Abstract
Background
Clarithromycin may act as immune-regulating treatment in sepsis and acute respiratory dysfunction syndrome. However, clinical evidence remains inconclusive. We aimed to evaluate whether clarithromycin improves 28-day mortality among patients with sepsis, respiratory and multiple organ dysfunction syndrome.
Methods
We conducted a multicenter, randomized, clinical trial in patients with sepsis. Participants with ratio of partial oxygen pressure to fraction of inspired oxygen less than 200 and more than 3 SOFA points from systems other than the respiratory function were enrolled between December 2017 and September 2019. Patients were randomized to receive 1 gr of clarithromycin or placebo intravenously once daily for 4 consecutive days. The primary endpoint was 28-day all-cause mortality. Secondary outcomes were 90-day mortality; sepsis response (defined as at least 25% decrease in SOFA score by day 7); sepsis recurrence; and differences in peripheral blood cell populations and leukocyte transcriptomics.
Results
Fifty-five patients were allocated to each arm. By day 28, 27 (49.1%) patients in the clarithromycin and 25 (45.5%) in the placebo group died (risk difference 3.6% [95% confidence interval (CI) − 15.7 to 22.7]; P = 0.703, adjusted OR 1.03 [95%CI 0.35–3.06]; P = 0.959). There were no statistical differences in 90-day mortality and sepsis response. Clarithromycin was associated with lower incidence of sepsis recurrence (OR 0.21 [95%CI 0.06–0.68]; P = 0.012); significant increase in monocyte HLA-DR expression; expansion of non-classical monocytes; and upregulation of genes involved in cholesterol homeostasis. Serious and non-serious adverse events were equally distributed.
Conclusions
Clarithromycin did not reduce mortality among patients with sepsis with respiratory and multiple organ dysfunction. Clarithromycin was associated with lower sepsis recurrence, possibly through a mechanism of immune restoration.
Clinical trial registration clinicaltrials.gov identifier NCT03345992 registered 17 November 2017; EudraCT 2017-001056-55.
Similar content being viewed by others
Introduction
Sepsis mortality remains unacceptably high, reaching 26.7% for in-hospital cases and 41.9% for patients hospitalized in the intensive care unit (ICU) [1]. It accounts for 19.7% of global deaths [2], and it is accompanied by considerable long-term morbidity [3]. Despite early recognition, timely antimicrobial administration and organ support, further adjunctive therapies are required [4]. However, the majority of potential interventions targeting the host immune response yielded conflicting results [5,6,7,8,9,10,11], possibly due to incomplete understanding of underlying pathophysiological mechanisms [12].
Macrolides may exert immune-modulating effects [13], as demonstrated for the exacerbation of chronic obstructive pulmonary disease [14] and for the management of community-acquired pneumonia (CAP) [15, 16]. Combination therapy with β-lactams leads to decreased mortality and is currently recommended as first-line treatment in CAP [16]. Our group investigated the immune-modulating properties of clarithromycin in severe infections caused by bacteria outside the macrolide antimicrobial spectrum, i.e., ventilator-associated pneumonia (VAP) and Gram-negative infections. Results showed that adjunctive clarithromycin, compared to placebo, improved survival among the most severely ill patients, particularly those with acute respiratory dysfunction syndrome (ARDS) [17, 18]. This benefit has been associated with improving signs of sepsis-induced immunosuppression, a hallmark of the protracted course of healthcare-associated infections [19]. This was characterized by higher production of interleukin (IL)-6 from circulating monocytes, decrease in the ratio of circulating IL-10 to TNFα (tumor necrosis factor-alpha) and increase in CD86 expression on circulating monocytes.
Based on those observations, we initiated the INtravenous CLArithromycin in Sepsis and multiple organ dysfunction Syndrome (INCLASS) study with the aim to assess the adjunctive role clarithromycin on top of standard-of-care treatment for high-risk patients with healthcare-associated infections and sepsis.
Patients and methods
Ethics
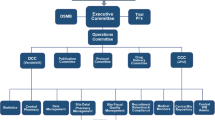
INCLASS was a phase 3, multi-center, randomized, placebo-controlled, double blind, clinical trial, conducted in thirteen study sites (11 multidisciplinary ICUs and 2 general Internal Medicine wards) in tertiary, teaching hospitals in Greece and Belgium (additional information in Additional files 1 and 2). The protocol and informed consent form were approved in Greece [National Organization for Medicines (51239/01-06-2017), National Ethics Committee (52086/2017)] and Belgium [Federal Agency of Medicines and Health Products (1078386/16-04-2018), Central Ethics Committee, Erasme University Hospital (P2018/376, 19-10-2018)]. Study registration was with EudraCT (2017-001056-55) and Clinicaltrials.gov (NCT03345992). Written informed consent was provided by patients or legal representatives, prior to inclusion. The complete study protocol and history of amended versions are provided in Additional files 1 and 2.
Participants
Adults with sepsis and multiple organ dysfunction syndrome (MODS) were eligible to participate. Inclusion criteria were sepsis associated with hospital-acquired (HAP), healthcare-associated pneumonia (HCAP), VAP, primary Gram-negative bacteremia or intra-abdominal infection; PaO2/ FiO2 < 200; and total Sequential Organ Failure Assessment (SOFA) score for non-respiratory organ dysfunctions more than 3. Main exclusion criteria were pregnancy or lactation, neutropenia (< 1000 neutrophils/ mm3), recent high-dose corticosteroid intake, macrolide allergy and macrolide intake for the current infection. A complete list of exclusion criteria and definitions is provided in Additional file 1.
Randomization and intervention
Patients were assigned to blind treatment with clarithromycin or placebo, following a random allocation sequence, with a 1:1 design and by block sizes of 10, stratified per study site. The allocation sequence was generated by an independent statistician prior to the study commencement and delivered to each study site within sealed individual envelopes, labeled as per study participant code. The envelope was unsealed by the study pharmacist, to prepare the study drug. All other parties involved (investigators, patients, healthcare providers, data collectors) were blinded to the study arm.
Patients were randomized to intravenous clarithromycin (1gr dissolved into 20 ml water for injection and then diluted to a final volume of 250 ml 5% dextrose in water) or placebo (equal volume of water for injection diluted to a final volume of 250 ml 5% dextrose in water), infused once daily within 1 h, for four consecutive days. The final preparations were visually similar. Other therapies were left at the discretion of the attending physicians. There was no specific time window from enrollment to study drug administration, which was required to be as soon as logistically possible.
Procedures
Patients were followed-up daily until day 28 or hospital discharge (whichever came first). In case of earlier discharge, visit of day 28 was performed by phone call, to assess the primary outcome and safety. Another phone call was performed at day 90 with the patient or their caregiver, to assess survival. Data were captured in one Case Report Form; source data verification was performed by trained clinical research associates. Adverse events were captured daily until day 28 or discharge, and as patient or provider-reported events up to day 90. National Cancer Institute Common Terminology Criteria for Adverse Events, version 5.0 (2017), were used for classification.
Blood cell populations and monocyte human leukocyte antigen (mHLA)-DR expression were measured on days 1, 5 and 10, using flow cytometry. Total ribonucleic acid (RNA) was isolated from PAXgene blood RNA tubes (Qiagen), collected on days 1 and 5, using PaxGene Blood miRNA kits according to the manufacturer’s instructions (Qiagen). RNA-sequencing libraries were prepared using KAPA RNA Hyperprep with RiboErase (Roche) kits. Libraries were sequenced using the Illumina HiSeq4000 instrument (Illumina). All day 1 sampling was performed before study drug administration. Detailed methodology and bioinformatics are shown in Additional file 1.
Outcomes
The primary outcome was 28-day all-cause mortality. Secondary outcomes were 90-day mortality; 28-day mortality in septic shock; early sepsis response (≥ 25% decrease in day 3 SOFA score from baseline); sepsis response (≥ 25% decrease in day 7 SOFA score from baseline); new sepsis among patients with sepsis response; the time to new sepsis episode; and differences in cell populations and gene expression.
Statistical analysis
The sample size was calculated for the primary endpoint, anticipating a 55% 28-day mortality, among control patients with sepsis and respiratory dysfunction, and 25% reduction with clarithromycin [17, 18]. To detect this difference, with 80% power at 10% significance level, 55 patients were required in each study arm. No interim analysis was planned.
Clinical outcomes were assessed on an intention-to-treat principle, according to the pre-defined statistical analysis plan (Additional file 2). The Fisher’s two-sided exact test, confirmed by logistic regression analysis, was used to assess the primary outcome. Kaplan–Meier curves were used to assess survival by arm, and the arm effect on 28-day mortality was evaluated with Cox-regression model. Univariate and stepwise multivariable logistic regression analyses were done using pre-specified co-variables (age, sex, SOFA, Acute Pathophysiology and Chronic Health Evaluation—APACHE II, Charlson comorbidity index—CCI, and adequacy of empirical antimicrobial treatment) associated with 28-day mortality. The treatment effect on secondary outcomes was compared with the Pearson Chi-square test, or the two-sided Fisher’s exact test, if categorical, whereas quantitative variables were assessed using Student’s t test, or Mann–Whitney U test, as appropriate. Subgroup analyses were pre-planned and are shown in Additional file 1.
A number of post hoc multivariable regression analyses were performed with regard to the primary outcome, to explore whether a simplified model, adapted for the study sample size (including SOFA, CCI, appropriateness of empirical antimicrobial treatment), early versus late start of treatment and co-administered antimicrobials would impact on 28-day mortality. The impact of enrollment site was assessed by the Breslow–Day test, and heterogeneity was further evaluated by the I2 statistic. Post hoc Cox- and Poisson regression analyses were performed to assess the cumulative incidence of new sepsis and further explore study outcomes (IBM SPSS statistics, version 24.0). Any two-tailed p < 0.05 was considered significant. No adjustment was performed for multiple comparisons, and secondary endpoints should be interpreted as exploratory.
RNA-sequencing data analysis, as well as the I2 statistic for study site heterogeneity, was performed in R (version 3.51, R Core Team 2014). Additional information is provided in Additional file 1.
Results
Baseline characteristics
From December 2017 to June 2019, 241 patients were assessed for eligibility and 110 were randomized to blind treatment. The first patient was enrolled on December 20, 2017, and the last visit of the last participant was on September 22, 2019. Main reasons for exclusion of patients were respiratory ratio ≥ 200, non-eligible infections and immunosuppression (Fig. 1). Fifty-five patients were included in each study arm within median 2 (1–4) days after meeting inclusion criteria and 4 (1–6) days after sepsis onset. One patient (1.8%) in the clarithromycin arm did not receive any dose of study drug due to early death, and another patient (1.8%) in the clarithromycin arm did not receive the fourth dose of the study drug due to protocol deviation judged to be a study team error. There were no losses to follow-up, nor consent withdrawals, and all 110 patients were included in the analysis of the primary endpoint and the 90-day outcomes.
Overall, baseline demographic and clinical characteristics were similar between study arms; patients were predominantly male, with high comorbidity burden and high SOFA and APACHE II scores. VAP was the most common infection (Table 1; Additional file 1: Tables S1 and S2). Enrollment by participating site is shown in Additional file 1: Table S3.
Primary outcome
By day 28, 27 (49.1%) patients in the clarithromycin group and 25 (45.5%) in the placebo group had died, yielding an absolute difference in mortality risk of 3.6% (95%CI − 15.7 to 22.7; P = 0.703); the unadjusted odds ratio (OR) for clarithromycin relative to placebo was 1.16 (95% CI 0.55–2.45; P = 0.849) (Table 2). This was confirmed by survival analysis (Fig. 2A). After adjustment for covariates, the OR was 1.03 (95%CI 0.35–3.06; P = 0.604) (Additional file 1: Table S4), and the model was able to explain 30.3% of 28-day mortality variance. No heterogeneity related to study site was detected (Additional file 1: Figure S1). Study enrollment within the first 48 h from sepsis onset did not impact final outcome (Additional file 1: Table S5). In post hoc regression analysis, the study drug treatment effect remained unaltered by the type of antimicrobial treatment (Additional file 1: Tables S6 to S10).
Twenty-eight-day survival among trial participants (A) 28-day survival analysis by Kaplan–Meier curves among patients with sepsis and multiple organ dysfunction syndrome, treated with clarithromycin or placebo. Hazard ratio is provided by Cox-regression analysis. (B) Risk of death within 28-days in pre-specified subgroups among patients treated with clarithromycin or placebo. P values for interactions between treatment arm and subgroup are provided by the Breslow–Day test. *Calculated using the Firth correction. ARDS, acute respiratory distress syndrome; CI, confidence intervals; ICU, intensive care unit; SOFA, Sequential Organ Failure Assessment
No differences regarding the primary outcome were detected in any of the 8 pre-planned subgroup analyses. However, treatment impacted differently patients with extreme disease severity (within the highest quartile of SOFA) compared to those with lower SOFA scores, as well as patients enrolled in the general ward, compared to those in the ICU (Fig. 2B).
Secondary outcomes
There were no significant differences between treatment arms in 90-day mortality (OR 1.31 [95%CI 0.57–3.05]; P = 0.672) (Table 2). Subgroup analysis suggested differential treatment response among patients with and without extremely severe disease, with clarithromycin favoring better outcomes among patients with SOFA score 12 or more (Additional file 1: Figure S2).
Early sepsis response by day 3 (OR 0.68 [95%CI 0.31–1.47]; P = 0.430) and sepsis response by day 7 did not differ (OR 0.69 [95%CI 0.33–1.47]; P = 0.445). Twenty-three patients in the clarithromycin group and 28 patients in the placebo group had sepsis response by day 7; in seven (30.4%) and 19 (67.9%), respectively, sepsis recurred (OR 0.21 [95%CI 0.06–0.68]; P = 0.012) (Table 2). In Poisson regression model, the incident rate of new septic episodes in the clarithromycin arm was lower than in the placebo arm (incident rate ratio [IRR] 0.44 [95% CI 0.19–0.99]; P = 0.048), and in Cox-regression analysis, survival free from new sepsis episode was significantly prolonged, following clarithromycin treatment (Additional file 1: Figure S3).
The type and pathogen of the first recurrent septic episode among patients with sepsis response by day 7 are shown in Additional file 1: Table S11 and did not differ between the two study arms. The distribution of recurrent septic sites, compared to the original infections, is presented in Additional file 1: Table S12 and mainly concerned cases of pneumonia.
Impact of clarithromycin treatment on the host immune response
Treatment with clarithromycin was associated with an increase in non-classical monocytes on day 10 (Additional file 1: Figure S4). Counts of classical monocytes, T cells, B cells and NK cells remained unaltered. A significant increase in mHLA-DR expression was also observed among clarithromycin-treated patients on day 10, compared to placebo (Additional file 1: Figure S5).
Similarly, among those with sepsis response on day 7, patients in the clarithromycin arm presented higher levels of HLA-DR on day 10 (Additional file 1: Figure S6).
Gene set enrichment analysis identified a cholesterol homeostasis gene set upregulated in the clarithromycin-treated group, relative to placebo (Additional file 1: Results and Figures S7–9).
Safety
At least one serious adverse event (SAE) was reported for most of the participants. SAEs were equally distributed among the groups of treatment (Table 3). Eight cases of acute kidney injury were reported as SAEs: seven in the clarithromycin arm and one in the placebo arm. Nil case was reported as associated with the study drug. With the exception of one case in each group, the other cases of acute kidney injury presented several days after the stop of the study drug. The investigators associated all eight cases either with sepsis progression or with the administration of other drugs (Additional file 1: Table S13). The two groups of treatment did not differ in the incidence of non-serious adverse events (Additional file 1: Table S14). In nil patient, the study drug was discontinued [20].
Discussion
In this randomized clinical trial, adjunctive clarithromycin treatment did not affect 28-day survival among patients with sepsis and MODS. Clarithromycin treatment was associated with fewer sepsis recurrences among patients with original sepsis response and findings compatible with modulation of the immune response toward return to homeostasis. However, due to the limited study size secondary outcomes were not adjusted for multiple comparisons and subgroup analyses showing treatment benefit need to be interpreted with caution. Overall study mortality was high. This was anticipated since the baseline SOFA score was high (median 10 in the placebo group; median 11 in the clarithromycin group).
The finding on sepsis recurrence is in agreement with the secondary benefit of clarithromycin treatment in patients with CAP. In this RCT, patients were randomized to β-lactam monotherapy or to combination of β-lactams and clarithromycin. Fewer patients receiving combination therapy were readmitted to hospital by day 30, mostly due to recurrence of pneumonia [21].
Subgroup analysis suggested 90-day survival benefit among extremely severe patients with SOFA score 12 or more. However, such a benefit was missing from patients with SOFA score less than 12 and these patients may be even harmed. However, the limited size of the study population makes this post hoc survival benefit inconclusive. The incidence of acute kidney was greater in the clarithromycin arm, although no association with the study drug was documented.
The above-described clinical benefit in the clarithromycin group may be linked with the modulation of the host immune response toward recovery from sepsis-induced immunosuppression. This is reflected by the increase in mHLA-DR expression and expansion of non-classical monocytes. Low mHLA-DR expression is a hallmark of sepsis-induced immune suppression, associated with secondary infections and mortality, while recovery is a surrogate of improved outcomes [22] and has been used to monitor immunotherapy efficacy [23, 24]. This is in line with previous observations from our group in VAP; clarithromycin treatment was associated with better ex vivo function of PBMCs, decreased IL-10/ TNFα ratio, improved antigen presentation and greater apoptosis of monocytes, consistent with immune restoration [20].
Although non-referring to the entire study population, transcriptomic data indicated that genes involved in cholesterol biosynthesis were altered in clarithromycin-treated patients, relative to placebo, at study day 5. Other data also indicate the presence of an axis between cholesterol synthesis, antigen presentation and monocyte reprogramming toward a trained immunity phenotype [25,26,27]. Whether this axis is modulated by clarithromycin remains to be demonstrated.
Our study had four main limitations: (a) the limited sample size to detect secondary outcomes with sufficient power and to account for multiple testing and differences among subgroups; (b) the probability for type II error. Although the anticipated 25% difference in the primary outcome used for power calculation was ambitious, the authors expected that the prognostic enrichment in MODS patients (where clarithromycin had shown maximum benefit) would translate into the same treatment effect, shown in both previous RCTs [17, 18]; (c) the high infection rate, exceeding 50%, by extremely or pan-drug-resistant isolates, particularly Acinetobacter baumannii, making direct comparisons with other European ICUs complicated. This may have also prevented survival benefit from being demonstrated, while lower sepsis recurrence in this high-resistance setting may be considered as a relevant clarithromycin treatment outcome; and (d) the delay in study enrollment reaching median of 4 days after sepsis onset.
Conclusions
Among patients with sepsis and MODS, clarithromycin did not affect all-cause 28-day mortality; sepsis recurrence among patients with sepsis response by day 7 was decreased. Reprogramming of genes involved in cholesterol biosynthesis pathway in circulatory immune cells may underlie this process.
Availability of data and materials
The sequence libraries generated in this study are publicly available through the National Center for Biotechnology Information (NCBI) gene expression omnibus (GEO) under the accession number GSE196117. Requests for de-identified and protected health information (PHI)-stripped patient data can be made to the corresponding author with specific data needs, analysis and dissemination plans. Previous Institutional Review Board (IRB)/Independent Ethics Committee (IEC) approval will be required, if applicable. Dates will be time-shifted to eliminate PHI, as needed. Requests for supporting documents, such as statistical analysis plan, complete trial protocol and subsequent protocol amendments, can also be addressed to the corresponding author with specific needs, analysis and dissemination plans. All the above requests will be reviewed by the study sponsor for release, upon publication. Contact: egiamarel@med.uoa.gr.
Abbreviations
- APACHE:
-
Acute Pathophysiology and Chronic Health Evaluation
- ARDS:
-
Acute respiratory distress syndrome
- CAP:
-
Community-acquired pneumonia
- CCI:
-
Charlson comorbidity index
- HAP:
-
Hospital-acquired pneumonia
- HCAP:
-
Healthcare-associated pneumonia
- ICU:
-
Intensive care unit
- IRR:
-
Incident rate ratio
- mHLA-DR:
-
Monocyte human leukocyte antigen-DR
- MODS:
-
Multiple organ dysfunction syndrome
- OR:
-
Odds ratio
- RCT:
-
Randomized controlled trial
- RNA:
-
Ribonucleic acid
- SOFA:
-
Sequential Organ Failure Assessment
- VAP:
-
Ventilator-associated pneumonia
References
Fleischmann-Struzek C, Mellhammar L, Rose N, Cassini A, Rudd KE, Schlattmann P, et al. Incidence and mortality of hospital- and ICU-treated sepsis: results from an updated and expanded systematic review and meta-analysis. Intensive Care Med. 2020;46:1552–62.
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the global burden of disease study. Lancet. 2020;395:200–11.
Prescott HC, Angus DC. Enhancing recovery from sepsis: a review. JAMA. 2018;319:62–75.
Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, et al. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015;372:1301–11.
WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J, Angus DC, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324:1330–1341.
Annane D, Bellissant E, Bollaert PE, Briegel J, Keh D, Kupfer Y, et al. Corticosteroids for treating sepsis in children and adults. Cochrane Database Syst Rev. 2019;12:CD002243.
Hotchkiss RS, Colston E, Yende S, Angus DC, Moldawer LL, Crouser ED, et al. Immune checkpoint inhibition in sepsis: a phase 1b randomized, placebo-controlled, single ascending dose study of antiprogrammed cell death-ligand 1 antibody (BMS-936559). Crit Care Med. 2019;47:632–42.
Shakoory B, Carcillo JA, Chatham WW, Amdur RL, Zhao H, Dinarello CA, et al. Interleukin-1 receptor blockade is associated with reduced mortality in sepsis patients with features of macrophage activation syndrome: reanalysis of a prior phase III trial. Crit Care Med. 2016;44:275–81.
Leentjens J, Kox M, Koch RM, Preijers F, Joosten LA, van der Hoeven JG, et al. Reversal of immunoparalysis in humans in vivo: a double-blind, placebo-controlled, randomized pilot study. Am J Respir Crit Care Med. 2012;186:838–45.
Vincent JL, Marshall JC, Dellinger RP, Simonson SG, Guntupalli K, Levy MM, et al. Talactoferrin in severe sepsis: results from the phase ii/iii oral talactoferrin in severe sepsis trial. Crit Care Med. 2015;43:1832–8.
Francois B, Jeannet R, Daix T, Walton AH, Shotwell MS, Unsinger J, et al. Interleukin-7 restores lymphocytes in septic shock: the IRIS-7 randomized clinical trial. JCI Insight. 2018;3:e98960.
Van der Poll T, Shankar-Hari M, Wiersinga WJ. The immunology of sepsis. Immunity. 2021;54:2450–64.
Reijnders TDY, Saris A, Schultz MJ, van der Poll T. Immunomodulation by macrolides: therapeutic potential for critical care. Lancet Respir Med. 2020;8:619–30.
Herath SC, Normansell R, Maisey S, Poole P. Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2018;10:CD009764.
Vardakas KZ, Trigkidis KK, Apiranthiti KN, Falagas ME. The dilemma of monotherapy or combination therapy in community-acquired pneumonia. Eur J Clin Invest. 2017. https://doi.org/10.1111/eci.12845.
Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and treatment of adults with community-acquired pneumonia—an official clinical practice guideline of the american thoracic society and infectious diseases society of America. Am J Respir Crit Care Med. 2019;200:e45–67.
Giamarellos-Bourboulis EJ, Mylona V, Antonopoulou A, Tsangaris I, Koutelidakis I, Marioli A, et al. Effect of clarithromycin in patients with suspected Gram-negative sepsis: results of a randomized controlled trial. J Antimicrob Chemother. 2014;69:1111–8.
Giamarellos-Bourboulis EJ, Pechère JC, Routsi C, Plachouras D, Kollias S, Raftogiannis M, et al. Effect of clarithromycin in patients with sepsis and ventilator-associated pneumonia. Clin Infect Dis. 2008;46:1157–64.
Tsaganos T, Raftogiannis M, Pratikaki M, Christodoulou S, Kotanidou A, Papadomichelakis E, et al. Clarithromycin leads to long-term survival and cost benefit in ventilator-associated pneumonia and sepsis. Antimicrob Agents Chemother. 2016;60:3640–6.
Spyridaki A, Raftogiannis M, Antonopoulou A, Tsaganos T, Routsi C, Baziaka F, et al. Effect of clarithromycin in inflammatory markers of patients with ventilator-associated pneumonia and sepsis caused by Gram-negative bacteria: results from a randomized clinical study. Antimicrob Agents Chemother. 2012;56:3819–25.
Garin N, Genné D, Carballo S, Chuard C, Eich G, Hugli O, et al. β-Lactam monotherapy vs β-lactam-macrolide combination treatment in moderately severe community-acquired pneumonia: a randomized noninferiority trial. JAMA Intern Med. 2014;174:1894–901.
Leijte GP, Rimmelé T, Kox M, Bruse N, Monard C, Gossez M, et al. Monocytic HLA-DR expression kinetics in septic shock patients with different pathogens, sites of infection and adverse outcomes. Crit Care. 2020;24:110.
Hotchkiss RS, Colston E, Yende S, Crouser ED, Martin GS, Albertson T, et al. Immune checkpoint inhibition in sepsis: a Phase 1b randomized study to evaluate the safety, tolerability, pharmacokinetics, and pharmacodynamics of nivolumab. Intensive Care Med. 2019;45:1360–71.
Meisel C, Schefold JC, Pschowski R, Baumann T, Hetzger K, Gregor J, et al. Granulocyte-macrophage colony-stimulating factor to reverse sepsis-associated immunosuppression: a double-blind, randomized, placebo-controlled multicenter trial. Am J Respir Crit Care Med. 2009;180:640–8.
Brands X, Haak BW, Klarenbeek AM, Butler J, Uhel F, Qin W, et al. An epigenetic and transcriptomic signature of immune tolerance in human monocytes through multi-omics integration. Genome Med. 2021;13:131.
Barlage S, Gnewuch C, Liebisch G, Wolf Z, Audebert FX, Glück T, et al. Changes in HDL-associated apolipoproteins relate to mortality in human sepsis and correlate to monocyte and platelet activation. Intensive Care Med. 2009;35:1877–85.
Arts RJ, Novakovic B, Ter Horst R, Carvalho A, Bekkering S, Lachmandas E, et al. Glutaminolysis and fumarate accumulation integrate immunometabolic and epigenetic programs in trained immunity. Cell Metab. 2016;24:807–19.
Acknowledgements
The authors acknowledge Miltiades Kyprianou (Hellenic Institute for the Study of Sepsis), who provided statistical advice and support throughout the clinical trial. They also wish to thank the patients, their families and the clinical, laboratory and research staff of each site, who contributed to the trial.
Notation of abstract publication/ presentation
Some of the results were presented as an abstract at the 32nd European Congress of Clinical Microbiology and Infectious Diseases (ECCMID-Abstract 03038); Lisbon, Portugal; April 23–26, 2022.
Funding
The study was supported by the Hellenic Institute for the Study of Sepsis and by the Horizon2020 Marie Skłodowska-Curie International Training Network “the European Sepsis Academy” (grant number 676129—granted to the National and Kapodistrian University of Athens). The funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
EJGB conceptualized the study design, participated in data analysis and drafting of the manuscript, had full access to all of the study data and takes responsibility for the integrity of the data and the accuracy of the data analysis. EK participated in data analysis and drafted the manuscript, had full access to all of the study data and takes responsibility for the integrity of the data and the accuracy of the data analysis. EJGB, EK, MR and IM verified the underlying data. BPS analyzed the RNA-sequencing data, participated in data analysis and critically revised the manuscript for important intellectual content. AK performed laboratory measurements and critically revised the manuscript for important intellectual content. MR, IM, NK, KP, EM, AP, PC, EP, ITS, FF, ML, ND, DDB, IF, SA, EA, MP, GV, EM, AA, DG and IT enrolled patients, collected clinical data and critically revised the manuscript for important intellectual content. ITS and TR analyzed the flow cytometry data and critically revised the manuscript for important intellectual content. WJW contributed in data interpretation and critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript to be submitted for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the declaration of Helsinki and national and institutional standards. The protocol and informed consent form were approved in Greece [National Organization for Medicines (51239/01-06-2017), National Ethics Committee (52086/2017)] and Belgium [Federal Agency of Medicines and Health Products (1078386/16-04-2018), Central Ethics Committee, Erasme University Hospital (P2018/376, 19-10-2018)]. Study registration was with EudraCT (2017-001056-55) and Clinicaltrials.gov (NCT03345992). Written informed consent was provided by patients or legal representatives, prior to inclusion.
Consent for publication
Not applicable.
Competing interests
E. Karakike is supported by the Horizon2020 Marie Skłodowska-Curie International Training Network “the European Sepsis Academy” (grant number 676129- granted to the National and Kapodistrian University of Athens). I.T. Schrijver is supported by the Horizon2020 Marie Skłodowska-Curie International Training Network “the European Sepsis Academy” (grant number 676129- granted to Lausanne University Hospital) and received a scholarship from the Société Académique Vaudoise (Lausanne, Switzerland). N. Dauby is a post-doctorate clinical master specialist of the Belgian F.R.S-FNRS and reports personal fees from Roche and Boehringer Ingelheim, and non-financial support from Pfizer, Janssen and Merck Sharp & Dohme, all outside the submitted work. T. Roger is funded by the European Union Horizon 2020 Marie Skłodowska-Curie Action Innovative Training Network European Sepsis Academy (ESA-ITN, grant number 676129) and by the European Union Horizon 2020 grant ImmunoSep (847422). W. J. Wiersinga is supported by the Netherlands Organization for Scientific Research (VIDI grant 91716475) and the Horizon2020 Marie Skłodowska-Curie International Training Network “the European Sepsis Academy” and received consulting fee paid to the host institution from MDS, GSK and Swedish Orphan Biovitrum AB. A. Antoniadou has received honoraria from Gilead, Pfizer, MSD, ViiV, BMS, Astellas and independent educational grants from Gilead, GSK and Biotest. D. Grimaldi received consultation fees from Transgene SA Illkirch-Graffenstaden (France). E. J. Giamarellos-Bourboulis has received honoraria from Abbott CH, bioMérieux, GSK, InflaRx GmbH, ThermoFisher Brahms GmbH, Sobi and XBiotech Inc; independent educational grants from Abbott CH, AxisShield, bioMérieux Inc, InflaRx GmbH, Johnson & Johnson, MSD, Sobi and XBiotech Inc.; and funding from the Horizon2020 Marie Skłodowska-Curie International Training Network “the European Sepsis Academy” (granted to the National and Kapodistrian University of Athens); the Horizon 2020 European Grants ImmunoSep and RISC in COVID (granted to the Hellenic Institute for the Study of Sepsis); and the Horizon Health grant EPIC-CROWN-2 (granted to the Hellenic Institute for the Study of Sepsis). The other authors do not report any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
^David De Bels This author passed away.
Supplementary Information
Additional file 1.
Contains Supplementary Methods and Results.
Additional file 2.
Contains the complete Study Protocol versions 1 and 2, a detailed description of amendments between protocol versions and the Statistical Analysis Plan.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Karakike, E., Scicluna, B.P., Roumpoutsou, M. et al. Effect of intravenous clarithromycin in patients with sepsis, respiratory and multiple organ dysfunction syndrome: a randomized clinical trial. Crit Care 26, 183 (2022). https://doi.org/10.1186/s13054-022-04055-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04055-4