Abstract
Liver Imaging Reporting and Data System (LI-RADS) is a system for interpreting and reporting of imaging features on multidetector computed tomography (MDCT) and magnetic resonance (MR) studies in patients at risk for hepatocellular carcinoma (HCC). American College of Radiology (ACR) sustained the spread of LI-RADS to homogenizing the interpreting and reporting data of HCC patients. Diagnosis of HCC is due to the presence of major imaging features. Major features are imaging data used to categorize LI-RADS-3, LI-RADS-4, and LI-RADS-5 and include arterial-phase hyperenhancement, tumor diameter, washout appearance, capsule appearance and threshold growth. Ancillary are features that can be used to modify the LI-RADS classification. Ancillary features supporting malignancy (diffusion restriction, moderate T2 hyperintensity, T1 hypointensity on hapatospecifc phase) can be used to upgrade category by one or more categories, but not beyond LI-RADS-4. Our purpose is reporting an overview and update of major and ancillary MR imaging features in assessment of HCC.
Similar content being viewed by others
Background
Hepatocellular carcinoma (HCC) is one of the most common human solid malignancies worldwide [1, 2]. The most important risk factor for the development of HCC is liver cirrhosis, regardless of its etiology [1]. Among patients with cirrhosis, those with chronic viral infection (hepatitis B and C) and high alcohol intake have the highest risks of HCC development. Imaging surveillance is a widely accepted tool that increases the likelihood of early detection of HCC and an accurate detection and characterization of focal liver nodule on patient at risk for HCC is mandatory since the management of HCC patients differs to other malignant or benign nodules [2]. According to National Comprehensive Cancer Network (NCCN) [3] and the guidelines of European Association for the Study of the Liver (EASL) and American Association for the Study Liver Diseases (AASLD), diagnostic criteria, to characterize HCC, can only be applied to cirrhotic patients and should be based on the detection of the typical hallmark of HCC (hypervascular in the arterial phase with washout in the portal venous or delayed phases) [4]. However, the current imaging-based criteria have several limitations, including the lack of established consensus regarding the exact definitions of imaging features, binary categorization (either definite or not definite HCC), and failure to address non-HCC malignancies and vascular invasion [5]. Therefore American College of Radiology (ACR) sustained the spread of Liver Imaging Reporting and Data System (LI-RADS) to homogenizing the interpreting, reporting and data collection of HCC imaging [6]. LI-RADS is a scheme for interpreting and reporting of imaging features on multidetector computed tomography (CT) and magnetic resonance (MR) studies in patients at risk for hepatocellular carcinoma (HCC) [5,6,7]. In the current (v. 2014) LI-RADS [6], the diagnosis of HCC is based on the presence of major imaging features. These are features used to categorize LI-RADS- category 3 (LR-3), LI-RADS- category 4 (LR-4), and LI-RADS- category 5 (LR-5) and include arterial-phase hyperenhancement, tumor diameter, washout appearance, capsule appearance, and threshold growth [6]. Ancillary features are imaging features that can be used to change the LI-RADS category [5]. Ancillary features favoring malignancy (diffusion restriction, moderate T2 hyperintensity, T1 hypointensity on hepatospecific phase) can upgrade category, but not beyond LR-4. In contrast, ancillary features favoring benignity can decrease category [5, 6].
As required in most clinical trials, MDCT presents the key imaging modality in the patient assessment. This is due to its wide availability, standardization, and ability to scan the whole abdomen and chest in one setting. MRI plays a role in HCC assessment of patients with contraindication to iodine contrast medium [8]. However, considering the evidences on the accuracy of the various imaging modalities on HCC assessment [9], so as the guidelines of the European Society of Gastrointestinal and Abdominal Radiology (ESGAR) Working Group [10], MRI is the technique to choose in pre-treatment setting. It is a valuable diagnostic tool providing lesion morphological and functional data, thanks to hepatospecific contrast medium and DW sequences [11,12,13,14].
To standardize imaging technique among institutions, LI-RADS outlines technical requirements for MRI. Precontrast, arterial phase, portal venous phase, and delayed phase are all required for MRI with extracellular agents. Each phase contributes to characterization of LI-RADS major features. For MRI with hepatobiliary agents, a delay of 15–20 min for gadoxetic acid and a delay of 1 h for gadobenate dimeglumine consistently provide high-quality hepatobiliary phase imaging. In the setting of cirrhosis increasing the delay for hepatobiliary phase imaging to 30 min or more for gadoxetic acid and 2–3 h for gadobenate dimeglumine may improve parenchymal enhancement somewhat [6]. Although the delayed phase cannot be used to evaluate washout appearance, it can be used to evaluate capsule appearance, a major feature of HCC. Also, the delayed phase and hepatobiliary phase can be used to evaluate hypointensity on both sequences; these are ancillary features favoring malignancy and so can be used to upgrade the category. Late arterial phase is strongly preferred over early arterial phase, as HCC enhancement usually is greater in the late than in the early phase, and some HCCs show hyperenhancement only in the late arterial phase [6]. Unenhanced T1-weighted (T1-W) out of phase (OP)/in phase (IP) is required. T1-W OP/IP allows identification of fat and iron and is necessary for assessment of some ancillary features. T2-W sequences are required, improving distinction between solid and nonsolid lesions and are necessary for assessment of some ancillary LI-RADS features. DWI is suggested but not required [6].
Our purpose is reporting an overview and update of major and ancillary MR imaging features in assessment of HCC.
Methods
This overview and update is the result of autonomous studies without protocol and registration number.
Search criterion
Several electronic dataset were searched: PubMed (US National Library of Medicine, http://www.ncbi.nlm.nih.gov/pubmed), Scopus (Elsevier, http://www.scopus.com/), Web of Science (Thomson Reuters, http://apps.webofknowledge.com/) and Google Scholar (https://scholar.google.it/). The following search criteria have been used: “hepatocellular carcinoma” AND “diffusion magnetic resonance imaging” AND “characterization, “hepatocellular carcinoma” AND “dynamic contrast enhanced magnetic resonance imaging” AND “characterization, “hepatocellular carcinoma” AND “EOB-GD-DTPA contrast medium” AND “characterization, “hepatocellular carcinoma” AND “multimodal imaging” AND “characterization”. The search covered the years from January 2000 to January 2017. Moreover, the reference lists of the found papers were analysed for papers not indexed in the electronic databases.
All titles and abstracts were analysed and exclusively the studies reporting MRI, EOB-GD-DTPA MRI, DWI results in the characterization of HCC were retained.
The inclusion criteria were: clinical study evaluating MR assessment of HCC, clinical study evaluating functional MR imaging criteria in the assessment of patients with HCC, and clinical study evaluating DWI and EOB-GD-DTPA to assessing HCC patient. Articles published in the English language from January 2000 to January 2017 were included. Exclusion criteria were unavailability of full text, general overview articles and congress abstracts; studies with lesion higher than 20 mm. There was not define a minimum number of patients as an inclusion criteria.
Results
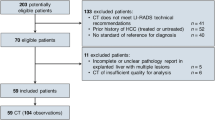
By using the search terms described earlier, we identified 5181 studies from January 2000 to January 2017. To identify additional relevant studies, the reference lists of the retrieved studies were checked manually. 1955 studies used other diagnostic techniques than MRI, EOB-GD-DTPA-MRI and DWI, 726 have different topic respect to characterization; 309 did not have sufficient data (case report, review, letter to editors); 2128 corresponded to more than one criteria so 63 articles were included at the end (Fig. 1).
Discussion
Early diagnosis is a critical step in the management of HCC patients. The identification of the specific vascular profile characterized by contrast arterial uptake followed by washout in the venous phases has allowed defining the non-invasive diagnostic criteria for HCC according to AASLD and EASL-EORTC guidelines [4, 5]. The typical hallmark has 100% specificity when demonstrated on dynamic contrast study, both on CT than on MRI, in patients at high risk of HCC [1]. However, arterial hyperehnancement and wash out appearance have a sensitivity rate of 50–60% in lesion smaller than 2 cm and thus a biopsy is still needed [15]. The typical vascular profile is correlated to hemodynamic changes in nodule during hepatocarcinogenesis, and to understand the hemodynamics of HCC is important for the accurate diagnostic analysis, because there is an intense correlation between their hemodynamics and pathophysiology [16]. Angiogenesis such as sinusoidal capillarization and unpaired arteries shows gradual increase during carcinogenesis from high-grade dysplastic nodule to classic hypervascular HCC. In accordance with this angiogenesis, the intranodular portal supply is decreased, whereas the intranodular arterial supply is first decreased during the early stage and then increased in parallel with increasing grade of malignancy of the lesion. On the other hand, the main drainage vessels of hepatocellular nodules change from hepatic veins to hepatic sinusoids and then to portal veins, mainly due to disappearance of the hepatic veins from the nodules [16]. The nodule appearance on arterial phase relative, considering the intra-lesion arterial supply, can be categorized into four types. Type I when the nodule is isodense to the surrounding cirrhotic liver parenchyma, and it is due to the same intranodular arterial blood supply relative to the surrounding liver. Type II, when the nodule is hypodense to the surrounding cirrhotic liver parenchyma, indicating decreased arterial blood supply. Type III a part of the nodule demonstrating hyperdensity due a partially increased arterial supply and type IV entirely hyperdense indicating entirely increased arterial supply [16, 17]. These findings reveal the significant correlation or strong tendency between type I and low grade dysplastic nodule and early HCC, type II and high grade dysplastic nodule and early HCC, type III and well differentiated HCC and type IV and moderately or poorly differentiated HCC [16, 17]. Also in early HCC, there is not perinodular enhancement on portal or equilibrium phase of contrast study, but it is definite in hypervascular classical HCC.
During hepatocarcinogenesis multi-step changes of drainage vessels and peritumoral enhancement occurred. In dysplastic nodules or early HCCs, the main drainage route from the tumor is intranodular or perinodular hepatic vein. However, because hepatic veins disappear from the tumor during very early stage of hepatocarcinogenesis, drainage vessels change to hepatic sinusoids. This drainage was well visualized in the late phase of contrast studies. Histological examination revealed continuity between a tumor sinusoid and a portal venule in the pseudocapsule (encapsulated HCC) or surrounding hepatic sinusoids (HCC without pseudocapsule). In moderately differentiated HCC with pseudocapsule formation, the communication between tumor sinusoids and the surrounding hepatic sinusoids are also blocked, and then, the portal venules in the pseudo-capsule finally become the main drainage vessel from the tumor. In accordance with the changes of the drainage vessels, thin to thick corona enhancement appears surrounding the tumor. Corona enhancement is thicker in encapsulated HCC and thin in HCC without pseudocapsule [16].
Arterial phase hyperenhancement
Arterial phase hyperenhancement is an essential prerequisite for definitely HCC (LR-5), but it is non-specific. In fact considering the hepatocarcinogenesis this feature may be not present, so as it may be observed in benign entities such as dysplastic nodules and arterio-portal shunts [1, 2]. Holland et al. showed, in proven HCC patients, that the majority (93%) of hypervascular lesions on arterial phase that were not detected on T2-W and portal and/or equilibrium phase of contrast study were non-neoplastic [18]. Conversely, Kim et coworkers [19] demonstrated that the most significant findings associated with HCC, in nodules smaller than 20 mm, were arterial phase hypernhancement. Ehman et al. demonstrated that arterial hypenhancement was the most commonly observed major criterion on 159 (86%) of 184 proven HCC, and was seen slightly more frequently at CT vs. MRI (87 vs. 86%, p = 1.00). Between the two readers, there was agreement on arterial phase characteristics in 156 (95%) cases (κ = 0.75) [20]. Conversely Burrel et al. [21] showed that sensitivity of MR was superior to CT to detect HCC (58/76 [76%] versus 43/70 [61%], respectively). Sensitivity of MR for detection of additional nodules decreased with size (>20 mm: 6/6 [100%]; 10–20 mm: 16/19 [84%]; <10 mm: 7/22 [32%]) and was superior to CT for nodules 10 to 20 mm (84 vs. 47%). Non specific hypervascular nodules >5 mm at MR were HCC in two thirds of the cases [21]. Special attention must be given to perfusion alterations, common condition in cirrhotic livers that may be false positive. These are areas of arterial hyperenhancement most frequently caused by arterioportal shunts [22, 23]. These alterations are usually peripheral, wedge shaped, and isointense relative to the surrounding parenchyma on T1- and T2-W MR images, and can be confidently characterized as LR-1. Perfusion alterations can also be nodular and it is difficult to distinguish from a true lesion [18, 23]. Areas of nodular arterial hyperenhancement seen exclusively during the arterial phase are more appropriately categorized as LR-2 [13, 18], but if corresponding others observations (eg, hyperintensity T2 signal or restricted diffusion) should be categorized as either LR-3 or LR-4 depending on its size and nonvascular features. Some areas of perfusion alteration can occur secondary to focal liver lesions, including HCC [24].
Arterial hyperenhancement is the most considerable feature in patients with HCC (Fig. 2) and is considered to be the most important feature for imaging diagnosis [25,26,27]. This feature reflects the neoangiogenesis, which is associated with the stepwise process of carcinogenesis and becomes the dominant blood supply in overt HCC lesions [16, 17].
Man 73 years old with typical HCC on VI hepatic segment. The HCC is hyperintense (arrow) on T2-W sequences (a), shows (arrows) restrict diffusion (b: b50 s/mm2, c: b800 s/mm2). After contrast medium injection, the nodule is hypervascular (arrow) on arterial phase (d), with wash-out appearance (arrow) on portal phase (e) and capsule appearance (arrow) on equilibrium phase (f) of contrast study with Gd-BT-DO3A
Washout appearance
Washout appearance is a reduction in contrast-enhancement relative to liver from an earlier to a later phase resulting in hypoenhancement in portal or delayed phase [28]. This may reflect multiple concomitant phenomena: rapid venous drainage, reduced portal venous supply and later enhancement of the background liver especially with hepatobiliary agents [28]. Jang et al. reported a variation in the timing of washout in the portal venous and delayed phases [29]. He reported, in a pilot study on enhancement of 112 histologically proven HCCs, that arterial phase hyperenhancement was present on 74 (77, 96%) and portal washout within 90 s on 72 (74, 97%) in the majority of moderately differentiated HCC. However, the authors found that well differentiated and poorly differentiated HCCs had an atypical enhancement patterns where 25 out of 97 (26%) showed washout between 91 and 180 s and 21 out of 97 (22%) showed late washout between 180 and 300 s [29]. Choi et al. [30] demonstrated as HCCs smaller than 1.5 cm showed typical features less frequently than HCCs 1.5 cm or larger in diameter. In subgroup analyses, HCCs with diameters between 1 and 1.5 cm showed similar MRI findings to HCCs with diameters 1 cm or less but significantly different findings compared with HCCs with diameters from 1.5 to 2 cm and 2–3 cm [31]. Portal or later hypoenhancement is considered a strong predictor of HCC, particularly when combined with arterial phase hyperenhancement [30]. Conversely Granito et al. [32] demonstrated that the most interesting result of their study was the finding of 8 HCC nodules, seven of which lacked the typical vascular pattern, which appeared as hypointense nodules on hepatobiliary phase with wash- out on portal phase, not preceded by arterial hyperenhancement (Fig. 3) [32]. This radiological pattern (wash-out and hypointense signal on hepatobiliary phase) could correspond to an early stage of carcinogenesis characterized by a reduction in both portal venous and arterial supplies [32]. The presence of wash out is a crucial step on LI-RADS decision tree for LR- 3–5 observations [1,2,3]. Becker et al. showed as the diameter and washout criteria using a step wise LI-RADS decision tree for LR- 3–5 observations allowed faster categorization with better inter-observer reliability while maintaining the excellent diagnostic accuracy of the most recent LI-RADS v2014 [33]. Fibrotic tissue in cirrhotic hepatic parenchyma typically shows hypointensity signal on portal or delayed phase of contrast study that may cause a false appearance of hypoenhancement of a regenerative nodule when these are surrounded by fibrosis. In some cases, fibrotic tissue may even mimic a delayed enhancing capsule or pseudocapsule [34].
Woman 73 years old with atypical HCC on VII-VIII hepatic segment. The HCC is hyperintense (arrow) on T2-W sequences (a) and hypointense (arrow) on T1-W sequences (b: out-of-phase). During arterial phase (c), it is not hypervascular (arrow), while there is wash-out appearance (arrow) and capsule appearance (arrow) on portal phase (d), on equilibrium phase (e) and hepatospecific phase (f) of contrast study
Capsule appearance
Capsule appearance is defined as a peripheral rim of smooth hyperenhancement in the portal or delayed phase (Fig. 3). The rim of enhancement is not always a true tumor capsule, but may represent a pseudocapsule corresponding to fibrous tissue and dilated sinusoids around a nodule [16, 17, 28]. Anis and coworkers showed as the capsule appearance has a high positive predictive value for HCC in at-risk patients [35]. Dioguardi Burgio et al. [36] showed as hyperintense capsule was present either on portal phase in 11/46 and in 24/25 HCCs imaged with gadoxetic acid and gadobenate dimeglumine-enhanced MR imaging, respectively (24 vs. 96%). A hypointense capsule appearance was present on hepatobiliary phase in 8/46 and 0/22 HCCs evaluated with gadoxetic acid and gadobenate dimeglumine-enhanced MR imaging, respectively (17 vs. 0%) [36]. Conversely to Dioguardi Burgio et al. that analyzed two different contrast media, Zhang et al. [37] compared diagnostic accuracy of CT and MRI to predicting of malignancy and showed that CT against MR produced false-negative findings of pseudo-capsule by 42.9% with an underestimated LI-RADS score by 16.9% for LR- 3, 37.3% for LR- 4, and 8.5% for LR- 5. CT produced significantly lower accuracy (54.3 versus 67.8%) and sensitivity (31.6 versus 71.1%) than MRI in the prediction of malignancy [37]. Also Corwin et al. [38] compared the diagnostic accuracy of CT respected to MR to grading LI-RADS. The most important finding of this study was that nearly half (42%) of observations were significantly upgraded on MRI compared with CT, and approximately one third of upgrades were to category 4, 5, or 5 V. The most common reason for the upgrade by MRI was the visualization of arterial hyperenhancement or a delayed enhancing capsule not seen on CT [38]. It is clear that these features should be correctly identified since they are major features on LI-RADS.
Hypointense signal on hepatobiliary phase
Hepatobiliary contrast agents are widely used in the evaluation of patients at high risk for HCC. GD-EOB-DTPA is a liver-specific agent, taken up by hepatocytes. It can be injected as an intravenous bolus, providing data about lesion vascularity in the different phases of contrast circulation. Additionally functional data can be obtained in the delayed, hepatobiliary phase [39]. Recently, the LI-RADS system incorporated the hepatobiliary phase appearance of observations as an ancillary feature that may be used to favor malignancy or benignity [40, 41]. Two ancillary features favoring malignancy on hepatobiliary phase include observation hypointensity, which is defined as the intensity of an observation lesser than the surrounding liver parenchyma, and hypointense rim, which is thought to correlate to a capsule (Fig. 4) [40, 41]. Conversely, iso-intensity of an observation to background liver favors benignity [41]; however, the study must have an adequate hepatobiliary phase, defined by LI-RADS as liver parenchyma being unequivocally hyperintense to the intrahepatic vessels. It has been demonstrated that the use of Gd-EOB-DTPA improves detection of HCC with higher sensitivity and specificity when compared to the studies with extracellular agents [40, 41]. Despites the advantages, there are also several limits. Hepatobiliary agents cost more than traditional extracellular contrast agents. Hepatobiliary agents have been associated with acute transient dyspnoea, independent of other patient risk factors [42, 43]. This dyspnoea occurs during the arterial phase imaging, therefore, degrading the study and limiting the evaluation for hepatic arterial hyperenhancement that is typical of HCC [42, 43]. Also the uptake of contrast medium by hepatocytes depends on function and the presence of membrane transporters, which are downregulated in the setting of cirrhosis [44,45,46]. Therefore, the utility of these agents may be clarified in patients with hepatic dysfunction. There have been several studies examining correlation of liver enhancement during the hepatobiliary phase with Child Pugh class, Model for End-stage Liver Disease (MELD) score, and various laboratory factors [47, 48]; however, no definitive cut-off values have been established for clinical parameters. As a suboptimal hepatobiliary phase would negate the advantage of these agents respect to extracellular agents [49]. Despite these limits several researches have demonstrated that EOB-GD-DTPA can favor the detection and the characterization of HCC nodule [50,51,52,53,54,55,56]. According to Golfieri et al. [53], during the hepatospecific phase, typical HCC and early HCC appear hypointense, whereas low-grade dysplastic or regenerative nodules appear as iso- or hyperintense lesions. The diagnostic accuracy of EOB-MRI for the diagnosis of early HCC is approximately 95–100% [53]. One third of hypovascular hypointense nodules in hepatospecific phase become hypervascular ‘progressed’ HCC, with a 1 and 3-year. Therefore, the authors suggested that these hypovascular nodules should be strictly followed up or definitely treated as typical HCC [53]. In the study by Ahn et al. [54], 9 out of 84 HCCs (10.7%) were exclusively identified by hepatospecific phase and three were early HCCs, while in Golfieri et al. [55] 19 out of 20 early HCC remained unclassified at dynamic MRI alone because of atypical behavior and were diagnosed only in the hepatospecific phase. Golfieri et al. [56], in a pilot study, suggested that in atypical cirrhotic nodule, hypointensity in the hepatospecific phase is the most relevant diagnostic sign for differentiating low-risk from high-risk nodules, since the reduction of Gd-EOB-DTPA uptake seems to occur at an early stage of hepatocarcinogenesis which precedes the reduction of portal blood flow and nodule arterialization [56]. In fact an experimental study showed a gradual loss of the ability of hepatocytes to take up Gd-EOB-DTPA during hepatocarcinogenesis, according to the progression from dysplastic nodules to poorly differentiated HCC [57]. However, several authors documented that 5–10% of human HCCs can show a paradoxical uptake of Gd-EOB-DTPA in the hepatobiliary phase, appearing as iso- or hyperintense, whereas some dysplastic nodules can exhibit hypointensity [58,59,60,61]. However, according to Golfieri et al. [56], for atypical HCC hepatospecific phase hypointensity should be used as the second marker of malignancy.
Woman 44 years old with multiple nodules of HCC. The nodules are hyperintense (arrow) on T2-W sequences (a), hypointense (arrow) on T1-W sequences (b: in-of-phase; c: out-of-phase), hypervascular (arrow) on arterial phase (d), with wash-out and capsule appearance (arrow) on portal phase (e) and hypointense signal (arrow) on hepatospecific phase (f) of contrast study with EOB-GD-DTPA
T2-W Hyperintensity
According to LI-RADS, T2-W hyperintensity is an ancillary imaging features (Fig. 5). Park et al. [17] showed that dysplastic nodules and HCCs cannot be distinguished on the basis of signal intensity characteristics on unenhanced MRI, since their signal intensities are similar on T1- and T2-W sequences. However, dysplastic nodules are almost never hyperintense on T2-W, early HCCs are mostly isointense on T2-W, while higher grade (moderately or poorly) of HCC is associated with high signal intensity on T2-W images, although the signal intensity may also be related with tumor vascularity and peliotic changes [17]. Previous study demonstrated that T2-W hyperintensity was a highly specific marker of nodule malignancy, although poorly sensitive [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62]. Golfieri et al. [56] showed that, compared to hypointensy on hepatospecific phase, T2-W hyperintensity was a poor predictor of malignancy in the early stages of HCC. Conversely to Golfieri [56], Ouedraogo et al. [63] demonstrated that the addition of T2-W hyperintensity to the AASLD criteria increased the detection rate of HCC, especially nodules smaller than 20 mm. In fact the sensitivity of MRI increased from 67.6 to 79%. Sofue et al. [64] evaluated the imaging features in MRI that are associated with upgrade of LI-RADS category observations to category 5, and demonstrated that the risk factors in the 56 LR-4 observations that upgraded to LR-5 were mild-moderate T2 hyperintensity (P < 0.001; hazard ratio = 1.84) and growth (P < 0.001; hazard ratio = 3.71). Although mild-moderate T2 hyperintensity was the most useful risk factor for predicting upgrade, actual risk level was only mildly elevated. Hwang et al. [65] compared the diagnostic performance of DWI and T2-W images, in differentiating between hypovascular HCC and dysplastic nodules seen as hypointense nodules at hepatobiliary phase. They showed that hyperintensity on T2-W and DWI were significant features for differentiating hypovascular HCCs from dysplastic nodules (P < 0.05), while there was no significant difference in mean ADC between hypovascular HCCs (1.06 ± 0.13) and dysplastic nodules (1.09 ± 0.13). The sensitivity of DWI was higher than T2-W (72.0% [18 of 25] versus 40.0% [10 of 25]). Hyperintensity on T2-W and DWI could be a useful imaging tool to differentiate hypovascular HCCs from dysplastic nodules seen as hypointense nodules in the hepatobiliary phase. Kim et al. [66] evaluated the most predictive finding among hyperintensity on T2-W, DWI, washout, capsular enhancement, and hypointensity on gadoxetic acid-enhanced hepatobiliary phase images in the detailed characterization of arterial phase enhancing nodules 1 cm in diameter and smaller. They showed that for hypervascular lesions 1 cm in diameter or smaller, T2-weighted images have the highest sensitivity among tests with an odds ratio statistically separable from 1 for differentiating HCC from benign hypervascular lesions 1 cm or smaller. Conversely Hussain et al. [67] concluded that T2-W images do not provide added diagnostic value in the detection and characterization of focal lesions because the heterogeneity and hyperintense fibrotic septa in the cirrhotic liver parenchyma can obscure moderately hyperintense HCC on T2-W images and that 42–53% of HCCs may be isointense to hypointense on T2-weighted images. Other researches also have reported that the combined use of hyperintensity on T2-W images improves differentiation of small non solid benign lesions from solid malignant tumors in the liver [68, 69].
Man 74 years old with HCC on II hepatic segment. The HCC is hyperintense (arrow) on T2-W sequence (a), isointense (arrow) on T1-W (b: in-of-phase) with peripheral fat suppression (arrow) on T1-out of phase (c). During arterial phase of contrast study (d) with EOB-GD-DTPA, the HCC shows hyperenhancement (arrow), with wash-out and capsule appearance (arrow) on portal phase (e). During hepatospecific phase (f) of contrast study the HCC is hypointense (arrow)
Restricted diffusion
The role of DWI in HCC patient has been evaluated by different studies [70,71,72,73,74,75,76]. Lee et al. [72] demonstrated that the addition of DWI to the gadoxetic acid-enhanced MRI could be a guideline in differentiating between HCCs and dysplastic nodules. In their study, 86 HCCs (84.3%) showed hyperintensity on DWI, whereas only three dysplastic nodules (13.0%) showed this feature. So they concluded that hyperintensity on DWI was highly indicative of HCC in patients with chronic hepatitis or cirrhosis. Also Piana et al. [73] showed that enhancement in the arterial phase and hyperintensity on DWI were found to be significantly more sensitive criteria for HCC than conventional criteria (77–76 vs. 60% for all HCCs and 66–60 vs. 37% for HCCs smaller than 20 mm). Sensitivity was even higher when enhancement in the arterial-dominant phase and washout (in the portal venous and/or equilibrium phases) or hyperintensity on DWI was used (84–85% for all HCCs and 71–74% for HCCs smaller than 20 mm). Granata et al. [74] demonstrated that that DWI could be used to predict the histological grade of HCC; in fact they found that there was a good correlation between ADC and grading, between perfusion fraction (fp) and grading, and between tissue pure diffusivity (Dt) and grading. Nakanishi et al. [75] showed not only the usefulness of DWI for histological grading, but also the possibility to use ADC as a preoperative prediction of early HCC recurrence within 6 months of operation. Conversely, Nasu et al., in a series of 125 resected HCCs (sizes range: 0.8–15 cm), found no correlation between histological grade and ADC (using b factors of 0 and 500 s/mm2), although the DWI and Signal Intensity of the HCCs increased in higher grade [76]. Sutherland et al. [77] compared ultrasound screening with DWI for detecting HCC. The sensitivity, specificity, positive predictive value and negative predictive values for US were 100, 90, 23 and 100%, respectively, while for MRI were 83, 98, 63 and 99%. The major advantage of DWI over US screening in this study has been the low false-positive rate of DWI. In fact US had false-positive studies 20 times (10%) while DWI had three false-positive examinations (2%). The reasons for the low false-positive rate of DWI include: not depicting macro regenerative and low grade dysplastic nodules and not depicting focal fatty heterogeneity, also the ability to correctly classify benign nodules as cavernous haemangiomas which usually have elevated apparent diffusion coefficient (ADC) values. They concluded that more studies are needed to validate the DWI as a screening tool and therefore it should replace US as a cost-effective screening tool [77]. DWI could be used as a helpful diagnostic tool for HCC in patients with chronic liver disease, since DWI can accurately detect HCC in patients with chronic liver disease regardless of the lesion size (Fig. 6). A potential reason for the better accuracy of DWI is that this does not rely on morphologic features only. Malignant tissues tend to be hypercellular with an accumulation of macromolecular proteins leaving a small extracellular space resulting in a decrease of the ADC value [78]. The major limits of DWI are the different parameters used in DWI sequences which may affect the results of ADC calculation. The different b values, selection method, bias of patient selection, pathological characteristic of lesions and measurement of ADC values may be reduced the reproducibility of the data, however all analyzed studies showed that the mean ADC value of malignant lesions was lower than that of benign lesions [70,71,72,73,74,75,76,77,78,79,80].
The same patient of Fig. 5. Restricted diffusion. The nodule (arrow) shows hyperintense signal on b0 s/mm2 (a), on b 500 s/mm2 (b) and on b 800 s/mm2(c)
Other ancillary features (intalesional fat, corona enhancement, mosaic architecture and iron sparing in iron overloaded)
MR imaging diagnosis of HCC is based mainly on assessment of vascularity, capsule appearance, and signal intensity in the hepatobiliary phase. MR imaging also permit assessment of ancillary imaging features, that can be divided into those that favor the diagnosis of HCC specifically (intralesional fat, corona enhancement, nodule-in-nodule architecture, and mosaic architecture) and those that favor the diagnosis of malignancy but are not specific for HCC (mild-moderate T2 hyperintensity, restricted diffusion, and lesional iron sparing) [5,6,7, 81].
Intralesional fat is the presence of lipid within a nodule in higher concentration than in the hepatic parenchyma [6]. This feature can be detected at MR by observing signal loss on out-of-phase compared with in-phase T1-weighted GRE images. In a patient at risk for HCC, the detection of intralesional fat in a solid nodule raises concern for malignancy or premalignancy. In fact, this feature does not establish the diagnosis of HCC, however, as the differential diagnosis includes high-grade dysplastic nodule and occasionally low-grade dysplastic nodule [82].
Corona enhancement is a feature of hypervascular, progressed HCC and refers to enhancement of the venous drainage area in the peritumoral parenchyma [16]. It is as a rim (“corona”) of enhancement around a progressed, hypervascular HCC in the late arterial phase or early portal venous phase, with fading to isoenhancement at subsequent phases. This feature begins a few seconds after tumor enhancement, so that corona and tumor enhancement may appear to overlap. This overlap may cause the tumor to appear larger than it really is. Its presence helps to differentiate small hypervascular HCCs from pseudolesions, however it is not a feature of early HCC [16, 82].
Mosaic architecture refers to the presence within a mass of randomly distributed internal nodules differing in enhancement, intensity, often separated by fibrous septa. This feature is characteristic of large HCCs and reflects the mosaic configuration observed at pathologic evaluation. It is unusual in tumors other than HCC [82].
Lesional iron sparing refers to relative paucity of iron in a solid mass compared with that of background iron-overloaded liver. This feature raises concern for premalignancy or malignancy because high-grade dysplastic nodules and HCCs characteristically are iron “resistant”. However it is not specific for high-grade dysplastic nodule or HCC, but other non-HCC malignancies may have this appearance [82].
Conclusion
Early diagnosis is a critical step in the management of HCC patients. The identification of the specific vascular profile characterized by contrast arterial uptake followed by washout in the venous phases has 100% specificity when demonstrated on dynamic contrast study, in patients at high risk of HCC. Although the arterial phase hyperenhancement is an essential prerequisite for definitely HCC, it is not sufficient for LR-5 categorization. Hypointensity on hepatospecific phase and wash-out appearance are the most relevant diagnostic sign for differentiating low-risk from high-risk nodules in patients at risk for HCC. Therefore the use of EOB-GD-DTPA should be considered in this category of patients. The capsule appearance, T2-W hyperintensity and restricted diffusion have a high positive predictive value for HCC and may be associated to other imaging features for LIRADS characterization.
References
Bruix J, Sherman M. Management of hepatocellular carcinoma: An update. Hepatology. 2011;53:1020–2.
Izzo F, Albino V, Palaia R, et al. Hepatocellular carcinoma: preclinical data on a dual-lumen catheter kit for fibrin sealant infusion following loco-regional treatments. Infect Agent Cancer. 2014;9(1):39.
NCCN Clinical Practice Guidelines in Oncology on hepatobiliary cancer. Version 2016. http://www.nccn.org.
European Association for Study of Liver. European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. Eur J Cancer. 2012;48(5):599–641. doi:10.1016/j.ejca.2011.12.021. Erratum in: Eur J Cancer. 2012 May; 48(8): 1255–6.
An C, Rakhmonova G, Choi JY, et al. Liver imaging reporting and data system (LI-RADS) version 2014: understanding and application of the diagnostic algorithm. Clin Mol Hepatol. 2016;22(2):296–307.
American College of Radiology. Liver Imaging Reporting and Data System Version 2014. ACR Web site < http://www.acr.org/Quality-Safety/Resources/LIRADS >. Accessed 15 Apr 2016.
Santillan CS, Tang A, Cruite I, et al. Understanding LI-RADS: a primer for practical use. Magn Reson Imaging Clin N Am. 2014;22:337–52.
Schima W, Ba-Ssalamah A, Kurtaran A, et al. Post-treatment imaging of liver tumours. Cancer Imaging. 2007;7(Spec No A):S28–36.
Granata V, Petrillo M, Fusco R, et al. Surveillance of HCC Patients after Liver RFA: Role of MRI with Hepatospecific Contrast versus Three-Phase CT Scan-Experience of High Volume Oncologic Institute. Gastroenterol Res Pract. 2013;2013:469097.
Neri E, Bali MA, Ba-Ssalamah A, et al. ESGAR consensus statement on liver MR imaging and clinical use of liver-specific contrast agents. Eur Radiol. 2016;26:921–31.
Granata V, de Lutio di Castelguidone E, Fusco R, et al. Irreversible electroporation of hepatocellular carcinoma: preliminary report on the diagnostic accuracy of magnetic resonance, computer tomography, and contrast-enhanced ultrasound in evaluation of the ablated area. Radiol Med. 2016;121(2):122–31.
Prince MR, Zhang H, Zou Z, et al. Incidence of immediate gadolinium contrast media reactions. AJR Am J Roentgenol. 2011;196(2):W138–43.
Izzo F, Palaia R, Albino V, et al. S. Hepatocellular carcinoma and liver metastases: clinical data on a new dual-lumen catheter kit for surgical sealant infusion to prevent perihepatic bleeding and dissemination of cancer cells following biopsy and loco-regional treatments. Infect Agent Cancer. 2015;10:11.
Granata V, Fusco R, Catalano O, et al. Percutaneous ablation therapy of hepatocellular carcinoma with irreversible electroporation: MRI findings. AJR Am J Roentgenol. 2015;204(5):1000–7.
Forner A, Vilana R, Ayuso C, et al. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: Prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology. 2008;47:97–104.
Matsui O, Kobayashi S, Sanada J, et al. Hepatocelluar nodules in liver cirrhosis: hemodynamic evaluation (angiography-assisted CT) with special reference to multi-step hepatocarcinogenesis. Abdom Imaging. 2011;36(3):264–72.
Park YN, Kim MJ. Hepatocarcinogenesis: imaging-pathologic correlation. Abdom Imaging. 2011;36:232–43.
Holland AE, Hecht EM, Hahn WY, et al. Importance of small (< or = 20-mm) enhancing lesions seen only during the hepatic arterial phase at MR imaging of the cirrhotic liver: evaluation and comparison with whole explanted liver. Radiology. 2005;237(3):938–44.
Kim TK, Lee KH, Jang HJ, et al. K. Analysis of gadobenate dimeglumine-enhanced MR findings for characterizing small (1-2-cm) hepatic nodules in patients at high risk for hepatocellular carcinoma. Radiology. 2011;259(3):730–8.
Ehman EC, Behr SC, Umetsu SE, et al. Rate of observation and inter-observer agreement for LI-RADS major features at CT and MRI in 184 pathology proven hepatocellular carcinomas. Abdom Radiol (NY). 2016;41(5):963–9.
Burrel M, Llovet JM, Ayuso C, et al. Barcelona Clínic Liver Cancer Group. MRI angiography is superior to helical CT for detection of HCC prior to live transplantation: an explant correlation. Hepatology. 2003;38(4):1034–42.
Brancatelli G, Baron RL, Peterson MS, et al. Helical CT screening for hepatocellular carcinoma in patients with cirrhosis: frequency and causes of false-positive interpretation. AJR Am J Roentgenol. 2003;180(4):1007–14.
Yu JS, Kim KW, Jeong MG, et al. Non- tumorous hepatic arterial-portal venous shunts: MR imaging findings. Radiology. 2000;217(3):750–6.
Colagrande S, Centi N, Galdiero R, et al. Transient hepatic intensity differences. 1. Those associated with focal lesions. AJR Am J Roentgenol. 2007;188(1):154–9.
Sharma P, Kalb B, Kitajima HD, et al. Optimization of single injection liver arterial phase gadolinium enhanced MRI using bolus track real-time imaging. J Magn Reson Imaging. 2011;33(1):110–8.
Hecht EM, Holland AE, Israel GM, et al. Hepatocellular carcinoma in the cirrhotic liver: gadolinium-enhanced 3D T1-weighted MR imaging as a stand-alone sequence for diagnosis. Radiology. 2006;239(2):438–47.
Willatt JM, Hussain HK, Adusumilli S, Marrero JA. MR imaging of hepatocellular carcinoma in the cirrhotic liver: challenges and controversies. Radiology. 2008;247(2):311–30.
Efremidis SC, Hytiroglou P. The multistep process of hepatocarcinogenesis in cirrhosis with imaging correlation. Eur Radiol. 2002;12:753–64.
Jang HJ, Kim TK, Burns PN, Wilson SR. Enhancement patterns of hepatocellular carcinoma at contrast-enhanced US: comparison with histologic differentiation. Radiology. 2007;244(3):898–906.
Marrero JA, Hussain HK, Nghiem HV, et al. Improving the prediction of hepatocellular carcinoma in cirrhotic patients with an arterially-enhancing liver mass. Liver Transpl. 2005;11(3):281–9.
Choi MH, Choi JI, Lee YJ, et al. MRI of Small Hepatocellular Carcinoma: Typical Features Are Less Frequent Below a Size Cutoff of 1.5 cm. AJR Am J Roentgenol. 2016;27:1–8.
Granito A, Galassi M, Piscaglia F, et al. Impact of gadoxetic acid (Gd-EOB-DTPA)-enhanced magnetic resonance on the non-invasive diagnosis of small hepatocellular carcinoma: a prospective study. Aliment Pharmacol Ther. 2013;37(3):355–63.
Becker AS, Barth BK, Marquez PH, et al. Increased interreader agreement in diagnosis of hepatocellular carcinoma using an adapted LI-RADS algorithm. Eur J Radiol. 2017;86:33–40.
Fowler KJ, Brown JJ, Narra VR. Magnetic resonance imaging of focal liver lesions: approach to imaging diagnosis. Hepatology. 2011;54(6):2227–37.
Anis M. Imaging of hepatocellular carcinoma: new approaches to diagnosis. Clin Liver Dis. 2015;19(2):325–40.
Dioguardi Burgio M, Picone D, Cabibbo G, et al. MR-imaging features of hepatocellular carcinoma capsule appearance in cirrhotic liver: comparison of gadoxetic acid and gadobenate dimeglumine. Abdom Radiol (NY). 2016;41(8):1546–54.
Zhang YD, Zhu FP, Xu X, et al. Liver Imaging Reporting and Data System: Substantial Discordance Between CT and MR for Imaging Classification of Hepatic Nodules. Acad Radiol. 2016;23(3):344–52.
Corwin MT, Fananapazir G, Jin M, et al. Differences in Liver Imaging and Reporting Data System Categorization Between MRI and CT. AJR Am J Roentgenol. 2016;206(2):307–12.
Granata V, Cascella M, Fusco R, et al. Immediate adverse reactions to gadolinium-based MR contrast media: a retrospective analysis on 10,608 examinations. Biomed Res Int. 2016;2016:3918292.
Hope TA, Fowler KJ, Sirlin CB, et al. Hepatobiliary agents and their role in LI-RADS. Abdom Imaging. 2015;40(3):613e25.
Ahn SS, Kim MJ, Lim JS, et al. Added value of gadoxetic acid-enhanced hepatobiliary phase MR imaging in the diagnosis of hepatocellular carcinoma. Radiology. 2010;255(2):459e66.
Davenport MS, Viglianti BL, Al-Hawary MM, et al. Comparison of acute transient dyspnea after intravenous administration of gadoxetate disodium and gadobenate dimeglumine: effect on arterial phase image quality. Radiology. 2013;266(2):452e61.
Kim SY, Park SH, Wu EH, et al. Transient respiratory motion artifact during arterial phase MRI with gadoxetate disodium: risk factor analyses. AJR Am J Roentgenol. 2015;204(6):1220e7.
Tsuda N, Harada K, Matsui O. Effect of change in transporter expression on gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging during hepatocarcinogenesis in rats. J Gastroenterol Hepatol. 2011;26(3):568e76.
Kim T, Murakami T, Hasuike Y, et al. Experimental hepatic dysfunction: evaluation by MRI with Gd-EOB-DTPA. J Magn Reson Imaging. 1997;7(4):683e8.
Nassif A, Jia J, Keiser M, et al. Visualization of hepatic uptake transporter function in healthy subjects by using gadoxetic acid-enhanced MR imaging. Radiology. 2012;264(3):741e50.
Kim H, Kim MJ, Park MS, et al. Potential conditions causing impairment of selective hepatobiliary enhancement of gadobenate dimeglumine-enhanced delayed magnetic resonance imaging. J Comput Assist Tomogr. 2010;34(1):113e20.
Chernyak V, Kim J, Rozenblit AM, et al. Hepatic enhancement during the hepatobiliary phase after gadoxetate disodium administration in patients with chronic liver disease: the role of laboratory factors. J Magn Reson Imaging. 2011;34(2):301e9.
Esterson YB, Flusberg M, Oh S, et al. Improved parenchymal liver enhancement with extended delay on Gd-EOB-DTPA-enhanced MRI in patients with parenchymal liver disease: associated clinical and imaging factors. Clin Radiol. 2015;70(7):723e9.
Tong HF, Liang HB, Mo ZK, et al. Quantitative analysis of gadoxetic acid-enhanced magnetic resonance imaging predicts histological grade of hepatocellular carcinoma. Clin Imaging. 2017;43:9–14.
Jeon I, Cho ES, Kim JH, et al. Feasibility of 10-Minute Delayed Hepatocyte Phase Imaging Using a 30° Flip Angle in Gd-EOB-DTPA-Enhanced Liver MRI for the Detection of Hepatocellular Carcinoma in Patients with Chronic Hepatitis or Cirrhosis. PLoS One. 2016;11(12):e0167701.
Toyoda H, Kumada T, Tada T, et al. Non-hypervascular hypointense nodules on Gd-EOB-DTPA-enhanced MRI as a predictor of outcomes for early-stage HCC. Hepatol Int. 2015;9(1):84–92.
Golfieri R, Garzillo G, Ascanio S, Renzulli M. Focal lesions in the cirrhotic liver: their pivotal role in gadoxetic acid-enhanced MRI and recognition by the Western guidelines. Dig Dis. 2014;32(6):696–704.
Ahn SS, Kim MJ, Lim JS, et al. Added value of gadoxetic acid-enhanced hepatobiliary phase MR imaging in the diagnosis of hepatocellular carcinoma. Radiology. 2010;255:459–66.
Golfieri R, Renzulli M, Lucidi V, et al. Contribution of the hepatobiliary phase of Gd-EOB-DTPA-enhanced MRI to Dynamic MRI in the detection of hypovascular small (≤2 cm) HCC in cirrhosis. Eur Radiol. 2011;21(6):1233–42.
Golfieri R, Grazioli L, Orlando E, et al. Which is the best MRI marker of malignancy for atypical cirrhotic nodules: hypointensity in hepatobiliary phase alone or combined with other features? Classification after Gd-EOB-DTPA administration. J Magn Reson Imaging. 2012;36(3):648–57.
Tsuda N, Kato N, Murayama C, et al. Potential for differential diagnosis with gadolinium- ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging in experimental hepatic tumors. Invest Radiol. 2004;39:80–8.
Huppertz A, Haraida S, Kraus A, et al. Enhancement of focal liver lesions at gadoxetic acid-enhanced MR imaging: correlation with histopathologic findings and spiral CT-initial observations. Radiology. 2005;234:468–78.
Saito K, Kotake F, Ito N, et al. Gd- EOB-DTPA enhanced MRI for hepatocellular carcinoma: quantitative evaluation of tumor enhancement in hepatobiliary phase. Magn Reson Med Sci. 2005;4:1–9.
Lee SA, Lee CH, Jung WY, et al. Paradoxical high signal intensity of hepatocellular carcinoma in the hepatobiliary phase of Gd-EOB- DTPA enhanced MRI: initial experience. Magn Reson Imaging. 2011;29:83–90.
Kudo M. Will Gd-EOB-MRI change the diagnostic algorithm in hepatocellular carcinoma? Oncology. 2010;78 Suppl 1:87–93.
Kim JI, Lee JM, Choi JY, et al. The value of gadobenate dimeglumine-enhanced delayed phase MR imaging for characterization of hepatocellular nodules in the cirrhotic liver. Invest Radiol. 2008;43:202–10.
Ouedraogo W, Tran-Van Nhieu J, et al. Evaluation of noninvasive diagnostic criteria for hepatocellular carcinoma on pretransplant MRI (2010): correlation between MR imaging features and histological features on liver specimen]. J Radiol. 2011;92(7–8):688–700.
Sofue K, Burke LM, Nilmini V, et al. Liver imaging reporting and data system category 4 observations in MRI: Risk factors predicting upgrade to category 5. J Magn Reson Imaging. 2017. doi:10.1002/jmri.25627.
Hwang J, Kim YK, Jeong WK, et al. Nonhypervascular Hypointense Nodules at Gadoxetic Acid-enhanced MR Imaging in Chronic Liver Disease: Diffusion-weighted Imaging for Characterization. Radiology. 2015;276(1):137–46.
Kim JE, Kim SH, Lee SJ, Rhim H. Hypervascular hepatocellular carcinoma 1 cm or smaller in patients with chronic liver disease: characterization with gadoxetic acid-enhanced MRI that includes diffusion-weighted imaging. AJR Am J Roentgenol. 2011;196(6):W758–65.
Hussain HK, Syed I, Nghiem HV, et al. T2- weighted MR imaging in the assessment of cirrhotic liver. Radiology. 2004;230:637–44.
Kim YK, Lee YH, Kim CS, Han YM. Added diagnostic value of T2-weighted MR imaging to gadolinium-enhanced three-dimensional dynamic MR imaging for the detection of small hepatocel- lular carcinomas. Eur J Radiol. 2008;67:304–10.
Brancatelli G, Federle MP, Blachar A, Grazioli L. Hemangioma in the cirrhotic liver: diagnosis and natural history. Radiology. 2001;219:69–74.
Shankar S, Kalra N, Bhatia A, et al. Role of Diffusion Weighted Imaging (DWI) for Hepatocellular Carcinoma (HCC) Detection and its Grading on 3 T MRI: A Prospective Study. J Clin Exp Hepatol. 2016;6(4):303–10.
Xu PJ, Yan FH, Wang JH, et al. Contribution of diffusion-weighted magnetic resonance imaging in the characterization of hepatocellular carcinomas and dysplastic nodules in cirrhotic liver. J Comput Assist Tomogr. 2010;34(4):506–12.
Lee MH, Kim SH, Park MJ, et al. Gadoxetic acid-enhanced hepatobiliary phase MRI and high-b-value diffusion-weighted imaging to distinguish well-differentiated hepatocellular carcinomas from benign nodules in patients with chronic liver disease. AJR Am J Roentgenol. 2011;197(5):W868–75.
Piana G, Trinquart L, Meskine N, et al. New MR imaging criteria with a diffusion-weighted sequence for the diagnosis of hepatocellular carcinoma in chronic liver diseases. J Hepatol. 2011;55:126–32.
Granata V, Fusco R, Catalano O, et al. Intravoxel incoherent motion (IVIM) in diffusion-weighted imaging (DWI) for Hepatocellular carcinoma: correlation with histologic grade. Oncotarget. 2016;7(48):79357–64.
Nakanishi M, Chuma M, Hige S, et al. Relationship between diffusion-weighted magnetic resonance imaging and histological tumor grading of hepatocellular carcinoma. Ann Surg Oncol. 2012;19(4):1302–9.
Nasu K, Kuroki Y, Tsukamoto T, et al. Diffusion-weighted imaging of surgically resected hepatocellular carcinoma: imaging characteristics and relationship among signal intensity, apparent diffusion coefficient, and histopathologic grade. AJR Am J Roentgenol. 2009;193:438–44.
Sutherland T, Watts J, Ryan M, et al. Diffusion-weighted MRI for hepatocellular carcinoma screening in chronic liver disease: Direct comparison with ultrasound screening. J Med Imaging Radiat Oncol. 2017;61(1):34–9.
Koh D, Collins DJ. Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol. 2007;188:1622–35.
Scialpi M, Palumbo B, Pierotti L, et al. Detection and characterization of focal liver lesions by split-bolus multidetector-row CT: diagnostic accuracy and radiation dose in oncologic patients. Anticancer Res. 2014;34(8):4335–44.
Sforza V, Martinelli E, Ciardiello F, et al. Mechanisms of resistance to anti-epidermal growth factor receptor inhibitors in metastatic colorectal cancer. World J Gastroenterol. 2016;22(28):6345–61.
Granata V, Fusco R, Avallone A, Filice F, Tatangelo F, Piccirillo M, Grassi R, Izzo F, Petrillo A. Critical analysis of the major and ancillary imaging features of LI-RADS on 127 proven HCCs evaluated with functional and morphological MRI: Lights and shadows. Oncotarget. 2017. doi:10.18632/oncotarget.17227.
Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology. 2014;273(1):30–50.
Acknowledgements
The authors are grateful to Alessandra Trocino, librarian at the National Cancer Institute of Naples, Italy. Moreover, for the collaboration, authors are grateful to Maria Bruno, Laura Galeani, Rita Guarino, Leandro Eto and Assunta Zazzaro.
Funding
Not applicable.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Authors’ contributions
VG conceived of the study, and participated in its design, coordination and drafting of the manuscript. RF participated in the studies collection and drafted the manuscript. AA, OC, FF, ML, RP, FI, AP participated in the studies collection. All authors read and approved the final manuscript.
Competing interests
The authors have no conflict of interest to be disclosed. The authors confirm that the article is not under consideration for publication elsewhere. Each author has participated sufficiently to take public responsibility for the manuscript content.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Granata, V., Fusco, R., Avallone, A. et al. Major and ancillary magnetic resonance features of LI-RADS to assess HCC: an overview and update. Infect Agents Cancer 12, 23 (2017). https://doi.org/10.1186/s13027-017-0132-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13027-017-0132-y