Abstract
Background
Stability is essential for the normal healing of a sternotomy. Mechanical vibration transmittance may provide a new means of early detection of diastasis in the sternotomy and thus enable the prevention of further complications. We sought to confirm that vibration transmittance detects sternal diastasis in human tissue.
Methods
Ten adult human cadavers (8 males and 2 females) were used for sternal assessments with a device constructed in-house to measure the transmittance of a vibration stimulus across the median sternotomy at the second, third, and fourth costal cartilage. Intact bone was compared to two fixed bone junctions, namely a stable wire fixation and an unstable wire fixation with a 10 mm wide diastasis mimicking a widely rupturing sternotomy. A generalized Linear Mixed Model with the lme function was used to determine the ability of the vibration transmittance device to differentiate mechanical settings in the sternotomy.
Results
The transmitted vibration power was statistically significantly different between the intact chest and stable sternotomy closure, stable and unstable closure, as well as intact and unstable closure (t-values and p-values respectively: t = 6.87, p < 0.001; t = 7.41, p < 0.001; t = 14.3, p < 0.001). The decrease of vibration transmittance from intact to stable at all tested costal levels was 78%, from stable to unstable 58%, and from intact to unstable 91%. The vibration transmittance power was not statistically significantly different between the three tested costal levels (level 3 vs. level 2; level 4 vs. level 2; level 4 vs. level 3; t-values and p-values respectively t = − 0.36, p = 0.723; t = 0.35, p = 0.728; t = 0.71, p = 0.484).
Conclusions
Vibration transmittance analysis differentiates the intact sternum, wire fixation with exact apposition, and wire fixation with a gap. The gap detection capability is not dependent on the tested costal level. The method may prove useful in the early detection of sternal instability and warrants further exploration.
Similar content being viewed by others
Background
Median sternotomy is the most common access in open heart surgery. The estimated annual number of sternotomies in Finland is approximately 3800 per a population of 5.5 million, and the equivalent figure in the USA is about 500,000 per a population of 323 million [1, 2]. The disruption of sternal steel wire fixation occurs when the separating forces exceed the mechanical holding properties of the closure. The reported incidence of post-sternotomy instability ranges from 0.39 to 1.6% up to 6 months postoperatively [3,4,5]. Even minor instability may cause subjective symptoms and can progress to complete wound disruption often complicated by deep sternal wound infection. Early detection of sternal instability may enable preventative measures such as the use of supportive vests as well as surgical exploration and re-fixation of the wound that may prevent the later more severe complications [6,7,8]. Risk factors for instability include numerous patient factors, as well as operative and postoperative variables [9,10,11,12,13,14,15,16,17,18].
The mechanical stability of the bone fracture or osteotomy is crucial for the formation of a callus and the maturation phase of the lamellar bone [19]. Stability is also essential for successful bone healing after sternotomy [9, 10], but it is fairly difficult to measure. Detection of a failing sternotomy is commonly done by manual palpation, which is a subjective method and prone to misinterpretations [20]. Computed tomography offers only indirect information on sternal stability, and signs of sternal bone healing appear months after surgery [21,22,23], whereas sternal instability leading to wound disruption and infection most often occurs within the first month of the operation [3]. Ultrasound has been used to evaluate sternal nonunion and gross instability years after surgery [24], but the method obviously carries a risk of contaminating the wound in the immediate postoperative period.
Vibration transmittance has been used to assess bone fractures and bone density as well as dental and orthopedic implant stability [25,26,27]. With fixed input excitation, i.e. power emitted by the vibration actuator, the detected power measured by the accelerometer sensor acts as a measure of the mechanical integrity of the studied object. We have reported vibration transmittance as a tool to assess and follow postoperative sternal stability [28], and we postulated that non-invasive detection of early sternotomy diastasis could be possible. The aim of the present study was to describe vibration transmittance in the human sterna in a cadaver model. The hypothesis of the study was that vibration transmittance assessment could be used to differentiate intact, surgically fixated, and unstable sterna.
Methods
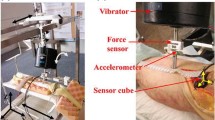
The study population consisted of 10 human cadavers. The age, height, weight, post-mortem time, soft tissue thickness, sternum thickness and presternal soft tissue temperature were recorded in each case, as shown in Table 1. The vibration transmittance measurement device used in this study was the third-generation version of an in-house-constructed, embedded vibration measurement system consisting of an actuator, a sensor, and a main controller unit. The device is compact, portable, and battery driven (Fig. 1). The actuator introduces a vibration stimulus to the tissue, sweeping a band of 20–2000 Hz over 3.7 s. The sensor consists of an accelerometer that records the transmitted vibration at a 10 kHz sample rate. During measurements, the actuator and sensor are held manually on the chest surface (Fig. 2). Figure 3 shows a typical vibration transmittance graph.
An example of a vibration sweep output. Above: a vibration sweep output picked up by the accelerometer sensor according to the time. Below: the same vibration sweep results according to the measured frequencies. The gray-shaded area under the curve represents the total power integral in the 20-2000 Hz band
The skin was covered with an adhesive plastic film. Three measurement levels were used: on the top of the second, third, and fourth costal cartilage. The vibration actuator was positioned 3 cm to the right and the sensor 3 cm to the left of the midline. The vibration transmittance measurements were first performed on an intact chest, followed by unstable chest, and finally in a closed chest, five times at each setting and costal level. In the unstable chest model, a standard median sternotomy was conducted, followed by the insertion of six single no. 7 sternal wires (Ethicon, NJ, USA), and by leaving a 10 mm space between the sternal halves. Ultrasound gel was used to fill the gap and to mimic fluid accumulation. As there was a tendency for the gap to close in rigid cadaver chests, lateral rib traction was used to maintain the gap without obstructing the measurements. The chest was then tightly closed and the soft tissues sutured in two layers for the final measurements.
The data were processed off-line on a personal computer using routines implemented in a MATLAB (Mathworks, MA, USA) scientific computing environment. Total vibration power (g2) in the 20-2000 Hz band was calculated for each measurement and logarithmic (ln) transformation was applied before statistical testing, since the raw data were not normally distributed. A generalized Linear Mixed Model with the lme function was used to determine the ability of the vibration transmittance device to differentiate mechanical settings in the sternotomy regardless of the costal level. The mean response was modelled as a linear combination of the population characteristics shared by all individuals (fixed effects), and subject-specific effects unique to a particular cadaver constituted the random effects. Three different mechanical settings and three costal levels were modelled as fixed effects and the number of repeated measurements per each cadaver constituted a potential source of variation and was included as random effects in the model [29]. The generalized linear mixed model analyses were performed with the Statistical Package R version 3.3.0 package lme4 (The R Foundation, www.r-project.org). All p-values are two-tailed. A p-value less than 0.05 was considered statistically significant.
The study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the Regional Ethics Committee (Approval number ETL R14131). The relatives of each study subject were contacted by the coroner (SG) and their consent sought before inclusion in the study.
Results
The measured vibration transmittances are given in Tables 2 and 3 shows the total amount and percentage of vibration transmittance reduction at different costal levels and each state of the sternum, calculated from the medians of raw data. There were clear and statistically significant differences between intact, stable, and unstable sterna, and the reduction in vibration transmittance was able to differentiate between stable and unstable sternum, as shown in Fig. 4. There were no statistically significant differences in the vibration transmittance between the three costal levels that were tested, which is presented in Table 4. The soft tissue thickness in cadavers showed a moderate inverse correlation to the transmitted vibration power when the raw data of all tested levels were analysed in the intact sterna (Spearman’s nonparametric rho = − 0.478).
Discussion
Current clinical practice is lacking proper methods for sternal stability assessment. This motivated us to test vibration transmittance as an objective, repeatable, fast, inexpensive and noninvasive tool for the sternotomy dehiscence detection. This method lacks the risks of ionizing radiation and intravenous contrast medium, which are obvious problems when fairly expensive computed tomography is used. Our main finding was that vibration transmittance can be applied as a measure of postoperative sternal integrity.
With the transmittance measurement we achieved diagnostic separation between the intact and split sterna, especially when there was a gap. While the magnitude of vibration transmittance reduction was greatest between an intact sternum and a loose closure with a gap, the method appeared to be able to differentiate between a tightly closed and an unstable sternum as well, the situation with the most clinical relevance. The analyzed 20–2000 Hz band was the same as the stimulation band. Generally, in the low frequency vibration transmittance analysis, the optimal frequency band may differ depending on the device function and measured objects. A deeper search could have also revealed other sub-bands that in turn might better discern sternal stability, however, it was not the goal to optimize the test performance on the cadavers, as the intended use is in postoperative patients recovering from surgery. Indeed, in the preceding study we discovered that the optimal band to depict the stability of normally healing sternotomy is 600–1500 Hz in clinical patients [28], probably because the patients studied were normothermic and recovering from a cardiopulmonary bypass with tissue swelling. The reduction in the vibration transmission caused by the sternotomy was roughly the same even when the explored frequency band was different from our preceding study. As the device technology development is still in the early phase, a10 mm gap resembling widely broken sternum fixation was chosen as a pathological reference. The gap detection capability in the current study was not dependent on the tested costal level which is a sound and clinically relevant finding.
The main problem of in vivo vibration measurements of bone arises from the damping effects of skin and soft tissues, especially in obese patients [25]. A minor damping effect of soft tissues was seen in our series. It should be noted, however, that this series was a proof of concept and feasibility test, and we intentionally chose cadavers with near normal body mass index to exclude the possible bias caused by excessive soft tissue damping. The role soft tissue thickness needs to be confirmed in a larger series. The cadaver model is a valuable platform for vibrational sternotomy stability studies because it offers opportunities to objectively settle different mechanical conditions in the human thorax for serial, repeated measurements. We acknowledge that e.g. the tissue rigidity and the temperature in the cadavers differ from living tissue, and this may somewhat limit the translation of our findings to clinical postoperative patients. The accuracy of the vibration transmittance method to detect smaller bone diastases, as well as characterizing the different stages of normal and disturbed healing in the sterna, requires further clinical study.
Conclusions
In conclusion, vibration transmittance analysis was applicable and able to differentiate intact sterna, tightly wire-fixed sterna, and sterna with diastasis in the wire-fixed bone halves. The gap detection capability is not dependent on the tested costal level. The concept was proven to be promising, as it offers a tool for the earlier detection of diastasis in sternotomies, which potentially enables the prevention of sternotomy wound complications.
References
Jacobs JP, O'Brien SM, Shahian DM, Edwards FH, Badhwar V, Dokholyan RS, Sanchez JA, Morales DL, Prager RL, Wright CD, Puskas JD, Gammie JS, Haan CK, George KM, Sheng S, Peterson ED, Shewan CM, Han JM, Bongiorno PA, Yohe C, Williams WG, Mayer JE, Grover FL. Successful linking of the Society of Thoracic Surgeons database to social security data to examine the accuracy of Society of Thoracic Surgeons mortality data. J Thorac Cardiovasc Surg. 2013;145(4):976–83.
Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, DK MG, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. American Heart Association statistics committee, stroke statistics subcommittee: heart disease and stroke Statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360.
Olbrecht VA, Barreiro CJ, Bonde PN, Williams JA, Baumgartner WA, Gott VL, Conte JV. Clinical outcomes of noninfectious sternal dehiscence after median sternotomy. Ann Thorac Surg. 2006;82(3):902–7.
Harjula A, Jarvinen A. Postoperative median sternotomy dehiscence. Scand J Thorac Cardiovasc Surg. 1983;17(3):277–81.
Bryan AJ, Lamarra M, Angelini GD, West RR, Breckenridge IM. Median sternotomy wound dehiscence: a retrospective case control study of risk factors and outcome. J R Coll Surg Edinb. 1992;37(5):305–8.
Gorlitzer M, Wagner F, Pfeiffer S, Folkmann S, Meinhart J, Fischlein T, Reichenspurner H, Grabenwoeger M. Prevention of sternal wound complications after sternotomy: results of a large prospective randomized multicentre trial. Interact Cardiovasc Thorac Surg. 2013;17(3):515–22.
Jacobson JY, Doscher ME, Rahal WJ, Friedmann P, Nikfarjam JS, D'Alessandro DA, Michler RE, Garfein ES. Asymmetric sternotomy and sternal wound complications: assessment using 3-dimensional computed tomography reconstruction. Innovations (Phila). 2015;10(1):52–6.
Robicsek F, Fokin A, Cook J, Bhatia D. Sternal instability after midline sternotomy. Thorac Cardiovasc Surg. 2000;48(1):1–8.
Losanoff JE, Richman BW, Jones JW. Disruption and infection of median sternotomy: a comprehensive review. Eur J Cardiothorac Surg. 2002;21(5):831–9.
Fowler VG Jr, O'Brien SM, Muhlbaier LH, Corey GR, Ferguson TB, Peterson ED. Clinical predictors of major infections after cardiac surgery. Circulation. 2005;112(9 Suppl):I358–65.
Celik S, Kirbas A, Gurer O, Yildiz Y, Isik O. Sternal dehiscence in patients with moderate and severe chronic obstructive pulmonary disease undergoing cardiac surgery: the value of supportive thorax vests. J Thorac Cardiovasc Surg. 2011;141(6):1398–402.
Kirbas A, Celik S, Gurer O, Yildiz Y, Isik O. Sternal wrapping for the prevention of sternal morbidity in elderly osteoporotic patients undergoing median sternotomy. Tex Heart Inst J. 2011;38(2):132–6.
Song DH, Lohman RF, Renucci JD, Jeevanandam V, Raman J. Primary sternal plating in high-risk patients prevents mediastinitis. Eur J Cardiothorac Surg. 2004;26(2):367–72.
Balachandran S, Lee A, Denehy L, Lin KY, Royse A, Royse C, El-Ansary D. Risk factors for sternal complications after cardiac operations: a systematic review. Ann Thorac Surg. 2016;102(6):2109–17.
Zeitani J, Penta de Peppo A, Moscarelli M, Guerrieri Wolf L, Scafuri A, Nardi P, Nanni F, Di Marzio E, De Vico P, Chiariello L. Influence of sternal size and inadvertent paramedian sternotomy on stability of the closure site: a clinical and mechanical study. J Thorac Cardiovasc Surg. 2006;132(1):38–42.
Casha AR, Yang L, Kay PH, Saleh M, Cooper GJ. A biomechanical study of median sternotomy closure techniques. Eur J Cardiothorac Surg. 1999;15(3):365–9.
McGregor WE, Trumble DR, Magovern JA. Mechanical analysis of midline sternotomy wound closure. J Thorac Cardiovasc Surg. 1999;117(6):1144–50.
Schimmer C, Sommer SP, Bensch M, Bohrer T, Aleksic I, Leyh R. Sternal closure techniques and postoperative sternal wound complications in elderly patients. Eur J Cardiothorac Surg. 2008;34(1):132–8.
Giannoudis PV, Einhorn TA, Marsh D. Fracture healing: the diamond concept. Injury. 2007;38(Suppl 4):S3–6.
Francel TJ. A rational approach to sternal wound complications. Semin Thorac Cardiovasc Surg. 2004;16(1):81–91.
Bitkover CY, Cederlund K, Aberg B, Vaage J. Computed tomography of the sternum and mediastinum after median sternotomy. Ann Thorac Surg. 1999;68(3):858–63.
Raman J, Lehmann S, Zehr K, De Guzman BJ, Aklog L, Garrett HE, MacMahon H, Hatcher BM, Wong MS. Sternal closure with rigid plate fixation versus wire closure: a randomized controlled multicenter trial. Ann Thorac Surg. 2012;94(6):1854–61.
Allen KB, Thourani VH, Naka Y, Grubb KJ, Grehan J, Patel N, Guy TS, Landolfo K, Gerdisch M, Bonnell M, Cohen DJ. Randomized, multicenter trial comparing sternotomy closure with rigid plate fixation to wire cerclage. J Thorac Cardiovasc Surg. 2017;153(4):888–96.e1.
El-Ansary D, Waddington G, Adams R. Measurement of non-physiological movement in sternal instability by ultrasound. Ann Thorac Surg. 2007;83(4):1513–6.
Nokes LD. The use of low-frequency vibration measurement in orthopaedics. Proc Inst Mech Eng H. 1999;213(3):271–90.
Sennerby L, Meredith N. Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol. 2008;2000(47):51–66.
Pastrav LC, Jaecques SV, Jonkers I, Perre GV, Mulier M. In vivo evaluation of a vibration analysis technique for the per-operative monitoring of the fixation of hip prostheses. J Orthop Surg Res. 2009;4:10.
Hautalahti J, Beev N, Hyttinen J, Tarkka M, Laurikka J. Postoperative sternal stability assessed by vibration: a preliminary study. Ann Thorac Surg. 2012;94(1):260–4.
Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. 2nd ed. New Jersey, United States of America: Hoboken, N.J.: Wiley cop; 2011.
Acknowledgements
The third-generation version of the device used in this study was designed by Esa Jaatinen and Atte Joutsen and built by Esa Jaatinen, MSc. The previous versions were designed by Nikolai Beev and Jari Hyttinen and built by Nikolai Beev, MSc. Thanks to Matthew James, BA, for editing the English language.
Funding
This research received a grant from Tampere Tuberculosis Foundation, Instrumentarium Science Foundation, and the State Research Fund for Pirkanmaa Hospital District, but no other not-for-profit or commercial funding was received.
Availability of data and materials
The datasets used and analyzed in the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Contributions
JHa took part in designing the work, performed the sternotomies and vibration transmittance measurements, and participated in the interpretation of the data and manuscript writing. AJ took part in designing the work, and the prototype device, participated in the vibration transmittance measurement sessions, conducted the signal processing and data analysis, and participated in the interpretation of the data and manuscript writing. SG took part in designing the work, chose the cadavers for the measurements, and participated in the measurement sessions. TL conducted the statistical analysis of the data and took part in the manuscript writing. JK took part in the interpreting of the results and manuscript writing. JHy and JL took part in designing the work, interpreting the data, and writing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the Regional Ethics Committee (Approval number ETL R14131). The relatives of each study subject were contacted by the coroner (SG) and their consent sought before inclusion in the study.
Consent for publication
Consent was obtained from the relative of the study subject for publication of Fig. 2.
Competing interests
Tampere Heart Hospital Co. holds a patent on the vibration transmittance device, as agreed upon by the inventors (Nikolai Beev, Juha Hautalahti, Matti Tarkka, Jari Hyttinen, Jari Laurikka; U.S. Patent No. 9,788,726; EU: 11867251.8–1657 – EPO. PCT Pub No: WO2012/168534). The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hautalahti, J., Joutsen, A., Goebeler, S. et al. Vibration transmittance measures sternotomy stability – a preliminary study in human cadavers. J Cardiothorac Surg 14, 2 (2019). https://doi.org/10.1186/s13019-018-0823-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-018-0823-5
Keywords
- Sternum
- Sternotomy
- Wound healing
- Postoperative complications
- Integrity
- Vibration transmittance
- Electronics