Abstract
Background
The association between body mass index (BMI) and Alzheimer's disease (AD) remains controversial. Genetic and environmental factors are now considered contributors to AD risk. However, little is known about the potential interaction between genetic risk and BMI on AD risk.
Objective
To study the causal relationship between BMI and AD, and the potential interaction between AD genetic risk and BMI on AD risk.
Methods and Results
Using the UK Biobank database, 475,813 participants were selected for an average follow-up time of more than 10 years. Main findings: 1) there was a nonlinear relationship between BMI and AD risk in participants aged 60 years or older (p for non-linear < 0.001), but not in participants aged 37–59 years (p for non-linear = 0.717) using restricted cubic splines; 2) for participants aged 60 years and older, compared with the BMI (23–30 kg/m2) group, the BMI (< 23 kg/m2) group was associated with a higher AD risk (HR = 1.585; 95% CI 1.304–1.928, p < 0.001) and the BMI (> 30 kg/m2) group was associated with a lower AD risk (HR = 0.741; 95% CI 0.618–0.888, p < 0.01) analyzed using the Cox proportional risk model; 3) participants with a combination of high AD genetic risk score (AD-GRS) and BMI (< 23 kg/m2) were associated with the highest AD risk (HR = 3.034; 95% CI 2.057–4.477, p < 0.001). In addition, compared with the BMI (< 23 kg/m2), the higher BMI was associated with a lower risk of AD in participants with the same intermediate or high AD-GRS; 4) there was a reverse causality between BMI and AD when analyzed using bidirectional Mendelian randomization (MR).
Conclusion
There was a reverse causality between BMI and AD analyzed using MR. For participants aged 60 years and older, the higher BMI was associated with a lower risk of AD in participants with the same intermediate or high AD genetic risk. BMI (23–30 kg/m2) may be a potential intervention for AD.
Similar content being viewed by others
Background
Dementias are chronic, progressive neurological diseases characterized by memory loss and cognitive impairment [1]. Among the dementias, the most common one is Alzheimer's disease (AD), which accounts for approximately 50–70% of all dementia patients [2]. Critically, its prevalence is rising sharply, owing to the global population aging [3]. Therefore, reducing the burden of AD has become an important global public health issue [4].
The main pathological features of AD include amyloid plaques and neuronal filament entanglement [5, 6]. AD is believed to arise from a combination of genetic and environmental factors and it can be divided into early-onset AD (EOAD) and late-onset AD (LOAD) [3, 7]. It is important to identify the gene-environment interactions behind the development of AD, which would allow for the development of personalized intervention strategies for early intervention of AD, thereby ultimately reducing the global incidence of AD [8].
In conjunction with the rising rate of AD, there is also a worrying epidemic of high levels of obesity worldwide [9]. As an indicator of body nutrition, body mass index (BMI) has been reported to be associated with cerebrovascular adverse events, a variety of cancers, and other diseases [10,11,12,13]. However, the association between BMI and AD risk remains controversial [14]. Several studies have shown that obesity and weight loss in middle age are associated with an increased risk of dementia [15, 16], while other studies have shown that obesity in old age does not increase the risk of AD [16, 17]. Moreover, a large UK population study has shown that low BMI across all age groups increases the risk of AD [18]. Although many previous studies have focused on the association between BMI and AD, these conflicting results suggest that the causal relationship between BMI and AD requires further exploration. Moreover, gene-environment interactions behind the development of AD also need deep investigation. However, little is known about the potential interaction between genetic risk and BMI on AD risk so far.
Understanding the causal relationship between BMI and AD is crucial for AD prevention. However, simple observational studies tend to result in reverse causality and residual confusion [19]. Mendelian randomization (MR) based on genetic variations is useful to overcome some of these limitations [20]. Numerous previous studies using MR analysis to assess the causal effect of BMI on AD found that polygenic scores strongly related to a higher BMI are unrelated to higher dementia risk and may even predict a lower dementia risk. This is surprising, however, there has been no further assessment of reverse causality [21]. Fortunately, bidirectional MR overcomes this limitation [22]. For the first time, this study used bidirectional MR to assess the causal relationship between BMI and AD. In addition, since we conducted observational studies and MR in the same study population, the conclusions could be more stable and reliable.
Therefore, we sought to use the UK Biobank (UKB) to investigate the relationship between BMI and risk of developing AD. To further assess the relationship between BMI and genetic susceptibility on AD risk, we also explored potential genetic and BMI interactions after calculating the AD genetic risk score (AD-GRS) of each participant. Finally, bidirectional MR was used to further explore the causal relationship between BMI and AD.
Methods
Study population
A public database is specifically designed to store scientific research data on an open platform [23]. The UK Biobank (UKB) is the world's largest biomedical sample database and contains data from a population-based cohort study consisting of more than 500,000 volunteers. The UKB study was approved by the Northwest Multicenter Research Ethics Committee, and all participants agreed to their inclusion [24, 25]. Importantly, it has collected—and continues to collect—a large number of participant data regarding phenotypes and genotypes [26, 27].
Initially, 502,490 participants were enrolled, excluding the participants who.
had been diagnosed with AD prior to registration (n = 18) and who either did not undergo genetic testing (n = 13,121) or did not complete baseline data collection (n = 26,659). This resulted in 475,813 participants who were enrolled in our study. A study flow chart of the analysis process is presented in Fig. 1. All participants have a complete case analysis.
Ascertainment of exposure and basic characteristics
According to the UKB, BMI was measured by weight (kg) divided by height measured per square meter (m2). The basic characteristics of each participant were primarily identified using registration records. Follow-up occurred from the registration date to the time of AD diagnosis, death, or final follow-up time (December 2020), whichever occurred first.
Definition of genetic risk score
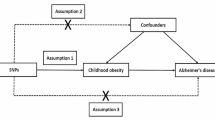
Regarding quality control, the input procedures and genotyping for participants included in the UKB have been described previously [28]. In this study, the newly discovered loci from the UKB were not included to reduce false positives. 29 independent single nucleotide polymorphisms (SNPs) with significant association with AD were selected based on a previous genome-wide association study (GWASs) [29,30,31].
The selected SNPs are listed in the Additional file 2: Table S1. For each individual included in the UKB, an AD-GRS was determined using the previously published method [32]. The effect size (beta-coefficient) of each SNP was derived from the reported GWAS results [30]. Each participant was assigned as one of the following genetic risks for AD: High (5 quintile), intermediate (2–4 quartile), or low (1 quintile).
Outcome assessment
In the UKB database, the AD outcome of each participant is determined by algorithmically-defined outcomes (https://www.ukbiobank.ac.uk).
MR analyses
MR is based on the natural and random classification of genetic variation during meiosis to produce the random distribution of genetic variation in a population [20]. Genetic variation has been used as an instrumental variable (IV). In bidirectional MR, exposure instruments and outcome are used to assess whether the “exposure” variable causes the “outcome” or the “outcome” causes the “exposure"[33], and it is done using the SNPs to study the causal relationship in the separate GWASs [34]. The BMI genetic IV was obtained from a GWAS of UKB participants (https://gwas.mrcieu.ac.uk/; GWAS ID: ukb-b-19953). AD genetic IV data were also obtained from a GWAS [(https://gwas.mrcieu.ac.uk/; GWAS ID: ieu-b-2; data from Alzheimer Disease Genetics Consortium (ADGC), European Alzheimer's Disease Initiative (EADI)]. To remove IVs with linkage disequilibrium, SNPs were clumped for independence if they had a correlation of r2 > 0.001 [35]. Two methods—Inverse variance weighted (IVW)-MR and MR-Egger—have been primarily used for MR analysis [36]. To further ensure the reliability of the MR results, three other methods including Weighted median, Simple mode and Weighted mode were also used simultaneously.
First, we explored the causal relationship between BMI (exposure) and AD (outcome). The exposure and outcome data are available in the Additional file 2: Tables S2 and S3, respectively. After harmonizing the effect allele and removing the SNPs for being palindromic with intermediate allele frequencies, the remaining 433 SNPS were further analyzed using MR. After calculating the MR results, we next conducted a sensitivity analysis [37] mainly from the following three aspects: (1) Heterogeneity test: To test for differences among IVs. As these results showed a strong heterogeneity among IVs (p < 0.05), we next used a random effects model to estimate MR effect size. However, the random effects model yielded similar causal association results (p > 0.05). (2) Pleiotropy test: To test for horizontal pleiotropy in multiple IVs, which is often expressed by the intercept of MR Egger's law. Our results showed that there was no horizontal pleiotropy across multiple IVs (p > 0.05). (3) Leave-one-out sensitivity test: To calculate MR results of the remaining IVs after successive elimination of each IV. No matter which SNP was removed, it had no fundamental effect on the result, showing that our results were robust (Additional file 1: Figure S1). The visualization of the Mendelian randomization results and a detailed explanation of the conclusion are shown in Additional file 1: Figures S2–S4.
Second, we explored the reverse causal relationship between BMI (outcome) and AD (exposure). The exposure and outcome data are shown in Additional file 2: Tables S4 and T5, respectively. After calculating these MR results, we next performed a sensitivity analysis as previously described: (1) Heterogeneity test: These results showed a strong heterogeneity among IVs (p < 0.05), and a further random effects model yielded similar causal association results (p < 0.001). (2) Pleiotropy test: Our results showed that there was no horizontal pleiotropy across multiple IVs (p > 0.05). (3) Leave-one-out sensitivity test: Regardless of which SNP was removed, it had no fundamental effect on the results, indicating that our MR results were robust (Additional file 1: Figure S5). Meanwhile, the funnel figure showed that the funnel plot was symmetrical on the whole, without any obvious heterogeneity (Additional file 1: Figure S6).
R software (version 4.1.0) was used for all statistical analyses and the Two Sample MR package was used for MR analyses.
Statistical analyses
Comparison of the baseline characteristics between control and AD groups was performed using the Chi-square (or univariate logistic regression) or Wilcoxon rank sum test. The P values were tested and adjusted by Benjamini–Hochberg false discovery rate (FDR) method. Continuous variables are represented as mean ± standard deviation or median ± interquartile range (IQR).
A restricted cubic spline (RCS) was used to further study the potential nonlinear relationship between BMI and AD. Moreover, an age subgroup analysis was also performed. The model was adjusted for age, Townsend deprivation index (TDI), sex, smoking, ethnicity, education level, alcohol use, hypertension, stroke, myocardial infarction, and diabetes. In addition, we divided BMI into three groups (< 23 kg/m2, 23–30 kg/m2, > 30 kg/m2) according to the RCS results.
A Kaplan–Meier survival curve was used to show the risk of AD among the three BMI groups (< 23 kg/m2, 23–30 kg/m2, > 30 kg/m2). The BMI (23–30 kg/m2) group was used as the control group, and the differences between the three groups were evaluated using log-rank tests.
A Cox proportional risk model was used to test the association between BMI and AD. The multivariable model 1 was unadjusted, model 2 was adjusted for age and sex, and model 3 was adjusted for age, TDI, sex, smoking, ethnicity, education level, alcohol use, hypertension, stroke, myocardial infarction, and diabetes.
A Cox proportional risk model was used to estimate the association between BMI and AD-GRS for risk of AD. The multivariable model was adjusted for age, TDI, sex, education level, alcohol use, hypertension, stroke, myocardial infarction, and diabetes.
All statistical analyses were performed with the R package (version 4.1.0). A p value < 0.05 was considered statistically significant.
Results
Basic characteristics of control and AD groups
The mean follow-up time was 11.58 years. We compared the basic characteristics of participants who developed AD (AD group, n = 886) and those who did not (control group, n = 474,927). As shown in Table 1, the AD group had a higher age and a larger TDI (p < 0.05). Those that were male, had a history of smoking, or were of mixed race as well as those with hypertension, diabetes, or a history of myocardial infarction or stroke had higher rates of AD (p < 0.05). Moreover, a lower education level correlated with a higher incidence of AD (p < 0.05). In addition, there were no significant differences in BMI between the AD and control groups.
The association between BMI and the risk of AD analyzed using RCS
When assessing the results from previous studies, the effect of BMI on AD risk remains controversial [15,16,17]. As shown in Fig. 2A, there was a nonlinear relationship in the 37–73 years age group (p for non-linear < 0.001). Previous studies have defined 40–59 years as middle-aged and 60 years and older as elderly [38]. We further analyzed these age subgroups. Interestingly, as shown in Fig. 2B, there was no significant association between BMI and AD risk in the 37–59 years age group (p for non-linear = 0.717). However, as shown in Fig. 2C, there was a nonlinear relationship in the 60 years and older age group (p for non-linear < 0.001).
To further explore the appropriate BMI range between BMI and the risk of AD, we divided BMI into three groups according to the RCS results shown in Fig. 2. We used Kaplan–Meier survival curves to demonstrate the risk of AD among the three BMI groups (< 23 kg/m2, 23–30 kg/m2, and > 30 kg/m2). As shown in Fig. 3A, there was no significant difference in risk of developing AD across the three BMI groups of the 37–59 years old group. However, for participants aged 60 years and older, there was a significant difference across the three BMI groups (Fig. 3B). Compared with the BMI (23–30 kg/m2) group, the BMI (< 23 kg/m2) group had a significant association with a higher risk of AD (p < 0.001), while the BMI (> 30 kg/m2) group had an association with a lower AD risk (p = 0.17).
In summary, our results indicated a nonlinear relationship between BMI and AD risk in participants aged 60 years or older, but not in participants aged 37–59 years. Moreover, for participants aged 60 years and older, the BMI (< 23 kg/m2) group had a significant association with a higher risk of AD.
Hazard ratio estimation for AD using Cox proportional risk model
As shown in Fig. 4A, for participants aged 60 years and older, compared with the BMI (23–30 kg/m2) group, the BMI (< 23 kg/m2) group was associated with a higher AD risk (HR = 1.35; 95% CI 1.118–1.64, p < 0.01) in the unadjusted model 1, the BMI (< 23 kg/m2) group was associated with a higher AD risk (HR = 1.585; 95% CI 1.304–1.928, p < 0.001) and the BMI (> 30 kg/m2) group was associated with a lower AD risk (HR = 0.741; 95% CI 0.618–0.888, p < 0.01) in the multivariable adjusted model 3.
The Cox proportional risk model estimating the hazard ratio of AD. A: model 1 was unadjusted, model 2 was adjusted for age and sex, and model 3 was adjusted for age, TDI, sex, smoking, ethnicity, education level, alcohol use, hypertension, stroke, myocardial infarction, and diabetes. B: Joint association between long BMI and genetic risk score for AD. The multivariable model was adjusted for age, TDI, sex, education level, alcohol use, hypertension, stroke, myocardial infarction, and diabetes. The vertical line indicates a reference value of 1
For participants aged 60 years and older, our results indicated that the participants with the BMI (< 23 kg/m2) were associated with a higher AD risk.
Joint association between BMI and AD-GRS for risk of AD
In combination, genetic and environmental factors have been considered main contributors to the progression of AD [3]. Therefore, we further investigated the potential interaction between genetic susceptibility and BMI on the risk of AD. As shown in Fig. 4B, there was no statistically significant interaction between BMI and GRS (p for interaction = 0.14). Additionally, participants with a combination of high AD-GRS and BMI (< 23 kg/m2) were associated with the highest AD risk (HR = 3.034; 95% CI 2.057–4.477, p < 0.001). In addition, compared with the BMI (< 23 kg/m2), the higher BMI was associated with lower risk of AD in participants with the same intermediate or high AD-GRS.
Bidirectional MR of BMI and AD
First, we explored the causal relationship between BMI (exposure) and AD (outcome). A summary of the MR-based analysis of BMI and AD risk is shown in Fig. 5A. Our five MR analysis results indicated that genetically predicted higher risk of BMI was not associated with the risk of AD (p > 0.05).
A: Summary of the Mendelian Randomization-Based Analysis of BMI (exposure) and AD (outcome). B: Summary of the Mendelian Randomization-Based Analysis of AD (exposure) and BMI (outcome).C: Scatter plot. Each point on this graph represents an IV, and the line on each point reflects a 95% confidence interval. D: The MR effect size for AD on BMI through the IVW and MR Egger methods
Second, we further explored the reverse causal relationship between BMI (outcome) and AD (exposure). The summary of the MR-based analysis of BMI and AD risk is shown in Fig. 5B. In the reverse direction, our five MR analysis results indicated that genetically predicted higher risk of AD was associated with lower BMI (OR < 1, p < 0.001). Figure 5C and D are visualizations of the MR results, which further confirmed the results shown in Fig. 5B.
Our results indicated there was a reverse causality between BMI and AD risk, and genetically predicted higher risk of AD was associated with lower BMI, suggesting that reduced BMI could be one of the early manifestations of AD.
Discussion
In this large-scale study with an average follow-up time of more than 10 years, we have the following main findings: 1. our results indicated there was a nonlinear relationship between BMI and AD risk in participants aged 60 years or older, but not in participants aged 37–59 years; 2. for participants aged 60 years and older, our results indicated that participants with the BMI (< 23 kg/m2) were associated with a higher AD risk; 3. compared with the BMI (< 23 kg/m2), the higher BMI was associated with lower risk of AD in participants with the same intermediate or high AD-GRS; 4. there was a reverse causality between BMI and AD analyzed using bidirectional MR.
With global incidence of both obesity and dementia increasing year by year, understanding the causal relationship between BMI and AD risk has become a public health priority [39]. To the best of our knowledge, our study is the first to use bidirectional MR to establish a causal relationship between BMI and AD risk. Our results showed that there is a reverse causality between BMI and AD risk analyzed using bidirectional MR, suggesting that reduced BMI could be one of the early manifestations of AD.
Possible pathogenesis of BMI declines in AD patients has been investigated in previous studies. Reduced hippocampal volume and thinning of the entorhinal and medial temporal cortices are common imaging findings in AD patients [40]. Imaging data also indicate that brain structural changes, including changes of whole brain and hippocampal atrophy, are associated with alterations in body composition, including reductions in more specific measures of lean mass [41]. The potential mechanisms underlying the pathophysiological relationship between BMI and AD risk include neuropathological changes occur in regions like hypothalamus that play critical roles in regulation of energy metabolism and food intake [42]. Behavioral and cognitive changes associated with dementia can also affect weight by interfering with nutrition (forgetting to eat) or by reducing physical activity (a strong predictor of sarcopenia) [43]. In addition, Apolipoprotein E (APOE), produced primarily by astrocytes in the central nervous system, is a major cholesterol carrier that transports lipids to neurons to maintain synapses and promote damage repair, which is linked to increased accumulation of cortical amyloid-β (Aβ) [44]. The E4 allele of APOE gene (APOE4) is the strongest genetic risk factor for late AD [45]. The accumulation of Aβ in APOE4 + individuals is regulated by leptin signaling in the hypothalamus [46], and leptin signaling pathway itself could lead to the synthesis and release of anorexia neuropeptides that may contribute to weight loss [47, 48].
Although our bidirectional MR results showed no positive causal relationship between BMI and AD risk due to the limitations of the MR method, a false-negative result cannot be ruled out. Our MR method mainly studied linear causality. However, our observational study found that the association between higher BMI and AD risk was non-linear. In addition, after the participants were grouped according to AD-GRS, a lower BMI was still associated with a higher risk of AD in the intermediate or high AD-GRS groups. Studies also showed that higher BMI-related genetic variants may slightly reduce the risk of AD [18], however, their non-linear relationship has been studied. Therefore, we speculated that there might be a non-linear causal relationship between BMI and the risk of AD. However, more research is needed to clarify this.
The possible mechanism underlying that high BMI is associated with lower risk of AD in older individuals remains poorly understood. Blautzik et al. showed that even among APOE4 carriers, BMI was negatively associated with cortical amyloid load, glucose metabolism in posterior cingulate gyrus, and recent cognitive decline [47]. Adipose tissue releases molecules such as leptin and adiponectin, which bind to receptors in the hippocampus to regulate neuronal excitability, increase synaptogenesis, and prevent amyloid-induced neuronal cell death [49, 50]. In addition, microglia are innate immune cells of the central nervous system, which can prevent development of AD by inhibiting accumulation of Aβ [51]. Adiponectin can inhibit Aβ-induced inflammation and promote anti-inflammatory properties of microglia [52, 53]. Adiponectin receptor agonists can suppress microglia and astrocyte activation and restore microglia Aβ phagocytosis in mouse models of AD [54]. Since AD is an age-related disease, this might partially explain why high BMI in old age is associated with a lower risk of AD development [55]. However, further research will be needed to understand this mechanistic basis.
There is no significant association between BMI and AD risk in observational studies of participants aged 37–59 years old using RCS. Because the preclinical phase of dementia can last for more than 10 years [56], most of the participants may not have reached the diagnostic criteria for AD, and this population (37–59 years old) requires further follow-up in the future. Genetic and environmental factors have been considered contributors to the progression of AD [3]. To our knowledge, this is the first study to investigate the interaction between BMI and GRS on development of AD. As expected, for participants aged 60 and older, we observed that participants with high genetic risk had a higher risk of AD. In addition, a lower BMI (< 23 kg/m2) was associated with a higher risk of AD in the intermediate and high AD-GRS groups. Since genetic factor is an unmodifiable factor for the risk of AD, more attention should be paid to the management of BMI, especially in the populations with intermediate or high AD-GRS. It is considered that increased BMI (greater than 30 kg/m2) may lead to cardiovascular and metabolic diseases [57]. In addition, we also found that there was a U-shaped association between BMI and all-cause mortality, and higher BMI (BMI > 30 kg/m2) and lower BMI (BMI < 23 kg/m2) were associated with a higher risk of all-cause mortality (Additional file 1: Figure S7). These findings suggest that a higher BMI (BMI > 30 kg/m2) was not associated with a higher risk of AD, possibly due to the complications that had led to death in participants before AD was diagnosed, further validation is needed in future studies. Therefore, BMI (23–30 kg/m2) may be a potential intervention for AD without increasing complications and all-cause mortality.
Conclusions
There was a reverse causality between BMI and AD risk analyzed using MR. For participants aged 60 and older, the higher BMI was associated with a lower risk of AD in participants with the same intermediate or high AD genetic risk. BMI (23–30 kg/m2) may be a potential intervention for AD.
Limitations
This study was based on the UKB, which includes participants of a predominantly European ancestry. While this may affect the applicability of the results to other ethnicities, it does not change the internal validity of this study. During our follow-up, the BMI of participants may change, which is also one of the limitations of this study. However, the design of randomized trials for BMI is hardly feasible, and future longitudinal trajectory changes may overcome this limitation.
Availability of data and materials
The data that support the findings of this study are available from UK Biobank but restrictions may apply to the availability of these data, so they are not publicly available. However, the data are available from the authors with permission from the UK Biobank.
Abbreviations
- BMI:
-
Body mass index
- AD:
-
Alzheimer's disease
- AD-GRS:
-
Alzheimer's disease genetic risk score
- UKB:
-
UK Biobank
- MR:
-
Mendelian randomization
- SNPs:
-
Single nucleotide polymorphisms
- GWASs:
-
Genome-wide association study
- IV:
-
Instrumental variable
- RCS:
-
Restricted cubic spline
- TDI:
-
Townsend deprivation index
References
Groot C, Hooghiemstra AM, Raijmakers PG, van Berckel BN, Scheltens P, Scherder EJ, et al. The effect of physical activity on cognitive function in patients with dementia: a meta-analysis of randomized control trials. Ageing Res Rev. 2016;25:13–23.
Winblad B, Amouyel P, Andrieu S, Ballard C, Brayne C, Brodaty H, et al. Defeating Alzheimer’s disease and other dementias: a priority for European science and society. Lancet Neurol. 2016;15:455–532.
Lane CA, Hardy J, Schott JM. Alzheimer’s disease. Eur J Neurol. 2018;25:59–70.
Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10:819–28.
Yuan S, Li H, Yang C, Xie W, Wang Y, Zhang J, et al. DHA attenuates Abeta-induced necroptosis through the RIPK1/RIPK3 signaling pathway in THP-1 monocytes. Biomed Pharmacother. 2020;126: 110102.
Serrano-Pozo A, Frosch MP, Masliah E, Hyman BT. Neuropathological alterations in Alzheimer disease. Cold Spring Harb Perspect Med. 2011;1: a6189.
Zusso M, Barbierato M, Facci L, Skaper SD, Giusti P. Neuroepigenetics and Alzheimer’s Disease: an Update. J ALZHEIMERS DIS. 2018;64:671–88.
Dunn AR, O’Connell K, Kaczorowski CC. Gene-by-environment interactions in Alzheimer’s disease and Parkinson’s disease. Neurosci Biobehav Rev. 2019;103:73–80.
Luchsinger JA, Gustafson DR. Adiposity and Alzheimer’s disease. Curr Opin Clin Nutr Metab Care. 2009;12:15–21.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 2019;140:e596-646.
Mariscalco G, Wozniak MJ, Dawson AG, Serraino GF, Porter R, Nath M, et al. Body mass index and mortality among adults undergoing cardiac surgery: a nationwide study with a systematic review and meta-analysis. Circulation. 2017;135:850–63.
Qin B, Yang M, Fu H, Ma N, Wei T, Tang Q, et al. Body mass index and the risk of rheumatoid arthritis: a systematic review and dose-response meta-analysis. Arthritis Res Ther. 2015;17:86.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–78.
Nordestgaard LT, Tybjaerg-Hansen A, Nordestgaard BG, Frikke-Schmidt R. Body mass index and risk of Alzheimer’s disease: a mendelian randomization study of 399,536 individuals. J Clin Endocrinol Metab. 2017;102:2310–20.
Loef M, Walach H. Midlife obesity and dementia: meta-analysis and adjusted forecast of dementia prevalence in the United States and China. Obesity (Silver Spring). 2013;21:E51–5.
Fitzpatrick AL, Kuller LH, Lopez OL, Diehr P, O’Meara ES, Longstreth WJ, et al. Midlife and late-life obesity and the risk of dementia: cardiovascular health study. Arch Neurol. 2009;66:336–42.
Dahl AK, Lopponen M, Isoaho R, Berg S, Kivela SL. Overweight and obesity in old age are not associated with greater dementia risk. J Am Geriatr Soc. 2008;56:2261–6.
Qizilbash N, Gregson J, Johnson ME, Pearce N, Douglas I, Wing K, et al. BMI and risk of dementia in two million people over two decades: a retrospective cohort study. Lancet Diabetes Endocrinol. 2015;3:431–6.
Kumari M, Holmes MV, Dale CE, Hubacek JA, Palmer TM, Pikhart H, et al. Alcohol consumption and cognitive performance: a Mendelian randomization study. Addiction. 2014;109:1462–71.
Smith GD, Ebrahim S. “Mendelian randomization”: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32:1–22.
Mukherjee S, Walter S, Kauwe J, Saykin AJ, Bennett DA, Larson EB, et al. Genetically predicted body mass index and Alzheimer’s disease-related phenotypes in three large samples: Mendelian randomization analyses. Alzheimers Dement. 2015;11:1439–51.
Davey SG, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23:R89-98.
Wu WT, Li YJ, Feng AZ, Li L, Huang T, Xu AD, et al. Data mining in clinical big data: the frequently used databases, steps, and methodological models. Mil Med Res. 2021;8:44.
Yang J, Li Y, Liu Q, Li L, Feng A, Wang T, et al. Brief introduction of medical database and data mining technology in big data era. J Evid Based Med. 2020;13:57–69.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. Plos Med. 2015;12: e1001779.
Tao F, Cao Z, Jiang Y, Fan N, Xu F, Yang H, et al. Associations of sleep duration and quality with incident cardiovascular disease, cancer, and mortality: a prospective cohort study of 407,500 UK biobank participants. Sleep Med. 2021;81:401–9.
Petermann-Rocha F, Parra-Soto S, Gray S, Anderson J, Welsh P, Gill J, et al. Vegetarians, fish, poultry, and meat-eaters: who has higher risk of cardiovascular disease incidence and mortality? A prospective study from UK Biobank. Eur Heart J. 2021;42:1136–43.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Leng Y, Ackley SF, Glymour MM, Yaffe K, Brenowitz WD. Genetic risk of Alzheimer’s disease and sleep duration in non-demented elders. Ann Neurol. 2021;89:177–81.
Jansen IE, Savage JE, Watanabe K, Bryois J, Williams DM, Steinberg S, et al. Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Nat Genet. 2019;51:404–13.
Marioni RE, Harris SE, Zhang Q, McRae AF, Hagenaars SP, Hill WD, et al. GWAS on family history of Alzheimer’s disease. Transl Psychiatry. 2018;8:99.
Fan M, Sun D, Zhou T, Heianza Y, Lv J, Li L, et al. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: a prospective study of 385 292 UK biobank participants. Eur Heart J. 2020;41:1182–9.
Timpson NJ, Nordestgaard BG, Harbord RM, Zacho J, Frayling TM, Tybjaerg-Hansen A, et al. C-reactive protein levels and body mass index: elucidating direction of causation through reciprocal Mendelian randomization. Int J Obes (Lond). 2011;35:300–8.
Zheng J, Baird D, Borges MC, Bowden J, Hemani G, Haycock P, et al. Recent developments in Mendelian randomization studies. Curr Epidemiol Rep. 2017;4:330–45.
Sproviero W, Winchester L, Newby D, Fernandes M, Shi L, Goodday SM, et al. High blood pressure and risk of dementia: a two-sample Mendelian randomization study in the UK Biobank. Biol Psychiatry. 2021;89:817–24.
Bowden J, Holmes MV. Meta-analysis and Mendelian randomization: a review. Res Synth Methods. 2019;10:486–96.
Harrison S, Davies NM, Howe LD, Hughes A. Testosterone and socioeconomic position: Mendelian randomization in 306,248 men and women in UK Biobank. Sci Adv. 2021. https://doi.org/10.1126/sciadv.abf8257.
Anstey KJ, Cherbuin N, Budge M, Young J. Body mass index in midlife and late-life as a risk factor for dementia: a meta-analysis of prospective studies. Obes Rev. 2011;12:e426–37.
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–67.
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet. 2020;396:413–46.
Burns JM, Johnson DK, Watts A, Swerdlow RH, Brooks WM. Reduced lean mass in early Alzheimer disease and its association with brain atrophy. Arch Neurol. 2010;67:428–33.
Loskutova N, Honea RA, Brooks WM, Burns JM. Reduced limbic and hypothalamic volumes correlate with bone density in early Alzheimer’s disease. J Alzheimers Dis. 2010;20:313–22.
Baumgartner RN, Waters DL, Gallagher D, Morley JE, Garry PJ. Predictors of skeletal muscle mass in elderly men and women. Mech Ageing Dev. 1999;107:123–36.
Bu G. Apolipoprotein E and its receptors in Alzheimer’s disease: pathways, pathogenesis and therapy. Nat Rev Neurosci. 2009;10:333–44.
Liu CC, Zhao N, Fu Y, Wang N, Linares C, Tsai CW, et al. ApoE4 accelerates early seeding of amyloid pathology. Neuron. 2017;96:1024–32.
Mun YS, Park HK, Kim J, Yeom J, Kim GH, Chun MY, et al. Association between body mass index and cognitive function in mild cognitive impairment regardless of APOE epsilon4 status. Dement Neurocogn Disord. 2022;21:30–41.
Blautzik J, Kotz S, Brendel M, Sauerbeck J, Vettermann F, Winter Y, et al. Relationship between body mass index, ApoE4 status, and PET-based amyloid and neurodegeneration markers in amyloid-positive subjects with normal cognition or mild cognitive impairment. J Alzheimers Dis. 2018;65:781–91.
Juhasz A, Katona E, Csongradi E, Paragh G. The regulation of body mass and its relation to the development of obesity. Orv Hetil. 2007;148:1827–36.
Hamilton K, Harvey J. The Neuronal Actions of Leptin and the Implications for treating Alzheimer’s Disease. Pharmaceuticals (Basel). 2021. https://doi.org/10.3390/ph14010052.
Irving AJ, Harvey J. Leptin regulation of hippocampal synaptic function in health and disease. Philos Trans R Soc Lond B Biol Sci. 2014;369:20130155.
Hansen DV, Hanson JE, Sheng M. Microglia in Alzheimer’s disease. J Cell Biol. 2018;217:459–72.
Jian M, Kwan JS, Bunting M, Ng RC, Chan KH. Adiponectin suppresses amyloid-beta oligomer (AbetaO)-induced inflammatory response of microglia via AdipoR1-AMPK-NF-kappaB signaling pathway. J Neuroinflammation. 2019;16:110.
Song J, Choi SM, Kim BC. Adiponectin regulates the polarization and function of microglia via PPAR-gamma signaling under amyloid beta toxicity. Front Cell Neurosci. 2017;11:64.
Ng RC, Jian M, Ma OK, Bunting M, Kwan JS, Zhou GJ, et al. Chronic oral administration of adipoRon reverses cognitive impairments and ameliorates neuropathology in an Alzheimer’s disease mouse model. Mol Psychiatry. 2021;26:5669–89.
Liu B, Liu J, Shi JS. SAMP8 mice as a model of age-related cognition decline with underlying mechanisms in Alzheimer’s disease. J Alzheimers Dis. 2020;75:385–95.
Amieva H, Le Goff M, Millet X, Orgogozo JM, Peres K, Barberger-Gateau P, et al. Prodromal Alzheimer’s disease: successive emergence of the clinical symptoms. Ann Neurol. 2008;64:492–8.
Kim MS, Kim WJ, Khera AV, Kim JY, Yon DK, Lee SW, et al. Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur Heart J. 2021;42:3388–403.
Acknowledgements
We would like to thank all the participants, the members of the research and investigation team, as well as the members of the project development and management team.
Funding
This study was funded by General project of national Natural Science Foundation of China (Grant No. 81971121) and Guangdong Provincial Key Laboratory of Traditional Chinese Medicine Informatization (Grant No. 2021B1212040007).
Author information
Authors and Affiliations
Contributions
JL and AX conceptualized the research aims. SY and WW guided the literature review and planned the analyses. WM, XH and TH extracted the data from the UK biobank. SY, MP, and WM participated in data analysis and interpretation. SY wrote the first draft of the paper and the other authors provided comments and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The UK Biobank study was approved by the Northwest Multicenter Research Ethics Committee, and all participants agreed to their inclusion. Our study was conducted under a UK Biobank license (Applications ID:76636).
Consent for publication
All the authors agreed to publish this article.
Competing interests
The authors have no funding and conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Leave-one-out sensitivity test (BMI served as the exposure and AD as outcome), no matter which SNP was removed, it had no fundamental effect on the result, and it showed that the MR result was robust. Figure S2. Scatter plot. Each point on this graph actually represents an IV, and the line on each point reflects the 95% confidence interval. The horizontal axis is the effect of SNP on exposure (BMI), the vertical axis is the effect of SNP on outcome (AD), and the colored line represents the MR fitting result. It suggested that exposure (BMI) had no positive causal relationship with outcome (AD). Figure S3. Forest map. MR effect size for AD on BMI. Each solid horizontal line in the forest map reflects the estimated result of a single SNP using the Wald ratio method. It indicated that the increased BMI did not significantly reduce the risk of AD by the IVW and MR Egger methods. Figure S4. Funnel figure. The funnel plot was symmetrical on the whole without obvious heterogeneity. Figure S5. Leave-one-out sensitivity test (AD served as the exposure and BMI as outcome), no matter which SNP was removed, it had no fundamental effect on the result, and it showed that the MR result was robust. Figure S6. Funnel figure. The funnel plot was symmetrical on the whole without obvious heterogeneity. Figure S7. A: Restricted cubic splines (RCS) for analysis of the relationship between BMI and incidence of AD. Adjusted for age, TDI, sex, smoking, ethnicity, education level, alcohol use, hypertension, stroke, myocardial infarction, and diabetes. B: Cox proportional risk model estimating the hazard ratio of AD. model 1 was unadjusted, model 2 was adjusted for age and sex, model 3 was adjusted for age, TDI, sex, smoking, ethnicity, education level, alcohol use, hypertension, stroke, myocardial infarction, and diabetes.
Additional file 2: Table S1.
the single nucleotide polymorphisms (SNPs) that showed significant genome-wide association with AD,(the SNP loci of newly discovered genes in the UKB database were not included). Table S2. BMI served as the exposure (based on the UKB study , https://gwas.mrcieu.ac.uk/; GWAS ID: ukb-b-19953). Table S3. The datasets as AD outcome (based on another GWASs, https://gwas.mrcieu.ac.uk/; GWAS ID: ieu-b-2). Table S4. AD served as the exposure (based on another GWASs, https://gwas.mrcieu.ac.uk/; GWAS ID: ieu-b-2). Table S5. BMI served as the outcome (based on the UKB study , https://gwas.mrcieu.ac.uk/; GWAS ID: ukb-b-19953)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yuan, S., Wu, W., Ma, W. et al. Body mass index, genetic susceptibility, and Alzheimer's disease: a longitudinal study based on 475,813 participants from the UK Biobank. J Transl Med 20, 417 (2022). https://doi.org/10.1186/s12967-022-03621-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-022-03621-2