Abstract
Background
Although minimally invasive coronary artery bypass grafting (MICS-CABG) has been shown to result in excellent clinical outcomes overall adoption rates still remain low. Traditional strategies for minimally invasive multivessel revascularization - usually performed through single-thoracotomy – have to deal with restricted grafting possibilities and possible increased susceptibility of arterial grafts to competitive flow, restraining their applicability to very specific indications or hybrid approaches and on top, are prone to conversion to full-sternotomy in case of left internal thoracic artery (LITA) insufficiency.
Methods
Here, we present a novel alternative to the traditional MICS-CABG approaches by adding a right-sided upper “half-mini-thoracotomy”, which allows for aortocoronary bypass grafting in standard “off-pump” manner and adoption of similar revascularization principles as with conventional CABG during minimally invasive multivessel revascularization, though reducing restrictions inherent to current MICS-CABG strategies.
Results
So far, feasibility and safety of this new approach has been successfully shown in 7 consecutive patients requiring surgical revascularization with no procedure-specific complications and graft configuration as well as intraoperative flow assessment comparable to those of similar patients operated via standard full-sternotomy off-pump coronary artery bypass (OPCAB) surgery.
Conclusions
Further evaluation warranted, this technique might have the potential to develop into an additional approach for minimally invasive multivessel revascularization, especially in cases where competitive flow to arterial grafts is feared, while also serving as a bailout-strategy for traditional approaches in case of LITA insufficiency.
Similar content being viewed by others
Background
Despite the increasing numbers of percutaneous interventions, coronary artery bypass grafting (CABG) still remains the gold standard for the treatment of multivessel coronary artery disease in many patients. However, although clinical outcomes have dramatically improved since first introduction of CABG five decades ago, invasiveness of the procedure has not significantly changed, with most of the routinely performed CABG procedures still involving full-sternotomy and aortic clamping [1]. Although minimally invasive coronary artery bypass grafting (MICS-CABG) alternatives have been widely explored showing excellent clinical outcomes overall adoption rates still remain low.
Traditional strategies for minimally invasive multivessel revascularization are of high technical complexity - usually performed through a single-thoracotomy - and have to deal with restricted grafting possibilities and subsequent possible increased susceptibility of arterial grafts to competitive flow, restraining their applicability to very specific indications or hybrid approaches. On top, they are prone to conversion to full-sternotomy in case of left internal thoracic artery (LITA) insufficiency, due to lacking possibilities of aortocoronary venous bypass grafting.
Here, we present a sternotomy-free and clampless alternative to the standard CABG procedure, which allows for aortocoronary bypass grafting in standard “off-pump” manner, while reducing restrictions inherent to current minimally invasive cardiac surgery (MICS) CABG approaches.
Methods
Surgical technique description
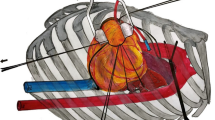
The patient is prepped for surgery as if a minimally invasive direct coronary artery bypass (MIDCAB) procedure was to be performed [2] with addition of a double-lumen endotracheal tube for selective lung ventilation. Pleural cavity is accessed through a left-sided anterolateral mini-thoracotomy via an 8 cm incision over the 5th-6th intercostal space. The incision is performed more laterally than the traditional MIDCAB access in order to gain better exposition to the lateral and inferior portions of the heart. After left lung-deflation the pleural space is entered and the pericardium is obliquely dissected anterior to the phrenic nerve from the right outflow tract down to the apex and then anteriorly to the right cardiophrenic angle. Pericardial sutures are placed to facilitate exposure of targeted myocardial areas, while at the same time allowing for continuous ventilation of the left lung by retaining the left lower lobe. If target vessel exposition and ability to graft is satisfactory, the left internal thoracic artery (LITA) and the saphenous vein (SV) are harvested simultaneously. LITA anastomosis to primary target vessel is sewn in standard manner using an epicardial tissue stabilizer (Octopus™, Medtronic). Patient is tilted left-wards and access is gained to the ascending aorta through an additional, right-sided upper “half-mini-thoracotomy” via a parasternal 4 cm incision over the third intercostal space. After right lung-deflation the pleural space is entered and the pericardium is dissected transversally from the ascending aorta down to the right atrial appendage. Pericardial sutures are placed to facilitate exposure of the aortic landing zone, while at the same time allowing for continuous ventilation of the right lung by retaining the right upper lobe. One or multiple proximal vein-graft anastomoses can be hand-sewn in clampless manner using the HeartString™ device (Guidant). The blood-filled vein-graft(s) are tunneled under the sternum inside the pericardium to the target secondary vessel(s) (Fig. 1). Patient is tilted back to the initial position and distal anastomoses are sewn in standard manner under epicardial stabilization, verifying graft patency via transit time flow measurement (VeriQ™, Medistim). In case of hemodynamic instability or poor exposition the same procedure can be carried out under cardiopulmonary bypass (CPB) via standard femoral cannulation.
Schematics showing additional right-sided upper mini-thoracotomy for aortocoronary bypass grafting during minimally invasive multivessel revascularization. a Overview showing aortocoronary bypass course under intact sternum. b Proximal vein-graft anastomosis onto ascending aorta through a right-sided, anterior, parasternal mini-thoracotomy over the third intercostal space. c Distal vein-graft anastomosis onto target coronary vessel through a left-sided anterolateral mini-thoracotomy over the 5th-6th intercostal space. *aortocoronary bypass
Patients
So far, feasibility and safety of this approach has been successfully shown in 7 consecutive patients requiring surgical revascularization. 6 of the patients were elderly patients (mean age 76.3 ± 4.2 years) with no indication for extended arterial revascularization. The remaining patient was a 46-year old male, who firmly declined a conventional approach via sternotomy and in which we refrained from total arterial revascularization via standard multivessel small thoracotomy (MVST) approach because of expected increased susceptibility of the radial artery graft to competitive flow.
Results
For bypass grafting the LITA (n = 7; 100 %) and an endoscopically harvested SV (n = 7; 100 %) were used, with a mean of 2.14 ± 0.35 distal anastomoses per patient (LAD, n = 7 (100 %); RCX marginal branch, n = 7 (100 %); RCA branch, n = 1 (14.3 %)). Proximal aortic anastomoses were handsewn via HeartString™ device in all 7 patients (100 %), while in one of the patients additional intraoperative proximal anastomoses revision via partial aortic clamping was necessary due to excessive graft length (14.3 %). In 5 of the patients (71.4 %) CPB via femoral cannulation was used for aortocoronary bypass grafting, mainly due to safety issues concerning the learning curve of implementing a new technique. Conversion rate to sternotomy was 0 % for all cases. All 7 patients (100 %) underwent complete revascularization (defined as revascularization of each major myocardial territory subtended by a coronary artery of 1.5 mm or more in diameter with stenosis ≥ 70 %) with no procedure-specific complications. In all patients, macroscopic anastomosis quality, graft configuration and intraoperative flow assessment were comparable to those of similar patients operated via standard full-sternotomy off-pump coronary artery bypass (OPCAB) surgery. Further, patient satisfaction at discharge in terms of having being able to avoid full-sternotomy, was particular high.
Discussion
Evolving surgical strategies, such as OPCAB and MICS, are specifically developed to improve short- and long-term outcomes and to reduce the level of invasiveness of CABG. However, although prone to be beneficial for the patients in terms of reduced rates of transfusion and wound-infection as well as enhanced recovery to full activity and greater patient acceptance [3], overall adoption rates of MICS-CABG approaches remain low [1]. Usually performed through single-thoracotomy or port-access based they are either restrained to specific indications or hybrid approaches because of restricted grafting possibilities (MIDCAB), have to deal with increased susceptibility of arterial grafts to competitive flow [4] (MVST), need specialized infrastructure and training (totally endoscopic coronary artery bypass - TECAB) and are usually prone to conversion to full-sternotomy in case of LITA insufficiency.
Although, minimally invasive multivessel revascularization with aortocoronary bypass grafting performed through single-thoracotomy [5] is possible and has been shown to result in excellent clinical outcomes [6] as well as angiographic graft patency [7] adoption rates remain low. Here, the technical complexity - demanding intricate exposure maneuvers to anastomose grafts onto the ascending aorta while being highly dependent on favorable patient anatomy – is probably one of the major concerns in surgeons not experienced with this approach, restraining the applicability of MICS-CABG surgery to a small number of surgeons and patients.
As demonstrated in this report, an additional right-sided upper “half-mini-thoracotomy” can be an easy to adopt alternative to current MICS-CABG approaches, allowing for aortocoronary bypass grafting in standard OPCAB manner and liberal adoption of similar revascularization principles as with conventional CABG. Although this means having an additional “small scar” on the upper right thorax, patients can hereby potentially be spared a full-sternotomy without need to compromise in the number of employed grafts.
Conclusion
Further evaluation warranted, this technique might have the potential to develop into an additional approach for minimally invasive multivessel revascularization, especially in cases where competitive flow to arterial grafts is feared, while also serving as a bailout-strategy for traditional approaches in case of LITA insufficiency.
Abbreviations
- CABG:
-
Coronary artery bypass grafting
- CPB:
-
Cardiopulmonary bypass
- LAD:
-
Left anterior descending coronary artery
- LITA:
-
Left internal thoracic artery
- MICS:
-
Minimally invasive cardiac surgery
- MICS-CABG:
-
Minimally invasive coronary artery bypass grafting
- MIDCAB:
-
Minimally invasive direct coronary artery bypass
- MVST:
-
Multivessel small thoracotomy
- OPCAB:
-
Off-pump coronary artery bypass
- RCA:
-
Right coronary artery
- RCX:
-
Circumflex coronary artery LAD
- SV:
-
Saphenous vein
- TECAB:
-
Totally endoscopic coronary artery bypass
References
Head SJ, Börgermann J, Osnabrugge RL, Kieser TM, Falk V, Taggart DP, et al. Coronary artery bypass grafting: Part 2--optimizing outcomes and future prospects. Eur Heart J. 2013;34(37):2873–86.
Calafiore AM, Vitolla G, Mazzei V, Teodori G, Di Giammarco G, Iovino T, et al. The LAST operation: techniques and results before and after the stabilization era. Ann Thorac Surg. 1998;66(3):998–1001.
Grossi EA, Galloway AC, Ribakove GH, Zakow PK, Derivaux CC, Baumann FG, et al. Impact of minimally invasive valvular heart surgery: a case–control study. Ann Thorac Surg. 2001;71(3):807–10.
Glineur D, D’hoore W, de Kerchove L, Noirhomme P, Price J, Hanet C, et al. Angiographic predictors of 3 years patency of bypass grafts implanted on the right coronary artery system: a prospective randomized comparison of gastroepiploic artery, saphenous vein grafts and RITA. J Thorac Cardiovasc Surg. 2011;142:980–8.
Chan V, Lapierre H, Sohmer B, Mesana TG, Ruel M. Handsewn proximal anastomoses onto the ascending aorta through a small left thoracotomy during minimally invasive multivessel coronary artery bypass grafting: a stepwise approach to safety and reproducibility. Semin Thorac Cardiovasc Surg. 2012;24(1):79–83.
McGinn Jr JT, Usman S, Lapierre H, Pothula VR, Mesana TG, Ruel M. Minimally invasive coronary artery bypass grafting: dual-center experience in 450 consecutive patients. Circulation. 2009;120(11 Suppl):S78–84.
Ruel M, Shariff MA, Lapierre H, Goyal N, Dennie C, Sadel SM, et al. Results of the Minimally Invasive Coronary Artery Bypass Grafting Angiographic Patency Study. J Thorac Cardiovasc Surg. 2014;147(1):203–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
HA and AA developed and performed the presented surgical technique and collected the data. PA and AL made substantial conceptual contributions and helped drafting and revising the manuscript. All authors read and approved the final manuscript.
Authors’ information
All authors are practicing cardiovascular surgeons at the Department of Cardiovascular Surgery, Heinrich-Heine-University, Düsseldorf, Germany. (HA, resident; PA and AA, attending surgeons; AL, head of department).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Aubin, H., Akhyari, P., Lichtenberg, A. et al. Additional right-sided upper “Half-Mini-Thoracotomy” for aortocoronary bypass grafting during minimally invasive multivessel revascularization. J Cardiothorac Surg 10, 130 (2015). https://doi.org/10.1186/s13019-015-0334-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-015-0334-6