Abstract
Throughout human life, bone is constantly in a delicate dynamic equilibrium of synthesis and resorption, hosting finely-tuned bone mineral metabolic processes for bone homeostasis by collaboration or symphony among several cell types including osteoclasts (OCs), osteoblasts (OBs), osteocytes (OYs), vascular endothelial cells (ECs) and their precursors. Beyond these connections, a substantial level of communication seems to occur between bone and other tissues, and together, they form an organic unit linked to human health and disease. However, the current hypothesis, which includes growth factors, hormones and specific protein secretion, incompletely explains the close connections among bone cells or between bone and other tissues. Extracellular vesicles (EVs) are widely-distributed membrane structures consisting of lipid bilayers, membrane proteins and intravesicular cargo (including proteins and nucleic acids), ranging from 30 nm to 1000 nm in diameter, and their characters have been highly conserved throughout evolution. EVs have targeting abilities and the potential to transmit multidimensional, abundant and complicated information, as powerful and substantial “dogrobbers” mediating intercellular communications. As research has progressed, EVs have gradually become thought of as “dogrobbers” in bone tissue—the “eternal battle field” —in a delicate dynamic balance of destruction and reconstruction. In the current review, we give a brief description of the major constituent cells in bone tissues and explore the progress of current research on bone-derived EVs. In addition, this review also discusses in depth not only potential directions for future research to breakthrough in this area but also problems existing in current research that need to be solved for a better understanding of bone tissues.
Similar content being viewed by others
Background
Bone is a very well-adapted tissue in a delicate dynamic balance, hosting finely-tuned bone mineral metabolic processes for the homeostasis of both bone itself and other organs [1]. Emerging evidence has gradually shown that cells in bone are responsible for many effects on other systems, including the central nervous system (CNS), blood sugar, energetic metabolism and gonad function [2,3,4]. Moreover, other systems (including the endocrine system, CNS and digestive system) are also responsible for many effects on bone metabolism [5, 6]. Various kinds of growth factors and hormones impact the dynamic balance and homeostasis of bone tissue [7,8,9]. Osteocalcin (OCN), a specific protein secreted by osteoblasts (OBs), showed modulatory functions on gonad function and pancreatic insulin secretion [2,3,4].
In the bone remodelling compartment (BRC), remodelling takes place throughout the whole life of organisms, including mammals, to maintain bone homeostasis via the replacement of senescent bone and repair of micro-damage [10]. The normal status of this remodelling is essential for the maintenance of both bone mass and bone mechanical properties [11]. In pathological conditions or with ageing, bone resorption exceeds bone formation, leading to low bone mass (osteopenia) or more seriously, osteoporosis [12]. In the opposite situation, bone formation can exceed bone resorption, leading to abnormally high bone mass, or osteosclerosis [12]. During the process of remodelling, a collaboration or symphony exists between two cell types with opposite functions—bone resorption by osteoclasts (OCs) and bone synthesis by OBs [13]. In addition to the two types of precursor cells, osteocytes (OYs) and vascular endothelial cells (ECs) are also responsible for regulating the balance of bone resorption and formation (Fig. 1) [10].
Bone remodelling compartment. OBs: osteogenic cells; OCs: osteoclasts; preOCs: pre-osteoclasts; OYs: osteocytes; HSCs: haematopoietic stem cells; BMSCs: bone mesenchymal stem cells; H-type ECs: endothelial cells strongly expressing both CD31 and endomucin (Emcn); L-type ECs: endothelial cells strongly expressing Emcn but not CD31
However, identification of the specific mechanisms and agents that are responsible for directly triggering and coordinating the processes of remodelling remains difficult. Considering the elaborateness of the regulation of bone remodelling, some communication methods among bone cells are needed to carry abundant information and help coordinate the regulatory processes.
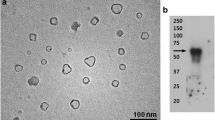
Extracellular vesicles (EVs) have complex membrane structures and range from 30 nm to 1000 nm in diameter [14,15,16,17]. Almost all kinds of cells can secrete EVs, and the process has been highly conserved throughout evolution across many organisms from bacteria to plants and mammals [18,19,20]. In the human body, EVs can be isolated from almost every kind of biological body fluid, including saliva, plasma, ascitic fluid, amniotic fluid, breast milk, and urine [21,22,23].
EVs are composed of lipid bilayers, membrane proteins and intravesicular cargo (including proteins and nucleic acids) [15, 24]. The lipid bilayers provide protection from the complex and potentially-harmful body fluid environment to the bioactive substances within EVs, the membrane proteins give EVs targeting abilities, and the various intravesicular contents (proteins, messenger RNAs [mRNAs], microRNAs [miRNAs], long noncoding RNAs [lncRNAs], circular RNAs [circRNAs], etc.) give EVs the ability to transmit multidimensional, abundant and complicated information [15, 24]; thus, EVs are powerful and substantial “liaison officers” or “dogrobbers” mediating intercellular communications (Fig. 2).
Constituents of EVs. EVs are composed of lipid bilayers, membrane proteins, intravesicular proteins, DNA, messenger RNAs (mRNAs), microRNAs (miRNAs), long noncoding RNAs (lncRNAs), and circular RNAs (circRNAs). The lipid bilayers provide protection from the complex and potentially harmful body fluid environment to the bioactive substances within EVs, the membrane proteins give EVs targeting abilities, and the various intravesicular contents give EVs the ability to transmit multidimensional, abundant and complicated information
Classification of EVs is based on their size and mechanisms of biogenesis [24]. EVs can be simply divided into two main classes: exosomes and microvesicles [14]. Exosomes (ranging from 30 to 100 nm in diameter) originate from multi-vesicular bodies (MVBs) via “inward budding” and are released after fusion between MVBs and the cytoplasmic membrane [14, 15]. Microvesicles (ranging from 100 to 1000 nm in diameter) originate and are released simultaneously at specific sites on the cytoplasmic membrane, named “microdomains”, via “outward budding” from the cytoplasmic membrane [14, 15]. In addition to the main classes, apoptotic bodies (ranging from 800 to 5000 nm in diameter) are vesicles that are shed during the apoptotic process [15]. However, apoptotic bodies rarely participate in intercellular communications, and one potential hypothesis suggests that they are eliminated by phagocytes immediately after their release [15].
Leading researchers in the EV research area, such as Clotilde Thery, suggested that although exosomes and microvesicles have different mechanisms of biogenesis, the present isolation technology is not capable of separating the sub-populations of EVs [25]. The term exosomes in most studies has been used to refer to a mixed sub-population of small EVs, so these researchers have suggested using a more generic term—EVs—when discussing the biological functions but not the mechanisms of biogenesis [25]. Hence, in the later sections of our review, we have used ‘EVs’ instead of ‘exosomes’ or ‘microvesicles’.
The continuous evolution of EV research may be essential for understanding the underlying mechanisms of communications not only among bone cells but also between bone and other body systems. Finally, our understanding of physiology and pathology may be dramatically enhanced. In this review, we introduce the major constituent cells in bone tissues, present the current research progress on EVs derived from these kinds of bone cells, and then point out the problems existing in current research with possible future research directions to achieve a breakthrough in this area.
Cells in bone
Bone is constantly in a delicate dynamic equilibrium of both synthesis and resorption throughout the lives of animals including humans to withstand the demands of their activities. In the process of bone modelling and remodelling, bone-building cells (OBs) are responsible for osteogenesis (or bone synthesis), while bone-resorbing cells (OCs) are responsible for osteolysis (or bone resorption) [13]. In addition to the two ‘executors’, there are several kinds of cells proven to be responsible for the equilibrium of bone mineral metabolism as ‘supervisors’ or ‘regulators’. We will first introduce the background information about the major players in bone modelling and remodelling in order to summarize EVs as intracellular communicators among these cell types.
OBs
OBs make up approximately 5% of the total resident cells in bones [26]. OBs are derived from bone mesenchymal stem cells (BMSCs) [27] and produce bone extracellular matrix (ECM) containing specific proteins, including OCN, alkaline phosphatase (ALP) and type I collagen (Col-I) [28]. In the osteogenic process, the crucial signalling pathways contain bone morphogenetic proteins (BMPs), Wnt proteins, ATF4, Runx2 and Osterix [26, 27, 29,30,31,32,33].
Theoretically speaking, OBs can be classified as preosteoblasts, mature OBs, and bone-lining cells [28]. This classification is based on in vivo histological analysis. However, the problem with this classification is the lack of a definite boundary between these subclasses [28]. Although there are methods for isolating OBs and cell lines that are usually used to study the function of OBs in vitro [34, 35], strictly defined mature OBs should be post mitosis, remain stationary [28] and can be very difficult to culture in vitro. Although in vitro cultured OBs are not strictly defined OBs, they perform well as a good cell model to study the functions of broadly defined OBs in vitro. Some recent viewpoints suggest giving these cells, which have similar functions and are responsible for osteogenesis, a unified name—osteogenic cells [36]. In this review, we use the more widely used term ‘OBs’ to refer to broadly defined OBs or osteogenic cells.
OCs and preOCs
OCs are derived from haematopoietic stem cells (HSCs) [37]. In the process of osteoclastogenesis, the pre-osteoclasts (preOCs), which are tartrate-resistant acid phosphatase–positive (TRAP+) mononuclear cells, are formed first [38]. Then, preOCs form OCs, the TRAP+ multi-nuclear cells, via fusion [38, 39]. The functional disruption of OCs—the only known type of cell that is responsible for the resorption of bone matrix—is the key to pathogenesis related to bone metabolism. For instance, excessively activated OCs will cause osteoporosis and bone destruction [40]. In contrast, the impairment of OC formation or function will cause osteopetrosis [41,42,43].
According to current research, the most important signalling pathway regulating the differentiation of OCs is the receptor activator of nuclear factor kappa-B ligand (RANKL) signalling pathway. After receptor activator of nuclear factor kappa-B (RANK) is bound by RANKL, tumour necrosis factor receptor-associated factor 6 (TRAF6) is recruited to activate nuclear factor kappa-B (NF-κB) and the downstream cascades [44, 45]. Then, after NF-κB translocates into the nucleus, the transcription of OC-specific genes is initiated [44, 45]. In addition, mitogen-associated protein kinase (MAPK) signalling pathways, including p38, extracellular signal-regulated kinase (Erk), Jun N-terminal kinase (JNK), c-Fos and AP-1, are also essential for the formation of OCs [46,47,48,49].
Furthermore, cross-talk between signalling pathways is also important in osteoclastogenesis, such as partial calcium-signalling pathway activation by RANKL [50, 51] and nuclear factor of activated T-cells 1 (NFATc1), which are key during terminal OC differentiation and are common downstream of NF-κB, MAPK, and calcium-signalling pathways [52]. In contrast, the essential modulator responsible for cellular and systemic energy homeostasis, the AMP-activated protein kinase (AMPK) pathway, works as a suppressor of OC formation [53].
For a long time, PreOCs were considered to be simply precursors of OCs [54]. However, the true purpose will always be revealed. Interestingly, an increasing number of studies implied that preOCs may play a role in bone mineral metabolism that is completely different from that of OCs [55]. A large number of preOCs were found in regions associated with rapid growth of bone tissues, such as the periosteal bone surface [54,55,56]. In a more in-depth study using v-ATPase V0 subunit d2-deficient mice, Lee et al. blocked the fusion process of preOCs, leading to a deficiency of OC maturation, and then stimulated bone formation [40]. Xie et al. reported that preOCs promoted both angiogenesis and osteogenesis by targeting H-type vessels (or vessels expressing high levels of both CD31 & endomucin [Emcn]), and the potential key factor may be platelet-derived growth factor-BB (PDGF-BB) [55].
Some signalling pathways of preOCs have been discussed above. In addition, macrophage colony-stimulating factor (M-CSF) plays an important role in triggering the proliferation and differentiation of preOCs via activation of MAPK-Erk and phosphoinositide 3-kinase (PI3K)/protein kinase B (PKB; also known as Akt) signalling [57]. However, the research on preOCs is in its relative infancy with strong potential as not only a therapeutic target but also a candidate for cell therapy or EV-mediated non-cell therapy and thus needs further investigation.
OYs
OYs, which are terminally-differentiated from OBs, are the most abundant sub-population of bone cells at over 90% [58,59,60]. OYs, which measure 9 μm by 20 μm in Homo sapiens, are star-shaped OB-derived cells embedded in mineralized bone matrix that reside in the lacunae as an interconnected network and are bathed in the canalicular fluid [61,62,63]. The highly-organized three-dimensional network of OYs gives them an enhanced adaptive ability [64]. Furthermore, the unique canalicular fluid is one of the information exchange hubs between OYs and the extracellular space containing important substances, including oxygen, nutrients, hormones and growth factors [63]. In the past, OYs were once considered quiescent within the mineralized matrix of bone to observational researchers [61]. As research technologies for studying OYs have advanced, the crucial role of OYs in the regulation of bone mineral metabolism has been gradually revealed.
There are two fundamental and well-recognized concepts in the research area of bone biology [65,66,67,68,69]: (1) Remodelling is primarily ‘damage-driven’, including ‘micro-damage’; (2) the processes of ‘damage-driven’ remodelling are mainly orchestrated by OYs.
The dendritic processes of OYs, which extend through the canaliculi, are essential for forming a highly-connected network not only between OYs but also between OYs and their neighbours, including OBs, OCs and cells in the blood supply in bone [70, 71]. OYs are generally believed to be important mechanosensors of bone tissue and are able to transduce mechanical signals into chemical signals after mechanical stimuli [70, 72]. OYs are also responsible for directly sensing ‘damage’ that interrupts the canaliculi [73,74,75].
Several signalling pathways are involved in OY-predominated regulation and control of OBs and OCs. These pathways are the major sources of sclerostin, the primary candidate for regulating OBs [59, 76, 77], and RANKL, the key modulatory factor of bone resorption via regulating OCs [78]. These two proteins are the major signals involved in bone metabolism [79,80,81].
Sclerostin has been reported to inhibit the Wingless-related integration site (Wnt) pathway and then keep the status ‘inhibition of OB differentiation’ (Fig. 3). However, mechanical loading or ‘damage’ would shut down sclerostin, causing a loss of efficacy of the ‘inhibition of OB differentiation’ function, in other words, increasing OB differentiation and bone mass [82,83,84,85]. Interestingly, mechanical unloading causes high sclerostin levels together with profound bone loss, and this phenomenon might be corroborative evidence of sclerostin’s function in OY-mediated bone mass modulation [86]. RANKL derived from OYs participates in osteoclastogenesis and OC activity and then modulates the resorption of bone tissue [87].
‘Micro-damage-driven’ remodelling orchestrated by OYs via sclerostin. OYs are responsible for directly sensing ‘damage’ that interrupts the canaliculi. Sclerostin has been reported to maintain the status ‘inhibition of OB differentiation’. However, mechanical loading or ‘damage’ would shut down sclerostin, causing a loss of efficacy of the ‘inhibition of OB differentiation’ function; in other words, increasing OB differentiation and bone mass
Thus, OYs have the potential to be an orchestrator of mineral metabolism and bone remodelling [61, 88] and may be potential targets of osteoporosis treatment [89, 90]. However, there are many mysteries about how OYs transmit key molecules to target cells.
In addition, recent evidence implied that OYs regulate not only bone but also systemic processes of multiple organs. Sato et al. reported that ablation of OYs in mice (OY-less mice) leads to both severe lymphopenia and the loss of white adipose tissue [91]. In a separate study, Sato and his colleagues found that the long distance and systemic functions may be due to EVs secreted by OYs [92].
ECs
In the beginning, the endothelium was once considered to be just a ‘cellophane wrapper’ providing selective permeability to electrolytes and water, without any further function. As research progressed, more and more evidence has led to a more in-depth understanding of the multitudinous functions of the endothelium [93, 94]. The basic unit of the endothelium is the EC. These cells have very special properties and functions which dominate vascular biology, including fluid filtration, blood flow regulation, interaction with platelets and leukocytes, and very importantly, angiogenesis. [94,95,96].
The coupling of angiogenesis and osteogenesis plays an essential role in maintaining appropriate bone homeostasis [97, 98]. The specific performance is the result of the coincidence between vascular invasion and the appearance of OBs and OCs [97, 99]. There are highly branched, irregular, and discontinuous networks known as bone marrow capillaries, in addition to feeding arteries and draining veins [100, 101]. Recently, bone marrow capillaries have been classified as two specific subtypes—H-type vessels (or vessels strongly expressing both CD31 & Emcn) and L-type vessels [99].
Specifically, the H-type vessel may be the key to coupling, while the L-type vessel (hierarchically downstream of H-type vessels) is not associated with promoting osteogenesis and coupling [99, 102]. In addition, the ECs of H-type vessels (H-type ECs), which are found at the front of the vascular growth direction in bone tissue and express high levels of Emcn and CD31, are key in promoting osteogenesis [99, 102].
In mouse models, there is a very interesting phenomenon in which the total number of ECs in bone is not significantly different after maturation but the ratio of H-type:L-type ECs decreases with age after adolescence, and this phenomenon implies that the relationship between the transformation from H-type ECs to L-type ECs and the bone mass loss during ageing is caused by a loss of osteogenic ability [99]. Furthermore, the Notch and hypoxia-inducible factor (HIF) signalling pathways have been identified as essential signalling pathways that promote H-type vessel expansion together with the associated osteogenesis [99, 102].
Current research shows that there are two main communication approaches: a direct action and a remote action. At present, a direct action approach has only been found between ECs and BMSCs. EC-derived PDGF-BB recruits PDGF-receptor β (Rβ)–expressing BMSCs into a pericyte fate [103]. Recruited BMSCs (or pericytes), which wrap around a blood vessel like a stocking, express angiopoietin-1, which signals via Tie-2 expressed in ECs, and is essential for the integrity and stabilization of blood vessels [104]. For a remote action, early studies have mainly focussed on protein factors. ECs produce several factors that support HSCs including chemokine CXC ligand 12 (CXCL12), angiopoietin and stem cell factor (SCF) [105]. ECs also produce factors including BMPs, and have direct effects on OBs [106]. Besides, there are studies reporting that EC-derived netrin-4 participates in the regulation of OCs to maintain bone stabilization [107]. With advances in this area, EVs derived from ECs have gradually received more attention, which will be introduced later. Nonetheless, some confusing issues remain regarding how ECs communicate with other cells in bone and cooperate with each other for bone homeostasis. In future studies, there are several questions that must be answered: 1) whether there are more direct interactions between ECs and other bone cells; 2) what other important protein factors are involved; 3) the function and mechanism of EVs derived from ECs; 4) what differences exist between H-type ECs and L-type ECs in communication with other bone cells; 5) whether and how H-type ECs and L-type ECs communicate with each other.
BMSCs
In the bone marrow, BMSCs (also called bone marrow stromal cells) are mononuclear stem cells that are osteogenic precursors and can differentiate into OBs and other kinds of skeletal cells [108, 109]. There is a widely-used method to isolate BMSCs. After bone marrow cells are seeded into culture flasks, the cell population rapidly grows, with cells having a spindle-shaped fibroblast-like morphology and the potential to differentiate into osteocytes, adipocytes and chondrocytes, and this multilineage potential lasts for several passages. The multipotential cells isolated using this method are usually called ‘BMSCs’ [110, 111].
However, after years of research, some problems have received increasing attention. The in vivo BMSCs have been reported to be very different from ex vivo expanded ‘BMSCs’ [111, 112], and even multilineage potential stem cells similar to these ex vivo ‘BMSCs’ can be isolated from several tissues other than bone marrow [113, 114]. Thus, the so-called ex vivo expanded ‘BMSCs’ are best identified as skeletal stem cells (SSCs), which lack markers to identify them in situ [111, 112]. Unfortunately, these problems might mean that we have little or almost no knowledge of true in vivo BMSCs, which we had thought was very clear.
Nevertheless, optimistically speaking, there have been many achievements. In the field of application, SSCs (or what we usually called ‘BMSCs’) are very good seed cells for tissue repair and one of the representative cells used to observe the response of bone cells after repeated stimulation. The gaps in in vivo BMSC knowledge are tremendous opportunities for future research to better understand the fascinating mysteries of biology.
EVs in bone
OB-EVs
Proteins and nucleic acids, contained within OB-derived EVs (OB-EVs), play important roles in intercellular communication in bone tissue [115]. OB-EVs were once called matrix vesicles several years ago and were considered to be OB-originated EVs only recently [116,117,118].
OB-EVs contain RANKL, which can be transferred to precursors of OCs. Via receptor–ligand interaction, OB-EVs can stimulate RANKL–RANK signalling to promote osteoclast formation [119]. Inhibition of OB-EV production can prevent bone loss [120]. These results mean that OBs can stimulate the formation and activation of OCs via EVs without direct cell-to-cell contact. Interestingly, parathyroid hormone (PTH) can induce an increase in RANKL expression in OB-EVs [119]. This finding may imply that OB-EVs are participants in the regulation of hormone-related bone remodelling.
In addition to RANKL, galectin-3 has also been found to be important in OB-EVs. Weilner et al. reported that EVs from elderly people can inhibit the osteogenic ability of BMSCs unlike those from younger people [121]. Interestingly, the galectin-3 content was decreased in EVs from elderly people [121]. Through several in vitro assays, Weilner et al. proved that the intravesicular galectin-3 levels are positively correlated with osteogenic potential and are responsible for the biological responses of BMSCs to OB-EVs [121].
Recently, Ge et al. reported the results of a proteomics study on EVs derived from MC3T3 cells (mouse OBs) and showed that many proteins, which were highly enriched in EVs derived from MC3T3 cells, are enriched in osteogenesis-related pathways, including eukaryotic initiation factor 2 (EIF2) signalling, integrin signalling and mammalian target of rapamycin (mTOR) signalling [122]. EIF2 signalling participates in bone morphogenetic protein 2 (BMP2)-induced OB differentiation [123]. Integrin signalling promotes angiogenesis and thus participates in bone formation, remodelling, and fracture healing [124]. Furthermore, the activation of mTOR signalling can increase osteogenesis via the suppression of peroxisome proliferator-activated receptor-γ (PPARγ) [125]. However, proteomics studies are just for preliminary screening of key molecules, and more in-depth studies are needed in the future.
OB-EVs also contained microRNAs (miRNAs). Cui et al. found that several miRNAs in OB-EVs were increased during mineralization [126]. Through co-target analysis and in vitro assays, they found that five upregulated miRNAs (miR-667-3p, miR-6769b-5p, miR-7044-5p, miR-7668-3p and miR-874-3p) can co-target a negative regulator of the Wnt signalling pathway—Axin1—and then enhance the expression level of β-catenin [126].
OC-EVs and PreOC-EVs
Proteins and nucleic acids in EVs derived from OCs (OC-EVs) may also play an important role in bone mineral metabolism. Huynh et al. found that OC-EVs, which contain RANK on the surface, are paracrine regulators of osteoclastogenesis [127]. RANK-containing OC-EVs may target OBs via the RANK–RANKL interaction, and RANKL-containing OB-EVs may also target OCs via the RANK–RANKL interaction. RANK/RANKL may give EVs a natural targeting ability to transfer other proteins and nucleic acids and contribute to the reprogramming of target cells. In addition, RANK-containing OC-EVs may block the function of RANKL-containing OB-EVs, thus inhibiting the formation of OCs (Fig. 4) [127].
Increased levels of serum miR-214-3p contained within EVs were found in both elderly women with fractures and ovariectomized (OVX) mice [128]. Li et al. observed that OCs are the primary source of EVs containing miR-214-3p. Hence, they employed an OC-specific miR-214-3p knock-in mouse model and found that the serum level of miR-214-3p contained within EVs increased while bone formation decreased, but could be rescued by using the OC-targeted RNA antagonist antagomir-214-3p [128]. Sun et al. found similar results showing that miR-214 is responsible for the inhibition of osteogenesis by targeting OBs. With more in-depth studies, they also found that OC-EVs specifically recognized OBs through the interaction between ephrin-A2 (carried by OC-EVs) and EphA2 (on OBs) [129]. miR-214 directly targets activating transcription factor 4 (ATF4) to inhibit the activity of OBs [130]. These results implied that OCs communicate with OBs via EVs to inhibit osteogenic ability. Furthermore, miR-214 in EVs could be a possible diagnostic, prognostic and therapeutic target for osteoporosis.
Huynh et al. found RANK in OC-EVs but not in EVs derived from preOCs (preOC-EVs) [127]. More interestingly, preOC-EVs can promote the formation of OCs, but OC-EVs can inhibit the formation of OCs [127]. This phenomenon is very similar to positive and negative feedback and may be essential for the stabilization of bone mineral metabolism. Hence, it is possible that the constitution and function of preOC-EVs might be completely different from those of OC-EVs, consistent with the functional differences between preOCs and OCs. However, research is still lacking in this area, and further research is needed.
OY-EVs
As briefly described in a previous section, Sato and his colleagues found that EVs derived from OYs (OY-EVs) may transfer their components, including miRNAs, to recipient cells via circulation in the blood [92]. This finding might be the key to solving the puzzle of the mechanisms underlying the regional and systemic functions of OYs.
Morrell et al. found that mechanical stimulation upregulates the production of EVs containing bone regulatory proteins, coupled with Ca2+-dependent contractions [131]. miR-218, contained within OY-EVs, inhibits sclerostin and influences the differentiation of OBs [132]. Interestingly, the OY-derived miR-218 contained in OY-EVs can be suppressed by myostatin, which is secreted by muscles [132]. These results provide potential mechanisms for muscle–bone communications and may be one of the potential hypotheses explaining why muscle activity is essential for maintaining normal bone density. However, this research is still in its infancy. RANKL and sclerostin are key molecules derived from OYs, but there is no evidence about whether they are found in OY-EVs. Hence, there is an urgent need for proteomics and transcriptomics studies to reveal the core of OY-EVs.
EC-EVs
miR-31 is highly expressed in EC-derived EVs (EC-EVs) from elderly and osteoporotic patients [133]. miR-31 contained within EVs derived from senescent ECs was taken up by BMSCs and targeted Frizzled-3 to inhibit osteogenic ability [133]. miR-31 from within the senescent EC-EVs might be a potential valuable biomarker and therapeutic target of osteoporosis. Nonetheless, there is still not enough research. It would be better to execute a specific study about H-type EC-EVs rather than general EC-EVs.
BMSC-EVs
EVs derived from BMSCs (BMSC-EVs) are also important participants in the remodelling of bone tissue via direct regulation of the proliferation and activity of OBs [134]. Davis et al. found that oxidative stress could elevate miR-183 levels in BMSC-derived EVs (BMSC-EVs), which could induce senescence [135]. Recently, Xu et al. [136] observed that in aged rats, which exhibited increased adipogenesis and decreased osteogenesis, miR-31a-5p was significantly increased in BMSCs. Furthermore, they found that miR-31a-5p was also significantly increased in BMSC-EVs and that miR-31a-5p in BMSC-EVs was responsible for the activated osteoclastogenesis in aged rats. Thus, age-related miR-31a-5p in BMSCs could be a potential therapeutic target due to its dual functions as an inhibitor of osteogenesis and activator of osteoclastogenesis.
However, most recent studies related to BMSC-EVs have concentrated on therapeutic use under a variety of conditions, including anti-inflammation, tissue repair and tissue protection. Another focus of BMSC-EV research is the relationship between BMSC-EVs and tumours. Nevertheless, the in-depth study of BMSC-EVs in bone cell communications under physiological and pathogenic conditions is still relatively insufficient. Certainly, BMSC-EVs have a powerful potential as therapeutic drugs for regenerative medicine or targets of tumour therapy, but revealing the specific details of BMSC-EVs in the communication of other bone tissue cells is important.
Recently, the so-called ex vivo expanded ‘BMSCs’ have been identified as SSCs [111, 112]. Optimistically speaking, the massive amount of research on the therapeutic use of EVs derived from SSCs (or what we usually call ‘BMSCs’) will receive very little attention (at most, the name might change). These results also mean that we have virtually no knowledge about the in vivo function of BMSC-EVs. In other words, the lack of in vivo BMSC-EV knowledge may be a tremendous opportunity for future studies to better understand the intercellular communication among bone cells.
Discussion and outlook
With the development of research, EVs have gradually come to be thought of as correspondents or “dogrobbers” in bone tissue, the “eternal battle field” in a delicate dynamic balance of destruction and reconstruction. An in-depth understanding of the EVs in bone helps to understand both how bone maintains a delicate homeostatic balance and the pathogenesis of disease.
Furthermore, there is another mystery—how bone communicates with other systems. The conventional hypothesis is that growth factors, hormones and specific proteins such as OCN participate in the communication between bone and other systems [2,3,4, 7,8,9]. However, growth factors, hormones and specific proteins (such as Wnt) were also found to be carried by EVs in many studies [137,138,139,140]. Relative to the free state, EVs provide protection for bioactive macromolecules from a complex humoral environment [15, 141, 142]. According to this evidence, EVs may also be the “trucks” used by OCN to make it possible to influence other organs/systems, but this hypothesis needs confirmation from future studies. Several studies have shown that OCN can be carried by EVs [143, 144]. Soriano et al. found that EVs may participate directly in the process of vascular calcification via OCN [144]. However, at present, there is still too little relevant research, and current research is also not sufficiently in depth. Nevertheless, this situation means that EVs carrying bone-specific contents and their functions in other organs will be very promising future research areas. Furthermore, EVs can carry much more complex information than hormones and growth factors [145,146,147], and they have certain targeting properties to precisely regulate specific organs/systems [15, 148]. Therefore, future research can focus on EVs, and a breakthrough in this field is most likely.
Due to the limitations of current research techniques, the functional similarities and differences among sub-populations of EVs cannot be explained clearly. Moreover, many studies do not make clear distinctions. We have used the term ‘EVs’ rather than the terms of their sub-populations in this review. However, the sub-populations of EVs is a topic attracting considerable interest, and increasing attention has been paid to it [149, 150]. Increasing numbers of researchers will be involved in this area, and the understanding of both bones and the function of their EVs will be more in depth.
OBs and OCs can exist within the periosteum and the bone marrow. There are obvious differences between these two sites. OBs/OCs in the periosteum have more possibilities to communicate with tendons, muscles and nerves. In addition, OCs in the periosteum are derived from circulating monocytes [151], while OCs in the bone marrow are derived from HSCs. Although the precursors of both are the same—HSCs—whether the two have some differences has yet to be determined. In current research, there is no good distinction in the sub-population of OBs. In particular, there is a lack of in vitro research tools for studying specific subtypes of OBs in different stages, and progress in this area will bring about profound changes.
OYs, the most abundant sub-population of bone cells, are the least-studied cell type. Current research suggests that sclerostin is a very important molecule. Micro-damage causes sclerostin shut-down and triggers bone remodelling. However, it is not clear whether sclerostin is present in a free state or in EVs. We suspect that sclerostin exists in EVs and that the EVs are present in canalicular fluid. Moreover, micro-damage may block the mobility of canalicular fluid and then cause a shut-down of EV-carried sclerostin. Follow-up studies should first confirm what is affected by the micro-damage—the OYs, the mobility of canalicular fluid, or both.
There are many studies on EC-derived EVs. However, current studies have not focused on H-type ECs. Not only are there few studies on H-type ECs, but there is also almost no research on EVs derived from H-type ECs. Future research in this direction is likely to be one of the most important advances. Beyond that topic, there are large gaps with enormous research potential regarding the true nature of BMSCs, as mentioned in the previous section.
EVs have gradually become a focus of the new generation of treatment and diagnosis. With all kinds of new technologies [152], we can likely use non-invasive and convenient methods to monitor the status of bone and prevent many joint system-related diseases, and ultimately to improve human health with a high quality of life.
Conclusions
Bone is a very well-adapted tissue in a delicate dynamic balance, hosting finely-tuned bone mineral metabolic processes for bone homeostasis by collaboration or symphony among several cell types including OCs, OBs, OYs, ECs and their precursors. EVs are widely-distributed vesicles, ranging from 30 nm to 1000 nm in diameter, with targeting abilities and potential to transmit multidimensional, abundant and complicated information. In this review, we introduce the major constituent cells of bone tissues and explore the progress of current research into bone-derived EVs and then point out the problems existing in current research with possible future research directions to break through in this area.
Abbreviations
- ALP:
-
Alkaline phosphatase
- AMPK:
-
AMP-activated protein kinase
- ATF4:
-
Activating transcription factor 4
- BMP2:
-
Bone morphogenetic protein 2
- BMPs:
-
Bone morphogenetic proteins
- BMSC-EVs:
-
EVs derived from BMSCs
- BMSCs:
-
Bone mesenchymal stem cells
- BRC:
-
Bone remodelling compartment
- circRNAs:
-
Circular RNAs
- CNS:
-
Central nervous system
- Col-I:
-
Type I collagen
- CXCL12:
-
Chemokine CXC ligand 12
- EC-EVs:
-
EC-derived EVs
- ECM:
-
Extracellular matrix
- ECs:
-
Vascular endothelial cells
- EIF2:
-
Eukaryotic initiation factor 2
- Emcn:
-
Endomucin
- Erk:
-
Extracellular signal-regulated kinase
- EVs:
-
Extracellular vesicles
- HIF:
-
Hypoxia-inducible factor
- HSCs:
-
Haematopoietic stem cells
- JNK:
-
Jun N-terminal kinase
- lncRNAs:
-
Long noncoding RNAs
- MAPK:
-
Mitogen-associated protein kinase
- M-CSF:
-
Macrophage colony-stimulating factor
- miRNAs:
-
MicroRNAs
- mRNAs:
-
Messenger RNAs
- mTOR:
-
Mammalian target of rapamycin
- MVBs:
-
Multi-vesicular bodies
- NFATc1:
-
Nuclear factor of activated T-cells 1
- NF-κB:
-
Nuclear factor kappa-B
- OB-EVs:
-
OB-derived EVs
- OBs:
-
Osteoblasts
- OC-EVs:
-
EVs derived from OCs
- OCN:
-
Osteocalcin
- OCs:
-
Osteoclasts
- OVX:
-
Ovariectomized
- OY-EVs:
-
EVs derived from OYs
- OYs:
-
Osteocytes
- PDGF-BB:
-
Platelet-derived growth factor-BB
- PDGF-Rβ:
-
Platelet-derived growth factor-receptor β
- PI3K:
-
Phosphoinositide 3-kinase
- PKB:
-
Protein kinase B
- PPARγ:
-
Peroxisome proliferator-activated receptor-γ
- preOC-EVs:
-
EVs derived from preOCs
- preOCs:
-
Pre-osteoclasts
- PTH:
-
Parathyroid hormone
- RANK:
-
Receptor activator of nuclear factor kappa-B
- RANKL:
-
Receptor activator of nuclear factor kappa-B ligand
- SCF:
-
Stem cell factor
- SSCs:
-
Skeletal stem cells
- TRAF6:
-
Tumour necrosis factor receptor-associated factor 6
- TRAP+:
-
Tartrate-resistant acid phosphatase-positive
- Wnt:
-
Wingless-related integration site
References
Cappariello A, Ponzetti M, Rucci N. The “soft” side of the bone: unveiling its endocrine functions. Horm Mol Biol Clin Investig. 2016;28:5–20.
Fernandez-Real JM, Izquierdo M, Ortega F, Gorostiaga E, Gomez-Ambrosi J, Moreno-Navarrete JM, Fruhbeck G, Martinez C, Idoate F, Salvador J, et al. The relationship of serum osteocalcin concentration to insulin secretion, sensitivity, and disposal with hypocaloric diet and resistance training. J Clin Endocrinol Metab. 2009;94:237–45.
Clemens TL, Karsenty G. The osteoblast: an insulin target cell controlling glucose homeostasis. J Bone Miner Res. 2011;26:677–80.
Breuil V, Euller-Ziegler L. Gonadal dysgenesis and bone metabolism. Joint Bone Spine. 2001;68:26–33.
Martin TJ. Parathyroid hormone-related protein, its regulation of cartilage and bone development, and role in treating bone diseases. Physiol Rev. 2016;96:831–71.
Spohn SN, Mawe GM. Non-conventional features of peripheral serotonin signalling - the gut and beyond. Nat Rev Gastroenterol Hepatol. 2017;14:412–20.
Xiao W, Wang Y, Pacios S, Li S, Graves DT. Cellular and molecular aspects of bone remodeling. Front Oral Biol. 2016;18:9–16.
Delgado-Calle J, Tu X, Pacheco-Costa R, McAndrews K, Edwards R, Pellegrini GG, Kuhlenschmidt K, Olivos N, Robling A, Peacock M, et al. Control of bone anabolism in response to mechanical loading and PTH by distinct mechanisms downstream of the PTH receptor. J Bone Miner Res. 2017;32:522–35.
Li X, Ye JX, Xu MH, Zhao MD, Yuan FL. Evidence that activation of ASIC1a by acidosis increases osteoclast migration and adhesion by modulating integrin/Pyk2/Src signaling pathway. Osteoporos Int. 2017;28:2221–31.
Henriksen K, Karsdal MA, Martin TJ. Osteoclast-derived coupling factors in bone remodeling. Calcif Tissue Int. 2014;94:88–97.
Miyazaki T, Tokimura F, Tanaka S. A review of denosumab for the treatment of osteoporosis. Patient Prefer Adherence. 2014;8:463–71.
Karner CM, Long F. Wnt signaling and cellular metabolism in osteoblasts. Cell Mol Life Sci. 2017;74:1649–57.
Matsuo K, Irie N. Osteoclast-osteoblast communication. Arch Biochem Biophys. 2008;473:201–9.
Tao SC, Guo SC, Zhang CQ. Platelet-derived extracellular vesicles: an emerging therapeutic approach. Int J Biol Sci. 2017;13:828–34.
Tao SC, Guo SC, Zhang CQ. Modularized extracellular vesicles: the Dawn of prospective personalized and precision medicine. Adv Sci (Weinh). 2018;5:1700449.
Yanez-Mo M, Siljander PR, Andreu Z, Zavec AB, Borras FE, Buzas EI, Buzas K, Casal E, Cappello F, Carvalho J, et al. Biological properties of extracellular vesicles and their physiological functions. J Extracell Vesicles. 2015;4:27066.
Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol. 2013;200:373–83.
Schorey JS, Cheng Y, Singh PP, Smith VL. Exosomes and other extracellular vesicles in host-pathogen interactions. EMBO Rep. 2015;16:24–43.
Deatherage BL, Cookson BT. Membrane vesicle release in bacteria, eukaryotes, and archaea: a conserved yet underappreciated aspect of microbial life. Infect Immun. 2012;80:1948–57.
Robinson DG, Ding Y, Jiang L. Unconventional protein secretion in plants: a critical assessment. Protoplasma. 2016;253:31–43.
Keller S, Ridinger J, Rupp AK, Janssen JW, Altevogt P. Body fluid derived exosomes as a novel template for clinical diagnostics. J Transl Med. 2011;9:86.
Thery C, Amigorena S, Raposo G, Clayton A. Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Curr Protoc Cell Biol. 2006;30:3.22.1–29.
Lasser C, Alikhani VS, Ekstrom K, Eldh M, Paredes PT, Bossios A, Sjostrand M, Gabrielsson S, Lotvall J, Valadi H. Human saliva, plasma and breast milk exosomes contain RNA: uptake by macrophages. J Transl Med. 2011;9:9.
Colombo M, Raposo G, Thery C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev Cell Dev Biol. 2014;30:255–89.
Tkach M, Thery C. Communication by extracellular vesicles: where we are and where we need to go. Cell. 2016;164:1226–32.
Capulli M, Paone R, Rucci N. Osteoblast and osteocyte: games without frontiers. Arch Biochem Biophys. 2014;561:3–12.
Grigoriadis AE, Heersche JN, Aubin JE. Differentiation of muscle, fat, cartilage, and bone from progenitor cells present in a bone-derived clonal cell population: effect of dexamethasone. J Cell Biol. 1988;106:2139–51.
Long F. Building strong bones: molecular regulation of the osteoblast lineage. Nat Rev Mol Cell Biol. 2011;13:27–38.
Ducy P, Zhang R, Geoffroy V, Ridall AL, Karsenty G. Osf2/Cbfa1: a transcriptional activator of osteoblast differentiation. Cell. 1997;89:747–54.
Lee B, Thirunavukkarasu K, Zhou L, Pastore L, Baldini A, Hecht J, Geoffroy V, Ducy P, Karsenty G. Missense mutations abolishing DNA binding of the osteoblast-specific transcription factor OSF2/CBFA1 in cleidocranial dysplasia. Nat Genet. 1997;16:307–10.
Komori T, Yagi H, Nomura S, Yamaguchi A, Sasaki K, Deguchi K, Shimizu Y, Bronson RT, Gao YH, Inada M, et al. Targeted disruption of Cbfa1 results in a complete lack of bone formation owing to maturational arrest of osteoblasts. Cell. 1997;89:755–64.
Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, de Crombrugghe B. The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell. 2002;108:17–29.
Zhong Z, Ethen NJ, Williams BO. WNT signaling in bone development and homeostasis. Wiley Interdiscip Rev Dev Biol. 2014;3:489–500.
McCarthy TL, Centrella M, Canalis E. Parathyroid hormone enhances the transcript and polypeptide levels of insulin-like growth factor I in osteoblast-enriched cultures from fetal rat bone. Endocrinology. 1989;124:1247–53.
Robey PG, Termine JD. Human bone cells in vitro. Calcif Tissue Int. 1985;37:453–60.
Marie PJ, Cohen-Solal M. The expanding life and functions of osteogenic cells: from simple bone-making cells to multifunctional cells and beyond. J Bone Miner Res. 2018;33:199–210.
Xing L, Schwarz EM, Boyce BF. Osteoclast precursors, RANKL/RANK, and immunology. Immunol Rev. 2005;208:19–29.
Del Fattore A, Teti A, Rucci N. Bone cells and the mechanisms of bone remodelling. Front Biosci (Elite Ed). 2012;4:2302–21.
Ishii M, Saeki Y. Osteoclast cell fusion: mechanisms and molecules. Mod Rheumatol. 2008;18:220–7.
Lee SH, Rho J, Jeong D, Sul JY, Kim T, Kim N, Kang JS, Miyamoto T, Suda T, Lee SK, et al. V-ATPase V0 subunit d2-deficient mice exhibit impaired osteoclast fusion and increased bone formation. Nat Med. 2006;12:1403–9.
Hofbauer LC, Heufelder AE. Osteopetrosis in cathepsin K-deficient mice. Eur J Endocrinol. 1999;140:376–7.
Ta HM, Nguyen GT, Jin HM, Choi J, Park H, Kim N, Hwang HY, Kim KK. Structure-based development of a receptor activator of nuclear factor-kappaB ligand (RANKL) inhibitor peptide and molecular basis for osteopetrosis. Proc Natl Acad Sci U S A. 2010;107:20281–6.
Ochotny N, Flenniken AM, Owen C, Voronov I, Zirngibl RA, Osborne LR, Henderson JE, Adamson SL, Rossant J, Manolson MF, Aubin JE. The V-ATPase a3 subunit mutation R740S is dominant negative and results in osteopetrosis in mice. J Bone Miner Res. 2011;26:1484–93.
Maruyama T, Fukushima H, Nakao K, Shin M, Yasuda H, Weih F, Doi T, Aoki K, Alles N, Ohya K, et al. Processing of the NF-kappa B2 precursor p100 to p52 is critical for RANKL-induced osteoclast differentiation. J Bone Miner Res. 2010;25:1058–67.
Novack DV, Yin L, Hagen-Stapleton A, Schreiber RD, Goeddel DV, Ross FP, Teitelbaum SL. The IkappaB function of NF-kappaB2 p100 controls stimulated osteoclastogenesis. J Exp Med. 2003;198:771–81.
Grigoriadis AE, Wang ZQ, Cecchini MG, Hofstetter W, Felix R, Fleisch HA, Wagner EF. C-Fos: a key regulator of osteoclast-macrophage lineage determination and bone remodeling. Science. 1994;266:443–8.
Kashiwada M, Shirakata Y, Inoue JI, Nakano H, Okazaki K, Okumura K, Yamamoto T, Nagaoka H, Takemori T. Tumor necrosis factor receptor-associated factor 6 (TRAF6) stimulates extracellular signal-regulated kinase (ERK) activity in CD40 signaling along a ras-independent pathway. J Exp Med. 1998;187:237–44.
Matsumoto M, Sudo T, Saito T, Osada H, Tsujimoto M. Involvement of p38 mitogen-activated protein kinase signaling pathway in osteoclastogenesis mediated by receptor activator of NF-kappa B ligand (RANKL). J Biol Chem. 2000;275:31155–61.
Keshet Y, Seger R. The MAP kinase signaling cascades: a system of hundreds of components regulates a diverse array of physiological functions. Methods Mol Biol. 2010;661:3–38.
Park KH, Park B, Yoon DS, Kwon SH, Shin DM, Lee JW, Lee HG, Shim JH, Park JH, Lee JM. Zinc inhibits osteoclast differentiation by suppression of Ca2+-Calcineurin-NFATc1 signaling pathway. Cell Commun Signal. 2013;11:74.
Sato K, Suematsu A, Nakashima T, Takemoto-Kimura S, Aoki K, Morishita Y, Asahara H, Ohya K, Yamaguchi A, Takai T, et al. Regulation of osteoclast differentiation and function by the CaMK-CREB pathway. Nat Med. 2006;12:1410–6.
Asagiri M, Sato K, Usami T, Ochi S, Nishina H, Yoshida H, Morita I, Wagner EF, Mak TW, Serfling E, Takayanagi H. Autoamplification of NFATc1 expression determines its essential role in bone homeostasis. J Exp Med. 2005;202:1261–9.
Kang H, Viollet B, Wu D. Genetic deletion of catalytic subunits of AMP-activated protein kinase increases osteoclasts and reduces bone mass in young adult mice. J Biol Chem. 2013;288:12187–96.
Baroukh B, Cherruau M, Dobigny C, Guez D, Saffar JL. Osteoclasts differentiate from resident precursors in an in vivo model of synchronized resorption: a temporal and spatial study in rats. Bone. 2000;27:627–34.
Xie H, Cui Z, Wang L, Xia Z, Hu Y, Xian L, Li C, Xie L, Crane J, Wan M, et al. PDGF-BB secreted by preosteoclasts induces angiogenesis during coupling with osteogenesis. Nat Med. 2014;20:1270–8.
Ochareon P, Herring SW. Cell replication in craniofacial periosteum: appositional vs. resorptive sites. J Anat. 2011;218:285–97.
Ross FP. M-CSF, c-Fms, and signaling in osteoclasts and their precursors. Ann N Y Acad Sci. 2006;1068:110–6.
Bonewald LF. Osteocytes as dynamic multifunctional cells. Ann N Y Acad Sci. 2007;1116:281–90.
Burgers TA, Williams BO. Regulation of Wnt/beta-catenin signaling within and from osteocytes. Bone. 2013;54:244–9.
Kalajzic I, Matthews BG, Torreggiani E, Harris MA, Divieti Pajevic P, Harris SE. In vitro and in vivo approaches to study osteocyte biology. Bone. 2013;54:296–306.
Bonewald LF. The amazing osteocyte. J Bone Miner Res. 2011;26:229–38.
Noble BS. The osteocyte lineage. Arch Biochem Biophys. 2008;473:106–11.
Knothe Tate ML, Niederer P, Knothe U. In vivo tracer transport through the lacunocanalicular system of rat bone in an environment devoid of mechanical loading. Bone. 1998;22:107–17.
Aarden EM, Burger EH, Nijweide PJ. Function of osteocytes in bone. J Cell Biochem. 1994;55:287–99.
Taylor D. Bone maintenance and remodeling: a control system based on fatigue damage. J Orthop Res. 1997;15:601–6.
Burr DB. Targeted and nontargeted remodeling. Bone. 2002;30:2–4.
Parfitt AM. Targeted and nontargeted bone remodeling: relationship to basic multicellular unit origination and progression. Bone. 2002;30:5–7.
Seeman E. Bone modeling and remodeling. Crit Rev Eukaryot Gene Expr. 2009;19:219–33.
Robling AG, Turner CH. Mechanical signaling for bone modeling and remodeling. Crit Rev Eukaryot Gene Expr. 2009;19:319–38.
Burra S, Nicolella DP, Francis WL, Freitas CJ, Mueschke NJ, Poole K, Jiang JX. Dendritic processes of osteocytes are mechanotransducers that induce the opening of hemichannels. Proc Natl Acad Sci U S A. 2010;107:13648–53.
Kerschnitzki M, Wagermaier W, Roschger P, Seto J, Shahar R, Duda GN, Mundlos S, Fratzl P. The organization of the osteocyte network mirrors the extracellular matrix orientation in bone. J Struct Biol. 2011;173:303–11.
Batra N, Riquelme MA, Burra S, Kar R, Gu S, Jiang JX. Direct regulation of osteocytic connexin 43 hemichannels through AKT kinase activated by mechanical stimulation. J Biol Chem. 2014;289:10582–91.
Frost HM. Micropetrosis. J Bone Joint Surg Am. 1960;42-A:144–50.
Verborgt O, Gibson GJ, Schaffler MB. Loss of osteocyte integrity in association with microdamage and bone remodeling after fatigue in vivo. J Bone Miner Res. 2000;15:60–7.
Burr DB. Repair mechanisms for microdamage in bone. J Bone Miner Res. 2014;29:2534–6.
McClung MR, Grauer A, Boonen S, Bolognese MA, Brown JP, Diez-Perez A, Langdahl BL, Reginster JY, Zanchetta JR, Wasserman SM, et al. Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med. 2014;370:412–20.
Tu X, Delgado-Calle J, Condon KW, Maycas M, Zhang H, Carlesso N, Taketo MM, Burr DB, Plotkin LI, Bellido T. Osteocytes mediate the anabolic actions of canonical Wnt/beta-catenin signaling in bone. Proc Natl Acad Sci U S A. 2015;112:E478–86.
O'Brien CA, Nakashima T, Takayanagi H. Osteocyte control of osteoclastogenesis. Bone. 2013;54:258–63.
Nakashima T, Hayashi M, Fukunaga T, Kurata K, Oh-Hora M, Feng JQ, Bonewald LF, Kodama T, Wutz A, Wagner EF, et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med. 2011;17:1231–4.
Xiong J, Onal M, Jilka RL, Weinstein RS, Manolagas SC, O'Brien CA. Matrix-embedded cells control osteoclast formation. Nat Med. 2011;17:1235–41.
Wijenayaka AR, Kogawa M, Lim HP, Bonewald LF, Findlay DM, Atkins GJ. Sclerostin stimulates osteocyte support of osteoclast activity by a RANKL-dependent pathway. PLoS One. 2011;6:e25900.
Li X, Ominsky MS, Niu QT, Sun N, Daugherty B, D'Agostin D, Kurahara C, Gao Y, Cao J, Gong J, et al. Targeted deletion of the sclerostin gene in mice results in increased bone formation and bone strength. J Bone Miner Res. 2008;23:860–9.
Lara-Castillo N, Kim-Weroha NA, Kamel MA, Javaheri B, Ellies DL, Krumlauf RE, Thiagarajan G, Johnson ML. In vivo mechanical loading rapidly activates beta-catenin signaling in osteocytes through a prostaglandin mediated mechanism. Bone. 2015;76:58–66.
Spatz JM, Wein MN, Gooi JH, Qu Y, Garr JL, Liu S, Barry KJ, Uda Y, Lai F, Dedic C, et al. The Wnt inhibitor Sclerostin is up-regulated by mechanical unloading in osteocytes in vitro. J Biol Chem. 2015;290:16744–58.
Robling AG, Bellido T, Turner CH. Mechanical stimulation in vivo reduces osteocyte expression of sclerostin. J Musculoskelet Neuronal Interact. 2006;6:354.
Morse LR, Sudhakar S, Danilack V, Tun C, Lazzari A, Gagnon DR, Garshick E, Battaglino RA. Association between sclerostin and bone density in chronic spinal cord injury. J Bone Miner Res. 2012;27:352–9.
Prideaux M, Findlay DM, Atkins GJ. Osteocytes: the master cells in bone remodelling. Curr Opin Pharmacol. 2016;28:24–30.
Jacobs CR, Temiyasathit S, Castillo AB. Osteocyte mechanobiology and pericellular mechanics. Annu Rev Biomed Eng. 2010;12:369–400.
Spyropoulou A, Karamesinis K, Basdra EK. Mechanotransduction pathways in bone pathobiology. Biochim Biophys Acta. 2015;1852:1700–8.
Khosla S, Shane E. A crisis in the treatment of osteoporosis. J Bone Miner Res. 2016;31:1485–7.
Sato M, Asada N, Kawano Y, Wakahashi K, Minagawa K, Kawano H, Sada A, Ikeda K, Matsui T, Katayama Y. Osteocytes regulate primary lymphoid organs and fat metabolism. Cell Metab. 2013;18:749–58.
Sato M, Suzuki T, Kawano M, Tamura M. Circulating osteocyte-derived exosomes contain miRNAs which are enriched in exosomes from MLO-Y4 cells. Biomed Rep. 2017;6:223–31.
Cines DB, Pollak ES, Buck CA, Loscalzo J, Zimmerman GA, McEver RP, Pober JS, Wick TM, Konkle BA, Schwartz BS, et al. Endothelial cells in physiology and in the pathophysiology of vascular disorders. Blood. 1998;91:3527–61.
Rajendran P, Rengarajan T, Thangavel J, Nishigaki Y, Sakthisekaran D, Sethi G, Nishigaki I. The vascular endothelium and human diseases. Int J Biol Sci. 2013;9:1057–69.
Durand MJ, Gutterman DD. Diversity in mechanisms of endothelium-dependent vasodilation in health and disease. Microcirculation. 2013;20:239–47.
Verhamme P, Hoylaerts MF. The pivotal role of the endothelium in haemostasis and thrombosis. Acta Clin Belg. 2006;61:213–9.
Portal-Nunez S, Lozano D, Esbrit P. Role of angiogenesis on bone formation. Histol Histopathol. 2012;27:559–66.
Brandi ML, Collin-Osdoby P. Vascular biology and the skeleton. J Bone Miner Res. 2006;21:183–92.
Kusumbe AP, Ramasamy SK, Adams RH. Coupling of angiogenesis and osteogenesis by a specific vessel subtype in bone. Nature. 2014;507:323–8.
Pannarale L, Morini S, D'Ubaldo E, Gaudio E, Marinozzi G. SEM corrosion-casts study of the microcirculation of the flat bones in the rat. Anat Rec. 1997;247:462–71.
Zamboni L, Pease DC. The vascular bed of red bone marrow. J Ultrastruct Res. 1961;5:65–85.
Ramasamy SK, Kusumbe AP, Wang L, Adams RH. Endothelial notch activity promotes angiogenesis and osteogenesis in bone. Nature. 2014;507:376–80.
Lindahl P, Johansson BR, Leveen P, Betsholtz C. Pericyte loss and microaneurysm formation in PDGF-B-deficient mice. Science. 1997;277:242–5.
Suri C, Jones PF, Patan S, Bartunkova S, Maisonpierre PC, Davis S, Sato TN, Yancopoulos GD. Requisite role of angiopoietin-1, a ligand for the TIE2 receptor, during embryonic angiogenesis. Cell. 1996;87:1171–80.
Anthony BA, Link DC. Regulation of hematopoietic stem cells by bone marrow stromal cells. Trends Immunol. 2014;35:32–7.
Hankenson KD, Gagne K, Shaughnessy M. Extracellular signaling molecules to promote fracture healing and bone regeneration. Adv Drug Deliv Rev. 2015;94:3–12.
Enoki Y, Sato T, Tanaka S, Iwata T, Usui M, Takeda S, Kokabu S, Matsumoto M, Okubo M, Nakashima K, et al. Netrin-4 derived from murine vascular endothelial cells inhibits osteoclast differentiation in vitro and prevents bone loss in vivo. FEBS Lett. 2014;588:2262–9.
Friedenstein AJ, Chailakhjan RK, Lalykina KS. The development of fibroblast colonies in monolayer cultures of Guinea-pig bone marrow and spleen cells. Cell Tissue Kinet. 1970;3:393–403.
Owen M, Friedenstein AJ. Stromal stem cells: marrow-derived osteogenic precursors. CIBA Found Symp. 1988;136:42–60.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–7.
Bianco P, Robey PG, Simmons PJ. Mesenchymal stem cells: revisiting history, concepts, and assays. Cell Stem Cell. 2008;2:313–9.
Bianco P, Cao X, Frenette PS, Mao JJ, Robey PG, Simmons PJ, Wang CY. The meaning, the sense and the significance: translating the science of mesenchymal stem cells into medicine. Nat Med. 2013;19:35–42.
Jiang Y, Vaessen B, Lenvik T, Blackstad M, Reyes M, Verfaillie CM. Multipotent progenitor cells can be isolated from postnatal murine bone marrow, muscle,and brain. Exp Hematol. 2002;30:896–904.
Beltrami AP, Cesselli D, Bergamin N, Marcon P, Rigo S, Puppato E, D'Aurizio F, Verardo R, Piazza S, Pignatelli A, et al. Multipotent cells can be generated in vitro from several adult human organs (heart, liver, and bone marrow). Blood. 2007;110:3438–46.
Yin P, Lv H, Li Y, Deng Y, Zhang L, Tang P. Exosome-mediated genetic information transfer, a missing piece of osteoblast-osteoclast communication puzzle. Front Endocrinol (Lausanne). 2017;8:336.
Anderson HC, Garimella R, Tague SE. The role of matrix vesicles in growth plate development and biomineralization. Front Biosci. 2005;10:822–37.
Morhayim J, van de Peppel J, Demmers JA, Kocer G, Nigg AL, van Driel M, Chiba H, van Leeuwen JP. Proteomic signatures of extracellular vesicles secreted by nonmineralizing and mineralizing human osteoblasts and stimulation of tumor cell growth. FASEB J. 2015;29:274–85.
Shapiro IM, Landis WJ, Risbud MV. Matrix vesicles: are they anchored exosomes? Bone. 2015;79:29–36.
Deng L, Wang Y, Peng Y, Wu Y, Ding Y, Jiang Y, Shen Z, Fu Q. Osteoblast-derived microvesicles: a novel mechanism for communication between osteoblasts and osteoclasts. Bone. 2015;79:37–42.
Deng L, Peng Y, Jiang Y, Wu Y, Ding Y, Wang Y, Xu D, Fu Q. Imipramine protects against bone loss by inhibition of osteoblast-derived microvesicles. Int J Mol Sci. 2017;18(5):1013.
Weilner S, Keider V, Winter M, Harreither E, Salzer B, Weiss F, Schraml E, Messner P, Pietschmann P, Hildner F, et al. Vesicular Galectin-3 levels decrease with donor age and contribute to the reduced osteo-inductive potential of human plasma derived extracellular vesicles. Aging (Albany NY). 2016;8:16–33.
Ge M, Ke R, Cai T, Yang J, Mu X. Identification and proteomic analysis of osteoblast-derived exosomes. Biochem Biophys Res Commun. 2015;467:27–32.
Saito A, Ochiai K, Kondo S, Tsumagari K, Murakami T, Cavener DR, Imaizumi K. Endoplasmic reticulum stress response mediated by the PERK-eIF2(alpha)-ATF4 pathway is involved in osteoblast differentiation induced by BMP2. J Biol Chem. 2011;286:4809–18.
Chim SM, Kuek V, Chow ST, Lim BS, Tickner J, Zhao J, Chung R, Su YW, Zhang G, Erber W, et al. EGFL7 is expressed in bone microenvironment and promotes angiogenesis via ERK, STAT3, and integrin signaling cascades. J Cell Physiol. 2015;230:82–94.
Sun H, Kim JK, Mortensen R, Mutyaba LP, Hankenson KD, Krebsbach PH. Osteoblast-targeted suppression of PPARgamma increases osteogenesis through activation of mTOR signaling. Stem Cells. 2013;31:2183–92.
Cui Y, Luan J, Li H, Zhou X, Han J. Exosomes derived from mineralizing osteoblasts promote ST2 cell osteogenic differentiation by alteration of microRNA expression. FEBS Lett. 2016;590:185–92.
Huynh N, VonMoss L, Smith D, Rahman I, Felemban MF, Zuo J, Rody WJ Jr, McHugh KP, Holliday LS. Characterization of regulatory extracellular vesicles from osteoclasts. J Dent Res. 2016;95:673–9.
Li D, Liu J, Guo B, Liang C, Dang L, Lu C, He X, Cheung HY, Xu L, Lu C, et al. Osteoclast-derived exosomal miR-214-3p inhibits osteoblastic bone formation. Nat Commun. 2016;7:10872.
Sun W, Zhao C, Li Y, Wang L, Nie G, Peng J, Wang A, Zhang P, Tian W, Li Q, et al. Osteoclast-derived microRNA-containing exosomes selectively inhibit osteoblast activity. Cell Discov. 2016;2:16015.
Wang X, Guo B, Li Q, Peng J, Yang Z, Wang A, Li D, Hou Z, Lv K, Kan G, et al. miR-214 targets ATF4 to inhibit bone formation. Nat Med. 2013;19:93–100.
Morrell AE, Brown GN, Robinson ST, Sattler RL, Baik AD, Zhen G, Cao X, Bonewald LF, Jin W, Kam LC, Guo XE. Mechanically induced ca(2+) oscillations in osteocytes release extracellular vesicles and enhance bone formation. Bone Res. 2018;6:6.
Qin Y, Peng Y, Zhao W, Pan J, Ksiezak-Reding H, Cardozo C, Wu Y, Divieti Pajevic P, Bonewald LF, Bauman WA, Qin W. Myostatin inhibits osteoblastic differentiation by suppressing osteocyte-derived exosomal microRNA-218: a novel mechanism in muscle-bone communication. J Biol Chem. 2017;292:11021–33.
Weilner S, Schraml E, Wieser M, Messner P, Schneider K, Wassermann K, Micutkova L, Fortschegger K, Maier AB, Westendorp R, et al. Secreted microvesicular miR-31 inhibits osteogenic differentiation of mesenchymal stem cells. Aging Cell. 2016;15:744–54.
Qin Y, Wang L, Gao Z, Chen G, Zhang C. Bone marrow stromal/stem cell-derived extracellular vesicles regulate osteoblast activity and differentiation in vitro and promote bone regeneration in vivo. Sci Rep. 2016;6:21961.
Davis C, Dukes A, Drewry M, Helwa I, Johnson MH, Isales CM, Hill WD, Liu Y, Shi X, Fulzele S, Hamrick MW. MicroRNA-183-5p increases with age in bone-derived extracellular vesicles, suppresses bone marrow stromal (stem) cell proliferation, and induces stem cell senescence. Tissue Eng Part A. 2017;23:1231–40.
Xu R, Shen X, Si Y, Fu Y, Zhu W, Xiao T, Fu Z, Zhang P, Cheng J, Jiang H. MicroRNA-31a-5p from aging BMSCs links bone formation and resorption in the aged bone marrow microenvironment. Aging Cell. 2018;17:e12794.
Javeed N, Sagar G, Dutta SK, Smyrk TC, Lau JS, Bhattacharya S, Truty M, Petersen GM, Kaufman RJ, Chari ST, Mukhopadhyay D. Pancreatic Cancer-derived exosomes cause paraneoplastic beta-cell dysfunction. Clin Cancer Res. 2015;21:1722–33.
Guo SC, Tao SC, Yin WJ, Qi X, Yuan T, Zhang CQ. Exosomes derived from platelet-rich plasma promote the re-epithelization of chronic cutaneous wounds via activation of YAP in a diabetic rat model. Theranostics. 2017;7:81–96.
Tao SC, Yuan T, Rui BY, Zhu ZZ, Guo SC, Zhang CQ. Exosomes derived from human platelet-rich plasma prevent apoptosis induced by glucocorticoid-associated endoplasmic reticulum stress in rat osteonecrosis of the femoral head via the Akt/bad/Bcl-2 signal pathway. Theranostics. 2017;7:733–50.
Gross JC, Chaudhary V, Bartscherer K, Boutros M. Active Wnt proteins are secreted on exosomes. Nat Cell Biol. 2012;14:1036–45.
Tao SC, Guo SC, Li M, Ke QF, Guo YP, Zhang CQ. Chitosan wound dressings incorporating exosomes derived from MicroRNA-126-overexpressing synovium mesenchymal stem cells provide sustained release of exosomes and heal full-thickness skin defects in a diabetic rat model. Stem Cells Transl Med. 2017;6:736–47.
Tao SC, Yuan T, Zhang YL, Yin WJ, Guo SC, Zhang CQ. Exosomes derived from miR-140-5p-overexpressing human synovial mesenchymal stem cells enhance cartilage tissue regeneration and prevent osteoarthritis of the knee in a rat model. Theranostics. 2017;7:180–95.
Koyama Y, Ito T, Hasegawa A, Eriguchi M, Inaba T, Ushigusa T, Sugiura K. Exosomes derived from tumor cells genetically modified to express Mycobacterium tuberculosis antigen: a novel vaccine for cancer therapy. Biotechnol Lett. 2016;38:1857–66.
Soriano S, Carmona A, Trivino F, Rodriguez M, Alvarez-Benito M, Martin-Malo A, Alvarez-Lara MA, Ramirez R, Aljama P, Carracedo J. Endothelial damage and vascular calcification in patients with chronic kidney disease. Am J Physiol Renal Physiol. 2014;307:F1302–11.
Guay C, Regazzi R. Exosomes as new players in metabolic organ cross-talk. Diabetes Obes Metab. 2017;19(Suppl 1):137–46.
Sagar G, Sah RP, Javeed N, Dutta SK, Smyrk TC, Lau JS, Giorgadze N, Tchkonia T, Kirkland JL, Chari ST, Mukhopadhyay D. Pathogenesis of pancreatic cancer exosome-induced lipolysis in adipose tissue. Gut. 2016;65:1165–74.
Tao SC, Guo SC. Extracellular vesicles: potential participants in circadian rhythm synchronization. Int J Biol Sci. 2018;14:1610–20.
Tao SC, Rui BY, Wang QY, Zhou D, Zhang Y, Guo SC. Extracellular vesicle-mimetic nanovesicles transport LncRNA-H19 as competing endogenous RNA for the treatment of diabetic wounds. Drug Deliv. 2018;25:241–55.
Kowal J, Arras G, Colombo M, Jouve M, Morath JP, Primdal-Bengtson B, Dingli F, Loew D, Tkach M, Thery C. Proteomic comparison defines novel markers to characterize heterogeneous populations of extracellular vesicle subtypes. Proc Natl Acad Sci U S A. 2016;113:E968–77.
Tkach M, Kowal J, Zucchetti AE, Enserink L, Jouve M, Lankar D, Saitakis M, Martin-Jaular L, Thery C. Qualitative differences in T-cell activation by dendritic cell-derived extracellular vesicle subtypes. EMBO J. 2017;36:3012–28.
Zhou Y, Deng HW, Shen H. Circulating monocytes: an appropriate model for bone-related study. Osteoporos Int. 2015;26:2561–72.
Guo S-C, Tao S-C, Dawn H. Microfluidics-based on-a-chip systems for isolating and analysing extracellular vesicles. Journal of Extracellular Vesicles. 2018;7:1508271.
Ethical approval and consent to participate
Not applicable.
Funding
The National Natural Science Foundation of China [Nos. 81871834, 81802226 and 81301589], and Shanghai Jiao Tong University K.C.Wong Medical Fellowship Fund supported this work.
Author information
Authors and Affiliations
Contributions
S-CT planned and wrote this manuscript. S-CG helped with planning and writing. Both authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declared that they no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tao, SC., Guo, SC. Extracellular vesicles in bone: “dogrobbers” in the “eternal battle field”. Cell Commun Signal 17, 6 (2019). https://doi.org/10.1186/s12964-019-0319-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12964-019-0319-5