Abstract
Background
Abnormal body mass index (BMI) has been related to a higher risk of adverse outcomes in patients undergoing cardiac surgery. However, the effects of BMI in patients with acute type A aortic dissection (AAAD) on postoperative outcomes remain unclear. This study aimed to explore the relationships between BMI and in-hospital major adverse outcomes (MAO) in AAAD patients.
Methods
Patients who underwent AAAD surgery at Cardiac Medical Center of Fujian Province from June 2013 to March 2020 were retrospectively evaluated. They were divided into three groups on the basis of Chinese BMI classification established by the World Health Organization: normal weight group (BMI 18.5–23.9 kg/m2), overweight group (BMI 24–27.9 kg/m2), and obese group (BMI >28 kg/m2). Patients’ baseline characteristics, preoperative, operative, and postoperative data were collected. A multivariable logistic regression analysis model was performed to identify the association between BMI and MAO in AAAD patients.
Results
Of 777 cases, 31.9% were normal weight, 52.5% were overweight, and 15.6% were obese. A total of 160(20.6%) patients died in-hospital. There was a significant difference between the three groups for MAO (62.9% vs 72.1% vs 77.7%, respectively, P = 0.006). The incidence of postoperative complications did not differ among the three groups, except for postoperative bleeding, and prolonged mechanical ventilation, the proportion of which were higher in the overweight and obese groups. Besides, multivariable logistic regression analysis demonstrated that a higher risk of MAO in the overweight [odds ratios (ORs):1.475, 95%CI:1.006–2.162], and obese patients (ORs:2.147, 95%CI:1.219–3.782) with reference to the normal weight patients, and age, white blood cell, prior stroke and cardiopulmonary bypass time were also associated with in-hospital MAO (P<0.05).
Conclusions
BMI is independently associated with higher in-hospital MAO in patients who underwent AAAD surgery.
Similar content being viewed by others
Background
Obesity is generally considered to be a strong risk factor for morbidity and mortality during the perioperative period in patients with heart disease [1]. Studies have reported obesity patients who underwent cardiac surgery were associated with adverse outcomes in recent years [2, 3]. However, some reports suggest that obesity is unable to increase the incidence rate of in-hospital mortality and even reduce it [4, 5]. The improved survival and functional outcomes in overweight and obese cardiac surgery patients are termed as the ‘obesity paradox’ in the literature [6].
So far, the ‘obesity paradox’ has been demonstrated in patients undergoing coronary artery bypass grafting or valve surgery [7,8,9]. However, it has not been fully studied in patients with acute type A aortic dissection (AAAD). Only two studies have evaluated the effect of body mass index (BMI) on postoperative clinical outcomes in patients with AAAD [10, 11], but the study was in western countries whose cases were categorized by the World Health Organization (WHO) standard. Considering ethnic differences, the WHO standard of BMI is not suitable for the Chinese population which the results of the mentioned studies might therefore not be valid for. No existing studies have reported the associations between BMI and adverse outcomes in AAAD patients undergoing surgery. Moreover, it is unknown whether the ‘obesity paradox’ in Chinese AAAD patients exists. This study adopted the Chinese BMI classification standard to determine the relationship between BMI and in-hospital major adverse outcomes (MAO) in patients with AAAD.
Methods
Study population
This retrospective study enrolled 777 consecutive patients aged 18–80 years at Cardiac Medical Center of Fujian Province that underwent AAAD surgery between June 2013 and March 2020.
Patients with the following conditions were excluded: (1) Pregnant women; (2) Patients with malignancy; (3) Traumatic dissection; (4) Patients lost to follow-up within 30 days; (5) Patients with incomplete clinical data.
All patients were divided into three groups on the basis of Chinese BMI classification established by WHO: BMI = 18.5–23.9 kg/m2(normal weight group); BMI = 24–27.9 kg/m2(overweight group); BMI>28 kg/m2(obese group). Underweight patients (BMI<18.5 kg/m2) were excluded to avoid biased results because of the small sample size. Ethics approval has been obtained from the ethics committee of Fujian Medical University Union Hospital (approval number:2013002) and conformed to the Declaration of Helsinki.
Data collection
All data were collected by two investigators who had been uniformly trained, including baseline characteristics, preoperative characteristics, intraoperative, and postoperative data. The primary outcomes were frequency of in-hospital MAO and mortality. According to the consensus statement from the International Aortic Arch Surgery Study Group [12], MAO in this study were defined as the events including death, stroke, myocardial infarction, low cardiac output syndrome, arrhythmia, aortic dissection rupture, respiratory insufficiency, acute renal failure, gastrointestinal bleeding, deep sternal wound infection, septicemia, postoperative bleeding, prolonged mechanical ventilation (MV). Besides, the duration of intensive care unit (ICU) stays and hospital stays were also recorded.
Criteria
In-hospital mortality was defined as both all-cause deaths occurring during the hospitalization or in the first 30 postoperative days despite discharge status [13]. Stroke was defined as acute onset focal neurologic deficit caused by a disturbance in blood supply to the brain that last ≥24 h [14]. Acute renal failure was defined as a creatinine level that was 3 times higher than preoperative creatinine or a new requirement for dialysis [15]. Respiratory insufficiency was defined as one of the following conditions: atelectasis, pneumonia, pulmonary edema, or acute respiratory distress syndrome, requiring intubation >72 h or a tracheostomy [12]. Prolonged mechanical ventilation was defined as the duration of mechanical ventilation (>48 h) [16].
Statistical analysis
Continuous variables were presented as mean ± standard deviation (SD) or median (interquartile range), based on Gaussian distribution, and categorical variables were presented as numbers/percentages. Continuous variables were analyzed using analysis of variance (ANOVA) or the Kruskal-Wallis tests, and categorical variables were done using Chi-squared test or Fisher’s exact test. Multivariable logistic regression analyses were done to assess the relationship between BMI and in-hospital MAO, introducing variables with P<0.1 on univariate analysis and based on professional knowledge. Data were performed using the Statistical Package for the Social Science (IBM-SPSS version 23.0). P<0.05 was considered to be statistically significant.
Results
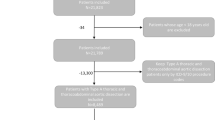
From June 2013 to March 2020, a total of 807 AAAD patients aged 18–80 years received surgical treatment. We excluded 5 pregnant women, 2 patients caused by traffic accidents, 1 patient had malignancy, 14 with incomplete data, and 8 lost to follow-up. Finally, a cohort of 777 AAAD patients was enrolled. The flow chart of patient inclusion is demonstrated in Fig. 1.
Table 1 shows the baseline characteristics of the three groups. Among the 777 AAAD patients, 248(31.9%) were classified into the normal weight group with a BMI of (21.7 ± 1.5) kg/m2, 408(52.5%) were classified into the overweight group with a BMI of (25.4 ± 1.0) kg/m2, and 121(15.6%) patients were classified into the obese group with a BMI of (31.6 ± 6.5) kg/m2. The youngest age was seen in the obese group (age of 48.5 ± 11.5 years, P<0.001) as compared with the overweight and normal weight groups, and with a high proportion of male, drinker, and Marfan syndrome (P<0.05). There was no significant difference in smoker, the history of hypertension, type 2 diabetes, previous cardiac surgery, coronary artery heart disease, prior stroke, prior shock, prior resuscitation, extension of AAAD, and time from symptom onset to surgery among the three groups (P>0.05).
Patient preoperative, and operative variables are summarized in Table 2. The mean of systolic blood pressure (BP) was much higher in the obese group compared with the overweight and normal weight groups(147.1 ± 27.9 vs 143.6 ± 31.0 vs 133.7 ± 27.4, respectively; P<0.001), the same with diastolic BP (78.1 ± 15.7 vs 76.8 ± 17.8 vs 71.9 ± 14.7, respectively; P<0.001), and pulse pressure (69.0 ± 22.8 vs 67.0 ± 23.5 vs 61.7 ± 21.1, respectively, P = 0.003). The obese patients had higher white blood cell counts (WBC), hemoglobin, and serum creatinine compared to the normal weight and overweight patients (P<0.05). No significant differences were observed among other preoperative and operative variables (P>0.05).
As shown in Table 3, the in-hospital mortality was no significant difference among the three groups(16.9% vs 21.8% vs 24.0%, respectively; P = 0.198), but there was a significant difference among three groups in MAO (62.9% vs 72.1% vs 77.7%, respectively; P<0.006). The duration of ICU stays was the longest in the obese group followed by the overweight and normal weight groups [12.0 (10.0, 14.1) vs 9.5 (8.6, 10.5) vs 8.1 (7.1, 9.2), respectively; P = 0.001], which was corresponded to the hospital stays [27.4 (24.3, 30.5) vs 22.6 (21.3, 23.9) vs 21.0 (19.8, 22.2), respectively; P<0.001]. No significant difference was present in stroke, myocardial infarction, low cardiac output syndrome, arrhythmia, aortic dissection rupture, respiratory insufficiency, acute renal failure, gastrointestinal bleeding, deep sternal wound infection, septicemia among the three groups(P>0.05) except prolonged MV (44.8% vs 55.6% vs 66.1%, respectively; P<0.001), and postoperative bleeding (0.8% vs 0.5% vs 3.3%, respectively, P = 0.024).
The results of the multivariable logistic regression analysis are presented in Table 4. It demonstrated a higher risk of in-hospital MAO in the overweight (ORs:1.475, 95%CI:1.006–2.162), and obese patients (ORs: 2.147, 95%CI:1.219–3.782) with reference to the normal weight patients. Besides, WBC (ORs:1.111, 95%CI:1.058–1.167), age (ORs:1.030, 95%CI:1.014–1.047), cardiopulmonary bypass (CPB) time (ORs:1.005, 95%CI:1.002–1.008), and prior stroke (ORs:7.525, 95%CI:1.740–32.552) were associated with MAO(P < 0.05).
Discussion
Several previous studies have investigated the impact of BMI on the prognosis of cardiac disease [10, 11], but the conclusions remain in dispute. The present study is innovative to demonstrate the impact of BMI on MAO in Chinese AAAD patients undergoing surgery. A total of 777 AAAD patients were included in the study, which we found that the incidence of in-hospital mortality was 20.6%. We observed BMI was independently associated with MAO of patients with AAAD, and patients who were overweight and obese were significantly longer in the duration of ICU stays and hospital stays compared with the normal group. Besides, WBC, age, CPB time, and prior stroke were significantly and strongly related to MAO in patients following AAAD surgery, even after adjusting for other risk factors. Therefore, BMI was a useful marker to stratify the high-risk patients with AAAD.
It is unclear why overweight and obese affects the prognosis of AAAD patients, but variability in adherence to DNA methylation or adipose tissue in overweight and obese patients may explain our observations. Recently, Dr. Simone Wahl and colleagues carried out studies [17] about epigenome-wide association amongst 5387 individuals from three different population, demonstrating that alterations in DNA methylation are more likely to be the consequence of overweight or obesity, which methylation loci are related to lipid and lipoprotein metabolism, substrate transport, and inflammatory pathways. In addition, large amounts of bioactive mediators can be released from the adipose tissue, affecting blood pressure, inflammation, and other changes, and lead to endothelial dysfunction and arteriosclerosis [18]. Based on these analyses, it could be concluded that overweight and obese may affect postoperative inflammatory reactions in AAAD patients, thus lead to an increase in mortality.
Although there is a huge amount of literature in support of the concept of the ‘obesity paradox’, which indicates that a protective effect or no effect was observed in overweight or even obese on adverse outcomes [6]. However, a recent network meta-analysis suggested that the ‘obesity paradox’ disappeared in Asians, which is consistent with our results [8]. Lio et al. reported that obese patients were more likely to develop postoperative mortality and adverse outcomes compared to non-obese patients [10]. Kreibich et al. pointed out that obesity was not significantly associated with postoperative adverse outcomes in AAAD patients [11]. Our findings indicated that overweight and obese are at increased risk of MAO in AAAD patients, which wasn’t consistent with Kreibich’s studies. The inconsistency might be explained by the three follows: first, BMI showed great differences in different racial persons and especially between the Caucasian and the yellow race [19]; second, the BMI cutoffs of underweight, normal weight, overweight and obese in Chinese are different from those in other countries; third, there are differences between the studies at baseline, for example, patients with acute aortic dissection (AAD) in China had an earlier onset about 10 years than the International Registry of Acute Aortic Dissection [20]. Finally, the body fat content of Asian people is generally higher than white people of the same gender, age, and BMI even if their BMI is less than 25 kg/m2, they are more likely to develop type II diabetes and cardiovascular disease [21]. Therefore, it is not surprising that the results are quite different.
In this study, we found that the longer ICU stay and the higher proportion of prolonged MV in the overweight and obese group, whose finding was compatible with those of other studies [22, 23]. The reasons could be as follows: (1) The proportion of smokers is higher in overweight and obese groups when compared to the normal group respectively. The decreased pulmonary function in smokers may lead to the inconsistency of baseline lung function on admission in different BMI groups. In this study, the group with a higher proportion of smokers has a higher incidence of prolonged MV. (2) The adipose tissue creates a number of estrogens in overweight and obese patients that play an important role in pulmonary hypertension and remodeling [24]. It generally focuses on the changes in pulmonary and chest wall structures, which led to the increase of residual lung volume and chest wall impedance, a decrease of lung compliance and ventilation driving force, and abnormal ventilation-perfusion [25]. Furthermore, reduction or loss of lung volume due to the weight of adipose tissue can occur in obese or overweight patients during operation [26], leading to impaired lung function and delayed extubation. And prolonged time on mechanical ventilation may result in prolonged ICU stay and vice versa [27]. In summary, medical staff should establish reasonable ventilation strategies to shorten the length of mechanical ventilation and ICU stay.
An important finding of this study is that the MAO in AAAD patients was associated with age. It has been reported that age was an established risk factor for perioperative adverse outcomes in AAAD patients [28, 29]. Then we have a deep analysis of reasons. In the first instance, elderly patients are often poorly performed having asymptomatic clinical features in comparison with the young patients which usually led to a delay in diagnosis and treatment. It may also reflect that patients do not obtain timely medical attention [30]. Secondly, it is known that older patients often suffered from concomitant comorbidities, such as hypertension, coronary heart, diabetes, and a history of cardiac surgery. That means older patients are more serious when they arrive at the hospital, which may thereby lead to a worse surgical prognosis. Moreover, compared with younger, older patients were more seem to have a poor prognosis due to their low cardiopulmonary reserve, and the poor responses to cardiopulmonary bypass surgery, anesthesia, various drugs, and fluid infusion. The elderly people are more physically to have weakness [31, 32], which can cause physiological disorders including heart rate variability, systemic inflammatory states, a decline in immune function, and hormonal changes [33,34,35], and thus increased risk of mortality.
Another notable finding was that WBC, CPB time, and prior stroke were the independent factors for MAO. There are multiple lines of studies and clinical observations that suggest that the inflammatory process plays an important role in the progress and prognosis of aortic dissection [36]. WBC is a sensitive marker of the non-specific inflammatory response, demonstrated as a strong independent predictor of in-hospital clinical events for AAAD patients in previous studies [8, 37]. Elevated WBC count directly reflects acute inflammatory reaction and the extent of aortic injury in aortic dissection, which may result in an endothelial injury, procoagulant reaction, and microvascular injury, increase the release of vascular toxic factors and finally lead to an increased risk of adverse outcomes [38]. In addition, the CPB time is particularly associated with mortality in AAAD patients that has been observed by other investigators as well [39]. The longer the CPB time, the longer the organ is in the relative ischemic state, the greater the probability of ischemic injury after the operation, leading to serious complications and even death. We noted that patients who had a prior stroke had significantly higher adverse outcomes, as reported previously [40, 41]. This may be explained that these patients are necessary to guarantee sufficient cerebral perfusion due to a higher cerebral perfusion pressure during CPB, which is more vulnerable to hemodynamic instability. For the above reasons, the incidence of MAO will inevitably increase.
However, there are several limitations. First, this was a single-center retrospective study which has its inherent shortcomings, and the findings may not be generalizable to other regions. Second, the measure of body proportion relies solely on BMI which does not yield information on the distribution of body fat. Third, the follow-up period (30 days) in this study was relatively shorter, further studies with longer follow-up periods would be explored to provide additional insight into the impact of BMI on long-term prognosis. Finally, we excluded the underweight patients (<18.5 kg/m2) with a small sample size in order to avoid the error of the results, which may affect the results when their cases are large enough.
Conclusions
In summary, the present study demonstrates that BMI is independently associated with higher MAO in patients who underwent AAAD surgery. And WBC, age, CPB time, and prior stroke are significant factors for MAO. The focus should be placed on overweight and obese patients in risk assessment before surgery. Further works need to provide additional insight into the impact of BMI on long-term prognosis.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MAO:
-
Major adverse outcomes
- BMI:
-
Body mass index
- AAAD:
-
Acute type A aortic dissection
- CPB:
-
Cardiopulmonary bypass
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- ANOVA:
-
Analysis of variance
- ORs:
-
Odds ratios
- CI:
-
Confidence intervals
- WHO:
-
World Health Organization
- SOFA:
-
The Sequential Organ Failure Assessment
- SPSS:
-
The Statistical Package for the Social Science
- AAD:
-
Acute aortic dissection
- WBC:
-
White blood cell
- BP:
-
Blood pressure
- PP:
-
Pulse pressure
- ICU:
-
Intensive care unit
- MV:
-
Mechanical ventilation
- BUN:
-
Blood urea nitrogen
References
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9(1):88. https://doi.org/10.1186/1471-2458-9-88.
Gao M, Sun J, Young N, Boyd D, Atkins Z, Li Z, Ding Q, Diehl J, Liu H. Impact of body mass index on outcomes in cardiac surgery. J Cardiothorac Vasc Anesth. 2016;30(5):1308–16. https://doi.org/10.1053/j.jvca.2016.03.002.
Ghanta RK, LaPar DJ, Zhang Q, et al. Obesity increases risk-adjusted morbidity, mortality, and cost following cardiac surgery. J Am Heart Assoc. 2017;6(3):e003831.
Engel AM, Mcdonough S, Smith JM. Does an obese body mass index affect hospital outcomes after coronary artery bypass graft surgery? Ann Thorac Surg. 2009;88(6):1793–800. https://doi.org/10.1016/j.athoracsur.2009.07.077.
Borracci RA, Ingino CA, Miranda JM. Association of body mass index with short-term outcomes after cardiac surgery: retrospective study and meta-analysis. Medicina. 2018;78(3):171–9.
Doehner W, Clark A, Anker SD. The obesity paradox: weighing the benefit. Eur Heart J. 2010;31(2):146–8. https://doi.org/10.1093/eurheartj/ehp339.
Rapetto F, Bruno VD, King M, Benedetto U, Caputo M, Angelini GD, Ascione R, Ciulli F, Vohra HA. Impact of body mass index on outcomes following mitral surgery: does an obesity paradox exist? Interact Cardiovasc Thorac Surg. 2018;26(4):590–5. https://doi.org/10.1093/icvts/ivx383.
Ma WQ, Sun XJ, Wang Y, Han XQ, Zhu Y, Liu NF. Does body mass index truly affect mortality and cardiovascular outcomes in patients after coronary revascularization with percutaneous coronary intervention or coronary artery bypass graft? A systematic review and network meta-analysis. Obes Rev. 2018;19(9):1236–47. https://doi.org/10.1111/obr.12713.
Johnson AP, Parlow JL, Whitehead M, et al. Body mass index, outcomes, and mortality following cardiac surgery in Ontario, Canada. J Am Heart Assoc. 2015;4(7):e002140.
Lio A, Bovio E, Nicolò F, Saitto G, Scafuri A, Bassano C, Chiariello L, Ruvolo G. Influence of body mass index on outcomes of patients undergoing surgery for acute aortic dissection: a propensity-matched analysis. Tex Heart Inst J. 2019;46(1):7–13. https://doi.org/10.14503/THIJ-17-6365.
Kreibich M, Rylski B, Bavaria JE, Branchetti E, Dohle D, Moeller P, Vallabhajosyula P, Szeto WY, Desai ND. Outcome after operation for aortic dissection type a in morbidly obese patients. Ann Thorac Surg. 2018;106(2):491–7. https://doi.org/10.1016/j.athoracsur.2018.03.035.
Yan TD, Tian DH, LeMaire SA, et al. Standardizing clinical end points in aortic arch surgery: a consensus statement from the international aortic arch surgery study group. Circulation. 2014;129(15):1610–6. https://doi.org/10.1161/CIRCULATIONAHA.113.006421.
Allama A, Ibrahim I, Abdallah A, Ashraf S, Youhana A, Kumar P, Bhatti F, Zaidi A. Effect of body mass index on early clinical outcomes after cardiac surgery. Asian Cardiovasc Thorac Ann. 2014;22(6):667–73. https://doi.org/10.1177/0218492313504092.
Debette S, Seshadri S, Beiser A, Au R, Himali JJ, Palumbo C, Wolf PA, DeCarli C. Midlife vascular risk factor exposure accelerates structural brain aging and cognitive decline. Neurology. 2011;77(5):461–8. https://doi.org/10.1212/WNL.0b013e318227b227.
Koza Y. Acute kidney injury: current concepts and new insights. J Inj Violence Res. 2016;8(1):58–62. https://doi.org/10.5249/jivr.v8i1.610.
Kimura N, Tanaka M, Kawahito K, Sanui M, Yamaguchi A, Ino T, Adachi H. Risk factors for prolonged mechanical ventilation following surgery for acute type a aortic dissection. Circ J. 2008;72(11):1751–7. https://doi.org/10.1253/circj.CJ-08-0306.
Wahl S, Drong A, Lehne B, Loh M, Scott WR, Kunze S, Tsai PC, Ried JS, Zhang W, Yang Y, Tan S, Fiorito G, Franke L, Guarrera S, Kasela S, Kriebel J, Richmond RC, Adamo M, Afzal U, Ala-Korpela M, Albetti B, Ammerpohl O, Apperley JF, Beekman M, Bertazzi PA, Black SL, Blancher C, Bonder MJ, Brosch M, Carstensen-Kirberg M, de Craen AJM, de Lusignan S, Dehghan A, Elkalaawy M, Fischer K, Franco OH, Gaunt TR, Hampe J, Hashemi M, Isaacs A, Jenkinson A, Jha S, Kato N, Krogh V, Laffan M, Meisinger C, Meitinger T, Mok ZY, Motta V, Ng HK, Nikolakopoulou Z, Nteliopoulos G, Panico S, Pervjakova N, Prokisch H, Rathmann W, Roden M, Rota F, Rozario MA, Sandling JK, Schafmayer C, Schramm K, Siebert R, Slagboom PE, Soininen P, Stolk L, Strauch K, Tai ES, Tarantini L, Thorand B, Tigchelaar EF, Tumino R, Uitterlinden AG, van Duijn C, van Meurs JBJ, Vineis P, Wickremasinghe AR, Wijmenga C, Yang TP, Yuan W, Zhernakova A, Batterham RL, Smith GD, Deloukas P, Heijmans BT, Herder C, Hofman A, Lindgren CM, Milani L, van der Harst P, Peters A, Illig T, Relton CL, Waldenberger M, Järvelin MR, Bollati V, Soong R, Spector TD, Scott J, McCarthy MI, Elliott P, Bell JT, Matullo G, Gieger C, Kooner JS, Grallert H, Chambers JC. Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature. 2017;541(7635):81–6. https://doi.org/10.1038/nature20784.
Oikonomou EK, Antoniades C. The role of adipose tissue in cardiovascular health and disease. Nat Rev Cardiol. 2019;16(2):83–99. https://doi.org/10.1038/s41569-018-0097-6.
Heymsfield SB, Peterson CM, Thomas DM, Heo M, Schuna JM Jr, Hong S, Choi W. Scaling of adult body weight to height across sex and race/ethnic groups: relevance to BMI. Am J Clin Nutr. 2014;100(6):1455–61. https://doi.org/10.3945/ajcn.114.088831.
Wang W, Duan W, Xue Y, et al. Clinical features of acute aortic dissection from the registry of aortic dissection in China. J Thorac Cardiovasc Surg. 2014;148(6):2995–3000. https://doi.org/10.1016/j.jtcvs.2014.07.068.
Ko T, Higashitani M, Sato A, Uemura Y, Norimatsu T, Mahara K, Takamisawa I, Seki A, Shimizu J, Tobaru T, Aramoto H, Iguchi N, Fukui T, Watanabe M, Nagayama M, Takayama M, Takanashi S, Sumiyoshi T, Komuro I, Tomoike H. Impact of acute kidney injury on early to long-term outcomes in patients who underwent surgery for type a acute aortic dissection. Am J Cardiol. 2015;116(3):463–8. https://doi.org/10.1016/j.amjcard.2015.04.043.
Sharma V, Rao V, Manlhiot C, Boruvka A, Fremes S, Wąsowicz M. A derived and validated score to predict prolonged mechanical ventilation in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2017;153(1):108–15. https://doi.org/10.1016/j.jtcvs.2016.08.020.
Fernandez-Zamora MD, Gordillo-Brenes A, Banderas-Bravo E, Arboleda-Sánchez JA, Hinojosa-Pérez R, Aguilar-Alonso E, Herruzo-Aviles Á, Curiel-Balsera E, Sánchez-Rodríguez Á, Rivera-Fernández R, the ARIAM Andalucía Group. Prolonged mechanical ventilation as a predictor of mortality after cardiac surgery. Respir Care. 2018;63(5):550–7. https://doi.org/10.4187/respcare.04915.
Mair KM, Harvey KY, Henry AD, Hillyard DZ, Nilsen M, MacLean MR. Obesity alters oestrogen metabolism and contributes to pulmonary arterial hypertension. Eur Respir J. 2019;53(6):1801524. https://doi.org/10.1183/13993003.01524-2018.
Dixon AE, Peters U. The effect of obesity on lung function. Expert Rev Respir Med. 2018;12(9):755–67. https://doi.org/10.1080/17476348.2018.1506331.
Imber DA, Pirrone M, Zhang C, Fisher DF, Kacmarek RM, Berra L. Respiratory Management of Perioperative Obese Patients. Respir Care. 2016;61(12):1681–92. https://doi.org/10.4187/respcare.04732.
Li B, Sun G, Cheng Z, Mei C, Liao X, Li J, Yuan Y. Analysis of nosocomial infections in post-cardiac surgery extracorporeal membrane oxygenation support therapy. Heart Surg Forum. 2018;21(5):E387–e391. https://doi.org/10.1532/hsf.1789.
Huang B, Chen Z, Lu H, Zhao Z, Hui R, Yang Y, Fan X. Influence of age on clinical presentation, therapeutic options, and outcome in Chinese patients with acute aortic dissection. Int Heart J. 2019;60(6):1373–80. https://doi.org/10.1536/ihj.18-532.
Trimarchi S, Eagle KA, Nienaber CA, et al. Role of age in acute type a aortic dissection outcome: report from the international registry of acute aortic dissection (IRAD). J Thorac Cardiovasc Surg. 2010;140(4):784–9. https://doi.org/10.1016/j.jtcvs.2009.11.014.
Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Catheter Cardiovasc Interv. 2010;76(2):E43–86.
Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J, Fried LP. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6):901–8. https://doi.org/10.1016/j.jamcollsurg.2010.01.028.
Lin HS, Watts JN, Peel NM, Hubbard RE. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr. 2016;16(1):157. https://doi.org/10.1186/s12877-016-0329-8.
Varadhan R, Chaves PH, Lipsitz LA, et al. Frailty and impaired cardiac autonomic control: new insights from principal components aggregation of traditional heart rate variability indices. J Gerontol A Biol Sci Med Sci. 2009;64(6):682–7.
Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 2018;15(9):505–22. https://doi.org/10.1038/s41569-018-0064-2.
Wilson D, Jackson T, Sapey E, Lord JM. Frailty and sarcopenia: the potential role of an aged immune system. Ageing Res Rev. 2017;36:1–10. https://doi.org/10.1016/j.arr.2017.01.006.
Cifani N, Proietta M, Tritapepe L, di Gioia C, Ferri L, Taurino M, del Porto F. Stanford-a acute aortic dissection, inflammation, and metalloproteinases: a review. Ann Med. 2015;47(6):441–6. https://doi.org/10.3109/07853890.2015.1073346.
Wen D, Wu HY, Jiang XJ, Zhang HM, Zhou XL, Li JJ, Hui RT. Role of plasma C-reactive protein and white blood cell count in predicting in-hospital clinical events of acute type a aortic dissection. Chin Med J. 2011;124(17):2678–82.
Libby P, Nahrendorf M, Swirski FK. Leukocytes link local and systemic inflammation in ischemic cardiovascular disease: an expanded "cardiovascular continuum". J Am Coll Cardiol. 2016;67(9):1091–103. https://doi.org/10.1016/j.jacc.2015.12.048.
Wei J, Chen Z, Zhang H, Sun X, Qian X, Yu C. In-hospital major adverse outcomes of acute type a aortic dissection. Eur J Cardiothorac Surg. 2019;55(2):345–50. https://doi.org/10.1093/ejcts/ezy269.
Kreibich M, Desai ND, Bavaria JE, Szeto WY, Vallabhajosyula P, Itagaki R, Okamura H, Kimura N, Yamaguchi A, Beyersdorf F, Czerny M, Rylski B. Preoperative neurological deficit in acute type a aortic dissection. Interact Cardiovasc Thorac Surg. 2020;30(4):613–9. https://doi.org/10.1093/icvts/ivz311.
Merkle J, Sabashnikov A, Liebig L, Weber C, Eghbalzadeh K, Liakopoulos O, Zeriouh M, Kuhn-Régnier F, Wahlers T. Factors predictive for early and late mortality after surgical repair for Stanford a acute aortic dissection. Perfusion. 2019;34(5):375–83. https://doi.org/10.1177/0267659118822947.
Acknowledgements
The authors thanks to the Cardiac Medical Center of Fujian Province.
Funding
This work was supported by grants from the Joint Finds for the innovation of science and Technology, Fujian province (Grant number: 2017Y9052) and Guiding project of science and technology department of Fujian province (Grant number:2017Y0038).
Author information
Authors and Affiliations
Contributions
L-YL and S-LL assessed the delirium of the subjects. Y-CP and QC collected socio-demographic and clinical data. X-ZH, Y-JL, and L-WC analyzed and interpreted the data; L-YL and QC drafted the manuscript; all authors critically revised the manuscript. All authors read and approved the final manuscript.
Authors’ information (optional)
Not applicable.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The work was conducted at the Department of Cardiac Surgery, Fujian Medical University Union Hospital. The study was approved by the Ethics Committee of Fujian Medical University Union Hospital (approval number:2013002). Informed consent was waived because of the retrospective nature of this study.
Consent for publication
Not applicable.
Competing interests
The Authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, L., Lin, Y., Chen, Q. et al. Association of body mass index with in-hospital major adverse outcomes in acute type A aortic dissection patients in Fujian Province, China: a retrospective study. J Cardiothorac Surg 16, 47 (2021). https://doi.org/10.1186/s13019-021-01432-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01432-y