Abstract
Background
Although favorable long-term survival of Oxford unicompartmental knee arthroplasty (UKA) has been reported regardless of postoperative varus alignment, the effect of degree of varus alignment on patient-reported outcome measures (PROMs) remains unclear. Furthermore, the Forgotten Joint Score-12 (FJS-12), which has a low ceiling effect, may be useful for such assessment. The objective of this study was to evaluate short-term clinical outcomes after Oxford UKA in knees with a greater degree of preoperative varus alignment focusing on use of the FJS-12.
Methods
This retrospective study involved 66 knees that had undergone primary Oxford UKA. Based on the hip-knee-ankle angle, the knees were divided into two alignment groups: severe varus group (≥ 185° varus alignment) and a mild varus group (< 185° varus alignment). PROMs, including the FJS-12, Knee Injury and Osteoarthritis Outcome Score, and Knee Society Score, were obtained pre- and postoperatively for assessment of clinical outcomes. In addition, the ceiling effect of the FJS-12 was evaluated.
Results
All PROMs showed significant improvement after surgery. However, there were no statistically significant differences between the severe varus group and the mild varus group. Moreover, no ceiling effect was found for the FJS-12 in this study.
Conclusion
Short-term results were good for Oxford UKA in knees with a greater degree of varus alignment and were not significantly different from those in knees with mild varus alignment.
Similar content being viewed by others
Introduction
Unicompartmental knee arthroplasty (UKA) is widely known to have good outcomes in patients with medial knee osteoarthritis or osteonecrosis [1,2,3,4]. Oxford mobile-bearing UKA (Oxford UKA; ZimmerBiomet Ltd., Bridgend, UK) is one of the most widely used implants and has been used for a long time [5, 6]. However, total knee arthroplasty (TKA) or high tibial osteotomy (HTO) may be considered for patients with severe varus alignment. Although the survival rate after Oxford UKA is reported to be excellent for varus alignment [7], the effect of the degree of varus alignment on patient-reported outcome measures (PROMs) remains unclear. Kennedy et al. [7] found no relationship between the degree of varus alignment and PROMS using the Oxford Knee Score (OKS). However, the OKS has been reported to have a ceiling effect, and it is unclear whether it is an appropriate measurement [8]. In fact, Kennedy et al. reported a mean of 40 points with a standard deviation of 8 points for the OKS, which has a maximum score of 48 points [7], suggesting that the ceiling effect was present in many patients.
The concept of preserving the constitutional limb alignment in arthroplasty has been attracting attention [9, 10]. Several studies have reported good clinical results using kinematically aligned TKA as a method of preserving constitutional limb alignment [11, 12]. Moreover, using UKA, the patient’s native limb alignment can be restored [13]. Therefore, it is possible that the varus alignment after UKA does not affect PROMs. Nevertheless, patients with a greater degree of varus may have greater concerns about their varus limb alignment preoperatively and be disappointed if there is no change in varus alignment postoperatively. Investigations using more sensitive PROMs with a low ceiling effect are needed.
The Forgotten Joint Score (FJS)-12 is now being widely used as a PROM [14]. This measure has a low ceiling effect and can discriminate results in patients with high scores on other PROMs [15]. There is limited information available on use of the FJS-12 to evaluate outcomes after Oxford UKA in knees with a greater degree of preoperative varus alignment. The objective of this study was to address this gap in the literature, focusing on short-term clinical outcomes.
Materials and methods
This study had a retrospective design and was approved by our hospital ethics committee (approval number: 4952). Informed consent was obtained via an opt-out procedure.
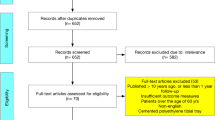
Seventy-two consecutive knees that were treated by primary Oxford UKA between August 2017 and April 2020 were enrolled. We performed the medial UKA for patients with symptomatic medial compartment disease, no symptoms in other compartments, functional cruciate and collateral ligaments, and preserved range of movement (< 15° extension loss, > 100° flexion). We generally assessed the correctability of limb alignment on a valgus stress radiograph and included patients who showed an anatomical femoro-tibial angle of ≤ 180° on a short film. The exclusion criteria were (1) PROMs including FJS-12 not obtained pre- and postoperatively, (2) lateral UKA, and (3) long-leg standing radiographs not obtained pre- and postoperatively. Finally, the study included 66 knees of 59 patients (13 men, 46 women). Mean age at surgery was 75.3 ± 7.1 years and mean body mass index (calculated as kg/m2) was 25.1 ± 4.4. Fifty-four of the 66 knees had primary osteoarthritis and 12 had osteonecrosis.
The knees were divided according to the preoperative and postoperative hip-knee-ankle (HKA) angle measured on digital long-leg standing radiographs into two alignment groups: a severe varus group (≥ 185° of varus alignment) and a mild varus group (< 185° of varus alignment). Postoperative long-leg standing radiographs were obtained at 1 year after surgery. The pre-postoperative change in the radiological parameter (ΔHKA) was calculated.
Surgical technique
All surgical procedures were performed using the same technique and by any of four knee surgery specialists, all of whom were trained in knee replacement surgery. Oxford UKA was performed using a minimally invasive approach with Microplasty instruments and a tourniquet [16, 17]. The tibial component was cemented in all cases, and the femoral side was either cementless or cemented at the surgeon’s discretion. A postoperative closed-suction drain was placed in some cases. Full weight bearing was permitted immediately after surgery in all patients.
Outcome measures
Clinical outcomes were assessed using the FJS-12, Knee Injury and Osteoarthritis Outcome Score (KOOS) [18], and Knee Society Score (KSS) [19] obtained preoperatively and 1 year postoperatively. Patients were asked by their attending surgeon to complete these PROMs. For patients who underwent bilateral UKA, PROMs were assessed for each knee.
To evaluate the ceiling effect of the FJS-12 for Oxford UKA, a ceiling score was defined according to a previous study [8]. The minimal clinically important difference (MCID) in the FJS-12 score after UKA has been defined as 12.5 points [20]. Therefore, the ceiling score was defined as ≥ 87.5 points (i.e., greater than or equal to the maximal score of 100 minus the MCID). The ceiling effect was deemed to be reached when > 15% of the responders achieved the ceiling score.
Complications
Complications occurring up to 1 year postoperatively were retrospectively analyzed using the patients’ medical data.
Statistical analysis
The differences over time within a group were assessed using paired t tests. Differences between the groups were assessed by analysis of variance. Spearman’s rank correlation coefficient was used to assess correlations between preoperative and postoperative varus alignment (HKA) and each of the PROMs postoperatively. All statistical analyses were performed using JMP software (SAS Institute Inc., Cary, NC). A p value of ≤ 0.05 was accepted as statistically significant.
Results
Assessment of perioperative lower limb alignment
Mean HKA was 185.7° ± 4.1° preoperatively and 183.5° ± 3.4° postoperatively. Postoperative ΔHKA was 2.1° ± 3.1° (Table 1).
The 66 knees were divided according to the degree of preoperative HKA (classification 1) into a severe varus group (n = 36) and a mild varus group (n = 30). Mean HKA was 188.5° ± 2.9° preoperatively and 185.1° ± 3.3° postoperatively in the severe varus group and 182.2° ± 2.0° and 181.7° ± 2.3°, respectively, in the mild varus group (Table 2). There was a significant change in alignment, with mean ΔHKA of 3.4° ± 3.5° in the severe varus group and 0.5° ± 1.4° in the mild varus group (p < 0.0001, Table 2).
The 66 knees were similarly divided according to the degree of postoperative HKA (classification 2) into a severe varus group (n = 19) and a mild varus group (n = 47). Mean HKA was 189.0° ± 3.6° preoperatively and 187.4° ± 2.0° postoperatively in the severe varus group and 184.3° ± 3.4° and 182.0° ± 2.3°, respectively, in the mild varus group (Table 2). There was no significant change in alignment, with mean ΔHKA of 1.5° ± 3.5° in the severe varus group and 2.3° ± 2.9° in the mild varus group (p = 0.34, Table 2).
Assessment of perioperative PROMs
All PROMs showed significant improvement postoperatively (Table 3). However, there were no statistically significant differences in PROMs between the severe and mild varus groups either preoperatively or postoperatively according to whether we used classification 1 (preoperative varus; Tables 4 and 5) or classification 2 (postoperative varus; Tables 6 and 7). Moreover, there was no statistically significant difference in the change in KSS for satisfaction between the two groups (Table 8).
The correlations of postoperative PROMs with the preoperative and postoperative HKA angle were assessed in the severe varus group. The FJS-12 value was not significantly correlated with either the preoperative or postoperative HKA angle (preoperative varus: r = 0.18, p = 0.27; postoperative varus: r = 0.27, p = 0.24; Fig. 1). Similarly, postoperative KSS showed no significant correlation with either the preoperative or postoperative HKA angle (preoperative varus: r = 0.07, p = 0.66; postoperative varus: r = 0.27, p = 0.26; Fig. 2). Furthermore, there was no significant correlation between any of the postoperative KOOS subscale values and preoperative or postoperative varus alignment (HKA).
Preoperative degree of varus alignment (HKA) compared with the postoperative FJS-12 value. There was no significant correlation between preoperative varus alignment (HKA angle) and the postoperative FJS-12 value (r = 0.18, p = 0.27) or between postoperative varus alignment (HKA angle) and the postoperative FJS-12 value (r = 0.27, p = 0.24). HKA, hip-knee-ankle; FJS-12, Forgotten Joint Score
Preoperative degree of varus alignment (HKA) versus postoperative KSS. There was no significant correlation between preoperative varus alignment (HKA angle) and postoperative KSS (r = 0.07, p = 0.66) or between preoperative varus alignment (HKA angle) and postoperative KSS (r = 0.27, p = 0.26). HKA, hip-knee-ankle; KSS, Knee Society Score
The ceiling effect of the FJS-12 was assessed using a histogram (Fig. 3). This showed that less than 15% of participants achieved the ceiling score, defined as 87.5 points or more, indicating that there was no ceiling effect for FJS-12 following UKA.
Complications
There were no revision cases requiring conversion to TKA. Furthermore, no additional surgery following UKA was required during the study period. There were no cases of bearing dislocation or fatal thromboembolism.
Discussion
The most important finding of this study was that the short-term results of Oxford UKA for knees with a greater degree of preoperative and postoperative varus alignment were good. There were no significant differences in the results for any of the PROMs used, including the FJS-12, according to whether varus alignment (HKA) was classified as ≥ 5° or < 5° either preoperatively (classification 1) or postoperatively (classification 2). Furthermore, there was no correlation of any of the PROMs with either preoperative HKA in the varus group based on classification 1 or postoperative HKA in the varus group based on classification 2. Moreover, the FJS-12 had no ceiling effect in this study.
Candidates for UKA have recently expanded to include younger and more active patients [21]. UKA is often compared with HTO [22,23,24], and the indications for surgery may also overlap. Although patients with severe varus alignment (HKA ≥ 185°) may be candidates for HTO, this study demonstrates that PROMs following Oxford UKA for knees with more than 5° of varus alignment were relatively good and not significantly different from those in the mild varus group. A study by Jin et al. that included a propensity score matching analysis found that the clinical outcomes were better after UKA than after HTO [25]. Moreover, Kennedy et al. [7] found no correlation between the degree of postoperative varus alignment and postoperative PROMs, which is in line with our present findings. The results of our study support the concept of the Oxford UKA technique [16], which aims to achieve correct ligament balance and restore constitutional limb alignment.
The definition of ceiling effect has been controversial [8]. Various methods have been reported, with some authors using the maximum score and others using scores within 1 standard deviation of the highest score [15, 26]. In this study, the ceiling effect was rigorously evaluated using the MCID according to the method described in a previous study [8]. The MCID for the FJS-12 has been reported to be 12.5 points [20]. Therefore, for example, an FJS-12 of 90 points may not show a clinically significant difference from a maximum FJS-12 score of 100 points. Using this definition, we determined that there is no ceiling effect for the FJS-12 following UKA.
When classification 1 was used, the ΔHKA in the severe varus group was significantly greater than that in the mild varus group. This suggests that the severe varus group in classification 1 included many cases with significant intra-articular deformities as a result of cartilage and bone wear and that the native medial joint line was restored by relatively thin bone resection and/or insertion of a relatively thick bearing [27]. Kuwashima et al. reported that correction of limb alignment was correlated with restoration of medial joint height in fixed bearing UKA [28]. Using classification 1, significant correction of limb alignment was achieved in varus cases. Nevertheless, in some cases with preoperative varus, correction of limb alignment was inadequate as a result of extraarticular deformity, and these cases were subsequently classified as having postoperative varus according to classification 2. Severe preoperative varus alignment has been reported to affect postoperative alignment following UKA [22]. However, in our mild varus group, there was very little change in alignment postoperatively. Given the minimal effect of osteophytes and intra-articular deformities, the concept of resurfacing surgery in Oxford UKA could have been directly implemented [13].
This study has several limitations. First, it did not include a postoperative assessment of radiographic parameters, such as radiolucent lines or malposition of the implant. The correlation between the common finding of physiological radiolucent lines following Oxford UKA and PROMs is still unclear [29]. Although most radiolucent lines are considered not to progress, some adverse phenomena such as micromotion of the implant may be involved [22]. In addition, poorer outcomes have been observed with malpositioning of the implant [30]. However, no apparent implant failure was observed in this cohort. Second, the results were assessed only in the short term and may have changed over time. A previous study found that scores for clinical outcomes, including the OKS, were highest at 1 year postoperatively and declined over a 10-year period [6]. In terms of evaluating the efficiency of the FJS-12, the assessment at 1 year postoperatively may be considered appropriate. Third, the sample size was relatively small. Further studies in larger cohorts are warranted. Fourth, there were a few cases of marked malalignment, such as a fixed varus deformity > 15°, which is not indicated for Oxford UKA [4, 16]. Although we assessed the correctability of preoperative varus deformity based on a valgus stress radiograph, a few patients had > 10° varus postoperatively. The results for marked malalignment remain unclear.
Conclusions
Short-term results for Oxford UKA were good, with no significant difference in outcome according to the degree of varus alignment. The FJS-12 had no ceiling effect when used to assess PROMs following Oxford UKA and was a useful outcome measure.
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Abbreviations
- FJS-12:
-
Forgotten Joint Score-12
- HKA:
-
Hip-knee-ankle
- HTO:
-
High tibial osteotomy
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- KSS:
-
Knee Society Score
- MCID:
-
Minimum clinically important difference
- OKS:
-
Oxford Knee Score
- Oxford UKA:
-
Oxford mobile-bearing unicompartmental knee arthroplasty
- PROMs:
-
Patient-reported outcome measures
- TKA:
-
Total knee arthroplasty
- UKA:
-
Unicompartmental knee arthroplasty
References
Kennedy JA, Palan J, Mellon SJ, Esler C, Dodd CAF, Pandit HG, et al. Most unicompartmental knee replacement revisions could be avoided: a radiographic evaluation of revised Oxford knees in the National Joint Registry. Knee Surg Sports Traumatol Arthrosc. 2020;28:3926–34. https://doi.org/10.1007/s00167-020-05861-5.
Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101 330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet. 2014;384:1437–45. https://doi.org/10.1016/s0140-6736(14)60419-0.
White SH, Ludkowski PF, Goodfellow JW. Anteromedial osteoarthritis of the knee. J Bone Joint Surg Br. 1991;73:582–6. https://doi.org/10.1302/0301-620X.73B4.2071640.
Emerson RH, Alnachoukati O, Barrington J, Ennin K. The results of Oxford unicompartmental knee arthroplasty in the United States: a mean ten-year survival analysis. Bone Joint J. 2016;98-B(10 Supple B):34–40. https://doi.org/10.1302/0301-620X.98B10.
Liddle AD, Pandit H, Judge A, Murray DW. Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the National Joint Registry for England and Wales. Bone Joint J. 2015;97-B:1506–11. https://doi.org/10.1302/0301-620X.97B11.
Pandit H, Jenkins C, Gill HS, Barker K, Dodd CAF, Murray DW. Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br. 2011;93:198–204. https://doi.org/10.1302/0301-620X.93B2.
Kennedy JA, Molloy J, Jenkins C, Mellon SJ, Dodd CAF, Murray DW. Functional outcome and revision rate are independent of limb alignment following Oxford medial unicompartmental knee replacement. J Bone Joint Surg Am. 2019;101:270–5. https://doi.org/10.2106/JBJS.18.00497.
Clement ND, Afzal I, Demetriou C, Deehan DJ, Field RE, Kader DF. The preoperative Oxford Knee Score is an independent predictor of achieving a postoperative ceiling score after total knee arthroplasty. Bone Jount J. 2020;102-B:1519–26. https://doi.org/10.1302/0301-620X.102B11.BJJ-2019-1327.R1.
Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45–53. https://doi.org/10.1007/s11999-011-1936-5.
MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB. Coronal plane alignment of the knee (CPAK) classification: a new system for describing knee phenotypes. Bone Joint J. 2021;103-B:329–37. https://doi.org/10.1302/0301-620X.103B2.
Howell SM, Shelton TJ, Hull ML. Implant survival and function ten years after kinematically aligned total knee arthroplasty. J Arthroplasty. 2018;33:3678–84. https://doi.org/10.1016/j.arth.2018.07.020.
Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Joint J. 2017;99-B:640–6. https://doi.org/10.1302/0301-620X.99B5.
Nishida R, Hiranaka T, Kamenaga T, Hida Y, Fujishiro T, Okamoto K, et al. Impact of joint line orientation on clinical outcomes in bilateral Oxford mobile-bearing unicompartmental knee arthroplasty. Knee. 2021;28:186–93. https://doi.org/10.1016/j.knee.2020.11.018.
Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty. 2012;27(430–6): e1. https://doi.org/10.1016/j.arth.2011.06.035.
Itoh M, Itou J, Kuwashima U, Okazaki K. Good validity and high internal consistency of the Forgotten Joint Score-12 in patients after medial opening wedge high tibial osteotomy. J Arthroplasty. 2021;36:2691–7. https://doi.org/10.1016/j.arth.2021.03.028.
Pandit H, Jenkins C, Barker K, Dodd CAF, Murray DW. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br. 2006;88:54–60. https://doi.org/10.1302/0301-620X.88B1.
Kamenaga T, Hiranaka T, Hida Y, Fujishiro T, Okamoto K. Effect of tibial component position on short-term clinical outcome in Oxford mobile bearing unicompartmental knee arthroplasty. J Orthop Sci. 2018;23:807–10. https://doi.org/10.1016/j.jos.2018.04.012.
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. https://doi.org/10.2519/jospt.1998.28.2.88.
Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH, et al. Development of a new Knee Society scoring system. Clin Orthop Relat Res. 2012;470:20–32. https://doi.org/10.1007/s11999-011-2152-z.
Longo UG, De Salvatore S, Candela V, Berton A, Casciaro C, Sciotti G, et al. Unicompartmental knee arthroplasty: minimal important difference and patient acceptable symptom state for the Forgotten Joint Score. Medicina (Kaunas). 2021;57:324. https://doi.org/10.3390/medicina57040324.
Fu D, Li G, Chen K, Zhao Y, Hua Y, Cai Z. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty in the treatment of unicompartmental osteoarthritis: a meta-analysis. J Arthroplasty. 2013;28:759–65. https://doi.org/10.1016/j.arth.2013.02.010.
Mittal A, Meshram P, Kim WH, Kim TK. Unicompartmental knee arthroplasty, an enigma, and the ten enigmas of medial UKA. J Orthop Traumatol. 2020;21:15. https://doi.org/10.1186/s10195-020-00551-x.
Vajapey SP, Alvarez PM, Greco NJ, Chonko DJ. Medial osteoarthritis in an ACL-deficient knee: a critical analysis review. JBJS Rev. 2021. https://doi.org/10.2106/JBJS.RVW.20.00132.
Mancuso F, Hamilton TW, Kumar V, Murray DW, Pandit H. Clinical outcome after UKA and HTO in ACL deficiency: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:112–22. https://doi.org/10.1007/s00167-014-3346-1.
Jin QH, Lee WG, Song EK, Jin C, Seon JK. Comparison of long-term survival analysis between open-wedge high tibial osteotomy and unicompartmental knee arthroplasty. J Arthroplasty. 2021;36(1562–7): e1. https://doi.org/10.1016/j.arth.2020.11.008.
Jenny JY, Louis P, Diesinger Y. High Activity Arthroplasty Score has a lower ceiling effect than standard scores after knee arthroplasty. J Arthroplasty. 2014;29:719–21. https://doi.org/10.1016/j.arth.2013.07.015.
Kim SJ, Bae JH, Lim HC. Factors affecting the postoperative limb alignment and clinical outcome after Oxford unicompartmental knee arthroplasty. J Arthroplasty. 2012;27:1210–5. https://doi.org/10.1016/j.arth.2011.12.011.
Kuwashima U, Okazaki K, Tashiro Y, Mizu-Uchi H, Hamai S, Okamoto S, et al. Correction of coronal alignment correlates with reconstruction of joint height in unicompartmental knee arthroplasty. Bone Joint Res. 2015;4:128–33. https://doi.org/10.1302/2046-3758.48.
Gulati A, Chau R, Pandit HG, Gray H, Price AJ, Dodd CAF, et al. The incidence of physiological radiolucency following Oxford unicompartmental knee replacement and its relationship to outcome. J Bone Joint Surg Br. 2009;91:896–902. https://doi.org/10.1302/0301-620X.91B7.
Kamenaga T, Hiranaka T, Kikuchi K, Hida Y, Fujishiro T, Okamoto K. Influence of tibial component rotation on short-term clinical outcomes in Oxford mobile-bearing unicompartmental knee arthroplasty. Knee. 2018;25:1222–30. https://doi.org/10.1016/j.knee.2018.06.016.
Acknowledgements
The authors thank ThinkSCIENCE for English language editing.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
JI and KO designed the study. JI analyzed the data and wrote the manuscript draft. UK, MI, and KO revised the manuscript. All authors agreed to the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study had a retrospective design and was approved by our hospital ethics committee (approval number: 4952). Informed consent was obtained via an opt-out procedure.
Consent for publication
Not applicable.
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Itou, J., Kuwashima, U., Itoh, M. et al. Perioperative varus alignment does not affect short-term patient-reported outcome measures following mobile-bearing unicompartmental knee arthroplasty. J Orthop Surg Res 17, 98 (2022). https://doi.org/10.1186/s13018-022-02999-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-02999-5