Abstract
The investigation about association between vitamin D level and clinical outcomes of assisted reproductive treatment showed various outcomes. This study aimed to review the correlation between vitamin D and outcomes of assisted reproductive treatment. The search was registered on the PROSPERO database (CRD42023458040). PubMed, Embase, Medline, ClinicalTrials.gov, and Cochrane databases were searched up to July 2023. Twenty-three observational studies were selected for meta-analysis. Comparing groups with deficient and ‘insufficient + sufficient’ vitamin D level, meta-analysis showed positive correlation between clinical pregnancy rate and vitamin D (OR 0.81, 95%CI: 0.70, 0.95, P = 0.0001). Comparing groups with ‘deficient + insufficient’ and sufficient vitamin D level, meta-analysis showed positive correlation between vitamin D and clinical pregnancy rate (OR 0.71, 95%CI: 0.55, 0.91, P = 0.006), vitamin D and live birth rate (OR 0.69, 95%CI: 0.54, 0.89, P = 0.003). Subgroup analysis did not show the source of high heterogeneity. No correlation was found in biochemical pregnancy rate, ongoing pregnancy rate, miscarriage rate and implantation rate. In dose-response meta-analysis, a nonlinear association was found between vitamin D levels and outcomes when levels are below approximately 24 ng/L. The study shows that vitamin D level is associated with clinical pregnancy rate and live birth rate. Low vitamin D level does not influence biochemical pregnancy rate, ongoing pregnancy rate, miscarriage rate and implantation rate. Furthermore, 24 ng/L may be a possible threshold of vitamin D concentration in assisted reproduction therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has been a growing focus on the role of vitamin D in the field of reproductive medicine. In foundational research, vitamin D has demonstrated significant modulation of Anti-Mullerian hormone (AMH) signaling and follicle-stimulating hormone receptor (FSHR) gene expression [1], thus modulating follicle development. Furthermore, vitamin D has been hypothesized to exert an influence on embryo implantation [2]. Evidence supports the notion that vitamin D upregulates essential target genes, which play critical roles in endometrial development, uterine receptivity, and implantation [3].
In clinical research, inquiries into the interplay between levels of vitamin D and the clinical outcomes of assisted reproductive treatment (ART) are abundant, but the outcomes remain controversial. Several studies have showed robust association between vitamin D and the success of ART [4,5,6,7,8]. Contrastingly, certain investigations have yielded inconclusive results, showing no evident correlation between vitamin D levels and pregnancy outcomes [9,10,11,12,13,14,15,16]. Meanwhile, there are studies showing adverse association between vitamin D and clinical pregnancy rate (CPR), chemical pregnancy rate, ongoing pregnancy rate, miscarriage rate, implantation rate, live birth rate (LBR) or embryo quality after ART [17,18,19]. Thus, a systematic review and meta-analysis is needed.
The threshold of serum vitamin D remains controversial till now. Vitamin D level is classified as deficiency (25(OH)D ≤ 20 ng/ml), insufficiency (21ng/ml ≤ 25(OH)D ≤ 29 ng/ml) according to American Endocrine Society Clinical Practice Guideline [20]. However, it has been suggested that assay only be used in monitoring certain conditions. Institute of Medicine (IOM) Committee Members claimed that serum 25(OH)D ≥ 20ng/ml was replete [21]. In this meta-analysis, infertile female patients were divided into 3 groups, namely 25(OH)D sufficient (≥ 30 ng/ml or ≥ 75nmol/ml), insufficient (20-30ng/ml or 50–75 nmol/ml) and deficient (< 20 ng/ml or < 50 nmol/ml). The primary objective of this systematic review and meta-analysis is to comprehensively examine the existing literature and investigate the association between vitamin D levels and ART outcomes. Also, we hope to find out potential influential factors by subgroup analysis and determine a more proper threshold for vitamin D by employing dose-response analysis.
Method
This systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO; CRD42023458040) and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Statement (For detailed information, please refer our PRISMA 2020 Checklist and MOOSE Checklist within the supplementary material).
Search Strategy
Two investigators independently carried out a literature search across multiple databases, including PubMed, Web of Science, ClinicalTrials.gov, Embase, MEDLINE, and the Cochrane Library. The search utilized a set of predefined keywords and medical subject heading (MeSH) terms, namely [(Vitamin D) OR (25-Hydroxyvitamin D) OR (Ergocalciferols) OR (Cholecalciferol) OR (Calcitriol)] AND [(assisted reproductive technology) OR (Fertilization in Vitro) OR (Sperm Injections, Intracytoplasmic) OR (Test Tube Babies) OR (IVF) OR (ICSI)] (see Supplementary file 1). The search was limited to English-language articles published until July 2023.
Selection Criteria
Two reviewers independently conducted the process of selection. If there was disagreement, a third reviewer would be consulted to help make the final decision through discussion among all three people. The study protocol established predefined criteria for inclusion and exclusion. Published observational studies were selected for analysis, including retrospective or prospective cohort studies, case-control studies, and cross-sectional studies. Vitamin D levels were stratified into three categories: deficient (< 20 ng/mL), insufficient (20–30 ng/mL), and sufficient (≥ 30 ng/mL). Inclusion criteria includes: (i) recruitment of women undergoing ART treatment, such as in vitro fertilization-embryo transfer (IVF-ET), intracytoplasmic sperm injection (ICSI), and preimplantation genetic testing/screening (PGT-PGS/PGD); (ii) report of vitamin D concentrations measured through either blood serum or follicular fluid tests. (iii) observational studies, and (iv) were published in English. Exclusion criteria includes: (i) reviews, conference articles, letters, animal studies or guidelines; (ii) reports related to patients participating in multicenter trials. (iii) studies with incomplete data.
Data Extraction
Two investigators independently performed data extraction. The extracted information from all included studies encompassed the following types: authors and year of publication, type of the studies, number of patients, female age, race and country, type of ART treatment, type of oocyte used in in-vitro fertilization (IVF) cycles (autologous or donated oocytes), time of sample collection, method of vitamin D assessment, vitamin D concentration, outcomes (clinical pregnancy rate, live birth rate, ongoing pregnancy rate, miscarriage rate and implantation rate) and conclusions (Tables 1 and 2).
Quality Assessment
The evaluation of the included studies’ quality was executed utilizing the Newcastle-Ottawa Scale (NOS) independently by two reviewers.
Statistical Analysis
We utilized Review Manager 5.3 and Stata 17.0 to conduct all statistical analyses. Heterogeneity among studies was assessed using both chi square and the heterogeneity index, in instances where significant heterogeneity was observed (I2 > 50%), we adopted the random effects model. Conversely, when heterogeneity was minimal (I2 ≤ 50%), the fixed effects model was employed. We conducted a sensitivity analysis to identify any studies that may have had an outsized impact on the overall pooled results. To assess publication bias, we employed funnel plot asymmetry and Egger’s test. Subgroup analyses were performed to isolate potential confounding factors and included the source of oocyte, source of vitamin D, race, study design, method of vitamin D assessment, and time of sample collection.
Dose-Response Meta-Analysis
In August 2017, the Methodology Group introduced a groundbreaking meta-regression method known as the Robust-error meta-regression (REMR) for synthesizing dose-response data. We employed this novel method to conduct the dose-response analysis. We calculated study-specific slopes (representing linear trends) and their corresponding 95% confidence intervals by employing natural logarithms of the odds ratios and confidence intervals. This analysis was conducted across various categories of vitamin D levels [22].
The method necessitated the availability of case distributions or non-case and odds ratios, along with their corresponding variance estimates, for a minimum of three quantitative usage categories. Studies that categorize patients into two groups based on their vitamin D levels were excluded from the dose-response meta-analysis.
Some original studies presented exposure ranges without indicating the average or median levels of exposure. To address this, we adopted the following estimation approach: for closed intervals, we determined the exposure level as the midpoint between the upper and lower limits; for open intervals (where either the upper or lower endpoint was provided), we treated the interval length of the adjacent group as the interval length of the target group and calculated the midpoint as the estimated average exposure level [23, 24].
Results
Literature Selection
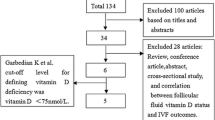
The electronic database search produced a total of 1,536 citations. Twenty-three [4,5,6,7,8,9,10, 13,14,15,16,17,18,19, 25,26,27,28,29,30,31,32,33] studies were included for meta-analysis. The PRISMA flow diagram of the review process is shown in Fig. 1.
Description of Studies and Participants
Table 1 demonstrates a summary of the main characteristics. Table 2 presents the extracted information pertaining to subgroup analysis from the original studies.
Quality of Studies
Newcastle–Ottawa Quality Assessment Scale (NOS) was used to evaluate the quality of the twelve studies. Studies were regarded as ‘high quality’ if they had a score > 5. Thirteen studies achieved a score of 6. Ten studies achieved a score between 7 and 8 (Supplementary file 2).
Clinical Pregnancy Rate
Deficient Vitamin D Level Versus ‘Insufficient + Sufficient’ Vitamin D Level
21 studies investigated the association between clinical pregnancy rate and vitamin D levels (Fig. 2C). The comparison was between ‘Deficient’ vitamin D level and ‘Insufficient + Sufficient’ vitamin D level. 5,588 infertile patients had sufficient or insufficient vitamin D, 6,054 had deficient vitamin D. Meta-analysis showed positive correlation between CPR and vitamin D (OR 0.81, 95%CI: 0.70, 0.95, P = 0.01). Since I2 > 50%, subgroup analyses were conducted.
(a) Meta-analysis of studies reporting CPR in sufficient vitamin D(≥ 30ng/ml) + insufficient vitamin D(20-30ng/ml) and deficient vitamin D(< 20ng/ml). (b) Meta-analysis of studies reporting CPR in sufficient vitamin D(≥ 30ng/ml) and deficient vitamin D(< 20ng/ml) + insufficient vitamin D(20-30ng/ml). (c) Sensitivity analysis on Deficient vitamin D level versus ‘Insufficient + Sufficient’ vitamin D level. (d) Sensitivity analysis on ‘Deficient + Insufficient’ vitamin D level versus Sufficient vitamin D level. Note: (1) refers to the data of follicular vitamin D, (2) refers to the data of serous vitamin D
To detect the origin of the heterogeneity, six subgroup analyses were conducted, including source of oocyte, source of vitamin D, race, study design, method of vitamin D assessment and time of sample collection (Table 3). The detailed forest plot results of the subgroup analyses can be found in Supplementary file 5.
‘Deficient + Insufficient’ Vitamin D Level Versus Sufficient Vitamin D Level
16 studies (7,450 participants) investigated the association between clinical pregnancy rate and serum vitamin D levels (Fig. 2b). The comparison was between ‘Deficient + Insufficient’ vitamin D level and ‘Sufficient’ vitamin D level. 1,076 infertile patients had sufficient vitamin D, 6,374 had deficient or insufficient vitamin D. Meta-analysis showed positive correlation between CPR and vitamin D (OR 0.71, 95%CI: 0.55, 0.91, P = 0.007). Since I2 > 50%, subgroup analyses were conducted.
To detect the origin of the heterogeneity, six subgroup analyses were conducted, including source of oocyte, source of vitamin D, race, study design, method of vitamin D assessment and time of sample collection (Table 4). The detailed forest plot results of the subgroup analysis can be found in Supplementary file 5.
Secondary Outcomes
In comparison between Deficient vitamin D level versus ‘Insufficient + Sufficient’ vitamin D level, no correlation was found in biochemical pregnancy rate, ongoing pregnancy rate, miscarriage rate, live birth rate, implantation rate. Specific information is provided in Supplementary file 3.
In comparison between ‘Deficient + Insufficient’ vitamin D level versus Sufficient vitamin D level, no correlation was found in biochemical pregnancy rate, ongoing pregnancy rate, miscarriage rate, implantation rate. However, a positive correlation was found (OR 0.69, 95%CI: 0.54, 0.89, P = 0.003) between vitamin D level and live birth rate, with a relatively low I2. Specific information is provided in Supplementary file 3.
Sensitivity Analysis
The outcomes of the sensitivity analysis are visually depicted in Fig. 2c and d. Notably, the removal of each individual study did not exert a substantial influence on the pooled odds ratios (ORs).
Publication Bias
Supplementary file 4 showed the funnel plot was relatively asymmetrical. However, Egger’s test (P = 0.367, P = 0.035) indicated no publication bias, with P = 0.367 in the first comparison between groups with ‘deficient + insufficient’ and sufficient vitamin D level, and P = 0.035 in the second comparison between groups with deficient and ‘insufficient + sufficient’ vitamin D level.
Dose-Response Analysis
Fifteen studies were included in the dose-response analysis, with 4283 cases among 7886 participants. The summary odds ratio was 0.89 (95%CI: 0.82,0.97) comparing ‘Deficient + Insufficient’ and ‘Sufficient’, with moderate heterogeneity (I2 = 44%, P = 0.04) (Fig. 3b). Publication bias was not evident in Egger’s test (P = 0.42) or Begg’s test (P = 0.30). In sensitivity analysis excluding one study at one time, the summary of odds ratio ranged from 0.88 (95%CI: 0.81, 0.97) when Fabris, 2014 was excluded to 0.88 (95%CI: 0.79, 0.97) when Rudick, 2014 or Chu, 2019was excluded (Fig. 3d). The summary odds ratio was 0.71 (95%CI: 0.56, 0.90) comparing ‘Deficient’ and ‘Insufficient + Sufficient’, with moderate heterogeneity (I2 = 54%, P = 0.008) (Fig. 3a). Publication bias was not evident in Egger’s test (P = 0.36) or Begg’s test (P = 0.39). The summary of odds ratio ranged from 0.67 (95%CI: 0.52, 0.86) when Anifandis, 2010 was excluded to 0.74 (95%CI: 0.58, 0.95) when Rudick, 2014 was excluded in sensitivity analysis (Fig. 3e).
(a) Meta-analysis of studies reporting CPR in sufficient vitamin D(≥ 30ng/ml) + insufficient vitamin D(20-30ng/ml) and deficient vitamin D(< 20ng/ml) among selected 15 studies; (b) Meta-analysis of studies reporting CPR in sufficient vitamin D(≥ 30ng/ml) and deficient vitamin D(< 20ng/ml) + insufficient vitamin D(20-30ng/ml) among selected 15 studies (c) Dose-response analyses between vitamin D levels and CPR. Hollow circles indicate logarithms of the odd ratios with size proportional to inverse of their variance; (d) Sensitivity analysis on Deficient vitamin D level versus Insufficient + Sufficient vitamin D level; (e) Sensitivity analysis on Deficient + Insufficient vitamin D level versus Sufficient vitamin D level. Note: (1) refers to the data of follicular vitamin D, (2) refers to the data of serous vitamin D
When the level of vitamin D is below approximately 60 nmol/L (24 ng/L), a clear non-linear association exists between the clinical pregnancy rate and dosage. However, as the vitamin D level exceeds approximately 24 ng/L, there is a slight improvement in the linear correlation between the two variables, and a modest increase in the degree of linear correlation with higher dosage can be observed (Fig. 3c).
Discussion
This systematic review and meta-analysis, comprising 23 individual studies, presents compelling evidence suggesting a potential link between serum vitamin D levels and the outcomes of ART. The results obtained from our analysis indicate that women who maintain sufficient vitamin D levels tend to exhibit increased probabilities of achieving successful live births, as well as positive pregnancy tests and clinical pregnancies, when undergoing ART procedures. Conversely, those individuals with deficient or insufficient levels of vitamin D demonstrate comparatively lower chances of achieving these favorable outcomes. However, there was no observed association between vitamin D levels and miscarriage rate, ongoing pregnancy rate, or biochemical pregnancy rate. Performing a sensitivity analysis is crucial in the meta-analysis of observational studies as it allows researchers to evaluate the stability and credibility of the combined point estimate [34]. The exclusion of any single study in turn did not result in substantial changes to the pooled ORs. This demonstrates the robustness of our research findings.
In the past few years, there have been five distinct meta-analyses published, examining the impact of vitamin D on the outcomes of IVF/ICSI, with varying and inconclusive findings [27, 35,36,37,38]. Compared to previous studies, our study has several advantages. (i) It includes the largest number of participants and the most extensive dataset among all published research in this field. (ii) Our sensitivity analysis yielded highly favorable results, which was not achieved in earlier studies. (iii) We conducted six subgroup analyses to identify potential sources of clinical heterogeneity in the relationship between vitamin D levels and ART outcomes. (iv) we introduced a novel approach by conducting a dose-response analysis, providing a new perspective on the issue of vitamin D threshold levels.
We performed 6 subgroup analyses to detect the origin of the heterogeneity of the clinical pregnancy rate, which is source of vitamin D, source of oocyte, race, study design, method of vitamin D assessment and time of sample collection. Unfortunately, none of these six subgroup analyses showed satisfactory heterogeneity test results. Nevertheless, some of the analyses still provided suggestive findings.
Muyayalo et al. measured the concentrations of vitamin D in both serum and follicular fluid concurrently, and examined their respective correlations with ART treatment outcomes [32]. They found that vitamin D levels in follicular fluid (FF), but not in serum, were associated with it. The observed result may be attributed to the potential antioxidant effect of vitamin D in human female gametes. It is possible that this effect is more pronounced within the follicular fluid compared to the bloodstream. Higher total antioxidant concentrations are linked to enhanced ovarian stimulation efficiency and pregnancy success in infertile patients [39]. Most studies did not differentiate between the concentrations of vitamin D in serum and follicular fluid, resulting in only three articles [5, 17, 32] being included in our subgroup analysis specifically focusing on follicular fluid. Most studies consistently show a positive link between serum and follicular fluid vitamin D levels, indicating that assessing vitamin D status in peripheral blood can reliably indicate its availability in the ovaries [9, 28, 32, 40,41,42,43,44,45].
Although there is clinical heterogeneity in the detection methods of vitamin D, our subgroup analysis did not reveal this result. Within-group heterogeneity only decreased in the ELISA and LC-MS group, with no significant statistical differences observed between groups.
According to a recent study, the administration of vitamin D supplements has been shown to enhance the survival and growth of antral follicles in addition to promoting oocyte maturation [46, 47]. Furthermore, vitamin D has been hypothesized to enhance endometrial receptivity and exert an influence on embryo implantation [2]. Evidence supports the notion that vitamin D, upon binding to its receptor (VDR), upregulates essential target genes, including HoxA10, which plays a critical role in endometrial development, uterine receptivity, and implantation [3]. Besides, sufficient vitamin D status is vital to ensure optimal gestation and maintain a healthy pregnancy [48].
The Endocrine Society defines vitamin D deficiency as serum calcitriol levels below 50 nmol/l (< 20 ng/ml), insufficiency as 50–75 nmol/l (21–29 ng/ml), and sufficiency as above 75 nmol/l (30 ng/ml). The Institute of Medicine defines deficiency as below 30 nmol/l (< 12 ng/ml), insufficiency as 30–50 nmol/l (12–20 ng/ml), and sufficiency as above 50 nmol/l (> 20 ng/ml). Besides, in the original studies included in our analysis, different cutoff points were used for vitamin D levels. Furthermore, the number of groups created based on vitamin D levels varied among studies, ranging from two to four or more groups. It is important to note that analyzing the data using only a single cutoff point may obscure potential effects of these thresholds on the outcomes. Consequently, utilizing a dose-response analysis offers a more thorough and reliable research methodology for exploring the connection between vitamin D levels and clinical pregnancy rate.
A recent study [49] carried out by Yu et al. at a hospital in China has demonstrated that there exists a non-linear connection between vitamin D levels and favorable pregnancy outcomes in women receiving ART when their vitamin D levels are below 25 ng/ml (approximately 79.5 nmol/L). The correlation becomes stronger when the vitamin D level exceeds 25 ng/ml. In our dose-response analysis, we integrated data from a total of 15 original studies, comprising reported intra-group mean values of vitamin D levels and estimated mean values obtained using scientific methods. The results of our study presented similarities to those of Yu et al. A nonlinear relationship was observed between vitamin D levels and outcome measures when levels were below approximately 24 ng/L. Specifically, below this threshold, vitamin D levels showed little impact on the pooled OR. However, beyond this threshold, the degree of correlation increased, indicating that higher levels of vitamin D directly contributed to an increase in the pooled effect size, as measured by OR.
Several studies have suggested the existence of biological thresholds for 25(OH)D conversion, below which sufficient conversion to 1,25-dihydroxyvitamin D may not be maintained [50]. We postulate that, from a clinical perspective, it is possible that minimal variations in vitamin D levels, whether slightly higher or lower than a very low threshold, do not yield qualitative changes and have no significant impact on pregnancy rates. This observation aligns with the previously mentioned conversion process of vitamin D within the body. In terms of statistical analysis, if the women included in the study predominantly exhibit vitamin D levels below a certain threshold (approximately 24 ng/L according to this study; approximately 25 ng/ml according to Yu et al.), or if appropriate grouping has not been conducted, it becomes challenging to observe intergroup differences. Thus, establishing a direct link between vitamin D levels and the likelihood of pregnancy may be hampered.
Certainly, our research does have some limitations. First, the dose-response analysis conducted in our study has revealed substantial challenges that warrant careful consideration. Many of the original studies included in this research have missing values for vitamin D levels. Although our estimation and conversion methods have been widely used in many reputable high-impact journals [51], there is still insufficient evidence to validate their accuracy, and they may introduce certain biases into the calculations [52]. Currently, IPD-based meta-analysis models have been proposed [53], and more data are becoming openly accessible to each researcher. IPD-based meta-analysis can provide results of higher evidential value, offering an excellent approach to producing more convincing conclusions in this field. Secondly, we cannot fully exclude the potential influence of seasonality and age on our study. Many studies have demonstrated that the season exerts a significant influence on an individual’s vitamin D status [54, 55]. The existing literature highlights the significant impact of seasonal fluctuations on vitamin D status, which is closely linked to solar (ultraviolet radiation B) UVB intensity [56, 57]. Thirdly, we contend that utilizing a uniform set of vitamin D level standards to assess vitamin D deficiency across different ethnicities lacks scientific rigor. Multiple studies have indicated there are variations in VDR gene polymorphisms across different ethnic groups [58, 59]. Therefore, a focused effort on establishing large-scale cohort studies specific to each ethnic group is crucial to investigate the threshold levels of vitamin D corresponding to different ethnicities. Such research aids in accurately assessing the extent of vitamin D deficiency among different ethnicities and formulating tailored intervention strategies. Additionally, it provides more precise reference values, enabling clinicians to offer personalized vitamin D supplementation recommendations to patients.
In the future, we anticipate the emergence of more extensive prospective clinical studies in this field, with the objective of elucidating the intricate association between vitamin D levels and comprehensive patient profiles during the ART process. By doing so, we aspire to accelerate the unraveling of the elusive threshold values pertaining to vitamin D, thereby enhancing our comprehension of its significance in optimizing ART outcomes.
Overall, the results of this review indicate that there is a correlation between vitamin D levels and both clinical pregnancy rates and live birth rates. Low vitamin D level does not influence ART outcomes in terms of biochemical pregnancy rate, ongoing pregnancy rate, miscarriage rate and implantation rate. Additionally, a nonlinear correlation was found between vitamin D levels and outcome measures when levels were below approximately 24 ng/L. Vitamin D levels showed little impact on the pooled OR below this threshold, while the degree of correlation increased beyond this threshold, suggesting that 24 ng/L may be a possible threshold of vitamin D concentration in assisted reproduction. More cohorts focusing on subgroups analysis and large size RCTs are needed in the future.
Data Availability
All figures and tables including template data collection forms, data extracted from included studies, data used for all analyses are publicly available in the manuscript.
References
Irani M, Merhi Z. Role of vitamin D in ovarian physiology and its implication in reproduction: a systematic review. Fertil Steril. 2014;102(2):460–e4683.
Subramanian A, et al. Preconception vitamin D and miscarriage in a prospective cohort study. Hum Reprod. 2022;37(10):2465–73.
Du H et al. Direct regulation of HOXA10 by 1,25-(OH)2D3 in human myelomonocytic cells and human endometrial stromal cells. Mol Endocrinol. 2005;19(9):2222–33.
Garbedian K, et al. Effect of vitamin D status on clinical pregnancy rates following in vitro fertilization. CMAJ Open. 2013;1(2):E77–82.
Neysanian GH, et al. The effects of serum and follicular fluid vitamin D levels on assisted Reproductive techniques: a prospective cohort study. Int J Fertil Steril. 2021;15(4):280–5.
Paffoni A, et al. Vitamin D deficiency and infertility: insights from in vitro fertilization cycles. J Clin Endocrinol Metab. 2014;99(11):E2372–6.
Polyzos NP, et al. Vitamin D deficiency and pregnancy rates in women undergoing single embryo, blastocyst stage, transfer (SET) for IVF/ICSI. Hum Reprod. 2014;29(9):2032–40.
Rudick BJ, et al. Influence of vitamin D levels on in vitro fertilization outcomes in donor-recipient cycles. Fertil Steril. 2014;101(2):447–52.
Firouzabadi RD, et al. Value of follicular fluid vitamin D in predicting the pregnancy rate in an IVF program. Arch Gynecol Obstet. 2014;289(1):201–6.
Franasiak JM, et al. Vitamin D levels do not affect IVF outcomes following the transfer of euploid blastocysts. Am J Obstet Gynecol. 2015;212(3):e3151–6.
Hosseinisadat R, et al. Assessment of the effect of serum and follicular fluid vitamin D and glucose on assisted reproductive technique outcome: a cross-sectional study. Int J Reprod Biomed. 2021;20(3):221–30.
Jiang L, et al. The effect of serum vitamin D levels in couples on embryo development and clinical outcomes. Reprod Biomed Online. 2019;38(5):699–710.
Ko JKY et al. 100 years of vitamin D: Effect of serum vitamin D level before ovarian stimulation on the cumulative live birth rate of women undergoing in vitro fertilization: a retrospective analysis. Endocr Connect. 2022;11(2).
van de Vijver A, et al. Vitamin D deficiency and pregnancy rates following frozen-thawed embryo transfer: a prospective cohort study. Hum Reprod. 2016;31(8):1749–54.
Yu Z, et al. Does vitamin D level associate with pregnancy outcomes in Chinese women undergoing in vitro fertilization/intracytoplasmic sperm injection-embryo transfer? A retrospective cohort study. J Obstet Gynaecol Res. 2023;49(3):835–45.
Cai S, et al. Impact of vitamin D on human embryo implantation-a prospective cohort study in women undergoing fresh embryo transfer. Fertil Steril. 2021;115(3):655–64.
Anifandis GM, et al. Prognostic value of follicular fluid 25-OH vitamin D and glucose levels in the IVF outcome. Reprod Biol Endocrinol. 2010;8:91.
Liu X, et al. Effect of vitamin D status on normal fertilization rate following in vitro fertilization. Reprod Biol Endocrinol. 2019;17(1):59.
Walz NL, et al. Serum vitamin D status is associated with increased blastocyst development rate in women undergoing IVF. Reprod Biomed Online. 2020;41(6):1101–11.
Holick MF, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30.
Rosen CJ, et al. IOM committee members respond to Endocrine Society vitamin D guideline. J Clin Endocrinol Metab. 2012;97(4):1146–52.
Xu C, Doi SAR. The robust error meta-regression method for dose–response meta-analysis. Int J Evid Based Healthc. 2018;16(3):138–44.
Bagnardi V et al. Light alcohol drinking and cancer: a meta-anal-ysis. Ann Oncol. 2013;24(2):301–308.
Aune D et al. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis . JAMA. 2014;311(15):1536–46.
Abadia L, et al. Serum 25-hydroxyvitamin D concentrations and treatment outcomes of women undergoing assisted reproduction. Am J Clin Nutr. 2016;104(3):729–35.
Banker M, Sorathiya D, Shah S. Vitamin D Deficiency does not Influence Reproductive outcomes of IVF-ICSI: a study of oocyte donors and recipients. J Hum Reprod Sci. 2017;10(2):79–85.
Chu J, et al. Vitamin D and assisted reproductive treatment outcome: a prospective cohort study. Reprod Health. 2019;16(1):106.
Ciepiela P, et al. Vitamin D as a follicular marker of human oocyte quality and a serum marker of in vitro fertilization outcome. J Assist Reprod Genet. 2018;35(7):1265–76.
Fabris A, et al. Impact of circulating levels of total and bioavailable serum vitamin D on pregnancy rate in egg donation recipients. Fertil Steril. 2014;102(6):1608–12.
Fabris AM, et al. Impact of vitamin D levels on ovarian reserve and ovarian response to ovarian stimulation in oocyte donors. Reprod Biomed Online. 2017;35(2):139–44.
Hasan HA, et al. Preconception Vitamin D Level and in Vitro fertilization: pregnancy outcome. Endocr Pract. 2023;29(4):235–9.
Muyayalo KP, et al. Low vitamin D levels in follicular fluid, but not in serum, are associated with adverse outcomes in assisted reproduction. Arch Gynecol Obstet. 2022;305(2):505–17.
Rudick B, et al. Characterizing the influence of vitamin D levels on IVF outcomes. Hum Reprod. 2012;27(11):3321–7.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-Value. Ann Intern Med. 2017;167(4):268–274.
Zhao J, et al. Whether vitamin D was associated with clinical outcome after IVF/ICSI: a systematic review and meta-analysis. Reprod Biol Endocrinol. 2018;16(1):13.
Cozzolino M, et al. How vitamin D level influences in vitro fertilization outcomes: results of a systematic review and meta-analysis. Fertil Steril. 2020;114(5):1014–25.
Iliuta F, et al. Women’s vitamin D levels and IVF results: a systematic review of the literature and meta-analysis, considering three categories of vitamin status (replete, insufficient and deficient). Hum Fertil (Camb). 2022;25(2):228–46.
Lv SS, et al. Serum vitamin D status and in vitro fertilization outcomes: a systematic review and meta-analysis. Arch Gynecol Obstet. 2016;293(6):1339–45.
Velthut A, et al. Elevated blood plasma antioxidant status is favourable for achieving IVF/ICSI pregnancy. Reprod Biomed Online. 2013;26(4):345–52.
Firouzabadi RD, et al. Value of follicular fluid vitamin D in predicting the pregnancy rate in an IVF program. Arch Gynecol Obstet. 2013;289(1):201–6.
Dabrowski F, Grzechocinska B, Wielgos M. The role of Vitamin D in Reproductive Health—A trojan horse or the Golden Fleece? Nutrients. 2015;7(6):4139–53.
Liu X, et al. Effect of vitamin D status on normal fertilization rate following in vitro fertilization. Reproductive Biology Endocrinol. 2019;17(1):59.
Aleyasin A, et al. Predictive value of the level of vitamin D in follicular fluid on the outcome of assisted reproductive technology. Eur J Obstet Gynecol Reproductive Biology. 2011;159(1):132–7.
Ozkan S, et al. Replete vitamin D stores predict reproductive success following in vitro fertilization. Fertil Steril. 2010;94(4):1314–9.
Anifandis GM, et al. Prognostic value of follicular fluid 25-OH vitamin D and glucose levels in the IVF outcome. Reproductive Biology Endocrinol. 2010;8(1):91.
Xu J et al. Vitamin D3 regulates follicular development and intrafollicular vitamin D biosynthesis and signaling in the primate ovary. Front Physiol.2018;9:1600.
Parikh G et al. Vitamin D regulates steroidogenesis and insulin-like growth factor binding protein-1 (IGFBP-1) production in human ovarian cells. Horm Metab Res. 2010;42(10):754–7.
Varshney S et al. Disrupted placental vitamin D metabolism and calcium signaling in gestational diabetes and pre-eclampsia patients. Endocrine. 2023;80(1):191–200.
Yu Z, et al. Does vitamin D level associate with pregnancy outcomes in Chinese women undergoing in vitro fertilization/intracytoplasmic sperm injection-embryo transfer? A retrospective cohort study. J Obstet Gynecol Res. 2022;49(3):835–45.
de Boer IH et al. Serum 25-hydroxyvitamin D concentration and risk for major clinical disease events in a community-based population of older adults: a cohort study. Ann Intern Med. 2012;156(9):627–34.
Aune D et al. Dietary fibre, whole grains, and risk of colorectal cancer: systematic review and dose-response meta-analysis of prospective studies. BMJ. 2011;343:d6617.
Xu C et al. Fat intake is not linked to prostate cancer: a systematic review and dose-response meta-analysis. PLoS ONE. 2015;10(7):e0131747.
Vale CL et al. Adjuvant or early salvage radiotherapy for the treatment of localised and locally advanced prostate cancer: a prospectively planned systematic review and meta-analysis of aggregate data. Lancet. 2020;396(10260):1422–1431.
Hu Y et al. Vitamin D nutritional status and its related factors for Chinese children and adolescents in 2010–2012. Nutrients. 2017;9(9):1024.
Michaëlsson K et al. The seasonal importance of serum 25-hydroxyvitamin D for bone mineral density in older women. J Intern Med. 2017;281(2):167–178.
Yu HJ et al. Analysis of 25-hydroxyvitamin D status according to age, gender, and seasonal variation. J Clin Lab Anal. 2016;30(6):905–911.
O’Neill CM et al. Seasonal changes in vitamin D-effective UVB availability in Europe and associations with population serum 25-hydroxyvitamin D. Nutrients. 2016;8(9):533.
Ingles SA. Can diet and/or sunlight modify the relationship between vitamin D receptor polymorphisms and prostate cancer risk? Nutr Rev. 2007;65(8 Pt 2):S105–7.
Ingles SA et al. Strength of linkage disequilibrium between two vitamin D receptor markers in five ethnic groups: implications for association studies. Cancer Epidemiol Biomarkers Prev. 1997;6(2):93–8.
Acknowledgements
Not applicable.
Funding
The study was supported by funding from the projects of Sichuan Science and Technology Program (H.Y, Sichuan Natural Science Foundation for Youth, China, NO. 2022NSFSC1281) and Sichuan Medical Association Foundation (H.Y, China, NO. S21006).
Author information
Authors and Affiliations
Contributions
CHX and XQA jointly screened and analyzed all the data. CHX provided the main conceptual framework for the analysis, while XQA made significant contributions to manuscript writing. XMT, DZY, YH contributed to the interpretation of the data. QD and QLK contributed to the revision of the manuscript.
All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Consent for Publication
Informed consent was obtained from all authors in the study.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Competing Interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, C., An, X., Tang, X. et al. Association Between Vitamin D Level and Clinical Outcomes of Assisted Reproductive Treatment: A Systematic Review and Dose-Response Meta-Analysis. Reprod. Sci. (2024). https://doi.org/10.1007/s43032-024-01578-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43032-024-01578-9