Abstract
Background
Gut damage allows translocation of bacterial lipopolysaccharide (LPS) and fungal β-D-glucan (BDG) into the blood. This microbial translocation contributes to systemic inflammation and risk of non-AIDS comorbidities in people living with HIV, including those receiving antiretroviral therapy (ART). We assessed whether markers of gut damage and microbial translocation were associated with cognition in ART-treated PLWH.
Methods
Eighty ART-treated men living with HIV from the Positive Brain Health Now Canadian cohort were included. Brief cognitive ability measure (B-CAM) and 20-item patient deficit questionnaire (PDQ) were administered to all participants. Three groups were selected based on their B-CAM levels. We excluded participants who received proton pump inhibitors or antiacids in the past 3 months. Cannabis users were also excluded. Plasma levels of intestinal fatty acid binding protein (I-FABP), regenerating islet-derived protein 3 α (REG3α), and lipopolysaccharides (LPS = were quantified by ELISA, while 1–3-β-D-glucan BDG) levels were assessed using the Fungitell assay. Univariable, multivariable, and splines analyses were performed.
Results
Plasma levels of I-FABP, REG3α, LPS and BDG were not different between groups of low, intermediate and high B-CAM levels. However, LPS and REG3α levels were higher in participants with PDQ higher than the median.
Multivariable analyses showed that LPS association with PDQ, but not B-CAM, was independent of age and level of education. I-FABP, REG3α, and BDG levels were not associated with B-CAM nor PDQ levels in multivariable analyses.
Conclusion
In this well characterized cohort of ART-treated men living with HIV, bacterial but not fungal translocation was associated with presence of cognitive difficulties. These results need replication in larger samples.
Similar content being viewed by others
Background
The gut mucosa plays key roles in physiology and health. By targeting mucosal CD4 T-cells, HIV profoundly affects gut homeostasis, promotes epithelial cell death and decreases cell–cell adhesion. Circulating markers of gut integrity have been used to characterized levels of leaky gut in people living with HIV (PLWH). Intestinal fatty acid-binding protein (I-FABP) is released in the circulation upon gut epithelium cell death. I-FABP blood levels have been found elevated in PLWH taking or not antiretroviral therapy (ART) compared to control without HIV in numerous studies. Higher levels of regenerating islet-derived protein 3 α have also been found in PLWH, regardless of their use of ART, compared to controls [1]. REG3α is an antimicrobial peptide produced in the gut lumen. Upon gut damage, REG3α translocate in the submucosa and its presence in the circulation reflects gut permeability.
HIV-associated gut damage allows passage of microbial products in the submucosa and systemic circulation. This microbial translocation is commonly characterized by quantification of bacterial product lipopolysaccharide (LPS) in blood. Indeed, LPS levels have been shown elevated in both ART-naïve and ART-treated PLWH. Translocation of fungal products β-D-glucan (BDG) has also been described during HIV infection and elevated blood levels of BDG persist in ART-treated PLWH [2, 3]. Both bacterial and fungal products have been shown to participate in persisting levels of inflammation and increased risk of non-AIDS comorbidities in ART-treated PLWH [2, 4,5,6].
Gut damage and microbial translocation have been recurrently associated with inflammation and increased risk of non-AIDS comorbidities in ART-treated PLWH such as adiposity [7], cardiopulmonary function [3], and neurocognitive impairment [8,9,10]. LPS levels have been associated with HIV-associated neurocognitive disorder (HAND), especially in PLWH with hepatitis C infection [11], and with slower processing speed in suppressed alcohol heavy drinkers [12]. Circulating BDG levels have been associated with neurocognitive performance assessed with Global Deficit Score (GDS) [8, 9].
Markers of gut damage, bacterial and fungal translocations have not been compared in their association with neurocognitive performance in ART-treated PLWH. We performed such comparisons in a well characterized group of ART-treated men living with HIV. Cognition was assessed in two ways: performance-based cognitive ability was quantified using the B-CAM [13]; and self-reported cognitive difficulties were documented with the 20-item Patient Deficit Questionnaire (PDQ) that assess memory (retrospective and prospective), attention, organization and planning over the previous 4 weeks.
Methods
Study design and population
In a cross-sectional analysis, a total of 80 ART-treated men living with HIV (MLWH) were selected from the Positive Brain Health Now (CIHR/CTN 372) cohort. The study design and protocol of the study have been reported [14, 15]. Samples were drawn from all participants who completed Visit 1, had available measures of cognition (performance-based and self-report) and frozen biological samples, after excluding participants (i) using anti-acids or proton pump inhibitors as those drugs modulate inflammation; and (ii) with high alcohol use (six or more drinks on one occasion more than once per month or more than 14 standard drinks/week) or cannabis use in the past 3 months. Participants with known inflammatory bowel diseases were also excluded. Current smoking was also excluded at selection, but due to additions to the data after the sample was drawn, 4 people were in fact current smokers. Men were selected as they represent the largest group and the association between inflammation and cognition could vary by sex [16, 17]. Blood collection was performed in the morning in fasting participants.
Participants were classified into three different groups (around 26–27 per group) based on an earlier version of B-CAM score at baseline (low [20–56], intermediate [58–68] or high [70–100]).
Cognitive assessment
To assess performance based self reported cognition, we used B-CAM, a computerized measure of cognition that yields a continuous score. The B-CAM consists of a series of tests including Corsi block task (forward and backward), Eriksen flanker task-incongruent reaction time, mini Trail Making test B (as in the Montreal Cognitive Assessment (MoCA), letter fluency (F-A-S in English, P-L-S in French, 1 min) and word list learning with recall of 8 words [13, 18]. The scoring range of the version available from 0 to 100, with higher values indicating better cognitive ability, with a standard deviation (SD) of 15 (when transformed from the original scale [19]). This test is administered at all visits in the Positive Brain Health Now study.
Presence of cognitive difficulties was documented using the self-reported 20-item Patient Deficit Questionnaire (PDQ), which assesses self-reported memory, attention, organization, and planning over the previous 4 weeks. The questionnaire contains 20 items and leads to a total score on 80, with a SD of 17.5 [19]. A higher score is associated with more cognitive difficulties. The questionnaire pertains to everyday activities of interest to clinicians, such as adherence to care (e.g., “I forget to take medication” or “I forget medical appointments”) and safety (e.g., “I forget to turn off the stove”) and elicits cognitive difficulties that are frequent among PLWH (e.g., “trouble with concentration”). Importantly, the PDQ is brief and can be successfully completed by people with mild to moderate cognitive impairment [20].
Laboratory measurements
HIV infection was diagnosed by quantifying HIV-1 p24 antigen/antibody in plasma and confirmed by Western blot as previously reported [21]. Plasma viral load was quantified by the Abbott RealTime HIV-1 assay (Abbott Laboratories). Plasma samples of study participants were drawn fasting and stored at − 80 °C until used. CD4 and CD8 T-cell counts were measured using 4-color flow cytometry [22]. Peripheral blood mononuclear cell samples of study participants were stored in liquid nitrogen until used.
Measurement of markers of epithelial gut damage and microbial translocation
I-FABP, REG3α and LPS were measured by ELISA as previously described [1, 23]. Plasma BDG was measured by the Fungitell assay in duplicate as per the manufacturer’s instructions with lower extended range (as low as 3.9 pg/mL) (Associates of Cape Cod, Inc East Falmouth, MA).
Statistical analyses
Medians with interquartile range were calculated for all continuous variables. Unpaired comparisons were conducted using t tests or Mann–Whitney's U tests. Spearman's rank correlation test identified associations between two quantitative measures. The Kruskal–Wallis’s test was used to compare more than 2 study groups. P values < 0.05 were considered significant. To control for potential confounding by classical neurocognitive risk factors on the association between each factor and neurocognition indexes, we performed multivariable linear regression analyses using SAS statistical software. Strength of associations were categorized based on effect sizes where β is the numerator and the SD of the B-CAM and PDQ in the entire cohort is the denominator. Cohen’ effect sizes ≤ 0.2 are considered small, effect sizes around 0.5 are considered medium and large is ≥ 0.8. GraphPad Prism 8.0 (GraphPad Software), SAS and R-software were used to perform descriptive statistical analyses. Splines were generated using R.
Patient consent statement
This study was approved by the research ethics board of each participating institutions, including the McGill University Health Centre. Study participants provided written informed consent for study enrollment and participation. All matters were conducted in accordance with the principals of the Declaration of Helsinki.
Results
Characteristics of study participants
As shown in Table 1, all participants were male, living with HIV, and receiving ART. Their HIV viral load was below or equal 50 copies/mL. Their median age was 52. Participants received ART for an average of 12 years (6.6–17.8). Approximatively 36.2% of participants were non-white, and 80% had a post-secondary education level. Fifty-four percent had never smoked (Table 1).
Interestingly, B-CAM and PDQ values did not correlate. Similarly, gut damage and microbial translocation markers did not correlate with each other [24]. Participants appear to have similar LPS, BDG and REG3α levels to those of ART-treated PLWH in our previous work [25]. Levels of I-FABP appear similar to the one of HIV-uninfected controls, although highly variable.
Higher plasma levels of the gut permeability marker REG3α are associated with lower self-reported cognition in ART-treated men living with HIV
We first compared plasma levels of gut permeability markers among ART-treated MLWH with different levels of cognition.
When participants were grouped according to their B-CAM values (low [20–56], intermediate [58–68] or high [70–100]), although their levels tended to increase with worst outcome, no statistically significant differences in I-FABP (median 963, 979 and 1088 pg/mL respectively) or REG3α (4.7, 3.8 and 4.2 ng/mL respectively) levels were observed between groups (Fig. 1A, B).
Levels of gut damage markers among groups of ART-treated men living with HIV with different cognitive function. Levels of the gut damage marker I-FABP (A, C) and gut permeability marker REG3α (B, D) in ART-treated men living with HIV with higher than the B-CAM groups (A, B) or with median PDQ lower or higher than the median of 26.25 (C, D). A, B: Kruskal–Wallis’s test with Dunn’s post-test. C, D: Mann Whitney’s test
When participants were grouped based on their PDQ levels, those with PDQ higher than the median 26.25 had similar levels of IFABP (1038 and 931 pg/mL respectively, p = 0.97) but higher levels of REG3α (3.3 and 5.1 ng/mL respectively, p = 0.004) (Fig. 1C, D).
Microbial translocation of LPS is associated with low self-reported cognition with ART-treated men living with HIV
We then compared plasma levels of microbial translocation markers among ART-treated MLWH with different levels of cognition.
When participants were grouped according to their B-CAM values (low, intermediate or high), plasma levels of LPS (median 42.6, 57.5 and 53.0 pg/mL respectively) or BDG (16.0, 12.0 and 15.0 pg/mL respectively) were similar between groups (Fig. 2A, B).
Levels of microbial translocation markers among groups of ART-treated men living with HIV with different cognitive function. Levels of the bacterial marker LPS (A, C) and fungal marker BDG (B, D) in ART-treated men living with HIV with higher than the B-CAM groups (A, B) or with median PDQ lower or higher than the median of 26.25 (C, D). A, B: Kruskal–Wallis’s test with Dunn’s post-test. C, D: Mann Whitney’s test. LPS Lipopolysaccharides, BDG 13-β-D-Glucan, B-CAM brief cognitive ability measure, PDQ patient deficit questionnaire
When participants were grouped based on their PDQ levels, those with PDQ higher than the median 26.25 had higher levels of LPS (median 39.0 and 54.6 pg/mL respectively, p = 0.01) and similar levels of BDG (16.0 and 13.0 pg/mL respectively, p = 0.15) (Fig. 2C, D).
Translocation of LPS is independently associated with low self-reported cognition
We then performed multivariable analyses to assess the influence of known confounding factors on the association between gut markers and cognition by including age and education category in our models. Data were considered continuous, ordinal in 4 groups or binary. β was considered to assess the influence of each biomarker on cognition (Fig. 3).
multivariable analyses of gut permeability and microbial translocation biomarkers with self-reported cognition. Influence of each cognition parameter on biomarkers levels is indicated with color levels. Cohen’ effect sizes ≤ 0.2 are considered small, effect sizes around 0.5 are considered medium and large is ≥ 0.8
When accounting for age and education, multivariable analyses showed only weak effects: REG3α seems to have a deleterious effect with increase in plasma levels associated with lower B-CAM values (negative β) when transformed into ordinal and binary data. LPS and BDG levels appeared to have weak protective effect, with plasma levels associated with higher B-CAM (positive β). None of those logistic regression analyses appeared statistically significant (Additional file 1: Table S1).
When looking at PDQ values, regression analyses showed that the association of LPS with worst self-reported cognition was independent of age and education category. Although a tendency was observed, higher levels of REG3α were not linked with lower cognitive abilities after adjustment (Fig. 3, Additional file 1: Table S1). Education but not age appeared to influence REG3α association with PDQ. Higher plasma BDG levels had a small effect on self-reported cognition (lower PDQ score), with an effect size of 0.27. However, the magnitude of the association was not statistically significant (Fig. 3, Additional file 1: Table S1).
None of the gut permeability markers correlated with CD4 T-cell count, and addition of CD4 T-cell count as a confounding variable to the multivariable analysis mildly changed R, β, and p-values, and did not influence our conclusion.
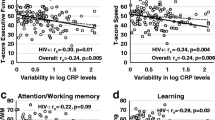
Splines analyses were performed for each association (Fig. 4). Confidence intervals were selected for each biomarker (Fig. 3). Between 20 and 70 pg/mL, LPS seemed to have a positive association with B-CAM, indicating that higher LPS levels were unexpectedly associated with better cognition (Fig. 4C).
Splines analyses of each biomarker and PDQ score showed that LPS appeared to have a strong link with worst cognition between 20 and 70 pg/mL (Fig. 5C). REG3α levels had a similar but weaker link with cognition (Fig. 5B). I-FABP and BDG levels had weaker protective effect (Fig. 5A and D).
Spline graphs of gut damage markers vs. PDQ adjusted for age and education category in men living with HIV. I-FABP (A), REG3α (B), LPS (C) or BDG (D) levels. Splines with 2 degrees of freedom are depicted. Confidence interval is shown in a blue frame. I-FABP intestinal fatty acid binding protein, REG3α regenerating islet-derived protein 3 α, B-CAM brief cognitive ability measure, PDQ patient deficit questionnaire, LPS Lipopolysaccharides, BDG 1-3-β-D-Glucan, B-CAM brief cognitive ability measure, PDQ patient deficit questionnaire
Discussions
Herein, we show that microbial translocation of bacterial LPS in the blood is associated with worst self-reported cognition in ART-treated MLWH, independent of age and education levels. Such association was observed using univariable, multivariable logistic and splines analyses. REG3α levels also showed such an association with self reported cognition, which was decreased after consideration of education categories. We did not find an association between self-reported cognitive function with levels of I-FABP or between any of the measured biomarkers of microbial translocation and performance-based cognitive ability. Interestingly, we have also previously shown that I-FABP levels were stable after 2 years on ART, when REG3α levels decreased, indicating that decreased REG3α but not I-FABP levels might indicate mucosal epithelium reparation. Hence, elevated REG3α levels could reflect a lack of gut repair, then being associated with chronic inflammation and decreased cognition [1].
BDG can be associated with stronger immune functions by trained immunity, a form of memory of the innate immune system allowing stronger responses to repeated stimuli. However, BDG stimulation of trained immunity in the context of chronic stimulation, such as the one we would expect from microbial translocation in PLWH, has not been described and still under debate [26, 27]. Hence, the link between BDG and self-reported cognition should be replicated in larger cohorts.
Our study is unique in considering both performance-based and self-reported cognition. While existing studies have found an association between a diagnosis of HAND and various biomarkers of microbial translocation, we are the first to report an association between markers of gut permeability and self-reported cognitive function. This finding is important because self-reported cognition is associated with everyday function and quality of life to a much greater extent than a diagnosis of HAND [28, 29], suggesting that microbial translocation is of clinical importance to outcomes that are meaningful for persons living with HIV.
A few reasons may explain the discrepancy between the findings of association with self-reported cognition versus the lack of association with performance-based cognition. First, there are two construct that, while overlapping, represent distinct aspects of cognition. A recent NIMH-sponsored meeting on biotypes of CNS complications in persons living with HIV highlighted the heterogeneity of manifestations of neuro-HIV [30] and the presence of self-reported cognitive difficulties may represent one phenotype of brain involvement. We did not test the association between biomarkers of gut permeability and a diagnosis of HAND for several reasons. This diagnosis, which required administration of neuropsychological testing, was not available in all participants; the diagnosis is prone to misclassification [28]; and continuous measures are more likely to uncover small associations. The B-CAM, which was developed specifically to measure cognition in persons living with HIV, has the strong psychometric properties required to maximize the likelihood of identifying relationships.
The source of microbial translocation is still debated in ART-treated PLWH. A consensus in forming toward microbial product found in blood being of gut origin. Moreover, the concurrent association of cognitive dysfunction with both the gut permeability marker REG3α and LPS are in accordance with this statement. We have showed that translocation markers are independent of food intake [31], although they vary during the day [23]. Daily variations of microbial translocation markers should be considered with time of blood collection and circadian rhythm of participants taken into account in future analyses.
Possible mechanisms of microbial translocation-associated decrease in cognitive abilities also lend support to the importance of inflammatory pathways. Interestingly, LPS [32] and BDG [9] have been found to cross the blood–brain barrier. There, they could induce inflammation, and participate in disorganisation of neuronal networks. Also, systemic levels of LPS and BDG induce inflammation [5, 12]. For instance, LPS activation of monocytes has been associated with dementia in AIDS patients [33]. Direct activation of cells or cells activated in an LPS-induced inflammatory environment have the capacity to cross the blood brain barrier and disrupt brain homeostasis. Finally, the gut microbiota could also play a role as dysbiosis has been implicated in disruption of gut homeostasis, gut permeability and inflammation. For instance, different abundance of the mucin-degrading Akkermansia muciniphila in the gut has been link with variations in brain functions through a gut-brain axis [34, 35]. Indeed, we have also observed that gut dysbiosis was linked with microbial translocation in PLWH [36]. Overall, microbial translocation-induced inflammation perturbs brain function, and persisting gut permeability on ART could be associated with brain inflammation and decreased cognitive abilities.
In addition to the cross-sectional nature of our studies, our study is limited by the lack of prospective data. Indeed, microbial translocation could have participated in deteriorating cognitive function, before partly resorbing. Also, we have shown that I-FABP and LPS plasma levels variate daily in ART-treated PLWH, time of blood collection and circadian rhythm of participants should be considered in further analyses [23]. Finally, the link between microbial translocation and cognitive abilities in women living with HIV will have to be assessed in further studies.
It is difficult to compare our results in HIV negative people as behaviour and lifestyle are different. Future studies could compare PLWH to HIV negative controls recruited in the same medical centres and sex-health clinics.
Conclusion
Lower cognitive performance is still burdening PLWH even after years of ART. Persisting inflammation is responsible for the increased risk of non-AIDS comorbidities and accelerated aging in ART-treated PLWH, including for neurocognitive disorders. Our study findings suggest that gut permeability and microbial translocation are associated with the presence of self-reported cognitive difficulties in some PLWH. The findings need to be replicated and our estimates of effect size can be used to inform optimal sample sizes for future studies. The relationship between these biomarkers and changes in cognition should also be examined, as is the co-calibration between biomarkers values and cognition longitudinally. New therapeutic interventions are required to improve gut health in PLWH, reduce the risk of developing non-AIDS comorbidities to prevent cognitive disorders in ART-treated PLWH [37,38,39,40].
Availability of data and materials
Data and materials are available upon reasonable request to corresponding author. Data were presented in part virtually at the AIDS 2022 conference in Montréal, QC, Canada.
References
Isnard S, Ramendra R, Dupuy FP, et al. Plasma levels of C-Type Lectin REG3alpha and gut damage in people with human immunodeficiency virus. J Infect Dis. 2020;221(1):110–21.
Mehraj V, Ramendra R, Isnard S, et al. Circulating (1–>3)-beta-D-glucan Is associated with immune activation during human immunodeficiency virus infection. Clin Infect Dis. 2020;70(2):232–41.
Morris A, Hillenbrand M, Finkelman M, et al. Serum (1–>3)-beta-D-glucan levels in HIV-infected individuals are associated with immunosuppression, inflammation, and cardiopulmonary function. J Acquir Immune Defic Syndr. 2012;61(4):462–8.
Brenchley JM, Douek DC. Microbial translocation across the GI tract. Annu Rev Immunol. 2012;30:149–73.
Brenchley JM, Price DA, Schacker TW, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12(12):1365–71.
Hoenigl M, de Oliveira MF, Perez-Santiago J, et al. Correlation of (1–>3)-beta-D-glucan with other inflammation markers in chronically HIV infected persons on suppressive antiretroviral therapy. GMS Infect Dis. 2015. https://doi.org/10.1097/MD.0000000000003162.
Dirajlal-Fargo S, Moser C, Rodriguez K, et al. Changes in the Fungal Marker β-D-glucan after antiretroviral therapy and association with adiposity. Open Forum Infect Dis. 2019. https://doi.org/10.1093/ofid/ofz434.
Gianella S, Letendre SL, Iudicello J, et al. Plasma (1 –> 3)-beta-D-glucan and suPAR levels correlate with neurocognitive performance in people living with HIV on antiretroviral therapy: a CHARTER analysis. J Neurovirol. 2019;25(6):837–43.
Hoenigl M, de Oliveira MF, Perez-Santiago J, et al. (1–>3)-beta-D-Glucan levels correlate with neurocognitive functioning in HIV-infected persons on suppressive antiretroviral therapy: a cohort study. Medicine. 2016;95(11): e3162.
Bandera A, Taramasso L, Bozzi G, et al. HIV-associated neurocognitive impairment in the modern ART Era: are we close to discovering reliable biomarkers in the setting of virological suppression? Front Aging Neurosci. 2019;11:187.
Vassallo M, Dunais B, Durant J, et al. Relevance of lipopolysaccharide levels in HIV-associated neurocognitive impairment: the Neuradapt study. J Neurovirol. 2013;19(4):376–82.
Monnig MA, Kahler CW, Cioe PA, et al. Markers of microbial translocation and immune activation predict cognitive processing speed in heavy-drinking men living with HIV. Microorganisms. 2017. https://doi.org/10.3390/microorganisms5040064.
Brouillette MJ, Fellows LK, Finch L, Thomas R, Mayo NE. Properties of a brief assessment tool for longitudinal measurement of cognition in people living with HIV. PLoS ONE. 2019;14(3): e0213908.
Mayo NE, Brouillette MJ, Fellows LK. Understanding and optimizing brain health in HIV now: protocol for a longitudinal cohort study with multiple randomized controlled trials. BMC Neurol. 2016. https://doi.org/10.1186/s12883-016-0527-1.
Quigley A, Brouillette MJ, Fellows LK, Mayo N. Action for better brain health among people living with HIV: protocol for a randomized controlled trial. BMC Infect Dis. 2021;21(1):843.
Raghavan A, Rimmelin DE, Fitch KV, Zanni MV. Sex differences in select non-communicable HIV-associated comorbidities: exploring the role of systemic immune activation/inflammation. Curr HIV/AIDS Rep. 2017;14(6):220–8.
Stadtler H, Shaw G, Neigh GN. Mini-review: Elucidating the psychological, physical, and sex-based interactions between HIV infection and stress. Neurosci Lett. 2021;747: 135698.
Koski L, Brouillette MJ, Lalonde R, et al. Computerized testing augments pencil-and-paper tasks in measuring HIV-associated mild cognitive impairment(*). HIV Med. 2011;12(8):472–80.
Mayo NE, Brouillette MJ, Scott SC, et al. Relationships between cognition, function, and quality of life among HIV+ Canadian men. Qual Res. 2019. https://doi.org/10.1007/s11136-019-02291-w.
Brouillette MJ, Fellows LK, Palladini L, Finch L, Thomas R, Mayo NE. Quantifying cognition at the bedside: a novel approach combining cognitive symptoms and signs in HIV. BMC Neurol. 2015;15:224.
Farhour Z, Mehraj V, Chen J, Ramendra R, Lu H, Routy JP. Use of (1→3)-β-d-glucan for diagnosis and management of invasive mycoses in HIV-infected patients. Mycoses. 2018;61(10):718–22.
Mehraj V, Cox J, Lebouche B, et al. Socio-economic status and time trends associated with early ART initiation following primary HIV infection in Montreal, Canada: 1996 to 2015. J Int AIDS Soc. 2018. https://doi.org/10.1002/jia2.25034.
Ouyang J, Isnard S, Lin J, et al. Daily variations of gut microbial translocation markers in ART-treated HIV-infected people. AIDS Res Ther. 2020;17(1):15.
Dang J, King KM, Inzlicht M. Why are self-report and behavioral measures weakly correlated? Trends Cogn Sci. 2020;24(4):267–9.
Isnard S, Fombuena B, Sadouni M, et al. Circulating beta-d-Glucan as a marker of subclinical coronary plaque in antiretroviral therapy-treated people with human immunodeficiency virus. Open Forum Infect Dis. 2021;8(6):109.
Isnard S, Lin J, Bu S, Fombuena B, Royston L, Routy JP. Gut leakage of fungal-related products: turning up the heat for HIV infection. Front Immunol. 2021;12: 656414.
Divangahi M, Aaby P, Khader SA, et al. Trained immunity, tolerance, priming and differentiation: distinct immunological processes. Nat Immunol. 2021;22(1):2–6.
Brouillette MJ, Koski L, Forcellino L, et al. Predicting occupational outcomes from neuropsychological test performance in older people with HIV. AIDS. 2021;35(11):1765–74.
Heaton RK, Marcotte TD, Mindt MR, et al. The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychol Soc. 2004;10(3):317–31.
Mukerji SS, Petersen KJ, Pohl KM, et al. Machine learning approaches to understand cognitive phenotypes in people with HIV. J Infect Dis. 2022. https://doi.org/10.1093/infdis/jiac293.
Hoenigl M, Lin J, Finkelman M, et al. Glucan rich nutrition does not increase gut translocation of beta-glucan. Mycoses. 2021;64(1):24–9.
Jiang W, Luo Z, Stephenson S, et al. Cerebrospinal fluid and plasma lipopolysaccharide levels in human immunodeficiency virus type 1 infection and associations with inflammation, blood-brain barrier permeability, and neuronal injury. J Infect Dis. 2021;223(9):1612–20.
Ancuta P, Kamat A, Kunstman KJ, et al. Microbial translocation is associated with increased monocyte activation and dementia in AIDS patients. PLoS ONE. 2008;3(6): e2516.
Xu R, Zhang Y, Chen S, et al. The role of the probiotic Akkermansia muciniphila in brain functions: insights underpinning therapeutic potential. Crit Rev Microbiol. 2022. https://doi.org/10.1080/1040841X.2022.2044286.
Ouyang J, Lin J, Isnard S, et al. The bacterium Akkermansia muciniphila: a sentinel for gut permeability and its relevance to HIV-related inflammation. Front Immunol. 2020;11:645.
Ellis RJ, Iudicello JE, Heaton RK, et al. Markers of Gut Barrier function and microbial translocation associate with lower gut microbial diversity in people with HIV. Viruses. 2021;13(10):1891.
Isnard S, Fombuena B, Ouyang J, et al. Camu Camu effects on microbial translocation and systemic immune activation in ART-treated people living with HIV: protocol of the single-arm non-randomised Camu Camu prebiotic pilot study (CIHR/CTN PT032). BMJ Open. 2022;12(1): e053081.
Isnard S, Lin J, Fombuena B, et al. Repurposing metformin in nondiabetic people with HIV: influence on weight and gut microbiota. Open Forum Infect Dis. 2020;7(9):338.
Ouyang J, Isnard S, Lin J, et al. Metformin effect on gut microbiota: insights for HIV-related inflammation. AIDS Res and Ther. 2020. https://doi.org/10.1186/s12981-020-00267-2.
Ouyang J, Isnard S, Lin J, et al. Treating from the inside out: relevance of fecal microbiota transplantation to counteract gut damage in GVHD and HIV infection. Front Med. 2020;7:421.
Acknowledgements
The authors are grateful to Fernando Gonzales Aste, Josée Girouard, Angie Massicotte, Eshel Espaldon, and Reynan Espaldon for study coordination and assistance.
Funding
This study was funded by the Canadian Institute of Health Research Team Grant [TCO-125272] and a grant from CIHR/Canadian HIV Clinical Trials Network (CTN 273). This study was also financed by the Fonds de la Recherche Québec-Santé (FRQ-S): Réseau SIDA/Maladies Infectieuses; the CIHR (Grant Numbers MOP 103230 and PJT 166049).
Author information
Authors and Affiliations
Contributions
SI participated in study design, performed measurements in plasma samples with TM, JL, BF and SB. SI, LR, SS, and MK and performed statistical analysis. CAB helped with study design and regulatory implementations. MF performed BDG measurements in plasma. SI prepared the first and final drafts of the manuscript. Study was designed by MJB, LF, NEM and JPR. Funds were obtained by MJB, LF, NEM and JPR. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethics board of each participating institutions, including the McGill University Health Centre. Study participants provided written informed consent for study enrollment and participation. All matters were conducted in accordance with the principals of the Declaration of Helsinki.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
: Univariable and multivariable analyses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Isnard, S., Royston, L., Scott, S. et al. Translocation of bacterial LPS is associated with self-reported cognitive abilities in men living with HIV receiving antiretroviral therapy. AIDS Res Ther 20, 30 (2023). https://doi.org/10.1186/s12981-023-00525-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-023-00525-z