Abstract
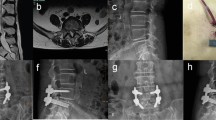
This study was performed to prospectively compare the clinical and radiographic outcomes between robot-assisted minimally invasive transforaminal lumbar interbody fusion (RA MIS-TLIF) and fluoroscopy-assisted minimally invasive transforaminal lumbar interbody fusion (FA MIS-TLIF) in patients with degenerative lumbar spinal diseases. One hundred and twenty-three patients with lumbar degenerative diseases (lumbar spinal stenosis with instability and spondylolisthesis [degenerative spondylolisthesis or isthmic spondylolisthesis]) who underwent MIS-TLIF in our hospital were included in this study. Sixty-one patients underwent RA MIS-TLIF (Group A) and 62 patients underwent FA MIS-TLIF (Group B). Group A was further divided into Subgroup AI (46 single-level procedures) and Subgroup AII (15 double-level procedures). Group B was further divided into Subgroup BI (45 single-level procedures) and Subgroup BII (17 double-level procedures). The clinical outcome parameters were the visual analog scale (VAS) score, Oswestry Disability Index (ODI) score, operative time, number of intraoperative fluoroscopies, blood loss, postoperative hospital stay, and postoperative complications. The radiographic change measures were the accuracy of screw placement, facet joint violation (FJV), fusion status, and change in disc height at the proximal adjacent segment at the 2-year follow-up. There were no significant differences in the VAS and ODI scores, blood loss, or postoperative hospital stay between Groups A and B (p > 0.05). The operative time was longer in Group A than B (p = 0.018). The operative time was longer in Subgroup AI than BI (p = 0.001). However, there was no significant difference between Subgroups AII and BII (p > 0.05). There was no significant difference in the number of intraoperative fluoroscopies for patients between Groups A and B (p > 0.05). Although the number of intraoperative fluoroscopies for patients was significantly higher in Subgroup AI than BI (p = 0.019), there was no significant difference between Subgroups AII and BII (p > 0.05). The number of intraoperative fluoroscopies for the surgeon was significantly lower in Group A than B (p < 0.001). For surgeons, the difference in the average number of intraoperative fluoroscopies between Subgroups AI and AII was 2.98, but that between Subgroups BI and BII was 10.73. In Group A, three guide pins exhibited drift and one patient developed a lateral wall violation by a pedicle screw. One pedicle screw perforated the anterior wall of the vertebral body and another caused an inner wall violation in Group B. The rate of a perfect screw position (grade A) was higher in Group A than B (p < 0.001). However, there was no significant difference in the proportion of clinically acceptable screws (grades A and B) between the two groups. The mean FJV grade was significantly higher in Group B than A (p < 0.001). During at 2-year postoperative follow-up, there was no significant difference in the fusion status between the two groups (p > 0.05); however, the decrease in disc height at the proximal adjacent segment was significantly less in Group A than B (p < 0.001). Robot-assisted percutaneous pedicle screw placement is a safer and more accurate alternative to conventional freehand fluoroscopy-assisted percutaneous pedicle screw insertion in MIS-TLIF.






Similar content being viewed by others
Data availability
All data available for this study were reported in the manuscript.
Code availability
Not applicable.
References
Harms J, Rolinger H (1982) A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author’s transl). Z Orthop Ihre Grenzgeb 120:343–347. https://doi.org/10.1055/s-2008-1051624
Foley KT, Lefkowitz MA (2002) Advances in minimally invasive spine surgery. Clin Neurosurg 49:499–517
Goldstein CL, Macwan K, Sundararajan K, Rampersaud YR (2014) Comparative outcomes of minimally invasive surgery for posterior lumbar fusion: a systematic review. Clin Orthop Relat Res 472:1727–1737. https://doi.org/10.1007/s11999-014-3465-5
Jin-Tao Q, Yu T, Mei W, Xu-Dong T, Tian-Jian Z, Guo-Hua S, Lei C, Yue H, Zi-Tian W, Yue Z (2015) Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: a meta-analysis. Eur Spine J 24:1058–1065. https://doi.org/10.1007/s00586-015-3890-5
Khan NR, Clark AJ, Lee SL, Venable GT, Rossi NB, Foley KT (2015) surgical outcomes for minimally invasive vs open transforaminal lumbar interbody fusion: an updated systematic review and meta-analysis. Neurosurgery 77:847–874; discussion 874. https://doi.org/10.1227/NEU.0000000000000913
Jutte PC, Castelein RM (2002) Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J 11:594–598. https://doi.org/10.1007/s00586-002-0469-8
Katonis P, Christoforakis J, Kontakis G, Aligizakis AC, Papadopoulos C, Sapkas G, Hadjipavlou A (2003) Complications and problems related to pedicle screw fixation of the spine. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000068761.86536.1d
Fan Y, Du JP, Zhang JN, Liu SC, Xue XK, Huang YF, Zhang J, Hao D (2017) Comparison of accuracy of pedicle screw insertion among 4 guided technologies in spine surgery. Med Sci Monit 23:5960–5968. https://doi.org/10.12659/Msm.905713
Fan Y, Du JP, Liu JJ, Zhang JN, Qiao HH, Liu SC, Hao DJ (2018) Accuracy of pedicle screw placement comparing robot-assisted technology and the free-hand with fluoroscopy-guided method in spine surgery: an updated meta-analysis. Medicine (Baltimore) 97:e10970. https://doi.org/10.1097/MD.0000000000010970
D’Souza M, Gendreau J, Feng A, Kim LH, Ho AL, Veeravagu A (2019) Robotic-assisted spine surgery: history, efficacy, cost, and future trends. Robot Surg 6:9–23. https://doi.org/10.2147/RSRR.S190720
Nolte LP, Zamorano L, Visarius H, Berlemann U, Langlotz F, Arm E, Schwarzenbach O (1995) Clinical evaluation of a system for precision enhancement in spine surgery. Clin Biomech (Bristol, Avon) 10:293–303. https://doi.org/10.1016/0268-0033(95)00004-5
Park P, Foley KT, Cowan JA, Marca FL (2010) Minimally invasive pedicle screw fixation utilizing O-arm fluoroscopy with computer-assisted navigation: feasibility, technique, and preliminary results. Surg Neurol Int 1:44. https://doi.org/10.4103/2152-7806.68705
Tian NF, Huang QS, Zhou P, Zhou Y, Wu RK, Lou Y, Xu HZ (2011) Pedicle screw insertion accuracy with different assisted methods: a systematic review and meta-analysis of comparative studies. Eur Spine J 20:846–859. https://doi.org/10.1007/s00586-010-1577-5
Wolf A, Shoham M, Michael S, Moshe R (2004) Feasibility study of a mini, bone-attached, robotic system for spinal operations: analysis and experiments. Spine (Phila Pa 1976) 29:220–228. https://doi.org/10.1097/01.BRS.0000107222.84732.DD
Fujishiro T, Nakaya Y, Fukumoto S, Adachi S, Nakano A, Fujiwara K, Baba I, Neo M (2015) Accuracy of pedicle screw placement with robotic guidance system: a cadaveric study. Spine (Phila Pa 1976) 40:1882–1889. https://doi.org/10.1097/BRS.0000000000001099
Han X, Tian W, Liu Y, Liu B, He D, Sun Y, Han X, Fan M, Zhao J, Xu Y, Zhang Q (2019) Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomized controlled trial. J Neurosurg Spine. https://doi.org/10.3171/2018.10.SPINE18487
Kim HJ, Lee SH, Chang BS, Lee CK, Lim TO, Hoo LP, Yi JM, Yeom JS (2015) Monitoring the quality of robot-assisted pedicle screw fixation in the lumbar spine by using a cumulative summation test. Spine (Phila Pa 1976) 40:87–94. https://doi.org/10.1097/BRS.0000000000000680
Gertzbein SD, Robbins SE (1990) Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 15:11–14. https://doi.org/10.1097/00007632-199001000-00004
Babu R, Park JG, Mehta AI, Shan T, Grossi PM, Brown CR, Richardson WJ, Isaacs RE, Bagley CA, Kuchibhatla M, Gottfried ON (2012) Comparison of superior-level facet joint violations during open and percutaneous pedicle screw placement. Neurosurgery 71:962–970. https://doi.org/10.1227/NEU.0b013e31826a88c8
Son S, Lee SG, Kim WK, Ahn Y, Jung JM (2021) Disc height discrepancy between supine and standing positions as a screening metric for discogenic back pain in patients with disc degeneration. Spine J 21:71–79. https://doi.org/10.1016/j.spinee.2020.07.006
Selby MD, Clark SR, Hall DJ, Freeman BJ (2012) Radiologic assessment of spinal fusion. J Am Acad Orthop Surg 20:694–703. https://doi.org/10.5435/JAAOS-20-11-694
Fogel GR, Toohey JS, Neidre A, Brantigan JW (2008) Fusion assessment of posterior lumbar interbody fusion using radiolucent cages: X-ray films and helical computed tomography scans compared with surgical exploration of fusion. Spine J 8:570–577. https://doi.org/10.1016/j.spinee.2007.03.013
Kim HJ, Kang KT, Chun HJ, Hwang JS, Chang BS, Lee CK, Yeom JS (2018) Comparative study of 1-year clinical and radiological outcomes using robot-assisted pedicle screw fixation and freehand technique in posterior lumbar interbody fusion: a prospective, randomized controlled trial. Int J Med Robot 14:e1917. https://doi.org/10.1002/rcs.1917
Chang M, Wang L, Yuan S, Tian Y, Zhao Y, Liu X (2022) Percutaneous endoscopic robot-assisted transforaminal lumbar interbody fusion (PE RA-TLIF) for lumbar spondylolisthesis: a technical note and two years clinical results. Pain Phys 25:E73–E86
Ravi B, Zahrai A, Rampersaud R (2011) Clinical accuracy of computer-assisted two-dimensional fluoroscopy for the percutaneous placement of lumbosacral pedicle screws. Spine 36:84–91. https://doi.org/10.1097/BRS.0b013e3181cbfd09
Hyun SJ, Kim KJ, Jahng TA, Kim HJ (2017) Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions: a randomized controlled trial. Spine 42:353–358. https://doi.org/10.1097/brs.0000000000001778
Roser F, Tatagiba M, Maier G (2013) Spinal robotics: current applications and future perspectives. Neurosurgery 72:A12–A18. https://doi.org/10.1227/NEU.0b013e318270d02c
Hyun SJ, Kim KJ, Jahng TA, Kim HJ (2017) Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions a randomized controlled trial. Spine 42:353–358. https://doi.org/10.1097/Brs.0000000000001778
Kantelhardt S, Martinez R, Baerwinkel S, Burger R, Giese A, Rohde V (2011) Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J 20:860–868. https://doi.org/10.1007/s00586-011-1729-2
Molliqaj G, Schatlo B, Alaid A, Solomiichuk V, Rohde V, Schaller K, Tessitore E (2017) Accuracy of robot-guided versus freehand fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery. Neurosurg Focus 42:E14. https://doi.org/10.3171/2017.3.Focus179
Lieberman IH, Hardenbrook MA, Wang JC, Guyer RD (2012) Assessment of pedicle screw placement accuracy, procedure time, and radiation exposure using a miniature robotic guidance system. J Spinal Disord Tech 25:241–248. https://doi.org/10.1097/BSD.0b013e318218a5ef
Phillips FM (2009) Percutaneous placement of pedicle screws in the lumbar spine using a bone mounted miniature robotic system first experiences and accuracy of screw placement point of view. Spine 34:399–399. https://doi.org/10.1097/BRS.0b013e3181973450
Hu X, Ohnmeiss DD, Lieberman IH (2013) Robotic-assisted pedicle screw placement: lessons learned from the first 102 patients. Eur Spine J 22:661–666. https://doi.org/10.1007/s00586-012-2499-1
Moshirfar A, Jenis LG, Spector LR, Burke PJ, Losina E, Katz JN, Rand FF, Tromanhauser SG, Banco RJ (2006) Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine (Phila Pa 1976) 31:2624–2629. https://doi.org/10.1097/01.brs.0000240691.35707.e8
Tian W, Xu YF, Liu B, Liu YJ, He D, Yuan Q, Lang Z, Lyu YW, Han XG, Jin PH (2014) Lumbar spine superior-level facet joint violations: percutaneous versus open pedicle screw insertion using intraoperative 3-dimensional computer-assisted navigation. Chin Med J 127:3852–3856. https://doi.org/10.3760/cma.j.issn.0366-6999.20141860
Park Y, Ha JW, Lee YT, Sung NY (2011) Cranial facet joint violations by percutaneously placed pedicle screws adjacent to a minimally invasive lumbar spinal fusion. Spine J 11:295–302. https://doi.org/10.1016/j.spinee.2011.02.007
Moshirfar A, Jenis LG, Spector LR, Burke PJ, Losina E, Katz JN, Rand FF, Tromanhauser SG, Banco RJ (2006) Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine 31:2624–2629. https://doi.org/10.1097/01.brs.0000240691.35707.e8
Zhang Q, Xu YF, Tian W, Le XF, Liu B, Liu YJ, He D, Sun YQ, Yuan Q, Lang Z, Han XG (2019) Comparison of superior-level facet joint violations between robot-assisted percutaneous pedicle screw placement and conventional open fluoroscopic-guided pedicle screw placement. Orthop Surg 11:850–856. https://doi.org/10.1111/os.12534
Zhao Y, Yuan S, Tian Y, Liu X (2020) Risk factors related to superior facet joint violation during lumbar percutaneous pedicle screw placement in minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF). World Neurosurg 139:e716–e723. https://doi.org/10.1016/j.wneu.2020.04.118
Knox JB, Dai JM 3rd, Orchowski JR (2011) Superior segment facet joint violation and cortical violation after minimally invasive pedicle screw placement. Spine J 11:213–217. https://doi.org/10.1016/j.spinee.2011.01.024
Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, Baldus C (2007) Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine 32:2253–2257. https://doi.org/10.1097/BRS.0b013e31814b2d8e
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29:1938–1944. https://doi.org/10.1097/01.brs.0000137069.88904.03
Kim HJ, Kang KT, Park SC, Kwon OH, Son J, Chang BS, Lee CK, Yeom JS, Lenke LG (2017) Biomechanical advantages of robot-assisted pedicle screw fixation in posterior lumbar interbody fusion compared with freehand technique in a prospective randomized controlled trial-perspective for patient-specific finite element analysis. Spine J 17:671–680. https://doi.org/10.1016/j.spinee.2016.11.010
Acknowledgements
We thank Angela Morben, DVM, ELS, from Liwen Bianji (Edanz) (www.liwenbianji.cn), for editing the English text of a draft of this manuscript.
Funding
This work was supported in part by the National Natural Science Foundation of China (81874022 and 82172483 to Xinyu Liu; 82102522 to Lianlei Wang) and Natural Science Foundation of Shandong province (ZR202102210113 to Lianlei Wang).
Author information
Authors and Affiliations
Contributions
LW, CL, and ZW carried out the entire procedure including the study design, data extraction, statistical analysis, manuscript writing and editing. XL conceived of the study, coordinated and participated in the entire process of drafting and editing the manuscript. DL and YT contributed to the data extraction, literature reviewing and statistical analysis. SY contributed to the study design and data analysis. All the authors have contributed significantly. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical approval
This study was approved by the ethics committee of Qilu Hospital of Shandong University [KYLL-2021(KS)-055] and performed according to the tenets of the Declaration of Helsinki.
Informed consent
Written informed consent was obtained from all the enrolled patients.
Consent for publication
The authors agree to publication. This manuscript has not been published in any journals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, L., Li, C., Wang, Z. et al. Comparison of robot-assisted versus fluoroscopy-assisted minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar spinal diseases: 2-year follow-up. J Robotic Surg 17, 473–485 (2023). https://doi.org/10.1007/s11701-022-01442-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-022-01442-5