Abstract
Background
Wolfram syndrome is a rare genetic, progressive, neurodegenerative disorder characterised by childhood-onset diabetes mellitus, diabetes insipidus, optic atrophy and deafness. To date, the economic burden of Wolfram syndrome has not been well-studied or reported. The aim of this study was to evaluate the cost of illness (COI) of all people with Wolfram syndrome in the UK and to identify major determinants of cost from a service provider perspective (National Health Service, NHS).
Methods
A prevalence-based approach was used to model the UK Wolfram syndrome specialist service. Model inputs were informed by a pragmatic literature review and UK reference costs, in conjunction with patient interviews and expert opinion. A deterministic sensitivity analysis (DSA) was run at 10% to identify major cost drivers.
Results
The total COI of all people with Wolfram syndrome to the NHS was £1,055,899 per year, with an average annual cost per person with Wolfram syndrome of £16,498. Costs associated with diabetes mellitus care, late-stage diabetes mellitus complications and hearing impairment contributed most to the COI (18.9, 21.4 and 15.8% of the COI, respectively). The DSA identified costs associated with hearing impairment, diabetes mellitus care and end-stage renal disease (a diabetes mellitus complication) as major model drivers.
Conclusions
The annual cost of Wolfram syndrome to the NHS was found to be substantial, with areas of potential cost savings identified, such as diabetes mellitus management. This model provides crucial information to facilitate economic evaluation of prospective therapies for this disease.
Similar content being viewed by others
Background
Wolfram syndrome is a rare, progressive, neurodegenerative disorder with an estimated UK prevalence of 1 in every 770,000 individuals [1]. This multisystem disease is characterised by 4 hallmark features: diabetes insipidus (DI), diabetes mellitus (DM), optic atrophy (OA) and deafness (D). These features give Wolfram syndrome its alternative name, DIDMOAD [2]. In addition to these hallmark DIDMOAD symptoms, patients often manifest a number of other symptoms, including psychiatric problems and neurologic abnormalities [2, 3].
Wolfram syndrome is a recessive genetic disorder, with two genetic types. People with Wolfram syndrome type 1 comprise almost all Wolfram syndrome cases. In these individuals, Wolfram syndrome is caused by mutations in the WFS1 gene [1], which encodes the protein wolframin. Wolframin has many roles in the regulation of cellular processes such as cell death, protein folding and insulin production, and is a regulator of the unfolded protein response and endoplasmic reticulum calcium homeostasis [1]. A small number of Wolfram syndrome patients have Wolfram syndrome type 2, which is caused by mutations in the CISD2 gene [1]. This gene encodes a protein found in the outer membrane of mitochondria [1]. Wolfram syndrome type 2 is prevalent in a distinct founder population in Jordan, who suffer similar symptoms to people with WFS1 mutations, but with upper gastrointestinal ulcers and a bleeding disorder rather than DI and psychiatric disorders [2].
Individuals with Wolfram syndrome typically present with one or more of the main DIDMOAD symptoms, and diagnosis is confirmed by genetic testing of the WFS1 gene; the CISD2 mutation is not commonly screened for [1]. Typically, the earliest symptom is childhood-onset DM from age 6, followed by OA from age 11 and blindness by age 18–19 [2, 3]. The life expectancy of people with Wolfram syndrome was thought to be only 30 years; however, it is now known that some individuals live well into middle age [2, 4]. Data from the National Health Service (NHS) England highly specialised multidisciplinary service for Wolfram syndrome show that the median age of adults attending the specialised service is 37 years, with the oldest patient being 62 years. Death is commonly due to neurodegenerative atrophy of the brain stem [5, 6].
At present, there is no cure or disease-modifying treatment for Wolfram syndrome; the focus is only on the management of symptoms through existing treatments. NHS England highly specialised multidisciplinary services for Wolfram syndrome (paediatric and adults) are available at specialist centres in Birmingham, UK (Birmingham Women’s and Children’s Hospital and Queen Elizabeth Hospital, respectively). These specialist services allow monitoring of disease progression, provision of treatments, advice regarding symptom management and participation in registry studies and clinical trials.
To date, the economic burden of Wolfram syndrome has not been well-studied or reported. As yet, there are no published cost of illness (COI) studies investigating Wolfram syndrome. Such studies are an important first step in understanding the current resource use and to inform the UK’s NHS resource allocation. COI studies can be a valuable addition to the evidence base in rare and neglected genetic conditions, and help to provide support for the research of new treatments.
The purpose of this study was to estimate the COI of Wolfram syndrome to the NHS and Personal Social Services, based on the treatment pathway followed by patients receiving NHS care, typically at the specialist centres for children and adults in Birmingham. The key cost and clinical inputs of the model are highlighted and the factors leading to the largest contribution to annual costs are discussed.
Methods
A COI model was developed in Microsoft Excel® 2016 (Microsoft, Redmond, Washington) to calculate the annual direct costs to the NHS and Personal Social Services incurred by all individuals diagnosed with Wolfram syndrome in the UK at the time of the model development. A prevalence-based approach was used to estimate the annual cost associated with the diagnosis of Wolfram syndrome, the treatment of Wolfram syndrome symptoms and the running of the Wolfram syndrome specialist services at the Birmingham Children’s Hospital and Queen Elizabeth Hospital.
The treatment pathway was divided into diagnosis and referral processes, running of specialist services and treatment of symptom groups (Fig. 1). The typical ‘per person with Wolfram syndrome cost’ for each of these resources was calculated by multiplying the expected resource use with the unit cost. Resource use was defined as the use of healthcare staff time, facilities, or consumables such as medicines. The unit cost refers to the cost per ‘unit’ of resource, e.g. the cost per consultation, cost per hour of nursing time, cost per blood test or cost per box of medicine. The ‘per person with Wolfram syndrome cost’ was then multiplied by the number of individuals expected to require the resource in question, with the expected service utilisation based on the age group distribution of affected individuals and the symptoms expected in each age group. The number of patients expected to have a particular symptom was estimated by excluding any patients younger than the median age of symptom onset. The total COI was calculated by summing costs for each service, i.e. diagnosis and referral, specialist services and treatment of symptom groups.
Model inputs
Clinical inputs, such as the number of children and adults diagnosed with Wolfram syndrome and the age distribution of Wolfram syndrome patients, were sourced from published literature, routine data from Wolfram specialist centres and clinical experts (Table 1 and Fig. 2) [2,3,4, 7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30].
Based on routine records from the Birmingham Children’s Hospital, there were at least 64 individuals diagnosed with Wolfram syndrome at the time of the COI model development. Nine further paediatric patients are expected to be newly diagnosed and seen at the specialist centre at Birmingham Children’s Hospital annually. Each year, 15 paediatric patients and 14 adult patients are seen as follow-up patients at specialist clinics. In addition, 7 previously diagnosed paediatric patients are expected to transition to adult services at the specialist centre at Queen Elizabeth Hospital each year. These numbers are averages based on audit data for patients seen at Wolfram syndrome specialist clinics from March 2014 to November 2015. Individuals in the UK are typically diagnosed with Wolfram syndrome type 1 and thus individuals with Wolfram syndrome type 2 were not considered in this model.
The services and resource use required for diagnosis, annual review and management of symptoms were obtained from published literature, as well as clinical experts from the specialist Wolfram centre at Birmingham Children’s Hospital (Table 2). Unit costs were derived from NHS Reference Costs (2015-16) [19], British National Formulary (BNF, 2016) [14], Personal Social Services Research Unit 2016 [25] and the literature. A small number of unit cost inputs were estimated from expert opinion (Professor Timothy Barrett) in the absence of published inputs. All clinical inputs were verified by clinical experts at the specialist Wolfram centre at Birmingham Children’s Hospital. Feedback from these experts was obtained via face-to-face meetings and questionnaire completion. Where applicable, all costs were inflated to correspond to 2016 costs. Wolfram syndrome and its associated treatments were assumed to have no effect on mortality: a mortality rate of 0% was applied to all patients and procedures.
Deterministic sensitivity analysis
A univariate DSA was carried out to assess the sensitivity of the model results to variations in each of the model inputs. The values of the parameters were varied, one at a time, by ±10% to assess the impact of these changes on the total annual COI estimated by the model. The parameters were ranked in order of largest to smallest impact on costs when varied. These parameters represent the ‘cost drivers’ of the model.
Results
Cost of Wolfram syndrome
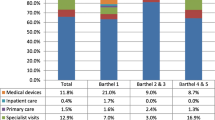
The estimated annual costs for people with Wolfram syndrome are shown in Fig. 3. The total annual COI to the NHS was £1,055,899 per year, and the average cost of Wolfram syndrome to the NHS per person with Wolfram syndrome per year was £16,498. The costs of treatment of symptoms (£935,350) represented 88.6% of the total costs, with the greatest annual costs being associated with DM care (£199,640; 18.9%) and the treatment of late-stage DM complications (£225,459; 21.4%).
Costs considered for DM care included the costs of insulin treatment, consultations with endocrinologists, diabetes specialist nurse services, diabetes education, gastrointestinal examinations, dietician appointments and inpatient care for ketoacidosis and severe hypoglycaemic events. Twelve late-stage complications, such as myocardial infarction, end-stage renal disease, neuropathy and major hypoglycaemic event, were included in the model [10]. Hearing impairment care was also a key contributor to costs: the annual costs associated with hearing impairment care made up 15.8% of the total annual costs of all Wolfram syndrome patients (Fig. 3). As a percentage of the total annual costs of Wolfram syndrome patients, the remaining annual costs related to treatment of symptom groups were: 10.0%, visual impairment care; 9.2%, neurological care; 7.1%, psychological/psychiatric care; 5.3%, renal/neurogenic bladder care; and 0.9%, DI and other endocrine disorders care.
The costs of diagnosis and referral to specialist centres (2.9% of total costs), and the costs of providing specialist services (8.5% of total costs; this includes the cost of annual review services, the cost of running specialist centres and the cost of transition services for children when transferring to adulthood) only contributed to a minor proportion of the total costs.
Deterministic sensitivity analysis
The DSA identified costs associated with hearing impairment and DM as major drivers in the model (Fig. 4). The results from the COI model were robust to uncertainty in the input parameters, as the total costs stayed within ±1.5% of the original point estimate, even when the most influential model inputs were varied by ±10%. These inputs are listed in Table 3.
Tornado plot: the twenty greatest cost drivers identified by the DSA. [a] Average cost of consumables. Upper estimate demonstrates the impact on the final COI by increasing the variable by 10%. Lower estimate demonstrates the impact on the final COI by decreasing the variable by 10%. COI cost of illness, DM diabetes mellitus, SNHL sensorineural hearing loss
Discussion
Despite being a rare disease affecting fewer than 100 individuals in the UK, the current COI model found that Wolfram syndrome costs the NHS over £1 million annually. The model consolidated information on the disease and treatment pathway from a variety of sources, including care providers, medical experts and national statistics. The costs identified were across all areas of care, from diagnosis, to standard care and late-stage complications. This reflects the multisystemic and progressive nature of Wolfram syndrome, as well as the many various tests, screening and multidisciplinary interventions required by individuals throughout their lives [1]. The combination of this and the range of debilitating symptoms has a profound impact on health, quality of life and caregiver burden.
The annual cost per person with Wolfram syndrome estimated by the COI model (£16,498) is roughly comparable with COIs previously estimated for other ultra-rare diseases, although the COI varies widely between diseases [5, 31]. A COI study of Niemann-Pick disease (NPD), an ultrarare disease with a prevalence of 1:150,000 [32], estimated the average annual UK cost per person with NPD to be £18,012 in 2008 [33]. COI studies for other rare diseases have also been reported, including for cystic fibrosis (CF), where the annual direct treatment costs per person with CF reported ranged from €7108 to €51,551 in 2010, depending on country, age of patients and advances in standard of care [5, 31].
A key result of the Wolfram syndrome COI study is the identification of DM management as a major cost driver, which highlights the need for effective treatments which could potentially mitigate such consequences. The current lack of proven treatment options means that there is an imminent need for effective interventions to slow down or halt the progression of this life-shortening disease [2]. As with any rare disease, future directions for the treatment of Wolfram syndrome include investigations into drug repurposing, as well as novel drug development. One example is sodium valproate, which has shown promise for the treatment of Wolfram syndrome in experimental models [34] by mitigating the consequence of low levels of wolframin protein in people with Wolfram syndrome [35]. In cells that would ordinarily have high levels of wolframin, such as those in the pancreas or brain, the reduction in wolframin causes increased levels of cell death (apoptosis). Sodium valproate may reduce apoptosis in these wolframin-deficient models, in doing so slowing progression or ameliorating some symptoms of Wolfram syndrome [35]. Limiting disease progression would reduce the symptom-related costs and therefore reduce the economic burden, motivating further studies into sodium valproate as a potential Wolfram syndrome treatment.
Since the early 2000s, there has been a considerable increase in expenditure on research and development into treatments for rare diseases, likely aided by regulatory frameworks such as the Orphan Medicinal Products Regulation (2000) in the EU [36]. Despite this drive to develop new treatments for rare diseases, there is a lack of robust clinical, economic and epidemiological data for most rare diseases [31]. This limits the knowledge of the existing unmet need, and therefore the potential real-world impact of new treatments, including their likely effect on healthcare budgets if those treatments are introduced. Wolfram syndrome is no exception in terms of the lack of existing data in the literature. To our knowledge, this is the first COI model to be developed for this condition, providing a much-needed estimate of the healthcare burden of Wolfram syndrome in the UK, while also incorporating an expert-informed evaluation of the steps and resources involved in the care of individuals with this rare disease.
The lack of published COI data emphasises the need for studies such as this, but in turn means that there was a limit on the number of published sources from which to derive and verify inputs into the model. Expert opinion from the specialist centre at the NHS Wolfram Syndrome Service (Birmingham Children’s Hospital) was utilised to gain knowledge of factors not covered in the public domain to account for this lack of published data. By using this Wolfram syndrome expertise to inform the selection of model parameters, there can be greater confidence in the accuracy of estimates of the annual cost of Wolfram syndrome disease. However, with fewer than 10 new individuals with Wolfram syndrome diagnosed per year, the age distribution of affected individuals can vary year-on-year (Fig. 2), which will affect the symptoms and disease progression stages observed in clinical practice in any given year. Given this variability in age distribution, the use of the median age of symptom onset to estimate the number of individuals with a particular symptom could result in an underestimation of the number of complications in the Wolfram syndrome population. However, this is unlikely to have substantially impacted the model results, given that median ages of onset were not found to be within the top twenty cost drivers in the model (Fig. 4). All individuals in the model are assumed to have Wolfram syndrome type 1; individuals with Wolfram syndrome type 2 would slightly differ symptomatically, however, these individuals are not typically seen in the UK setting and thus this assumption is unlikely to bias the results. It is also possible that some of the patients diagnosed with Wolfram syndrome may have been misdiagnosed and therefore should not have been considered by this study.
The model considers a healthcare payer perspective, and therefore only represents the direct costs of Wolfram syndrome to the NHS. This is a clear limitation of the study as the substantial burden of the disease on affected families, and the resulting costs to them as well as wider society, were not included in this model (for example, costs associated with provision of teaching support for the visually impaired in schools or attending colleges for the blind). However, inclusion of indirect costs was deemed impractical for this study due to a lack of available information to determine appropriate study inputs. Establishing an effective treatment regimen for each individual can be a slow and time-consuming process. Costs associated with lost time, such as lost earnings, were not included in the model. A focus group of individuals with Wolfram syndrome highlighted that a major financial cost to families is loss of working hours, often due to extensive time off for illness, appointments and caring responsibilities [30]. Furthermore, frequent travel, in addition to accommodation may incur significant out-of-pocket expenditure for parents and carers. The existence of centralised services such as the Birmingham centre is valuable to both researchers and patients alike, as specialist centres are likely to offer a setting for rare disease research as well as to help standardise the treatment strategies and improve the overall standard of healthcare provided to those with the disorder.
It is important to highlight that the limitations noted above are common to all COI models that only present a healthcare payer perspective. As the first COI model developed for Wolfram syndrome, it represents a crucial step forward in understanding the true cost of this disease to the NHS. The model accurately reflects the diagnosis process and symptom progression followed by these patients, as validated by clinical experts. The model provides a detailed view of the cost of this illness and offers a novel tool to aid in identifying potential areas of cost savings.
A number of potential policy implications come with the publication of this Wolfram syndrome COI data. Both the UK Strategy for Rare Diseases [37] and the EU-supported RARE-Bestpractices program [38] have indicated the value in undertaking research to address the gaps in knowledge and to help to define the best care pathways for rare diseases. Results from health economic studies such as this one can inform evidence-based policies, and as a result, help to ensure that patients across the UK and beyond receive the same, high quality standard of care.
Conclusions
This study is the first COI model for Wolfram syndrome and provides important information to facilitate economic evaluation of prospective therapies for this disease. The costs associated with DM care and late-stage complications of DM, hearing impairment and visual impairment made the greatest contribution to the final COI. These findings add much-needed information to a scarce evidence base, although additional research into the indirect costs associated with this disease is recommended.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Abbreviations
- ABR:
-
Auditory brain response
- BNF:
-
British National Formulary
- CCG:
-
Clinical Commissioning Group
- CF:
-
Cystic fibrosis
- CISD2 :
-
CDGSH iron sulphur domain protein 2 (gene)
- COI:
-
Cost of illness
- D:
-
Deafness
- DI:
-
Diabetes insipidus
- DIDMOAD:
-
Diabetes insipidus, diabetes mellitus, optic atrophy and deafness (alternative name for Wolfram syndrome)
- DM:
-
Diabetes mellitus
- DSA:
-
Deterministic sensitivity analysis
- EMA:
-
Endomysial antibodies
- ENT:
-
Ear, nose and throat
- GP:
-
General practitioner
- HbA1c:
-
Haemoglobin A1c
- IgA:
-
Immunoglobulin A
- MDT:
-
Multi-disciplinary team
- MI:
-
Myocardial infarction
- MRI:
-
Magnetic resonance imaging
- NCGC:
-
National Clinical Guideline Centre
- NHS:
-
National Health Service
- NPD:
-
Niemann-Pick disease
- OA:
-
Optic atrophy
- OT:
-
Occupational therapist
- PSSRU:
-
Personal Social Services Research Unit
- PY:
-
Per year
- SALT:
-
Speech and Language Therapists
- SC:
-
Subcutaneous
- SNHL:
-
Sensorineural hearing loss
- SPH:
-
Sphere
- tTG:
-
Tissue transglutaminase
- UTI:
-
Urinary tract infection
- WFS1 :
-
Wolfram syndrome type 1 (gene)
References
Orphanet. The portal for rare diseases and orphan drugs, Wolfram syndrome. Available from: http://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN&Expert=3463. Last accessed 19 Oct 2018.
Barrett TG, Bundey SE, Macleod AF. Neurodegeneration and diabetes: UK nationwide study of Wolfram (DIDMOAD) syndrome. Lancet. 1995;346:1458–63.
Chaussenot A, Bannwarth S, Rouzier C, Vialettes B, Mkadem SA, Chabrol B, Cano A, Labauge P, Paquis-Flucklinger V. Neurologic features and genotype-phenotype correlation in Wolfram syndrome. Ann Neurol. 2011;69:501–8.
Urano F. Wolfram syndrome: diagnosis, management, and treatment. Curr Diab Rep. 2016;16:6.
Barrett TG, Bundey SE. Wolfram (DIDMOAD) syndrome. J Med Genet. 1997;34:838–41.
Kinsley BT, Swift M, Dumont RH, Swift RG. Morbidity and mortality in the Wolfram syndrome. Diabetes Care. 1995;18:156670.
National Health Service. Diabetes UK. Available from: https://jdrf.org.uk/wp-content/uploads/2015/10/The_United_Kingdom_Insulin_Pump_Audit_May_2013.pdf. Last accessed 19 Oct 2018.
Rohayem J, Ehlers C, Wiedemann B, Holl R, Oexle K, Kordonouri O, Salzano G, Meissner T, Burger W, Schober E, Huebner A, Lee-Kirsch MA. Diabetes and neurodegeneration in Wolfram syndrome: a multicenter study of phenotype and genotype. Diabetes Care. 2011;34:1503–10.
Tranebjaerg L. WFS1-related disorders. Seattle: University of Washington, Seattle; 2009.
Pratoomsoot C, Smith HT, Kalsekar A, Boye KS, Arellano J, Valentine WJ. An estimation of the long-term clinical and economic benefits of insulin lispro in type 1 diabetes in the UK. Diabet Med. 2009;26:803–14.
Karzon RK, Hullar TE. Audiologic and vestibular findings in Wolfram syndrome. Ear Hear. 2013;34:809–12.
National Health Service. NCGC 2012 (2010). Available from: https://www.nice.org.uk/guidance/cg148/evidence/full-guideline-188123437. Last accessed 19 Oct 2018.
Swift RG, Sadler DB, Swift M. Psychiatric findings in Wolfram syndrome homozygotes. Lancet. 1990;336:667–9.
British National Formulary. Available from: https://www.bnf.org/products/bnf-online/. Last accessed 19 Oct 2018.
Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, Waugh N. Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation. Health Technol Assess. 2010;14:iii–iv, xi-xvi, 1–181.
Expert Opinion. NHS Wolfram Syndrome Service (Birmingham Children’s Hospital). 2016.
Expert Opinion. NHS Wolfram Syndrome Service (Queen Elizabeth Hospital). 2016.
Federation of (Ophthalmic and Dispensing) Opticians. Available from: http://www.fodo.com. Last accessed 19 Oct 2018.
National Health Service. Reference costs (2015–2016). Available from: https://www.gov.uk/government/publications/nhs-reference-costs-2015-to-2016. Last accessed 19 Oct 2018.
National Health Service. National Tariff (2016-2017). Available from: https://www.gov.uk/government/publications/nhs-national-tariff-payment-system-201617. Last accessed 19 Oct 2018.
National Health Service. Vale of York CCG. Available from: https://www.valeofyorkccg.nhs.uk/. Last accessed 19 Oct 2018.
National Health Service. Drug Tariff (May 2016). Available from: https://www.nhsbsa.nhs.uk/pharmacies-gp-practices-and-appliance-contractors/drug-tariff. Last accessed 19 Oct 2018.
National Health Service. Bolton Foundation Trust (2015). Available from: http://www.boltonft.nhs.uk. Last accessed 19 Oct 2018.
National Health Service. Southern Derbyshire CCG 2016. Available from: https://www.derbyhospitals.nhs.uk. Last accessed 19 Oct 2018.
Personal Social Services Research Unit. Available from: http://www.pssru.ac.uk/project-pages/unit-costs/2016/. Last accessed 19 Oct 2018.
Roze S, Valentine WJ, Zakrzewska KE, Palmer AJ. Health-economic comparison of continuous subcutaneous insulin infusion with multiple daily injection for the treatment of type 1 diabetes in the UK. Diabet Med. 2005;22:1239–45.
UK Genetic Testing Network. Available from: https://ukgtn.nhs.uk. Last accessed 19 Oct 2018.
Warren M. Providing low vision rehabilitation services with occupational therapy and ophthalmology: a program description. Am J Occup Ther. 1995;49:877–83.
Wolfram Syndrome Guideline Development Group. Management of Wolfram Syndrome A Clinical Guideline. 2014. Available from: http://www.orpha.net/national/data/IE-EN/www/uploads/Wolfram2014.pdf. Last accessed 04 July 2019.
Findacure. Patient focus group report: Wolfram syndrome. 2016. Available from: https://www.findacure.org.uk/wp-content/uploads/2018/06/Wolfram-syndrome-Findacure-Rare-Disease-Perspectives-2016.pdf. Last accessed 04 July 2019.
Angelis A, Tordrup D, Kanavos P. Socio-economic burden of rare diseases: a systematic review of cost of illness evidence. Health Policy. 2015;119:964–79.
Patterson M. Niemann-pick disease type C. GeneReviews®. Seattle: University of Washington, Seattle; 1993.
Imrie J, Galani C, Gairy K, Lock K, Hunsche E. Cost of illness associated with Niemann-pick disease type C in the UK. J Med Econ. 2009;12:219–29.
Kakiuchi C, Ishigaki S, Oslowski CM, Fonseca SG, Kato T, Urano F. Valproate, a mood stabilizer, induces WFS1 expression and modulates its interaction with ER stress protein GRP94. PLoS One. 2009;4:e4134.
Terasmaa A, Soomets U, Oflijan J, Punapart M, Hansen M, Matto V, Ehrlich K, Must A, Koks S, Vasar E. Wfs1 mutation makes mice sensitive to insulin-like effect of acute valproic acid and resistant to streptozocin. J Physiol Biochem. 2011;67:381–90.
European Parliament and of the Council Regulation (EC) 141/2000 of 16 December 1999 on Orphan Medicinal Products. OJL 018/1, 22.01.2000. Available from: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2000:018:0001:0005:en:PDF. Last accessed 19 Oct 2018.
UK Department of Health. The UK Strategy for Rare Diseases. Available from: http://www.raredisease.org.uk/uk-strategy-for-rare-diseases/. Last accessed 19 Oct 2018.
RARE-Bestpractices. Available from: http://www.rarebestpractices.eu/. Last accessed 19 Oct 2018.
Acknowledgements
The authors thank the teams at the Birmingham Wolfram syndrome specialist service, the National Institute for Health Research Wellcome Clinical Research Facility and the NIHR Rare Diseases Translational Research Collaboration for their support. The authors also acknowledge Dr. Ben Wright from Queen Elizabeth Hospital, Birmingham, UK, for his input on the cost of illness model and all Findacure employees, in particular Flóra Raffai, in addition to Aimée Hall (MPhys) and Gengshi Chen (MSc) from Costello Medical, Cambridge, UK, for medical writing and editorial assistance in preparing this manuscript for publication based on the authors’ input and direction.
Funding
This work is part of Findacure’s rare disease drug repurposing social impact bond proof of concept study, which was funded by the Big Lottery Fund (Unique Reference Number: 10270530). The manuscript was developed on a pro bono basis by Costello Medical.
Author information
Authors and Affiliations
Contributions
SE, WG, SDS, AG, TB and RT made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; SE, WG, SDS, AG, TB and RT were involved in drafting the manuscript or revising it critically for important intellectual content; SE, WG, SDS, AG, TB and RT gave final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All authors of the manuscript have read and agreed to its content and are accountable for all aspects of the accuracy and integrity of the manuscript in accordance with ICMJE criteria.
This article is original, has not already been published in a journal, and is not currently under consideration by another journal. Results from this model have previously been presented at the 2016 International Society for Pharmacoeconomics and Outcomes Research European conference and have since been updated for this manuscript.
All authors agree to the terms of the BioMed Central Copyright and License Agreement.
Consent for publication
Not applicable.
Competing interests
At the time of study, authors SE and SDS were affiliated with Costello Medical. SE is currently affiliated with the Acteon Consultancy LLP, and SDS is currently affiliated with the University of Warwick. The authors have nothing further to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Eljamel, S., Ghosh, W., De Stone, S. et al. A cost of illness study evaluating the burden of Wolfram syndrome in the United Kingdom. Orphanet J Rare Dis 14, 185 (2019). https://doi.org/10.1186/s13023-019-1149-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-019-1149-7