Abstract
Study design
Meta-analysis and systematic review.
Background
Robot-assisted pedicle screw placement technique offers greater accuracy than the traditional freehand screw placement technique. However, it is controversial whether there is a difference between the two procedures in terms of improved clinical outcomes.
Materials and methods
We systematically searched PubMed, EMBASE, Cochrane, and Web of Science to identify potentially eligible articles. Indispensable data such as the year of publication, study type, age, number of patients, sex distribution, and outcomes were extracted. The outcome indicators of interest included Oswestry disability index (ODI), visual analog scale (VAS) score, operative time, intraoperative blood loss, and post-operative length of stay. RevMan 5.4.1 was used for the meta-analysis.
Results
A total of eight studies with 508 participants were included. Eight were related to ΔVAS, six were related to ΔODI, seven were related to operative time, five were related to intraoperative blood loss, and seven were related to the length of hospitalization. The results showed that, in terms of ΔVAS (95% CI, −1.20 to −0.36, P = 0.0003) and ΔODI (95% CI, −2.50 to −0.48, P = 0.004), robot-assisted pedicle screw placement technique scored higher than traditional freehand technique. Additionally, the intraoperative blood loss (95% CI, −140.34 to −10.94, P = 0.02) and the length of hospitalization (95% CI, −2.59 to −0.31, P = 0.01) for patients who underwent robotic-assisted pedicle screw placement were less than that of those who underwent the conventional freehand screw placement. No significant difference was found between robot-assisted techniques and conventional freehand techniques in pedicle screw placement in surgical time (95% CI, −2.24 to 26.32, P = 0.10).
Conclusions
Robot-assisted technique helps improve short-term clinical outcomes, reduce intraoperative blood loss and patient suffering, and shorten recovery time compared to the freehand technique.
Similar content being viewed by others
Introduction
Pedicle screw fixation is an effective treatment option for all spinal disorders. Pedicle screw placement provides an excellent three-column fixation and is widely used in spinal surgery. However, the traditional freehand screw placement method has limitations because the operator's field of vision and body posture are limited by space, which affects the accuracy of screw placement and can lead to pedicle violations. The misplacement rate of conventional freehand pedicle screws ranges from 5 to 41% in the lumbar spine and 3% to 55% in the thoracic spine [1], which may lead to nerve injury, dural tearing, and other complications. In recent years, the development of robot-assisted pedicle screw placement has gradually advanced, and an increasing number of clinical cases have shown the advantages of robot-assisted screw placement over freehand screw placement in terms of improved accuracy and reduced intraoperative bleeding [2]. Feng et al. [3] performed a randomized controlled trial (RCT). They reported that 98.5% of robot-assisted pedicle screw placements achieved an accuracy of grade A. Fu et al. performed a meta-analysis [2] and reported that robot-assisted techniques were more accurate in pedicle screw placement than freehand techniques.
However, whether robot-assisted techniques are superior to freehand techniques in terms of post-operative clinical outcomes remains unclear. Only a few reviews and meta-analyses have focused on this issue. Karamian et al. [4] concluded that the benefits of robot-assisted pedicle screw placement may not apply to patients in terms of clinical outcomes, in a study that compared the post-operative clinical outcomes of robot-assisted screw placement with freehand screw placement. In contrast, Cui et al. [5] reported that the robot-assisted technique significantly reduced post-operative suffering compared with freehand screw placement, in a retrospective cohort study. Therefore, whether robot-assisted pedicle screw placement can improve clinical outcomes remains controversial. Thus, this meta-analysis aimed to determine whether robot-assisted pedicle screw placement technique offers an advantage in short-term clinical outcomes compared with the freehand screw placement technique. The clinical indicators we used were the difference between the pre- and post-operative visual analog scores (ΔVAS), difference between the pre- and post-operative Oswestry disability index (ΔODI), operative time, intraoperative blood loss, and the length of hospital stay (post-operative stay).
Materials and methods
Data search strategy
This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis procedures. We systematically searched the PubMed, EMBASE, Cochrane, and Web of Science databases to identify potentially eligible articles. All the databases were updated on November 10, 2022. Medical subject headings (MeSHs) and free-text words were used to search for potential literature. The PubMed, EMBASE, Cochrane, and Web of Science databases were searched using the following keywords: ‘‘robotics’’ (or ‘‘robot’’ or ‘‘robotic’’ or ‘‘robotics’’) (MeSH) and ‘‘pedicle screws’’ (or ‘‘bone screws’’ or ‘‘spine’’ or ‘‘spinal column’’) (MeSH) (Table 1). Two reviewers (YYL and YDS) independently searched all titles and abstracts, and the references of relevant studies were reviewed for additional relevant literature. Any discrepancies were resolved through discussion or consultation with a third reviewer (WY).
Study selection
The following inclusion criteria were identified before the search: articles involving spinal robotic pedicle screw placement, articles with post-operative computed tomography scans to assess accuracy, and articles providing sufficient data for meaningful comparison (more than 10 pedicle screws per study group). The exclusion criteria were as follows: duplicate publications; articles without traditional freehand pedicle screw placement in the control group; and articles that did not include patient visual analog scores, Oswestry disability index, and post-operative length of stay. Both RCTs and retrospective cohort studies (RCSs) were eligible for inclusion. Only human studies were considered. The inclusion of studies was not limited by sample size or publication type. Review articles and commentaries were excluded from the analysis.
Quality assessment and data extraction
The two reviewers independently assessed all included studies according to the Cochrane risk-of-bias criteria and the Newcastle–Ottawa Quality Assessment Scale using the risk-of-bias tool. The Cochrane risk-of-bias criteria were used to assess the quality of RCTs in terms of selection, performance, detection, attrition, reporting, and other biases. We defined other biases as differences in baseline characteristics between the experimental and control groups. Retrospective cohort studies were evaluated using the Newcastle–Ottawa Quality Assessment Scale, rated from 0 to 9 stars. Six stars or higher indicated sufficiently high quality.
The two reviewers independently performed data extraction. Disagreements were resolved through discussion or consultation with the third reviewer. Indispensable data such as the year of publication, study type, age, number of patients, sex distribution, and outcomes were extracted. The outcome indicators of interest included ODI, VAS score, operative time, intraoperative blood loss, and post-operative length of stay.
Results
Characteristics of the included studies
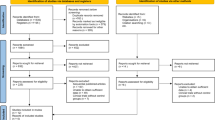
The process of inclusion of these studies is illustrated in Fig. 1. A total of 7124 relevant studies were identified through the web search. A total of 1929 studies were excluded, because they were duplicates. After assessing the titles and abstracts, 5158 studies were excluded because their contents did not meet the criteria. After verifying the full text of the remaining 37 studies, four RCTs [6,7,8,9] and four RCSs [5, 10,11,12] with a total of 508 patients were finally included in this meta-analysis. The main characteristics of the included studies are summarized in Table 2. Baseline information was balanced and comparable across the eight studies. Among the eight studies, the type of robot used in two studies was Renaissance and in six studies was TiRobot. RCTs were shown to have a low risk of bias (Fig. 2 and Table 3), and all RCSs had evaluation scores greater than six stars (Table 4). All included studies demonstrated satisfactory quality.
ΔVAS and ΔODI
Eight studies provided data on pre- and post-operative VAS scores; seven studies provided data on pre- and post-operative ODIs. After obtaining the data from each study, we calculated the ΔVAS and ΔODI for each study, using statistical methods. The results showed that in terms of ΔVAS (SMD = −0.78, 95% CI, −1.20 to −0.36, P = 0.0003; Fig. 3) and ΔODI (SMD = −1.49, 95% CI, −2.50 to −0.48, P = 0.004; Fig. 4), robot-assisted pedicle screw placement technique scored higher than the traditional freehand technique.
Operative time
Seven studies provided data on operative time. No significant difference was found between robot-assisted techniques and conventional freehand techniques in pedicle screw placement in surgical time (SMD = 12.04, 95% CI, −2.24 to 26.32, P = 0.10; Fig. 5).
Intraoperative blood loss
Five studies provided data on intraoperative blood loss. The results showed that the intraoperative blood loss for patients who underwent robotic-assisted pedicle screw placement (SMD = −75.64, 95% CI, −140.34 to −10.94, P = 0.02; Fig. 6) was less than that those who underwent the conventional freehand screw placement.
Length of hospitalization
Seven studies provided data on the length of hospitalization. The results showed that the post-operative length of hospitalization for patients who underwent robotic-assisted pedicle screw placement (SMD = −1.45, 95% CI, −2.59 to −0.31, P = 0.01; Fig. 7) was less than that those who underwent the conventional freehand screw placement.
Discussion
Robot-assisted pedicle screw placement has been designed to improve the accuracy and safety of pedicle screw placement. Theoretically, robot-assisted screw placement technology has the advantages of high precision, repeatability, and fatigue resistance compared with traditional freehand screw placement technology. A meta-analysis [13] was conducted to demonstrate the benefits of the robot-assisted technology in terms of screw placement accuracy. However, the benefits of robot-assisted technology remain controversial. Regarding post-operative rehabilitation outcomes, most available meta-analyses used direct comparisons of post-operative VAS scores and ODIs. They concluded that there was no significant difference in terms of clinical outcomes between robot-assisted and conventional freehand screw placement techniques [14]. However, we believe that their comparisons have certain limitations. In clinical studies addressing post-operative rehabilitation outcomes, the initial VAS scores and ODIs differed between patients in the experimental and control groups, and experimental conclusions obtained can be inaccurate if only the corresponding post-operative scores were compared without considering the differences in their pre-operative scores; therefore, statistical methods were used to address this issue.
In this meta-analysis, eight studies with a total of 2408 screws were included to compare the differences between robot-assisted and traditional freehand pedicle screw placement methods in terms of five clinical indicators: ΔVAS, ΔODI, operative time, intraoperative blood loss, and length of hospitalization. The results for four metrics were significantly different between the two methods. The robot-assisted technique was superior to the traditional freehand screw placement technique in four metrics. Hence, the results recommend the use of the robot-assisted technique for screw placement.
Notably, we compared the difference between the pre- and post-operative VAS scores and ODIs of patients who underwent the two procedures. Because the VAS scores and ODIs gradually decrease with time, as reported in previous studies, there is no significant difference in long-term clinical outcomes between the two surgical techniques [15]. It is equally important to focus on short-term clinical outcomes in the clinical practice of healthcare professionals. A good short-term clinical outcome means that patients recover faster, experience less pain, and incur less expense from rehabilitation and hospitalization; therefore, we uniquely compared and analyzed the short-term clinical outcomes of the two surgical modalities.
The original data of each clinical study were not available; therefore, we used statistical methods to calculate the mean and standard deviation of ΔVAS and ΔODI in each study. The calculation of VAS score is presented as an example of a specific calculation method.
The pre-operative visual analog score was set as \(VAS_{1}\), and its mean was \(\mu \left( {VAS_{1} } \right)\), with a standard deviation of \(\sigma \left( {VAS_{1} } \right)\). The post-operative visual analog score was \(VAS_{2}\), and its mean was \(\mu \left( {VAS_{2} } \right)\), with a standard deviation of \(\sigma \left( {VAS_{2} } \right)\). When the index used to measure the reduction in the VAS score was \({\Delta }VAS\) with mean \(\mu \left( {{\Delta }VAS} \right)\) and standard deviation \(\sigma \left( {{\Delta }VAS} \right)\), and the number of patient cases was \(n\), then:
In previous studies, patients were followed up over time to investigate the advantages of robot-assisted screw placement technique over the traditional freehand screw placement technique in terms of clinical outcomes. The follow-up results were compared directly. Su et al. [16] and Lee et al. [17] compared the ODIs and VAS scores of patients after 1 or 2 years and concluded that there was no significant difference between the two methods in terms of long-term clinical outcomes. However, with technological advances in the development of robot-assisted pedicle screw placement technique, controversy regarding its accuracy has been resolved to some extent. An RCT by Kim et al. [18] and a meta-analysis by Lee et al. [19] showed that the robot-assisted screw placement has a significantly higher accuracy than that of the traditional freehand technique and has a lower rate of proximal tuberosity joint invasion. In this context, there is a need to re-evaluate the advantages of robot-assisted pedicle screw placement technique in post-operative rehabilitation; however, the available meta-analyses do not yet include an analysis of short-term clinical outcomes. In this study, we compared the short-term clinical outcomes of the two surgical methods using the difference between the pre- and post-operative VAS scores and ODIs as a measure of short-term post-operative clinical outcomes. We also compared the operative time, the intraoperative blood loss, and the post-operative length of hospitalization.
We believe that the ultimate goal of developing orthopedic surgical robots is to reduce patient suffering and that patients' subjective perceptions of post-operative recovery outcomes are an important measure of the success of robot-assisted technology. This study identified significant differences between the robot-assisted and freehand screw placement techniques as indicators of short-term post-operative clinical outcomes. The results showed that the robot-assisted screw placement technique was more effective in reducing the patient's VAS score, ODI, and intraoperative blood loss than the freehand screw placement technique and thus reduced the patient's post-operative hospital stay. Furthermore, the robot-assisted screw placement technique did not significantly prolong the operative time.
The present study has some limitations. First, four of the included studies were retrospective cohort studies, and the level of evidence was not as high as that of RCTs. Second, only two robot models were included in this study, and six of the eight included studies used the same robot model, which may have rendered the conclusions of this study inapplicable to other robot models. Despite these limitations, all RCSs included in this meta-analysis had scores ≥ 7 stars and were of high quality.
Conclusion
The robot-assisted pedicle screw placement technique showed a significant reduction in the patients’ VAS scores, ODIs, intraoperative blood loss, and post-operative length of hospitalization compared with the traditional unassisted technique. And the robot-assisted screw placement technique did not significantly prolong the operative time. These results suggest that robot-assisted techniques help improve short-term clinical outcomes, reduce patient suffering, and shorten recovery time compared with the freehand technique.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- VAS:
-
Visual analog scale
- ΔVAS:
-
Difference between pre-operative and post-operative VAS values
- ODI:
-
Oswestry disability index
- ΔODI:
-
Difference between pre-operative and post-operative ODI values
- NOS:
-
Newcastle–Ottawa scale
- MD:
-
Mean difference
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- RCT:
-
Randomized controlled trial
- RCS:
-
Retrospective cohort study
References
Mason A, Paulsen R, Babuska JM, Rajpal S, Burneikiene S, Nelson EL, Villavicencio AT. The accuracy of pedicle screw placement using intraoperative image guidance systems. J Neurosurg Spine. 2014;20(2):196–203. https://doi.org/10.3171/2013.11.SPINE13413.
Fu W, Tong J, Liu G, Zheng Y, Wang S, Abdelrahim MEA, Gong S. Robot-assisted technique vs conventional freehand technique in spine surgery: a meta-analysis. Int J Clin Pract. 2021;75(5):e13964. https://doi.org/10.1111/ijcp.13964.
Feng S, Tian W, Sun Y, Liu Y, Wei Y. Effect of robot-assisted surgery on lumbar pedicle screw internal fixation in patients with osteoporosis. World Neurosurg. 2019;125:e1057–62. https://doi.org/10.1016/j.wneu.2019.01.243.
Karamian BA, DiMaria SL, Sawires AN, Canseco JA, Basques BA, Toci GR, Radcliff KE, Rihn JA, Kaye ID, Hilibrand AS, Lee JK, Kepler CK, Vaccaro AR, Schroeder GD. Clinical outcomes of robotic versus freehand pedicle screw placement after one-to three-level lumbar fusion. Glob Spine J. 2021;21925682211057491. https://doi.org/10.1177/21925682211057491
Cui GY, Tian W, He D, Xing YG, Liu B, Yuan Q, Wang YQ, Sun YQ. Effects of robot⁃assisted minimally invasive transforaminal lumbar interbody fusion and traditional open surgery in the treatment of lumbar spondylolisthesis. Zhonghua wai ke za zhi [Chinese journal of surgery]. 2017;55(7):543–8. https://doi.org/10.3760/cma.j.issn.0529-5815.2017.07.013.
Cui GY, Han XG, Wei Y, Liu YJ, He D, Sun YQ, Liu B, Tian W. Robot-assisted minimally invasive transforaminal lumbar interbody fusion in the treatment of lumbar spondylolisthesis. Orthop Surg. 2021;13(7):1960–8. https://doi.org/10.1111/os.13044.
Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions: a randomized controlled trial. Spine. 2017;42(6):353–8. https://doi.org/10.1097/BRS.0000000000001778.
Feng S, Tian W, Wei Y. Clinical effects of oblique lateral interbody fusion by conventional open versus percutaneous robot-assisted minimally invasive pedicle screw placement in elderly patients. Orthop Surg. 2020;12(1):86–93. https://doi.org/10.1111/os.12587.
Wang L, Li C, Wang Z, Li D, Tian Y, Yuan S, Liu X. Comparison of robot-assisted versus fluoroscopy-assisted minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar spinal diseases: 2-year follow-up. J Robot Surg. 2022. https://doi.org/10.1007/s11701-022-01442-5.
Zhang TT, Wang ZP, Wang ZH, Weng J, Chi F, Xue W, Song YX, Liu L. Clinical application of Orthopedic Tianji Robot in surgical treatment of thoracolumbar fractures. China J Orthopaedics Traumatol. 2021;34(11), 1034–9. https://doi.org/10.12200/j.issn.1003-0034.2021.11.010.
Lin S, Hu J, Wan L, Tang L, Wang Y, Yu Y, Zhang W. Short-term effectiveness comparision between robotic-guided percutaneous minimally invasive pedicle screw internal fixation and traditional open internal fixation in treatment of thoracolumbar fractures. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese journal of reparative and reconstructive surgery, 2020;34(1), 76–82. https://doi.org/10.7507/1002-1892.201906105.
Tian Y, Zhang J, Chen H, Ding K, Liu T, Huang D, Hao D. A comparative study of spinal robot-assisted and traditional fluoroscopy-assisted percutaneous reduction and internal fixation for single-level thoracolumbar fractures without neurological symptoms. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese Journal of Reparative and Reconstructive Surgery, 2020;34(1), 69–75. https://doi.org/10.7507/1002-1892.201905057.
Fan Y, Du JP, Liu JJ, Zhang JN, Qiao HH, Liu SC, Hao DJ. Accuracy of pedicle screw placement comparing robot-assisted technology and the free-hand with fluoroscopy-guided method in spine surgery: an updated meta-analysis. Medicine, 2018;97(22), e10970. https://doi.org/10.1097/MD.0000000000010970.
Li HM, Zhang RJ, Shen CL. Accuracy of pedicle screw placement and clinical outcomes of robot-assisted technique versus conventional freehand technique in spine surgery from nine randomized controlled trials: a meta-analysis. Spine. 2020;45(2):E111–9. https://doi.org/10.1097/BRS.0000000000003193.
Park SM, Kim HJ, Lee SY, Chang BS, Lee CK, Yeom JS. Radiographic and clinical outcomes of robot-assisted posterior pedicle screw fixation: two-year results from a randomized controlled trial. Yonsei Med J. 2018;59(3):438–44. https://doi.org/10.3349/ymj.2018.59.3.438.
Su XJ, Lv ZD, Chen Z, Wang K, Zhu C, Chen H, Han YC, Song QX, Lao LF, Zhang YH, Li Q, Shen HX. Comparison of accuracy and clinical outcomes of robot-assisted versus fluoroscopy-guided pedicle screw placement in posterior cervical surgery. Glob Spine J. 2022;12(4):620–6. https://doi.org/10.1177/2192568220960406.
Lee NJ, Boddapati V, Mathew J, Marciano G, Fields M, Buchana IA, Lehman RA. Does robot-assisted spine surgery for multi-level lumbar fusion achieve better patient-reported outcomes than free-hand techniques? Interdisciplinary Neurosurgery, 2021;25, 101214. https://doi.org/10.1016/j.inat.2021.101214
Kim HJ, Jung WI, Chang BS, Lee CK, Kang KT, Yeom JS. A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery. Int J Med Robotics + Computer Assisted Surg: MRCAS, 2017;13(3). https://doi.org/10.1002/rcs.1779. https://doi.org/10.1002/rcs.1779
Zhou LP, Zhang RJ, Li HM, Shen CL. Comparison of cranial facet joint violation rate and four other clinical indexes between robot-assisted and freehand pedicle screw placement in spine surgery: a meta-analysis. Spine. 2020;45(22):E1532–40. https://doi.org/10.1097/BRS.0000000000003632.
Acknowledgements
Not applicable.
Funding
National Natural Science Foundation of China (81871777); Tianjin Science and Technology Program (18PTLCSY00070); National Key R&D Program of China (2019YFC1511202-01); Tianjin Health Science and Technology Project (TJWJ2022QN053).
Author information
Authors and Affiliations
Contributions
Y.Y.L. and Y.W. designed the project. Y.Y.L. and Y.D.S. collected all medical records. B.C.D. and P.C.Y. prepared all figures. Y.Y.L., L.Y.Z., and J.H.S. completed all statistical analyses and wrote the manuscript. X.L.M. and J.X.M. have been involved supervision. All authors discussed the results and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Although the present study involved human participants, ethical approval was not required because all data were based on previously published studies that were analyzed anonymously without any potential harm to the participants. Informed consent from the participants was not required because all data were based on previously published studies that were analyzed anonymously without any potential harm to the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Y., Wang, Y., Ma, X. et al. Comparison of short-term clinical outcomes between robot-assisted and freehand pedicle screw placement in spine surgery: a meta-analysis and systematic review. J Orthop Surg Res 18, 359 (2023). https://doi.org/10.1186/s13018-023-03774-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-03774-w