Abstract
Background
Public hospitals are facing a critical shortage of health workers. The area-based network consolidations could be the solution to increase the system capacity for human resources by improving local allocative efficiency.
Methods
This study develops counterfactual simulations for area-based network allocations for the health workforce in 10500 public hospitals in Thailand and examines improvements in allocative efficiency from the health workforce redistribution at different administrative levels such as sub-districts, districts, provinces, and health service areas. The workload per worker is calculated from the output measured by numbers of outpatient and inpatient cases and the input measured by numbers of health workers. Both output and input are weighted with their economic values and controlled for heterogeneity through regression analysis. Finally, this study compares the workload per worker and economic valuation of the area-based networks or ex-ante scenarios with the hospital-level or status quo scenario.
Results
Network consolidations of the sub-district primary-level hospitals within the same district could reduce workload per worker by seven percentage points. Another practical policy option is to consolidate similar hospital levels such as primary, first-level secondary, and mid-level secondary hospitals altogether within the same province which could result in the reduction of the workload per worker by 6–7 percentage points. The total economic value gained from consolidating similar hospital levels within the same province is about 15–18 percentage points of total labor cost in the primary hospitals.
Conclusion
This study illustrates the improvement in allocative efficiency of the health workforce in public hospitals from the area-based network consolidations. The results provide an insightful example of economic gains from efficiently reallocating the medical workforce within the same local areas. Major reforms are required such that the health care delivery units can automate their resources in corresponding to the population's health needs through a strengthening gatekeeping system.
Similar content being viewed by others
Introduction
An important goal of human resource planning in a health system is to settle an adequate health workforce with balanced allocation in any specific administrative areas [1]. The major challenges of health resource allocation in Thailand are the scarcity of health workforce and the inequitable access to quality health care [2]. The country is facing the problem of higher demand for health services that exceeds the available capacity of the public health system [3].
Even though the geographical allocations of health workers in Thailand have been improved significantly over the last three decades with higher workforce availability, the number of health workers is still lower than the official requirement, and the public hospitals under the Office of the Permanent Secretary in the Ministry of Public Health (MOPH) still have chronic shortages in the health workforce. In addition to the insufficient budget [4], there are geographical allocation issues such that the health workforce is more concentrated in Bangkok and big cities and the inequity gap in proportions of the targeted population to medical doctors could reach almost ten times differential among provinces [5].
In particular, the shortage of nurses has been a critical issue for the Thai public health system, and the problem could be more severe [6, 7]. Unfortunately, the nurse resignations are quite consecutively high due to the fact that the health system cannot retain skilled and experienced nurses, not because of the inadequate production of nurses [8]. A study of 19 912 registered nurses revealed that 10 percent of the surveyed sample would like to quit their career within the next 2 years [9]. Another study [10] found that the young and less-skilled nurses have a stronger intention of resignation for having less time off, less job satisfaction, and higher stress. Other studies reported similar conclusions from community hospitals [11], a tertiary care hospital [12], and a university hospital [13].
In the future, Thailand will be facing higher demand for the health workforce in primary [14] and tertiary [15] hospital levels. The projections of demand and supply for medical specialists demonstrated severe shortages in almost all specialized medical professions as the consequences of the aged society [16]. Therefore, it is an urgency for the government to manage health workforce in order to improve allocative efficiency and achieve the desirable population health objectives.
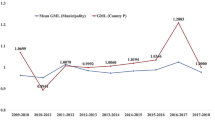
Comparing with the other countries, Thailand has limited availability of health workforce. Appendix Table 7 and Figs. 1, 2 show that the Thai medical workforce per 1000 people is much lower than the developed countries or the selected countries in Asia. Appendix Table 8 illustrates that the workforce shortage in the MOPH hospitals is critical but seems to be mitigable if there is an improvement in allocative efficiency due to variations in the shortage severity at different hospital levels.
Successful health resource planning requires not only the balance in both quantitative and qualitative goals of the health workforce management, but also the adaptation to varying health system needs. Certainly, the effective reallocation for the supply of medical workers in accordance with the demand for health care will lead to the more desirable clinical outcomes [17].
This study reports efficiency gains and associated economic values from the area-based human resource allocation of hospitals under the Office of the Permanent Secretary, the MOPH. The area-based network of the health workforce in this study is a simulation application of consolidating the public hospitals within local administrative areas. It is a counterfactual quantitative exercise to measure the hospital outputs per worker and subsequent results of reduction in workload per worker from network allocation scenarios. The network consolidation should simultaneously mitigate the health workforce shortage and enhance allocative efficiency of the health workers within their local areas from improvements in the workload per worker. Due to the health workforce shortage in public hospitals in Thailand, the lower workload per worker implies increase in workforce sufficiency rather than decrease in efficiency of the health system.
In fact, the area-based network of the health workforce is not a new concept for Thailand. It has been developed and implemented by the health system and medical staffs to collaborate in the primary service of the district health administration systems for many years [18,19,20,21]. Jithitiikulchai [22] studied the area-based network consolidations for the health workforce in the MOPH hospitals. The author [22] found that the shortage situation is severe, and that the shortage could be mitigated from network reallocations. However, the analysis in the study [22] was considered by each medical profession such as doctor, nurse, dentist, pharmacist, and others. Thus, this pioneered work did not consider the aggregated output of health care service delivery units relative to the total health workforce, but only investigated by medical profession based on the number of health workforce relative to the minimum manpower requirement.
Therefore, this study endeavors to quantify whether and how the area-based resource allocation at different levels of hospital services and administrative areas could mitigate the health workforce shortage in terms of per capita workload reductions and proposes a general framework for the area-based network consolidation simulations. Specifically, this study develops the counterfactual simulation model to compare the workload per worker between (a) the hospital-level averages (status quo) and (b) the area-based network averages after consolidations at different levels of hospital services within the local administrative areas (ex ante). This approach is an application of the gatekeeping concept to optimally allocate resources according to the demand and supply of health care services to mitigate the shortage problem of the health workforce.
The methodology is straightforward, duplicable, and scalable. Simple linear regression approach is used to estimate the weights of output and input reflecting their economic values. The status quo and ex ante scenario comparisons use basic arithmetic operations. The simple economic valuation could help to recommend consolidation options that provide higher monetary values. This analysis could be an aspiring example of network consolidations for other countries facing a shortage in health workforce.
Methods
This study develops the counterfactual network simulation exercises for the area-based health workforce allocation at different levels of hospital services within levels of local health administrative areas. The objective is to measure allocative efficiency from redistributing the health workforce to improve health system’s capacity.
The network consolidation approach is considered an application of the gatekeeping system to manage health system resources in corresponding to the demand for health care services and the workforce supply capacity within each of the local system networks. This study assumes an efficient gatekeeping system such that local health systems could automate the seamless referral system for the outpatient (OP) and inpatient (IP) patients and, accordingly, allocate the area-based workforce to minimize the shortage of the workers.
The counterfactual simulation for network consolidation analysis provides comparisons of the “workload per worker” between (a) the hospital-level averages (status quo) and (b) the network averages after consolidations at different levels of hospitals and administrative-areas (ex-ante). See Additional file 1: Figure S1 for an illustrative example of local network by the four hospitals in the same area.
The geographical administrative area levels in this study follow the national health system which are the sub-district, district, province, and health service area levels. There are five hospital levels which are primary, first-level secondary, mid-level secondary, high-level secondary, and tertiary.
This study considers network consolidations within local administrative areas with different hospital classifications:
-
1.
All hospital levels altogether
-
2.
Only within the same hospital level
-
3.
Similar hospital levels:
-
3.1.
Type A: {Primary, First-level Secondary} and {Mid-level Secondary, High-level Secondary, Tertiary}
-
3.2.
Type B: {Primary, First-level Secondary, Mid-level Secondary} and {High-level Secondary, Tertiary}.
-
3.1.
Measurement of workload per worker
The workload per worker is the output divided by input, in which this study calculates both output and input to reflect their costs of human resources. The weights of each outpatient and inpatient case are the relative cost of workforce assigned for each discharge. The weights of the health workforce are the weekly work hour multiplied with the hourly earnings of each health occupation. Using the relative weights implicitly assume that the relative costs of output and input could capture the differences in severity of the medical treatment cases, availability of health workforce, and intensity of the workload per worker.
Output calculation
The outputs of hospital or area-based network are the aggregation of the weighted OP and IP cases to reflect the relative workforce costs allocated to each discharge. The approach used to measure output in this study thus applies the case mix index (CMI) concept that provides a standard reference for the standard IP costs as the diagnosis-related group (DRG) for reimbursements from the national health insurance schemes [23].
This study calculated the average costs with the regression models separately for the five hospital levels within each of the OP or IP categories. Separating cost regression equations for different cohorts or sampling groups are common in applied econometric analysis [24,25,26]. Separating cost regressions provides different cost levels according to the average costs incurred by hospital level and patient category. Finally, the OP and IP cases can be weighted with the standardized costs given observable characteristics and then aggregated into the total output of each hospital or network.
The average costs of each treatment case from the regression analysis are determined by the observable characteristics such as ICD-10 principal diagnosis (PDx) codes of 140 disease categories, sex and age of patients, service time, service type, insurance type, number of days admitted (only IP treatments), and health region. The total cost of each treatment case reported from hospitals covers labor, material, capital costs, and other indirect costs. The log-linear total cost regression functions are calculated separately for OP and IP services from five different hospital levels to standardize relative weight values to each medical treatment case. For instance, medical treatments in higher-level hospitals tend to be more costly than those in the primary hospitals. Similarly, IP cases should be more expensive than OP cases.
As the cost from each treatment case is the total cost reported from hospitals, this study multiplies the predicted costs of each OP and IP case with the hospital-level share of labor cost. The share of labor cost at the hospital-level can adjust the fitted total cost of each medical case into the approximated labor cost to be used as the output weights. Thus, output is the weighted numbers of outpatient (OP) and inpatient (IP) cases.
Input calculation
The input factor in this study is the total number of health workers in which each medical profession is weighted with their regional averages of hourly earnings and work hours per week. Thus, the aggregation of the weighted numbers of health workers is the total workforce of hospitals or area-based networks evaluated in monetary terms to reflect economic costs of health workforce. The average work hours per week and average earning per hour are obtained from the regression models controlling for observable characteristics of the health workers in the public sector aged 15–64, using the national labor force surveys. The health professions include medical doctors, nurses, dentists, pharmacists, and other medical professions. Therefore, input is the weighted numbers of health workers.
Area-based network allocation
This study compares workload per worker between the hospital-level average before network consolidations (status quo) and the area-based averages after network consolidations (ex ante). The workload per worker is calculated as the ratio of the weighted aggregate output and the weighted number of workforces. The counterfactual network consolidation simulations quantify the area-based health workforce reallocation within the local administrative areas at different hospital levels. The hypothesis in this study is that the network consolidation could improve the health system efficiency by alleviating the shortage of health workforce.
This study calculates average reductions in workload per worker as the percentage differences between the averages of workload per worker from the status quo and ex ante scenarios, whereas the unit of measurements is the OP case in primary hospitals. The standardized measurement unit, using the average labor costs for OP treatments in primary health care units to calculate the number of OP cases in primary hospitals, allows comparisons of the OP and IP services across different hospital levels.
Finally, this study estimates the economic value to compare the network consolidation options across different administrative areas and hospital-level classifications, using the status quo situation as the baseline scenario. The reduction in workload per worker can be valued financially by multiplying the total workloads reduced from network consolidation with the average labor costs. The reduced number of total workloads are the multiplications of the number of health care service delivery units, average health workers per service delivery unit, average workload per worker, and the percentage reduction in workload per worker. The workload and labor costs are in units of OP cases in primary hospitals. Technical details are available in Additional file 1 for output and workforce measurements, cost regressions, weights reflecting economic valuation, and area-based network allocations.
Data
The outpatient and inpatient discharge data from the Information and Communication Technology Center of the MOPH used in this study covers principal diagnosis (PDx), sex, age, service time (office hours or after hours), service type (walk-in, referral, among others), insurance type (Universal Coverage Scheme, Civil Servant Medical Benefit Scheme, Social Security Scheme, and others), number of days admitted (IP treatments only), and total costs of each treatment case. The OP and IP cases are the discharges in the fiscal year 2019.
Numbers of each medical profession such as the doctor, nurse, dentist, pharmacist, and other medical occupations are the hospital-level data from the Human Resource Management Division of the Office of the Permanent Secretary, the MOPH. There are 100 320 nurses, 16 593 doctors, 7906 pharmacists, and 4662 dentists who worked in the hospitals for the fiscal year 2019 as reported in Appendix Table 8.
The average hourly earnings and work hours per week of each medical profession are calculated from the quarterly Labor Force Survey (LFS) 2002Q1 to 2020Q1 of the National Statistical Office. The health workers aged 15–64 employed in the public sector are selected for each medical profession using the International Standard Classification of Occupations, ISCO-88 codes. The health workforce weights as adjustment factors are reported in Additional file 1: Table S3.
Results
This study uses the medical case data from 10 500 public hospitals under the Office of the Permanent Secretary, MOPH, across geographical units and health regions. The output is based on 284 273 598 OP discharges and 18 971 271 IP discharges in the budget year 2019. The OP and IP cases are weighted with their estimated costs, in which the estimated OP and IP costs are controlled for observable heterogeneity through linear regression estimations separately for each of five hospitals levels. Additional file 1: Tables S4, S5 provide the regression results of the cost of OP and IP cases.
The output, the aggregations of weighted average costs of OP and IP treatments in each hospital are normalized with the average labor cost of the OP cases in primary hospitals and resulted in 1 204 133 398 normalized OP discharges in primary hospitals as the standardized output unit. There are 155 377 health workers calculated from the total workforce weighted with their regional averages of work hours per week and earnings per hour of each occupation. The output per worker is a standard unit of measurement calculated as the “OP cases in primary hospitals per worker” used in comparing the status quo and ex ante scenarios across different hospital and geographical administrative area levels. Both output and input estimates reflect the labor resources expended for medical treatments in the fiscal year 2019.
The results from the consolidation of all hospital levels altogether illustrate that the networking at the district levels can reduce the average workload per worker by about 1.8% on average or reduce from 7924 to 7785 OP cases in the primary hospitals, as shown in Table 1. Meanwhile, at the province and health region levels, the workforce consolidation could reduce by 1.5% and 1.6%. However, the networking at the sub-district level has no impact on average, such that the primary-level OP cases per worker are about the same.
The results from the networking within the same hospital levels are illustrated in Table 2. The results show that the consolidation of workforce at the primary level and the approach of networking at the district, province, and health region levels could reduce workload per worker by 7%, 10%, and 14%, respectively. For the first-level secondary hospitals, area-based networking cannot reduce the workload. For the mid-level secondary hospitals, networking at the administrative levels of the province and health region could reduce workload per worker by 2–3%. For the high-level secondary and the tertiary hospitals, the area-based network consolidations cannot reduce the workload quantity per worker.
In an effort to network workforce in lower hospital levels, there are two options, {Primary, First-level Secondary} of Option A and {Primary, First-level Secondary, Mid-level Secondary} of Option B, as illustrated in Tables 3, 4. The results show that both options of network consolidations for similar hospital levels could reduce the average workload per worker for the lower hospital levels. When combined at the province level, Option A could reduce the workload by 6%, while Option B could reduce the workload by 7%, on average.
However, both options could reduce the average cases per worker only by 1–2% within the health regional networks in the upper hospital levels, which are {Mid-level Secondary, High-level Secondary, Tertiary} of Option A and {High-level Secondary, Tertiary} of Option B.
Economic valuation of network consolidation options
The economic valuation can be compared between the status quo and ex ante scenarios. Thus, we can appraise the network consolidation options. For each network consolidation option, the aggregated reduction in a standardized unit of OP cases conducted at primary hospitals are calculated using the multiplication of the reduced primary OP cases per worker, average primary OP cases per worker, the average number of workforces in each service-delivery unit, and the total number of units. In the end, we obtain the aggregate numbers of reducible primary OP cases multiplied with the average labor cost per OP case at primary hospitals, the economic value gained from the network consolidation.
In Table 5, the total reductions in number of primary OP cases, which could be obtained from each network consolidation option comparing with the status quo scenario, are illustrated. The most reduced number in the aggregate workloads occurs from consolidating all hospital levels altogether. However, combining all hospital levels seems unrealistic and unpractical. The more reasonable options are to network similar hospital levels and combine within the provinces or health service areas.
Table 6 illustrates the economic values in Thai Baht and US dollar in correspondence with Table 5. A practical alternative with high economic outcomes is the application of combining hospitals with similar hospital levels at the provincial level. The calculation shows that, if comparing with the aggregate labor cost incurred at hospitals in the same budget year, the network consolidations of similar hospital levels within the same provinces could gain about 15–18% of total labor cost in the primary hospitals at 10 billion Thai Baht.
Discussion
The area-based network consolidations can redistribute the health workforce and improve allocative efficiency of human resource administration. Suggested by the most practical results from the analysis in this study, networking the primary-level hospitals within the same district could reduce workload per worker by 7% on the national average. Another feasible option is the method of consolidating similar hospital levels such as primary, first-level secondary, and mid-level secondary hospitals within the same province which is estimated to reduce the workload per worker by 6–7%. Definitely, the implementation requires the strengthened primary health care units of the primary-level hospitals within each district.
Conceptually, we assume that the network consolidations occur in the situation that we have the efficient gatekeeping system to optimize resources according to the demand for health care service and the workforce supply capacity within each network. However, we should realize that the health service units are still independent of each other in planning, budgeting, and performance assessment. In addition, the current health system does not allow such flexibility to reflect in the promotion and career path for public health workers in Thailand.
Therefore, this requires what Leerapan et al. [27] proposed as “major reforms of MOPH care delivery models” such that the health care delivery units can adjust and adapt their resources and services in corresponding to the population health needs. Leerapan et al. [27]’s proposal includes the capacity reallocation of health care delivery teams to be enlarged in the areas with excess demand and to be reduced in the areas with excess supply. This proposal of “major reforms of MOPH care delivery models” is conceptually consistent with the allocative efficiency; the health system utilizes the management capacity to establish and prioritize local objectives to redistribute health system resources corresponding to the demand–supply gaps of health workforce.
Noree et al. [28] defined distinguished properties of the desirable health care delivery system as a seamless health service network of an integrated system of primary, secondary, and tertiary hospitals. Pooling resources and planning through the management information system within a local health care network are critical for a robust referral management system with the gatekeeping application. Both Noree et al. and Leerapan et al. [27, 28] aligns with the goal of the “value-based health care” concept [29, 30], which is a health care delivery model to maximize the value of care for patients and minimizing the cost of health care.
The practical possibilities in my opinion are to consolidate primary hospitals within each district, similar hospital levels within each province, or a mixture of both. Although the evaluations in this study center on the results at average, this study can provide some guidance of the policy options for optimal allocation of public health workers to mitigate workforce shortage. A good policy is not one-size-fits-all. It requires decentralization for the provincial and district health systems to have their autonomy over decision-making processes and be equipped with accountability to monitor and evaluate their performance through the health and management information systems.
The area-based networking approach at the district or provincial level could add a commuting and time burden to the health workers. This is inevitably undeniable. Therefore, we need financial incentives, career advancement mechanisms, and team development programs, among others, to facilitate the local health care system development. See [31,32,33,34,35,36,37,38,39,40] for evidence of the effective financial and non-financial incentives in Thailand and developing countries.
In addition, the gatekeeping system must consider the potentially increased travel cost burdens to the patients especially the poor living in the remote rural areas. The primary hospitals are available in every sub-district of Thailand in which those patients who can commute to their sub-district hospital should be able to access to the district-level primary healthcare network. However, the higher-level hospitals mostly locate in the city areas. The transportation services for referrals are required to support the health care accessibility of the poor and vulnerable people.
Finally, any country with community health networks should have a national strategic plan for area-based health system development that aligns with the national human resource plan. Not only the more equitable distribution is required for health workforce management across geographical and administrative areas, but also the more fiscal resources to produce the medical workforce to solve the shortage severity, as we can observe from Appendix Table 7 and Figs. 1, 2 which illustrate that Thailand has poorly low medical workforce. The author strongly encourages the health workforce organizations to call out for reprioritizing more national budget for the health system to mitigate the workforce shortage.
Limitation
First, this study has some limitations on total output calculations. Health workforce positions have the responsibility not only on treatment service delivery used in this study. They also have some other tasks such as health promotion and disease prevention services, and administrative works, among others. Due to data limitations of the additional roles of health personnel, this study cannot consider other duties beyond the OP and IP discharges.
Second, the area-based network consolidations in this study assumed that the health workforce could move freely within the network to serve the local health care needs. However, the calculations are the technical results for the policymakers to consider policy and program options on human resource management. It requires considerate evaluations of positive and negative externalities that potentially occurred to the health workers within each hospital and the local area. The practical possibilities seem to consolidate primary hospitals within each district, similar hospital levels within each province, or combinations of both approaches. Instead of the workforce relocation, the robust referral system could assign patients to the most appropriate hospitals at the time. This could be actualized by digital transformation of the local health systems.
Third, the calculations in this study did not explicitly consider the capital inputs of hospitals. It is perhaps difficult in terms of conceptualization to incorporate the capital component into the cost regression models. Nevertheless, this study reflects the capital factor by providing a more realistic consolidation within the same or similar hospital levels to regard the capital differences between hospital levels.
Lastly, this study uses the estimated labor cost for weights of each OP and IP case. However, Porter [29, 30] suggested that achieving the goal of health care delivery requires that the value determinant should be the health outcomes achieved per every monetary unit spent. Therefore, the future research can measure the value of each discharge with the framework for performance improvement in health care that creates value for patients, measured by the outcomes achieved, not inputs nor volume of services delivered.
Conclusion
This study evaluates shortage mitigation from the area-based network consolidations of health workers. The analytical results confirm improvement in allocative efficiency of the health workforce in the MOPH hospitals. The economic valuation reveals that consolidating similar hospital levels within the same province is an optimal solution. The benefits from efficient area-based networks are equal to 15–18% of total labor cost in the primary-level hospitals.
Availability of data and materials
The datasets used for this study are available from the corresponding author upon reasonable request and with the authorized approvals from the government offices which own the original raw data.
Abbreviations
- CSMBS:
-
Civil Servant Medical Benefit Scheme
- MOPH:
-
Thai Ministry of Public Health
- PDx:
-
Principal diagnosis
- SSS:
-
Social Security Scheme
- UCS:
-
Universal Coverage Scheme
References
Pagaiya N. Human resources for health requirements projection: crucial baseline to support human resources for health planning. J Health Syst Res. 2018;12(2):342–55.
Noree T, Thanomwat Y, Phanthunane P, Gongkulawat K. Research for synthesize options and policy recommendations for planning the human resources for health needs in the future decade. Final report. The Human Resources for Health Research and Development Office (HRDO). International Health Policy Program (IHPP); 2017.
Leerapan B, Teekasap P, Jaichuen W, Chiangchaisakulthai K, Cooper Meeyai A, Urwannachotima N, et al. Report of data collection and synthesis of Thailand’s demands for health workforce in the next 20 years. Final report; 2018.
Working Group on Efficiency Development of System Resources Allocation. Public health steering and reform sub-committee for health finance and universal health coverage. A study project for proposal on UHC financing for efficiency development of system resources allocation: human resources for health. Final report; 2016.
Strategy and Planning Division PSO, Ministry of Public Health. Report on public health resources in 2016. Nonthaburi: Ministry of Public Health; 2018.
Srisuphan W, Sawangdee K. Policy recommendation for nurse shortage in Thailand. Thai J Nurs Counc. 2012;27(5):5–12.
Pagaiya N, Phanthunane P, Bamrung A, Noree T, Kongweerakul K. Forecasting imbalances of human resources for health in the Thailand health service system: application of a health demand method. Hum Resour Health. 2019;17(4):1–12.
Sawaengdee K. Crisis of nursing shortage in health service facilities under the Office of the Permanent Secretary, Ministry of Public Health: policy recommendations. J Health Sci. 2017;26(2):457–68.
Sawaengdee K, Tangcharoensathien V, Theerawit T, Thungjaroenkul P, Thinkhamrop W, Prathumkam P, Chaichaya N, Thinkhamrop K, Tawarungruang C, Thinkhamrop B. Thai nurse cohort study: cohort profiles and key findings. BMC Nurs. 2016;5(10):1–12.
Seema K, Intaraprasong B, Pattara-achachai J. Registered nurse’s intention to leave the profession in Bangkok Metropolitan Administration hospitals. J Nurs Division. 2015;42(3):142–58.
Thongniran N, Intaraprasong B, Pattara-Archachai J. Intention to stay in occupation of registered nurses at a community hospital region 1: Central, Thailand. J Nurs Division. 2015;42(3):69–83.
Muneerat S, Suwannapong N, Tipayamongkholgul M, Manmee C. Job characteristics, job-related stress and intention to stay in professional nursing in a tertiary care hospital, Ministry of Public Health. J Health Sci. 2019;28(1):133–41.
Jeawkok J, Dhammasaccakarn W, Keawpimon P. Retention and intention of resignation to the job of registered nurses in the university hospital, Songkhla Province. NIDA Dev J. 2015;55(3):109–44.
Pagaiya N, Khaonuan B, Phanthunane P, Bamrung A, Jirawattanapisal T. Human resources for health projections for primary health care services in Thailand 2026. J Health Syst Res. 2018;12(2):189–204.
Phanthunane P, Bamrung A, Jirawattanapisal T, Pagaiya N, Khaonuan B, Noree T. A utilization-based model to predict human resources for health (HRH) in secondary care services of Thailand 2026. J Health Syst Res. 2018;12(2):205–20.
Phanthunane P, Pannarunothai P, Pagaiya N. Requirement and supply projection of selected medical specialists in Thailand in 2021. Malays J Public Health Med. 2017;17(2):70–9.
Leelarasamee A, Intragumtornchai T, Pannarunothai S, Laohavinij S, Patjanasoontorn B, Suntorntham S, et al. Need for internal medicine subspecialists in Thailand. J Med Assoc Thai. 2017;100(2):239–53.
Hasuwannakit S. Network management for contracted unit for primary care (CUP). Nonthaburi: Office of Community Based Health Care Research and Development; 2007.
Bookboon P. Population-centered district health system development. Nonthaburi: Office of Community Based Health Care Research and Development; 2016.
Office of Community Based Health Care Research and Development. Family physicians: driving force for NCDs. Synthesis from NCD 2015 forum, Nonthaburi; 2018.
Office of Community Based Health Care Research and Development. Lessons from district health system administration: participatory primary health worker and network management; Nonthaburi; 2018.
Jithitikulchai T. Area-based network allocations: a solution to mitigate the shortage of health workforce. J Health Syst Res. 2020;14(3):243–73.
Suphanchaimat R. “Health insurance card scheme” for cross-border migrants in Thailand: responses in policy implementation & outcome evaluation. Doctoral dissertation. London School of Hygiene & Tropical Medicine; 2017.
Deng L, Lou W, Mitsakakis N. Modeling right-censored medical cost data in regression and the effects of covariates. Stat Methods Appl. 2019;28(1):143–55.
Jones AM, Lomas J, Rice N. Applying beta‐type size distributions to healthcare cost regressions. J Appl Econom. 2014;29(4):649–70
Jones AM, Lomas J, Rice N. Healthcare cost regressions: going beyond the mean to estimate the full distribution. Health Econ. 2015;24(9):1192–212
Noree T, Thanormwat Y, Phanthunane P, Gongkulawat K. Research project on synthesis of alternatives and policy recommendation for planning health workforce in the next decade (2017–2026). International Health Policy Program. Ministry of Public Health; 2017.
Leerapan B, Teekasap P, Jaichuen W, Chiangchaisakulthai K, Meeyai AC, Urwannachotima N, Udomaksorn K. Strategic planning of human resources for health to address the challenges of Thailand’s Universal Health Coverage: a system dynamics approach. Final report to the Office of the Permanent Secretary, Ministry of Public Health; 2018.
Porter ME, Teisberg EO. Redefining health care: creating value-based competition on results. Boston: Harvard Business School Press; 2006.
Porter ME, Teisberg EO. What is value in health care? N Engl J Med. 2010;363(26):2477–81.
Lagarde M, Pagaiya N, Tangcharoensathian V, Blaauw D. One size does not fit all: investigating doctors’ stated preference heterogeneity for job incentives to inform policy in Thailand. Health Econ. 2013;22(12):1452–69.
Pagaiya N, Noree T. Thailand’s health workforce: a review of challenges and experiences. Health, nutrition and population (HNP) discussion paper. Washington, DC: World Bank; 2009.
Pagaiya N, Sriratana S, Tangchareonsathien V, Noree T, Lagarde M, and Blaauw D. Health workers’ preferences and policy interventions to improve retention in rural areas in Thailand. Consortium for Research on Equitable Health Systems (CREHS) Cohort Study; 2011.
Panda P, Chaijaroen P. Do rural health worker incentive schemes work? Evidence from Thailand. Econ Bull. 2020;40(2):1583–95.
Prakongsai P, Srivanichakorn S, Yana T. Enhancing the primary care system in Thailand to improve equitable access to quality health care. In: 2nd national health assembly in Thailand, November; 2009.
Putri LP, O’Sullivan BG, Russell DJ, Kippen R. Factors associated with increasing rural doctor supply in Asia-Pacific LMICs: a scoping review. Hum Resour Health. 2020;18(1):1–21.
Rakhab A, Jackson C, Nilmanat K, Butterworth T, Kane R. Factors supporting career pathway development amongst advanced practice nurses in Thailand: a cross-sectional survey. Int J Nurs Stud. 2021;117: 103882.
Wibulpolprasert S, Pengpaibon P. Integrated strategies to tackle the inequitable distribution of doctors in Thailand: four decades of experience. Hum Resour Health. 2003;1(1):1–17.
Wibulpolprasert S, Pachanee CA. Addressing the internal brain drain of medical doctors in Thailand: the story and lesson learned. Glob Soc Policy. 2008;8(1):12–5.
Willis-Shattuck M, Bidwell P, Thomas S, Wyness L, Blaauw D, Ditlopo P. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Serv Res. 2008;8(1):1–8.
Acknowledgements
The author would like to thank two anonymous referees who kindly reviewed the earlier versions of this manuscript and provided highly valuable suggestions and comments. The author gratefully acknowledges dialogue with and advice from Ammar Siamwalla, Suwit Wibulpolprasert, Supasit Pannarunothai, Tinakorn Noree, Piya Hanvoravongchai, Walaiporn Patcharanarumol, and Wilailuk Ruangrattanatrai. This project was conducted with the support of the Takemi Program in International Health at Harvard T. H. Chan School of Public Health. The views expressed herein are those of the author and do not necessarily reflect the views of the World Bank Group or any institutional affiliations.
Funding
The research received funding from the Health Systems Research Institute (HSRI), Ministry of Public Health of Thailand under Grant HSRI 63-014.
Author information
Authors and Affiliations
Contributions
TJ solely worked on the study. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable as secondary and anonymous data were used in the study.
Consent for publication
Not applicable.
Competing interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary material for methods and regression results.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jithitikulchai, T. Improving allocative efficiency from network consolidation: a solution for the health workforce shortage. Hum Resour Health 20, 59 (2022). https://doi.org/10.1186/s12960-022-00732-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12960-022-00732-1