Abstract
Background
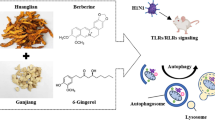
Influenza viruses, especially Influenza A virus and Influenza B virus, are respiratory pathogens and can cause seasonal epidemics and pandemics. Severe influenza viruses infection induces strong host-defense response and excessive inflammatory response, resulting in acute lung damage, multiple organ failure and high mortality. Isoquercitrin is a Chinese medicine monomer, which was reported to have multiple biological activities, including antiviral activity against HSV, IAV, SARS-CoV-2 and so on. Aims of this study were to assess the in vitro anti-IAV and anti-IBV activity, evaluate the in vivo protective efficacy against lethal infection of the influenza virus and searched for the more optimal method of drug administration of isoquercitrin.
Methods
In vitro infection model (MDCK and A549 cells) and mouse lethal infection model of Influenza A virus and Influenza B virus were used to evaluate the antiviral activity of isoquercitrin.
Results
Isoquercitrin could significantly suppress the replication in vitro and in vivo and reduced the mortality of mouse lethal infection models. Compared with virus infection group, isoquercitrin mitigated lung and multiple organ damage. Moreover, isoquercitrin blocked hyperproduction of cytokines induced by virus infection via inactivating NF-κB signaling. Among these routes of isoquercitrin administration, intramuscular injection is a better drug delivery method.
Conclusion
Isoquercitrin is a potential Chinese medicine monomer Against Influenza A Virus and Influenza B Virus infection.
Similar content being viewed by others
Introduction
Influenza virus, belonging to the Orthomyxoviridae family, is a single-stranded, negative sense RNA virus and is one of the most significant pathogens threatening to human health. Influenza viruses are classified into four types (A, B, C, and D), of which influenza A virus (IAV) comprised the majority of global seasonal influenza case. Co-circulating with IAV, influenza B virus (IBV) is also responsible for about 25% of all influenza-related hospitalisations, especially cause high morbidity and mortality in children. [1, 2]. Continuing antigenic drift and shift of IAV and IBV results in new variants which facilitates the cross-species transmission and reduced efficacy of current vaccines and antiviral drugs. Thus, identifying new, more effective drugs against both IAV and IBV is of critical importance.
Isoquercitrin, also known as Quercetin-3-O-glucoside, is a kind of flavonol and widely exists in plants, like Houttuynia cordata, Hedyotis diffusa, et al. Currently, besides the direct extraction from plants, the chemical synthesis method was extensively used to prepare isoquercitrin. As a mono-glycoside derivative of quercetin which has diverse biological functions, isoquercitrin has been demonstrated to exhibit anti-tumor [3,4,5], anti-apoptotic [6], antioxidant [7] and anti-inflammatory [8] activities. Additionally, isoquercitrin also exerts antiviral activity against herpes simplex virus (HSV) [9, 10], influenza virus (IV) [11, 12], coronavirus (HCoV-229E, SARS-CoV-2) [13, 14], zika virus (ZIKV) [15, 16], mayaro virus (MAYV) [17], varicella-zoster virus (VZV) and human cytomegalovirus (HCMV) [18] in vitro. However, most of these studies have focused on in vitro studies and relatively few reports were performed on its in vivo treatment efficacy, especially against lethal infection of these viruses.
In this study, we found that isoquercitrin exhibited suppressive effect on influenza A (H1N1) virus and influenza B virus in vitro. Furthermore, isoquercitrin possesses a therapeutic effect in animal models through enhancing virus clearance, suppressing inflammation and attenuating lung pathological injury. Additionally, compared with other drug administrations, intramuscular injection is a better drug delivery method. These findings suggested that isoquercitrin might be a potential antiviral candidate against influenza A virus and influenza B virus.
Materials and methods
Cell culture, virus and compounds preparation
Human lung adenocarcinoma A549 cells and Madin-Darby canine kidney cells (MDCK) [19,20,21] were cultured in Dulbecco’s modified Eagle’s medium (DMEM) with 10% fetal bovine serum (FBS, Sigma), 1% penicillin and streptomycin. H1N1/UI182 strain was a mouse-adapted strain of the 2009 influenza A (H1N1) virus (A/Changchun/01/2009 (H1N1)). H1N1/PR8 virus, a laboratory adapted influenza A (H1N1) virus (A/Puerto Rico/8/34), was passaged in MDCK cells. Influenza B virus IBV/S9-E2 strain was rescued by Changchun Veterinary Research Institute according to the sequence of B/Yamagata/16/88 (GenBank Accession: CY018765-CY018772) and IBV/S9-MD stain was a mouse-adapted strain of IBV/S9-E2 strain. Isoquercitrin (CAS Number: 21637-25-2), purchased from Shanghai yuanye Bio-Technology Co., Ltd, was dissolved in dimethyl sulfoxide (DMSO) and diluted in DMEM with 2% FBS or Phosphate Buffered Saline (PBS, pH 7.4) before use.
Cytotoxicity assay, in vitro antiviral assay and time-of-addition assay
MDCK and A549 cells were seeded in 96-well plate (104 cells/well) and incubated at 37 °C with 5% CO2. When the confluence reached 70–80%, different concentrations of the drug (8, 15, 30, 60, 125, 250 μg/mL) were added. After 48 h, cell viability was measured by CCK-8 assay using Cell Counting Kit-8 (Beyotime, C0039) following manufactory’s instruction. For in vitro antiviral assay, cells were washed with PBS and infected with influenza A virus (H1N1/PR8 and H1N1/UI182) and influenza B virus (IBV/S9-E2 and IBV/S9-MD) (MOI = 0.1) when cell confluence reached 70–80%. After 1 h post infection, isoquercitrin were added. After 48 h, cell viability was measured by CCK-8 assay. As for time-of-addition assay, cells were treated with isoquercitrin for 1 h before virus infection or inoculated with isoquercitrin-viruses mixture, after 1 h virus adsorption. At 48 h post-infection, cell viability was measured by CCK-8 assay.
Immunofluorescence staining
The cells were seeded in 12-well plates and infected with H1N1/UI182 (MOI = 0.5) when confluence reached 70%. At 48 h post-infection, cells were washed three times with cold PBS and fixed with 4% paraformaldehyde (PFA) for 20 min, then the plate was infiltrated with 0.2% Triton-X100 and blocked with 2% BSA for 1 h. The primary antibody against influenza virus Nucleocapsid protein (Abcam, ab104870, 1:200) was added and incubated with cells overnight at 4 ℃. After the primary antibodies, cells were washed three times using PBS and incubated with the secondary antibodies (Goat Anti-Rabbit IgG H&L (Alexa Fluor® 488), Abcam, ab150077, 1:500) for 2 h without light. After nuclei staining with Hoechst 33,258 (Thermo Fisher Scientific, H3569, 1 µg/mL) for 10 min, fluorescence was observed under a fluorescence microscope (Carl Zeiss, Germany).
In vivo experiments in mice
Female BALB/c mice (18–20 g, 6 weeks old) were purchased from Beijing Vital River Laboratory Animal Technology Co., Ltd (Beijing, China). After 3 days of adaptive feeding, mice were randomly divided into uninfected group (Control), virus-infected groups (H1N1/PR8 and IBV/S9-MD), isoquercitrin-treated group, oseltamivir phosphate (a NA inhibitor)-treated group. Mice in each group, except uninfected group, were challenged with 50 µL virus dilution (10 × LD50) using nasal drop method, respectively. Control group and virus-infected groups were treated with 0.9% saline by intraperitoneal injection (i.p.). The isoquercitrin treatment (10 mg/kg/day, i.p) [22] and oseltamivir phosphate treatment (25 mg/kg/day, p.o.) [23] started after 12 h post-infection and until the fifth day. Mouse body weight and survival status were monitored each day for 14 days.
Pathological analysis and immunohistochemical assay
At 3 day post-infection (3 dpi) and 5 day post-infection (5 dpi), lung, heart, liver, spleen and kidney of mice in each group were collected, part of tissue was used for analysis of gene and protein expression, part of tissue was fixed in the 4% paraformaldehyde (PFA), preparing for tissue sections. For pathological analysis, tissue sections were stained with hematoxylin and eosin (H&E), dried and observed under a light microscope (Olympus, Japan). Immunohistochemical assay was performed as described previously [47].
RNA isolation and quantitative RT-PCR
Total RNA from mouse lung tissues of mice was extracted using the HiPure Universal RNA Kit (Magen, R4130-03). About 1 μg RNA was used to synthesize cDNA using PrimeScript™ RT reagent Kit (Takara, RR047A). The expression level of target mRNA was measured by qRT-PCR assay using TB Green Premix Ex Taq II (Takara, RR820A) based on TB Green chimeric fluorescence method. The primer pairs were listed in Table 1, β-actin was used as a loading control.
EID50 detection
9 day-old embryonated chicken eggs were used to detect EID50 (50% egg-infective dose) of virus. An equivalent number of mouse lung tissues from each group were crushed in DMEM supplemented with 400 units/mL penicillin and streptomycin. Followed by centrifugation, the supernatant was serially diluted tenfold from 10–1 to 10–8 and were inoculated into eggs for 48 h at 37 ℃ (for IBV, eggs should incubate for 72 h at 33 ℃). Then 50 μL allantoic fluid in each egg was collected and mixed with 50 μL 1% chicken RBC. After standing for 15 min, the highest dilutions that completely agglutinated chicken RBC were recorded. Viral titer was calculated by the Reed-Muench method, and the result was expressed as log10 EID50.
Western blot
The mouse lung tissues from each group were lysed with RIPA Lysis Buffer (Beyotime, P0013B) to collect total proteins. After protein quantification and electrophoresis, the proteins were transferred on a PVDF membrane. The protein expression was detected by relative antibody and β-actin (Abcam, ab6276, 1:5000) was used as an internal reference protein for quantitative analysis.
Statistical analysis
Statistical comparisons were performed using ANOVA analysis. Quantitative data sets were expressed as the means ± standard error (SE), and the statistical significance was evaluated by Graphpad Prism 8.0 software. Compared with the Virus-infected group, P < 0.05 was regarded to have significant differences.*P < 0.05, **P < 0.01, and ***P < 0.001.
Results
Isoquercitrin inhibits influenza virus in vitro
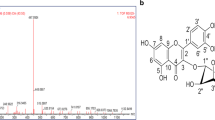
To determinate whether isoquercitrin can inhibit different subtypes of influenza virus, the antiviral assays were performed in vitro against IAV and IBV. We first assessed antiviral activity of isoquercitrin in MDCK and A549 cells. Cells, infected with or without virus, were treated with isoquercitrin at different concentrations for 48 h, and cell proliferation was assessed using CCK-8 assay. The results showed that isoquercitrin inhibited IAV and IBV infection without inducing significant cytotoxicity (CC50 > 800 μg/mL), with EC50 of 46.77 ± 1.31 μg/mL for H1N1/PR8 (Fig. 1A), 46.52 ± 4.70 μg/mL for H1N1/UI182 (Fig. 1B), 48.90 ± 7.49 μg/mL for IBV/S9-MD (Fig. 1C) and 42.63 ± 3.64 μg/mL for IBV/S9-E2 (Fig. 1D) in MDCK cells. Likewise, isoquercitrin blocked IAV and IBV infection in A549 cells, with selectivity index (SI = CC50/EC50) higher than 10 (Fig. 1E–H). To investigate which stage of influenza virus infection does isoquercitrin exert the antiviral effect, time-of-addition assay was performed. The inhibitory effect of different drug administration protocols showed that isoquercitrin played an antiviral role main in late stage of influenza virus infection, as treatment after infection exerted the maximum antiviral effect against both IAV and IBV (Additional file 1: Fig. S1). Additionally, the results of immunofluorescence experiments indicated that isoquercitrin suppressed Nucleoprotein (NP) expression of IAV (Fig. 2A, B) and IBV (Fig. 2C, D) in MDCK cells. Taken together, these data showed that isoquercitrin could potently inhibit both IAV and IBV infection in different cell lines.
Isoquercitrin inhibits influenza virus in vitro. The inhibitory efects of isoquercitrin on the influenza A A, E-PR8, B, F-UI182) virus and influenza B C, G S9-MD, D, H-S9-E2) virus in MDCK cells A–D and A549 cells E–H. As shown in the figure, pink curve represents the dose-dependent relationship between drug inhibition rate against virus and dosage, blue curve represents the dose-dependent relationship between drug’s cytotoxicity and dosage. Three independent experiments were repeated and the figure showed the results of one representative experiment out of three performed. The EC50/IC50 values in the figure were obtained through curve fitting using Graphpad Prism 8.0 software and only represented the data from this experiment. The SI indicated the selection index (SI = IC50/EC50) of isoquercitrin
Isoquercitrin inhibits influenza virus in vitro. The effect of isoquercitrin on the expression of influenza A (H1N1/PR8) virus A and influenza B (S9-MD) virus C proteins NP in infected MDCK cells at low dose (20 μg/mL) and high dose (100 μg/mL). B, D The percentage of NP-positive cells in A and B was calculated
Isoquercitrin protects mice from a lethal infection of the influenza virus
To assess the protection efficacy of isoquercitrin in a mouse lethal infection model, BALB/c mice were challenged with a lethal dose of influenza A virus (H1N1/PR8) and influenza B virus (IBV/S9-MD). After corresponding treatment, four mice of each group were euthanized and tissues (lung, heart, liver, spleen, kidney) were collected for further analysis. The remained mice are used to monitor the body weight change and survival status. The results showed that virus infection induced obvious reduction of mouse body weight from day 2 and all mice in H1N1/PR8-infected group and IBV/S9-MD-infected group dead by day 6 after infection. In contrast, isoquercitrin and oseltamivir treatment attenuated weight loss and increased the survival rate of infected mice. Surprisingly, isoquercitrin significantly promoted mouse body weight recovery, which was better than oseltamivir, but its protective effect was inferior to Oseltamivir (Fig. 3A, B, E, F). Meanwhile, the effect of isoquercitrin on viral titer in mouse lungs was determined at 3 dpi and 5 dpi. The results showed that viral titer of IAV (Fig. 3C, D) and IBV (Fig. 3G, H) was significantly reduced by isoquercitrin. These results reveal that isoquercitrin has a potently inhibitory effect against H1N1/PR8 and IBV/S9-MD, and protects mice from a lethal infection of influenza virus.
Isoquercitrin protects mice from a lethal infection of the influenza virus. A Body weight changes of H1N1/PR8-infected mice and drug-treated mice. B Survival status of H1N1/PR8-infected mice and drug-treated mice. C–D The effects of isoquercitrin and oseltamivir phosphate on viral titer in mouse lungs at 3 dpi and 5 dpi. E Body weight changes of IBV/S9-MD-infected mice and drug-treated mice. F Survival status of IBV/S9-MD-infected mice and drug-treated mice. G–H The effects of isoquercitrin and oseltamivir phosphate on viral titer in mouse lungs at 3 dpi and 5 dpi
Effect of isoquercitrin on pathological damage caused by influenza virus infection
Influenza virus infection can cause variable degree of lung injury in host which is an important standard of therapeutic efficacy of antiviral drugs [24]. Thus, we evaluated the effect of isoquercitrin on influenza virus-induced pathological damage in mouse infection models. Morphologically, H1N1/PR8 and IBV/S9-MD infection caused wade-range of visible hemorrhage and lesions on surface of the lungs and these symptoms were alleviated after treatment with isoquercitrin and oseltamivir. (Fig. 4A, B). H and E staining of the lung tissues showed that after infection with influenza virus, thickened alveolar walls were observed, accompanied by necrotic cell debris in partial bronchiolar lumen (red arrow), infiltration of a large number of lymphocytes and neutrophils (black arrow), and effusion of eosinophilic material within alveolar spaces (blue arrow), and these damages were reversed by isoquercitrin and oseltamivir. Furthermore, analysis of lung index (Fig. 4C, F) and lung pathology score (Fig. 4D, G) of mice in each group visually revealed the potent protective effects of isoquercitrin and oseltamivir against H1N1/PR8 and IBV/S9-MD infection. The results of viral NP immunohistochemistry (IHC) (Fig. 4E, H) showed that isoquercitrin significantly inhibited influenza virus nucleoprotein (NP) expression in lung tissues. Similarly, isoquercitrin also attenuated pathological damage (Additional file 1: Fig. S2A) and decreased the percentages of NP-positive cells (Additional file 1: Fig. S2B, C) in mouse heart, liver, spleen, kidney. Together, these results suggest that isoquercitrin suppresses the viral protein expression and mitigates influenza virus-caused pathological damage in major organs of mice.
Effect of isoquercitrin on pathological damage caused by influenza virus infection. A Lung morphology, H and E staining and Immunohistochemistry staining of virus protein NP in H1N1/PR8-infected mice and drug-treated mice at 5 days post-infection (dpi). B Lung morphology, H and E staining and Immunohistochemistry staining of virus protein NP in IBV/S9-MD-infected mice and drug-treated mice at 5 dpi. C–E Lung index, lung pathology score and percentage of NP-positive cell in lung tissues in A. F–H Lung index, lung pathology score and percentage of NP-positive cell in lung tissues in B
Isoquercitrin inhibits cytokines induced by influenza virus infection by inactivating NF-κB signal
The activation of innate immune cells and the production of cytokines are important markers of influenza virus infection. Continuous generation of cytokines exacerbates the influenza virus-induced “cytokine storm”, which is main cause of lung damage of host [25]. To evaluate the effect of isoquercitrin on the cytokines production, Western blot and quantitative real-time PCR assay (qPCR) were performed. The results of Western blot (Fig. 5A, F) revealed that IBV/S9-MD infection increased protein expression of inflammatory factors, IL-10 (Fig. 5D) and LI-1β (Fig. 5E) in mouse lung tissues. Similarly, qPCR results showed that a lethal dose of IBV/S9-MD infection could significantly upregulated mRNA expression of cytokines, IFN-α (Fig. 5G), IFN-β (Fig. 5H), TNF-α (Fig. 5I), IL-6 (Fig. 5J), IL-10 (Fig. 5K), and IL-1β (Fig. 5L) and interferon-stimulated gene, ISG54 (Fig. 5M) and ISG56 (Fig. 5N), but this induction was potently suppressed by isoquercitrin and oseltamivir. Meanwhile, isoquercitrin also had a significantly inhibitory effect on cytokines production caused by H1N1/PR8 infection (Additional file 1: Figure S3), with a similar or even better inhibition than oseltamivir. NF-κB pathway plays as a major regulator of cytokine and chemokine expression after influenza virus infection and also influences influenza virus replication [26]. Thus, the protein expression of phosphorylated NF-κB (p65) and IκBα were detected. Western Blot results (Fig. 5A) indicated that isoquercitrin could reduced the phosphorylation of IκBα (Fig. 5B) and p65 (Fig. 5C) which were up-regulated by influenza B virus, resulting the inactivity of NF-κB signaling. These findings demonstrate that isoquercitrin is able to suppress the inflammatory response induced by influenza virus infection via inactivating NF-κB signaling.
Isoquercitrin inhibits cytokines expression induced by influenza B virus infection by inactivating NF-κB signal. At 5 days post infection, mouse lung tissues were harvested for Western blot experiments and qPCR analysis. A Western blot images of IκBα, phosphorylated IκBα (p-IκBα), NF-κB (p65), p-p65, IL-10, IL-1β, viral Nucleoprotein (NP) and β-actin was shown. B p-IκBα/IκBα ratio was quantified. C p-p65/p65 ratio was quantified. D Quantification of Western blot bands of IL-10. E Quantification of Western blot bands of IL-1β. F Quantification of Western blot bands of viral NP. Relative mRNA expression level of type I IFN, IFN-α G and IFN-β H, pro-inflammatory cytokines, TNF-α I, IL-6 J and IL-1β L, anti-inflammatory cytokine, IL-10 K and IFN induced gene, ISG54 M and ISG56 N in mouse lung tissues of each group were detected
Intramuscular injection is a better drug delivery method of isoquercitrin
Mode of drug administration affects absorption, distribution, metabolism and ultimately drug efficacy. To compare the antiviral effect of different drug delivery method of isoquercitrin, lethal mouse model of IBV infection was treated with isoquercitrin using different modes of drug administration, including intraperitoneal injection (i.p.), intramuscular injection (i.m.), oral gavage (p.o.), and subcutaneous injection (s.c.). The results displayed in Fig. 6 shown that isoquercitrin treatment sped up weight restoration of infected mice (Fig. 6B), and improved the survival rate (Fig. 6A). Noticeably, treated by the i.m. could achieve better therapeutic outcomes compared with other drug delivery methods, providing better improvement of mouse lung damage (Fig. 6C–E) and more significant reduction in virus titers (Fig. 6F–G). These results indicate that intramuscular injection is a better method of administration for isoquercitrin.
The comparison of antiviral efficacy of different drug delivery method of isoquercitrin. A Survival status of mice in each group. B Body weight changes of mice in each group. C Lung morphology of mice in each group at 3 dpi. D Lung index of mice in each group. E Lung pathology score of mice in each group. F Virus titer in lung tissues of mice in each group. G Virus titer in turbinates of mice in each group
Discussion
IAV infection is main causes of seasonal influenza epidemics and pandemics which can induce human respiratory disease and acute lung injury (ALI). Meanwhile, IBV often co-circulates with IAV and even becomes major epidemic strains worldwide [27]. Existing antiviral strategies to control emerging influenza strains mainly focus on vaccines and antiviral drugs development. However, frequent antigenic drift and antigenic switch of IAV generates novel strains which can escape from available vaccines and reduce efficiency of antiviral drugs. For example, 100% of seasonal H3N2 and 99.8% of 2009 pandemic influenza samples was found resistant to adamantanes, M2 inhibitor [28]. Similarly, due to mutation at particular amino acid, NA inhibitors-resistant human isolates gradually emerged, like H1N1 (NA-I222V/M/L/R/T, H274Y and S334N) [29], H3N2 (NA-E119V, E11V) [30], H7N9 (NA-R292K) [31] and IBV (NA-G104R) [32]. Given that IBV also has the antigenic drift and can develop drug-resistance, identifying and developing new antiviral drugs is imperative. In our study, although our drug has weaker in vitro antiviral effects than oseltamivir, whose EC50 values for influenza A virus were in the low nanomolar (~ 2–13 nM) concentration range [33], but in vivo, 10 mg/kg/day of isoquercitrin had equivalent efficacy to 25 mg/kg/day of oseltamivir phosphate, suggesting this drug is a better in vivo therapeutic drug. Given the continuous emergence of resistance of oseltamivir, perhaps isoquercitrin can become a new treatment option for drug-resistant strains of influenza A virus and influenza B virus.
Isoquercitrin is a flavonoid that can be extracted from natural plants and exhibits antiviral activity against multiple viruses. Isoquercitrin was reported to be the main component of some Traditional Chinese medicine (TCM) that suppressed HSV by inhibiting ROS production and NF-κB activation [9, 10], suppressed IAV (H1N1) replication by inhibiting ROS production [11] and exerted antiviral activity against SARS-CoV-2 [34] and HCoV-229E [13] by blocked Spike protein and Mpro. Isoquercitrin also blocked ZIKV infection through reduced ZIKV NS2B-NS3 protease and NS5 RNA dependent RNA polymerase (RdRp) activity in cells and Ifnar1−/− mice [16, 35]. Taken its inhibitory effect on many RNA viruses and even DNA viruses and results of our researches, isoquercitrin could become a broad-spectrum antiviral candidate.
Cytokine is a kind of peptide or glycoprotein secreted by the cells and perform diverse biological functions, such as immune modulation, involvement in inflammatory responses, etc. Cytokine is a crucial component of antiviral innate immune, but severely viral infections are always accompanied by cytokine dysregulation and amplification, even becomes the main factor for viral pneumonia during the later phase after virus infection [36]. Considering that, reducing cytokine production is a potential treatment strategy. Thus, multiple immunomodulators, such as Janus kinase (JAK) inhibitors [37] and anti‐IL‐6 antibody [38], are developed to control virus-induced “cytokine storm” and mitigate disease progression. In addition to chemical molecules and antibodies, traditional Chinese medicine gradually become an alternative source for anti-influenza virus drugs [39]. Fructuscorni and Radix salviae miltiorrhizae possess resistance to influenza because they can enhance specific and non-specific immunity [40]. As a natural drug, isoquercitrin was reported to reduce the virus-induced ROS production and NF-κB activation [10]. Taken together, isoquercitrin not only has antiviral activity against IAV and IBV, but also represses the expression of pro-inflammatory cytokines by inactiviating NF-κB signal.
The pathogenicity of an influenza virus depends on many factors, such as cell tropism, replicate efficiency, and host immunity. Both IAV and IBV prefer to replicate in respiratory system and innate immune cells are recruited to lung and produce massive cytokines and chemokines after influenza virus infection, inducing pneumonia, even multi-organ failure [41]. Unexpectedly, adolescents and children are more susceptible to IBV and sometimes IBV-associated diseases develop earlier and more severe than IAV [42]. Characterized by inflammatory cell infiltration, alveolar epithelial cells sloughing, alveolar wall hyperemia and thickness, alveolar hemorrhage and damage, interstitial-alveolar edema, etc. the degree of which always becomes a standard for assess the pathogenicity of viruses and the efficacy of therapeutic drugs [43]. Fortunately, in this study, isoquercitrin was found as a treatment drug for viral pneumonia.
The dose and route of administration are main factors affecting the drug efficacy [44]. In other researches, isoquercitrin was demonstrated to exert therapeutic effect at lower doses, so we only explore its dose-dependent relationship. In a murine model, the common route for drug administration include tail-vein injection, intraperitoneal injection, intramuscular injection, subcutaneous injection, oral gavage and intranasal administration. Compared to tail-vein injection, which can increase the risk of infection and thromboembolic events [45], intraperitoneal injection, intramuscular injection and subcutaneous injection are more safe and long-acting. Oral administration is the predominant method of drug administration of natural products [46], but its bioavailability should be considered. In our study, isoquercitrin treatment via different administration could exert antiviral effect, suggesting that this drug may directly exert the pharmacodynamic effect in target organ, without requirement of metabolic conversion. Additionally, considering the influence of different drug administration on the antiviral effect of isoquercitrin, more experiments should be considered be implemented to identify the optimal dosing regimen.
Conclusion
Above findings suggest that isoquercitrin has potent antiviral activity against influenza A (H1N1) virus and influenza B virus in vitro and in vivo. Lethal infection of influenza virus induced excessive production of cytokines and severe lung damage, but these outcomes were suppressed by isoquercitrin, indicating that this drug could benefit severe patients with influenza virus infection. Additionally, through comparison between different drug delivery methods, the i.m. was proved as a better method for administration of isoquercitrin.
Availability of data and materials
The data produced from this study are available from the first author and the corresponding author on reasonable request.
References
Dumm RE, Heaton NS. The development and use of reporter influenza B viruses. Viruses. 2019;11(8):736.
Yazici Özkaya P, Turanli EE, Metin H, Aydın Uysal A, Çiçek C, Karapinar B. Severe influenza virus infection in children admitted to the PICU: comparison of influenza A and influenza B virus infection. J Med Virol. 2022;94(2):575–81.
Chen Q, Li P, Li P, Xu Y, Li Y, Tang B. Isoquercitrin inhibits the progression of pancreatic cancer in vivo and in vitro by regulating opioid receptors and the mitogen-activated protein kinase signaling pathway. Oncol Rep. 2015;33(2):840–8.
Huang G, Tang B, Tang K, Dong X, Deng J, Liao L, Liao Z, Yang H, He S. Isoquercitrin inhibits the progression of liver cancer in vivo and in vitro via the MAPK signaling pathway. Oncol Rep. 2014;31(5):2377–84.
Chen F, Chen X, Yang D, Che X, Wang J, Li X, Zhang Z, Wang Q, Zheng W, Wang L, Wang X, Song X. Isoquercitrin inhibits bladder cancer progression in vivo and in vitro by regulating the PI3K/Akt and PKC signaling pathways. Oncol Rep. 2016;36(1):165–72.
Wang H, Xia W, Long G, Pei Z, Li Y, Wu M, Wang Q, Zhang Y, Jia Z, Chen H. Isoquercitrin Ameliorates Cisplatin-Induced Nephrotoxicity Via The Inhibition Of Apoptosis, Inflammation, And Oxidative Stress. Front Pharmacol. 2020;11: 599416.
Kim JH, Lee S, Cho EJ. Acer okamotoanum and isoquercitrin improve cognitive function via attenuation of oxidative stress in high fat diet and amyloid beta-induced mice. Food Funct. 2019;10(10):6803–14.
Liang S, Xu Z, Ruan Y, Niu T, Guo W, Jiang W, Hou J. Isoquercitrin attenuates renal ischemia/reperfusion injury through antioxidation, anti-inflammation, and anti-apoptosis in mice. Transplant Proc. 2020;52(3):1014–9.
Chen X, Wang Z, Yang Z, Wang J, Xu Y, Tan RX, Li E. Houttuynia cordata blocks HSV infection through inhibition of NF-κB activation. Antiviral Res. 2011;92(2):341–5.
Kim B, Kim YS, Hwang YH, Yang HJ, Li W, Kwon EB, Kim TI, Go Y, Choi JG. Quercus acuta Thunb (Fagaceae) and Its component, isoquercitrin, inhibit HSV-1 replication by suppressing virus-induced ROS production and NF-κB activation. Antioxidants. 2021;10(10):1638.
Nile SH, Kim DH, Nile A, Park GS, Gansukh E, Kai G. Probing the effect of quercetin 3-glucoside from Dianthus superbus L against influenza virus infection- In vitro and in silico biochemical and toxicological screening. Food Chem Toxicol. 2020;135: 110985.
Kim Y, Chang KO. Protein disulfide isomerases as potential therapeutic targets for influenza A and B viruses. Virus Res. 2018;247:26–33.
Zhu Y, Scholle F, Kisthardt SC, Xie DY. Flavonols and dihydroflavonols inhibit the main protease activity of SARS-CoV-2 and the replication of human coronavirus 229E. Virology. 2022;571:21–33.
Johnson TO, Adegboyega AE, Ojo OA, Yusuf AJ, Iwaloye O, Ugwah-Oguejiofor CJ, Asomadu RO, Chukwuma IF, Ejembi SA, Ugwuja EI, Alotaibi SS, Albogami SM, Batiha GE, Rajab BS, Conte-Junior CA. A computational approach to elucidate the interactions of chemicals from Artemisia annua targeted toward SARS-CoV-2 main protease inhibition for COVID-19 treatment. Front Med. 2022;9: 907583.
Gaudry A, Bos S, Viranaicken W, Roche M, Krejbich-Trotot P, Gadea G, Desprès P, El-Kalamouni C. The flavonoid isoquercitrin precludes initiation of Zika virus infection in human cells. Int J Mol Sci. 2018;19(4):1093.
Wong G, He S, Siragam V, Bi Y, Mbikay M, Chretien M, Qiu X. Antiviral activity of quercetin-3-β-O-D-glucoside against Zika virus infection. Virol Sin. 2017;32(6):545–7.
dos Santos AE, Kuster RM, Yamamoto KA, Salles TS, Campos R, de Meneses MD, Soares MR, Ferreira D. Quercetin and quercetin 3-O-glycosides from Bauhinia longifolia (Bong) steud show anti-mayaro virus activity. Parasit Vectors. 2014;7:130.
Kim CH, Kim JE, Song YJ. antiviral activities of quercetin and isoquercitrin against human herpesviruses. Molecules. 2020;25(10):2379.
Dai J, Gu L, Su Y, Wang Q, Zhao Y, Chen X, Deng H, Li W, Wang G, Li K. Inhibition of curcumin on influenza A virus infection and influenzal pneumonia via oxidative stress, TLR2/4, p38/JNK MAPK and NF-κB pathways. Int Immunopharmacol. 2018;54:177–87.
Dai JP, Wang QW, Su Y, Gu LM, Zhao Y, Chen XX, Chen C, Li WZ, Wang GF, Li KS. Emodin inhibition of influenza A virus replication and influenza viral pneumonia via the Nrf2, TLR4, p38/JNK and NF-kappaB pathways. Molecules. 2017;22(10):1754.
Ilyushina NA, et al. Comparative study of influenza virus replication in MDCK cells and in primary cells derived from adenoids and airway epithelium. J Virol. 2012;86:11725–34.
Kim Y, Narayanan S, Chang KO. Inhibition of influenza virus replication by plant-derived isoquercetin. Antiviral Res. 2010;88(2):227–35.
Smee DF, Hurst BL, Wong MH, Bailey KW, Tarbet EB, Morrey JD, Furuta Y. Effects of the combination of favipiravir (T-705) and oseltamivir on influenza A virus infections in mice. Antimicrob Agents Chemother. 2010;54(1):126–33.
Klomp M, Ghosh S, Mohammed S, Nadeem KM. From virus to inflammation, how influenza promotes lung damage. J Leukoc Biol. 2021;110(1):115–22.
Teijaro JR, Walsh KB, Cahalan S, Fremgen DM, Roberts E, Scott F, Martinborough E, Peach R, Oldstone MB, Rosen H. Endothelial cells are central orchestrators of cytokine amplification during influenza virus infection. Cell. 2011;146(6):980–91.
Kumar N, Xin ZT, Liang Y, Ly H, Liang Y. NF-kappaB signaling differentially regulates influenza virus RNA synthesis. J Virol. 2008;82(20):9880–9.
Heikkinen T, Ikonen N, Ziegler T. Impact of influenza B lineage-level mismatch between trivalent seasonal influenza vaccines and circulating viruses, 1999–2012. Clin Infect Dis. 2014;59(11):1519–24.
Shi Y, Zhang B, Lu Y, Qian C, Feng Y, Fang L, Ding Z, Cheng D. Antiviral activity of phenanthrenes from the medicinal plant Bletilla striata against influenza A virus. BMC Complement Altern Med. 2017;17(1):273.
Garcia V, Aris-Brosou S. Comparative dynamics and distribution of influenza drug resistance acquisition to protein M2 and neuraminidase inhibitors. Mol Biol Evol. 2014;31(2):355–63.
Zhu Q, Bang TH, Ohnuki K, Sawai T, Sawai K, Shimizu K. Inhibition of neuraminidase by Ganoderma triterpenoids and implications for neuraminidase inhibitor design. Sci Rep. 2015;5:13194.
Hai R, Schmolke M, Leyva-Grado VH, Thangavel RR, Margine I, Jaffe EL, Krammer F, Solórzano A, García-Sastre A, Palese P, Bouvier NM. Influenza A(H7N9) virus gains neuraminidase inhibitor resistance without loss of in vivo virulence or transmissibility. Nat Commun. 2013;4:2854.
Tsedenbal N, Tsend-Ayush A, Badarch D, Jav S, Pagbajab N. Influenza B viruses circulated during last 5 years in Mongolia. PLoS ONE. 2018;13(11): e0206987.
Cáceres CJ, Hu Y, Cárdenas-García S, Wu X, Tan H, Carnaccini S, Gay LC, Geiger G, Ma C, Zhang QY, Rajao D, Perez DR, Wang J. Rational design of a deuterium-containing M2–S31N channel blocker UAWJ280 with in vivo antiviral efficacy against both oseltamivir sensitive and—resistant influenza A viruses. Emerg Microbes Infect. 2021;10(1):1832–48.
Ye M, Luo G, Ye D, She M, Sun N, Lu YJ, Zheng J. Network pharmacology, molecular docking integrated surface plasmon resonance technology reveals the mechanism of Toujie Quwen Granules against coronavirus disease 2019 pneumonia. Phytomedicine. 2021;85: 153401.
Kumar S, El-Kafrawy SA, Bharadwaj S, Maitra SS, Alandijany TA, Faizo AA, Khateb AM, Dwivedi VD, Azhar EI. Discovery of bispecific lead compounds from Azadirachta indica against ZIKA NS2B-NS3 protease and NS5 RNA dependent RNA polymerase using molecular simulations. Molecules. 2022;27(8):2562.
Peiris JS, Yu WC, Leung CW, Cheung CY, Ng WF, Nicholls JM, Ng TK, Chan KH, Lai ST, Lim WL, Yuen KY, Guan Y. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet. 2004;363(9409):617–9.
Lin CM, Cooles FA, Isaacs JD. Basic mechanisms of JAK inhibition. Mediterr J Rheumatol. 2020;31(Suppl 1):100–4.
Vanderbeke L, Van Mol P, Van Herck Y, De Smet F, Humblet-Baron S, Martinod K, Antoranz A, Arijs I, Boeckx B, Bosisio FM, Casaer M, Dauwe D, De Wever W, Dooms C, Dreesen E, Emmaneel A, Filtjens J, Gouwy M, Gunst J, Hermans G, Jansen S, Lagrou K, Liston A, Lorent N, Meersseman P, Mercier T, Neyts J, Odent J, Panovska D, Penttila PA, Pollet E, Proost P, Qian J, Quintelier K, Raes J, Rex S, Saeys Y, Sprooten J, Tejpar S, Testelmans D, Thevissen K, Van Buyten T, Vandenhaute J, Van Gassen S, Velásquez Pereira LC, Vos R, Weynand B, Wilmer A, Yserbyt J, Garg AD, Matthys P, Wouters C, Lambrechts D, Wauters E, Wauters J. Monocyte-driven atypical cytokine storm and aberrant neutrophil activation as key mediators of COVID-19 disease severity. Nat Commun. 2021;12(1):4117.
Dai JP, Wang QW, Su Y, Gu LM, Deng HX, Chen XX, Li WZ, Li KS. Oxymatrine inhibits influenza A virus replication and inflammation via TLR4, p38 MAPK and NF-κB pathways. Int J Mol Sci. 2018;19(4):965.
Shen X, Zhao Z, Wang H, Guo Z, Hu B, Zhang G. Elucidation of the anti-inflammatory mechanisms of bupleuri and scutellariae radix using system pharmacological analyses. Mediators Inflamm. 2017;2017:3709874.
de Jong MD, Simmons CP, Thanh TT, Hien VM, Smith GJ, Chau TN, Hoang DM, Chau NV, Khanh TH, Dong VC, Qui PT, Cam BV, do Ha Q, Guan Y, Peiris JS, Chinh NT, Hien TT, Farrar J. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat Med. 2006;12(10):1203–7.
He D, Chiu AP, Lin Q, Yu D. Spatio-temporal patterns of proportions of influenza B cases. Sci Rep. 2017;7:40085.
Zaraket H, Hurt AC, Clinch B, Barr I, Lee N. Burden of influenza B virus infection and considerations for clinical management. Antiviral Res. 2021;185: 104970.
Sharma A, Anumanthan G, Reyes M, Chen H, Brubaker JW, Siddiqui S, Gupta S, Rieger FG, Mohan RR. Epigenetic modification prevents excessive wound healing and scar formation after glaucoma filtration surgery. Invest Ophthalmol Vis Sci. 2016;57(7):3381–9.
Liu G, Franssen E, Fitch MI, Warner E. Patient preferences for oral versus intravenous palliative chemotherapy. J Clin Oncol. 1997;15:110–5.
Li Y, Cao H, Liu M, Zhang B, Zhang X, Shi D, Guo L, Duan J, Zhou X, Zhu H, Zhang Q. Different modulation of Panax notoginseng on the absorption profiling of triptolide and tripterine from Tripterygium wilfordii in rat intestine. Chin Med. 2018;13:1.
Sima M, Lv C, Qi J, Guo J, Luo R, Deng X, Li Y, Wang T, Yue D, Gao Y. Anti-inflammatory effects of theaflavin-3′-gallate during influenza virus infection through regulating the TLR4/MAPK/p38 pathway. Eur J Pharmacol. 2023;938: 175332.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Key Research and Development Program of China (2021YFC2301701), the Youth Science and Technology Innovation Outstanding Talents Special Project of Jilin Provincial Department of Science and Technology (NO.20210509004RQ) and the National Natural Science Foundation of Jilin (NO.YDZJ202201ZYTS174).
Author information
Authors and Affiliations
Contributions
YG, DY and TW designed experiments and provided guidance. Experiments were performed by RL and CL. XD and Mingwei Sima provided drugs. All viruses used in this research were provided by YL, WS. JG and JQ provided experimental guidance and manuscript revision.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Animal experiments were conducted following the protocols of Changchun Veterinary Research Institute, Chinese Academy of Agricultural Sciences (Approval Number: IACUC of AMMS-11-2022-036). Additionally, all influenza virus infection experiments are conducted in a biosafety level 2 laboratory of Changchun Veterinary Research Institute, Chinese Academy of Agricultural Sciences according to biosafety regulations.
Consent for publication
All authors consent to publish this manuscript.
Competing interests
Authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Fig. S1. The effect of timing of drug administration and dose on anti-IAV A–B and anti-IBV C–D activity of isoquercitrin in MDCK cells and A549 cells. Colors annotate three drug administration protocols, pre-treatment (gray), co-treatment (black) and post-treatment (pink). Fig. S2. Effect of isoquercitrin on pathological damage caused by influenza virus infection. A HE staining of heart, liver, spleen and kidney tissues in influenza virus-infected mice and drug-treated mice at 5 dpi. B Immunohistochemistry staining of heart, liver, spleen and kidney tissues in influenza virus-infected mice and drug-treated mice at 5 dpi. C The percentage of NP positive cells in main tissues (heart, liver, spleen, kidney) in B. Fig. S3. Isoquercitrin inhibits cytokines induced by influenza A virus infection. Relative mRNA expression level of type I IFN (IFN-α and IFN-β), pro-inflammatory cytokines (TNF-α, IL-6 and IL-1β), anti-inflammatory cytokine (IL-10) and IFN induced gene (ISG54 and ISG56) in mouse lung tissues of each group at 5 dpi.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Luo, R., Lv, C., Wang, T. et al. A potential Chinese medicine monomer against influenza A virus and influenza B virus: isoquercitrin. Chin Med 18, 144 (2023). https://doi.org/10.1186/s13020-023-00843-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13020-023-00843-4