Abstract
Purpose
Liposomal bupivacaine demonstrated promise decreasing postoperative pain in total hip and total knee arthroplasty (THA/TKA). Some randomized trials have shown non-superior results; however, confounding variables were not accounted for in such analyses. This study attempts to determine risk factors associated with failure of pain management in patients receiving liposomal bupivacaine.
Methods
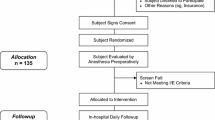
Postoperative pain scores were collected following primary or revision arthroplasties between January 2016 and December 2017. Retrospective analysis of institutional total joint quality and outcomes registry was screened and patients undergoing primary or revision arthroplasties who completed a multi-modal pain management including liposomal bupivacaine were included in the study. Patients with a history of infection/deviated from the institutional pain management protocol were excluded.
Results
A total of 237 patients were included for analysis. Younger patients less than 64 years old had significantly higher pain scores between 0 and 12 h and > 24 h. Active smokers had significantly higher pain scores between 0 and 6 h and > 24 h. Patients with a history of opioid use/pain management had significantly higher pain scores at 6-12 h and 24-48 h. Regression analysis indicated risk factors for resistance to liposomal bupivacaine are younger patients less than 64 years old, those undergoing primary THA, and patients with a history of smoking/pain management/opioid use.
Conclusion
We identify risk factors for resistance to liposomal bupivacaine, which include younger age less than 64 years old, history of smoking/pain management/opioid use. Future studies should use these risk factors as exclusion criteria when using liposomal bupivacaine or initiating any randomized trials regarding efficacy.
Similar content being viewed by others
Introduction
Control of postoperative pain in the setting of primary total hip and total knee arthroplasty (THA/TKA) is critical for successful outcomes leading to quicker recovery, reduced readmission rates, and lower treatment costs [1]. Currently, multi-modal pain protocols are the standard for postoperative pain control following THA/TKA [2,3,4,5]. Recently, liposomal bupivacaine gained popularity due to its extended release and initial, promising results [6]. However, not long after popularity grew, a few randomized trials reported data noting non-superior results when comparing liposomal bupivacaine to other pain modalities (within an operating multi-modal pain protocol) [7,8,9,10].
While most of the bias was removed with these level 1 trials, these studies, along with its predecessors, do not include subset analyses that may provide more insight into pain control failure [11]. In this observational regression analysis, a single-surgeon, consecutive cohort is analyzed to identify any significant risk factors for liposomal bupivacaine resistance.
Methods
Institutional Review Board (IRB) approval, study number 20171537, was obtained to collect patient outcome data following THA and TKA at our institution. A single surgeon, consecutive cohort of 286 consecutive patients undergoing either THA or TKA between January 2016 and December 2017 were retrospectively reviewed. Retrospective analysis of institutional total joint quality and outcomes registry was screened for inclusion. Inclusion criteria consisted of any patient undergoing primary or revision arthroplasties with completed multi-modal pain management strategy and received liposomal bupivacaine (Table 1). Exclusion criteria were those undergoing any THA or TKA in the setting or past history of infection or those who were unable to receive liposomal bupivacaine (i.e. allergy).
The standardized pain management protocol included a multi-modal approach focusing on both preoperative and postoperative pain control (Table 1). As part of a multimodal pain control regimen, liposomal bupivacaine was administered after final implants were placed prior to closure. Twenty cc of liposomal bupivacaine was diluted with 40 cc of normal saline for a total administration dose of 60 cc. Another injection is given within the surgical site consisting of 0.5% bupivacaine, morphine, and ketorolac. A 30 cc mixture of equal parts bupivacaine, morphine, and ketorolac were injected systematically into the periosteum, joint capsule, and subcutaneous tissue using an 18-guage needle. The determination of which patients would receive blocks and/or patient controlled analgesia (PCA) were at the discretion of the surgeon and anesthesiologist taking care of the patient.
As per institutional standard post-anesthesia care unit (PACU) and orthopaedic floor nursing protocol, pain scores were assessed and recorded via the Wong-Baker Visual Analog scale (VAS). Timepoints included times at 2, 4, 6, 8, 12, 24, and 48 h post-operatively.
Statistical analysis
Frequencies and proportions of categorical patient demographic and surgical variables are reported. Means and standard deviations (SD) of continuous patient demographics and pain score variables are reported. To test for differences in demographic and surgical variables based on pain failure at 0–6, 6–12, 12–24, and 24–48 h time intervals, chi-square tests were calculated for categorical variables and one-way ANOVA tests were calculated for continuous variables. Fischer-Exact tests were used in place of chi-square tests to obtain p-values where > 25% of cells have expected counts < 5. The main outcome measured was highest pain score (0–10) recorded within a 48 h window post-op. The relationship between patient demographics and surgical variables with highest post-op pain score was assessed with absolute differences (AD) and 95% confidence intervals (95% CI) using bivariate and multivariable linear regression analysis. Variables with a p-value < 0.05 from the bivariate analysis were included in the multivariable model. A p-value of < 0.05 was considered to be statistically significant in all calculations. All statistical analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
A total of 237 patients were included in the cohort for analysis. The average age at surgery was 62.8 years, average BMI was 32.4 kg/m2, and 155 (68.6%) patients were female. Surgery was performed in the right lower extremity in 133 (58.3%) patients with a primary total knee making up a majority of the procedures (54.7%), followed by primary total hip (29.6%), then revision total knee (8.1%), revision total hip (6.7%) and bilateral knee (0.9%). A majority of patients did not receive PCA (78.7%). Spinal/epidural blocks were administered to 26 (11.3%) patients, femoral/intraarticular blocks to 11 (4.8%) patients, and 193 (83.9%) received no blocks. A total of 47 (21.0%) of patients were current/former smokers, and 42 (18.7%) used alcohol. Patients with a history of pain management made up 41.8% of the population, and 42.5% of patients took pain medication at home (31% opioids, 4.0% Neurontin/Lyrica, 7.5% other). A total of 21 (9.3%) of patients were taking steroids and 23 (10.1%) taking antidepressants at the time of surgery. Diabetics made up 29.7% of the population (Table 2).
Demographic and surgical characteristics of patients who experienced pain failure at 0-6 h, 6-12 h, 12-24 h, and 24-48 h intervals post-Op
Pain scores were measured at 0–6 h, 6–12 h, 12–24 h, and 24–48 h intervals post-op and recorded as the highest pain score within that time interval. A pain score of ≥5 was considered to be pain failure while a pain score < 5 was considered to be adequately controlled pain. A total of 91 (38.4%) patients experienced pain failure at 0–6 h post-op, 65 (35.7%) patients at 6–12 h post-op, 147 (71.4%) patients at 12–24 h post-op, and 171 (79.5%) patients at 24–48 h post-op. Mean highest pain score was 1.8 ± 1.8 in the PACU, 4.3 ± 3.1 at 0–6 h post-op, 4.2 ± 3.1 at 6–12 h post-op, 6.4 ± 2.8 at 12–24 h post-op, and 6.8 ± 2.6 at 24–48 h post-op. Overall, within the first 48 h post-op, mean highest pain score was 7.5 ± 2.2 and a total of 205 (86.5%) of patients experienced pain failure at least once (Table 3).
Overall, younger patients less than 64 years old, smokers, and patients with a history of pain management had a higher rate of pain failure within the first 48 h post-op (Table 2). Patients who were younger than 64 years old at the time of surgery had a higher proportion of pain failure at 0–6 h (60.0 yrs. vs. 64.6 yrs.; p = 0.002), 6–12 h (63.5 yrs. vs. 71.1 yrs.; p = 0.004), and 24–48 h (61.8 yrs. vs. 66.5 yrs.; p = 0.01) intervals. Among patients with a history of pain management, a higher proportion of patients had pain failure at 6–12 h (61.3% pain score ≥ 5 vs. 33.3% pain score < 5; p-value = 0.0003) and 24–48 h (48.2% pain score ≥ 5 vs. 26.2% pain score < 5; p = value = 0.01) intervals. A higher proportion of pain failure was also observed in patients who were on opioid pain medication at home at 6–12 h (50.8% pain score ≥ 5 vs. 23.7% pain score < 5; p-value = 0.001) and 24–48 h (38.2% pain score ≥ 5 vs. 11.9% pain score < 5; p-value = 0.004) intervals. Patients who were not on any pain medication at home were less likely to experience pain failure at 6–12 h (66.7% pain score < 5 vs. 38.1% pain score ≥ 5; p-value = 0.001) and 24–48 h (73.8% pain score < 5 vs. 50.9% pain score ≥ 5; p-value = 0.004) intervals. A higher proportion of smokers experienced pain failure within the first 0-6 h postop (28.2% pain score ≥ 5 vs. 16.6% pain score < 5; p-value = 0.04) and patients who received PCA after surgery experienced a higher rate of pain failure 12–24 h after surgery (83.3% pain score ≥ 5 vs. 69.1% pain score < 5; p-value = 0.03). Gender, BMI, side of surgery, type of surgery, type of block received, alcohol usage, steroid usage, antidepressant usage, and prior diagnosis of diabetes were not significantly associated with pain failure at any time interval 0-48 h after surgery (p-value> 0.05) (Table 2).
Bivariate and multivariable linear regression of highest pain score recorded within 48 h post-Op
Linear regression models were constructed with the highest pain score recorded within the first 48 h post-op as the main outcome measure (Table 4). In bivariate analysis, older patients over 64 years old had lower pain score (AD -0.05; 95% CI -0.07, 0.02) and patients with a higher BMI had a higher pain score (AD 0.03; 95% CI 0.01, 0.05). Primary THA was associated with a lower pain score compared to primary TKA (AD -0.83; 95% CI -1.48, − 0.19) and patients who received PCA after surgery had a higher pain score compared to those who did not (AD 0.70; 95% CI 0.01, 1.39). Patients who had a history of pain management had a higher pain score compared to those who had no history of pain management (AD 0.69; 95% CI 0.12, 1.27) and patients who used opioid pain medications at home had a higher pain score by 1 point compared to those who did not use any pain medications at home (AD 0.97; 95% CI 0.34, 1.59) (Table 3). Patients who underwent spinal nerve blocks were not found to have statistically significant better pain control when compared to those who had general anesthesia (AD 0.69; 95% CI -0.20, 1.59). Similar results were found when peripheral nerve blocks were compared with those patients who underwent general anesthesia (AD 0.94; 95% CI -0.39, 2.27).
In multivariable analysis, age and primary total hip procedure were both negatively associated with higher pain scores. Older patients greater than 64 years old scored lower on pain compared to younger patients (AD -0.05; 95% CI -0.07, − 0.02) and primary total hip procedure was associated with a lower pain score by greater than 1 point compared to primary total knee procedure (AD -1.03; 95% CI -1.68, − 0.38) (Table 4).
Discussion
Multi-modal pain protocols following THA/TKA have become the standard of care [2,3,4,5]. Oral medications, with or without the use of regional and local anesthesia make up a plethora of pain regimens, and recently liposomal bupivacaine became an important component allowing for improved pain relief for up to 72 h [12]. Several studies reported lower pain scores as the benefits of extended release bupivacaine exhibited promising results [12,13,14,15,16]. However, as usage grew, results of several randomized trials, made even devoted users skeptical as the data exhibited non-superior results when compared to other modalities [7,8,9,10]. As a result, many orthopaedic surgeons have moved away from use of liposomal bupivacaine citing high cost for no presumed benefit [9]. To our knowledge, however, none of these studies performed sub-cohort analyses to determine if any risk factors for liposomal bupivacaine resistance (LBR); anecdotally (and exhibited in the literature), some patients do experience a clear benefit, and this formulates the base hypothesis for this study.
Our current study investigated the efficacy of pain control after liposomal bupivacaine injection following TKA/THA at various time intervals in order to ascertain risk factors leading to resistance of liposomal bupivacaine. Results from our study demonstrated that a total of 86% of the 237 patients included had pain failure at least once during the first 48 h. Not surprisingly, smokers, younger patients less than 64 years old, and patients with prior opioid use, experienced significantly higher rates of pain failure at various time intervals (Table 2) [17,18,19,20]. Previous literature has demonstrated that older patients tend to use less opioids than younger patients which may result from changes in metabolism and clearance of opioid drugs with increased age [17,18,19]. Recent literature on how age influences post operative pain following TKA or THA is contradictory and has demonstrated no difference in pain in some studies, while others show younger patients have more pain [21, 22]. In addition, prior studies have demonstrated that smoking has been associated with high pain scores when compared with non-smoker counterparts [20]. Smoking has shown associated with changes in levels of neuropeptides that play a role in chronic pain, and patients who smoke typically have lower plasma beta-endorphin levels [23, 24]. Lastly, the induction of cytochrome P-450 isoenzymes by tobacco smoke can increase the metabolism of opioids thus leading to inadequate pain control [25, 26].
This study does have some limitations. Power calculation at 0.80 and alpha of 0.05, yielded a R-squared coefficient of 87.5% indicating significance for the regression analysis performed. At a power of 0.90, however, R-squared coefficient fell to 52.3%, offering a less reliable significance at a higher power. However, with a significant R-squared at a power of 0.80, the authors considered the statistical significance appropriately interpreted for the conclusions found in this study. Another limitation of this study is a lack of control group. When examining our data, we found that our baseline pain scores were in line with historical controls; therefore, a control group was assessed. In addition, retrospective analysis of a registry may have led to potential inherent bias; however, the goal of this study was not to demonstrate superiority but rather identify risk factors for failure of pain management with liposomal bupivacaine. Lastly, there were select patients who were provided with PCA, regional block, or spinal anesthesia, which may influence pain scores for patients receiving liposomal bupivacaine, but this was also taken into consideration in our statistical analysis.
Conclusion
Liposomal bupivacaine has been shown to be efficacious in pain control management following primary and revision arthroplasties. However, our study demonstrated that younger age less than 64, and a history of smoking, pain management, and opioid use, led to failed pain management after use of liposomal bupivacaine as part of a multi-modal pain regimen. Future studies should use these criteria as exclusion criteria when using liposomal bupivacaine or initiating any randomized trials regarding efficacy.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AD:
-
Absolute Difference
- BMI:
-
Body Mass Index
- CI:
-
Confidence Interval
- IRB:
-
Institutional Review Board
- LBR:
-
Liposomal Bupivacaine Resistance
- PACU:
-
Post-Anesthesia Care Unit
- PCA:
-
Patient Controlled Analgesia
- SD:
-
Standard Deviation
- THA:
-
Total Hip Arthroplasty
- TKA:
-
Total Knee Arthroplasty
- VAS:
-
Visual Analogue Scale
References
Rutherford RW, Jennings JM, Dennis DA. Enhancing recovery after Total knee Arthroplasty. Orthop Clin North Am. 2017;48(4):391–400.
Lamplot JD, Wagner ER, Manning DW. Multimodal pain management in total knee arthroplasty: a prospective randomized controlled trial. J Arthroplast. 2014;29(2):329–34.
Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic center. Clin Orthop Relat Res. 2009;467(6):1418–23.
Parvizi J, Miller AG, Gandhi K. Multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am. 2011;93(11):1075–84.
Ranawat AS, Ranawat CS. Pain management and accelerated rehabilitation for total hip and total knee arthroplasty. J Arthroplast. 2007;22(7 Suppl 3):12–5.
Branney J, Izadpanah M. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Nurs Stand. 2017;31(33):42–3.
Bagsby DT, Ireland PH, Meneghini RM. Liposomal bupivacaine versus traditional periarticular injection for pain control after total knee arthroplasty. J Arthroplast. 2014;29(8):1687–90.
Perets I, Walsh JP, Mu BH, et al. Intraoperative infiltration of liposomal bupivacaine vs bupivacaine hydrochloride for pain Management in Primary Total hip Arthroplasty: a prospective randomized trial. J Arthroplast. 2018;33(2):441–6.
Schroer WC, Diesfeld PG, Lemarr AR, Morton DJ, Reedy ME. Does extended-release liposomal bupivacaine better control pain than bupivacaine after Total knee Arthroplasty (TKA)? A prospective, Randomized Clinical Trial. J Arthroplasty. 2015;30(9 Suppl):64–7.
Zhao B, Ma X, Zhang J, Ma J, Cao Q. The efficacy of local liposomal bupivacaine infiltration on pain and recovery after Total joint Arthroplasty: a systematic review and meta-analysis of randomized controlled trials. Medicine. 2019;98(3):e14092.
Yu ZX, Yang ZZ, Yao LL. Effectiveness of liposome bupivacaine for postoperative pain control in total knee arthroplasty: a PRISMA-compliant meta-analysis of randomized controlled trials. Medicine. 2018;97(13):e0171.
Dasta J, Ramamoorthy S, Patou G, Sinatra R. Bupivacaine liposome injectable suspension compared with bupivacaine HCl for the reduction of opioid burden in the postsurgical setting. Curr Med Res Opin. 2012;28(10):1609–15.
Asche CV, Ren J, Kim M, Gordon K, McWhirter M, Kirkness CS, Maurer B. Local infiltration for postsurgical analgesia following total hip arthroplasty: a comparison of liposomal bupivacaine to traditional bupivacaine. Curr Med Res Opin. 2017;33(7):1283–90.
Barrington JW, Olugbode O, Lovald S, Ong K, Watson H, Emerson RH. Liposomal bupivacaine: a comparative study of more than 1000 Total joint Arthroplasty cases. Orthop Clin North Am. 2015;46(4):469–77.
Bramlett K, Onel E, Viscusi ER, Jones K. A randomized, double-blind, dose-ranging study comparing wound infiltration of DepoFoam bupivacaine, an extended-release liposomal bupivacaine, to bupivacaine HCl for postsurgical analgesia in total knee arthroplasty. Knee. 2012;19(5):530–6.
Wu ZQ, Min JK, Wang D, Yuan YJ, Li H. Liposome bupivacaine for pain control after total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2016;11(1):84.
Bellville JW, Forrest WH, Miller E, Brown BW. Influence of age on pain relief from analgesics. JAMA. 1971;217:1835–41.
Kaiko RF. Age and morphine analgesia in cancer patients with postoperative pain. Clin Pharmacol Ther. 1980;28(6):823–6.
Macintyre PE, Jarvis DA. Age is the best predictor of postoperative morphine requirements. Pain. 1996;64:357–64.
Weingarten TN, Moeschler SM, Ptaszynski AE, Hooten WM, Beebe TJ, Warner DO. An assessment of the association between smoking status, pain intensity, and functional interference in patients with chronic pain. Pain Physician. 2008;11(5):643–53.
Kennedy JW, Johnston L, Cochrane L, Boscainos PJ. Total knee arthroplasty in the elderly: does age affect pain, function or complications? Clin Orthop Relat Res. 2013;471(6):1964–9.
Singh JA, Gabriel S, Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008;466(11):2717–23.
del Arbol JL, Muñoz JR, Ojeda L, Cascales AL, Irles JR, Miranda MT, Ruiz Requena ME, Aguirre JC. Plasma concentrations of beta-endorphin in smokers who consume different numbers of cigarettes per day. Pharmacol Biochem Behav. 2000;67:25–8.
Girdler SS, Maixner W, Naftel HA, Stewart PW, Moretz RL, Light KC. Cigarette smoking, stress-induced analgesia and pain perception in men and women. Pain. 2005;114(3):372–85.
Ackerman WE III, Ahmad M. Effect of cigarette smoking on serum hydrocodone levels in chronic pain patients. J Ark Med Soc. 2007;104:19–21.
Kroon LA. Drug interactions with smoking. Am J Health Syst Pharm. 2007;64(18):1917–21.
Acknowledgements
Not applicable.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
SB- study design, literature search, data analysis, manuscript draft. AG- study design, literature search, data analysis, manuscript draft. LI- data/statistical analysis, data interpretation. AV-data collection. SE- data collection. DK- manuscript draft. RY- study design, execution, data interpretation/analysis, manuscript fixation. FL- study design, execution, data interpretation/analysis, manuscript fixation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Due to the retrospective nature of this study, the requirement of written informed consent was waived by the institutional IRB.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Buzin, S., Gianakos, A.L., Li, D. et al. Risk factors for liposomal bupivacaine resistance after total hip or knee arthroplasties: a retrospective observational cohort in 237 patients. Patient Saf Surg 14, 6 (2020). https://doi.org/10.1186/s13037-020-0230-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13037-020-0230-4