Abstract
Background
Dynamic hip screws (DHS) and proximal femoral nail anti-rotation (PFNA) were recommended for basicervical femoral neck fracture (BFNF), however, with high rate of postoperative femoral neck shortening. The proximal femoral bionic nail (PFBN) was designed to decrease the postoperative complications associated with DHS and PFNA. The aim of this study is to compare the biomechanical characters of DHS, PFNA, and PFBN for fixation of BFNF.
Methods
Using finite element analysis, we created a three-dimensional model of the BFNF for this investigation. The PFBN group, the PFNA group and the DHS + DS group were our three test groups. For each fracture group, the von Mises stress and displacements of the femur and internal fixation components were measured under 2100 N axial loads.
Results
The PFBN group demonstrated the lowest stress on the implants, significantly lower than the PFNA and DHS + DS groups. In terms of stress on the implants, the PFBN group exhibited the best performance, with the lowest stress concentration at 112.0 MPa, followed by the PFNA group at 124.8 MPa and the DHS + DS group at 149.8 MPa. The PFBA group demonstrated the smallest displacement at the fracture interface, measuring 0.21 mm, coupled with a fracture interface pressure of 17.41 MPa, signifying excellent stability.
Conclusions
Compared with DHS and PFNA, PFBN has advantages in stress distribution and biological stability. We believe the concept of triangle fixation will be helpful to reduce femoral neck shortening associated with DHS and PFNA and thus improve the prognosis of BFNF.
Similar content being viewed by others
Background
Basicervical femoral neck fracture (BFNF) is positioned between the femoral neck and the intertrochanteric region, constituting approximately 1.8% to 7.7% of all hip fractures [1,2,3]. BFNF exhibits a larger fracture angle and experiences higher forces and moments transmitted through the hardware in comparison with intertrochanteric fractures. Consequently, it can be regarded as a more unstable fracture compared to intertrochanteric fractures [4]. Considering that immobilization can result in severe complications, including pneumonia, urinary tract infections, pressure sores, and venous thromboembolism [5], early surgical intervention becomes imperative for the majority of these patients [6]. Nonetheless, BFNF remains labeled as an “unresolved fracture” due to its frequent association with avascular necrosis or non-union even following surgical treatment [7].
Dynamic hip screws (DHS), cannulated cancellous screws (CCS) and proximal femoral nail anti-rotation (PFNA) are commonly used devices in the treatment of BFNF [8]. However, the outcomes have been inconsistent. Mousapour et al. [9] observed that CCS fixation, typically employed for intracapsular fractures, exhibits limited effectiveness when applied to BFNF. Moreover, even the addition of extra cancellous screws to DHS to enhance its anti-rotational properties did not yield favorable outcomes. While PFNA imposes a smaller bending moment on the implant, which helps prevent further fracture site collapse and minimizes bone loss compared to DHS, its efficacy in addressing BFNF remains suboptimal. This is primarily due to the relatively narrow cortical base of the proximal fragment and the subsequent limited contact area at the primary fracture site, compounded by inadequate cancellous interdigitation [10, 11].
To address these issues, we introduced the proximal femoral bionic nail (PFBN), which draws inspiration from the well-established Gamma nail and employs a cross-structured configuration of the fixating screw and supporting screw, mirroring the proximal femur's cantilever beam structure. In light of the above, the objective of this study was to conduct a comparative analysis of the biomechanical properties of the proximal femoral bionic nail (PFBN), the dynamic hip screw with de-rotation screw (DHS + DS), and the proximal femoral nail anti-rotation (PFNA) for the treatment of BFNF. We postulated that the PFBN would exhibit superior biomechanical properties.
Methods
This study was reviewed and approved by the institutional review board, and the informed consent was obtained from the volunteer before the examination.
Finite element model establishment
A healthy 35-year-old man with a body weight of 75 kg was recruited as a volunteer participant. After excluding the deformity and abnormal condition of hip by X-ray examination, the left femur was scanned with the spiral computed tomography scanner (Sensation 64, Siemens Medical Solutions, Forchheim, Germany). The scanning involved a slicing distance of 0.625 mm, and the raw data were stored as DICOM format. After that, the raw data were inputted into Mimics20.0 software (Materialise, Leuven, Belgium) to establish the 3-dimension model and then the non-uniform rational basis spline (NURBS) was built by using the Geomagic Studio13.0 software (Geomagic Company, USA). For accuracy, the authors employed manual segmentation to delineate the regions of cortical and cancellous bone within the CT images. The thickness of cortical bone varied across different regions due to anatomical differences. In our study, the cortical thickness ranged from 7.6 mm (femoral shaft) to 1.3 mm (femoral head). The Hypermesh 2014 software (Altair Company, USA) was used to mesh the solid model of femur with C3D4 elements. The models of the DHS + DS, PFNA and PFBN were constructed in UG-NX 12.0 (Siemens Product Life cycle Management Software Inc, USA) according to implants provided by the manufacturer (Naton Institute of Medical Technology, China). BFNF models were established and fixed with three devices by the UG-NX 12.0 (Fig. 1). According to the latest 2018 AO/OTA classification [12], the primary fracture line in the BFNF model (classified as 31-B3) is located at the base of the femoral neck, forming a 70-degree angle with the horizontal plane (Fig. 2a).
Material properties
The material properties of femur bone model were considered to be linear elastic isotropic. In addition, titanium alloy was assigned to the implant material. The material parameters of each component are presented in Table 1 [13].
Boundary and loading conditions
A single-cycle load condition of 2100 N was applied to the finite element models using distributed coupling conditions, ensuring the uniform distribution of individual force over the bone tissue surface corresponding to the area of the femoral head [14] (Fig. 2b). The direction was normal standing angle vertical down, and the distal end of the femur was completely fixed.
The contact conditions were set as friction contact, the friction coefficient between bone and bone was 0.46, the friction coefficient between bone and nail was 0.30, and the friction coefficient between nail and nail was 0.23 [15].
Finite element models validation
The von Mises stress on the intact femur was tested to analyze the mesh convergence. The convergence criterion used was a change of < 5%. The mesh size was set to 2 mm. To emphasize the mechanical performance of the implant in the specific region of interest, a mesh size of 1 mm was employed for all implant components. The femur was composed of 69,734 nodes and 282,872 elements (Table 2).
The ElectroForce 3330 Series II (TA Instruments, USA) was employed to apply axial pressure ranging from 0 to 600 N onto the surface of the femoral head at a rate of 5 N/s. Concurrently, the high-speed camera integrated within the GOM non-contact optical strain measurement system (GOM GmbH, Germany) captured the loading process at a frame rate of 7 frames/s. The resultant images were subsequently subjected to computer processing to derive displacement images and quantify displacement specific to the femur under an axial pressure of 600 N. Subsequent to data acquisition, the GOM Software 2021 was employed to select the appropriate starting point for calculations based on the collected images and to define the calculation area. Upon completion of the calculations, the displacement cloud diagram was automatically generated (Fig. 2c).
Under the same loading and boundary conditions as the biomechanical experiment, the displacement at the corresponding position were calculated for the normal femur finite element model (Fig. 2d). The correlation analysis result indicates that our model is appropriate for the subsequent study (Fig. 2e).
Results
Stress on the implanted femur
Figure 3 compares the peak values of the maximum von Mises stress in the three fixation models. Among the three models, the PFBN group exhibited the lowest overall femoral stress, measuring 35.87 MPa. The maximum von Mises stress was observed beneath the inner cortical bone of the femoral neck. Similarly, in the PFNA group, which utilizes intramedullary fixation, the maximum stress was concentrated beneath the inner cortical bone of the femoral neck, measuring 46.34 MPa. The DHS + DS group experienced the highest stress, reaching 59.37 MPa, with the maximum von Mises stress appearing at the distal end screw hole in the outer cortical bone.
Stress on the implants
To assess the performance of the implant components, Fig. 4 compares the maximum von Mises (equivalent) stress in three fixation styles. The DHS + DS group exhibited the highest internal fixation stress at 149.8 MPa, with the stress concentrated primarily on the shaft of the lag screw. In the PFNA group, the maximum internal fixation stress reached 124.8 MPa, primarily concentrated around the screw-blade interface. The PFBN group experienced a maximum internal fixation stress of 112.0 MPa, with the highest stress concentration occurring at the intersection of the fixating screw and the main nail, significantly lower than the internal fixation stress in the DHS + DS and PFNA groups.
Model displacement of the femur
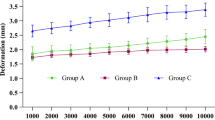
The deformation of the femoral models in the three groups (Fig. 5) primarily occurred in the proximal femoral region. The DHS + DS group exhibited an overall femoral model displacement of 5.939 mm, while the PFNA group had an overall displacement of 5.377 mm. In the PFBN group, the overall femoral model displacement measured 4.156 mm.
Model displacement and contact pressure of fracture surfaces
Figure 6 illustrates the displacement and contact pressure at the fracture interfaces of the three models. At the fracture interface, the PFBN group exhibited the smallest displacement of 0.212 mm and a fracture interface pressure of 17.41 MPa, demonstrating excellent stability. In the PFNA group, the fracture face displacement measured 0.241 mm, with a fracture interface pressure of 32.19 MPa. The DHS + DS group displayed relatively lower stability, with a fracture interface displacement of 0.254 mm and a fracture interface pressure of 37.76 MPa.
Discussion
In the present study, we investigated the mechanical properties of PFBN, DHS + DS and PFNA for the treatment of vertical BFNF using finite element analysis. Our study found that the primary stability of BFNF fixed with PFBN was significantly improved compared with DHS + DS and PFNA. Besides, the peak stress and stress distribution of PFBN and proximal femur were lower than that of DHS + DS and PFNA. PFBN demonstrated better ability to resist shearing force of BFNF, which may be crucial to improve the clinical outcomes of BFNF.
Currently, the selection of the most suitable implant for internal fixation in the treatment of BFNF is a subject of ongoing debate. Osteosynthesis using DHS or CCS is the standard care [16,17,18]. However, the postoperative femoral neck shortening has raised growing concerns. This was due to weakness of abductor muscles and inferior hip function resulted from the subsequent decrease of abductor lever arm. In addition, femoral neck shortening after BFNF can increase the risk of femoral head collapse [19]. Given that BFNF treated by sliding implants is not as stable as previous believed, various devices or techniques for length-stability of femoral neck have been developed [20,21,22]. The use of intramedullary fixation system has been suggested by some authors [23, 24]. In a retrospective clinical study, Guo [25] reported that intramedullary nails had a trend to decrease the femoral neck shortening compared with CCS in treatment of unstable BFNF (5.0% vs 14.29%). Other researchers have investigated the biomechanical properties between cephalomedullary nails and DHS. In a comparative study with synthetic femora, Imren et al. [26] found the PFNA has higher failure loads and possesses biomechanical benefits for fixation of unstable basicervical fractures compared with DHS. Nevertheless, Seyhan and colleagues discovered a heightened likelihood of encountering the following conditions within the PFNA group: reverse displacement of the proximal screw, proximal femur shortening, and a reduction in the varus angle of the proximal femur [27]. When managing unstable hip fractures in geriatric patients, PFNA demonstrates a mechanical failure rate of 7.5% [28]. This encompasses a range of complications, including implant cut-out with an incidence between 5.4 and 13% [29, 30], coxa vara occurring at a rate of 2.5% [31], and a 1% incidence of internal fixation failure [32]. Due to the substantial risk of a reverse wedge effect associated with PFNA fixation for basicervical fractures, this may not effectively mitigate neck collapse or prevent mechanical cut-out failure, even with the enhanced rotational stability provided by the helical blade [33].
The occurrence of various mechanical failures may be attributed to the mismatch between these implants and the proximal femoral anatomical structure and mechanical transmission. In their investigation of complications associated with internal fixation, Zhang et al. have suggested that a triangular stabilization structure (Chinese patents: ZL200920254063.4, ZL200920254062.x, ZL201120370391.8) could potentially reduce the likelihood of internal fixation failure, thereby contributing to the development of proximal femoral bionic nail (PFBN). The innovation of PFBN lies in its double triangle structure, composed of the supporting screw, fixating screw, and main nail. This design closely replicates the cantilever beam structure typically found in a normal proximal femur, resulting in a significant improvement in the postoperative stability following BFNF. The first component, known as the mixed triangle, is formed by the combination of the supporting screw, fixating screw, and the cancellous bone of the femoral head. This configuration significantly enhances the rotational stability of the hardware within three-dimensional space, ensuring a stable transfer of body-weight load to the junction of the supporting screw and fixating screw. The second component, referred to as the metal triangle, is constructed from the fixating screw, supporting screw, and main nail. The combined triangle and the main nail together create a stable cantilever beam structure that aligns with the anatomical structure and mechanical characteristics of the femoral neck. Moreover, the fixating screw is supported by both the main nail and the supporting screw, resulting in a double-pivot fixation. Consequently, this shortens the force arm, ultimately reducing stress concentration and enhancing fracture stability. Moreover, the tension stress of fixating screw can be significantly shared by the supporting screw due to horizontal placement. In our study, the PFBN group reduced stress on the implanted femur by 39.6% and 22.6% compared to the DHS and PFNA groups, respectively.
As shown in displacement distribution, the fracture section stability and overall construct stability were higher in the PFBN model than that of DHS + DS and PFNA models, which meant that PFBN had good ability to resist compression and tension force. The peak stress of DHS + DS and PFNA was 1.3 and 1.1 times higher than that of PFBN. We believe the supporting screw plays an important role in reducing the stress concentration of fixation screw in PFBN, which could decrease the incidence of screw withdrawal, cut-out, and hip varus. In elderly patients with BFNF, who often have osteoporosis, PFBN could potentially offer improved stability and support for early postoperative rehabilitation exercises. However, it should be noted that our study did not specifically investigate the mechanical performance of PFBN in an osteoporotic model, and further research is needed to validate these assumptions.
In addition, the peak stress of proximal femur in the PFBN model had the least value among all models, which demonstrated that PFBN had a decreased dependence on the integrity of femoral medial cortex. However, the peak stress and stress concentration of proximal femur in DHS + DS and PFNA models were located at the medial cortex of femur, which was different from that of PFBN. We consider that the results could be partially explained by the poor construct stability of the DHS + DS and PFNA. In a study on fracture morphology of BFNF patients, Collinge et al. [34] found 96% of cases had femoral neck comminution, which was located at the inferior in most cases (94%). Therefore, the PFBN is a suitable internal fixation for treating the BFNF, especially associated with comminution of medial cortex. Taken together, our study indicated that PFBN can not only enhance the mechanical stability of BFNF model, but also make improvement in the stress distribution of implant and proximal femur.
Limitation
To our knowledge, our study is the first study to test the mechanical properties of PFBN in BFNF. However, there are some limitations to this study. Firstly, despite superior biomechanical stability of PFBN, we did not verify whether the use of PFBN would result in better clinical outcomes. Further randomized comparative studies are needed to verify the clinical benefit. Additionally, it is important to consider that patients with osteoporosis may exhibit lower mechanical properties than healthy patients, potentially leading to higher displacements in such cases.
Conclusions
In conclusion, we investigated the mechanical properties of PFBN, DHS and PFNA in the treatment of BFNF by using finite element analysis. Our study indicated that PFBN had better ability to resist shearing force and could improve the mechanical character compared with DHS and PFNA. Therefore, the use of PFBN should be considered in BFNF. Our findings provide a basis for further research and clinical utility of PFBN in BFNF patients.
Availability of data and materials
Please contact author for data requests.
Abbreviations
- FEA:
-
Finite element analysis
- BFNF:
-
Basicervical femoral neck fracture
- DHS:
-
Dynamic hip screws
- DS:
-
De-rotation screw
- PFBN:
-
Proximal femoral bionic nail
- PFNA:
-
Proximal femoral nail anti-rotation
References
Zhu J, Deng X, Hu H, Cheng X, Tan Z, Zhang Y. Comparison of the effect of rhombic and inverted triangle configurations of cannulated screws on internal fixation of nondisplaced femoral neck fractures in elderly patients. Orthop Surg. 2022;14(4):720–9. https://doi.org/10.1111/os.13223.
Arakaki H, Owan I, Kudoh H, Horizono H, Arakaki K, Ikema Y, et al. Epidemiology of hip fractures in Okinawa, Japan. J Bone Miner Metab. 2011;29(3):309–14. https://doi.org/10.1007/s00774-010-0218-8.
Chen W, Lv H, Liu S, Liu B, Zhu Y, Chen X, et al. National incidence of traumatic fractures in China: a retrospective survey of 512,187 individuals. Lancet Glob Health. 2017;5(8):e807–17. https://doi.org/10.1016/s2214-109x(17)30222-x.
Yoo JI, Cha Y, Kwak J, Kim HY, Choy WS. Review on basicervical femoral neck fracture: definition, treatments, and failures. Hip Pelvis. 2020;32(4):170–81. https://doi.org/10.5371/hp.2020.32.4.170.
Pincus D, Desai SJ, Wasserstein D, Ravi B, Paterson JM, Henry P, et al. Outcomes of after-hours hip fracture surgery. J Bone Jt Surg Am. 2017;99(11):914–22. https://doi.org/10.2106/jbjs.16.00788.
Swart E, Roulette P, Leas D, Bozic KJ, Karunakar M. ORIF or arthroplasty for displaced femoral neck fractures in patients younger than 65 years old: an economic decision analysis. J Bone Jt Surg Am. 2017;99(1):65–75. https://doi.org/10.2106/jbjs.16.00406.
Falsetto A, Dobransky J, Kreviazuk C, Papp S, Beaulé PE, Grammatopoulos G. Instability after hip hemiarthroplasty for femoral neck fracture: an unresolved problem. Can J Surg. 2022;65(1):E128-e134. https://doi.org/10.1503/cjs.021220.
Okike K, Hasegawa IG. Current trends in the evaluation and management of nondisplaced femoral neck fractures in the elderly. J Am Acad Orthop Surg. 2021;29(4):e154–64. https://doi.org/10.5435/jaaos-d-20-00349.
Mousapour A, Mardanpour K, Hojabrian A, Saeb M, Khabiri SS, Safari-Faramani R, et al. A comparison of bipolar hemiarthroplasty versus dynamic hip screw fixation of basicervical femoral neck fractures. J Orthop Spine Trauma. 2019;5:25–8. https://doi.org/10.18502/jost.v5i1.3321.
Watson ST, Schaller TM, Tanner SL, Adams JD, Jeray KJ. Outcomes of low-energy basicervical proximal femoral fractures treated with cephalomedullary fixation. J Bone Jt Surg Am. 2016;98(13):1097–102. https://doi.org/10.2106/jbjs.15.01093.
Tan BY, Lau AC, Kwek EB. Morphology and fixation pitfalls of a highly unstable intertrochanteric fracture variant. J Orthop Surg (Hong Kong). 2015;23(2):142–5. https://doi.org/10.1177/230949901502300204.
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32 Suppl 1:S1–170. https://doi.org/10.1097/bot.0000000000001063.
Cun Y, Dou C, Tian S, Li M, Zhu Y, Cheng X, et al. Traditional and bionic dynamic hip screw fixation for the treatment of intertrochanteric fracture: a finite element analysis. Int Orthop. 2020;44(3):551–9. https://doi.org/10.1007/s00264-019-04478-9.
Bartoska R, Baca V, Horak Z, Hrubina M, Skala-Rosenbaum J, Marvan J, et al. The importance of intramedullary hip nail positioning during implantation for stable pertrochanteric fractures: biomechanical analysis. Surg Radiol Anat. 2016;38(5):577–85. https://doi.org/10.1007/s00276-015-1595-4.
Goffin JM, Pankaj P, Simpson AH, Seil R, Gerich TG. Does bone compaction around the helical blade of a proximal femoral nail anti-rotation (PFNA) decrease the risk of cut-out?: A subject-specific computational study. Bone Jt Res. 2013;2(5):79–83. https://doi.org/10.1302/2046-3758.25.2000150.
Gjertsen JE, Vinje T, Engesaeter LB, Lie SA, Havelin LI, Furnes O, et al. Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. J Bone Jt Surg Am. 2010;92(3):619–28. https://doi.org/10.2106/jbjs.H.01750.
Johansson T. Internal fixation compared with total hip replacement for displaced femoral neck fractures: a minimum fifteen-year follow-up study of a previously reported randomized trial. J Bone Jt Surg Am. 2014;96(6):e46. https://doi.org/10.2106/jbjs.K.00244.
Reina N, Bonnevialle P, Rubens Duval B, Adam P, Loubignac F, Favier T, et al. Internal fixation of intra-capsular proximal femoral fractures in patients older than 80 years: Still relevant? Multivariate analysis of a prospective multicentre cohort. Orthop Traumatol Surg Res. 2017;103(1):3–7. https://doi.org/10.1016/j.otsr.2016.10.013.
Nanty L, Canovas F, Rodriguez T, Faure P, Dagneaux L. Femoral neck shortening after internal fixation of Garden I fractures increases the risk of femoral head collapse. Orthop Traumatol Surg Res. 2019;105(5):999–1004. https://doi.org/10.1016/j.otsr.2019.05.009.
Weil YA, Qawasmi F, Liebergall M, Mosheiff R, Khoury A. Use of fully threaded cannulated screws decreases femoral neck shortening after fixation of femoral neck fractures. Arch Orthop Trauma Surg. 2018;138(5):661–7. https://doi.org/10.1007/s00402-018-2896-y.
Shin KH, Hong SH, Han SB. Posterior fully threaded positioning screw prevents femoral neck collapse in Garden I or II femoral neck fractures. Injury. 2020;51(4):1031–7. https://doi.org/10.1016/j.injury.2020.01.032.
Sun H, Shu LY, Sherrier MC, Zhu Y, Liu JW, Zhang W. Decreased complications but a distinctive fixation loosening mechanism of fully threaded headless cannulated screw fixation for femoral neck fractures in young adults. J Orthop Surg Res. 2021;16(1):234. https://doi.org/10.1186/s13018-021-02335-3.
Mereddy P, Kamath S, Ramakrishnan M, Malik H, Donnachie N. The AO/ASIF proximal femoral nail antirotation (PFNA): a new design for the treatment of unstable proximal femoral fractures. Injury. 2009;40(4):428–32. https://doi.org/10.1016/j.injury.2008.10.014.
Penzkofer J, Mendel T, Bauer C, Brehme K. Treatment results of pertrochanteric and subtrochanteric femoral fractures: a retrospective comparison of PFN and PFNA. Unfallchirurg. 2009;112(8):699–705. https://doi.org/10.1007/s00113-009-1642-x.
Guo J, Dong W, Yin B, Jin L, Lin Z, Hou Z, et al. Intramedullary nails with cannulated screw fixation for the treatment of unstable femoral neck fractures. J Int Med Res. 2019;47(2):557–68. https://doi.org/10.1177/0300060518816185.
Imren Y, Gurkan V, Bilsel K, Desteli EE, Tuna M, Gurcan C, et al. Biomechanical comparison of dynamic hip screw, proximal femoral nail, cannulated screw, and monoaxial external fixation in the treatment of basicervical femoral neck fractures. Acta Chir Orthop Traumatol Cech. 2015;82(2):140–4.
Seyhan M, Turkmen I, Unay K, Ozkut AT. Do PFNA devices and Intertan nails both have the same effects in the treatment of trochanteric fractures? A prospective clinical study. J Orthop Sci. 2015;20(6):1053–61. https://doi.org/10.1007/s00776-015-0750-4.
Zhang W, Antony Xavier RP, Decruz J, Chen YD, Park DH. Risk factors for mechanical failure of intertrochanteric fractures after fixation with proximal femoral nail antirotation (PFNA II): a study in a Southeast Asian population. Arch Orthop Trauma Surg. 2021;141(4):569–75. https://doi.org/10.1007/s00402-020-03399-2.
Raghuraman R, Kam JW, Chua DTC. Predictors of failure following fixation of intertrochanteric fractures with proximal femoral nail antirotation. Singap Med J. 2019;60(9):463–7. https://doi.org/10.11622/smedj.2019114.
Kashigar A, Vincent A, Gunton MJ, Backstein D, Safir O, Kuzyk PR. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Jt J. 2014;96-b(8):1029–34. https://doi.org/10.1302/0301-620x.96b8.33644.
Li H, Wang Q, Dai GG, Peng H. PFNA vs. DHS helical blade for elderly patients with osteoporotic femoral intertrochanteric fractures. Eur Rev Med Pharmacol Sci. 2018;22(1 Suppl):1–7. https://doi.org/10.26355/eurrev_201807_15346.
Sawaguchi T, Sakagoshi D, Shima Y, Ito T, Goldhahn S. Do design adaptations of a trochanteric nail make sense for Asian patients? Results of a multicenter study of the PFNA-II in Japan. Injury. 2014;45(10):1624–31. https://doi.org/10.1016/j.injury.2014.06.002.
Kim JW, Oh CW, Kim BS, Jeong SL, Jung GH, Lee DH. Structure-mechanical analysis of various fixation constructs for basicervical fractures of the proximal femur and clinical implications; finite element analysis. Injury. 2023;54(2):370–8. https://doi.org/10.1016/j.injury.2022.12.004.
Collinge CA, Mir H, Reddix R. Fracture morphology of high shear angle “vertical” femoral neck fractures in young adult patients. J Orthop Trauma. 2014;28(5):270–5. https://doi.org/10.1097/bot.0000000000000014.
Acknowledgements
I would like to thank all authors for help and support in the process of data analysis and article writing.
Funding
This study was funded by the National Natural Science Foundation of China (No. 82272578) and the Health Commission of Hebei Province (No. 20242277).
Author information
Authors and Affiliations
Contributions
ZY and ZQ developed the idea. YY and ZJ wrote an initial draft of the manuscript. YY was responsible for data collection. CX and YY were responsible for model building and finite element analysis. ZJ and YY wrote the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors. This study received approval from the Institutional Review Board (IRB) of the Third Hospital of Hebei Medical University. Informed consent was obtained from all individual participants included in the study. All methods were performed in accordance with the Declarations of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, X., Yang, Y., Zhu, J. et al. Finite element analysis of basicervical femoral neck fracture treated with proximal femoral bionic nail. J Orthop Surg Res 18, 926 (2023). https://doi.org/10.1186/s13018-023-04415-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04415-y