Abstract
Background
Significant scientific research has been conducted concerning menopausal syndrome(MPS), yet few bibliometric analyses have been performed. Our aim was to recognise the 100 most highly cited published articles on MPS and to analytically evaluate their key features.
Methods
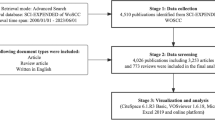
To identify the 100 most frequently cited articles, a search was conducted on Web of Science using the term 'menopausal syndrome'. Articles that matched the predetermined criteria were scrutinised to obtain the following data: citation ranking, year of publication, publishing journal, journal impact factor, country of origin, academic institution, authors, study type, and keywords.
Results
The publication period is from January 1, 2000, to August 31, 2022. The maximum number of citations was 406 and in 2012. The median citations per year was 39.70. Most of the articles focused on treatment and complications. These articles were published in 36 different journals, with the Journal of MENOPAUSE having published the greatest number (14%). Forty-eight articles (48%) were from the United States, with the University of Pittsburgh being the leading institute (9%). Joann E. Manson was the most frequent first author (n = 6). Observational studies were the most frequently conducted research type (n = 53), followed by experimental studies (n = 33). Keyword analysis identified classic research topics, including genitourinary syndrome of menopause, bone mineral density (BMD), and anti-mullerian hormone (AMH) loci.
Conclusion
Using bibliometrics, we conducted an analysis to identify the inadequacies, traditional focal points, and potential prospects in the study of MPS across current scientific areas. Treatment and complications are at the core of MPS research, whereas prediction and biomarkers have less literature of high quality. There is a necessity for innovative analytical metrics to measure the real effect of these papers with a high level of citation on clinical application.
Similar content being viewed by others
Introduction
Menopausal syndrome (MPS) is a series of disorders of autonomic nervous system, accompanied by neuropsychological symptoms, caused by estrogen fluctuation or decrease in the period of before and after menopause. The core reason lies in the gradual decline of ovarian function, including natural menopause and artificial menopause. In particular, this is not the end of old age, but the beginning of senescence in biological age. The life expectancy of women further increased to 80.88 years [1], which means the irreversible state of low estrogen will last for at least 30 ~ 40 years. 1/3 or even longer time will be in the post-menopausal senescence state for women, and the more incidence of complication will be significantly increased [2, 3]. We conduct a comprehensive statistical overview of all literature in the MPS field, providing a broad perspective from a macroscopic viewpoint to understand the research trends and knowledge structure of this area, presenting an overview of the research landscape across the entire field. Aims to revealing the milestones and discovering the research direction, it evaluates the status quo of MPS by quantitatively analyzing the selected articles in this study.
Methods
Inclusion criteria and exclusion criteria
Electronic database of Web of Science was used to query the MPS related articles. The retrieval strategy was TS = (‘perimenopausal syndrome’) OR TS = (‘postmenopausal syndrome’) OR TS = (‘premenopausal Syndrome’) OR TS = (‘menopausal syndrome’) OR TS = (‘Climacteric syndrome’). The inclusion criteria included the core subject as MPS in ‘journal article’, or ‘original article’. The publication year restricted from January 1st, 2000 to August 31st, 2022. The exclusion criteria included MPS articles in position papers, guidelines, reviews, meta-analysis, letters, or editorials. All the included articles independently examined and verified by two reviewers (W. Zhang and Z. Jin). Discrepancies were resolved by consensus with the third senior reviewer (L. Zhao).
Citation analysis
This study was strictly operated following the previous bibliometric literatures [4,5,6]. The data was extracted, besides the keywords, which also including type of the study, authors, country and institution, title, quote frequency, publication year, journal. All the words must be uniformly standardized. And, little information provided words, such as women, disease, etc., has been eliminated for the subsequent analysis. The most important information was focus on the co-relationship of authorship, institution, country and keywords in this database. Additionally, a systematic literature review was carried out around keywords.
Statistical analysis and bibliometric network construction
All the statistical analysis was performed by the IBM SPSS Statistics (version 26.0), following the continuous variables with normal distribution expressed as the means with standard deviation (SD). VOSviewer software (version 1.6.18, Leiden University Center for Science and Technology Studies, Leiden, Netherlands) and CiteSpace software (version 6.1.3,) was used to structure the bibliometric network.
Results
The 100 top-cited articles were summarized in descending order according to the number of total citations (Table 1). With the publishing date from 2012 to 2022, the largest number of literature published in the year 2012, 2013, 2014, respectively. Among 100 top-cited articles, 53 publications were observational study. Next up were experimental study(n = 33), in vivo study(n = 10), in vitro study(n = 3). Of 36 different journals, MENOPAUSE (n = 14), J CLIN ENDOCR METAB (n = 12), MATURITAS(n = 6) and JAMA related journal (n = 6) published the greatest number of these articles. The median times cited all databases of MPS was 111 (IQR, 98.25–147.5). The maximum of total citations was 406 in BRIT MED J, which reported by Hvidovre Univ Hosp of Denmark in 2012. And, the median of average times per year of cited all databases of MPS was 14.07 (IQR, 10.44–20.07). And, the maximum of average times per year was 62.5 in CELL, which reported by the scientific researchers of Chinese Academy of Sciences of China in 2020.
Active authors
In order to finding the information on influential author and research groups, the fruitful partnership network of authors was constructed (Fig. 1). Of the top 2 active authors (published above 3 articles), Manson, joann e. contributed the most papers (6 publications, 5%), focusing on MPS related biological aging, breast cancer, cardiovascular risk factors, vasomotor symptoms, cognitive function, vaginal estrogens. Followed by Freeman, ellen w., Hodis, howard n., Budoff, matthew j. with 5, 4 and 4 publications respectively, which also paid more attention on the anxiety or depression on the above MPS related topic. We conducted correlation analyses to assess the relationships between journal impact factors and both citation frequency and average citations per article. Initial normality tests for these variables revealed that they did not follow a normal distribution (P < 0.000), thus Spearman's rank correlation was utilized. A weak positive correlation was identified between journal impact factors and average citation counts (r = 0.258, P = 0.010), and a low-to-moderate positive correlation between journal impact factors and citation frequency (r = 0.310, P = 0.002).
Active countries and institutions
The partnership network of countries and institutions was constructed. In the database, with established good cooperative relations with scientists from many countries, the leading country was the USA, which published 48 articles, followed by Italy (n = 19), England (n = 15), and Australia (n = 12) (Fig. 2). As the most productive institution,University of Pittsburgh has been published 9 articles (Fig. 3). Followed by Università degli Studi di Pavia (n = 8), Harvard University (n = 7) and Stanford University(n = 7).
Active Keywords
CiteSpace 5.8.R3 was used to construct the keywords analysis, which showed a reasonable description of research focus in MPS. Of the 10 types in keywords, the top 5 types were interlace, genitourinary syndrome of menopause, bone mineral density (BMD), anti-mullerian hormone (AMH), loci (Fig. 4). Of the 10 types in classification, the top 5 types were obstetrics and gynecology, cardiac and cardiovascular systems, physiology, reproductive biology, genetics and heredity (Fig. 5). Of the 10 types in title, the top 5 types were individual patient data, cardiovascular event, body composition, ovarian reserve, estrogen treatment (Fig. 6). These involve the prominent problems from the vasomotor symptom (VMS) in MPS to vulvovaginal atrophy and genitourinary syndrome of menopause in menopausal related diseases(Table 2).
Discussion
MPS has developed into a global health epidemic. Under the circumstances that the aging society has formed and gradually intensified, it will suffer more chronic diseases especially in countries and regions with high life expectancy. In particular, the post-menopause time are expected on average to live more than another 30 years. In this bibliometric study and systematic review of MPS related top-cited articles, the analysis showed the information of authorship, country, institution and keywords. It systematically summarized the development status in this field in the past 10 years in order to provide ideas for future research.
Genitourinary syndrome of menopause
The condition of hypoestrogenism related to menopause has a strong negative impact on vaginal and urinary health, often leading to a condition called genitourinary syndrome (GSM), a term put forward in 2014 [7], although it was used to be called vulvar and vaginal atrophy (VVA). Approximately 50% of postmenopausal women have vulvar, vaginal, and clitoral symptoms, including vaginal dryness, irritation, and itching; sexually related problems such as dyspareunia; and urinary problems including dysuria and recurrent urinary tract infections [8, 9]. The most recent surveys indicated that VVA affected most peri- and postmenopausal women with a prevalence ranging from 36% to almost 90% [10], so GSM is a common, under-diagnosed, and under-treated disorder [11, 12]. Measures to improve its early detection and its appropriate management are needed. However, significant barriers to treatment include a lack of knowledge about VVA, reluctance to discuss symptoms with healthcare professionals (HCPs), safety concerns, inconvenience, and inadequate symptom relief from available treatments [13].
People pay more attention to non-hormonal therapy and newer treatment options including selective estrogen receptor modulators, vaginal dehydroepiandrosterone, and laser therapy, etc. Treatment with the fractional CO2 laser has been proven to be feasible and induced a significant improvement of VVA symptoms by ameliorating vaginal health in postmenopausal women as well as a significant improvement of sexual function and satisfaction with sexual life [14, 15]. Its security has also been assessed, which indicated that it could produce a remodeling of vaginal connective tissue without causing damage to surrounding tissue [16]. Vaginal erbium laser is the second-generation thermotherapy for the genitourinary syndrome of menopause, and recent data suggested that laser energy can be used for the treatment of postmenopausal women suffering from GSM with rapid and more long-lasting effects compared to topical estriol treatment [17, 18].
Menopausal hormone therapy
The most-cited article was published by Schierbeck, Louise Lind from Denmark published in BRITISH MEDICAL JOURNAL in 2012 (cited 397 times) [19]. It focus on hormone replacement therapy (MHT). Although the situation has changed a lot since the 1942 approval of conjugated equine estrogens, menopausal hormone therapy (MHT) remains the most standard scheme to collectively address the menopausal related symptoms (such as vasomotor symptoms) and additional concerns (such as postmenopausal osteoporosis) [20]. However, including oestrogen or an oestrogenic compound, MHT is also associated with risks of serious health conditions including breast, ovarian and endometrial cancer, stroke and venous thromboembolism, etc.. Additionally, MHT related health risks are proportional to the duration of use. It should be used in before the average menopause age, not all age groups [21, 22]; and racial differences should be taken into account [23, 24]. Although the development of transdermal or vaginal drug delivery has greatly reduced the side effects, the acceptance of menopausal suffers is still low [25, 26]. Therefore, the optimal duration of MHT cannot be recommended, but the initial indications of MHT and the balance of interests and risks for each woman must be strictly considered (Mendoza et al. 2022; Trémollieres et al. 2022; Velentzis et al. 2021).
In recent years, studies have conducted in-depth research on the mechanism of adverse events (AEs) caused by MHT. Dydrogesterone has displayed a favorable safety and tolerability profile during its 60-year use. AEs concerning breast cancer risk, endometrial cancer risk, venous thromboembolism risk, and cardiovascular risk were found to be minimal when dydrogesterone was used as part of a menopausal hormone therapy regimen lasting ≤ 260 weeks [27]. Over a (median) 18-year follow-up period (1993–2016), conjugated equine estrogens nominally significant reduce for coronary heart disease, breast cancer, hip fracture, and all-cause mortality. However, estrogens plus progestin increased breast cancer risk, and reduced endometrial cancer risk [28]. With fewer AEs and more benefits in better sexual life, skin condition and physical activity, alternative therapies receives more and more attention [29]. Compared with, medroxyprogesterone acetate (MPA) and norethisterone (NET) which increased breast cancer risk, evidence suggests a differential effect of MHT containing E2 or natural progesterone (P4) and those containing CEE or progestins, with some evidence trending to a potentially better safety profile with E2 and/or P4 [30,31,32]
Cardiovascular disease
The decrease in estrogen level causing the dysfunction of the autonomic nervous system and the decrease of the protective effect on blood vessels, which increases the vasodilation and contraction symptoms that may adversely affect vascular health as well as the occurrence of cardiovascular diseases [33], such as atherosclerosis, stroke, hypertension, and arrhythmias.In the cardiovascular system, aging is accompanied by increased stiffness, increased fibrosis, loss of contractile reserve, increased ROS and endothelial dysfunction. All of these factors contribute to cardiovascular dysfunction [34]. Endothelial dysfunction, on the other hand, is characterized by reduced endothelium-dependent vasodilation, a biomarker of aging, and an important predictor of cardiovascular events in women [35]. Menopausal hormone therapies (MHT) may modulate endothelial function and reduce development of vascular lesions.
Sex hormone levels, especially those in which total testosterone is higher compared to estrogen in the postmenopausal [36], that is, lower endogenous estrogen levels resulting from menopausal transition [37] and higher endogenous androgens [38], may mediate the increased risk of cardiovascular disease (including blood pressure, C-reactive protein (CRP), and insulin resistance) in postmenopausal women [39].The Danish Osteoporosis Prevention Study (DOPS) randomized trial found that women treated with estradiol or in combination with sequential norethindrone acetate in the early postmenopausal period had a significantly lower risk of coronary heart disease than untreated women, demonstrating the effectiveness of hormone replacement therapy for cardiac diseases such as heart failure or myocardial infarction in perimenopausal women [40].The Early versus Late Intervention Trial with Estradiol (ELITE) suggests that the effect of hormone therapy on cardiovascular disease varies may depend on the timing of initiation of treatment relative to the perimenopausal period. Carotid intima-media thickness (CIMT) has been found to be inversely correlated with plasma total estradiol levels in the late postmenopausal period [41]. Early Menopausal hormone therapy (MHT) did not affect progression of atherosclerosis despite improving some markers of CVD risk [42]. Oral estradiol therapy within 6 years of postmenopausal significantly reduced CIMT progression but not when it was initiated in women who were 10 or more after menopause [41].Therefore, grasping the duration of menopause is helpful for the prevention and treatment of cardiovascular disease risk in menopausal women.
Breast cancer
In 2020, female breast cancer ranked first in the global incidence of malignant tumors, with about 2.3 million new cases, accounting for 11.7% of all new cases [43]. Numerous studies have shown that women have an increased risk of breast cancer after menopause. Changes in hormone levels are the underlying cause of the risk of disease and decreased serum luteinizing hormone and follicle-stimulating hormone levels after menopause are associated with increased ER and PR expression and decreased HER2 expression in breast cancer patients [44, 45]. Total testosterone TT, testosterone BT, dehydroepiandrosterone, and estradiol increase the risk of different subtypes of BCs [46]. Obesity is one of the main risk factors causes especially an increased incidence of ER + , low-grade breast cancer [47, 48]. Obesity-induced inflammation plays a role in the development and progression of breast cancer, and plasma levels of measured inflammatory biomarkers are positively associated with breast cancer risk in postmenopausal women, but the association between measured inflammatory biomarkers and breast cancer risk did not vary by breast cancer subtype [49], and serum uric acid plays an important mediating role in the obesity-breast cancer relationship [50, 51]. MHT use was associated with a lower risk of breast cancer mortality following surgical menopause before 45 years, at 45–49 years or at ≥ 50 years, and the association between MHT use and the risk of breast cancer mortality did not differ by MHT use duration (< 6 or 6–20 years). MHT use was also associated with a lower risk of breast cancer mortality following natural menopause before 45 years or hysterectomy before 45 years [52]. MHT use was associated with an increased risk of breast cancer (odds ratio [OR] 1.12, 95% CI 1.09–1.15). And, this risk appears predominantly mediated through formulations containing synthetic progestins. micronized progesterone may be the safer progestogen to be used [53,54,55]. Nearly half of the effect of MHT on the risk of hormone receptor-positive BC is mediated by breast density. Indicate that we should use MHT with caution for women [56, 57]. cCNE2 may be a candidate gene for estrogen-progestin-induced breast cancer. But strong evidence is still lacking to support for common genetic variants altering the effect of MHT on breast cancer risk in estrogen-progestin MHT combinations or in estrogen receptor (ER) positive cases [58, 59]. The gut microbiota can influence breast carcinogenesis, but it remains to be investigated whether there are differences in the abundance, diversity, and composition of the gut microbiota between postmenopausal breast cancer patients and controls [60, 61].Lack of physical activity, high postmenopausal body mass index, alcohol consumption, and use of menopausal hormone therapy are known risk factors for breast cancer [62,63,64]. There was a definite association between modifiable lifestyle factors and 10-year all-cause mortality. The strongest association was found between BMI ≥ 30 kg/m2 and all-cause mortality compared with BMI 18.5 ~ 25 kg/m2 [HR (95% confidence interval, 1.19,1.06 ~ 1.34)]. There was no evidence of associations between modifiable risk factors and 10-year mortality differed by subtype [65, 66].
Osteoporosis
Osteoporosis is recognized as the most common complication of menopause, which closely related to fracture and osteodynia [67]. A new discovery showed that hearing and body balance at baseline exceeded initial BMD in predicting incident fractures in menopausal women with osteoporosis regardless of treatment during 25-year follow-up [68, 69]. Genome-wide association studies (GWAS) identified 12 loci that were significantly associated with BMD at any site in Chinese population, and rs1239055408 G > GA (KCNJ2) was associated with BMD only in women [70]. And, High-fat diet-induced obesity augments the deleterious effects of estrogen deficiency on bone, which resulting in accelerated cellular senescence, expansion of BMAT and impaired bone formation leading to decreased bone mass [71]. Longer leukocyte telomere length (LTL) was weakly associated with reduced risk of any incident fracture in women, however with less evidence in men [72]. Additionally, with a higher bone loss rate in surgically induced menopausal women compared with a natural process, MHT could significantly suppress the high bone remodeling [73]. In a Women's Health Initiative (WHI) hormone therapy trials including 25,389 postmenopausal women aged 50–79 years, MHT reduced the risk of fracture regardless of baseline FRAX fracture probability and falls history [74]. The MHT scheme of percutaneous estradiol gel (1.5 mg/day) plus oral micronized progesterone (100 mg/day) for 4 years has a low probability in fracture recurrence and mortality [75]. Erxian Decoction (EXD), as a commonly used alternative therapy of traditional Chinese medicine, is exerted therapeutic effects for OP through multiple functional signal pathways [76]. Phytoestrogens represented by the nanoparticles of betulinic acid (BA/NPs), as an naturally occurring PPAR-γ inhibitor, has great potential to improve osteoporosis in the in vivo and in vitro model [77,78,79].
Cognitive impairment
E2 is important for regulating hippocampal learning and memory. With the increase of subjective cognitive dysfunction and elevated rates of depression in this period, premature estrogen decline can lead to mild cognitive impairment (MCI), even Alzheimer's disease (AD), dementia with Lewy bodies (DLB) and vascular dementia (VaD) [80, 81]. However, as continued interest and debate, whether the MHT cure or prevent cognitive impairment or not. Recent research shows that MHT to improve cognitive functioning has only a few scenarios where it would be recommended and that particular caution may be warranted for carriers of the APOE ε4 allele [82]. Additionally, women at genetic risk for AD (APOE e4 allele carriers) have particularly shown favorable results from MHT treatment [83]. A meta-analysis including 10 RCTs with 2,818 participants showed that current available evidence does not support MHT had no effect on verbal memory in postmenopausal women, and also may impair some domains of short-term memory [84]. Further research findings that it has shown a slightly increased risk of developing AD among long term users of oestrogen-progestogen therapies, rather than taking oestrogen-only therapy [85]. A new perspective study of Functional cerebral asymmetry (FCA) discovered that right hemisphere is mainly affected by aging, and hormonal modulation improves the interplay between the two hemispheres and reduces FCA [86]. And also, a PET Study showed post-menopausal women showed significantly higher tau-PET signal in parieto-occipital regions, but were not moderated by Aβ burden or APOEε4 [87]. Additionally, following lower side effects compared with MHT, phytoestrogens as neuroprotective agents or epigenetic modifiers recover and maintain cognitive functions [88, 89]. But, very little is known regarding the regulation of synaptic plasticity genes, and also the precise regulation mechanism needs to be further explored. Moreover, postmenopausal status and a family history of dementia were more frequent among women who had had COVID-19 [90].
Glucolipid metabolism disorder
Changes in hormone levels lead to abnormalities in lipid metabolism with elevated serum total cholesterol, LDL cholesterol, apolipoproteins, and triglycerides, and decreased high-density lipoprotein cholesterol (HDL-C) [91]. Reduced energy expenditure due to reduced lipid oxidation and reduced leptin sensitivity in menopausal women [92]. Postmenopausal women have a lower gut microbiome diversity, slightly similar to that of men, and are involved in sex hormone retention. One study found that the gut microbe Bacteroides fragilis contributes to obesity in perimenopausal women by suppressing acetic acid levels [93, 94]. In addition, overweight or obese women have more severe and moderate menopausal symptoms [95]. Central adipose tissue accumulation, production of cytokines, and other factors contribute to an increased risk of developing T2DM by causing low-grade systemic inflammation and insulin resistance [96]. The earlier the age of menopause, the higher the risk of developing type 2 diabetes mellitus in women. Autoimmune destruction of follicles, insulin deficiency, and exogenous hyperinsulinemia in diabetic patients disrupt the normal function of the female reproductive system. Making women with diabetes experience menopause earlier [97, 98]. Early hormone therapy in menopausal women improves BMI and lipid levels in women.
Conclusion
Using bibliometrics, we conducted an analysis to identify the inadequacies, traditional focal points, and potential prospects in the study of MPS across current scientific areas. Treatment and complications are at the core of MPS research, whereas prediction and biomarkers have less literature of high quality. There is a necessity for innovative analytical metrics to measure the real effect of these papers with a high level of citation on clinical application.
Availability of data and materials
The datasets used or analysed during the current study are available from the corresponding author on reasonable request.
Change history
21 June 2024
A Correction to this paper has been published: https://doi.org/10.1186/s12978-024-01807-z
References
National Bureau of Statistics. Final Statistical Monitoring Report of the China Women’s Development Program (2011–2020). China Information News.
Paschou SA, Anagnostis P, Pavlou DI, Vryonidou A, Goulis DG, Lambrinoudaki I. Diabetes in menopause: risks and management. Curr Vasc Pharmacol. 2019;17(6):556–63. https://doi.org/10.2174/1570161116666180625124405.
Ren Y, Zhang M, Liu Y, et al. Association of menopause and type 2 diabetes mellitus. Menopause. 2019;26(3):325–30. https://doi.org/10.1097/GME.0000000000001200.
Dmytriw AA, Hui N, Singh T, et al. Bibliometric evaluation of systematic review and meta analyses published in the top 5 “high-impact” radiology journals. Clin Imaging. 2021;71:52–62. https://doi.org/10.1016/j.clinimag.2020.11.008.
Azer SA, Azer S. Top-cited articles in medical professionalism: a bibliometric analysis versus altmetric scores. BMJ Open. 2019;9(7): e029433. https://doi.org/10.1136/bmjopen-2019-029433.
Liu C, Yuan Q, Mao Z, et al. The top 100 most cited articles on rhabdomyolysis: a bibliometric analysis. Am J Emerg Med. 2020;38(9):1754–9. https://doi.org/10.1016/j.ajem.2020.05.031.
Portman DJ, Gass MLS. Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21(10):1063–8. https://doi.org/10.1097/GME.0000000000000329.
Santoro N, Komi J. Prevalence and impact of vaginal symptoms among postmenopausal women. J Sex Med. 2009;6(8):2133–42. https://doi.org/10.1111/j.1743-6109.2009.01335.x.
Faubion SS, Sood R, Kapoor E. Genitourinary syndrome of menopause: management strategies for the clinician. Mayo Clin Proc. 2017;92(12):1842–9. https://doi.org/10.1016/j.mayocp.2017.08.019.
Alvisi S, Gava G, Orsili I, et al. Vaginal health in menopausal women. Medicina (Kaunas). 2019;55(10):615. https://doi.org/10.3390/medicina55100615.
Kingsberg SA, Krychman M, Graham S, Bernick B, Mirkin S. The women’s EMPOWER survey: identifying women’s perceptions on vulvar and vaginal atrophy and its treatment. J Sex Med. 2017;14(3):413–24. https://doi.org/10.1016/j.jsxm.2017.01.010.
Palma F, Volpe A, Villa P, Cagnacci A. Writing group of AGATA study. Vaginal atrophy of women in postmenopause. Results from a multicentric observational study: The AGATA study. Maturitas. 2016;83:40–4. https://doi.org/10.1016/j.maturitas.2015.09.001.
Kingsberg SA, Wysocki S, Magnus L, Krychman ML. Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal Women’s VIews of Treatment Options for Menopausal Vaginal ChangEs) survey. J Sex Med. 2013;10(7):1790–9. https://doi.org/10.1111/jsm.12190.
Salvatore S, Nappi RE, Parma M, et al. Sexual function after fractional microablative CO2 laser in women with vulvovaginal atrophy. Climacteric. 2015;18(2):219–25. https://doi.org/10.3109/13697137.2014.975197.
Salvatore S, Nappi RE, Zerbinati N, et al. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric. 2014;17(4):363–9. https://doi.org/10.3109/13697137.2014.899347.
Salvatore S, Leone Roberti Maggiore U, Athanasiou S, et al. Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause. 2015;22(8):845–9. https://doi.org/10.1097/GME.0000000000000401.
Gambacciani M, Levancini M, Cervigni M. Vaginal erbium laser: the second-generation thermotherapy for the genitourinary syndrome of menopause. Climacteric. 2015;18(5):757–63. https://doi.org/10.3109/13697137.2015.1045485.
Gaspar A, Brandi H, Gomez V, Luque D. Efficacy of Erbium:YAG laser treatment compared to topical estriol treatment for symptoms of genitourinary syndrome of menopause. Lasers Surg Med. 2017;49(2):160–8. https://doi.org/10.1002/lsm.22569.
Schierbeck LL, Rejnmark L, Tofteng CL, et al. Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women: randomised trial. BMJ. 2012;345: e6409. https://doi.org/10.1136/bmj.e6409.
Ren M, Ruan X, Gu L, Pexman-Fieth C, Kahler E, Yu Q. Ultra-low-dose estradiol and dydrogesterone: a phase III study for vasomotor symptoms in China. Climacteric. 2022;25(3):286–92. https://doi.org/10.1080/13697137.2021.1956894.
Xu Z, Chung HF, Dobson AJ, Wilson LF, Hickey M, Mishra GD. Menopause, hysterectomy, menopausal hormone therapy and cause-specific mortality: cohort study of UK Biobank participants. Hum Reprod. 2022;37(9):2175–85. https://doi.org/10.1093/humrep/deac137.
Yu Q, Chae HD, Hsiao SM, et al. Prevalence, severity, and associated factors in women in East Asia with moderate-to-severe vasomotor symptoms associated with menopause. Menopause. 2022;29(5):553–63. https://doi.org/10.1097/GME.0000000000001949.
Blanken A, Gibson CJ, Li Y, et al. Racial/ethnic disparities in the diagnosis and management of menopause symptoms among midlife women veterans. Menopause. 2022;29(7):877–82. https://doi.org/10.1097/GME.0000000000001978.
Pershad A, Morris JM, Pace D, Khanna P. Racial disparities in menopausal hormone therapy acceptance: a pilot study. Menopause. 2022;29(11):1263–8. https://doi.org/10.1097/GME.0000000000002061.
Heinig M, Braitmaier M, Haug U. Prescribing of menopausal hormone therapy in Germany: current status and changes between 2004 and 2016. Pharmacoepidemiol Drug Saf. 2021;30(4):462–71. https://doi.org/10.1002/pds.5186.
Park CY, Lim JY, Kim WH, Kim SY, Park HY. Evaluation of menopausal hormone therapy use in Korea (2002–2013): a nationwide cohort study. Maturitas. 2021;146:57–62. https://doi.org/10.1016/j.maturitas.2021.02.003.
Ott J, Egarter C, Aguilera A. Dydrogesterone after 60 years: a glance at the safety profile. Gynecol Endocrinol. 2022;38(4):279–87. https://doi.org/10.1080/09513590.2021.2016692.
Chlebowski RT, Anderson GL. Menopausal hormone therapy and cancer: changing clinical observations of target site specificity. Steroids. 2014;90:53–9. https://doi.org/10.1016/j.steroids.2014.06.001.
Prentice RL, Aragaki AK, Chlebowski RT, et al. Randomized trial evaluation of the benefits and risks of menopausal hormone therapy among women 50–59 years of age. Am J Epidemiol. 2021;190(3):365–75. https://doi.org/10.1093/aje/kwaa210.
Graham S, Archer DF, Simon JA, Ohleth KM, Bernick B. Review of menopausal hormone therapy with estradiol and progesterone versus other estrogens and progestins. Gynecol Endocrinol. 2022;38(11):891–910. https://doi.org/10.1080/09513590.2022.2118254.
Liu JH. The role of progestogens in menopausal hormone therapy. Clin Obstet Gynecol. 2021;64(4):772–83. https://doi.org/10.1097/GRF.0000000000000657.
Perkins MS, Louw-du Toit R, Jackson H, Simons M, Africander D. Upregulation of an estrogen receptor-regulated gene by first generation progestins requires both the progesterone receptor and estrogen receptor alpha. Front Endocrinol (Lausanne). 2022;13: 959396. https://doi.org/10.3389/fendo.2022.959396.
Nappi RE, Simoncini T. Menopause transition: a golden age to prevent cardiovascular disease. Lancet Diabetes Endocrinol. 2021;9(3):135–7. https://doi.org/10.1016/S2213-8587(21)00018-8.
Aryan L, Younessi D, Zargari M, et al. The role of estrogen receptors in cardiovascular disease. Int J Mol Sci. 2020;21(12):4314. https://doi.org/10.3390/ijms21124314.
Sharad P, Agarwal N, Chopra S, et al. Assessment of endothelial dysfunction by brachial artery flow-mediated dilatation in postmenopausal women at low risk for cardiovascular disease. J Midlife Health. 2021;12(3):193–8. https://doi.org/10.4103/jmh.jmh_111_21.
Armeni E, Lambrinoudaki I. Menopause, androgens, and cardiovascular ageing: a narrative review. Ther Adv Endocrinol Metab. 2022;13:20420188221129944. https://doi.org/10.1177/20420188221129946.
Hashemzadeh M, Romo R, Arreguin JM, Movahed MR. The effects of estrogen and hormone replacement therapy on cardiovascular systems. Future Cardiol. 2021;17(2):347–53. https://doi.org/10.2217/fca-2020-0054.
Moreau KL, Babcock MC, Hildreth KL. Sex differences in vascular aging in response to testosterone. Biol Sex Differ. 2020;11(1):18. https://doi.org/10.1186/s13293-020-00294-8.
Dela Justina V, Miguez JSG, Priviero F, Sullivan JC, Giachini FR, Webb RC. Sex differences in molecular mechanisms of cardiovascular aging. Front Aging. 2021;2: 725884. https://doi.org/10.3389/fragi.2021.725884.
Lundberg G, Wu P, Wenger N. Menopausal hormone therapy: a comprehensive review. Curr Atheroscler Rep. 2020;22(8):33. https://doi.org/10.1007/s11883-020-00854-8.
Karim R, Xu W, Kono N, et al. Effect of menopausal hormone therapy on arterial wall echomorphology: Results from the Early versus Late Intervention Trial with Estradiol (ELITE). Maturitas. 2022;162:15–22. https://doi.org/10.1016/j.maturitas.2022.02.007.
Anagnostis P, Lambrinoudaki I, Stevenson JC, Goulis DG. Menopause-associated risk of cardiovascular disease. Endocr Connect. 2022;11(4): e210537. https://doi.org/10.1530/EC-21-0537.
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Jiang C, Wu P, He X, et al. Associations between serum reproductive hormone concentrations and hormonal receptor status among postmenopausal chinese women with breast cancer: an observational study. Front Oncol. 2022;12: 819756. https://doi.org/10.3389/fonc.2022.819756.
Santen RJ, Stuenkel CA, Yue W. Mechanistic effects of estrogens on breast cancer. Cancer J. 2022;28(3):224–40. https://doi.org/10.1097/PPO.0000000000000596.
Nounu A, Kar SP, Relton CL, Richmond RC. Sex steroid hormones and risk of breast cancer: a two-sample Mendelian randomization study. Breast Cancer Res. 2022;24(1):66. https://doi.org/10.1186/s13058-022-01553-9.
Klintman M, Rosendahl AH, Randeris B, et al. Postmenopausal overweight and breast cancer risk; results from the KARMA cohort. Breast Cancer Res Treat. 2022;196(1):185–96. https://doi.org/10.1007/s10549-022-06664-7.
Body mass index, breast density, and the risk of breast cancer development in relation to the menopausal status; results from a population-based screening program in a native African-Arab country - PubMed. https://pubmed.ncbi.nlm.nih.gov/35795247/. Accessed 23 oct 2022.
Cairat M, Rinaldi S, Navionis AS, et al. Circulating inflammatory biomarkers, adipokines and breast cancer risk-a case-control study nested within the EPIC cohort. BMC Med. 2022;20(1):118. https://doi.org/10.1186/s12916-022-02319-y.
Feng Y, Fu M, Guan X, et al. Uric acid mediated the association between bmi and postmenopausal breast cancer incidence: a bidirectional mendelian randomization analysis and prospective cohort study. Front Endocrinol (Lausanne). 2021;12: 742411. https://doi.org/10.3389/fendo.2021.742411.
Cold S, Cold F, Jensen MB, Cronin-Fenton D, Christiansen P, Ejlertsen B. Systemic or vaginal hormone therapy after early breast cancer: a Danish observational cohort study. J Natl Cancer Inst. 2022;114(10):1347–54. https://doi.org/10.1093/jnci/djac112.
Messier TL, Boyd JR, Gordon JAR, et al. Epigenetic and transcriptome responsiveness to ER modulation by tissue selective estrogen complexes in breast epithelial and breast cancer cells. PLoS ONE. 2022;17(7): e0271725. https://doi.org/10.1371/journal.pone.0271725.
Stevenson JC, Farmer RDT. HRT and breast cancer: a million women ride again. Climacteric. 2020;23(3):226–8. https://doi.org/10.1080/13697137.2020.1735797.
Abenhaim HA, Suissa S, Azoulay L, Spence AR, Czuzoj-Shulman N, Tulandi T. Menopausal hormone therapy formulation and breast cancer risk. Obstet Gynecol. 2022;139(6):1103–10. https://doi.org/10.1097/AOG.0000000000004723.
Lambrinoudaki I. Menopausal hormone therapy and breast cancer risk: all progestogens are not the same. Case Rep Womens Health. 2021;29: e00270. https://doi.org/10.1016/j.crwh.2020.e00270.
Fornili M, Perduca V, Fournier A, et al. Association between menopausal hormone therapy, mammographic density and breast cancer risk: results from the E3N cohort study. Breast Cancer Res. 2021;23(1):47. https://doi.org/10.1186/s13058-021-01425-8.
Lester SP, Vegunta S. Influence of menopausal hormone therapy on the breast: counseling your patients before you prescribe. J Womens Health (Larchmt). 2022;31(2):167–70. https://doi.org/10.1089/jwh.2021.0322.
Deng Y, Huang H, Shi J, Jin H. Identification of candidate genes in breast cancer induced by estrogen plus progestogens using bioinformatic analysis. Int J Mol Sci. 2022;23(19):11892. https://doi.org/10.3390/ijms231911892.
Wang X, Kapoor PM, Auer PL, et al. Genome-wide interaction analysis of menopausal hormone therapy use and breast cancer risk among 62,370 women. Sci Rep. 2022;12(1):6199. https://doi.org/10.1038/s41598-022-10121-2.
Metagenomic Analyses Reveal Distinct Gut Microbiota Signature for Predicting the Neoadjuvant Chemotherapy Responsiveness in Breast Cancer Patients - PubMed. https://pubmed.ncbi.nlm.nih.gov/35433455/. Accessed 23 Oct 2022.
Aarnoutse R, Hillege LE, Ziemons J, et al. Intestinal microbiota in postmenopausal breast cancer patients and controls. Cancers (Basel). 2021;13(24):6200. https://doi.org/10.3390/cancers13246200.
Syal A, Aggarwal N. Postmenopausal hormone therapy and its association with breast cancer. J Midlife Health. 2020;11(4):187–95. https://doi.org/10.4103/jmh.jmh_284_20.
Wang T, Bradshaw PT, Moorman PG, et al. Menopausal hormone therapy use and long-term all-cause and cause-specific mortality in the Long Island Breast Cancer Study Project. Int J Cancer. 2020;147(12):3404–15. https://doi.org/10.1002/ijc.33174.
Chlebowski RT, Manson JE. Menopausal hormone therapy and breast Cancer. Cancer J. 2022;28(3):169–75. https://doi.org/10.1097/PPO.0000000000000601.
Lilleborge M, Falk RS, Sørlie T, Ursin G, Hofvind S. Can breast cancer be stopped? Modifiable risk factors of breast cancer among women with a prior benign or premalignant lesion. Int J Cancer. 2021;149(6):1247–56. https://doi.org/10.1002/ijc.33680.
Morra A, Jung AY, Behrens S, et al. Breast cancer risk factors and survival by tumor subtype: pooled analyses from the breast cancer association consortium. Cancer Epidemiol Biomarkers Prev. 2021;30(4):623–42. https://doi.org/10.1158/1055-9965.EPI-20-0924.
Moberg L, Hamrefors V, Fedorowski A, Rogmark C. Early menopause and weight loss are significant factors associated with risk of future fracture in middle-aged women. BMC Musculoskelet Disord. 2022;23(1):779. https://doi.org/10.1186/s12891-022-05744-5.
Cherukuri L, Kinninger A, Birudaraju D, et al. Coronary artery calcium and bone mineral density by serial CTA: does menopausal hormone therapy modify the association? Clin Imaging. 2022;90:26–31. https://doi.org/10.1016/j.clinimag.2022.06.023.
Dotevall A, Krantz E, Barrenäs ML, Landin-Wilhelmsen K. Hearing and balance exceed initial bone mineral density in predicting incident fractures: a 25-year prospective observational study in menopausal women with osteoporosis. JBMR Plus. 2022;6(1): e10551. https://doi.org/10.1002/jbm4.10551.
Zeng H, Ge J, Xu W, et al. Twelve Loci associated with bone density in middle-aged and elderly Chinese: the Shanghai Changfeng study. J Clin Endocrinol Metab. 2023;108(2):295–305. https://doi.org/10.1210/clinem/dgac597.
Ali D, Figeac F, Caci A, et al. High-fat diet-induced obesity augments the deleterious effects of estrogen deficiency on bone: evidence from ovariectomized mice. Aging Cell. 2022;21(12): e13726. https://doi.org/10.1111/acel.13726.
Curtis EM, Codd V, Nelson C, et al. Telomere length and risk of incident fracture and arthroplasty: findings from UK biobank. J Bone Miner Res. 2022;37(10):1997–2004. https://doi.org/10.1002/jbmr.4664.
Vatrasresth J, Suwan A, Panyakhamlerd K. Effects of early estradiol valerate administration on bone turnover markers in surgically induced menopausal women. BMC Womens Health. 2021;21(1):363. https://doi.org/10.1186/s12905-021-01508-w.
Lorentzon M, Johansson H, Harvey NC, et al. Menopausal hormone therapy reduces the risk of fracture regardless of falls risk or baseline FRAX probability-results from the Women’s Health Initiative hormone therapy trials. Osteoporos Int. 2022;33(11):2297–305. https://doi.org/10.1007/s00198-022-06483-y.
Park CW, Lim SJ, Moon YW, et al. Fracture recurrence in hip fracture with menopausal hormone therapy versus risedronate: a clinical trial. Climacteric. 2021;24(4):408–14. https://doi.org/10.1080/13697137.2021.1915271.
Yang L, Fan L, Wang K, et al. Analysis of molecular mechanism of erxian decoction in treating osteoporosis based on formula optimization model. Oxid Med Cell Longev. 2021;2021:6641838. https://doi.org/10.1155/2021/6641838.
Park DR, Yeo CH, Yoon JE, et al. Polygonatum sibiricum improves menopause symptoms by regulating hormone receptor balance in an ovariectomized mouse model. Biomed Pharmacother. 2022;153: 113385. https://doi.org/10.1016/j.biopha.2022.113385.
Pingali U, Nutalapati C. Shilajit extract reduces oxidative stress, inflammation, and bone loss to dose-dependently preserve bone mineral density in postmenopausal women with osteopenia: a randomized, double-blind, placebo-controlled trial. Phytomedicine. 2022;105: 154334. https://doi.org/10.1016/j.phymed.2022.154334.
Sardar A, Gautam S, Sinha S, et al. Nanoparticles of naturally occurring PPAR-γ inhibitor betulinic acid ameliorates bone marrow adiposity and pathological bone loss in ovariectomized rats via Wnt/β-catenin pathway. Life Sci. 2022;309: 121020. https://doi.org/10.1016/j.lfs.2022.121020.
Maki PM, Jaff NG. Brain fog in menopause: a health-care professional’s guide for decision-making and counseling on cognition. Climacteric. 2022;25(6):570–8. https://doi.org/10.1080/13697137.2022.2122792.
Xi H, Gan J, Liu S, et al. Reproductive factors and cognitive impairment in natural menopausal women: a cross-sectional study. Front Endocrinol (Lausanne). 2022;13: 893901. https://doi.org/10.3389/fendo.2022.893901.
Koire A, Joffe H, Buckley R. Menopausal hormone therapy and the mind: the role of hormone replacement in the prevention and treatment of cognitive decline, dementia, and cognitive dysfunction of depression. Harv Rev Psychiatry. 2022;30(4):215–25. https://doi.org/10.1097/HRP.0000000000000339.
Depypere H, Vergallo A, Lemercier P, et al. Menopause hormone therapy significantly alters pathophysiological biomarkers of Alzheimer’s disease. Alzheimers Dement. 2022. https://doi.org/10.1002/alz.12759
Chen L, Zheng W, Chen G, Liu LH, Yao J, Chen Y. Menopausal hormone therapy does not improve some domains of memory: a systematic review and meta-analysis. Front Endocrinol (Lausanne). 2022;13: 894883. https://doi.org/10.3389/fendo.2022.894883.
Vinogradova Y, Dening T, Hippisley-Cox J, Taylor L, Moore M, Coupland C. Use of menopausal hormone therapy and risk of dementia: nested case-control studies using QResearch and CPRD databases. BMJ. 2021;374: n2182. https://doi.org/10.1136/bmj.n2182.
Digesu GA, Riemma G, Torella M, et al. Functional brain asymmetry and menopausal treatments: is there a link? Medicina (Kaunas). 2022;58(5):616. https://doi.org/10.3390/medicina58050616.
Buckley RF, O’Donnell A, McGrath ER, et al. Menopause status moderates sex differences in tau burden: a framingham PET study. Ann Neurol. 2022;92(1):11–22. https://doi.org/10.1002/ana.26382.
Daodee S, Monthakantirat O, Tantipongpiradet A, et al. Effect of Yakae-Prajamduen-Jamod traditional Thai remedy on cognitive impairment in an ovariectomized mouse model and its mechanism of action. Molecules. 2022;27(13):4310. https://doi.org/10.3390/molecules27134310.
Singh P, Paramanik V. Neuromodulating roles of estrogen and phytoestrogens in cognitive therapeutics through epigenetic modifications during aging. Front Aging Neurosci. 2022;14: 945076. https://doi.org/10.3389/fnagi.2022.945076.
Vallejo MS, Blümel JE, Bencosme A, et al. Factors affecting climacteric women with SARS-CoV-2 infection: a multinational Latin America study (REDLINC XI). Maturitas. 2022;165:33–7. https://doi.org/10.1016/j.maturitas.2022.07.006.
Torosyan N, Visrodia P, Torbati T, Minissian MB, Shufelt CL. Dyslipidemia in midlife women: Approach and considerations during the menopausal transition. Maturitas. 2022;166:14–20. https://doi.org/10.1016/j.maturitas.2022.08.001.
Harraqui K, Oudghiri DE, Hannoun Z, et al. Frequency of metabolic syndrome and study of anthropometric, clinical and biological characteristics in peri- and postmenopausal women in the city of Ksar El Kebir (Northern Morocco). Int J Environ Res Public Health. 2022;19(10):6109. https://doi.org/10.3390/ijerph19106109.
Shen WD, Lin X, Liu HM, et al. Gut microbiota accelerates obesity in peri-/post-menopausal women via Bacteroides fragilis and acetic acid. Int J Obes (Lond). 2022;46(10):1918–24. https://doi.org/10.1038/s41366-022-01137-9.
Peters BA, Lin J, Qi Q, et al. Menopause is associated with an altered gut microbiome and estrobolome, with implications for adverse cardiometabolic risk in the hispanic community health study/study of latinos. mSystems. 2022;7(3):e0027322. https://doi.org/10.1128/msystems.00273-22.
Costa JG, Rodrigues RM, Puga GM, Cheik NC. Does obesity aggravate climacteric symptoms in postmenopausal women? Rev Bras Ginecol Obstet. 2022;44(6):586–92. https://doi.org/10.1055/s-0042-1745789.
Polyzos SA, Lambrinoudaki I, Goulis DG. Menopausal hormone therapy in women with dyslipidemia and nonalcoholic fatty liver disease. Hormones (Athens). 2022;21(3):375–81. https://doi.org/10.1007/s42000-022-00369-8.
Lambrinoudaki I, Paschou SA, Armeni E, Goulis DG. The interplay between diabetes mellitus and menopause: clinical implications. Nat Rev Endocrinol. 2022. https://doi.org/10.1038/s41574-022-00708-0.
Yi Y, El Khoudary SR, Buchanich JM, et al. Association of age at diabetes complication diagnosis with age at natural menopause in women with type 1 diabetes: The Pittsburgh Epidemiology of Diabetes Complications (EDC) Study. J Diabetes Complications. 2021;35(3): 107832. https://doi.org/10.1016/j.jdiacomp.2020.107832.
Hodis HN, Mack WJ, Henderson VW, et al. Vascular Effects of Early versus Late Postmenopausal Treatment with Estradiol. N Engl J Med. 2016;374(13):1221–31. https://doi.org/10.1056/NEJMoa1505241.
Moore HCF, Unger JM, Phillips KA, et al. Goserelin for ovarian protection during breast-cancer adjuvant chemotherapy. N Engl J Med. 2015;372(10):923–32. https://doi.org/10.1056/NEJMoa1413204.
Nappi RE, Kokot-Kierepa M. Vaginal health: insights, views & attitudes (VIVA)—results from an international survey. Climacteric. 2012;15(1):36–44. https://doi.org/10.3109/13697137.2011.647840.
Harman SM, Black DM, Naftolin F, et al. Arterial imaging outcomes and cardiovascular risk factors in recently menopausal women: a randomized trial. Ann Intern Med. 2014;161(4):249–60. https://doi.org/10.7326/M14-0353.
Day FR, Ruth KS, Thompson DJ, et al. Large-scale genomic analyses link reproductive aging to hypothalamic signaling, breast cancer susceptibility and BRCA1-mediated DNA repair. Nat Genet. 2015;47(11):1294–303. https://doi.org/10.1038/ng.3412.
Zhu L, Brown WC, Cai Q, et al. Estrogen treatment after ovariectomy protects against fatty liver and may improve pathway-selective insulin resistance. Diabetes. 2013;62(2):424–34. https://doi.org/10.2337/db11-1718.
Gold EB, Crawford SL, Avis NE, et al. Factors related to age at natural menopause: longitudinal analyses from SWAN. Am J Epidemiol. 2013;178(1):70–83. https://doi.org/10.1093/aje/kws421.
Bove R, Secor E, Chibnik LB, et al. Age at surgical menopause influences cognitive decline and Alzheimer pathology in older women. Neurology. 2014;82(3):222–9. https://doi.org/10.1212/WNL.0000000000000033.
Freeman EW, Sammel MD, Lin H, Gracia CR. Anti-mullerian hormone as a predictor of time to menopause in late reproductive age women. J Clin Endocrinol Metab. 2012;97(5):1673–80. https://doi.org/10.1210/jc.2011-3032.
Liu P, Ji Y, Yuen T, et al. Blocking FSH induces thermogenic adipose tissue and reduces body fat. Nature. 2017;546(7656):107–12. https://doi.org/10.1038/nature22342.
Shao H, Breitner JCS, Whitmer RA, et al. Hormone therapy and Alzheimer disease dementia: new findings from the Cache County Study. Neurology. 2012;79(18):1846–52. https://doi.org/10.1212/WNL.0b013e318271f823.
Wellons M, Ouyang P, Schreiner PJ, Herrington DM, Vaidya D. Early menopause predicts future coronary heart disease and stroke: the Multi-Ethnic Study of Atherosclerosis. Menopause. 2012;19(10):1081–7. https://doi.org/10.1097/gme.0b013e3182517bd0.
Schoemaker MJ, Nichols HB, Premenopausal Breast Cancer Collaborative Group, et al. Association of body mass index and age with subsequent breast cancer risk in premenopausal women. JAMA Oncol. 2018;4(11):e181771. https://doi.org/10.1001/jamaoncol.2018.1771.
Lee JE, Lee S, Lee H, et al. Association of the vaginal microbiota with human papillomavirus infection in a Korean twin cohort. PLoS ONE. 2013;8(5): e63514. https://doi.org/10.1371/journal.pone.0063514.
Kerr JB, Hutt KJ, Michalak EM, et al. DNA damage-induced primordial follicle oocyte apoptosis and loss of fertility require TAp63-mediated induction of Puma and Noxa. Mol Cell. 2012;48(3):343–52. https://doi.org/10.1016/j.molcel.2012.08.017.
Dólleman M, Faddy MJ, van Disseldorp J, et al. The relationship between anti-Müllerian hormone in women receiving fertility assessments and age at menopause in subfertile women: evidence from large population studies. J Clin Endocrinol Metab. 2013;98(5):1946–53. https://doi.org/10.1210/jc.2013-3105.
Dólleman M, Verschuren WMM, Eijkemans MJC, et al. Reproductive and lifestyle determinants of anti-Müllerian hormone in a large population-based study. J Clin Endocrinol Metab. 2013;98(5):2106–15. https://doi.org/10.1210/jc.2012-3995.
Moreau KL, Hildreth KL, Meditz AL, Deane KD, Kohrt WM. Endothelial function is impaired across the stages of the menopause transition in healthy women. J Clin Endocrinol Metab. 2012;97(12):4692–700. https://doi.org/10.1210/jc.2012-2244.
Wang S, Zheng Y, Li J, et al. Single-cell transcriptomic atlas of primate ovarian aging. Cell. 2020;180(3):585-600.e19. https://doi.org/10.1016/j.cell.2020.01.009.
Shimbo D, Newman JD, Aragaki AK, et al. Association between annual visit-to-visit blood pressure variability and stroke in postmenopausal women: data from the Women’s Health Initiative. Hypertension. 2012;60(3):625–30. https://doi.org/10.1161/HYPERTENSIONAHA.112.193094.
Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30(1):429–36. https://doi.org/10.1007/s10103-014-1677-2.
Duijts SFA, van Beurden M, Oldenburg HSA, et al. Efficacy of cognitive behavioral therapy and physical exercise in alleviating treatment-induced menopausal symptoms in patients with breast cancer: results of a randomized, controlled, multicenter trial. J Clin Oncol. 2012;30(33):4124–33. https://doi.org/10.1200/JCO.2012.41.8525.
Lambertini M, Boni L, Michelotti A, et al. Ovarian suppression with triptorelin during adjuvant breast cancer chemotherapy and long-term ovarian function, pregnancies, and disease-free survival: a randomized clinical trial. JAMA. 2015;314(24):2632–40. https://doi.org/10.1001/jama.2015.17291.
Greendale GA, Sowers M, Han W, et al. Bone mineral density loss in relation to the final menstrual period in a multiethnic cohort: results from the Study of Women’s Health Across the Nation (SWAN). J Bone Miner Res. 2012;27(1):111–8. https://doi.org/10.1002/jbmr.534.
Abdulnour J, Doucet E, Brochu M, et al. The effect of the menopausal transition on body composition and cardiometabolic risk factors: a Montreal-Ottawa New Emerging Team group study. Menopause. 2012;19(7):760–7. https://doi.org/10.1097/gme.0b013e318240f6f3.
Hara Y, Yuk F, Puri R, Janssen WGM, Rapp PR, Morrison JH. Presynaptic mitochondrial morphology in monkey prefrontal cortex correlates with working memory and is improved with estrogen treatment. Proc Natl Acad Sci U S A. 2014;111(1):486–91. https://doi.org/10.1073/pnas.1311310110.
Villa A, Rizzi N, Vegeto E, Ciana P, Maggi A. Estrogen accelerates the resolution of inflammation in macrophagic cells. Sci Rep. 2015;5:15224. https://doi.org/10.1038/srep15224.
Bellanti F, Matteo M, Rollo T, et al. Sex hormones modulate circulating antioxidant enzymes: impact of estrogen therapy. Redox Biol. 2013;1(1):340–6. https://doi.org/10.1016/j.redox.2013.05.003.
Zhu D, Chung HF, Dobson AJ, et al. Age at natural menopause and risk of incident cardiovascular disease: a pooled analysis of individual patient data. Lancet Public Health. 2019;4(11):e553–64. https://doi.org/10.1016/S2468-2667(19)30155-0.
Cruz VL, Steiner ML, Pompei LM, et al. Randomized, double-blind, placebo-controlled clinical trial for evaluating the efficacy of fractional CO2 laser compared with topical estriol in the treatment of vaginal atrophy in postmenopausal women. Menopause. 2018;25(1):21–8. https://doi.org/10.1097/GME.0000000000000955.
Labrie F, Archer DF, Koltun W, et al. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–56. https://doi.org/10.1097/GME.0000000000000571.
Chlebowski RT, Manson JE, Anderson GL, et al. Estrogen plus progestin and breast cancer incidence and mortality in the Women’s Health Initiative Observational Study. J Natl Cancer Inst. 2013;105(8):526–35. https://doi.org/10.1093/jnci/djt043.
Camporez JPG, Jornayvaz FR, Lee HY, et al. Cellular mechanism by which estradiol protects female ovariectomized mice from high-fat diet-induced hepatic and muscle insulin resistance. Endocrinology. 2013;154(3):1021–8. https://doi.org/10.1210/en.2012-1989.
Sweetland S, Beral V, Balkwill A, et al. Venous thromboembolism risk in relation to use of different types of postmenopausal hormone therapy in a large prospective study. J Thromb Haemost. 2012;10(11):2277–86. https://doi.org/10.1111/j.1538-7836.2012.04919.x.
Jonklaas J, Nogueras-Gonzalez G, Munsell M, et al. The impact of age and gender on papillary thyroid cancer survival. J Clin Endocrinol Metab. 2012;97(6):E878-887. https://doi.org/10.1210/jc.2011-2864.
Freeman EW, Sammel MD, Boorman DW, Zhang R. Longitudinal pattern of depressive symptoms around natural menopause. JAMA Psychiat. 2014;71(1):36–43. https://doi.org/10.1001/jamapsychiatry.2013.2819.
Perino A, Calligaro A, Forlani F, et al. Vulvo-vaginal atrophy: a new treatment modality using thermo-ablative fractional CO2 laser. Maturitas. 2015;80(3):296–301. https://doi.org/10.1016/j.maturitas.2014.12.006.
Miyauchi Y, Sato Y, Kobayashi T, et al. HIF1α is required for osteoclast activation by estrogen deficiency in postmenopausal osteoporosis. Proc Natl Acad Sci U S A. 2013;110(41):16568–73. https://doi.org/10.1073/pnas.1308755110.
Freeman EW, Sammel MD, Sanders RJ. Risk of long-term hot flashes after natural menopause: evidence from the Penn Ovarian Aging Study cohort. Menopause. 2014;21(9):924–32. https://doi.org/10.1097/GME.0000000000000196.
Ottewell PD, Wang N, Brown HK, et al. Zoledronic acid has differential antitumor activity in the pre- and postmenopausal bone microenvironment in vivo. Clin Cancer Res. 2014;20(11):2922–32. https://doi.org/10.1158/1078-0432.CCR-13-1246.
Epperson CN, Sammel MD, Freeman EW. Menopause effects on verbal memory: findings from a longitudinal community cohort. J Clin Endocrinol Metab. 2013;98(9):3829–38. https://doi.org/10.1210/jc.2013-1808.
Ayers B, Smith M, Hellier J, Mann E, Hunter MS. Effectiveness of group and self-help cognitive behavior therapy in reducing problematic menopausal hot flushes and night sweats (MENOS 2): a randomized controlled trial. Menopause. 2012;19(7):749–59. https://doi.org/10.1097/gme.0b013e31823fe835.
Simon JA, Kokot-Kierepa M, Goldstein J, Nappi RE. Vaginal health in the United States: results from the Vaginal Health: insights, views & attitudes survey. Menopause. 2013;20(10):1043–8. https://doi.org/10.1097/GME.0b013e318287342d.
Meyer MR, Fredette NC, Howard TA, et al. G protein-coupled estrogen receptor protects from atherosclerosis. Sci Rep. 2014;4:7564. https://doi.org/10.1038/srep07564.
Henderson VW, St John JA, Hodis HN, et al. Cognitive effects of estradiol after menopause: a randomized trial of the timing hypothesis. Neurology. 2016;87(7):699–708. https://doi.org/10.1212/WNL.0000000000002980.
Joffe H, Guthrie KA, LaCroix AZ, et al. Low-dose estradiol and the serotonin-norepinephrine reuptake inhibitor venlafaxine for vasomotor symptoms: a randomized clinical trial. JAMA Intern Med. 2014;174(7):1058–66. https://doi.org/10.1001/jamainternmed.2014.1891.
Espeland MA, Shumaker SA, Leng I, et al. Long-term effects on cognitive function of postmenopausal hormone therapy prescribed to women aged 50 to 55 years. JAMA Intern Med. 2013;173(15):1429–36. https://doi.org/10.1001/jamainternmed.2013.7727.
Mosconi L, Berti V, Quinn C, et al. Sex differences in Alzheimer risk: brain imaging of endocrine vs chronologic aging. Neurology. 2017;89(13):1382–90. https://doi.org/10.1212/WNL.0000000000004425.
Crandall CJ, Hovey KM, Andrews CA, et al. Breast cancer, endometrial cancer, and cardiovascular events in participants who used vaginal estrogen in the Women’s Health Initiative Observational Study. Menopause. 2018;25(1):11–20. https://doi.org/10.1097/GME.0000000000000956.
Greendale GA, Sternfeld B, Huang M, et al. Changes in body composition and weight during the menopause transition. JCI Insight. 2019;4(5):e124865. https://doi.org/10.1172/jci.insight.124865.
Li L, Wu J, Pu D, et al. Factors associated with the age of natural menopause and menopausal symptoms in Chinese women. Maturitas. 2012;73(4):354–60. https://doi.org/10.1016/j.maturitas.2012.09.008.
Qiu C, Chen H, Wen J, et al. Associations between age at menarche and menopause with cardiovascular disease, diabetes, and osteoporosis in Chinese women. J Clin Endocrinol Metab. 2013;98(4):1612–21. https://doi.org/10.1210/jc.2012-2919.
Kamada Y, Kiso S, Yoshida Y, et al. Estrogen deficiency worsens steatohepatitis in mice fed high-fat and high-cholesterol diet. Am J Physiol Gastrointest Liver Physiol. 2011;301(6):G1031-1043. https://doi.org/10.1152/ajpgi.00211.2011.
Pinkerton JV, Harvey JA, Lindsay R, et al. Effects of bazedoxifene/conjugated estrogens on the endometrium and bone: a randomized trial. J Clin Endocrinol Metab. 2014;99(2):E189-198. https://doi.org/10.1210/jc.2013-1707.
Schmidt PJ, Ben Dor R, Martinez PE, et al. Effects of estradiol withdrawal on mood in women with past perimenopausal depression: a randomized clinical trial. JAMA Psychiat. 2015;72(7):714–26. https://doi.org/10.1001/jamapsychiatry.2015.0111.
Kotlarczyk MP, Lassila HC, O’Neil CK, et al. Melatonin osteoporosis prevention study (MOPS): a randomized, double-blind, placebo-controlled study examining the effects of melatonin on bone health and quality of life in perimenopausal women. J Pineal Res. 2012;52(4):414–26. https://doi.org/10.1111/j.1600-079X.2011.00956.x.
Turkoz FP, Solak M, Petekkaya I, et al. Association between common risk factors and molecular subtypes in breast cancer patients. Breast. 2013;22(3):344–50. https://doi.org/10.1016/j.breast.2012.08.005.
Yasui T, Hayashi K, Mizunuma H, et al. Factors associated with premature ovarian failure, early menopause and earlier onset of menopause in Japanese women. Maturitas. 2012;72(3):249–55. https://doi.org/10.1016/j.maturitas.2012.04.002.
Bromberger JT, Kravitz HM, Chang Y, et al. Does risk for anxiety increase during the menopausal transition? Study of women’s health across the nation. Menopause. 2013;20(5):488–95. https://doi.org/10.1097/GME.0b013e3182730599.
Zhu LL, Blair H, Cao J, et al. Blocking antibody to the β-subunit of FSH prevents bone loss by inhibiting bone resorption and stimulating bone synthesis. Proc Natl Acad Sci U S A. 2012;109(36):14574–9. https://doi.org/10.1073/pnas.1212806109.
Romagnoli E, Cipriani C, Nofroni I, et al. “Trabecular Bone Score” (TBS): an indirect measure of bone micro-architecture in postmenopausal patients with primary hyperparathyroidism. Bone. 2013;53(1):154–9. https://doi.org/10.1016/j.bone.2012.11.041.
Mishra GD, Pandeya N, Dobson AJ, et al. Early menarche, nulliparity and the risk for premature and early natural menopause. Hum Reprod. 2017;32(3):679–86. https://doi.org/10.1093/humrep/dew350.
de Vries L, Behar DM, Smirin-Yosef P, Lagovsky I, Tzur S, Basel-Vanagaite L. Exome sequencing reveals SYCE1 mutation associated with autosomal recessive primary ovarian insufficiency. J Clin Endocrinol Metab. 2014;99(10):E2129-2132. https://doi.org/10.1210/jc.2014-1268.
Knapen MHJ, Drummen NE, Smit E, Vermeer C, Theuwissen E. Three-year low-dose menaquinone-7 supplementation helps decrease bone loss in healthy postmenopausal women. Osteoporos Int. 2013;24(9):2499–507. https://doi.org/10.1007/s00198-013-2325-6.
Sokol ER, Karram MM. An assessment of the safety and efficacy of a fractional CO2 laser system for the treatment of vulvovaginal atrophy. Menopause. 2016;23(10):1102–7. https://doi.org/10.1097/GME.0000000000000700.
Nappi RE, Palacios S, Panay N, Particco M, Krychman ML. Vulvar and vaginal atrophy in four European countries: evidence from the European REVIVE Survey. Climacteric. 2016;19(2):188–97. https://doi.org/10.3109/13697137.2015.1107039.
Mittelman-Smith MA, Williams H, Krajewski-Hall SJ, McMullen NT, Rance NE. Role for kisspeptin/neurokinin B/dynorphin (KNDy) neurons in cutaneous vasodilatation and the estrogen modulation of body temperature. Proc Natl Acad Sci U S A. 2012;109(48):19846–51. https://doi.org/10.1073/pnas.1211517109.
Zhao D, Guallar E, Ouyang P, et al. Endogenous Sex Hormones and Incident Cardiovascular Disease in Post-Menopausal Women. J Am Coll Cardiol. 2018;71(22):2555–66. https://doi.org/10.1016/j.jacc.2018.01.083.
Tehrani FR, Solaymani-Dodaran M, Tohidi M, Gohari MR, Azizi F. Modeling age at menopause using serum concentration of anti-mullerian hormone. J Clin Endocrinol Metab. 2013;98(2):729–35. https://doi.org/10.1210/jc.2012-3176.
Ryan J, Scali J, Carrière I, et al. Impact of a premature menopause on cognitive function in later life. BJOG. 2014;121(13):1729–39. https://doi.org/10.1111/1471-0528.12828.
Afonso RF, Hachul H, Kozasa EH, et al. Yoga decreases insomnia in postmenopausal women: a randomized clinical trial. Menopause. 2012;19(2):186–93. https://doi.org/10.1097/gme.0b013e318228225f.
Pieralli A, Fallani MG, Becorpi A, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294(4):841–6. https://doi.org/10.1007/s00404-016-4118-6.
Svejme O, Ahlborg HG, Nilsson JÅ, Karlsson MK. Early menopause and risk of osteoporosis, fracture and mortality: a 34-year prospective observational study in 390 women. BJOG. 2012;119(7):810–6. https://doi.org/10.1111/j.1471-0528.2012.03324.x.
Tepper PG, Randolph JF, McConnell DS, et al. Trajectory clustering of estradiol and follicle-stimulating hormone during the menopausal transition among women in the Study of Women’s Health across the Nation (SWAN). J Clin Endocrinol Metab. 2012;97(8):2872–80. https://doi.org/10.1210/jc.2012-1422.
Anagnostis P, Stevenson JC, Crook D, Johnston DG, Godsland IF. Effects of menopause, gender and age on lipids and high-density lipoprotein cholesterol subfractions. Maturitas. 2015;81(1):62–8. https://doi.org/10.1016/j.maturitas.2015.02.262.
Hamaguchi M, Kojima T, Ohbora A, Takeda N, Fukui M, Kato T. Aging is a risk factor of nonalcoholic fatty liver disease in premenopausal women. World J Gastroenterol. 2012;18(3):237–43. https://doi.org/10.3748/wjg.v18.i3.237.
Akazawa N, Choi Y, Miyaki A, et al. Curcumin ingestion and exercise training improve vascular endothelial function in postmenopausal women. Nutr Res. 2012;32(10):795–9. https://doi.org/10.1016/j.nutres.2012.09.002.
Klair JS, Yang JD, Abdelmalek MF, et al. A longer duration of estrogen deficiency increases fibrosis risk among postmenopausal women with nonalcoholic fatty liver disease. Hepatology. 2016;64(1):85–91. https://doi.org/10.1002/hep.28514.
Cordina-Duverger E, Truong T, Anger A, et al. Risk of breast cancer by type of menopausal hormone therapy: a case-control study among post-menopausal women in France. PLoS ONE. 2013;8(11): e78016. https://doi.org/10.1371/journal.pone.0078016.
Lin WT, Beattie M, Chen LM, et al. Comparison of age at natural menopause in BRCA1/2 mutation carriers with a non-clinic-based sample of women in northern California. Cancer. 2013;119(9):1652–9. https://doi.org/10.1002/cncr.27952.
Evans HM, Howe PRC, Wong RHX. Effects of resveratrol on cognitive performance, mood and cerebrovascular function in post-menopausal women; A 14-week randomised placebo-controlled intervention trial. Nutrients. 2017;9(1):27. https://doi.org/10.3390/nu9010027.
Dufour R, Winzenrieth R, Heraud A, Hans D, Mehsen N. Generation and validation of a normative, age-specific reference curve for lumbar spine trabecular bone score (TBS) in French women. Osteoporos Int. 2013;24(11):2837–46. https://doi.org/10.1007/s00198-013-2384-8.
Winters-Stone KM, Dobek J, Nail LM, et al. Impact + resistance training improves bone health and body composition in prematurely menopausal breast cancer survivors: a randomized controlled trial. Osteoporos Int. 2013;24(5):1637–46. https://doi.org/10.1007/s00198-012-2143-2.
Blümel JE, Cano A, Mezones-Holguín E, et al. A multinational study of sleep disorders during female mid-life. Maturitas. 2012;72(4):359–66. https://doi.org/10.1016/j.maturitas.2012.05.011.
Bentzen JG, Forman JL, Johannsen TH, Pinborg A, Larsen EC, Andersen AN. Ovarian antral follicle subclasses and anti-mullerian hormone during normal reproductive aging. J Clin Endocrinol Metab. 2013;98(4):1602–11. https://doi.org/10.1210/jc.2012-1829.
Wang ET, Pisarska MD, Bresee C, et al. BRCA1 germline mutations may be associated with reduced ovarian reserve. Fertil Steril. 2014;102(6):1723–8. https://doi.org/10.1016/j.fertnstert.2014.08.014.
Hodis HN, Mack WJ, Shoupe D, et al. Methods and baseline cardiovascular data from the Early versus Late Intervention Trial with Estradiol testing the menopausal hormone timing hypothesis. Menopause. 2015;22(4):391–401. https://doi.org/10.1097/GME.0000000000000343.
Sankaran-Walters S, Macal M, Grishina I, et al. Sex differences matter in the gut: effect on mucosal immune activation and inflammation. Biol Sex Differ. 2013;4(1):10. https://doi.org/10.1186/2042-6410-4-10.
Tamimi RM, Spiegelman D, Smith-Warner SA, et al. Population attributable risk of modifiable and nonmodifiable breast cancer risk factors in postmenopausal breast cancer. Am J Epidemiol. 2016;184(12):884–93. https://doi.org/10.1093/aje/kww145.
El Khoudary SR, Wildman RP, Matthews K, Thurston RC, Bromberger JT, Sutton-Tyrrell K. Progression rates of carotid intima-media thickness and adventitial diameter during the menopausal transition. Menopause. 2013;20(1):8–14. https://doi.org/10.1097/gme.0b013e3182611787.
Mishra GD, Kuh D. Health symptoms during midlife in relation to menopausal transition: British prospective cohort study. BMJ. 2012;344: e402. https://doi.org/10.1136/bmj.e402.
Acknowledgements
We thank Guixiang Xia for providing language suggestions.
Funding
This work was supported by the National Key Research and Development Plan of China.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection was performed by ZHANG Wei, JIN Zi-shan and TIAN Chuan-xi. Data analysis and visualization were performed by KANG Meng-jiao and HU Shi-wan, and they contributed equally to this work. The first draft of the manuscript was written by ZHANG Wei, JIN Zi-shan and ZHAO Lin-hua, and all authors commented on previous versions of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
No potential conflict of interest was reported by the author(s).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: in the Funding section, an incorrect grant number was given; it has been removed.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jin, Z., Tian, C., Kang, M. et al. The 100 top-cited articles in menopausal syndrome: a bibliometric analysis. Reprod Health 21, 47 (2024). https://doi.org/10.1186/s12978-024-01770-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12978-024-01770-9