Abstract
Background
Surgical site infection is a common complication in women undergoing Caesarean section and the second most common cause of maternal mortality in obstetrics. In Ethiopia, prevalence and root causes of surgical site infection post-Caesarean section are highly variable. This systematic review and meta-analysis estimate the overall prevalence of surgical site infection and its root causes among women undergoing Caesarean section in Ethiopia.
Method
Systematic review and meta-analysis were conducted to assess the prevalence and root causes of surgical site infection in Ethiopia. The articles were searched from the databases such as Medline, Google Scholar and Science Direct. A total of 13 studies from different regions of Ethiopia reporting the prevalence and root causes of surgical site infection among women undergoing Caesarean section were included. A random effect meta-analysis model was computed to estimate the overall prevalence. In addition, the association between risk factor variables and surgical site infection related to Caesarean section were examined.
Results
Thirteen studies in Ethiopia showed that the overall prevalence of surgical site infection among women undergoing Caesarean section was 8.81% (95% CI: 6.34–11.28). Prolonged labor, prolonged rupture of membrane, presence of anemia, presence of chorioamnionitis, presence of meconium, vertical skin incision, greater than 2 cm thickness of subcutaneous tissue, and general anesthesia were significantly associated with surgical site infection post-Caesarean section.
Conclusion
Prevalence of surgical site infection among women undergoing Caesarean section was relatively higher in Ethiopians compared with the report of center of disease control guideline. Prolonged labor, prolonged rupture of membrane, presence of anemia, chorioamnionitis, presence of meconium, vertical skin incision, greater than 2 cm thickness of subcutaneous tissue and/or general anesthesia were significantly associated with surgical site infection post-Caesarean section.
Similar content being viewed by others
Background
Caesarean section (C/S) is a surgical practice where a neonate is born via an incision through both the abdominal wall and uterus. It is the most frequent surgical procedure in obstetrics, occurring in approximately 15% of all deliveries, but ranges from approximately 3.5% across the African continent to 29.2% in Latin America [1].
While surgery is an essential element in health care, infections and complications following surgery contribute to maternal morbidity and mortality. Surgical site infections (SSIs) are those infections which are confined to the incisions and/or involve structures adjacent to the wounds that were exposed during surgery [2]. A C/S related SSI was previously defined operationally as an infection involving the abdominal incision or the uterus [3, 4]; however, more recently it has expanded to any infection occurring within 30 days post-surgery involving either the incision or deep tissue at the site [5, 6].
SSIs in obstetrics is the second most common cause of maternal mortality next to postpartum hemorrhage [7]. These events are one of the most common nosocomial infections accounting for 14–16% of the inpatient infections [8] and 20–25% of all hospital-acquired infections worldwide [9]. Women undergoing Caesarean deliveries have a 5 to 20-fold greater chance of getting an infection compared with women who give birth vaginally. These SSIs post-Caesarean birth can occur in the pelvic organs, around the surgical incision, and sometimes the uterine wall [10]. In addition, maternal morbidity related to infections post-C/S is eight times higher than post-vaginal delivery [11].
In Ethiopia, previous studies reported a 14.8–59% prevalence of hospital acquired infections [12,13,14,15];and SSIs were indicated as the most likely cause of nosocomial infection in obstetrics and gynecology than in general surgical wards [16].
Despite improvements in operating room practices, instrument sterilization methods, better surgical technique, and the best efforts of infection prevention strategies, SSIs remain a major cause of hospital-acquired infections and rates are increasing globally even in hospitals with modern facilities and standard protocols of preoperative preparation and antibiotic prophylaxis [17]. Worldwide, SSIs have been responsible for the growing cost; morbidity and mortality correlated with surgeries, and continued to be difficult to address [18].
Although antibiotics are available, SSIs are still responsible for much morbidity and far reaching socioeconomic consequences especially in developing countries like Ethiopia. A better understanding of magnitude and causes might improve SSIs infection control.
The overall prevalence and causes of SSI among women undergoing C/S in Ethiopia have not yet been investigated. Therefore, the main aim of this systematic review and meta-analysis was to estimate the pooled prevalence and to identify the root causes of SSI in Ethiopia. The findings of this meta-analysis will help policy makers and other concerned bodies in planning and implementing strategies to prevent and/or mitigate impacts of SSIs. The study could also be used as a baseline for researchers to carry out investigations on related topics. The review question is: What are the prevalence and associated risk factors for SSI among women undergoing C/S in Ethiopia?
Methods
Identification and study selection
Both peer reviewed published articles and unpublished research reporting the prevalence and root causes of SSI among women undergoing C/S in Ethiopia were searched by three authors (FA, AM, and AG). Eligible studies in English language only were identified through a literature search of Medline (PubMed), EMBASE, HINARI, Google Scholar, Science Direct, Cochrane Library, and other sources. The references of each included article were also searched manually to exhaustively retrieve the articles. The search of the articles was performed from January 9, 2019, until March 15, 2019. Unpublished studies such as theses/dissertation and reports from digital library catalogues were also searched through Google and Google Scholar. The terms for the search were pre-defined for a comprehensive search strategy that included all fields within records, and Medical Subject Headings (MeSH terms) for expanding the search in an advanced PubMed search. In the Boolean operator, within each axis, we combined keywords with the “OR” operator and we then linked the search strategies for the two axes with the “AND” operator. The search terms used for the search were “Prevalence” OR “Epidemiology” AND “Caesarean” AND/OR “Caesarean section” OR “Cesarean” AND/OR “Cesarean section” AND “SSI” AND/OR “Surgical site infection” AND/OR “Incision Infection” AND “Obstetric” AND/OR “Obstetrics” AND/OR “Obstetrical” AND” Mothers “OR “Maternal” AND/OR “Women” AND/OR “Females” AND” Ethiopia” AND/OR “Ethiopian hospitals”. The specific searching detail in pubmed with MeSH terms was (“surgical wound infection”[MeSH Terms] OR (“surgical”[All Fields] AND “wound”[All Fields] AND “infection”[All Fields]) OR “surgical wound infection”[All Fields] OR (“surgical”[All Fields] AND “site”[All Fields] AND “infection”[All Fields]) OR “surgical site infection”[All Fields]) AND (“Caesarean section”[All Fields] OR “Cesarean section”[MeSH Terms] OR (“Cesarean”[All Fields] AND “section”[All Fields]) OR “Cesarean section”[All Fields]) AND (“ethiopia”[MeSH Terms] OR “ethiopia”[All Fields]). All the literatures accessible until March 15, 2019 were included in the present study. The systematic review and meta-analysis was guided with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [19].
Eligibility criteria
Inclusion criteria
Studies reporting prevalence and causes of SSI among women undergoing C/S in Ethiopia were included.
Study area
Only articles conducted in or including Ethiopian hospitals.
Study design
All observational studies (cross-sectional, case controls and cohort) that contain original (primary) data reporting of the prevalence and associated risk factors SSI among women undergoing C/S in Ethiopia were considered.
Language
Literature published in the English language only was included.
Population
Studies conducted among women undergoing C/S were considered.
Publication condition
Both published articles and unpublished studies were considered.
Exclusion criteria
Non-accessible research whether published or unpublished if irretrievable from the internet or failures of reply to correspondences made by e-mail to the corresponding author within two weeks were excluded. Besides, research which did not report our outcome of interest, were excluded after reviewing (by three authors, FA, GS and AL) per our protocol described herein.
Data abstraction
All the necessary data were retrieved using a consistent data extraction format in Microsoft Excel™ by two authors (FA and AG). For the prevalence of SSI, the data extraction format included first author, the region where the study was conducted, and the hospital where the study was carried out, publication year, study design, sample size, and prevalence of SSI.
For the root causes, the data extraction format was prepared for each specific potential cause (i.e., rupture of membrane more than 12 h, chorioamnionitis, prolonged labor, meconium, anemia, type of incision, and type of anesthesia). The researchers chose these variables because they are the most commonly reported associated risk factors in the studies included in this meta-analysis. In this systematic review and meta-analysis, the investigator considered variables as root causes if two or more studies mentioned them as risk factors (cause). For every root cause, to compute the odds ratio, the data from the primary studies were extracted in the form of two by two tables by the two authors (FA and AG).
Outcome measurements
This systematic review and meta-analysis has two major outcomes. The primary outcome is to determine prevalence of SSI among women undergoing C/S in Ethiopia. The overall prevalence was calculated by dividing the number of mothers who develops SSI to the total number of mothers who delivered by C/S in the study period who have been included in the study (sample size) multiplied by 100. The second outcome of the study was to identify the root causes of surgical site infection.
Quality assessment
To evaluate the quality of the studies included in this review, two researchers (FA and AM) applied the Newcastle-Ottawa Scale tool as modified for cross-sectional studies’ quality assessment [20]. The tool consists of three major parts. The first part has potentially five stars and assesses the methodological quality of each study with one star indicating poor quality and five stars indicating excellent quality. The second part of the tool assesses the comparability of the studies with up to two stars to be assessed. The last part determines the quality of the original articles with respect to their statistical analysis and outcomes with a possibility of up to three stars. Using the tool as a checklist, the qualities of each of the original articles were evaluated independently by the two authors. Any difference between the authors on quality assessment result was solved by discussion. Articles with medium to high (at least three of five stars on the first part of the tool) and high quality (≥6out of 10 across the three parts) were included for the analysis.
Statistical analysis
The required data were collected using a Microsoft Excel™ form and analyzed by using STATA Version 15.0 software. The original articles were presented using tables and forest plot. The researcher calculated the standard error of prevalence for each original article by the binomial distribution formula. Heterogeneity among the reported prevalence of studies was checked by using heterogeneity χ2 test, I2 test and the p-values [21]. The above statistical tests indicated that there was a significant heterogeneity among the studies (I2 = 95.5%, p < 0.000). As a result, a random effects meta-analysis model was applied to estimate the Der Simonian and Laird’s pooled effect. In addition, univariate meta-regression model was conducted by taking publication year and sample size of the studies to assess the probable source of heterogeneity, but none was statistically significant. Possible publication bias was also evaluated objectively by using Egger’s correlation and Begg’s regression intercept tests at 5% significant level respectively [20, 22]. The Egger’s weighted regression and Begg’s rank correlation test methods were also used to assess publication bias and was insignificant (P < 0.059). Furthermore, to reduce the random discrepancies between the point estimates of the primary study, sub-group analysis was carried out based on region of studies.
Results
Search results
A total of 164 articles regarding prevalence and root causes of surgical site infection in Ethiopia were retrieved from the databases of Medline (PubMed), EMBASE, HINARI, Google Scholar, Science Direct, Cochrane Library and other sources described above. From these preliminary records, 124 articles were excluded due to duplication. From the remaining 40 articles, 14 articles were excluded as they were found to be not eligible to this review after assessing their titles and abstracts. The remaining 26 full text articles were then accessed, and assessed for eligibility based on the preset criteria, which resulted in further exclusion of 13 articles primarily due to the study population and/or outcome of interest. Among these, four of the studies were conducted in countries other than Ethiopia: Nigeria [23], China [24], India [25] and England [26]. The remaining nine studies were conducted in different regions of Ethiopia [27,28,29,30,31,32,33,34,35] and excluded because of the study population and unreported outcome of interest. Finally, 13 eligible studies were included in the review (Fig. 1).
Characteristics of original articles
A total of 13 original studies that reported the prevalence of SSI among women undergoing C/S and its root causes were included in this systematic review and meta-analysis. The studies were conducted from 2010 to 2019. The study design for all included research was cross-sectional. In this study, 8496 study participants were included to estimate the pooled prevalence of SSI and its root causes in Ethiopia. The quality score of the research ranged from 6 to 8 out of 10 as assessed by the Newcastle-Ottawa tool described previously. The studies were conducted in Oromia Region [36,37,38], Southern Nations and Nationalities of Peoples (SNNP) Region [39,40,41], Tigray Region [42,43,44], Amhara Region [45, 46] and Addis Ababa [47, 48]. The sample size ranged from 98 in Oromia Region [37] to 2911 Tigray Region [43] (Table 1).
Meta-analysis
Prevalence of surgical site infection among women undergoing caesarean section in Ethiopia
Thirteen studies across 5 regions of Ethiopia yielded an overall prevalence of SSI 8.81% (95% CI: 6.34–11.28) among mothers who delivered by C/S (Fig. 2). Considerable heterogeneity was found across the studies as revealed by I2 statistic (I2 = 95.5, p value < 0.05); hence, a random effect model was used to estimate the pooled prevalence of SSI post-C/S in Ethiopia. A univariate meta-regression model was also carried out to identify the possible sources of heterogeneity, by considering factors, such as publication year and sample size although none of these variables was found to be statistically significant. Beggs’ and Eggers’ tests also indicated the absence of statistically significant publication bias (p > 0.05 for both).
Sub-group analysis
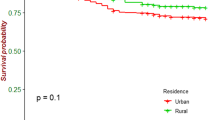
Due to considerable heterogeneity among the included articles in this study, sub-group analysis based on study region was considered to identify the possible source of heterogeneity across studies. The highest prevalence was observed in Oromia Region with a prevalence of 16.66 per 100(95% CI: 8.92, 24.40) followed by Amhara Region, 9.06 per 100 (95% CI: 6.93, 11.20);SNNP Region,8.28 per 100 (95% CI: 4.92, 11.63); Tigray Region, 6.38 per 100(95% CI: 0.97, 11.79) and Addis Ababa, 4.92 per 100 (95% CI: 0.81, 9.03) (Fig. 3).
Root causes of surgical site infection among women undergoing C/S in Ethiopia
Prolonged labor (≥25 h) (95% CI: 2.65–10.06), prolonged rupture of membrane (≥13 h) (95% CI: 3.33–8.29), presence of anemia (95% CI: 3.77–23.51), presence of chorioamnionitis (95% CI: 4.05–21.45), presence of meconium (95% CI: 1.41–9.99), vertical skin incision (95%CI 2.61–5.85), greater than 2 cm thickness of subcutaneous tissue (95%CI: 0.83–5.92 and general anesthesia (95%CI: 2.02–5.85) were significantly associated with surgical site infection.
Mothers with prolonged labor (25 or more hours) at the time of the C/S had 5.16(95% CI: 2.65–10.06) times increased odds of SSI than their counterparts. The odds of SSI were also increased by 5.26(95% CI: 3.33–8.29) among mothers who had prolonged rupture of membrane (rupture of membranes for 13 or more hours). Mothers who had anemia, chorioamnionitis and/or meconium were9.41 (95% CI: 3.77–23.51), 9.32(95% CI: 4.05–21.45) and 3.76 (95% CI: 1.41–9.99) times more likely at high risk for SSIs as compared to those mothers with none of these conditions prior to C/S, respectively.
Study subjects who underwent vertical skin incision were 3.91(95%CI: 2.61–5.85) times more likely to develop SSIs than those who had transverse skin incision. Mothers whose subcutaneous tissue thickness was greater than 2 cm were 2.82 (95%CI: 1.61–4.94) times more likely at risk for SSI than mothers whose subcutaneous tissue thickness was less than 2 cm.
Finally, mothers who had C/S by general anesthesia were 2.69(95%CI: 2.02–5.85) times more likely to develop SSI as compare with mothers who had C/S by spinal anesthesia (Table 2).
Discussion
The aim of this systematic review and meta-analysis was to estimate the pooled prevalence of SSI post-C/S and its root causes in Ethiopia. The study has found that the overall prevalence of SSI in Ethiopia among women undergoing C/S is 8.81%. This finding is similar to studies conducted in Cameroon [49] and Nigeria [23] which have reported SSIs prevalence of 9.16 and 9.1%, respectively. The prevalence of SSIs observed in the present study is slightly less than studies conducted in Tanzania and Nepal which reported prevalence of 10.9 and 12.6% respectively [50, 51]. However, this study has higher prevalence than reports from Turkey (0.3%), United States of America (5.2%), and Italy (1.6%) [18, 52, 53]. There could be numerous reasons for the heterogeneity of the prevalence rates among the various studies as compared with the present study. Higher prevalence rates of SSIs in developing countries may be due to limited hygienic practice unlike developed countries with relatively better standards of infection control policies and practices. Difference in population sampling, study design, and ethnicity may also contribute to the variation in the prevalence rates in the above studies as compared to the present study.
The sub-group analysis of this study demonstrated that the prevalence of SSI among women undergoing C/S significantly varies across regions. The highest prevalence of SSI was observed in Oromia Region, followed by Amhara, SNNP, and Tigray Regions, while the lowest prevalence was observed in the urban region of Addis Ababa. Possible justifications for this pattern could be population variation across the regions. According to Ethiopian Central Statistical Agency, in 2015, the total number of peoples were higher in Oromia followed by Amhara, SNNP, Tigray then Addis Ababa [54]. This population potentially leads to excessive numbers of mothers in obstetric wards with likely cases of infection [55]. Another possible reason could be due to poor dietary style, poor personal hygiene, and low socioeconomic capacity of rural people across regions than urban populations leading women to be vulnerable to nosocomial post-C/S SSIs.
The present study shows that there are significant associations between SSI and labor duration, rupture of membrane, anemia, chorioamnionitis, meconium, types of incision, thickness of subcutaneous tissue, and types of anesthesia. In this study, mothers with prolonged labor (≥25 h) and prolonged rupture of membrane (≥13 h) before operation had considerably increased risk of SSI than their counterparts. Studies carried out in Kenya [56], Nigeria [23], Qatar [57] and Israel [58] reported comparatively similar conclusions. Normally, during pregnancy, amniotic fluid and cervical mucus server as barriers to infection. However, if the membrane is ruptured, this protective effect is gradually reduced over time as amniotic fluid becomes no longer sterile. It, therefore, appears that prolonged labor and rupture of membranes contribute to amniotic fluid migration from the normal flora of the lower genital tract and direct to surgical site and peritoneal cavity [59].
In our study, anemia was found to be predicative of SSIs showing women with anemia having 9.41 times more likelihood to develop SSIs as compared to non-anemic women. This finding was in line with previous studies conducted in Nigeria [60], India [61], and China [59] and may reflect that low hemoglobin concentration reduces the oxygen tension in the wound site and increases the risk of SSI by compromising the activity of macrophages [49] and delaying infection healing progress [62].
In the current study, women with chorioamnionitis were 9.32 times more likely to develop SSIs when compared to those women who had no chorioamnionitis. Similar findings have been reported in Sub-Saharan African countries, India, and United States of America [63,64,65]. The potential explanation might be that unbroken membranes serve as a barrier to infections from the lower genital tract to the uterine cavity, which could also be due to iatrogenic infectivity of the peritoneum during surgery.
In the present study, women with meconium were 3.76 times more likely to develop SSIs when compared to those women who had no meconium. This finding is in line with a previous study which reported that occurrence of thick meconium in amniotic fluid is strongly associated with SSIs [66].
In addition, women who had vertical abdominal incisions were more likely to develop surgical site infections as compared to those women who had transverse incisions, which was also reflected in a study conducted in Nigeria [67]. The rationale may be due to the fact that a vertical incision is performed in the lower midline through the linea Alba which has poor blood supply. As a result, the area of incision may undergo necrosis and subsequent degeneration after incision if its edges are not aligned properly during closure.
Thickness of subcutaneous tissue more than 2 cm was also one of the causes for surgical site infection in this study. Similar findings were reported in an American study [68]. This risk factor could be due to reduced vascularity of the subcutaneous tissue, serous fluid collection, and hematoma formation in an overweight woman.
Finally, mothers for whom operations were under general anesthesia were more likely to have SSIs compared to mothers under spinal anesthesia. This finding is in agreement with the studies conducted in various African countries which indicated that C/S and use of general anesthesia increase the risk of accidental internal organs damage and internal bleeding because of uterine atony [69,70,71].
Limitations of the study
All articles considered in this systematic review and meta-analysis were cross-sectional by design. As a result, temporal associations between the factors and the outcome variables cannot be established. Most of the studies included in this review had a relatively small sample size which may affect the final estimation. In addition, as this meta-analysis included available studies reported from a small number of hospitals in Ethiopia, there may be under-representation of the different regions in the country.
Conclusion
The prevalence of SSI among women undergoing C/S was higher compared to the standard center of disease control (CDC) guidelines of SSI [72]. The highest prevalence of SSI within the Ethiopian studies reviewed was observed in Oromia Region followed by Amhara Region, SNNP Region and Tigray Region, while the least prevalence was observed in Addis Ababa. Labor duration, rupture of membrane, anemia, chorioamnionitis, meconium, types of skin incision, thickness of subcutaneous tissue and types of anesthesia were significantly associated with SSI post-C/S. Therefore, based on the findings, it is recommended that efforts should be made to ensure that prevention of prolonged labor through early intervention in cases where there is protracted progress of labor. In addition, minimizing early artificial rupture of membranes should be encouraged to decrease incidence of prolonged rupture of membranes. Furthermore, effective post-operative antibiotics should be given to patients undergoing C/S, especially those who are at risk of post-C/S infection (i.e. anemia, chorioamnionitis, presence of meconium and obesity). Transverse incision and spinal anesthesia are recommended to minimize the incidence of SSI post-C/S. Finally, given the high prevalence of SSIs shown in this review, it is recommended that active SSI surveillance and infection prevention strategies be established nationally.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- C/S:
-
Caesarean section
- CDC:
-
Center of Disease Control
- SNNP:
-
Southern Nations and Nationalities of Peoples
- SSI:
-
Surgical site infection
References
Betrán AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, Van Look P, Wagner M. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol. 2007;21(2):98–113.
Petherick ES, Dalton JE, Moore PJ, Cullum N. Methods for identifying surgical wound infection after discharge from hospital: a systematic review. BMC Infect Dis. 2006;6(1):170.
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16(3):128–40.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13(10):606–8.
Dahms RA, Johnson EM, Statz CL, Lee JT, Dunn DL, Beilman GJ. Third-generation cephalosporins and vancomycin as risk factors for postoperative vancomycin-resistant enterococcus infection. Arch Surg. 1998;133(12):1343–6.
Bratzler DW. Strategies for the prevention of Surgical site infections: Review of New Multi-specialty Society Guidelines. Oklahoma: University of Oklahoma Health Sciences Center, 2012.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR, Committee HICPA. Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol. 1999;20(4):247–80.
Skarzyńska J, Cienciała A, Madry R, Barucha P, Kwaśniak M, Wojewoda T, Sroga J. Hospital infections in general surgery wards. Przeglad epidemiologiczny. 2000;54(3–4):299–304.
Martens MG, Kolrud B, Faro S, Maccato M, Hammill H. Development of wound infection or separation after cesarean delivery. Prospective evaluation of 2,431 cases. J Reprod Med. 1995;40(3):171–5.
Sun J, Ding M, Liu J, Li Y, Sun X, Liu T, Chen Y, Liu J. Prophylactic administration of cefazolin prior to skin incision versus antibiotics at cord clamping in preventing post-cesarean infectious morbidity: a systematic review and meta-analysis of randomized controlled trials. Gynecol Obstet Investig. 2013;75(3):175–8.
Ott WJ. Primary cesarean section: factors related to postpartum infection. Obstet Gynecol. 1981;57(2):171–6.
Taye M. Wound infection in Tikur Anbessa hospital, surgical department. Ethiop Med J. 2005;43(3):167–74.
Gedebou M, Habte-Gabr E, Kronvall G, Yoseph S. Hospital-acquired infections among obstetric and gynaecological patients at Tikur Anbessa hospital, Addis Ababa. J Hosp Infect. 1988;11(1):50–9.
Kotisso B, Aseffa A. Surgical wound infection in a teaching hospital in Ethiopia. East Afr Med J. 1998;75(7):402–5.
Habte-Gabr E, Gedebou M, Kronvall G. Hospital-acquired infections among surgical patients in Tikur Anbessa hospital, Addis Ababa, Ethiopia. Am J Infect Control. 1988;16(1):7–13.
Daniel A, Zemanuel T. Hospital acquired surgical site and catheter related urinary tract infections among patients admitted in Mekele hospital, Mekele, Tigray, Ethiopia. AAU libraries electronic thesis and dissertation. 2008;23.
B'erard F. Postoperative wound infections: the influence of ultraviolet irradiation of the operating room and of various other factors. Ann Surg. 1964;160(1):1–192.
Yalcin A, Bakir M, Bakici Z, Dökmetas I, Sabir N. Postoperative wound infections. J Hosp Infect. 1995;29(4):305–9.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–34.
Rücker G, Schwarzer G, Carpenter JR, Schumacher M. Undue reliance on I 2 in assessing heterogeneity may mislead. BMC Med Res Methodol. 2008;8(1):79.
Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54(10):1046–55.
Jido T, Garba I. Surgical-site infection following cesarean section in Kano, Nigeria. Ann Med Health Sci Res. 2012;2(1):33–6.
Gong SP, Guo HX, Zhou HZ, Chen L, Yu YH. Morbidity and risk factors for surgical site infection following cesarean section in Guangdong Province, China. J Obstet Gynaecol Res. 2012;38(3):509–15.
Dahiya P, Gupta V, Pundir S, Chawla D. Study of incidence and risk factors for surgical site infection after cesarean section at first referral unit. Int J Contemp Med Res. 2016;3(4):1102–4.
Wloch C, Wilson J, Lamagni T, Harrington P, Charlett A, Sheridan E. Risk factors for surgical site infection following caesarean section in England: results from a multicentre cohort study. BJOG Int J Obstet Gynaecol. 2012;119(11):1324–33.
Forrester JA, Koritsanszky L, Parsons BD, Hailu M, Amenu D, Alemu S, Jiru F, Weiser TG. Development of a surgical infection surveillance program at a tertiary hospital in Ethiopia: lessons learned from two surveillance strategies. Surg Infect. 2018;19(1):25–32.
Kuzma TO. Caesarean Sections in a National Referral Hospital in Addis Ababa, Ethiopia: Trends, Predictors and Outcomes; 2016.
Yallew WW, Kumie A, Yehuala FM. Point prevalence of hospital-acquired infections in two teaching hospitals of Amhara region in Ethiopia. Drug Healthcare Patient Saf. 2016;8:71.
Ephraim G, Makonnen A, Seid M, Fasil T. Analysis of deliveries in Jimma hospital, a four year retrospective study. Ethiop J Health Dev. 1991;5(1):3–6.
Weldu MG, Berhane H, Berhe N, Haile K, Sibhatu Y, Gidey T, Amare K, Zelalem H, Mezemir R, Hadgu T. Magnitude and determinant factors of surgical site infection in Suhul hospital Tigrai, northern Ethiopia: a cross-sectional study. Surg Infect. 2018;19(7):684–90.
Laloto TL, Gemeda DH, Abdella SH. Incidence and predictors of surgical site infection in Ethiopia: prospective cohort. BMC Infect Dis. 2017;17(1):119.
Woldegioris T, Bantie G, Getachew H. Nurses' knowledge and practice regarding prevention of surgical site infection in Bahir Dar, Northwest Ethiopia. Surg Infect. 2018;20(1):71–7.
Mengesha RE, Kasa BG-S, Saravanan M, Berhe DF, Wasihun AG. Aerobic bacteria in post surgical wound infections and pattern of their antimicrobial susceptibility in Ayder teaching and referral hospital, Mekelle, Ethiopia. BMC research notes. 2014;7(1):575.
Dessie W, Mulugeta G, Fentaw S, Mihret A, Hassen M, Abebe E. Pattern of bacterial pathogens and their susceptibility isolated from surgical site infections at selected referral hospitals, Addis Ababa, Ethiopia. Int J Microbiol. 2016;2016.
Amenu D, Belachew T, Araya F. Surgical site infection rate and risk factors among obstetric cases of Jimma University specialized hospital, Southwest Ethiopia. Ethiop J Health Sci. 2011;21(2):91–100.
Fantu S, Segni H, Alemseged F. Incidence, causes and outcome of obstructed labor in jimma university specialized hospital. Ethiopian journal of healthsciences. 2010;20(3):145–151.
Mamo T, Abebe TW, Chichiabellu TY, Anjulo AA. Risk factors for surgical site infections in obstetrics: a retrospective study in an Ethiopian referral hospital. Patient Saf Surg. 2017;11(1):24.
Angelo AMDaAT. Magnitude of post caesarean section surgical site infection and its associated factors among mothers who underwent caesarean section in Mizan Tepi University teaching hospital, south West Ethiopia. J Nurs Care. 2018;2(7):454.
Tesfaye T, Hailu D, Mekonnen N, Tesfaye R. Magnitude of Maternal Complication and Associated Factors among Mothers Undergone Cesarean Section at Yirgalem General Hospital, SNNPR, Ethiopia. Risk. 2017;100:11.
Wodajo S, Belayneh M, Gebremedhin S. Magnitude and factors associated with post-cesarean surgical site infection at Hawassa University teaching and referral hospital, southern Ethiopia: a cross-sectional study. Ethiop J Health Sci. 2017;27(3):283–90.
Gelaw KA, Aweke AM, Astawesegn FH, Demissie BW, Zeleke LB. Surgical site infection and its associated factors following cesarean section: a cross sectional study from a public hospital in Ethiopia. Patient Saf Surg. 2017;11(1):18.
Tadesse H, Gessessew A, Medhanyie AA. Trends and Outcomes of Cesarean Delivery in Ayder Comprehensive Specialized Hospital, Mekelle City, Northern Ethiopia. East African Journal of Health Sciences. 2019;1(1):62–77.
Wendmagegn TA, Abera GB, Tsehaye WT, Gebresslasie KB, Tella BG. Magnitude and determinants of surgical site infecion among women underwent cesarean section in Ayder comprehensive specialized hospital Mekelle City, Tigray region, northern Ethiopia, 2016. BMC Pregnancy Childbirth. 2018;18(1):489.
Gedefaw G, Asires A, Shiferaw S, Addisu D. Factors associated with surgical site infection among women undergoing obstetrics surgery at Felegehiwot referral hospital, Bahir Dar, Northwest Ethiopia: a retrospective cross-sectional study. Saf Health. 2018;4(1):14.
Anna Rose FB, Moore JNAND, Graham WJ. Post-caesarean section surgical site infections: a retrospective audit and case note review at an Ethiopian referral hospital. Obstet Gynecol Rep. 2018;2(2):5–6.
Guto BAaaA. Indications and outcomes of emergency caesarean section at St Paul’s HospitalMedical college, Addis Ababa, Ethiopia 2017: (afoul month retrospective cohort study). Invest Gynecol Res Womens Health. 2018;2(2):1–15.
Gelaw MW, Abdela A. Prevalence of surgical site infection and associated factors among mothers after cesarean delivery in zewditu memorial hospital. Ethiopian Journal of Reproductive Health. 2018;10(4):21–32.
Abdallah A, Rafeek MES. Risk factors of surgical site infection of cesarean section and role of skin cleansing and prophylactic antibiotic; 2018.
Haerskjold A, Hegaard H, Kjaergaard H. Emergency caesarean section in low risk nulliparous women. J Obstet Gynaecol. 2012;32(6):543–7.
Shrestha S, Shrestha R, Shrestha B, Dongol A. Incidence and risk factors of surgical site infection following cesarean section at Dhulikhel hospital. Kathmandu Univ Med J. 2014;12(2):113–6.
Wischnewski N, Kampf G, Gastmeier P, Schlingmann J, Schumacher M, Daschner F, Ruden H. Nosocomial wound infections: a prevalence study and analysis of risk factors. Int Surg. 1998;83(2):93–7.
Garner JS. The CDC hospital infection control practices advisory committee. Am J Infect Control. 1993;21(3):160–2.
Ababa A. Central statistical agency; 2007.
Maruta A. Surveillance of surgical site infections following caesarean section at two central hospitals in Harare, Zimbabwe. Stellenbosch: Stellenbosch University; 2015.
Koigi-Kamau R, Kabare L, Wanyoike-Gichuhi J. Incidence of wound infection after caesarean delivery in a district hospital in Central Kenya. East Afr Med J. 2005;82(7):357–61.
Al Jama FE. Risk factors for wound infection after lower segment cesarean section. Qatar Med J. 2013;2012(2):9.
Schneid-Kofman N, Sheiner E, Levy A, Holcberg G. Risk factors for wound infection following cesarean deliveries. Int J Gynecol Obstet. 2005;90(1):10–5.
Plummer FA, Laga M, Brunham RC, Piot P, Ronald AR, Bhullar V, Mati J, Ndinya-Achola JO, Cheang M, Nsanze H. Postpartum upper genital tract infections in Nairobi, Kenya: epidemiology, etiology, and risk factors. J Infect Dis. 1987;156(1):92–8.
Ezechi OC, Edet A, Akinlade H, Gab-Okafor CV, Herbertson E. Incidence and risk factors for caesarean wound infection in Lagos Nigeria. BMC Res Notes. 2009;2(1):186.
De D, Saxena S, Mehta G, Yadav R, Dutta R. Risk factor analysis and microbial etiology of surgical site infections following lower segment caesarean section. International Journal of Antibiotics. 2013;2013:1–7.
Gordillo GM, Sen CK. Revisiting the essential role of oxygen in wound healing. Am J Surg. 2003;186(3):259–63.
Mbim EN, Mboto CI, Agbo BE. A review of nosocomial infections in sub-Saharan Africa. Br Microbiol Res J. 2016;15(1):1–11.
Haley RW, Culver DH, Morgan WM, White JW, Emori TG, Hooton TM. Identifying patients at high risk of surgical wound infection: a simple multivariate index of patient susceptibility and wound contamination. Am J Epidemiol. 1985;121(2):206–15.
Pathak A, Mahadik K, Swami MB, Roy PK, Sharma M, Mahadik VK, Lundborg CS. Incidence and risk factors for surgical site infections in obstetric and gynecological surgeries from a teaching hospital in rural India. Antimicrob Resist Infect Control. 2017;6(1):66.
Piper JM, Newton ER, Berkus MD, Peairs WA. Meconium: a marker for peripartum infection. Obstet Gynecol. 1998;91(5):741–5.
Olowe OA, Titilolu F, Bisi-Johnson M, Mosanya J. Antibiogram of surgical site infection in a tertiary health Care Facility in Osogbo, South Western Nigeria. Curr Trends Technol Sci. 2014;3(2):93–7.
Kawakita T, Landy HJ. Surgical site infections after Cesarean delivery: epidemiology, prevention and treatment. Matern Health Neonatol Perinatol. 2017;3(1):12.
Teguete I, Traore Y, Sissoko A, Djire M, Thera A, Dolo T, Mounkoro N, Traore M, Dolo A. Determining factors of Cesarean delivery trends in developing countries: lessons from point G National Hospital In: Cesarean Delivery: IntechOpen; Bamako-Mali 2012.
Pallasmaa N, Ekblad U, Gissler M. Severe maternal morbidity and the mode of delivery. Acta Obstet Gynecol Scand. 2008;87(6):662–8.
Nielsen TF, Hökegård KH. Cesarean section and intraoperative surgical complications. Acta Obstet Gynecol Scand. 1984;63(2):103–8.
Anderson DJ, Kaye KS, Classen D, Arias KM, Podgorny K, Burstin H, Calfee DP, Coffin SE, Dubberke ER, Fraser V. Strategies to prevent surgical site infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29(S1):S51–61.
Acknowledgements
We would like to articulate our thankfulness and appreciation to all Addis Ababa & Debre Markos University College of Medicine and Health Sciences staff that supported us in this review. We would also like to extend our gratitude to Pammla Petrucka (PhD, Professor), College of Nursing, University of Saskatchewan, Saskatoon) for editing the English language of the manuscript.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
FA and AM involved in the design, selection of articles, data extraction, statistical analysis and manuscript writing. AM, AG and AL were involved in selection of articles, statistical analysis and manuscript editing. GS and FA reviewed the protocols, tools, analysis and provided manuscript editing. All the authors read and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Adane, F., Mulu, A., Seyoum, G. et al. Prevalence and root causes of surgical site infection among women undergoing caesarean section in Ethiopia: a systematic review and meta-analysis. Patient Saf Surg 13, 34 (2019). https://doi.org/10.1186/s13037-019-0212-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13037-019-0212-6