Abstract
Background
To minimize the rate of in vitro fertilization (IVF)- associated multiple-embryo gestation, significant efforts have been made. Previous studies related to machine learning in IVF mainly focused on selecting the top-quality embryos to improve outcomes, however, in patients with sub-optimal prognosis or with medium- or inferior-quality embryos, the selection between SET and DET could be perplexing.
Methods
This was an application study including 9211 patients with 10,076 embryos treated during 2016 to 2018, in Tongji Hospital, Wuhan, China. A hierarchical model was established using the machine learning system XGBoost, to learn embryo implantation potential and the impact of double embryos transfer (DET) simultaneously. The performance of the model was evaluated with the AUC of the ROC curve. Multiple regression analyses were also conducted on the 19 selected features to demonstrate the differences between feature importance for prediction and statistical relationship with outcomes.
Results
For a single embryo transfer (SET) pregnancy, the following variables remained significant: age, attempts at IVF, estradiol level on hCG day, and endometrial thickness. For DET pregnancy, age, attempts at IVF, endometrial thickness, and the newly added P1 + P2 remained significant. For DET twin risk, age, attempts at IVF, 2PN/ MII, and P1 × P2 remained significant. The algorithm was repeated 30 times, and averaged AUC of 0.7945, 0.8385, and 0.7229 were achieved for SET pregnancy, DET pregnancy, and DET twin risk, respectively. The trend of predictive and observed rates both in pregnancy and twin risk was basically identical. XGBoost outperformed the other two algorithms: logistic regression and classification and regression tree.
Conclusion
Artificial intelligence based on determinant-weighting analysis could offer an individualized embryo selection strategy for any given patient, and predict clinical pregnancy rate and twin risk, therefore optimizing clinical outcomes.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
For decades, discussions about how to improve the clinical outcomes of in vitro fertilization (IVF) treatment have persisted. Multiple-embryo transfer was suggested to increase the possibility of successful implantation but inevitably elevated the risk of multiple-embryo gestation. IVF-associated multiple pregnancies exhibit significant financial, social, and medical implications [1, 2]. Even though the transfer of embryos has been limited to no more than two in recent years, the overall twin rate worldwide after assisted reproduction has still varied from 15 to 30% [3]. The incidences of premature birth, low birth weight, cerebral palsy, neurological complications, and perinatal mortality of twin pregnancy markedly increased compared with singleton pregnancy [4]. To minimize the rate of multiple-embryo gestation, significant efforts, including individualized service provision and single embryo transfer (SET) enhancement, have been made in the course of these decades.
Embryo morphological analysis is the routine method for selecting the highest-quality embryos to transfer. It is commonly suggested to perform SET on prognostically good patients with a top-quality embryo and to perform double embryo transfer (DET) on prognostically poor patients in whom good-quality embryo is unavailable in the IVF lab. In a large proportion of IVF patients with sub-optimal prognosis or with medium- or inferior-quality embryos, the selection between SET and DET could be perplexing. Because many features have been shown to influence embryo implantation potential positively or negatively in IVF [5,6,7,8], developing an optimal embryo selection plan to balance maximum clinical pregnancy rate and minimum twin risk is complicated for IVF clinicians. Therefore, a more precise, quantified, stable embryo selection model based on all possible influencing determinants needs to be constructed. This will potentially offer evidence-based patient counseling and predictable successful chances for any given patient.
Artificial intelligence (AI) represents the combination of machine learning, and a moderation and self-adapting prediction model. Previous studies related to machine learning in IVF mainly focused on selecting the top-quality embryos to improve IVF outcomes [9,10,11,12,13]. Developing a flexible, individualized embryo selection approach based on available embryos of various qualities and different twin rate threshold settings is another promising issue.
The purpose of our study is to construct an individualized embryo selection strategy and pregnancy prediction model, developed by stacking machine learning, to identify features correlated with embryo implantation potential and to evaluate available embryos’ implantation chances quantitatively. We aim to balance maximal clinical pregnancy and minimal acceptable twin risk in IVF with this model and validate its clinical effectiveness and practicability in subsequent cycles.
Materials and methods
Study design and participants
IVF patients in Tongji Hospital between January 2016 and December 2018, with one or two embryo transfers in the fresh cycle, were enrolled in our study. Exclusion criteria included patients with (1) blastocyst transfer in fresh cycle; (2) oocyte donation cycles; (3) vitrified/warmed oocytes; (4) oocytes partially cryopreserved in fresh cycle; (5) combined vitrified/warmed embryo transfers. In total, 5828 patients, between January 2016 and March 2018 were included as the training set to construct our model. Thirty-eight features were analyzed in our study, and their baselines on training and validation sets were exhibited, among which 21 main variables were selected and listed in Table 1, including patient features, embryo morphology features, and embryo scores. After model construction, the developed embryo selection strategy was applied to guide the selection of SET or DET in 3383 individual cases between April and December 2018 as the validation set.
Controlled ovarian hyperstimulation, embryo culture, and pregnancy ascertain
IVF patients were treated with controlled ovarian hyperstimulation (COH) by gonadotropin-releasing hormone (GnRH) agonist or GnRH antagonist, as previously described [14, 15]. When two dominant follicles reached 17–18 mm in diameter, oocytes were retrieved transvaginally 36–38 h after a human chorionic gonadotropin (hCG) trigger. Embryos were cultured in G1 medium (Vitrolife, Sweden) after fertilization and transferred on day 3. Subsequently, biochemical pregnancy was ascertained by a positive serum hCG 2 weeks after embryo transfer with serial elevation. Clinical pregnancy was defined as a gestational sac and active fetal heartbeat on ultrasound demonstration 8 weeks after embryo transfer.
Model construction, feature selection, and validation
According to previous studies, the outcome of DET is not a simple binomial distribution with respect to two transferred embryos [16]. Therefore, a hierarchical model with two levels was established to learn single embryo implantation potential and the impact of double embryos transferred simultaneously. In the first level, patient and embryo features were applied to predict the implantation chance for single embryo, from which the output value was directly treated as the predicted pregnancy chance. For DET, the respective pregnancy probability of two embryos (P1 and P2) was initially predicted by the first level calculation, then another two features, generated by addition (P1 + P2) and multiplication (P1 × P2), were also included, followed by the combination of generated features and patient features as the input for the second level. Two models were developed in the second level, one to predict the DET pregnancy chance and the other to predict the DET twin risk. The overall flowchart of our model is shown in Fig. 1. The first-level model was trained by all data except DET with only one embryo implantation, whereas the second-level models were trained by all DET data.
The overall flowchart of the proposed hierarchical model. The first-level model was trained using all data except double embryo transfer (DET), with only one embryo implantation to predict single-embryo implantation outcomes. The second level contains two models, which were trained using DET data to predict both DET implantation outcomes and twin risks
The machine learning system applied here was XGBoost [17]. XGBoost is a scalable machine learning system for tree boosting, which uses the boosting technique to train multiple trees. In other words, XGBoost is an ensemble of multiple decision trees. Unlike random forest, which generates trees by randomly selecting a subset of training sets and features, XGBoost generates decision trees one by one, based on the performance of the previous generated trees. And comparing to single decision tree algorithm such as C4.5 or CART, ensemble of trees can achieve better performance. Moreover, this system can automatically deal with missing values and assign the importance score for each feature, which was applied for feature selection. Nineteen features were selected and are marked by asterisks in Table 1.
As the training procedure was completed, the performance of the model was evaluated with the area under the curve (AUC) of the receiver operating characteristic (ROC) curve [18]. Multiple regression analyses were also conducted on the 19 selected features, with the glm function in R [19] to demonstrate the differences between feature importance for prediction and statistical relationship with outcomes.
Embryo selection strategy development
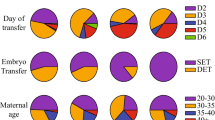
Subsequently, an embryo selection strategy to maximize the pregnancy chance with a controlled twin rate threshold setting was developed. As shown in Fig. 2, for any given acceptable twin rate threshold, the pregnancy and twin rate could be predicted for every possible embryo selection strategy, including one or two best embryos to transfer or the combination of one best embryo and one medium-quality embryo. Moreover, if the transfer failed in the fresh cycle, the plan would be redeveloped with the remaining embryos, following the same protocol until all embryos were transferred or a new cycle was started. With this selection strategy, the prediction model could effectively increase the percentages of elective SET patients and provide plausible plans for DET patients in IVF.
Statistical analysis
Continuous variables were presented as mean ± standard deviation. Categorical variables were presented as percentage encoded by one-hot encoding for analysis. For XGBoost algorithm, we used the implementation from scikit-learn (https://xgboost.readthedocs.io/en/latest/python/ python_api.html) using Python. The parameters were as follows: max_depth = 5, min_child_weight = 1, learning_rate = 0.1, n_estimators = 100, gamma = 0, subsample = 0.8, colsample_bytree = 0.8. Other parameters were set by default.
Results
Variable analysis using training data (January 2016 to march 2018)
The results of multiple regression analyses are shown in Table 2. For a SET pregnancy, the following variables remained significant: age, attempts at IVF, estradiol level on hCG day, and endometrial thickness. For DET pregnancy, age, attempts at IVF, endometrial thickness, and the newly added P1 + P2 remained significant. For DET twin risk, age, attempts at IVF, 2 pronucleus (PN)/ metaphase II (M II), and P1 × P2 remained significant.
Feature importance of the hierarchical model
In the XGBoost algorithm, the feature importance means the number of times that a feature is used to split the data across all trees. A higher feature importance score represents greater value for prediction. Figure 3 shows the feature importance in the hierarchical model for a SET pregnancy, a DET pregnancy, and DET twin risk. Some features are not shown in Fig. 3 because the corresponding importance was zero, which means these features were not used for prediction.
For SET, as shown in Table 2, the luteinizing hormone (LH) level and follicle-stimulating hormone (FSH) level were not statistically significant, yet they were the third- and sixth-important features for the first-level model. The same phenomenon was observed for FSH, LH, and antral follicle count (AFC) in DET pregnancy and DET twin risk prediction. Although P1 × P2 was significantly correlated with DET twin risk, it was hardly used by either level model.
Model validation results
The algorithm was repeated 30 times to eliminate the interference of random factors, and averaged AUCs of 0.7945, 0.8385, and 0.7229 were achieved for SET pregnancy, DET pregnancy, and DET twin risk, respectively. The ROC curve in one single run is shown in Fig. 4.
To validate the effectiveness of the developed embryo selection strategy, the consistency between the predicted chance and the observed actual outcomes was analyzed, as shown in Fig. 5. The trend of predictive and observed rates both in pregnancy and twin risk was basically identical, although with a slight elevation in predictive rates.
To validate the prediction performance among XGBoost and other algorithms such as logistic regression (LR) and classification and regression tree (CART), we also performed a non-parametric multiple comparison test using Dunn’s procedure [20], with a p-value correction using the False Discovery Rate method [21]. The results are shown in Fig. 6, where the significant ones (p < 0.05) are marked in asterisk. In general, XGBoost outperformed the other two algorithms with obvious prediction power in SET pregnancy prediction and DET twin risk prediction and similar performance in DET pregnancy prediction task.
Discussion
One of the most overwhelming challenges in contemporary assisted reproductive technology (ART) is how to narrow the gap in perinatal and neonatal outcomes between spontaneous pregnancy and assisted pregnancy, usually caused by multiple-embryo transfer and implantation [22]. In recent decades, SET has been advocated in IVF to prevent multiple pregnancies while led to the concerns of decreased IVF success [3, 23, 24]. Therefore, precise embryo selection for SET and twin risk warning for DET are particularly necessary. In this paper, a novel hierarchical model was constructed and validated to optimize embryo selection strategies and successfully predict pregnancy for both SET and DET, as well as predict the twin risk of DET for each individual. Subsequently, we validated our model on 3383 patients, and the results showed that our model had achieved an acceptable performance on embryo selection and twin risk prediction for each individual, as shown in Figs. 4 and 5.
It is generally accepted that embryos with similar morphology present variable implantation probability, depending on other assessed features such as patient characteristics and cycle demographics. Many features, including age, FSH level, anti-Mullerian hormone (AMH) and embryo quality, have been reported as independent impact factors on oocyte variability and embryo implantation potential [5, 25,26,27,28]. Machine learning is considered a powerful mathematical tool for correlation analysis when huge data is involved; therefore, AI has been introduced in embryo variability prediction in many articles [29, 30]. By increasing the information of the input features, the predictive power of the proposed model may be improved. Similarly, 19 features from the initial data sets were considered in the current study to construct the predictive power in our model. It is noteworthy that although previous models may have helped predict the implantation potential of a specific embryo, they did not offer a reasonable and optimal guidance to the embryo selection determination in clinical practice.
Minaretzis et al. [31] once presented an embryo selection strategy of transferring one additional good-quality embryo for each 5 years of incremental increase in maternal age to improve IVF outcome by multivariate analysis of factors predictive of successful live birth. Because maternal age was the only influencing factor to be considered, the recommended strategy was not so accurate or comprehensive. Kaufmann et al. [32] reported a neural networks predicting model in IVF, where four input parameters were included and the overall accuracy was 59%. Uyar et al. [33] proposed a Support Vector Machine (SVM) method in embryo implantation prediction in terms of Area Under ROC curve (0.712 ± 0.032), when 12 features were included.
Vaegter et al. [16] also constructed a predictive model for an embryo transfer strategy, in which only one embryo was transferred if the predictive risk of twin implantation was above 15%, using the two highest scored embryos. While validating this predictive model, the actual twin rate was 3.8%, which was far lower than the expected 15% setting, accompanied by a decreased live birth rate. Unlike previous studies, a novel strategy in embryo selection based on an accurate embryo potential prediction and twin risk assessment was developed in our model. The model not only guides a determination of the number of embryos for transfer and the specific embryo selection, but also presents a relatively accurate prediction of the pregnancy rate and twin risk of the corresponding selection scheme.
Because SET was not arbitrarily implemented in all IVF patients, twin pregnancy was inevitable. However, the acceptable twin rate threshold varied among different countries, even among different IVF centers. The greatest strength of our model was that the embryo selection strategy we developed varied correspondingly to patients’ characteristics and embryo morphology parameters as long as different twin rate thresholds were set. Therefore, the selection strategy model is applicable to any IVF center in any country. In such a situation, embryologists can input their accepted twin rate setting on the model to generate their guided embryo selection strategies and present a predictable pregnancy possibility and twin rate assessment.
More important, the predictive twin risk indicated that the transferred two embryos were neither a simplified embryo implantation nor an implantation of two independent samples. This principle was previously discussed in an embryo-uterus modeling framework [34,35,36]. A higher twin rate than expected would be achieved if the implantation chances of the embryos transferred together were completely independent of one another [16]. As shown in Fig. 3, E2 on hCG day, endometrial thickness, patient age, FSH, and AFC were ranked within top seven in the feature importance for the prediction of SET pregnancy, DET pregnancy, and twin risk, although with slightly different ranking. However, LH and attempt times of IVF, which were key in predicting SET pregnancy, were less weighted in DET pregnancy and twin risk prediction. Considering the variability of confounding factors, a two-level algorithm was introduced in our model for DET prediction to achieve a satisfying predictive model. Furthermore, unlike previous researches, which only considered significant influencing factors in model construction [37,38,39], concomitant investigation in our DET model provided a novel insight: that even if one variable were not statistically significant, it might still be important for machine learning models to predict final outcomes.
To minimize twin risk, some researchers also constructed a predictable model and validated it in subsequent IVF cycles, and the results showed a significantly reduced twin rate (from 25.2 to 3.8%) [16]. However, the proportion of SETs was greatly increased (11.3 to 75.5%), and surplus embryos would be preserved for future use, resulting in a reduced live birth rate in fresh cycle (29.0 to 25.1%). Even though the cumulative live birth rate (CLBR) was not affected, patients had to pay more fees and spend more time for a successful pregnancy in subsequent frozen-thawed cycles. Luke et al. [40] also reported a similar conclusion of comparative CLBR and decreased multiple births in SETs over two cycles, compared to DET in one cycle. In our algorithm, conversely, the pregnancy rate and twin risk were assessed and predicted simultaneously in the fresh cycle, and further validation showed that it effectively reduced twin risk without compromising clinical pregnancy in the fresh cycle.
The recommended embryo selection strategy in our model provides decision support to embryologists with higher accuracy and efficiency. For a large proportion of IVF patients with suboptimal prognosis, which plan to choose was a dilemma to embryologists, because prediction judgment was based on their clinical experience instead of on the analysis of thousands of embryos and patient records prior to each embryo transfer [41, 42]. Besides, it may also act as a counseling tool for clinicians to evaluate the chance of pregnancy before the transfer procedure.
Previous research to establish similar predictive models were problematic due to the limited number of involved features or dramatic distinction between the predicted value and the actual situation [16, 31]. The model in the current study guides a determination of the number of embryos for transfer and the specific embryo selection, based on the analysis of a large number of features. In addition, the predicted pregnancy rate and twin risk of the corresponding selection scheme were relatively more accurate. More significantly, our model provides a flexible strategy, with individualized embryo selection for any given patient and varied operations corresponding with any setting acceptable twin rate threshold.
One shortcoming of our predictive model was that the predicted mean value was slightly elevated compared to the actual observed rate for both pregnancy and twin rates in validation, although a modest discrimination was also reported in the previous prediction model in ART [43,44,45]. The model should be adjusted and improved to make the predictive value more closely agree with the actual virtue in the future verification. Besides, the model was developed and validated using data from a single center. As future work, we will need to be much more rigorous with additional data sets demonstrating the predictive value, using the same parameters, as well as applying them in different centers.
Conclusions
In our study, we constructed and validated an individualized embryo selection strategy and pregnancy prediction model developed by stacking machine learning. This prediction model could provide an accurate and individualized embryo selection strategy for any given patient as well as in any twin risk threshold setting and balance a delicate correlation between clinical pregnancy and twin risk rate; it therefore promises a better IVF outcome without compromising pregnancy success and controlled twin risk.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- IVF:
-
In vitro fertilization
- SET:
-
Single embryo transfer
- DET:
-
Double embryo transfer
- AI:
-
Artificial intelligence
- COH:
-
Controlled ovarian hyperstimulation
- GnRH:
-
Gonadotropin-releasing hormone
- hCG:
-
Human chorionic gonadotropin
- AUC:
-
Area under the curve
- ROC:
-
Receiver operating characteristic
- FSH:
-
Follicle-stimulating hormone
- LH:
-
Luteinizing hormone
- AFC:
-
Antral follicle count
- LR:
-
Logistic regression
- CART:
-
Classification and regression tree
- ART:
-
Assisted reproductive technology
- AMH:
-
Anti-Mullerian hormone
- CLBR:
-
Cumulative live birth rate
References
Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Warner L, et al. Assisted reproductive technology surveillance-United States, 2014. MMWR Surveill Summ. 2017;66(6):1–24. https://doi.org/10.15585/mmwr.ss6606a1.
Chambers GM, Ledger W. The economic implications of multiple pregnancy following ART. Semin Fetal Neonatal Med. 2014;19(4):254–61. https://doi.org/10.1016/j.siny.2014.04.004.
Meldrum DR, Adashi EY, Garzo VG, Gleicher N, Parinaud J, Pinborg A, et al. Prevention of in vitro fertilization twins should focus on maximizing single embryo transfer versus twins are an acceptable complication of in vitro fertilization. Fertil Steril. 2018;109(2):223–9. https://doi.org/10.1016/j.fertnstert.2017.12.005.
Bergh T, Ericson A, Hillensjö T, Nygren KG, Wennerholm UB. Deliveries and children born after in-vitro fertilisation in Sweden 1982-95: a retrospective cohort study. Lancet. 1999;354(9190):1579–85. https://doi.org/10.1016/S0140-6736(99)04345-7.
Van Loendersloot L, Van Wely M, Limpens J, Bossuyt PM, Repping S, van der Veen F. Predictive factors in in vitro fertilization (IVF): a systematic review and meta-analysis. Hum Reprod Update. 2010;16(6):577–89. https://doi.org/10.1093/humupd/dmq015.
Rienzi L, Vajta G, Ubaldi F. Predictive value of oocyte morphology in human IVF: a systematic review of the literature. Hum Reprod Update. 2010;17(1):34–45.
Iliodromiti S, Kelsey TW, Wu O, Anderson RA, Nelson SM. The predictive accuracy of anti-Müllerian hormone for live birth after assisted conception: a systematic review and meta-analysis of the literature. Hum Reprod Update. 2014;20(4):560–70. https://doi.org/10.1093/humupd/dmu003.
Fang T, Su Z, Wang L, Yuan P, Li R, Ouyang N, et al. Predictive value of age-specific FSH levels for IVF-ET outcome in women with normal ovarian function. Reprod Biol Endocrinol. 2015;13(1):63. https://doi.org/10.1186/s12958-015-0056-6.
Corani G, Magli C, Giusti A, Gianaroli L, Gambardella LM. A Bayesian network model for predicting pregnancy after in vitro fertilization. Comput Biol Med. 2013;43(11):1783–92. https://doi.org/10.1016/j.compbiomed.2013.07.035.
Debón A, Molina I, Cabrera S. Mathematical methodology to obtain and compare different embryo scores. Math Comput Model. 2013;57(5–6):1380–94. https://doi.org/10.1016/j.mcm.2012.11.027.
Guerif F, Le Gouge A, Giraudeau B, Poindron J, Bidault R, Gasnier O, et al. Limited value of morphological assessment at days 1 and 2 to predict blastocyst development potential: a prospective study based on 4042 embryos. Hum Reprod. 2007;22(7):1973–81.
Morales DA, Bengoetxea E, Larrañaga P. Selection of human embryos for transfer by Bayesian classifiers. Comput Biol Med. 2008;38(11–12):1177–86. https://doi.org/10.1016/j.compbiomed.2008.09.002.
Roberts SA. Models for assisted conception data with embryo-specific covariates. Stat Med. 2007;26(1):156–70. https://doi.org/10.1002/sim.2525.
Zhu L, Xi Q, Zhang H, Li Y, Ai J, Jin L. Blastocyst culture and cryopreservation to optimize clinical outcomes of warming cycles. Reprod BioMed Online. 2013;27(2):154–60. https://doi.org/10.1016/j.rbmo.2013.04.006.
Zhu L, Xi Q, Nie R, Chen W, Zhang H, Li Y. Rescue intracytoplasmic sperm injection: a prospective randomized study. J Reprod Med. 2011;56(9–10):410–4.
Vaegter KK, Berglund L, Tilly J, Hadziosmanovic N, Brodin T, Holte J. Construction and validation of a prediction model to minimize twin rates at preserved high live birth rates after IVF. Reprod BioMed Online. 2019;38(1):22–9. https://doi.org/10.1016/j.rbmo.2018.09.020.
Chen T, Guestrin C. XGBoost: A scalable tree boosting system. In: Proc Int’l Conf on Knowledge Discovery and Data Mining. San Francisco, CA; 2016.
Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148(3):839–43. https://doi.org/10.1148/radiology.148.3.6878708.
Dobson AJ, Barnett AG. An introduction to generalized linear models, fourth edition: Chapman and Hall/CRC; 2018.
Dunn OJ. Multiple comparisons using rank sums. Technometrics. 1964;6:214–52.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Stat Methodol. 1995;57:289–300.
Helmerhorst FM, Perquin DA, Donker D, Keirse MJ. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004;328(7434):261–0. https://doi.org/10.1136/bmj.37957.560278.EE.
Drakopoulos P, Blockeel C, Stoop D, Camus M, de Vos M, Tournaye H, et al. Conventional ovarian stimulation and single embryo transfer for IVF/ICSI. How many oocytes do we need to maximize cumulative live birth rates after utilization of all fresh and frozen embryos? Hum Reprod. 2016;31(2):370–6.
Van Voorhis B, Mejia RB. Single-embryo transfer point-it is the way forward. Fertil Steril. 2017;108(5):757. https://doi.org/10.1016/j.fertnstert.2017.08.030.
Cai Q, Wan F, Appleby D, Hu L, Zhang H. Quality of embryos transferred and progesterone levels are the most important predictors of live birth after fresh embryo transfer: a retrospective cohort study. J Assist Reprod Genet. 2014;31(2):185–94. https://doi.org/10.1007/s10815-013-0129-4.
Lee TH, Chen CD, Tsai YY, Chang LJ, Ho HN, Yang YS. Embryo quality is more important for younger women whereas age is more important for older women with regard to in vitro fertilization outcome and multiple pregnancy. Fertil Steril. 2006;86(1):64–9. https://doi.org/10.1016/j.fertnstert.2005.11.074.
Leijdekkers J, Eijkemans M, Van Tilborg T, Oudshoorn SC, McLernon DJ, Bhattacharya S, et al. Predicting the cumulative chance of live birth over multiple complete cycles of in vitro fertilization: an external validation study. Hum Reprod. 2018;33(9):1684–95. https://doi.org/10.1093/humrep/dey263.
Yanez LZ, Han J, Behr BB, Pera RAR, Camarillo DB. Human oocyte developmental potential is predicted by mechanical properties within hours after fertilization. Nat Commun. 2016;7(1):10809. https://doi.org/10.1038/ncomms10809.
Vaegter KK, Lakic TG, Olovsson M, Berglund L, Brodin T, Holte J. Which factors are most predictive for live birth after in vitro fertilization and intracytoplasmic sperm injection (IVF/ICSI) treatments? Analysis of 100 prospectively recorded variables in 8,400 IVF/ICSI single-embryo transfers. Fertil Steril. 2017;107(3):641–48. e2.
Siristatidis C, Pouliakis A, Chrelias C, Kassanos D. Artificial intelligence in IVF: a need. Syst Biol Reprod Med. 2011;57(4):179–85. https://doi.org/10.3109/19396368.2011.558607.
Minaretzis D, Harris D, Alper MM, Mortola JF, Berger MJ, Power D. Multivariate analysis of factors predictive of successful live births in in vitro fertilization (IVF) suggests strategies to improve IVF outcome. J Assist Reprod Genet. 1998;15(6):365–71. https://doi.org/10.1023/A:1022528915761.
Kaufmann SJ, Eastaugh JL, Snowden S, Smye SW, Sharma V. The application of neural networks in predicting the outcome of in-vitro fertilization. Hum Reprod. 1997;12(7):1454–7. https://doi.org/10.1093/humrep/12.7.1454.
Uyar A, Bener A, Ciray H, Bahceci M. A frequency based encoding technique for transformation of categorical variables in mixed IVF dataset. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:6214–7.
Hunault CC, Eijkemans MJ, Pieters MH, te Velde ER, Habbema JD, Fauser BC, et al. A prediction model for selecting patients undergoing in vitro fertilization for elective single embryo transfer. Fertil Steril. 2002;77(4):725–32. https://doi.org/10.1016/S0015-0282(01)03243-5.
Roberts S, Hirst W, Brison D. Vail a; towardSET collaboration. Embryo and uterine influences on IVF outcomes: an analysis of a UK multi-Centre cohort. Hum Reprod. 2010;25(11):2792–802. https://doi.org/10.1093/humrep/deq213.
Roberts SA, McGowan L, Mark Hirst W, Vail A, Rutherford A, Lieberman BA, et al. Reducing the incidence of twins from IVF treatments: predictive modelling from a retrospective cohort. Hum Reprod. 2010;26(3):569–75.
Luke B, Brown MB, Wantman E, Stern JE, Baker VL, Widra E, et al. A prediction model for live birth and multiple births within the first three cycles of assisted reproductive technology. Fertil Steril. 2014;102(3):744–52. https://doi.org/10.1016/j.fertnstert.2014.05.020.
Rongieres C, Colella C, Lehert P. To what extent does anti-Mullerian hormone contribute to a better prediction of live birth after IVF? J Assist Reprod Genet. 2015;32(1):37–43. https://doi.org/10.1007/s10815-014-0348-3.
Vogiatzi P, Pouliakis A. An artificial neural network for the prediction of assisted reproduction outcome. J Assist Reprod Genet. 2019;36(7):1441–8. https://doi.org/10.1007/s10815-019-01498-7.
Luke B, Brown MB, Wantman E, Stern JE, Baker VL, Widra E, et al. Application of a validated prediction model for in vitro fertilization: comparison of live birth rates and multiple birth rates with 1 embryo transferred over 2 cycles vs 2 embryos in 1 cycle. Am J Obstet Gynecol. 2015;212(5):676.
Van Der Steeg J, Steures P, Eijkemans M, Habbema JD, Bossuyt PM, Hompes PG, et al. Do clinical prediction models improve concordance of treatment decisions in reproductive medicine? BJOG. 2006;113(7):825–31. https://doi.org/10.1111/j.1471-0528.2006.00992.x.
Wiegerinck MA, Bongers MY, Mol BW, Heineman MJ. How concordant are the estimated rates of natural conception and in-vitro fertilization/embryo transfer success? Hum Reprod. 1999;14(3):689–93. https://doi.org/10.1093/humrep/14.3.689.
Choi B, Bosch E, Lannon BM, Leveille MC, Wong WH, Leader A, et al. Personalized prediction of first-cycle in vitro fertilization success. Fertil Steril. 2013;99(7):1905–11. https://doi.org/10.1016/j.fertnstert.2013.02.016.
Leushuis E, van der Steeg JW, Steures P, Bossuyt PM, Eijkemans MJ, van der Veen F, et al. Prediction models in reproductive medicine: a critical appraisal. Hum Reprod Update. 2009;15(5):537–52. https://doi.org/10.1093/humupd/dmp013.
Van Loendersloot L, Repping S, Bossuyt PM, van der Veen F, van Wely M. Prediction models in in vitro fertilization; where are we? A mini review. J Adv Res. 2014;5(3):295–301. https://doi.org/10.1016/j.jare.2013.05.002.
Acknowledgements
We would like to express our heartfelt gratitude to Yuqi CUI from Huazhong University of Science and Technology, China, for the great help in constructing our machine learning algorithms and developing the embryo selection strategy model.
Funding
This work was supported by research grants from the National Key Research and Development Project (grant number: 2018YFC1002103), Health Commission of Hubei Province Scientific Research Project (grant number: WJ2021M110), and the Chinese Medical Association (grant number: 16020520668) as well as the Natural Science Foundation of Hubei Province (grant number: 2017CFB752).
Author information
Authors and Affiliations
Contributions
Q.X., M.W., B.Z., Z.L., and B.H. conducted the experiment; Q.Y., L.Y., and S.L. analyzed the data, Q.X. and Q.Y. composed the manuscript, and L.Z. and L.J. were responsible for the concept and study design. All authors contributed to the interpretation, discussion and editing of the manuscript. All authors approved the last version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the medical ethics committee of Tongji Medical College of Huazhong University of Science and Technology and written informed consent was obtained from all patients before they were included. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xi, Q., Yang, Q., Wang, M. et al. Individualized embryo selection strategy developed by stacking machine learning model for better in vitro fertilization outcomes: an application study. Reprod Biol Endocrinol 19, 53 (2021). https://doi.org/10.1186/s12958-021-00734-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-021-00734-z