Abstract
Background
Post surgical wound infections are global problem in the field of surgery associated with long hospital stay, higher treatment expenditure, morbidity and mortality. Hence to address the limited data in Ethiopia on post surgical wound infections, we conducted this research to determine the prevalence and antimicrobial susceptibility patterns of aerobic bacteria in post-surgical wound infected patients in Ayder teaching and referral hospital, Mekelle, Ethiopia.
Methods
Hospital based prospective cross sectional study was carried-out in 128 patients who had undergone surgery in general surgery and orthopaedic wards, and showed symptoms of infection clinically from January to June 2012. Standard bacteriological methods were used for bacterial isolation and antimicrobial susceptibility pattern.
Results
A total of 128 patients (98 male and 30 female) with clinical signs of post surgical wound infections were enrolled. The age of the patients ranged from 15–79 years (with mean 35.95 ± 19.01 years). Out of the 128 wound swabs taken, 96/128 (75%) were culture positive aerobically, yielding 123 bacterial isolates. Out of these the predominant bacterial isolates were Staphylococcus aureus 44 (35.77%), Klebsiella species 29 (22.76%) and Coagulase negative Staphylococci (CoNS) 18 (14.63%). No bacterial isolates was found to be sensitive to all antibiotics tested. Isolated bacteria showed 102/123 (82.92%) multi drug resistance to the commonly used antibiotics in the hospital. However, 54/ 65 (83.1%) of Gram negative and 58/58 (100%) of Gram positive isolates were sensitive to Gentamicin and Vancomycin, respectively.
Conclusion
Prevalence of was Post-operative wound infections rate in this current study was 75% and multi drug resistance was seen in 102/123(82.92%) of the isolates leaving clinicians with few choices of drugs for the treatment of post surgical wound infected patients. This underscores for periodic surveillance of etiologic agent and antibiotic susceptibility to prevent further emergence and spread of resistant bacteria pathogens.
Similar content being viewed by others
Background
Post-operative wound infections are major global problem in the field of surgery leading to many complications, increased morbidity and mortality [1, 2]. Most post-surgical wound infections are hospital acquired and vary from one hospital to the other [3]. Lack of standardized criteria for diagnosis presents a challenge to monitor the global epidemiology of surgical site infection. In addition to this, emerging of high anti-microbial resistance among bacterial pathogens has made the management and treatment of post-operative wound infections difficult [4]. The situation is serious in developing countries due to irrational prescriptions of antimicrobial agents [5]. The inoculum size, virulence and invasive capability of the organisms have been reported to influence the risk of infection. Moreover, the physiological state of the tissue in the wound and immunological integrity of the host also has equal importance in determining occurrence of infection [6, 7].
In Ethiopia, different studies reported that the prevalence of post surgical wound infection ranges from 14.8% -60% [8–12]. S. aureus, Kelbsiella species, E. coli, Proteus species, Streptococcus species, Enterobacter species, Pseudomonas species and Coagulase negative Staphylococci were reported as the most common pathogens [10, 11].
P.aeruginosa is an epitome of opportunistic nosocomial pathogen, which causes a wide spectrum of infections and leads to substantial morbidity in immuno compromised patients. Due to its high drug resistance to many antibiotics, the mortality rate is substantial [12, 13]. It is known that specific therapeutic options to patients with post surgical wound infections are mainly depend on data from antimicrobial susceptibility tests generated by clinical laboratories or sound epidemiological data from ongoing nosocomial infection surveillance [11]. However, data on the spectrum of bacteria isolated from hospitalized patients and their antimicrobial susceptibility patterns to guide post operative wound infection in the region is scarce. Furthermore, the magnitude and impact of multidrug resistance bacteria from post wound infections are unknown in Ayder referral and teaching hospital. Thus, this study aimed at determining the prevalence and drug susceptibility pattern of aerobic bacterial pathogens in post surgical wound infection in Ayder referral and teaching hospital.
Methods
Study design and sampling process
Hospital based cross sectional study was conducted in Ayder referral and teaching hospital from January to June 2012. The hospital is the only referral in the region serving for about 9 million people in including the neighbouring regions.
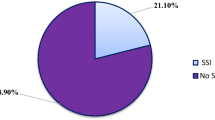
The study population consisted of patients who undergone surgery and developed SSI as diagnosed clinically by physicians within 30 days of having post surgical procedure. The sample size was estimated considering 92% prevalence (20), 5% precision, and 95% confidence level; with 10% contingency, thus, a total of 128 patients were included. During the study period, a total of 610 patients had undergone surgery, out of which swab samples were collected from 128 who showed clinical sings of post surgical wound infection.
Whereas surgical patients with community-acquired pyogenic infections such as abscess, furuncle and carbuncles; patients with infection of an episiotomy; and patients with open fractures were not included the study.
Postoperative wound infection: is defined as an infection in the tissues of the incision and operative area that can commonly occurs between the fifth and 30th days after surgery.
Data collection and laboratory procedures
Demographic and clinical characteristics from patients were collected using structured questionnaire. Infected site was cleaned using normal saline and sterile gauze then, two wound swabs were collected using sterile cotton swabs from each patient and immediately transported to the laboratory.
Bacterial identification
Wound swabs were processed in the bacteriology laboratory of the department of Medical Microbiology, Mekelle University, College of Health Sciences, within 1 hour of collection.
The first wound swab was used to make Gram stain smears whereas the second one was inoculated into blood agar, MacConkey agar and mannitol-salt agar, and incubated at 37°C for 24–48 hours. Identification of Gram positive bacteria was done using Gram stain, hemolytic activity on sheep blood agar plates, catalase reaction and coagulase test for Gram-positive bacteria. Gram-negative bacteria were identified based on colony morphology on blood agar and MacConkey agar, followed by biochemical reactions namely oxidase, triple sugar iron (TSI), Sulphur Indole and motility (SIM), citrate and urease tests [14].
Drug susceptibility tests
Following identification of the bacterial isolates, a standard disc diffusion technique for drug susceptibility test (DST) was performed as recommended by Clinical and Laboratory Standard Institute (CLSI) [15]. Ampicillin (10 μg), Gentamicin (10 μg), Erythromycin (15 μg), Amoxicillin- clavunilic acid (30 μg), Ceftriazone (30 μg) Cloxacilline (5 μg) (Cypress) and Vancomycin (30 μg) were used for Gram positive isolates. Ampicillin (10 μg), Gentamicin (10 μg), Amoxacillin-clavunilic acid (30 μg), Amoxicillin (30 μg), Tetracycline (30 μg) Ciprofloxacin (5 μg) and Ceftriazone (30 μg) (all Oxoid, England) Gram negative isolates were tested.
Quality control
Reference strains P.aeruginosa (ATCC-27853), E.coli (ATCC-25922) and S.aureus (ATCC- 25923) were used as reference strains for identification and drug susceptibility testing.
Data analysis
SPSS version 16 soft ware was used for statistical analysis. Chi-square test was used to determine the relationship between the dependent and the independent variables. P value <0.05 was considered as statistically significant.
Ethical issues
The study was approved and ethically cleared by the Research and Ethical Review Committee of Mekelle University, College of Health Sciences (# REC REF 2012–127).
Written informed consent was obtained from each study participants and parents or care takers. All patient information was kept confidential and secret using codes.
Results
We followed 610 successive patients (467 males and 143 female) who were referred for surgery to the hospital during the study period. From these, 128 patients were included (98 male and 30 female) with clinical sings of post surgical wound infections. The age of the patients ranged from 15–79 years (mean 35.95 ± 19.01 years). Bacterial growth was seen in 96/128(75%) of the patients yielding a total of 123 bacterial isolates. Among the isolates, 58(47.2%) were Gram positive and 65 (52.8%) were Gram negative. S. aureus 44 (35.77%) and Klebsiella species 29(22.76%) were the dominant isolates (Table 1). Single bacterial isolates were recovered from 73/96(76.05%) patients whereas 23/96(23.95%) had polymicrobial infections. S. aureus and Proteus species was the most common association (7 cases). Other frequent associations were: S. aureus and Klebsiella species (6 cases), Proteus species and CoNS (5 cases), S. aureus and CoNS (2 cases), CoNS and E.coli (2 cases) and Klebsiella species and CoNS (1 case). Sixty (46.87%), 36(28.12%) and 31(24.2%) of the patients were given Ceftriazone, Cloxacilline and combination of both, respectively for pre-surgical prophylaxis.
Drug resistance of isolated Gram negative bacteria, irrespective of species/genus, was 92.3% to Ampicillin, 92.3% to Tetracycline and 92.3% to Amoxicillin, 81.5% to Ceftriazone, 69.2% to Amoxicillin Clavunilic acid, 46.2% for Ciprofloxacin, 26.2% to Erythromycin and 16.9% for Gentamicin. Klebseilla species showed 100%, 93.1%, 89.7% and 86.2% resistance for Amoxicillin, Tetracycline and Ceftriazone, respectively. P. aeruginosa isolates were 100% resistant for Ceftriazone, Amoxicillin, Amoxicillin clavunilic acid and Tetracycline. All P. aeruginosa isolates were; however, 100% sensitive to Gentamicin. All the 15 (100%) Proteus species were resistant for Amoxicillin and Tetracycline whereas, Gentamicin was 12/15 (80%) sensitive. Isolated E.coli showed 100% resistance to Amoxicillin -clavulunic acid, Tetracycline and Ampicillin, whereas, all of them 6 (100%) were sensitive for Gentamicin.
Isolated Citrobacter species were 100% sensitive to Gentamicin, while all 4(100%) of them were resistant to Ampicillin (Table 2).
Resistance by S.aureus was 36/40 (90%) to Tetracycline, Ceftriazone and Ampicillin, and 34/40 (85%) to Cloxacilline. All of the isolates S.aureus 40(100%) were sensitive for Vancomycin. High resistance rate of CoNS was observed for Amoxicillin, Amoxicillin-clavunilic acid, Ampicillin and Tetracycline, 88.9%, 77.8%, 77.8% and 77.8%, respectively.
All isolates of CoNS 18(100%) were however, sensitive for Vancomycin (Table 3).
In the univariate analysis, statistically significant association was not seen between sex and bacterial infection though more bacteria were recovered from male (P = 0.055). Age of the patient has no significant association with the frequency of bacteria isolation (P =0.064).
On multivariate logistic regression analysis, longer duration from admission to discharge, longer duration of pre-operative, wound type, ward type and type of operation were statistically associated with bacteria isolation from post operative wound infection (Table 4).
Discussion
Wound infections rate in this present study was 75% which corroborates the reports from Niger 74.9% [16] and Nepal 80% [2] and rural tertiary hospital in Nigeria 70.1% [3] but higher than Addis Ababa 14.8% [8], North Ethiopia 44.1% [12], Kenya 7% [17] and tertiary care hospital in Gujarat, India 68.85% [13]. However, our finding was lower than reports from India 84% [18] , South Ethiopia 92% [19] and West Ethiopia 96.3%( 10). This difference in prevalence of post-operative infection may be due to variation in common nosocomial pathogens inhabitant, difference in policy of infection control and prevention between countries and hospitals, and study design used in the researches.
Multiple infections among post surgical wound infected patients was seen in 23(23.95%) of patients where S. aureus and Proteus species was the most common association where are the rest 77(87.5%) have shown single bacterial infection. S.aureus followed by Klebsiella spp was the predominant isolate which is in agreement to findings from Kenya [17] and Ethiopia [19]. S. aureus was the most prevalent isolates. This was in line with previous surveillance conducted in Ethiopia [10], Uganda [1], India [18] and Niger [20]. The normal flora nature of S.aureus in the skin and anterior nares, which can enter to deep site during surgery of the natural barrier of the skin, could be the possible justification for its high prevalence [1, 21].
Again the high prevalence rate of Entero-bacterial isolates in the current study could reveal faecal contamination due to poor personnel hygiene [16] or due to post procedural contamination [14].
Bacterial growth was not seen in 32/128 (25%) patients, which could attribute to the normal healing process of the wound by host immune system, antimicrobial activity or appropriate use of antiseptics for cleaning the wounds. It could also be due to anaerobic bacteria or fungi infection which we could miss due to the use of culture media that only support the aerobic bacteria [22, 23].
Patients who were given pre-operative antibiotic prophylaxis (Cloxacilline, Ceftriazone or both) developed more surgical site infections and drug resistance for these drugs. This was similar with the study done in Ethiopia by Taye (8) where patients who received preoperative antibiotics have a statistically significant higher wound infection rate (p < 0.001).
The present in vitro antimicrobial sensitivity test showed that isolated bacteria react differently to various antibiotics. Thirty six (90%) of the isolated S.aureus in our study were sensitive to Gentamicin similar to the report from Ethiopia [19, 24], Nepal [2] and Uganda [1]. However, 80% resistance of S.aureus to Gentamicin was reported elsewhere [25].
The difference could be due to the difference in prescribing this antibiotic for the treatment of the bacteria from hospital to hospital. All the isolated S.aureus 40(100%) were susceptible to Vancomycin in our finding exactly the same with that of report from Nepal 100% [2] and from West Ethiopia 100% [24]. But resistance of 66.7% to Vancomycin was seen elsewhere [12, 19]. Higher resistance 90% of S.aureus for Ceftriazone was observed in our current study than others [2, 19, 26]. High resistance rate (98.6-100%) was seen by Klebsiella spp. to Ceftriazone, Ampicillin and Amoxicillin similar to the report by from Ethiopia [24]. Less resistance 27.8.2% was observed to Gentamicin similar to study done elsewhere [2], but in contrary to our result, 100% resistance was reported from India [26]. The isolated P.aeruginosa were 100% resistant to Ceftriaxon, Amoxicillin, Tetracycline and Ampicillin similar resistance was reported elsewhere [19, 26] but as reported from Nepal [2] all isolates were 100% susceptible for Gentamicin.
Isolated E. coli were 100% resistant to Ampicillin similar result for Ampicillin was seen from Uganda [1], but all of them (100%) were sensitive for Gentamicin, similar to the result elsewhere [1, 19, 24]. Citrobacter spp were 100% resistant to Ampicillin exactly similar to the findings from Ethiopia 100% [24]. They were; however, all 100% sensitive to Gentamicin which is opposite to the result from Ethiopia [24] where all isolates were 100% resistant. Possible explanations for the disparity in drug resistance over places could attribute to the difference in the rational use of antibiotics in the study areas. In general multiple antibiotics resistance was seen in 81.4% of Gram negative and 82.8% of the Gram positive isolates. All isolated bacteria were highly resistant to Ampicillin, Ceftriazone, Tetracycline, Amoxicillin, Amoxicillin- clavunic acid and Cloxacilline. This remarkably higher resistance may be due to their easily availability and indiscriminate use of the drugs without proper prescription. Vancomycin, Gentamicin and Erythromycin in our study appear to be effective against post surgical wound infection in the study area that can be used with caution. On multivariate logistic regression analysis, longer duration from admission to discharge, longer duration of pre-operative, wound type, ward type and type of operation were statistically associated with bacteria isolation from postsurgical wound infection which in lines with studies done elsewhere [27, 28]. This is because patients with wound class III/contaminated (open, fresh, accidental wounds) and class IV/dirty-Infected (old traumatic wounds with retained devitalized tissue) and those that involve existing clinical infection or perforated viscera are at high risk to develop SSI (30). Orthopaedic wards, since patients require longer hospitalization time to recover from their bone cases, they become prone for post operative wound infections. In our present study patients who underwent emergency surgery type operation were at higher risk that those who underwent elective type operation. This may probably, due to the lack of readiness for operation on the patients’ side (8).
Limitation
The study did not isolate strict anaerobes bacteria and fungi, which could have increased the number of bacterial isolates reported as negative cultures.
Conclusion
Surgical site wound infection was high (75%) and multi drug resistance was seen in 102/123 (82.92%) of the isolates leaving clinicians with few choices of drugs for the treatment of post surgical wound infected patients. Wound type, longer preoperative stay, type of operation, wound class and ward type, showed statistically significant association with postoperative wound infection. Therefore, periodic surveillance of bacteria and antibiotic susceptibility is important to prevent further emergence and spread of resistant bacteria pathogens.
Authors’ information
Araya Gebreyesus Wasihun (BSc in medical lab Sciences, MSc in medical micro biology) Dr. Reiye Esayasis Mengesha (MD+, Ass. Professor) a senior general surgeon.
Dr. Berhe Gebre-Slassie Kasa (MD+, Ass. professor) is the only orthopedic surgeon in the hospital and department head of orthopedic surgery.
Dr Muthupandian Saravanan (PhD, Ass. Professor in medical microbiology and currently in the department of medical microbiology and immunology).
Mr. Derbew Fikadu Berhe (MSc, Ass.Professor in pharmacy, and PhD fellow in Netherlands.
References
Anguzu JR, Olila D: Drug sensitivity patterns of bacterial isolates from septic post-operative wounds in a regional referral hospital in Uganda. Afr Health Sci. 2007, 7 (3): 148-154.
Raza MS, Chander A, Ranabhat A: Antimicrobial susceptibility patterns of the bacterial isolates in post-operative wound infections in a tertiary care hospital, Kathmandu, Nepal. OJMM. 2013, 3 (3): 159-163. 10.4236/ojmm.2013.33024.
Isibor JO, Oseni A, Eyaufe A, Osagie R, Turay A: Incidence of aerobic bacteria & Candida albicans in post-operative wound infections. Afr J Microbial Res. 2008, 2: 288-291.
Andhoga J, Macharia AG, Maikuma IR, Wanyonyi ZS, Ayumba BR, Kakai R: Aerobic pathogenic bacteria in post-operative wounds at Moi teaching and referral hospital. East Afr Med J. 2002, 79 (12): 640-644.
Fadeyi A, Adigun I, Rahman G: Bacteriological pattern of wound swab isolates in patients with chronic leg ulcer. Int J Health Res. 2008, 1 (4): 183-188.
Masaadeh HA, Jaran AS: Incident of pseudomonas aeruginosa in post-operative wound infection. Am J Infect Dis. 2009, 5 (1): 1-6.
Ranjan K, Ranjan N, Bansal S, Arora D: Prevalence of pseudomonas aeruginosa in post-operative wound infection in a referral hospital in Haryana, India. J Lab Physicians. 2010, 2 (2): 74-77. 10.4103/0974-2727.72153.
Taye M: Wound infection in Tikur Anbessa hospital, surgical department. Ethiop Med J. 2005, 43 (3): 167-174.
Endalafer N, Gebre-Selassie S, Kotiso B: Nosocomial bacterial infections in a tertiary hospital in Ethiopia. J Infect Prevention. 2011, 12 (1): 38-43. 10.1177/1757177410376680.
Godebo G, Kibru G, Tassew H: Multidrug-resistant bacteria isolates in infected wounds at Jimma, Ethiopia. Ann Clin Microbiol Antimicrob. 2013, 12: 13-10.1186/1476-0711-12-13.
Mulu A, Moges F, Tessema B, Kassu A: Pattern and multiple drug resistance of bacterial pathogens isolated from wound infection at University of Gondar Teaching Hospital, North West Ethiopia. Ethiop Med J. 2006, 44 (2): 125-131.
Tesfahunegn Z, Asrat D, Woldeamanuel Y: Bacteriology of surgical site and catheter related urinary tract infections among patients admitted in Mekelle hospital, Mekelle, Tigray, Ethiopia. Ethiop Med J. 2009, 47 (2): 117-127.
Goswami NN, Trivedi HR, Goswami AP, Patel TK, Tripathi CB: Antibiotic sensitivity profile of bacterial pathogens in postoperative wound infections at a tertiary care hospital in Gujarat, India. Pharmacol Pharmacother. 2011, 2 (3): 158-164. 10.4103/0976-500X.83279.
Chaudhary SD, Vives MJ, Reiter MF: Postoperative spinal wound infections and postprocedural diskitis. J Spinal Cord Me. 2007, 30 (5): 441-451.
CLSI: Perfomance standars for antimicrobial susceptibility testing; twenty first information supplement, vol. CLSI document M100-S21. 2011, Wayne, PA: Clinical and Laboratory Standards Institute
Odedina EA, Eletta EA, Baloun RA, Idowu O: Isolates from wound infections at federal medical center, BIDA. Afr J clin exper microbio. 2007, 8 (2): 26-32.
Dinda V, Gunturu R, Kariuki S, Hakeem A, Raja A, Kimang A: Pattern of pathogens and their sensitivity isolated from surgical site infections at the Aga khan university hospital, Kenya. Ethiop J Health Sci. 2013, 23 (2): 141-149.
Amrita S, Sheetal R, Narendra N: Aerobic micro-organisms in post-operative wound infections and their antimicrobial susceptibility patterns. J Clin Diag Res. 2010, 4 (6): 3392-3396.
Guta M, Aragaw K, Merid Y: Bacteria from infected surgical wounds and their antimicrobial resistance in Hawassa University Referral Teaching Hospital, Southern Ethiopia. AJMR. 2014, 8 (11): 1118-1124.
Sani RA, Garba SA, Oyewole OA, Ibrahim A: Antibiotic resistance profile of gram positive bacteria isolated from wound infections in Minna, Bida, Kontagora and Suleja area of Niger State. J Health Sci. 2012, 2 (3): 19-22. 10.5923/j.health.20120203.01.
Bowler PG, Duerden BI, Armstrong DG: Wound microbiology and associated approaches to wound management. Clin Microbiol Rev. 2001, 14 (2): 244-269. 10.1128/CMR.14.2.244-269.2001.
Pondei K, Fente BG, Oladapo O: Current microbial isolates from wound swabs, their culture and sensitivity pattern at the Niger delta university teaching hospital, Okolobiri, Nigeria. Trop Med Health. 2013, 41 (2): 49-53. 10.2149/tmh.2012-14.
Rao R, Sumathi S, Anuradha K, Venkatesh D, Krishna S: Bacteriology of postoperative wound infections. Int J Pharm Biomed Res. 2013, 4 (2): 72-76.
Mulu W, Kibru G, Damtie M: Postoperative nosocomial infections and antimicrobial resistance pattern of bacteria isolates among patients admitted at felege hiwot referral hospital, bahirdar, Ethiopia. Ethiop J Health Sci. 2012, 22 (10): 7-18.
Adegoke AA, Tom M, Okoh AI, Jacob S: Studies on multiple antibiotic resistant bacteria isolated from surgical site infection. Sci Res Essays. 2010, 5 (24): 3876-3881.
Singh A, Sikka R, Maggu NK, Deep , Antrikshdeep , Chaudhary U, Gill PS, Sehgal PK: Prevalence and antibiotic sensitivity pattern of bacteria isolated from nosocomial patients. J Orthopaedics. 2010, 7 (2): e3-
Fehr J, Hatz C, Soka I, Kibatala P, Urassa H, Smith T, Mshinda H, Frei R, Widmer A: Risk factors for surgical site infection in a Tanzanian district hospital: a challenge for the traditional National Nosocomial Infections Surveillance system index. Infect Control Hosp Epidemiol. 2006, 27 (12): 1401-1404. 10.1086/509855.
Razavi SM, Ibrahimpoor M, Sabouri Kashani A, Jafarian A: Abdominal surgical site infections: incidence and risk factors at an Iranian teaching hospital. BM Surg. 2005, 5: 2-10.1186/1471-2482-5-2.
Acknowledgement
We would like to thank participants for their willing to participate in the study and health workers in surgical wards for their excellent technical assistance. We also acknowledge Mekelle University College of Health Sciences for giving grant to conduct the research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Conceived and designed the experiments: RE, BG, AG, and DF. Specimen collection, microbiological laboratory investigation: AG. Supervised the clinical component of research: BG and RE. Performed the experiments: AG DF and MS. Wrote the manuscript: RE, AG, BG, DF and MS. All authors have read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mengesha, R.E., Kasa, B.GS., Saravanan, M. et al. Aerobic bacteria in post surgical wound infections and pattern of their antimicrobial susceptibility in Ayder Teaching and Referral Hospital, Mekelle, Ethiopia. BMC Res Notes 7, 575 (2014). https://doi.org/10.1186/1756-0500-7-575
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-0500-7-575