Abstract
Background
Sepsis coincides with altered gene expression in different tissues. Accumulating evidence has suggested that microRNAs, long non-coding RNAs, and circular RNAs are important molecules involved in the crosstalk with various pathways pertinent to innate immunity, mitochondrial functions, and apoptosis.
Methods
We searched articles indexed in PubMed (MEDLINE), EMBASE and Europe PubMed Central databases using the Medical Subject Heading (MeSH) or Title/Abstract words (“microRNA”, “long non-coding RNA”, “circular RNA”, “sepsis” and/or “septic shock”) from inception to Sep 2016. Studies investigating the role of host-derived microRNA, long non-coding RNA, and circular RNA in the pathogenesis of and as biomarkers or therapeutics in sepsis were included. Data were extracted in terms of the role of non-coding RNAs in pathogenesis, and their applicability for use as biomarkers or therapeutics in sepsis. Two independent researchers assessed the quality of studies using a modified guideline from the Systematic Review Center for Laboratory animal Experimentation (SYRCLE), a tool based on the Cochrane Collaboration Risk of Bias tool.
Results
Observational studies revealed dysregulation of non-coding RNAs in septic patients. Experimental studies confirmed their crosstalk with JNK/NF-κB and other cellular pathways pertinent to innate immunity, mitochondrial function, and apoptosis. Of the included studies, the SYRCLE scores ranged from 3 to 7 (average score of 4.55). This suggests a moderate risk of bias. Of the 10 articles investigating non-coding RNAs as biomarkers, none of them included a validation cohort. Selective reporting of sensitivity, specificity, and receiver operating curve was common.
Conclusions
Although non-coding RNAs appear to be good candidates as biomarkers and therapeutics for sepsis, their differential expression across tissues complicated the process. Further investigation on organ-specific delivery of these regulatory molecules may be useful.
Similar content being viewed by others
Background
Sepsis is defined as the presence of a life-threatening organ dysfunction as a result of altered systemic host response to an infection [1, 2]. This leads to multiple organ failure and superimposed secondary infections. The in-hospital mortality may reach 40% in the presence of septic shock [2, 3]. Recently, genome-wide expression analysis of the critically ill revealed more than 80% of the essential genetic elements were altered [4].
A class of non-coding RNAs, comprising microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), are increasingly being recognized as regulators of various signaling pathways and are thus known as regulatory RNAs. These molecules play important roles in biological processes, including innate immunity, mitochondrial functions, and apoptosis [5–9].
miRNAs are RNA molecules of 21 to 25 nucleotides in length synthesized in all healthy and diseased cells. By binding to complementary sequences in the 3’ untranslated regions of target mRNAs, miRNAs regulate a range of genes post-transcriptionally [10]. These regulatory polynucleotides play dual roles, either protective or detrimental, in cancers, neurodegenerative diseases, and immune-related diseases [11]. Notably, miRNAs are essential for the production of proinflammatory tumor necrosis factor (TNF)-α and interleukin (IL)-1β via p38 mitogen-activated protein kinase (MAPK) and MAPK phosphatase 1 (MKP-1) pathways [6–9, 12–14]. In case-control studies, differential expression of miRNAs was detected in patients with sepsis compared to controls, suggesting that miRNAs may be used as biomarkers for diagnosis and prognostic stratification or as therapeutic targets [8, 12, 15–21].
lncRNAs comprise more than 200 nucleotides, representing another group of transcripts. The mechanisms of lncRNAs in health and disease have been comprehensively reviewed [22, 23]. Recently, several in-vitro studies have documented the differential expression of lncRNAs in human tubular epithelial cells, monocytes, and cardiomyocytes after exposure to the plasma of septic patients or lipopolysaccharide (LPS) [24–26]. The role of lncRNAs in sepsis remains largely unknown. Massive screening of lncRNAs in human umbilical vein endothelial cells revealed that LPS treatment altered the expression of these non-coding RNAs by 28- to 70-fold [27]. Sporadic studies indicate that these changes might modulate inflammatory response. For instance, a lncRNA designated lnc-IL7R interacts with the human IL-7 receptor α subunit gene and hence alleviates the LPS-induced proinflammatory response [28]. In a murine sepsis model, lncRNA-HOTAIR appeared to modulate TNF-α production in cardiomyocytes via the nuclear factor (NF)-κB pathway [25].
circRNAs have been recognized as a distinct entity of non-coding regulatory RNAs fairly recently [29]. The circular structure stabilizes these molecules, favoring their use as biomarkers. Although our understanding of this new molecular member in sepsis remains sparse, experimental knockdown of a circRNA, RasGEF1B, deciphers the complex interaction of multiple cellular pathways in sepsis [30].
In this systematic review, we discuss the new paradigms of regulatory non-coding RNAs in the pathogenesis of sepsis and their potential as biomarkers and therapeutic targets.
Methods
Searching strategy and selection of studies
We searched articles indexed in PubMed (MEDLINE), EMBASE and Europe PubMed Central databases using Medical Subject Heading (MeSH) or Title/Abstract words (“microRNA or miRNA or lncRNA or circRNA” and “sepsis or septic shock”) from inception up to 30 Sep 2016. There were no limitations imposed on language or type of study. We included original research articles in which the role of host-derived regulatory RNAs (miRNA, lncRNA, or circRNA) in sepsis was examined in relation to disease pathogenesis, diagnosis, prognosis, and treatment. Investigation on exogenous regulatory RNAs or non-original research articles such as review articles, conference proceedings, editorials, and book chapters were excluded. Titles and abstracts were independently screened for relevancy by two authors. Disagreement was resolved by consensus or consultation with senior authors.
Data extraction and study quality assessment
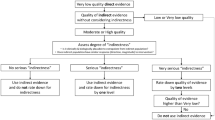
Data were extracted in terms of the role of non-coding RNAs (i.e., non-coding RNA species investigated, laboratory detection methods, and cellular pathways) and their use as biomarkers or therapeutic agents. The following data were abstracted: (1) first author and year of publication; (2) type of study; (3) non-coding RNA species investigated; (4) methods used to detect the corresponding non-coding RNA; (5) number of replicates/specimens (in vitro and in vivo studies) or patients (clinical studies); (6) cellular pathways involved; and (7) major conclusions. Two researchers independently performed the data extraction and evaluated the quality of the included studies using a modified guideline from the Systematic Review Center for Laboratory Animal Experimentation (SYRCLE), a tool based on the Cochrane Collaboration Risk of Bias tool [31]. One item concerning random housing of animals was removed in the modified version. This tool contains nine items assessing selection bias, performance bias, detection bias, attrition bias, and reporting bias. These factors are common amongst in vitro, in vivo, and human studies. The higher the SYRCLE score was, the better the quality of the study would be. The maximum achievable score is 9.
Results
A total of 239 papers were found based on the search criteria, in which 128 original studies investigating miRNAs, lncRNAs, or circRNAs in sepsis were included. Of these, eight articles examined the role of lncRNAs or circRNAs, whereas the remaining investigated miRNAs. The papers excluded were either not original articles, or not directly related to sepsis, or had lack of evidence of deregulation of the studied miRNA/lncRNAs/circRNAs in sepsis (Fig. 1). Two authors independently searched the literature database and agreed with the data abstracted as summarized in Additional file 1 (Table S1). Of the 128 included studies, 24, 28, and 20 were purely in vitro, in vivo, or human studies, respectively. The remaining employed multiple models (i.e., a combination of in vitro, in vivo, or human studies). The SYRCLE scores ranged from 3 to 7, with an average score of 4.55.
In general, studies of non-coding RNAs in sepsis focus on immunological dysregulation and evaluation of these as biomarkers. Other active research areas include the impact of their alteration on endothelial dysfunction, organ failure, and evaluation as therapeutic agents. These are summarized in Table 1. An altered expression of non-coding RNAs involves multiple cellular populations and signaling pathways leading to changes in immune response, hormonal imbalance, metabolic and mitochondrial dysfunction, epithelial integrity, and coagulation-defects [1, 3, 31–36].
Changes in miRNA expression are detectable after exposure of cells, animals, or healthy human volunteers to sublethal concentration of LPS. Some of the miRNAs (e.g., miR-155, miR-143) are upregulated while many others (e.g. miR-125b, miR-146b, miR-150, miR-340, let7g) are downregulated [12, 37–48]. The intricate crosstalk between miRNAs and various cellular pathways is depicted in Fig. 2.
Role of microRNA (miRNA) and long non-coding RNA (lncRNA) in sepsis. HuR, Human antigen R; eNOS, Endothelial nitric oxide synthase; MDSC, Myeloid derived suppressor cell; CISH, Cytokine-inducible SH2-containing protein; JNK, c-Jun N-terminal kinases (JNK); IRAK, Interleukin-1 receptor-associated kinase; MyD88, Myeloid differentiation primary response gene 88; TRAF6, TNF receptor-associated factor 6; BMPR2, Bone morphogenetic protein receptor type II; IkB, Inhibitor of Kappa B; NFkB, Nuclear factor kappa B; Sirt1, Sirtulin 1; Pim1, Proto-oncogene serine/threonine-protein kinase; SOX6, Sex-determining region Y box 6; PDCD4, Programmed cell death 4; BMAL1, Brain and muscle ARNT-like 1; PRKC, Primary rat kidney cell; PGC1a, PPAR gamma co-activator 1A
Expression of non-coding RNAs differs in response to the specific microbial moiety encountered. For instance, the expression level of let-7a in leukocytes was reduced in healthy humans after exposure to LPS but not after exposure to lipoteichoic acid or double-stranded RNA [38]. Similarly, the expression of miR-150 was reduced significantly after exposure to LPS but was elevated when challenged by lipoteichoic acid and polyinosinic-polycytidylic acid double-stranded RNA [13].
Of the 22 subpopulations included in the 10 articles evaluating non-coding RNAs as biomarkers, none of them included an external validation cohort. Selective reporting of sensitivity, specificity, and receiver operating curve was common. Reporting of sensitivity and specificity was absent in 13 subpopulations. Two authors reported only an area under the curve (AUC) value without a confidence interval. The study population and the non-coding RNAs investigated were heterogeneous, precluding the performance of meta-analysis. The sensitivity of miRNA biomarkers ranges from 38 to 80%, whereas specificity ranged from 71.4 to 100%. The predictability of miRNA markers is summarized in Table 2.
Discussion
Pathogenesis
This literature review indicates that the pattern of non-coding RNA expression differs substantially upon encountering various microbial moieties [38, 41]. Analysis of peripheral blood by quantitative RT-PCR and miRNA microarrays has been widely used for expression profiling of miRNA in septic patients [15, 16, 49, 50]. Notably, several miRNA species, including miR-126, miR-21, miR-16, and miR-27a, increased more than 30-fold in sepsis [15]. Single-candidate miRNA studies have established the association of miR-146a, miR-25, and miR-15a/16 with sepsis [17, 51–54]. Further stratification of the systemic inflammatory response syndrome (SIRS) from sepsis revealed differential miRNA deregulation [16]. These results suggest that miRNA expression may be pathogen-specific and that its pattern could be used as biomarkers or therapeutic targets.
Immunological changes
miRNAs and lncRNAs are involved in both proinflammatory and anti-inflammatory responses in sepsis [55–58]. Notably, the majority of lncRNAs responsive to LPS stimulus contain one or more binding sites for known inflammatory mediators such as p65, IRF3, JunB, and cJun [58]. Exposure of cell lines and animal models to LPS is a popular method for investigating their roles in inflammation. In an LPS model of murine sepsis, an increased expression of miR-15a/16 reduced the phagocytic activity of macrophages and increased mitochondrial oxidative stress, resulting in a proinflammatory phenotype [59, 60]. Overexpression of miR-15a/16 in the LPS-treated murine macrophage RAW264.7 downregulated the expression of Toll-like receptor (TLR)4 and IL-1 receptor-associated kinase 1 (IRAK1), contributing to immunosuppressive phenotypes [53, 61]. Similarly, expression of miR-205-5b alleviates the expression of high mobility group box 1 (HMGB1) [62].
The production of proinflammatory TNF-α is finely controlled at both the transcriptional and translational levels by miRNAs. Upregulation of miR-181 enhances TNF-α mRNA degradation [60]. In a THP-1 human promonocytic cell model, miR-146a increased in a time-dependent manner on LPS/TLR4 stimulation, suppressing the production of proinflammatory cytokines in a feed-forward loop [63, 64].
Cytokine homeostasis can also be achieved in a negative feedback manner. Upregulation of miR-146a inhibits IRAK-1 and p-IKBa in THP-1 cells exposed to S. typhimurium [65]. Binding of NF-κB to DICER increased the levels of mature miR-125b in hepatocytes, suppressing TNF-α expression [66]. In CD14+ neonatal monocytes, enforced expression of miR-125b suppresses translation of TNF-α [67]. Silencing of CD14 by small interfering (si)RNA abolishes the production of TNF-α and IL-6 [68].
As sepsis progresses, the immune system is reprogrammed into a stage characterized by persistent inflammation and immunosuppression [69, 70]. These are mediated in part by miRNAs, which promote immune cell polarization, suppress proinflammatory cytokines, and control leukocyte apoptosis [71–74]. For instance, the expression of miR21 and miR-181b in myeloid -derived suppressor cells in septic mice precludes the differentiation of macrophages and dendritic cells [72, 75–77]. Given the extensive crosstalk between miRNAs and other cellular pathways, inflammatory responses can be modulated by interfering upstream or downstream mediators. By targeting Bmal1, NF-κB-p65/RelA phosphorylation was inhibited by miR-155 [78, 79]. Interestingly, transcription of primary miR-155 and other three miRNAs (miR-455, miR-125a, and miR-146) is dependent on NF-κB [80]. The expression of NF-κB and its interaction with miRNAs has been demonstrated in trauma patients with sepsis [81]. Upregulation of miR-19a in patients with sepsis or SIRS correlates with the extent of systemic inflammation [82]. Experimental silencing of miRNAs has further confirmed the importance of these regulatory nucleotides in limiting inflammation in sepsis. Transfection of anti-miR-210 into the murine macrophage RAW264.7 and human HEK293 cells enhanced LPS-induced production of IL-6, TNF-α, and inducible nitric oxide synthase (iNOS) [83, 84].
Observational studies have demonstrated an association between sepsis-induced coagulopathy and miRNA expression [85, 86]. Compared with severe sepsis patients with normal platelet counts, the expression of miR-130a in peripheral blood monocytic cells was significantly lower in septic patients with thrombocytopenia [86]. Longitudinal samples of sepsis patients revealed a sustainable increase of miR-122 up to 14 days after admission to the intensive care unit and showed a strong correlation with antithrombin III (R = 0.913, p < 0.001) [87]. To determine direct or indirect effects of miRNAs on coagulation, further mechanistic studies are required to identify crosstalk, if any, between cytokines, thrombocyte synthesis/apoptosis, and deregulation of miRNAs.
Endothelial dysfunction
Sepsis-induced endothelial activation and injury is mediated in part by the Slit2-Robo4 pathway [88]. Downregulation of Slit2 reduced the expression of miR-218, modulating endothelial inflammation [88]. A disintegrin and metalloproteinase (ADAM)15 is another mediator responsible for increased endothelial permeability. An in-silico analysis of human vascular endothelial cells revealed that miR-147b degrades ADAM15 mRNA. The endothelial protective function of miR-147b was further confirmed by in vitro experiments of overexpression and co-incubation with miR-147b antagomir (a miRNA inhibitor) [89]. In response to proinflammatory cytokines, miR-146a/b expression in endothelial cells is also increased [90]. These miRNAs target NF-κB, activator protein-1 (AP-1), and MAPK/Egr-1 pathways and, in turn, abolish the production of proinflammatory cytokines in a negative-feedback loop. Knocking out miR-146a in mice aggravates the expression of VCAM-1 in the endothelium. These collectively suggest that miRNAs prevent endothelial activation, which may otherwise be aggravated by proinflammatory cytokines in sepsis [91–93].
Cardiopulmonary impairment
The lung accounts for more than 45% of the primary sites of infection in sepsis patients [79]. Development of acute respiratory distress syndrome is one of the serious complications seen in sepsis patients; the prevalence ranges from 6 to 16% [94–96]. Amongst those who developed severe sepsis, the prevalence of cardiovascular and respiratory failure increased up to 90% [97].
In the context of sepsis-associated pulmonary injury, miRNAs interfere with JNK/PPARγ and cholinergic pathways which, in turn, contribute to pulmonary inflammation or inflammatory resolution [98–103]. Exposure of rats to LPS increased the production of TNF-α and IL-1β in the myocardium accompanied by upregulation of miR-194-3p, miR-344a-3p, miR-465-3p, miR-501-5p, miR-3596c, miR-185-3p, and miR-877 [104]. In vitro studies showed that the increased expression of miR-127 de-represses Bcl6/Dusp1, which in turn activates JNK and promotes macrophage polarization toward the M1 phenotype [100, 105]. Intratracheal administration of miR-127 in mice has confirmed M1 skewing and exaggerated pulmonary edema and infiltration [100]. Peculiarly, the level of miR-127 decreased transiently during the very early stages of sepsis in an attempt to minimize pulmonary inflammation. The mechanisms leading to subsequent sustainable de-repression remain unknown.
Sepsis-induced cardiac dysfunction is characterized by impaired myocardial contractility and reduced ejection fraction [106]. Increasing evidence has suggested the role of lncRNAs and miRNAs in these processes [24, 25, 107–110]. In myocardial cells, a lncRNA, HOTAIR, was induced after exposure to LPS. This correlates with increased TNF-α production and NF-κB p65 phosphorylation [25]. Investigation of neonatal rat cardiomyocytes demonstrated that LPS inhibited the expression of miR-499, which in turn de-repressed SOX6 and PCDC4 leading to cardiomyocyte apoptosis through activation of the Bcl-2 family apoptotic pathway [111].
Implications on other major organs
A global observational study involving 14,573 severe sepsis patients from 37 countries revealed that a considerable proportion of them developed hepatic (20%) and renal impairment (40%) [97].
Ample evidence has indicated a change in miRNAs/lncRNAs in the liver [112, 113], kidneys [114, 115], and skeletal muscles [116, 117] in sepsis, associated with organ failure. In a rat model of sepsis, the upregulation of miR-142-3 was detected by 18 h after cecal ligation and puncture (CLP). This change in expression level reduced adenylyl cyclase 9 expression in liver macrophages, which may prevent macrophages from resolving the proinflammatory response in a cyclic adenosine monophosphate (cAMP)-dependent manner [112]. Experimental knockdown of miR-21 in LPS-septic mice resulted in upregulation of programmed cell death protein 4, increased apoptosis, and exacerbated LPS-induced kidney injury [114]. Sequencing of RNA extracted from human proximal tubular epithelial cells after exposure to plasma from septic humans with acute kidney injury revealed significantly increased expression of linc-ATP13A4-8 as compared with exposure to those from septic patients without kidney involvement [26]. Urosepsis caused by Candida spp., although infrequent, is responsible for high mortality and severe kidney injury. Intraperitoneal injection of Candida albicans into C57BL/6 mice revealed an impaired renal glomerular filtration rate accompanied by a significant reduction in miR-204/211, leading to upregulation of a heme oxygenase, Hmx1 [115]. Administration of miR-204/211 mimics reduced the expression of Hmx1 and alleviated kidney injury. These results confirmed the protective role of miR-204/211 in maintaining kidney functions via Hmx1 in sepsis.
Limited studies have investigated the role of miRNAs in sepsis-induced myopathy [117, 118]. Clinical studies revealed that muscle-associated miRNAs are dysregulated in sepsis [118]. In a porcine sepsis model, significant upregulation of two miRNA species (miR-146-5p and miR-221-5p) was detected, suggesting the possible involvement of these miRNAs in muscle catabolism in sepsis [117].
Biomarkers
While regulatory RNAs have been recognized for more than a decade, their use as biomarkers for sepsis diagnosis and prognostication has not been thoroughly investigated until recently (Table 1). Microarray analyses, next-generation sequencing, and quantitative RT-PCR are important tools in developing biomarkers [15–21, 50, 51, 53, 57, 71, 97, 107, 119–131]. To date, candidate regulatory RNAs are limited to miRNAs. No study has evaluated the feasibility of using lncRNAs or circRNAs as biomarkers in sepsis.
Investigations revealed that the expression level of miR-25, miR-143, miR-146a, miR-15a, miR-16, miR-126, miR-150, miR-223, and 472-5p-iso could differentiate SIRS from sepsis [16–21, 48–51, 107, 132]. However, an independent research group could not detect any difference in miR-223 expression between septic patients and healthy controls [110]. Recently, massive screening using Solexa sequencing has identified nine novel miRNAs which are correlated with sepsis mortality (AUC = 0.681–0.863) [50]. Of note, selective reporting of sensitivity, specificity, and the associated AUC value was common in several included studies. In addition, none of these studies used an external cohort to validate the biomarkers investigated. This reporting bias complicates the analysis of results between studies.
Other miRNAs have been investigated to predict complications associated with sepsis. For instance, miR-122 predicts the development of liver injury in septic patients [70, 126]. miR-574-5p and miR-155 may predict the development of septic shock, immunosuppression and respiratory failure [71, 127, 133, 134].
Clearly, genome-wide profiling of miRNA expression distinguished septic from nonseptic patients. However, prediction of the likelihood of a nonseptic patient developing sepsis may be more clinically relevant to reduce mortality and morbidity in critical care settings.
Therapeutic targets
Although cell and animal models have demonstrated the use of miRNA modulators in combating sepsis, considerable challenges have to be overcome in order to successfully translate these into clinical use. Apparently, the expression of miRNAs is tissue-dependent, questioning the appropriateness of systemic delivery of antagomir or miRNA mimics, as has been commonly performed in animal models. Although targeted drug delivery may be an alternative, this is further complicated by the technology of the delivery and the heterogeneity of clinical manifestations among septic patients.
Recent animal studies have recognized that miRNAs are associated with medical interventions and septic complications [125–138]. In SPRET/Ei mice, glucocorticoid induced miR-511 upregulation, inhibiting the TNF receptor TNFR1 and, hence, reducing their sensitivity to TNF-α [135]. Similarly, administration of dexamethasone in a LPS-induced murine sepsis model downregulated the expression of miR-155 in the liver and alleviated proinflammatory cytokine production [116, 138]. Interestingly, miRNAs are also involved in cortisol nonresponsiveness, which may occur during the therapy. This resistance phenotype is partly related to altered expression of one of the cortisol receptor isoforms, glucocorticoid receptor α. In sepsis patients, this isoform is significantly downregulated by miR-124, which is increased three-fold upon exposure to glucocorticoid [137].
After exposure to LPS for a while, our body switches to tolerance mode, which avoids prolonged proinflammatory response. Silencing transcription and translation of acute inflammatory genes in vitro during LPS tolerance is mediated by various miRNAs [139]. Regulation of this tolerance status can be significantly disrupted by overexpression of miR-146a in cellular models of sepsis [140]. While sepsis-induced differential miRNA expression involves a diversity of miRNA species in multiple organs, modulation of miRNAs in endotoxin tolerance is seen predominantly in macrophages mediated by miR-146a and miR-155 [141, 142]. As in sepsis, in vitro studies suggested that the regulation of miRNA during tolerance involves the TLR-NFkB-cytokine pathways [143–145].
Experimental evidence suggests that alternative therapies in treating sepsis involve modulation of miRNAs. Predominantly, these miRNA species are linked to some, if not all, pathways in innate immunity in cellular [146, 147] and in animal models [148, 149]. One of the well-known anti-inflammatory dietary components is flavonoids. In vitro investigation of a flavonoid, apigenin, revealed that it suppresses LPS-induced miR-155 expression in macrophages, leading to upregulation of the anti-inflammatory regulators forkhead box O3a and MAD-related protein 2 [146]. The protective effect was further elaborated by a murine sepsis model in which an apigenin-rich diet considerably reduced the expression of miR-155 and TNF-α in the lungs [146]. Recent innovations in septic treatment include stem cell therapy. In this regard, in vivo mechanistic studies revealed that mesenchymal stem cells improved survival of CLP-induced septic mice by downregulating miR-143 [147, 150]. Microarray analyses revealed more than 1.5-fold differential expression of 77 miRNAs in septic mice treated with noncultured-derived mesenchymal cells [149]. This was accompanied by a reduced inflammatory response and apoptosis [149]. Elucidating the mechanisms using animal models of sepsis in relation to a 20-HETE analog, N-(20-hydroxyeicosa-5Z,14Z-dienoyl glycine, revealed the involvement of miR-150, miR-223, and miR-297 [148]. Further in vitro studies revealed that these miRNAs were downregulated leading to suppression of the MyB88/NF-κB pathway [151].
Evaluation of the feasibility of miRNA as septic therapy predominantly employs two approaches: use of antagomir or miRNA mimics. Among all miRNAs, miR-146a is the most comprehensively studied candidate. By targeting IRAK1 and TRAF6, miR-146a attenuates cardiac dysfunction in septic mice [152]. Delivering miR-146a agomir by in vivo jetPEITM instillation into airways of septic mice inhibited proinflammatory cytokine production and alleviated lung tissue injury [153]. An independent group of researchers revealed that this miRNA additionally interferes in vitro with Th1 cell differentiation of human CD4+ T lymphocytes via PRKC [154]. Other miRNAs, including miR-124, miR-142-3p, and miR-195, have also been demonstrated to be useful in preventing hyperinflammation, apoptosis, and multiple organ injury in murine sepsis models [8, 140, 155, 156]. Similarly, indirect induction of miR-126 expression in vitro by CTEC-0214, a stromal cell-derived factor 1 alpha analog, preserved endothelial cell barrier integrity and attenuated pulmonary vascular leak [157].
Conclusion
In conclusion, regulatory non-coding RNAs are potential candidates as biomarkers and therapeutics for sepsis. Given organ-specific differentiation of these regulatory non-coding RNAs in addition to the pathological heterogeneity of patients with sepsis, future research is warranted to elucidate the temporal dynamics and cellular origins of regulatory RNAs. Development of organ-specific delivery of non-coding RNA mediators may be a promising approach.
Abbreviations
- ADAM:
-
A disintegrin and metalloproteinase
- AP-1:
-
Activator protein-1
- AUC:
-
Area under the curve
- circRNA:
-
Circular RNA
- CLP:
-
Cecal ligation and puncture
- HMGB1:
-
High mobility group box 1
- IL:
-
Interleukin
- iNOS:
-
Inducible nitric oxide synthase
- IRAK1:
-
Interleukin-1 receptor-associated kinase 1
- lncRNA:
-
Long non-coding RNA
- LPS:
-
Lipopolysaccharide
- MAPK:
-
Mitogen-activated protein kinase
- miRNA:
-
MicroRNA
- MKP-1:
-
MAPK phosphatase 1
- NF:
-
Nuclear factor
- SIRS:
-
systemic inflammatory response syndrome
- SYRCLE:
-
Systematic Review Center for Laboratory Animal Experimentation
- TLR:
-
Toll-like receptor
- TNF:
-
Tumor necrosis factor
References
Angus DC, Van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–51.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10.
Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:762–74.
Xiao W, Mindrinos MN, Seok J, et al. A genomic storm in critically injured humans. J Exp Med. 2011;208:2581–90.
Morris KV, Mattick JS. The rise of regualatory RNA. Nat Rev Genet. 2014;15:423–37.
Brudecki L, Ferguson DA, McCall CE, El Gazzar M. MicroRNA-146a and RBM4 form a negative feed-forward loop that disrupts cytokine mRNA translation following TLR4 responses in human THP-1 monocytes. Immunol Cell Biol. 2013;91:532–40.
Brudecki L, Ferguson DA, McCall CE, El Gazzar M. Mitogen-activated protein kinase phosphatase 1 disrupts proinflammatory protein synthesis in endotoxin-adapted monocytes. Clin Vaccine Immunol. 2013;20:1396–404.
Zheng D, Yu Y, Li M, et al. Inhibition of microRNA 195 prevents apoptosis and multiple-organ injury in mouse models of sepsis. J Infect Dis. 2016;213:1661–70.
Precone V, Stornaiuolo G, Amato A, et al. Different changes in mitochondrial apoptotic pathway in lymphocytes and granulocytes in cirrhotic patients with sepsis. Liver Int. 2013;33:834–42.
Ha M, Kim N. Regulation of microRNA biogenesis. Nat Rev Mol Cell Biol. 2016;15:509–24.
Li Y, Kowdley KV. MicroRNAs in common human diseases. Genomics, Proteomics Bioinformatics. 2012;5:246–53.
Tili E, Michaille JJ, Cimino A, et al. Modulation of miR-155 and miR-125b levels following lipopolysaccharide/TNF-alpha stimulation and their possible roles in regulating the response to endotoxin shock. J Immunol. 2007;179:5082–9.
How CK, Hou SK, Shih HC, et al. Expression profile of MicroRNAs in gram-negative bacterial sepsis. Shock. 2015;43:121–7.
Ho PC, Chang KC, Chuang YS, Wei LN. Cholesterol regulation of receptor interacting protein 140 via microRNA-33 in inflammatory cytokine production. FASEB J. 2011;25:1758–66.
Goodwin AJ, Guo C, Cook JA, et al. Plasma levels of microRNA are altered with the development of shock in human sepsis: an observational study. Crit Care. 2015;19:440.
Ma Y, Vilanova D, Atalar K, et al. Genome-wide sequencing of cellular microRNAs identifies a combinatorial expression signature diagnostic of sepsis. PLoS One. 2013;8, e75918.
Yao L, Liu Z, Zhu J, et al. Clinical evaluation of circulating microRNA-25 level change in sepsis and its potential relationship with oxidative stress. Int J Clin Exp Pathol. 2015;8:7675–84.
Wang H, Zhang P, Chen W, et al. Evidence for serum miR-15a and miR-16 levels as biomarkers that distinguish sepsis from systemic inflammatory response syndrome in human subjects. Clin Chem Lab Med. 2012;50:1423–8.
Wang HJ, Zhang PJ, Chen WJ, et al. Four serum microRNAs identified as diagnostic biomarkers of sepsis. J Trauma Acute Care Surg. 2012;73:850–4.
Huang J, Sun Z, Yan W, et al. Identification of microRNA as sepsis biomarker based on miRNAs regulatory network analysis. Biomed Res Int. 2014;2014:594350.
Wang JF, Yu ML, Yu G, et al. Serum miR-146a and miR-223 as potential new biomarkers for sepsis. Biochem Biophys Res Commun. 2010;394:184–8.
Dey BK, Mueller AC, Dutta A. Long non-coding RNAs as emerging regulators of differentiation, development, and disease. Transcription. 2014;5, e944014.
Wapinski O, Chang HY. Long noncoding RNAs and human disease. Trends Cell Biol. 2011;21:354–61.
Liu Y, Ferguson JF, Xue C, et al. Tissue-specific RNA-Seq in human evoked inflammation identifies blood and adipose LincRNA signatures of cardiometabolic diseases. Arterioscler Thromb Vasc Biol. 2014;34:902–12.
Wu H, Liu J, Li W, Liu G, Li Z. LncRNA-HOTAIR promotes TNF-alpha production in cardiomyocytes of LPS-induced sepsis mice by activating NF-kappaB pathway. Biochem Biophys Res Commun. 2016;471:240–6.
Lin J, Zhang X, Xue C, et al. The long noncoding RNA landscape in hypoxic and inflammatory renal epithelial injury. Am J Physiol Renal Physiol. 2015;309:F901–13.
Singh KK, Matkar PN, Muhammad S, et al. Investigation of novel LPS-induced differentially expressed long non-coding RNAs in endothelial cells. Mol Cell Biochem. 2016;421:157–68.
Cui H, Xie N, Tan Z, et al. The human long noncoding RNA lnc-IL7R regulates the inflammatory response. Eur J Immunol. 2014;44:2085–95.
Chen LL. The biogenesis and emerging roles of circular RNAs. Nat Rev Mol Cell Biol. 2016;17:205–11.
Ng WL, Marinov GK, Liau ES, et al. Inducible RasGEF1B circular RNA is a positive regulator of ICAM-1 in the TLR4/LPS pathway. RNA Biol. 2016;13:861–71.
Hooijmans CR, Rovers MM, de Vries RB, et al. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014;14:43.
Abraham E, Singer M. Mechanisms of sepsis-induced organ dysfunction. Crit Care Med. 2007;35:2408–16.
Kanaan Z, Gardner S, Carruba C, Mattingly J, Druen D, Cheadle WG. Macrophage genetic reprogramming during chronic peritonitis is augmented by LPS pretreatment. J Surg Res. 2012;1175:289–97.
Lederhuber H, Baer K, Altiok I, Sadeghi K, Herkner KR, Kasper DC. MicroRNA-146: tiny player in neonatal innate immunity? Neonatology. 2011;99:51–6.
Liu Y, Cao D, Mo G, Zhang L. Effects of microRNA-294 on inflammatory factor of sepsis by targeting triggering receptor expressed on myeloid cells-1. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2014;26:661–6.
Maier M, Wutzler S, Bauer M, Trendafilov P, Henrich D, Marzi I. Altered gene expression patterns in dendritic cells after severe trauma: implications for systemic inflammation and organ injury. Shock. 2008;30:344–51.
Billeter AT, Hellmann J, Roberts H, et al. MicroRNA-155 potentiates the inflammatory response in hypothermia by suppressing IL-10 production. FASEB J. 2014;28:5322–36.
Schmidt WM, Spiel AO, Jilma B, Wolzt M, Muller M. In vivo profile of the human leukocyte microRNA response to endotoxemia. Biochem Biophys Res Commun. 2009;380:437–41.
Wu SC, Yang JC, Rau CS, et al. Profiling circulating microRNA expression in experimental sepsis using cecal ligation and puncture. PLoS One. 2013;8, e77936.
Hsieh CH, Rau CS, Jeng JC, et al. Whole blood-derived microRNA signatures in mice exposed to lipopolysaccharides. J Biomed Sci. 2012;19:69.
Chen J, Jiang S, Cao Y, Yang Y. Altered miRNAs expression profiles and modulation of immune response genes and proteins during neonatal sepsis. J Clin Immunol. 2014;34:340–8.
Barnett RE, Conklin DJ, Ryan L, et al. Anti-inflammatory effects of miR-21 in the macrophage response to peritonitis. J Leukoc Biol. 2016;99:361–71.
Rossato M, Curtale G, Tamassia N, et al. IL-10-induced microRNA-187 negatively regulates TNF-α, IL-6, and IL-12p40 production in TLR4-stimulated monocytes. Proc Natl Acad Sci U S A. 2012;109:E3101–10.
Sweeney TE, Suliman HB, Hollingsworth JW, Piantadosi CA. Differential regulation of the PGC family of genes in a mouse model of Staphylococcus aureus sepsis. PLoS One. 2010;5, e11606.
Sun X, Icli B, Wara AK, et al. MicroRNA-181b regulates NF-kappaB-mediated vascular inflammation. J Clin Invest. 2012;122:1973–90.
Ma H, Wang X, Ha T, et al: MicroRNA-125b prevents cardiac dysfunction in polymicrobial sepsis by targeting TRAK6 mediated NFkB activation and p53 mediated apoptotic signaling. J Infect Dis. 2016. doi:10.1093/infdis/jiw449
Wang X, Hao L, Bu HF, et al. Spherical nucleic acid targeting microRNA-99b enhances intestinal MFG-E8 gene expression and restores enterocyte migration in lipopolysaccharide-induced septic mice. Sci Rep. 2016;6:31687.
Han Y, Dai QC, Shen HL, et al. Diagnostic value of elevated serum miRNA-143 levels in sepsis. J Int Med Res. 2016;44:875–81.
Moore CC, McKillop IH, Huynh T. MicroRNA expression following activated protein C treatment during septic shock. J Surg Res. 2013;182:116–26.
Wang HJ, Zhang PJ, Chen WJ, et al. Characterization and identification of novel serum microRNAs in sepsis patients with different outcomes. Shock. 2013;39:480–7.
Wang L, Wang HC, Chen C, et al. Differential expression of plasma miR-146a in sepsis patients compared with non-sepsis-SIRS patients. Exp Ther Med. 2013;5:1101–4.
Shao Y, Li J, Cai Y, et al. The functional polymorphisms of miR-146a are associated with susceptibility to severe sepsis in the Chinese population. Mediators Inflamm. 2014;2014:916202.
Wang X, Wang X, Liu X, et al. miR-15a/16 are upregulated in the serum of neonatal sepsis patients and inhibit the LPS-induced inflammatory pathway. Int J Clin Exp Med. 2015;8:5683–90.
Wu Y, Li C, He Y, et al. Relationship between expression of microRNA and inflammatory cytokines plasma level in pediatric patients with sepsis. Zhonghua Er Ke Za Zhi. 2014;52:28–33.
Wang LA, Oakes JL, Burton R, et al. The role of the E2F1 transcription factor in the innate immune response to systemic LPS. Am J Physiol Lung Cell Mol Physiol. 2012;303:L391–400.
Tudor S, Giza DE, Lin HY, et al. Cellular and Kaposi's sarcoma-associated herpes virus microRNAs in sepsis and surgical trauma. Cell Death Dis. 2014;5, e1559.
Zhou J, Chaudhry H, Zhong Y, et al. Dysregulation in microRNA expression in peripheral blood mononuclear cells of sepsis patients is associated with immunopathology. Cytokine. 2015;71:89–100.
Mao AP, Shen J, Zuo Z. Expression and regulation of long noncoding RNAs in TLR4 signaling in mouse macrophages. BMC Genomics. 2015;16:45.
Moon HG, Yang J, Zheng Y, Jin Y. miR-15a/16 regulates macrophage phagocytosis after bacterial infection. J Immunol. 2014;193:4558–67.
Dan C, Jinjun B, Zi-Chun H, et al. Modulation of TNF-α mRNA stability by human antigen R and miR181s in sepsis-induced immunoparalysis. EMBO Mol Med. 2015;7:140–57.
Heyn J, Ledderose C, Hinske LC, et al. Adenosine A2A receptor upregulation in human PMNs is controlled by miRNA-214, miRNA-15, and miRNA-16. Shock. 2012;37:156–63.
Zhou W, Wang J, Li Z, et al. MicroRNA-25-5b inhibits HMGB1 expression in LPS-induced sepsis. Int J Mol Med. 2016;38:312–8.
El Gazzar M, Church A, Liu T, McCall CE. MicroRNA-146a regulates both transcription silencing and translation disruption of TNF-alpha during TLR4-induced gene reprogramming. J Leukoc Biol. 2011;90:509–19.
Zou L, Feng Y, Xu G, Jian W, Chao W. Splenic RNA and microRNA mimics promote complement factor B production and alternative pathway activation via innate immune signaling. J Immunol. 2016;196:2788–98.
Quinn EM, Wang JH, O'Callaghan G, Redmond HP. MicroRNA-146a is upregulated by and negatively regulates TLR2 signaling. PLoS One. 2013;8, e62232.
Guan Y, Yao H, Wang J, Sun K, Cao L, Wang Y. NF-kappaB-DICER-miRs axis regulates TNF-alpha expression in responses to endotoxin stress. Int J Biol Sci. 2015;11:1257–68.
Huang HC, Yu HR, Huang LT, et al. MiRNA-125b regulates TNF-alpha production in CD14+ neonatal monocytes via post-transcriptional regulation. J Leukoc Biol. 2012;92:171–82.
Du L, Rong H, Cheng Y, et al. Identification of microRNAs dysregulated in CD14 gene silencing RAW264.7 macrophage cells. Inflammation. 2014;37:287–94.
Gentile LF, Cuenca AG, Efron PA, et al. Persistent inflammation and immunosuppresion: a common syndrome and new horizon for surgical intensive care. J Trauma Acute Care Surg. 2012;72:1491–501.
Ho J, Yu J, Wong SH, et al. Autophagy in sepsis: degradation into exhaustion? Autophagy. 2016;12:1073–82.
Liu J, Shi K, Chen M, et al. Elevated miR-155 expression induces immunosuppression via CD39(+) regulatory T-cells in sepsis patient. Int J Infect Dis. 2015;40:135–41.
McClure C, Brudecki L, Ferguson DA, et al. MicroRNA 21 (miR-21) and miR-181b couple with NFI-A to generate myeloid-derived suppressor cells and promote immunosuppression in late sepsis. Infect Immun. 2014;82:3816–25.
McClure C, Ali E, Youssef D, Yao ZQ, McCall CE, El Gazzar M. NFI-A disrupts myeloid cell differentiation and maturation in septic mice. J Leukoc Biol. 2016;99:201–11.
van der Heide V, Mohnle P, Rink J, Briegel J, Kreth S. Down-regulation of microRNA-31 in CD4+ T cells contributes to immunosuppression in human sepsis by promoting TH2 skewing. Anesthesiology. 2016;124:908–22.
Li Y, Dalli J, Chiang N, Baron RM, Quintana C, Serhan CN. Plasticity of leukocytic exudates in resolving acute inflammation is regulated by microRNA and proresolving mediators. Immunity. 2013;39:885–98.
Wang Y, Li T, Wu B, et al. STAT1 regulates MD-2 expression in monocytes of sepsis via miR-30a. Inflammation. 2014;37:1903–11.
McClure C, McPeak MB, Youssef D, et al. Stat3 and C/EBPβ synergize to induce miR-21 and miR-181b expression during sepsis. Immunol Cell Biol. 2016. doi:10.1038/icb.2016.63.
Curtis AM, Fagundes CT, Yang G, et al. Circadian control of innate immunity in macrophages by miR-155 targeting Bmal1. Proc Natl Acad Sci U S A. 2015;112:7231–6.
Piccinini AM, Midwood KS. Endogenous control of immunity against infection: tenascin-C regulates TLR4-mediated inflammation via microRNA-155. Cell Rep. 2012;2:914–26.
Monk CE, Hutvagner G, Arthur JS. Regulation of miRNA transcription in macrophages in response to Candida albicans. PLoS One. 2010;5, e13669.
Papurica M, Rogobete AF, Sandesc D et al. The expression of nuclear transcription facor kappa B in the case of critically ill polytrauma patients with sepsis and its interactions with microRNAs. Biochem Genet. 2016;54:337-47.
Jiang Y, Zhou H, Ma D, Chen ZK, Cai X. MicroRNA-19a and CD22 comprise a feedback loop for B cell response in sepsis. Med Sci Monit. 2015;21:1548–55.
Qi J, Qiao Y, Wang P, Li S, Zhao W, Gao C. MicroRNA-210 negatively regulates LPS-induced production of proinflammatory cytokines by targeting NF-κB1 in murine macrophages. FEBS Lett. 2012;586:1201–7.
Song X, Wang CT, Geng XH. MicroRNA-29a promotes apoptosis of monocytes by targeting STAT3 during sepsis. Genet Mol Res. 2015;14:13746–53.
Larkin CM, Santos-Martines MJ, Ryan T, Radomski MW. Sepsis-associated thrombocytopenia. Thromb Res. 2016;141:11–6.
Cui YL, Wang B, Gao HM, et al. Interleukin-18 and miR-130a in severe sepsis patients with thrombocytopenia. Patient Prefer Adherence. 2016;10:313–9.
Wang HJ, Deng J, Wang JY, et al. Serum miR-122 levels are related to coagulation disorders in sepsis patients. Clin Chem Lab Med. 2014;52:927–33.
Zhao H, Anand AR, Ganju RK. Slit2-Robo4 pathway modulates lipopolysaccharide-induced endothelial inflammation and its expression is dysregulated during endotoxemia. J Immunol. 2014;192:385–93.
Chatterjee V, Beard Jr RS, Reynolds JJ, et al. MicroRNA-147b regulates vascular endothelial barrier function by targeting ADAM15 expression. PLoS One. 2014;9, e110286.
Cheng HS, Sivachandran N, Lau A, et al. MicroRNA-146 represses endothelial activation by inhibiting pro-inflammatory pathways. EMBO Mol Med. 2013;5:949–66.
Rajput C, Tauseef M, Farazuddin M, et al. MicroRNA-150 suppression of angiopoetin-2 generation and signaling is crucial for resolving vascular injury. Arterioscler Thromb Vasc Biol. 2016;36:380–8.
Wu M, Gu JT, Yi B, Tang ZZ, Tao GC. MicroRNA-23b regulates the expression of inflammatory factors in vascular endothelial cells during sepsis. Exp Ther Med. 2015;9:1125–32.
Fan H, Goodwin AJ, Chang E, et al. Endothelial progenitor cells and a stromal cell-derived factor-1α analogue synergistically improve survival in sepsis. Am J Respir Crit Care Med. 2014;189:1509–19.
Gajic O, Dabbagh O, Park PK, et al. Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med. 2011;183:462–70.
Eggimann P, Harbarth S, Ricou B et al. Acute respiratory distress syndrome after bacteremic sepsis does not increase mortality. Am J Respir Crit Care Med. 2003;167:1210–4.
Kim WY, Hong SB. Sepsis and acute respiratory distress syndrome: recent update. Tuberc Respir Dis. 2016;79:53–7.
Martin G, Brunkhorst FM, Janes JM, et al. The international PROGRESS registry of patients with severe sepsis: drotrecogin alfa (activated) use and patient outcomes. Crit Care. 2009;13:R103.
Wang Z, Ruan Z, Mao Y, et al. MiR-27a is up regulated and promotes inflammatory response in sepsis. Cell Immunol. 2014;290:190–5.
Liu F, Li Y, Jiang R, et al. MiR-132 inhibits lipopolysaccharide-induced inflammation in alveolar macrophages by the cholinergic anti-inflammatory pathway. Exp Lung Res. 2015;41:261–9.
Ying H, Kang Y, Zhang H, et al. MiR-127 modulates macrophage polarization and promotes lung inflammation and injury by activating the JNK pathway. J Immunol. 2015;194:1239–51.
Adyshev DM, Moldobaeva N, Mapes B, Elangovan V, Garcia JG. MicroRNA regulation of nonmuscle myosin light chain kinase expression in human lung endothelium. Am J Respir Cell Mol Biol. 2013;49:58–66.
Drosatos K, Drosatos-Tampakaki Z, Khan R, et al. Inhibition of c-Jun-N-terminal kinase increases cardiac peroxisome proliferator-activated receptor alpha expression and fatty acid oxidation and prevents lipopolysaccharide-induced heart dysfunction. J Biol Chem. 2011;286:36331–9.
Sun B, Hu X, Liu G, et al. Phosphatase Wip1 negatively regulates neutrophil migration and inflammation. J Immunol. 2014;192:1184–95.
Ding T, Li Y, Tang R, et al. Differential expression of miRNAs in myocardial tissues of rats with lipopolysaccharide-induced endotoxemia. Nan Fang Yi Ke Da Xue Xue Bao. 2015;35:213–7.
Essandoh K, Li Y, Huo J, Fan GC. MiRNA-mediated macrophage polarization and its potential role in the regulation of inflammatory response. Shock. 2016;46:122-31.
Flierl MA, Rittirsch D, Huber-Lang MS. Molecular events in the cardiomyopathy of sepsis. Mol Med. 2008;14:327.
Vasilescu C, Rossi S, Shimizu M, et al. MicroRNA fingerprints identify miR-150 as a plasma prognostic marker in patients with sepsis. PLoS One. 2009;4, e7405.
Wang X, Huang W, Yang Y, et al. Loss of duplex miR-223 (5p and 3p) aggravates myocardial depression and mortality in polymicrobial sepsis. Biochem Biophysica Acta. 2014;1842:701–11.
Xue WL, Bai X, Zhang L. rhTNFR:Fc increases Nrf2 expression via miR-27a mediation to protect myocardium against sepsis injury. Biochem Biophys Res Commun. 2015;464:855–61.
Wang H, Bei Y, Shen S, et al. Mir-21-3p controls sepsis associated cardiac dysfunction via regulating SORBS2. J Mol Cell Cardiol. 2016;94:43–53.
Jia Z, Wang J, Shi Q, et al. SOX6 and PDCD4 enhance cardiomyocyte apoptosis through LPS-induced miR-499 inhibition. Apoptosis. 2016;21:174–83.
Risoe PK, Ryg U, Wang YY, et al. Cecal ligation and puncture sepsis is associated with attenuated expression of adenylyl cyclase 9 and increased miR142-3p. Shock. 2011;36:390–5.
Wang ZH, Liang YB, Tang H, et al. Expression and effects of microRNA-155 in the livers of septic mice. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2012;24:154–7.
Jia P, Teng J, Zou J, et al. Xenon protects against septic acute kidney injury via miR-21 target signaling pathway. Crit Care Med. 2015;43:e250–9.
Li XY, Zhang K, Jiang ZY, Cai LH. MiR-204/miR-211 downregulation contributes to candidemia-induced kidney injuries via derepression of Hmx1 expression. Life Sci. 2014;102:139–44.
Wang X, Zhao Q, Matta R, et al. Inducible nitric oxide synthase expression is regulated by mitogen-activated protein kinase phosphatase-1. J Biol Chem. 2009;284:27123–34.
Zhang J, Fu SL, Liu Y, Liu YL, Wang WJ. Analysis of microRNA expression profiles in weaned pig skeletal muscle after lipopolysaccharide challenge. Int J Mol Sci. 2015;16:22438–55.
Fredrisksson K, Tjader I, Keller P, et al. Dysregulation of mitochondrial dynamics and the muscle transcriptome in ICU patients suffering from sepsis induced multiple organ failure. PLoS One. 2008;3, e3686.
Zhang AQ, Gu W, Zeng L, et al. Genetic variants of microRNA sequences and susceptibility to sepsis in patients with major blunt trauma. Ann Surg. 2015;261:189–96.
Roderburg C, Benz F, Vargas Cardenas D, et al. Elevated miR-122 serum levels are an independent marker of liver injury in inflammatory diseases. Liver Int. 2015;35:1172–84.
Barnett RE, Keskey RC, Rao JM, et al. Poor outcome in bacterial peritonitis is associated with dysregulated microRNAs and an increased inflammatory response. Surgery. 2013;154:521–7.
Wang H, Zhang P, Chen W, Feng D, Jia Y, Xie L. Serum microRNA signatures identified by Solexa sequencing predict sepsis patients’ mortality: a prospective observational study. PLoS One. 2012;7, e38885.
Roderburg C, Luedde M, Vargas Cardenas D, et al. Circulating microRNA-150 serum levels predict survival in patients with critical illness and sepsis. PLoS One. 2013;8, e54612.
Tacke F, Roderburg C, Benz F, et al. Levels of circulating miR-133a are elevated in sepsis and predict mortality in critically ill patients. Crit Care Med. 2014;42:1096–104.
Benz F, Tacke F, Luedde M, et al. Circulating microRNA-223 serum levels do not predict sepsis or survival in patients with critical illness. Dis Markers. 2015;2015:384208.
Leelahavanichkul A, Somparn P, Panich T, et al. Serum miRNA-122 in acute liver injury induced by kidney injury and sepsis in CD-1 mouse models. Hepatol Res. 2015;45:1341–52.
Wang H, Meng K, Chen W, Feng D, Jia Y, Xie L. Serum miR-574-5p: a prognostic predictor of sepsis patients. Shock. 2012;37:263–7.
Schlosser K, McIntyre LA, White RJ, Stewart DJ. Customized internal reference controls for improved assessement of circulating microRNAs in disease. PLoS One. 2015;10, e0127443.
Wang HJ, Wang BZ, Zhang PJ, et al. Identification of four novel serum protein biomarkers in sepsis encoded by target genes of sepsis-related miRNAs. Clin Sci (Lond). 2014;126:857–67.
Wang H, Yu B, Deng J, Jin Y, Xie L. Serum miR-122 correlates with short term mortality in sepsis patients. Crit Care. 2014;18:704.
Yang WH, Wu HY, Zhang HZ, Liu HX, Wei YJ, Shi B. Prognostic value of Picco monitoring combined with plasma microRNA-150 detection in septic shock patients. Zhejiang Da Xue Bao Yi Xue Ban. 2015;44:659–64.
Caserta S, Kern F, Cohen J, et al. Circulating plasma microRNAs can differentiate human sepsis and systemic inflammatory response syndrome (SIRS). Sci Rep. 2016;6:28006.
Wang Q, Zhao C, Cai Q, Zhu H. Expression of microRNA-155 and regulative T cell in sepsis patients and their relationship. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2014;26:179–83.
Liu S, Liu C, Wang Z, Huang J, Zeng Q. MicroRNA-23a-5p acts as a potential biomarker for sepsis-induced acute respiratory distress syndrome in early stage. Cell Mol Biol. 2016;62:31–7.
Puimege L, Van Hauwermeiren F, Steeland S, et al. Glucocorticoid-induced microRNA-511 protects against TNF by down-regulating TNFR1. EMBO Mol Med. 2015;7:1004–17.
Acosta-Herrera M, Lorenzo-Diaz F, Pino-Yanes M, et al. Lung transcriptomics during protective ventilatory support in sepsis-induced acute lung injury. PLoS One. 2015;10, e0132296.
Ledderose C, Mohnle P, Limbeck E, et al. Corticosteroid resistance in sepsis is influenced by microRNA-124-induced downregulation of glucocorticoid receptor-alpha. Crit Care Med. 2012;40:2745–53.
Wang ZH, Liang YB, Tang H, et al. Dexamethasone down-regulates the expression of microRNA-155 in the livers of septic mice. PLoS One. 2013;8, e80547.
El Gazzar M, McGall CE. MicroRNAs distinguish translational from transcriptinal silencing during endotoxin tolerance. J Biol Chem. 2010;285:20940–51.
Banerjee S, Meng J, Das S, et al. Morphine induced exacerbation of sepsis is mediated by tempering endotoxin tolerance through modulation of miR-146a. Sci Rep. 2013;3:1977.
Nahid MA, Pauley KM, Satoh M, et al. miR-146a is critical for endotoxin-induced tolerance: implication in innate immunity. J Biol Chem. 2009;284:34590–9.
Doxaki C, Kampranis SC, Eliopoulos AG, et al. Coordinated regulation of miR-155 and miR-146a genes during induction of endotoxin tolerance in Macrophages. J Immunol. 2015;195:5750–61.
Androulidaki A, Iliopoulos D, Arranz A, et al. The kinase Akt1 controls macrophage response to lipopolysaccharide by regulating microRNAs. Immunity. 2009;31:220–31.
Nahid MA, Satoh M, Chan EK. Interleukin 1beta-responsive microRNA-146a is critical for the cytokine-induced tolerance and cross-tolerance to toll-like receptor ligands. J Innate Immun. 2015;7:428–40.
Dai Y, Jia P, Fang Y, et al. miR-146a is essential for lipopolysaccharide (LPS)-induced cross-tolerance against kidney ischemia/reperfusion injury in mice. Sci Rep. 2016;6:27091.
Arango D, Diosa-Toro M, Rojas-Hernandez LS, et al. Dietary apigenin reduces LPS-induced expression of miR-155 restoring immune balance during inflammation. Mol Nutr Food Res. 2015;59:763–72.
Zhao X, Liu D, Gong W, et al. The toll-like receptor 3 ligand, poly(I:C), improves immunosuppressive function and therapeutic effect of mesenchymal stem cells on sepsis via inhibiting miR-143. Stem cells. 2014;32:521–33.
Sari AN, Korkmaz B, Serin MS, et al. Effects of 5,14-HEDGE, a 20-HETE mimetic, on lipopolysaccharide-induced changes in MyD88/TAK1/IKKβ/IκB-α/NF-κB pathway and circulating miR-150, miR-223, and miR-297 levels in a rat model of septic shock. Inflamm Res. 2014;63:741–56.
Wang Y, Tan L, Jin J, et al. Non-cultured dermal-derived mesenchymal cells attenuate sepsis induced by cecal ligation and puncture in mice. Sci Rep. 2015;5:16973.
Ho MS, Mei SH, Stewart DJ. The immunomodulatory and therapeutic effects of mesenchymal stromal cells for acute lung injury and sepsis. J Cell Physiol. 2015;230:2606–17.
Shukla K, Sharma AK, Ward A, et al. Micro RNA-30c-2-3p negatively regulates NFκB signaling and cell cycle progression through downregulation of TRADD and CCNE1 in breast cancer. Mol Oncol. 2015;9:1106–19.
Gao M, Wang X, Zhang X, et al. Attenuation of cardiac dysfunction in polymicrobial sepsis by microRNA-146a is mediated via targeting of IRAK1 and TRAF6 expression. J Immunol. 2015;195:672–82.
Zhang J, Ding C, Shao Q, et al. The protective effects of transfected microRNA-146a on mice with sepsis induced acute lung injury in vivo. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2015;27:591–4.
Mohnle P, Schutz SV, van der Heide V, et al. MicroRNA-146a controls Th1-cell differentiation of human CD4+ T lymphocytes by targeting PRKCε. Eur J Immunol. 2015;45:260–72.
Sun Y, Li Q, Gui H, et al. MicroRNA-124 mediates the cholinergic anti-inflammatory action through inhibiting the production of pro-inflammatory cytokines. Cell Res. 2013;23:1270–83.
Zhao G, Su Z, Song D, et al. The long non-coding RNA MALAT1 regulates the lipopolysaccharide-induced inflammatory response through its interaction with NF-kB. FEBS Lett. 2016;590:2884–95.
Guo C, Goodwin AJ, Buie JN, et al. A stromal cell-derived factor 1 alpha analogue improves endothelial cell function in lipopolysaccharide-induced acute respiratory distress syndrome. Mol Med. 2016. doi:10.2119/molmed.2015.00240.
Funding
This work was supported by the Hong Kong Research Grant Council-General Research Fund (464212, 24115815) and the Food and Health Bureau-Commissioned Research on Control of Infectious Diseases (CU-15-B2) and Health and Medical Research Fund (15140132).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding authors on reasonable request.
Authors’ contributions
JH and HC performed the data abstraction. JH wrote the manuscript. WW, MC, and HW critically reviewed the manuscript. All authors assisted in editing the manuscript and approved the final version to be published, and agree to be accountable for all aspect of the work.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding authors
Additional file
Additional file 1: Table S1.
a Summary of the included studies. b Quality assessment of the included studies according to SYRCLE score. (DOCX 73 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ho, J., Chan, H., Wong, S.H. et al. The involvement of regulatory non-coding RNAs in sepsis: a systematic review. Crit Care 20, 383 (2016). https://doi.org/10.1186/s13054-016-1555-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-016-1555-3