive patients on the basis of our findings.
Clinical implications
Repeated exposure to tidal cycles that cause excessive strain of lung parenchyma is believed to be a proximate stimulus for ventilator-induced lung injury in ARDS [13]. Once a strain threshold is exceeded and mechanical forces disrupt structural microelements, previously functioning lung units will begin to drop out, initiating a positive feedback cycle whereby inflation energy (and power) concentrate among fewer and fewer units [10]. Lung heterogeneity exacerbates this process further, leading to the amplification of stress at the interface of open and closed lung units [14]. Tidal volumes operating in the ‘upper inflection zone’ not only encourage damaging strain—both global and regional, but also risk barotrauma, regional small airway remodeling, and distortion of vulnerable lung units that are hyperinflated at end-inspiration. Such mechanical processes may help explain the highly regionalized emphysematous changes [15], noteworthy incidence of pneumothorax [16], and rapidly evolving bronchiectasis encountered in C-ARDS [17].
In our study, not only was mechanical paradox encountered in all but two of the nineteen patients with ARDS who met our inclusion criteria, but also it was present in spite of consistent adherence to ventilator settings widely regarded as lung-protective; it was frequently encountered early in the course of invasive mechanical ventilation; and the mechanics of all patients with paradox responded favorably to even small reductions in VT and PEEP. The use of manual compression to detect paradox may thus serve as a valuable tool for revealing otherwise undetected excessive tidal strain, and its presence should prompt re-evaluation of modifiable determinants of end-tidal overdistension, including PEEP, VT, and positioning [18, 19]. In some patients with severe and unresolving ARDS, however, protection of the entire lung may simply be impossible without extracorporeal gas exchange as excessive end-tidal strain may be the unavoidable consequence of adequate ventilation.
Conclusions
A paradoxical response to chest wall loading is frequently observed in the setting of moderate to severe ARDS, particularly in the setting of low CRS. Our data demonstrate that paradox can be present early in the course of mechanical ventilation and occur despite conservative application of VT and PEEP. Paradox-positive patients demonstrate uniform improvement of CRS following minor reduction in either VT or PEEP, findings in keeping with prior evidence suggesting that paradox is a sign of tidal overdistension.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- C-ARDS:
-
Acute respiratory distress syndrome secondary to COVID-19
- CL :
-
Lung compliance
- CRS :
-
Respiratory system compliance
- CCW :
-
Chest wall compliance
- DP:
-
Driving pressure
- PEEP:
-
Positive end-expiratory pressure
- PBW:
-
Predicted body weight
- VT :
-
Tidal volume
References
Elmufdi FS, Marini JJ. Dorsal Push and abdominal binding improve respiratory compliance and driving pressure in proned Coronavirus disease 2019 acute respiratory distress syndrome. Crit Care Explor. 2021;3: e0593.
Kummer RL, Shapiro RS, Marini JJ, Huelster JS, Leatherman JW. Paradoxically improved respiratory compliance with abdominal compression in COVID-19 ARDS. Chest. 2021;160:1739–42.
Lassola S, Miori S, Sanna A, Pace R, Magnoni S, Vetrugno L, Umbrello M. Effect of chest wall loading during supine and prone position in a critically ill COVID-19 patient: a new strategy for ARDS? Crit Care. 2021;25:442.
Rezoagli E, Bastia L, Grassi A, Chieregato A, Langer T, Grasselli G, Caironi P, Pradella A, Santini A, Protti A, et al. Paradoxical effect of chest wall compression on respiratory system compliance: A multicenter case series of patients with ARDS. With Multimodal Assessment Chest. 2021;160:1335–9.
Stavi D, Goffi A, Al Shalabi M, Piraino T, Chen L, Jackson R, Brochard L. The pressure paradox: abdominal compression to detect lung hyperinflation in COVID-19 acute respiratory distress syndrome. Am J Respir Crit Care Med. 2022;205:245–7.
Carteaux G, Tuffet S, Mekontso Dessap A. Potential protective effects of continuous anterior chest compression in the acute respiratory distress syndrome: Physiology of an illustrative case. Crit Care. 2021;25:187.
Grasso S, Terragni P, Mascia L, Fanelli V, Quintel M, Herrmann P, Hedenstierna G, Slutsky AS, Ranieri VM. Airway pressure-time curve profile (stress index) detects tidal recruitment/hyperinflation in experimental acute lung injury. Crit Care Med. 2004;32:1018–27.
Force ADT, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–33.
Gattinoni L, Pesenti A. The concept of “baby lung.” Intensive Care Med. 2005;31:776–84.
Marini JJ, Gattinoni L. Time course of evolving ventilator-induced lung injury: The “shrinking baby lung.” Crit Care Med. 2020;48:1203–9.
Terragni PP, Rosboch G, Tealdi A, Corno E, Menaldo E, Davini O, Gandini G, Herrmann P, Mascia L, Quintel M, et al. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007;175:160–6.
Marini JJ, Gattinoni L. Improving lung compliance by external compression of the chest wall. Crit Care. 2021;225:264.
Marini JJ, Gattinoni L. Energetics and the root mechanical cause for ventilator-induced lung injury. Anesthesiology. 2018;128:1062–4.
Cressoni M, Cadringher P, Chiurazzi C, Amini M, Gallazzi E, Marino A, Brioni M, Carlesso E, Chiumello D, Quintel M, et al. Lung inhomogeneity in patients with acute respiratory distress syndrome. Am J Resp Crit Care Med. 2014;189:149–58.
Churg A, Golden J, Fligiel S, Hogg JC. Bronchopulmonary dysplasia in the adult. Am Rev Resp Dis. 1983;127:117–20.
Belletti A, Todaro G, Valsecchi G, Losiggio R, Palumbo D, Landoni G, Zangrillo A. Barotrauma in Coronavirus disease 2019 patients undergoing invasive mechanical ventilation: A systematic literature review. Crit Care Med. 2022;50:491–500.
Gilmartin M, Basirat A, Barry C, Rahman H, Doolan A, Halpenny D, Hogan B, Kooblall M, Lane SJ. Rapid onset cystic bronchiectasis in a mechanically ventilated COVID-19 patient. Am J Resp Crit Care Med. 2022;205:721–2.
Mezidi M, Guerin C. Effect of body position and inclination in supine and prone position on respiratory mechanics in acute respiratory distress syndrome. Intensive Care Med. 2019;45:292–4.
Marrazzo F, Spina S, Forlini C, Guarnieri M, Giudici R, Bassi G, Bastia L, Bottiroli M, Fumagalli R, Langer T. Effects of trunk inclination on respiratory mechanics in patients with COVID-19-associated acute respiratory distress syndrome: Let’s always report the angle! Am J Resp Crit Care Med. 2022;205:582–4.
Acknowledgements
Not applicable.
Funding
No financial support.
Author information
Authors and Affiliations
Contributions
JS, PT, DJD, JSh, LG and JJM contributed to study conception and design. JS and PT performed data acquisition. PSC and JS performed the statistical analysis. JS, PSC, DJD, LG, and JJM interpreted the data. JS, LG and JJM wrote the manuscript. All authors provided critical review of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study (A21-280) was approved by the HealthPartners Institutional Review Board. Written and verbal consent was obtained from legal surrogate decision makers in all cases prior to enrollment.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
Response to increased tidal volume and positive end-expiratory pressure VT was increased by 1 mL/kg PBW in a total of twelve patients (baseline values for these twelve patients in column A); PEEP was increased by 2.5 cmH2O in a total of fourteen patients (baseline values for these fourteen patients in column B). DP driving pressure, CRS system compliance, VT tidal volume, PEEP positive end-expiratory pressure.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Selickman, J., Tawfik, P., Crooke, P.S. et al. Paradoxical response to chest wall loading predicts a favorable mechanical response to reduction in tidal volume or PEEP. Crit Care 26, 201 (2022). https://doi.org/10.1186/s13054-022-04073-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04073-2