Abstract
Background
Low vitamin D status has been associated with an increased risk for infertility. Recent evidence regarding the efficacy of vitamin D supplementation in improving reproductive outcomes is inconsistent. Therefore, this systematic review was conducted to investigate whether vitamin D supplementation could improve the reproductive outcomes of infertile patients and evaluate how the parameters of vitamin D supplementation affected the clinical pregnancy rate.
Methods
We searched seven electronic databases (CNKI, Cqvip, Wanfang, PubMed, Medline, Embase, and Cochrane Library) up to March 2022. Randomized and cohort studies were collected to assess the reproductive outcomes difference between the intervention (vitamin D) vs. the control (placebo or none). Mantel-Haenszel random effects models were used. Effects were reported as odds ratio (OR) and their 95% confidence interval (CI). PROSPERO database registration number: CRD42022304018.
Results
Twelve eligible studies (n = 2352) were included: 9 randomized controlled trials (RCTs, n = 1677) and 3 cohort studies (n = 675). Pooled results indicated that infertile women treated with vitamin D had a significantly increased clinical pregnancy rate compared with the control group (OR: 1.70, 95% CI: 1.24–2.34; I2 = 63%, P = 0.001). However, the implantation, biochemical pregnancy, miscarriage, and multiple pregnancy rates had no significant difference (OR: 1.86, 95% CI: 1.00–3.47; I2 = 85%, P = 0.05; OR: 1.49; 0.98–2.26; I2 = 63%, P = 0.06; OR: 0.98, 95% CI: 0.63–1.53; I2 = 0%, P = 0.94 and OR: 3.64, 95% CI: 0.58–11.98; I2 = 68%, P = 0.21). The improvement of clinical pregnancy rate in the intervention group was influenced by the vitamin D level of patients, drug type, the total vitamin D dosage, the duration, administration frequency, and daily dosage of vitamin D supplementation. The infertile women (vitamin D level < 30 ng/mL) treated with the multicomponent drugs including vitamin D (10,000–50,000 IU or 50,000–500,000 IU), or got vitamin D 1000–10,000 IU daily, lasting for 30–60 days could achieve better pregnancy outcome.
Conclusion
To the best of our knowledge, this is the first meta-analysis systematically investigated that moderate daily dosing of vitamin D supplementation could improve the clinical pregnancy rate of infertile women and reported the effects of vitamin D supplementation parameters on pregnancy outcomes. A larger sample size and high-quality RCTs are necessary to optimize the parameters of vitamin D supplementation to help more infertile patients benefit from this therapy.
Similar content being viewed by others
Introduction
Infertility is a widespread health problem across the world. Approximately 9.3–16.7% of the females of child-bearing age suffered from infertility [1, 2]. In recent years, an increasing number of infertile women seek assistance from assisted reproductive techniques (ARTs) [3]. However, the efficacy of improvement in ARTs slowed down recently [4]. It is still necessary to improve the effectiveness of ARTs. Vitamin D, a steroid hormone, has five compounds in which vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol) are vital members associated with reproductive health [5]. Previous research found that 1α-hydroxylase (vitamin D enzymes) and vitamin D receptors were expressed in human first-trimester and decidua [6, 7]. Vitamin D receptors and 1,25(OH)2D3 regulated the transcription of HOXA10 which was the key target gene associated with implantation [6,7,8]. Accumulating evidence from prospective random and cohort observational studies proposed that vitamin D insufficiency or deficiency was related to infertility [9]. It is proposed that vitamin D status might influence initial embryo implantation by regulating the immunology cells (natural killer cells, dendritic cells, macrophages, and T cells) in uterine and decidua tissue [6, 7]. However, recent interest focused on the association between vitamin D levels and ART outcomes, but not on the influence of vitamin D supplementation on reproduction [9]. The animal experiment found the injection of vitamin D3 could induce the decidualization of rat endometrial cells [10]. In human clinical trials, some studies found vitamin D supplementation improved the reproductive outcomes of infertile women [11, 12], but other research showed the failed influence of vitamin D treatment on pregnancy outcomes [13, 14]. Whether vitamin D supplements could contribute to successful ARTs outcomes of infertile women was still uncertain. Similarly, the dosage and duration of vitamin D supplementation varied greatly in the previous reports [13, 15]. The high concentration of serum vitamin D could result in hypervitaminosis D (vitamin D poisoning) which was associated with nausea, vomiting, weakness, disturbed digestion, and elevated blood and tissue calcium levels [16,17,18]. Considering appropriate vitamin D supplementation for overall health benefits, it is of great significance to investigate the fertility effect of parameters of vitamin D supplementation.
There are lack of conclusive results and a comprehensive review regarding the actual fertility benefits of vitamin D supplementation and the potential effects of its parameters. Therefore, in this systematic review and meta-analysis, our purpose was to evaluate whether vitamin D supplementation could influence the reproductive outcomes of infertile women, and provide practical guidance on the parameters of vitamin D supplementation to ensure infertile patients could receive proper treatment and improve the treatment effectiveness for future trials.
Methods
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The protocol of this study was prospectively registered with the registration number CRD42022304018 at PROSPERO. The institutional review board approval was not required because all data were published previously.
Search strategy
English-language databases PubMed, Medline, Embase, and Cochrane Library and Chinese-language databases CNKI, Cqvip, and Wanfang were searched. The search strategy was devised for each outcome (Supplemental Search strategy, available online). Searches time was restricted to studies published up to March 2022. References from the selected articles, including relevant review papers, were reviewed to identify all relevant studies. Conference abstracts and prospective trial registries were also searched for relevant items.
Inclusion and exclusion criteria
Data were carefully extracted by 2 investigators independently. Any inconsistent opinions were resolved by discussion or with the help of a further investigator. The infertile women undergoing ART (IVF, ICSI, fresh embryo transfer, and frozen embryo transfer) who had vitamin D supplementation were recruited. Study characteristics [authors’ last name(s), year of publication, country, and population (number of cases and controls)], specific details about the interventions and reproductive outcome measures (implantation rate, biochemical pregnancy rate, clinical pregnancy rate, miscarriage rate, and multiple pregnancy rate) were recorded and summarized. Exclusion criteria were: (1) reviews and case reports; (2) duplicate publications; (3) data were not available or could not be extracted for the study groups; and (4) no appropriate case or control group.
Quality assessment
Quality assessment was evaluated by 2 investigators independently. Any inconsistent opinions were arbitrated by a third investigator. The risk of bias for RCTs was evaluated using Cochrane’s tool. The quality score of cohort studies was assessed using Newcastle-Ottawa Scale. The quality scores of studies ranged from 0 to 9 points and included three aspects: selection, comparability, and exposure.
Statistical Analysis
The extracted data were analyzed with Review Manager 5.3 software (Cochrane Collaboration, Oxford, U.K.). The Mantel-Haenszel method random-effects models were used for meta-analysis. The effect sizes were expressed as odds ratios (ORs) and calculated using their 95% confidence intervals (CIs). Summary ORs and 95% CIs were assessed graphically with forest plots. The Heterogeneity was quantified using the I2 value. To examine the potential heterogeneity sources, subgroup meta-analyses were performed according to the vitamin D level of patients, drug type, the total vitamin D dosage, and the duration, administration frequency, and daily dosage of vitamin D supplementation. Publication bias was evaluated using a funnel plot. To evaluate whether there was any study affecting the stability of the results, STATA 17.0 software was used for the sensitivity analysis (leave one out). A P-value <0.05 was considered statistically significant.
Results
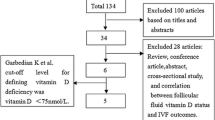
The PRISMA flow diagram of the study process is presented in Fig. 1. The search strategy yielded 700 publications (58 from CNKI, 13 from Cqvip, 66 from Wanfang, 96 from PubMed, 96 from Medline, and 146 from other sources), of which 313 were removed as duplicates. After records screening, 209 studies were excluded for not fulfilling the experiment criteria. The full manuscripts of 28 articles were evaluated. In two publications the full text was not accessible, and two of those were excluded for full-text duplication. Seven articles were removed for not meeting the inclusion criteria. Thus, a total of 12 publications with available full texts remained. Finally, we recruited 2548 infertile patients who met the eligibility criteria for quantitative data synthesis in twelve studies: nine RCT studies (n = 1773) and three clinical trial studies (n = 775) for investigating the effect of vitamin D supplementation on reproductive outcomes. A detailed summary of the included study characteristics is shown in Table 1 and Supplemental Tables S1 and S2.
Study characteristics
The main characteristics of the included studies are shown in Table 1. The publication dates of the eligible studies ranged between 2014 and 2021. The number of patients ranged from 74 to 630. Nine studies were RCTs [11,12,13,14,15, 19,20,21], and three studies were nonrandomized cohort studies [22,23,24]. The double-blind method was reported in five of the nine RCTs [12, 13, 15, 19, 21]. The risk of bias assessments for the RCTs and cohort studies are summarized in Supplementary Tables S1 and S2. The studies were conducted in Iran (four studies), China (four studies), Italy (two studies), the United Kingdom (one study), and Poland (one study). The serum vitamin D concentration before supplementation was lower than 20 ng/mL in 2 studies, lower than 30 ng/mL in 7 studies, and not limited in 5 studies. The data on serum vitamin D concentration after supplementation were accessible in 3 studies. The patients in the case group underwent vitamin D supplementation in all 12 studies, were treated with vitamin D only in 6 studies, and were multicomponent in 6 studies. The patients in the control group were treated with a placebo in 8 studies and without intervention in 4 studies. The fertilization methods were IVF (one study), IVF/ICSI (three studies), ICSI (three studies), or no information (five studies). All recruited women were infertile and undergoing IVF treatment. Recruited patients with PCOS in three studies or a variety of etiology in seven studies. The duration of vitamin D supplement was in the range of 1–90 days. The administration frequency of vitamin D was daily in 7 studies, weekly in 3 studies, and other 2 in studies. The total vitamin D dosage was in the range of 560–600,000 IU. The administration route of vitamin D was intramuscular injection (one study) or oral administration (ten studies). The embryo transfer type was fresh and frozen embryo transfer (two studies), fresh embryo transfer (one study), frozen embryo transfer (four studies), or undetermined (five studies).
Effects of Vitamin D supplementation on the reproductive outcomes of infertile patients
The implantation rate outcomes were based on the data derived from 6 studies (963 cases and 895 controls). The implantation rate had no significant difference between the case and control group (OR: 1.86, 95% CI: 1.00–3.47; P = 0.05; heterogeneity; I2 = 85%; Fig. 2A).
The biochemical pregnancy rate outcomes were based on the data derived from seven studies (772 cases and 711 controls). The biochemical pregnancy rate had no significant difference in the case group compared with that in the control group (OR: 1.49, 95% CI: 0.98–2.26; P = 0.06; heterogeneity; I2 = 63%; Fig. 2B).
The clinical pregnancy rate outcomes were based on the data derived from 12 studies (1235 cases and 1117 controls): nine RCTs and three cohort studies. In RCTs studies, the clinical pregnancy rate was significantly higher in the case group than in the control group (OR: 1.49, 95% CI: 1.05–2.11; P = 0.02; heterogeneity; I2 = 54%). In cohort studies, the clinical pregnancy rate was significantly higher in the case group than in the control group (OR: 2.21, 95% CI: 1.42–3.44; P = 0.0005; heterogeneity; I2 = 33%). Overall, the clinical pregnancy rate was significantly higher in the case group than in the control group in a total of 11 studies (OR: 1.70, 95% CI: 1.24–2.34; P = 0.001; heterogeneity; I2 = 63%; Fig. 2C).
The results of the sensitivity analysis are shown in Supplemental Fig. S1 and S2. It is suggested that data derived from Somigliana (2021) may have a remarkable effect on the merger results (Fig. S2) [13]. Somigliana (2021) was removed, the meta-analysis of the effect of vitamin D supplementation on the clinical pregnancy rate of infertile patients was drawn (Fig. S2) [13]. High heterogeneity suddenly decreased from 63 to 36% (Fig. 2C and S2). The pooled results still indicated that infertile women treated with vitamin D had a significantly increased clinical pregnancy rate compared with the control group (OR: 1.84, 95% CI: 1.39–2.43; P < 0.0001; heterogeneity; I2 = 36%; Fig. S2). And the conclusions of this study were statistically reliable.
However, the miscarriage rate outcomes were based on the data derived from seven studies (366 cases and 289 controls). No difference was found in the miscarriage rate between the case and control group (OR: 0.98, 95% CI: 0.63–1.53; P = 0.94; heterogeneity; I2 = 0%; Fig. 2D).
The multiple pregnancy rate outcomes were based on the data derived from three studies (332 cases and 319 controls). The multiple pregnancy rate had no significant difference between the case and control group (OR: 2.64, 95% CI: 0.58–11.98; P = 0.21; heterogeneity; I2 = 68%; Fig. 2E).
Effects of the parameters of vitamin D supplementation on the clinical pregnancy rates of infertile patients
The clinical pregnancy rate in studies with different vitamin D levels of infertile patients
No significant difference was found in the clinical pregnancy rate between the case and control groups when the vitamin D level in the serum of infertile patients was lower than 20 ng/mL or had no limited (OR: 0.84, 95% CI: 0.48–1.49; P = 0.56; heterogeneity; I2 = 35%; or OR: 1.27, 95%CI: 0.94–1.72; P = 0.12; heterogeneity; I2 = 0%). When the vitamin D level in serum before treatment was lower than 30 ng/mL, the clinical pregnancy rate was significantly increased in the case group than in the control group (OR: 2.06, 95% CI: 1.32–3.22; P = 0.001; heterogeneity; I2 = 58%; Fig. 3).
The clinical pregnancy rate in studies with different drug types
When the infertile patients were treated with vitamin D only, the clinical pregnancy rate had no significant difference between the case and control groups (OR: 1.67, 95% CI: 0.98–2.82; P = 0.06; heterogeneity; I2 = 66%). However, if the patients got multicomponent drug contained vitamin D, the clinical pregnancy rate was significantly higher in the case group than in the control group (OR: 1.75, 95% CI: 1.18–2.59; P = 0.005; heterogeneity; I2 = 53%; Fig. 4).
The results of the sensitivity analysis are shown in Supplemental Fig. S3 and S4. It is suggested that data derived from Somigliana (2021) might have a remarkable effect on the merger results (Fig. S3) [13]. Somigliana (2021) was removed, meta-analysis of the effect of vitamin D supplementation on the clinical pregnancy rate in the subgroup of vitamin D only supplementation was drawn (Fig. S3) [13]. The high heterogeneity suddenly decreased from 66 to 20% (Fig. 4 and S4). The pooled results indicated that infertile women treated with vitamin D only had a significantly increased clinical pregnancy rate compared with the control group (OR: 1.97, 95% CI: 1.26–3.09; P < 0.003; heterogeneity; I2 = 20%; Fig. S4).
The clinical pregnancy rate in studies with different total dosages of vitamin D supplementation
There was no significant difference in the clinical pregnancy rate between the case and control groups when the total vitamin D dosage was lower than 10,000 IU or higher than 500,000 IU (OR: 3.01, 95% CI: 1.00–9.11; P = 0.05; or OR: 0.86, 95% CI: 0.62–1.18; P = 0.34). Compared with the control group, the clinical pregnancy rate increased significantly in the case group when the infertile patients were treated with 10,000–50,000 IU or 50,000–500,000 IU vitamin D during the whole supplementation (OR: 1.69, 95% CI: 1.06–2.71; P = 0.03; heterogeneity; I2 = 62%; or OR: 2.12, 95% CI: 1.29–3.49; P = 0.003; heterogeneity; I2 = 14%; Fig. 5).
The clinical pregnancy rate in studies with different duration of vitamin D supplementation
The clinical pregnancy rate was similar in the case group compared with the control group when the duration of vitamin D supplementation was shorter than 30 days (OR: 1.45, 95% CI: 0.67–3.13; P = 0.34; heterogeneity; I2 = 69%). When the vitamin D supplementation lasted for 30–60 days or 60–90 days, the clinical pregnancy rate was significantly higher in the case group than in the control group (OR: 2.00, 95% CI: 1.07–3.76; P = 0.03; heterogeneity; I2 = 54%; or OR: 1.70, 95% CI: 1. 16–2.49; P = 0.007; heterogeneity; I2 = 52%; Fig. 6).
The clinical pregnancy rate in studies with different administration frequencies of vitamin D supplementation
The clinical pregnancy rate was significantly higher in the case group compared with the control group when vitamin D supplementation was given every day or weekly (OR: 1.83, 95% CI: 1.26–2.64; P = 0.001; heterogeneity; I2 = 49%; or OR: 2.16, 95% CI: 0.95–4.92; P = 0.07; heterogeneity; I2 = 49%). When the vitamin D was administrated at one time or other frequency, the clinical pregnancy rate was similar in the case group compared with the control group (OR: 1.10, 95% CI: 0.61–2.00; P = 0.74; heterogeneity; I2 = 69%; Fig. 7).
The clinical pregnancy rate in studies with different dosages of vitamin D supplementation daily
The clinical pregnancy rate was similar in the case group compared with the control group when the dosage of vitamin D supplementation daily was lower than 1000 IU (OR: 1.28, 95% CI: 0.78–2.10; P = 0.33; heterogeneity; I2 = 33%). When the dosage of vitamin D supplementation daily ranged from 1000 to 10,000 IU, the clinical pregnancy rate was significantly higher in the case group than in the control group (OR: 2.17, 95% CI: 1.63–2.89; P < 0.00001; heterogeneity; I2 = 0%). Compared with the control group, the clinical pregnancy rate was the same in the case group when the dosage of vitamin D supplementation daily was higher than 10,000 IU (OR: 1.87, 95% CI: 0.33–10.48; P = 0.48; heterogeneity; I2 = 87%; Fig. 8).
Discussion
This study demonstrated that vitamin D supplementation successfully improved the clinical pregnancy rate of infertile women, but failed to significantly alter the implantation and biochemical pregnancy rate. However, we found that the results were significantly influenced by the article reported by Somigliana et al. [13]. When the data from this article was removed, the implantation and biochemical pregnancy rate significantly increased [13]. The alteration might be caused by its research design [13]. Somigliana et al. designed that the patients took a single oral dose of 600,000 IU [13]. This single dosage was much higher than the maximum dose of supplementation for vitamin D-deficient adults recommended by the Scientific Advisory Committee on Nutrition (SACN) which should not exceed 4000 IU/day or suggested by the National Institute for Health and Care Excellence (NICE) 50,000 IU per week for 6 weeks (300,000 IU in total) [25, 26]. Even though vitamin D supplementation was suggested as a safe and well-tolerated intervention, the drug dosage of clinical intervention still needed careful consideration [16, 27,28,29]. Especially, the previous reports proposed that there were toxicity and counterproductive influence when serum vitamin D concentrations greater than 150 ng/mL (greater than 374 nmol/L) [16, 27, 28, 30]. Even previous articles showed that large bolus vitamin D dose could be cleared within a week, achieving little or no detectable effect on circulating the vitamin D status [31, 32]. All of these reasons could be used to explain the results bias caused by Somigliana et al. [13]. Increased clinical pregnancy rate might be associated with successful implantation, not resulting from reducing the risk of miscarriage. The results supported the hypothesis that vitamin D exerted pivotal effects on initial embryo implantation, the early trophoblast invasion, and the decidualization of endometrium, not on the second-trimester loss for infertile women undergoing IVF treatment [33, 34].
Many previous reports proposed that the low level of vitamin D was related to poor implantation and infertility [9, 35]. The cut-off value of serum vitamin D was adopted by the Endocrine Society [36]. The serum 25-hydroxy vitamin D3 concentration of <20 ng/mL was considered vitamin D deficiency, 21–29 ng/mL was considered insufficient, and > 30 ng/mL was considered replete [36]. We separated the recruited population according to these vitamin D levels into three groups and tried to check whether the vitamin D level before the supplementation could affect the reproductive outcomes of the vitamin D treatment. Only the patients whose vitamin D level was lower than 30 ng/mL could benefit from the supplementation, neither the vitamin D concentration in serum lower than 20 ng/mL nor non-limited. These results could be explained by the hypothesis that individuals with different genotypes of vitamin D-related genes had different responses to vitamin D supplementation [37]. Polymorphism in several vitamin D genes (CYP2R1, CYP27A1, CYP27B1, CYP24A1, VDBP, and VDR) had been associated with vitamin D metabolism and regulated the activity of vitamin D [37]. Single nucleotide polymorphisms (SNP) in GC (rs4588 and rs7041), VDR (rs10735810), and CYP27B1 (rs10877012) also were reported associated with vitamin D status [38, 39]. GC (rs4588 and rs2282679) were associated with lower vitamin D status both before and after vitamin D supplementation [37]. So the patients with vitamin D status lower than 20 ng/mL might carry related genes with poor vitamin D response, no significant benefit was provided. Overall, vitamin D supplementation was encouraged for infertile patients with vitamin D status lower than 30 ng/mL.
The previous article showed that a short period of dietary intervention containing omega-3 Fas and vitamin D could improve the quality of embryo cleavage [21]. Our results showed that the individual components (vitamin D only) resulting in improved clinical pregnancy rate might be underdetermined. The multicomponent including Myo-Inositol, folic acid, melatonin vitamin E and D ect, improved the pregnancy rate which confirmed that not vitamin D exerted a positive influence on reproductive outcomes independently but synergistically. However, the sensitivity analysis (the exclusion of the study by Somigliana et al.) showed that infertile women treated with vitamin D only also had a significantly increased clinical pregnancy rate compared with the control group [13]. More researches about the effect of vitamin D supplementation on the clinical pregnancy rate with different drug type were needed.
Vitamin D is a fat-soluble steroid hormone, has lipophilic nature, and distributes in adipose tissue [40, 41]. Vitamin D has a slow turnover in the body with a half-life of approximately 2 months [40, 42]. Vitamin D could be metabolized by 25-hydroxylase, a liver enzyme, into 25(OH) D which has a half-life of 15 days [40, 42]. The (25(OH)D) again could be converted into calcitriol or 1,25(OH)2 D by enzyme CYP27B1 [40, 42]. 1,25(OH)2 D has a half-life of 15 hours [40, 43]. The pharmacokinetics of vitamin D can impact the effects of vitamin D supplementation, so the dosing regimen of vitamin D supplementation had to be taken into consideration. To maximize the chance of achieving pregnancy and minimize and minimize the detrimental and toxicity effects of vitamin D supplementation, we set the subgroup of total vitamin D dosage, duration, administration frequency, and daily vitamin D dosage to confirm the suitable intervention. When the total vitamin D dosage was too low (lower than 10,000 IU) or too high (higher than 500,000 IU), the clinical pregnancy rate had no significant increase. The total vitamin D dosage ranged from 10,000–500,000 IU might be proper for infertile patients. The infertile patients could achieve better reproductive outcomes when they got vitamin D (1,000–10,000 IU) supplementation every day that lasts for more than 30 days. In comparison to the vitamin D administrated weekly or at others interverals (monthly or longer intervals), this study yielded only positive results for daily treatment. That could be explained by the hypothesis that only daily vitamin D supplementation could maintain stable circulating concentrations over time [31, 44]. The infertile patients treated with vitamin D dose varied from 1000-10,000 IU daily could benefit from the supplementation. A dose lower than 1000 IU or higher than 10,000 IU daily failed to show that vitamin D could improve the clinical pregnancy rate of infertile patients. These results indicated that patients treated with a small daily dose might still be at risk of vitamin D deficiency, so the improvement had failed. This finding was consistent with the past researches that approximately 280 IU/d or 400 IU/d dose for several months had minimal, or even no effect on the circulating vitamin D [44, 45]. While large bolus dosing with vitamin D caused a dramatic fluctuation circulating 25(OH) D levels, which have little benefit, or even be adverse [46, 47]. That might be because the sudden increased vitamin D levels caused by the bolus vitamin D could trigger countervailing factors. Low response to bolus dosing of vitamin D leaded to increase of vitamin D level not as expected [48, 49]. 24-hydroxylase (CYP24A1) up-regulated by the bolus dosing of vitamin D could significantly increase 24,25(OH)2D3, down-regulate 1,25(OH)2D and inhibits immune-modulation for weeks or even months [48,49,50]. We summarized and discussed that moderate daily dosing of vitamin D supplementation was an appropriate dosing regimen. A suitable vitamin D dosing regimen could have positive effects on the clinical pregnancy rate of infertile patients.
Even though several clinical parameters were analyzed to figure out which parameter might regulate the reproductive outcomes, several limitations still existed in our study. The limitations mainly originated from the clinical heterogeneity of the included publications, including the different ethnicities, uncertain vitamin D status before and after vitamin D supplementation, duration of vitamin D supplementation, and the recruited infertile women of different etiology. Even though vitamin D supplementation was thought a safe and low-cost treatment, we still found the variation of vitamin D supplementation was quite large. Proper doses of vitamin D supplementation should be determined. Furthermore, infertile women in 3 articles had been shown that their serum vitamin D level got significantly increased after the intervention. The lack of vitamin D data after the intervention might mean it was possible vitamin D insufficient or deficiency was not changed, and the full effect of the intervention was not elicited. It is necessary to monitor the response to vitamin D supplements. The analysis of subgroups, according to the duration of vitamin D supplementation, should not be overlooked. The heterogeneity was high in all subgroups, so the result might be not reliable. This might possible because the parameter - duration was not an independent factor influencing the clinical pregnancy rate. The duration of vitamin D supplementation could be affected by the administration frequencies and total dosages of vitamin D supplementation. Patients with different genotypes have different responses to the supplementation, so how the guide medication according to the genotype also should be paid attention to. Vitamin D could be self-synthesized by the human body, and the level of vitamin D is vitiated with the seasons’ change. Whether the vitamin D supplementation should be adjusted according to the seasons is to be considered in the future. Recognizing the limitations of studies included in meta-analyses may stimulate future studies with better designs and methods that will improve available evidence and definitively define the role of vitamin D in ART.
Conclusion
Our study provides important evidence to support that taking appropriate vitamin D in combination with other components, before pregnancy, can increase reproductive outcomes, but not prevent infertile women from experiencing miscarriages. What’s more, women taking vitamin D supplements can be affected by the parameters of vitamin D. And the infertile patients at risk of vitamin D deficiency received moderate daily dosing of vitamin D supplementation are more likely to have good reproductive outcomes. However, the included articles have a small sample size and high heterogeneity, so further investigating the mechanism of vitamin D treatment acting on the infertile population is still necessary.
Availability of data and materials
The datasets used and/or analyzed during this study are available in this published article and supplementary.
References
Inal ZO, Inal HA, Gorkem U. Sexual function and depressive symptoms in primary infertile women with vitamin D deficiency undergoing IVF treatment. Taiwan J Obstetrics Gynecol. 2020;59:91–8.
Zhou Z, Zheng D, Wu H, Li R, Xu S, Kang Y, et al. Epidemiology of infertility in China: a population-based study. BJOG. 2017;125:432–41.
Farquhar C, Marjoribanks J. Assisted reproductive technology: An overview of Cochrane Reviews. Cohrane Database Syst Rev. 2018;8:CD010537.
Busso CE, Melo MA, Fernandez M, Pellicer A, Simon C. Implantation in IVF. Int Surg. 2006;91:S63–76.
Wang X, Zhao S, Zhou M, Jiang L. Factors influencing vitamin D levels in women attending the fertility clinic and the effect on assisted fertility outcomes. Ann Palliat Med. 2021;10:7813–22.
Evans KN, Bulmer JN. MD K, Hewison M: Vitamin D and Placental-Decidual Function. J Soc Gynecol Investig. 2004;11:263–71.
Ganguly A, Tamblyn JA, Finn-Sell S, Chan SY, Westwood M, Gupta J, et al. Vitamin D, the placenta and early pregnancy: effects on trophoblast function. J Endocrinol. 2018;236:JOE-17-0491.
Lerchbaum E, Rabe T. Vitamin D and female fertility. Curr Opin Obstetr Gynecol. 2014;26:145.
Chu J, Gallos I, Tobias A, Tan B, Eapen A, Coomarasamy A. Vitamin D and assisted reproductive treatment outcome: a systematic review and meta-analysis. Hum Reprod. 2018;33:65–80.
Halhali A, Acker GM, Garabédian M. 1,25-Dihydroxyvitamin D3 induces in vivo the decidualization of rat endometrial cells. J Reprod Fertil. 1991;91:59–64.
Espinola MSB, Bilotta G, Aragona C. Positive effect of a new supplementation of vitamin D3 with myo-inositol, folic acid and melatonin on IVF outcomes: a prospective randomized and controlled pilot study. Gynecol Endocrinol. 2020;37:1–4.
Fatemi F, Mohammadzadeh A, Sadeghi MR, Akhondi MM, Mohammadmoradi S, Kamali K, et al. Role of vitamin E and D3 supplementation in Intra-Cytoplasmic Sperm Injection outcomes of women with polycystic ovarian syndrome: A double blinded randomized placebo-controlled trial. Clin Nutr ESPEN. 2017;18:23–30.
Somigliana E, Sarais V, Reschini M, Ferrari S, Makieva S, Cermisoni GC, et al. Single oral dose of vitamin D3 supplementation prior to in vitro fertilization and embryo transfer in normal weight women: the SUNDRO randomized controlled trial. Am J Obstet Gynecol. 2021;225:283.e281–10.
Aflatoonian A, Arabjahvani F, Eftekhar M, Sayadi M. Effect of vitamin D insufficiency treatment on fertility outcomes in frozen-thawed embryo transfer cycles: A randomized clinical trial. Iran J Reprod Med. 2014;12:595–600.
Doryanizadeh L, Morshed-Behbahani B, Parsanezhad ME, Dabbaghmanesh MH, Jokar A. Calcitriol Effect on Outcomes of in Vitro Fertilization in Infertile Women with Vitamin D Deficiency: A Double-Blind Randomized Clinical Trial. Z Geburtshilfe Neonatol. 2021;225:226–31.
Heaney RP. Vitamin D in health and disease. Clin J Am Soc Nephrol. 2008;3:1535–41.
Iqbal SJ, Taylor WH. Treatment of vitamin D2 poisoning by induction of hepatic enzymes. Br Med J (Clin Res Ed). 1982;285:541–2.
Galior K, Grebe S, Singh R. Development of Vitamin D Toxicity from Overcorrection of Vitamin D Deficiency: A Review of Case Reports. Nutrients. 2018;10:E953.
Abedi S, Taebi M, Esfahani MHN. Effect of Vitamin D Supplementation on Intracytoplasmic Sperm Injection Outcomes: A Randomized Double-Blind Placebo-Controlled Trial. Int J Fertil Steril. 2019;13:18–23.
Wdowiak A, Filip M. The effect of myo-inositol, vitamin D3 and melatonin on the oocyte quality and pregnancy in in vitro fertilization: a randomized prospective controlled trial. Eur Rev Med Pharmacol Sci. 2020;24:8529–36.
Ajkab C, Pl C, Sjwbs C, Hlfbs B, Mm D, Ying C, et al. g NSMPDabcf: Effect of a 6-week "Mediterranean" dietary intervention on invitro humanembryo development: the Preconception Dietary Supplements in Assisted Reproduction double-blinded randomized controlled trial. Fertil Steril. 2020;113:260–9.
Zhao J, Liu S, Wang Y, Wang P, Qu D, Liu M, et al. Vitamin D improves in-vitro fertilization outcomes in infertile women with polycystic ovary syndrome and insulin resistance. Minerva Med. 2019;110:199–208.
Zhuang L, Cui W, Cong J, Zhang Y. Efficacy of Vitamin D Combined with Metformin and Clomiphene in the Treatment of Patients with Polycystic Ovary Syndrome Combined with Infertility. Iran J Public Health. 2020;48:1802–9.
Huizhen T, Tingting T, Hong Y, Chaohua L, Huilian C, Yao Z. Application and effect evaluation of multivitamin in patients undergoing assisted reproductive technology. Matern Child Health Care China. 2017;32:5684–6.
The Scientific Advisory Committee on Nutrition (SACN) recommendations on vitamin D. SACN vitamin D and health report. Public Health England. 2016.
Excellence NIfHaC. Vitamin D deficiency in adults – treatment and prevention. NICE. 2016. https://cks.nice.org.uk/vitamin-d-deficiency-in-adults-treatment-and-prevention. Accessed 10 Apr 2018.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30.
Palacios C, Kostiuk LK, Peña-Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019;7:Cd008873.
Daftary GS, Taylor HS. Endocrine regulation of HOX genes. Endocr Rev. 2006;27:331–55.
Ellis S, Tsiopanis G, Lad T. Risks of the “Sunshine pill” - a case of hypervitaminosis D. Clin Med (Lond). 2018;18:311–3.
Hollis BW, Wagner CL. The role of the parent compound vitamin d with respect to metabolism and function: Why clinical dose intervals can affect clinical outcomes. J Clin Endocrinol Metab. 2013;12:4619–28.
Mazess RB, Bischoff-Ferrari HA, Dawson-Hughes B. Vitamin D: Bolus Is Bogus-A Narrative Review. JBMR Plus. 2021;5.
Lucas ES, Vrljicak P, Muter J, Diniz-da-Costa MM, Brighton PJ, Kong CS, Lipecki J, Fishwick KJ, Odendaal J, Ewington LJ, Quenby S, Ott S, Brosens JJ. Recurrent pregnancy loss is associated with a pro-senescent decidual response during the peri-implantation window. Commun Biol. 2020;3:37.
Guo J, Liu S, Wang P, Ren H, Li Y. Characterization of VDR and CYP27B1 expression in the endometrium during the menstrual cycle before embryo transfer: implications for endometrial receptivity. Reprod Biol Endocrinol. 2020;18:24.
Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM. Maternal vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab. 2007;92:3517–22.
Bouillon R, Norman AW, Lips P. Vitamin D deficiency. N Engl J Med. 2007;357:1980–1.
Muindi JR, Adjei AA, Wu ZR, Olson I, Huang H, Groman A, Tian L, Singh PK, Sucheston LE, Johnson CS, Trump DL, Fakih MG. Serum vitamin D metabolites in colorectal cancer patients receiving cholecalciferol supplementation: correlation with polymorphisms in the vitamin D genes. Horm Cancer. 2013;4:242–50.
Mcgrath JJ, Saha S, Burne TH, Eyles DW. A systematic review of the association between common single nucleotide polymorphisms and 25-hydroxyvitamin D concentrations. Steroid Biochem Mol Biol. 2010;121:471–7.
Bu FX, Armas L, Lappe J, Zhou Y, Gao G, Wang HW, et al. Comprehensive association analysis of nine candidate genes with serum 25-hydroxy vitamin D levels among healthy Caucasian subjects. Hum Genet. 2010;128:549–56.
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81.
Jones G. Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr. 2008;88:582s–6s.
Vieth R. Vitamin D toxicity, policy, and science. J Bone Miner Res. 2007;22(Suppl 2):V64–8.
Vieth R. The mechanisms of vitamin D toxicity. Bone Miner. 1990;11:267–72.
Hollis BW, Johnson D, Hulsey TC, Ebeling M, Wagner CL. Vitamin D supplementation during pregnancy: double-blind, randomized clinical trial of safety and effectiveness. J Bone Miner Res. 2011;26:2341–57.
Vieth R, Chan P, Macfarlane GD. Efficacy and safety of vitamin D 3 intake exceeding the lowest observed adverse effect level. Am J Clin Nutr. 2001;73:288–94.
Kearns MD, Alvarez JA, Tangpricha V. Large, single-dose, oral vitamin D supplementation in adult populations: a systematic review. Endocr Pract. 2014;20:341–51.
Malihi Z, Wu Z, Lawes CMM, Scragg R. Adverse events from large dose vitamin D supplementation taken for one year or longer. J Steroid Biochem Mol Biol. 2019;188:29–37.
Owens DJ, Tang JC, Bradley WJ, Sparks AS, Fraser WD, Morton JP, et al. Efficacy of High-Dose Vitamin D Supplements for Elite Athletes. Med Sci Sports Exerc. 2017;49:349–56.
Ketha H, Thacher TD, Oberhelman SS, Fischer PR, Singh RJ, Kumar R. Comparison of the effect of daily versus bolus dose maternal vitamin D(3) supplementation on the 24,25-dihydroxyvitamin D(3) to 25-hydroxyvitamin D(3) ratio. Bone. 2018;110:321–5.
Hewison M. Vitamin D and the immune system: new perspectives on an old theme. Rheum Dis Clin N Am. 2012;38:125–39.
Acknowledgments
Not applicable.
Funding
Ting Qu reports grants from the Sichuan Medical Association (Q20055) and the Science and Technology Department of Sichuan, China (Grant no. 2022NSFSC1508).
Author information
Authors and Affiliations
Contributions
Xiangqian Meng and Jiayao Zhang accomplished the literature search and identified the eligible studies. Qi Wan and Jihua Huang completed the data extraction. Tingting Han achieved the assessment of the quality of the literature. Ting Qu and Lin-lin Yu supervised, made the conception and designed the research, wrote the manuscript. All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All data were collected from published literature.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional files 1: Table S1.
Risk of bias assessment of the randomized controlled trials for meta-analysis using the Cochrane tool. Table S2. Quality assessment of the cohort studies for the meta-analysis using the Newcastle-Ottawa scale.
Additional files 2: Fig. S1.
Sensitivity analysis for the effect of vitamin D supplementation on clinical pregnancy rate of infertile patients using random effect model (Odds Ratio).
Additional files 3: Fig. S2.
Forrest plot for the effect of vitamin D supplementation on the clinical pregnancy rate of infertile patients [leave Somigliana (2021) out].
Additional files 4: Fig. S3.
Sensitivity analysis for the effect of vitamin D supplementation on the clinical pregnancy rate in studies of vitamin D only supplementation using random effect model (Odds Ratio).
Additional files 5: Fig. S4.
Forrest plot for the effect of vitamin D supplementation on the clinical pregnancy rate in studies of vitamin D only supplementation [leave Somigliana (2021) out].
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Meng, X., Zhang, J., Wan, Q. et al. Influence of Vitamin D supplementation on reproductive outcomes of infertile patients: a systematic review and meta-analysis. Reprod Biol Endocrinol 21, 17 (2023). https://doi.org/10.1186/s12958-023-01068-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-023-01068-8