Abstract
The rationale for the provision of nitrogen from proteins given via the enteral route or from intravenous amino acids is to boost the synthesis of muscle proteins, and thereby to limit the severity of intensive care unit-acquired weakness by the prevention of muscle loss. However, the optimal timing for supplemental nitrogen provision is a matter of debate and controversy. Indeed, consistent data from retrospective studies support an association between high early protein intakes and better outcomes, while recent post-hoc findings from prospective studies raise safety concerns. This pro–con paper details the arguments of both sides and highlights the need for large-scale prospective studies assessing the safety and efficacy of different levels of protein intake in combination with physical activity and summarizes the currently recruiting clinical trials.
Similar content being viewed by others
Introduction
A large consensus supports the provision of high protein intakes during the late phase of critical illness, e.g., during recovery when the ability to increase the synthesis of muscle proteins from the pool of circulating amino acids increases [1, 2]. However, controversial views are expressed regarding the amount of proteins to be given during the early phase of critical illness, when muscle protein breakdown outweighs muscle synthesis as a result of the resistance to anabolic stimuli [3, 4]. The proportion of nitrogen losses to be compensated by protein intake in the critically ill is a matter of debate, as reflected by recommendations cited in the most recently published guidelines: 1.2–2.5 g/kg of protein per day [5, 6] and the provision of an amount of protein lower than nitrogen losses [1, 4], in agreement with the “Baby stomach” concept [7]. These discrepant views based on experts’ opinions reflect the paucity of data from adequately powered clinical studies assessing the effects of different amounts of proteins on relevant endpoints [8].
Meanwhile, industrial companies recently started to market nutritional formulas containing high amounts of proteins or amino acids and promoted their use early during the course of critical illness, following experts’ opinions mainly based on associations between high nitrogen intakes and better outcomes and on biochemical arguments. The marketing of these solutions is possible as the legal standards do not require the same sequence of testing as for a new drug, i.e., phase I clinical trials to check the safety, phase II clinical trials to assess the efficacy, and phase III clinical trials to compare the new treatment with the current standard of care. In the field of nutrition, this sequence is usually not followed; as a result the issue of safety may have been overlooked [9]. Nonetheless, the issues raised by the three phases of clinical testing are relevant for nutritional solutions as well as for any new therapeutic modality.
The community of clinicians is then left with conflicting arguments either supporting the use of high protein solutions or cautioning against this practice (Fig. 1). This manuscript intends to summarize the arguments supporting both sides and the current clinical research.
High nitrogen intake during the early phase of critical illness: the pros
The renewed enthusiasm for high protein intake results mainly from attention paid to ICU-acquired muscle weakness (ICU-AW). Indeed, the importance of ICU-AW in the outcome of critically ill patients has been underlined by the description of long-term physical impairments and disabilities impairing the quality of life of survivors and increasing healthcare-related costs. The time course of muscle wasting is characterized by an initial abrupt drop in muscle mass and function followed by a slow, progressive recovery [10,11,12,13]. Recently, decreased mitochondrial biogenesis and dysregulated lipid oxidation have been reported as contributors to compromised skeletal muscle bioenergetic status [14]. Clinically, in addition to a decrease in functional autonomy and quality of life, this prolonged muscle weakness represents a huge burden for society as a high proportion of patients who required an ICU stay lasting several days are unable to return to work or even to home [15].
The prevention of ICU-AW requires a multi-modal “bundle” approach, including the avoidance of sedation, early mobilization, and ambulation. The inclusion of high protein intakes in this bundle of measures appears logical as an adjunctive measure to limit the loss of muscle mass and function by boosting the synthesis of muscle proteins. High protein intake is expected to stimulate new protein synthesis, thereby preserving muscle mass [6]. The combination of physical activity, including active and passive mobilization, with high protein nutritional formulas or supplemental intravenous amino acids was suggested as a “must” for physical rehabilitation. Research in this area was even ranked as the number one priority by a group of experts [16]. Compelling retrospective data on large cohorts of patients support these expectations, as improved survival was observed in patients who received the highest amounts of protein, regardless of their physical activity [17,18,19,20].
The results of a recent clinical prospective study confirm that it is possible to increase the circulating pool of amino acids with an enteral solution containing high amounts of proteins [21], in spite of high splanchnic extraction of some amino acids [22]. In other interventional studies, intravenous infusion of amino acids was found to be safe in patients at risk of acute renal failure [23] and transiently improved muscle function [24]. Improved 90-day survival was even found in a post-hoc analysis in the subset of patients with normal renal function [25].
Parallel to this quantitative approach, the qualitative aspects of proteins can also represent a promising area of clinical research. For instance, whey proteins could increase muscle synthesis more efficiently than soy or casein-based solutions as a result of their higher digestibility, their higher content in leucine, and their insulinotropic properties [26, 27]. Likewise, the effects of semi-elemental or elemental solutions should be re-considered as a means to improve digestibility and protein availability during enteral nutrition [28].
High nitrogen intake during the early phase of critical illness: the cons
On the “con” side of high protein intake, no clinical benefit has been reported from interventional studies comparing solutions containing high amounts of nutrients, including proteins, with standard amounts [29,30,31,32]. However, in contrast to a potential benefit on muscle protein synthesis, the issue of the safety of high nitrogen intake during the acute phase of critical illness is an emerging concern. Indeed, a preplanned post-hoc analysis of the PEPaNIC study [33] that evaluated the effects of withholding parenteral nutrition in critically ill children suggests a linear positive correlation between the amount of amino acids provided and poorer outcome in the children randomized to the early parenteral nutrition group, until day 4 after admission [34] . The underlying mechanisms are not fully understood and are currently being investigated. Besides increased urea generation reported in the EAT-ICU (Early Goal-Directed Nutrition in ICU Patients) trial [35], increased production of glucagon leading to further oxidation of amino acids has also been reported [36].
Teleologically, muscle wasting could be considered a desirable consequence of adaptive anabolic resistance and lasts a few hours or days after injury [37]. The inability to respond to anabolic stimuli during the acute phase can be considered as a component of an adaptive response designed to provide substrates for gluconeogenesis in order to meet the requirements of vital organs and systems, an event known as auto-cannibalization or auto-cannibalism [3]. In this scenario, the loss of muscle would serve to supply gluconeogenetic organs. Likewise, the ability of muscles to build myofibrils will be limited and the provision of high amounts of amino acids will not attenuate the muscle wasting and could even amplify the degradation of amino acids.
Conclusions
The risk-to-benefit ratio of the provision of high amounts of proteins or amino acids during the early phase of critical illness is largely unknown. Some aspects have been investigated, while others are still unexplored.
Importantly, the optimal combination of proteins and physical activity is unknown [38]. This is a key issue when early physical activity is feasible and probably beneficial. Of note, the needs and protein metabolism of elderly and/or obese patients can differ from those of the overall ICU population [6, 39, 40].
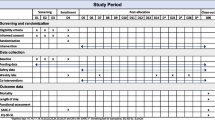
Hopefully, some of the pending issues could be answered by some of the ongoing trials registered on clinicaltrials.gov (Table 1). Most of the currently recruiting studies are prospective randomized controlled trials. The inclusion criteria studies are highly variable, even though an anticipated long stay and the requirement for mechanical ventilation are mandatory in most trials. The primary outcomes tend to focus on physical function in several studies, while all-cause mortality is less commonly used as a primary outcome. A wide range of interventions are being tested and compared to the standards of care, from supplemental proteins (1.5–3.0 g/kg/day) alone to combination with standardized physical activity.
Meanwhile, owing to the potential risks of high amounts of proteins, the principle of precaution should prevail, i.e., the provision of 0.3–0.8 g proteins/kg/day during the early phase of critical illness. We definitely need to appraise more precisely the risk-to-benefit ratio by characterizing the relevant risks and measuring muscle function at the bedside as a proxy for the benefit of high protein intake.
Abbreviations
- EAT-ICU:
-
Early Goal-directed Nutrition in ICU Patients
- ICU:
-
Intensive care unit
- ICU-AW:
-
ICU-acquired muscle weakness
- PEPaNIC:
-
Early versus late parenteral nutrition in the pediatric intensive care unit
References
Preiser J-C, van Zanten ARH, Berger MM, Biolo G, Casaer MP, Doig GS, et al. Metabolic and nutritional support of critically ill patients: Consensus and controversies. Crit Care. 2015;19:35.
Heyland D, Stapleton R, Compher C. Should we prescribe more protein to critically ill patients? Nutrients [Internet]. 2018;10:462.
Preiser J-C, Ichai C, Orban J-C, Groeneveld ABJ. Metabolic response to the stress of critical illness. Br J Anaesth. 2014;114:945–54.
Rooyackers O, Sundström Rehal M, Liebau F, Norberg Å, Wernerman J. High protein intake without concerns? Crit Care. 2017;21:106.
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. J Parenter Enter Nutr. 2016;40:159–211.
Hurt RT, McClave SA, Martindale RG, Ochoa Gautier JB, Coss-Bu JA, Dickerson RN, et al. Summary points and consensus recommendations from the International Protein Summit. Nutr Clin Pract. 2017;32(1_suppl):142S–51S.
Preiser J-C, Wernerman J. Provision of nutrients to the acutely ill. Introducing the “baby stomach” concept. Am J Respir Crit Care Med. 2017;196:1089–90.
Hoffer LJ, Bistrian BR. Appropriate protein provision in critical illness: A systematic and narrative review. Am J Clin Nutr. 2012;96:591–600.
Preiser J-C, Wernerman J. REDOXs: Important answers, many more questions raised! J Parenter Enter Nutr. 2013;37:566–7.
Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, et al. Acute skeletal muscle wasting in critical illness. JAMA. 2013;310:1591–600.
Reid CL, Campbell IT, Little RA. Muscle wasting and energy balance in critical illness. Clin Nutr. 2004;23:273–80.
Klaude M, Mori M, Tjäder I, Gustafsson T, Wernerman J, Rooyackers O. Protein metabolism and gene expression in skeletal muscle of critically ill patients with sepsis. Clin Sci. 2012;122:133–42.
Gamrin-Gripenberg L, Sundström-Rehal M, Olsson D, Grip J, Wernerman J, Rooyackers O. An attenuated rate of leg muscle protein depletion and leg free amino acid efflux over time is seen in ICU long-stayers. Crit Care. 2018;22:13.
Puthucheary ZA, Astin R, Mcphail MJW, Saeed S, Pasha Y, Bear DE, et al. Metabolic phenotype of skeletal muscle in early critical illness. Thorax. 2018;73:926–35.
Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–304.
Arabi YM, Casaer MP, Chapman M, Heyland DK, Ichai C, Marik PE, et al. The intensive care medicine research agenda in nutrition and metabolism. Intensive Care Med. 2017;43:1239–56.
Allingstrup MJ, Esmailzadeh N, Wilkens Knudsen A, Espersen K, Hartvig Jensen T, Wiis J, et al. Provision of protein and energy in relation to measured requirements in intensive care patients. Clin Nutr. 2012;31:462–8.
Nicolo M, Heyland DK, Chittams J, Sammarco T, Compher C. Clinical outcomes related to protein delivery in a critically ill population: a multicenter, multinational observation study. JPEN J Parenter Enteral Nutr. 2016;40:45–51.
Weijs PJM, Stapel SN, de Groot SDW, Driessen RH, de Jong E, Girbes ARJ, et al. Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients. J Parenter Enter Nutr. 2012;36:60–8.
Compher C, Chittams J, Sammarco T, Nicolo M, Heyland DK. Greater protein and energy intake may be associated with improved mortality in higher risk critically ill patients. Crit Care Med. 2017;45:156–63.
van Zanten ARH, Petit L, De Waele J, Kieft H, de Wilde J, van Horssen P, et al. Very high intact-protein formula successfully provides protein intake according to nutritional recommendations in overweight critically ill patients: a double-blind randomized trial. Crit Care. 2018;22:156.
Liebau F, Wernerman J, Van Loon LJC, Rooyackers O. Effect of initiating enteral protein feeding on whole-body protein turnover in critically ill patients. Am J Clin Nutr. 2015;101:549–57.
Doig GS, Simpson F, Bellomo R, Heighes PT, Sweetman EA, Chesher D, et al. Intravenous amino acid therapy for kidney function in critically ill patients: a randomized controlled trial. Intensive Care Med. 2015;41:1197–208.
Ferrie S, Allman-Farinelli M, Daley M, Smith K. Protein requirements in the critically ill: a randomized controlled trial using parenteral nutrition. JPEN J Parenter Enteral Nutr. 2016;40:795–805.
Zhu R, Allingstrup MJ, Perner A, Doig GS, Nephro-Protective Trial Investigators Group. The effect of IV amino acid supplementation on mortality in ICU patients may be dependent on kidney function: post hoc subgroup analyses of a multicenter randomized trial. Crit Care Med. 2018;46:1293–301.
Marik PE. Feeding critically ill patients the right ‘whey’: thinking outside of the box. A personal view. Ann Intensive Care. 2015;5:11.
Adams RL, Broughton KS. Insulinotropic effects of whey: mechanisms of action, recent clinical trials, and clinical applications. Ann Nutr Metab. 2016;69:56–63.
Seres DS, Ippolito PR. Pilot study evaluating the efficacy, tolerance and safety of a peptide-based enteral formula versus a high protein enteral formula in multiple ICU settings (medical, surgical, cardiothoracic). Clin Nutr. 2017;36:706–9.
Rugeles S, Villarraga-Angulo LG, Ariza-Gutiérrez A, Chaverra-Kornerup S, Lasalvia P, Rosselli D. High-protein hypocaloric vs normocaloric enteral nutrition in critically ill patients: A randomized clinical trial. J Crit Care. 2016;35:110–4.
Petros S, Horbach M, Seidel F, Weidhase L. Hypocaloric vs normocaloric nutrition in critically ill patients: a prospective randomized pilot trial. JPEN J Parenter Enteral Nutr. 2014;40:242–9.
Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, et al. Early versus late parenteral nutrition in critically ill adults. N Engl J Med. 2011;365:506–17.
Rice TW, Wheeler AP, Thompson BT, Steingrub J, Hite RD, Moss M, et al. Initial trophic vs full enteral feeding in patients with acute lung injury: the EDEN randomized trial. JAMA. 2012;307:795–803.
Fivez T, Kerklaan D, Mesotten D, Verbruggen S, Wouters PJ, Vanhorebeek I, et al. Early versus late parenteral nutrition in critically ill children. N Engl J Med. 2016;374:1111–22.
Vanhorebeek I, Verbruggen S, Casaer MP, Gunst J, Wouters PJ, Hanot J, et al. Effect of early supplemental parenteral nutrition in the paediatric ICU: a preplanned observational study of post-randomisation treatments in the PEPaNIC trial. Lancet Respir Med. 2017;5:475–83.
Allingstrup MJ, Kondrup J, Wiis J, Claudius C, Pedersen UG, Hein-Rasmussen R, et al. Early goal-directed nutrition versus standard of care in adult intensive care patients: the single-centre, randomised, outcome assessor-blinded EAT-ICU trial. Intensive Care Med. 2017;43(11):1637–47.
Thiessen SE, Derde S, Derese I, Dufour T, Vega CA, Langouche L, et al. Role of glucagon in catabolism and muscle wasting of critical illness and modulation by nutrition. Am J Respir Crit Care Med. 2017;196:1131–43.
Soeters MR, Soeters PB. The evolutionary benefit of insulin resistance. Clin Nutr. 2012;31:1002–7.
Preiser JC, De Prato C, Harvengt A, Peters L, Bastin M-H, Fraipont V, et al. Passive cycling limits myofibrillar protein catabolism in unconscious patients : a pilot study. J Nov Physiother. 2014;4:1–6.
Dickerson RN. Hypocaloric, high-protein nutrition therapy for critically ill patients with obesity. Nutr Clin Pract. 2014;29:786–91.
Dickerson R. Nitrogen balance and protein requirements for critically ill older patients. Nutrients. 2016;8:226.
Author information
Authors and Affiliations
Contributions
JCP drafted and wrote this manuscript. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author declares that he has no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Preiser, JC. High protein intake during the early phase of critical illness: yes or no?. Crit Care 22, 261 (2018). https://doi.org/10.1186/s13054-018-2196-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-018-2196-5