Abstract
Background
Prompt and accurate staging of pancreatic cancer is essential to distinguish patients to benefit from resection with curative intent and those with unresectable disease. A staging laparoscopy is used preoperatively to identify macroscopic or occult metastases not identified on imaging. This single-institution study aims to evaluate the role of staging laparoscopy in patients with pancreatic adenocarcinoma and its effect on overall survival.
Method
Clinicopathologic data were evaluated for all patients undergoing staging laparoscopy for pancreatic adenocarcinoma from July 2014 to December 2019. The study identified 155 patients eligible for analysis. All patients were followed for at least 2 years. Clinical backgrounds, survival curves and prognostic factors were investigated.
Results
Resectability status among the cohort was 62 (40%) upfront resectable, 53 (34%) borderline resectable and 40 (26%) locally advanced disease. The median age was 69, with 44% male patients. Median CA19-9 value was 125 kU/L, and median CA125 value was 22 kU/L. Staging laparoscopy resulted in upstaging nine (15%) upfront resectable patients, five (9%) borderline resectable patients and ten (25%) locally advanced patients. There was positive cytology in 19 (12%), peritoneal deposits in six (4%) and peritoneal liver deposits in seven (5%) patients. Overall, the number needed to treat (NNT) to avoid an unnecessary laparotomy was eight patients.
Conclusion
Staging laparoscopy continues to be a valuable investigation of pancreatic adenocarcinoma. In this institution, one in every eight patients undergoing a staging laparoscopy was upstaged to metastatic disease, thus avoiding an unnecessary laparotomy or a non-curative resection.
Similar content being viewed by others
Background
Pancreatic cancer which is predominantly pancreatic ductal adenocarcinoma (PDAC) is the eighth most commonly diagnosed cancer in Australia [1]. The 5-year survival rates for pancreatic cancer are among the lowest of all cancers in Australia (11.2% for men and 11.8% for women) [1]. Prompt and accurate staging of pancreatic cancer is essential to distinguish patients to benefit from resection with curative intent and those with unresectable disease. A staging laparoscopy is used preoperatively to identify macroscopic or occult metastases that were not identified on imaging and thus is used to exclude patients from futile radical surgery.
Staging PDAC is primarily achieved with high-quality contrast-enhanced computed tomography (CT) imaging (sensitivity 89–91%, specificity 85–90%) [2]. High-quality multiphase imaging allows for enhanced visualisation of the surrounding vasculature which can be used to categorise PDAC into upfront resectable, borderline, locally advanced (LA) disease or metastatic disease. National Comprehensive Cancer Network (NCCN) guidelines recommend positron emission tomography (PET) as an adjunct modality in patients at high risk of metastatic disease, such as those with borderline resectable disease, markedly elevated CA19-9, large primary tumours, large regional nodes or very symptomatic presentations [3].
Staging laparoscopy is a minimally invasive procedure used to assess for macroscopic or occult metastases for tumours of the abdomen. These cancers include oesophageal, gastric, pancreatic and periampullary, hepatic and biliary tract [4]. Staging laparoscopy potentially avoids unnecessary laparotomy due to the finding of radiographically occult metastatic disease and assists in further staging of the pancreatic cancer with identifying neoplastic cells in peritoneal fluid cytology.
First developed in 1982, staging laparoscopy carried a positive result of 31–51% [5]. However, with modern diagnostic imaging modalities such as CT and PET, the routine use of staging laparoscopy in modern practice has become controversial. The NCCN guidelines suggest staging laparoscopy to be considered in higher risk pancreas cancer patients with upfront resectable disease, for example markedly elevated serum CA19-9, and for patients with borderline resectable disease before administration of neoadjuvant therapy[3].
Given the significant improvements in the quality of imaging and its evaluation, we undertook this single institution study to examine the impact of the routine addition of staging laparoscopy in the treatment of patients with potentially operable PDAC.
Methods
Study design
This study is a retrospective analysis of a prospectively maintained database in a single high-volume pancreatic surgery unit in Sydney, Australia. Ethical approval and consent were obtained from the Northern Sydney Local Health District Human Resources Ethics Council (re:HREC/16/HAWKE/105).
Patients
All patients who underwent staging laparoscopy for pancreatic adenocarcinoma at the Royal North Shore Pancreatic Surgery Unit from July 2014 to January 2020 were included in this study. Only patients with histologically proven pancreatic ductal adenocarcinoma were included in the cohort. Omissions included patients who had a confirmed cholangiocarcinoma, ampullary cancer or known metastatic neoplasm including metastases to the pancreas. Staging included a CT chest, abdomen and pelvis, and tumour resectability was determined by triple-phase CT scan with pancreatic protocol. All patients were followed for at least 2 years from the time of the staging laparoscopy.
In this unit, staging laparoscopy is performed in all patients with malignant pancreatic tumours who were deemed to have resectable disease. This is determined by fortnightly PDAC-specific multidisciplinary team (MDT) review with case discussion at diagnosis and further discussion following treatment response. Treatment consists of either folfirinox or gemcitabine with albumin-bound paclitaxel chemotherapy agents, while palliative therapy consists of gemcitabine with albumin-bound paclitaxel or solely gemcitabine chemotherapy agents. Patients who show a good response to chemotherapy which is defined as shrinkage or lack of progression of tumour size, resectability of the tumour as determined at MDT review and no evidence of metastatic disease on post chemotherapy imaging were restaged including a repeat staging laparoscopy. Additional factors including a significant drop in either serum CA19-9 or 18FDG-PET maximum standardised uptake values (SUVmax) were also considered. Surgical resection is undertaken in those considered at MDT to have a resectable primary tumour with no evidence of metastatic disease on restaging.
Perioperative variables
Patient demographics including age, sex and the presence of diabetes or jaundice were extracted from the prospectively collected pancreatic surgery database. Tumour markers including preoperative serum CA19-9 and CA125 were extracted from the electronic medical records. CT scan and PET results conducted at the time of diagnosis were reviewed for evidence of metastatic disease and to clarify disease resectability.
Outcomes definition
A positive macroscopic staging laparoscopy is defined if an identifiable tissue sample collected during the procedure is found to contain malignant cells on histopathological analysis. A positive microscopic staging laparoscopy is defined as peritoneal washings which have shown malignant cells on cytology. The pathological distinction between ‘atypical cells suspicious but not diagnostic of cancer’ and a definitive diagnosis of carcinoma may be subtle and is often dependent on the experience of the individual reporting pathologists. We used standard morphological criteria as suggested by the World Health Organization 2019 classification [6] to make this distinction. If there was any doubt, cases were referred to a specialist pancreaticobiliary pathologist. Immunohistochemistry for epithelial markers (useful for the distinction between atypical reactive mesothelial cells and well-differentiated adenocarcinoma cells) was not performed routinely on all cases; rather, it was performed only on selected cases at the discretion of the reporting pathologists — that is those cases where the degree of cytological atypia was mild and there were sufficient atypical cells in the cell block for testing.
Laparoscopy technique
After establishing pneumoperitoneum through a 10 mm trocar inserted at the umbilical area, a 30-degree laparoscope is inserted, and two additional 5-mm ports are placed. Firstly, the liver and parietal peritoneum are inspected closely examining for the presence of nodular lesions. Secondly, a small bowel run is performed, closely examining the mesentery to identify any further nodules. Lastly, peritoneal lavage is performed with approximately 500 mL of normal saline. The fluid is aspirated and sent for peritoneal cytology. Washings are performed regardless of the presence or absence of macroscopic disease at laparoscopy.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 9. Spearman’s Rho test and Mantel-Cox test were used for analysis. Significance was defined as P < 0.05. Ethical approval was obtained from the Northern Sydney Local Health District Human Research Ethics Council.
Results
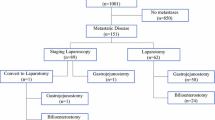
From the 3rd of July 2014 to the 20th of December 2019, 155 staging laparoscopies were performed at this unit for upfront, borderline or LA pancreatic ductal adenocarcinoma. The median age was 69 (47–88), with 44% male patients. Median CA19-9 value was 125 kU/L, and median CA125 value was 22 kU/L (Table 1). The median follow-up time for patients reported alive was 41 months. Spearman correlation analysis showed no correlation among tumour location, tumour size, serum CA19-9, serum CA125 or SUVmax on 18FDG-PET scan and the outcome of the staging laparoscopy (Table 2).
Outcome measures of staging laparoscopy
Staging laparoscopy resulted in upstaging of nine upfront resectable patients (14.5%), five borderline resectable patients (9.4%) and ten patients with LA tumours (25.0%) (Table 3). There was positive cytology in 19 patients (12.2%), peritoneal deposits in six patients (3.9%) and peritoneal liver deposits in seven patients (4.5%). Eleven patients had positive peritoneal cytology for metastasis without any macroscopic evidence of disease (7.1%).
Of the nine upfront resectable patients with positive staging laparoscopy, one patient with positive macroscopic disease and positive cytology had a good response to chemotherapy and a subsequent negative staging laparoscopy followed by curative intent resection. The remaining eight patients commenced palliative chemotherapy, subsequently developing progression of disease. The one patient that underwent resection lived for 32 months compared with a median survival of 8 months in the other eight upfront disease patients with positive staging laparoscopy that did not have resection.
Among 53 patients with borderline resectable tumours with no metastatic disease on imaging, five had a positive staging laparoscopy (9.4%), with three patients showing macroscopic disease and the remaining two only having microscopic disease on peritoneal wash cytology. All three patients with macroscopic disease underwent chemotherapy. Of these, two had a negative repeat staging laparoscopy and underwent a curative resection. The two patients with persisting microscopic disease on staging laparoscopy had rapid disease progression and passed away in 11 and 17 months, respectively. Of the two patients that underwent resection, one survived 17 months, while the other patient is still alive after 82 months, compared to a median of 11 months for the three patients that did undergo resection.
Among 40 patients with LA disease, 10 had a positive staging laparoscopy (25.0%). Three had macroscopic metastasis, one with negative cytology and two with positive microscopic disease on cytology. Seven patients with LA disease had only positive microscopic disease on cytology with no macroscopic metastasis (Table 3). All seven underwent chemotherapy with follow-up review and repeat imaging. Two patients had a favourable response to treatment, and after MDT discussion, they underwent a repeat staging laparoscopy, both of which did not demonstrate macroscopic or microscopic disease so underwent curative resection. These patients had a survival of 37 and 10 months, respectively, compared to a median of 4.5 months for the eight patients that did not have a resection.
Combining upfront, borderline and LA disease, staging laparoscopy resulted in 24 of the 155 patients (15.5%) being upstaged to metastatic disease.
In summary, patients that had no evidence of metastatic disease on preoperative imaging and that subsequently had a positive staging laparoscopy with either macroscopic deposits or positive cytology were upstaged and underwent chemotherapy with ongoing MDT review of the response to chemotherapy. For patients with upfront, borderline and LA disease, the overall survival of the patients that had a positive staging laparoscopy with a subsequent resection was 32 months compared with 6 months for the 19 patients who did not have a resection (Fig. 1, P = 0.003) and compared with 34 months for the 96 patients that underwent resection with a negative staging laparoscopy (Fig. 2, P = 0.642).
Kaplan–Meier analysis of overall survival of patients after a positive staging laparoscopy that A did not undergo resection and B underwent resection after chemotherapy and a subsequent negative staging laparoscopy. P, positive staging laparoscopy without resection. P + R, positive staging laparoscopy with resection. P = 0.003 (log -rank test)
Management
Across the cohort of 155 patients, 31 underwent upfront surgical resection (20.0%) after staging laparoscopy (median 17 days, range 4- − 74 days after staging laparoscopy), and 67 underwent surgical resection after neoadjuvant chemotherapy (43.2%) (median 135 days, range 40- − 315 days after staging laparoscopy) (Table 4).
A total of 54 patients received palliative therapy (34.8%). Three patients proceeded to laparotomy but had an abandoned resection due to undiagnosed metastatic disease. All three of these cases were due to the presence of liver peritoneal surface metastases that were undetected on staging laparoscopy.
Number needed to treat
Staging laparoscopy resulted in 15.5% of patients being upstaged to metastatic disease with a remaining 3.0% having a nontherapeutic laparotomy despite negative staging laparoscopy. Thus, the absolute risk reduction for patients undergoing a staging laparoscopy to avoid a nontherapeutic laparotomy is 12.5%. This produces a number needed to treat value of 8.
Discussion
Staging laparoscopy continues to have a significant role in the preoperative assessment of PDAC [7,8,9]. At the Royal North Shore Hospital, 14 patients with either upfront resectable or borderline resectable PDAC had a positive staging laparoscopy (12.2%). Staging laparoscopy was of value for 10 of these patients by avoiding an unnecessary laparotomy by diagnosing macroscopic disease, which would have been noted at the time of attempt for resection. Also, four patients avoided non-curative resection through the finding of microscopic disease at the laparoscopy. This unit’s nontherapeutic laparotomy rate was 3.0%, due to hepatic metastatic deposits not identified on imaging or laparoscopy. While NCCN guidelines suggest MRI as a helpful adjunct to CT staging [3], it is not routinely used at this institution. New intraoperative imaging modalities have emerged to further enhance the utility of staging laparoscopy. Oba et al. (2021) [10] utilised intraoperative ultrasound and fluorescence imaging during staging laparoscopy and detected occult liver metastases in an additional six of the 31 patients.
The NCCN guidelines [3] recommend selective use of staging laparoscopy in pancreatic adenocarcinoma patients who are considered to be high risk for occult metastatic disease including high CA19.9 (> 100 U/mL [11]) and patients with borderline resectable tumours. In their meta-analysis, De Rosa et al. (2016) found CA19-9 ≥ 150 U/Ml and tumour size > 3 cm to be the strongest predictors of unresectable disease [12]. However, this study found no correlation in the outcome of the staging laparoscopy and with the serum CA19-9, tumour size or location.
NCCN guidelines do not comment on the utility of peritoneal washing cytology [3]. Recent studies have shown that patients with positive cytology that undergo resection have poorer outcomes than cytology-negative patients. Ferrone et al. [13] found the median survival of its 10 patients undergoing resection in the setting of positive cytology to be 8 months compared to 16 months for the remaining 208 resected patients with negative cytology. Similarly, Aoki et al. [14] in their study found that the 123 resected patients who were cytology negative after neoadjuvant therapy had significantly better survival than the 13 resected patients that were cytology positive after neoadjuvant therapy (30.8 months vs 14.8 months, respectively). This study is one of the few in the world to report on patients who have had positive cytology, neoadjuvant chemotherapy leading to conversion to negative cytology with favourable outcomes.
There were five patients that had positive macroscopic disease without positive cytology in the peritoneal washings collected. This highlights the imperfect sensitivity of morphologic observation of the peritoneal washings in detecting occult metastases. Recent studies have described the prognostic relevance of microRNA and DNA PCR testing in patients treated for pancreatic ductal adenocarcinoma which could compliment cytology assessment [15]. In their study of 89 patients, Suenaga et al. [16] found that patients with high levels of peritoneal tumour DNA had significantly poorer disease-free survival. Kubo et al. [17] found higher expression of microRNA (miRNA 194-5p) in peritoneal washings to be associated with peritoneal recurrence after radical resection.
We acknowledge the limitations of this study. The follow-up for patients with the most recent staging laparoscopy at the end of 2019 was limited to a follow-up period of 2 years.
We acknowledge that longer follow-up than 2 years is necessary to identify the true value of neoadjuvant therapy for patients with positive cytology. Furthermore, this study is limited to a single high-volume referral centre. We believe this data are convincing enough to warrant a prospective multi-institutional trial with rigid enrolment criteria and methods of care to further explore the utility of neoadjuvant chemotherapy followed by surgical resection in patients that convert to negative staging laparoscopy.
Conclusion
Staging laparoscopy continues to be a valuable investigation in the staging of potentially operable pancreatic adenocarcinoma. In this institution, one in every eight patients undergoing a staging laparoscopy was upstaged to metastatic disease, thus avoiding an unnecessary laparotomy or a non-curative resection.
Availability of data and materials
Raw data were generated at the Royal North Shore Public and Royal North Shore Private Hospitals. Derived data supporting the findings of this study are available from the corresponding author (MJ) on request.
Abbreviations
- PDAC:
-
Pancreatic ductal adenocarcinoma
- CT:
-
Computed tomography
- NCNN:
-
National Comprehensive Cancer Network
- PET:
-
Positron emission tomography
- MDT:
-
Multidisciplinary team
- SUVmax:
-
Maximum standardised uptake values
- LA:
-
Locally advanced
- GOJ:
-
Gastroesophageal junction
References
Health AIo, Welfare. Cancer data in Australia. AIHW: Canberra; 2021.
Rhee H, Park MS. The role of imaging in current treatment strategies for pancreatic adenocarcinoma. Korean J Radiol. 2021;22(1):23–40.
Tempero MA, Malafa MP, Al-Hawary M, Asbun H, Bain A, Behrman SW, et al. Pancreatic adenocarcinoma, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2017;15(8):1028–61.
Hori Y. Diagnostic laparoscopy guidelines : this guideline was prepared by the SAGES guidelines committee and reviewed and approved by the Board of Governors of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), November 2007. Surg Endosc. 2008;22(5):1353–83.
Warshaw AL, Tepper JE, Shipley WU. Laparoscopy in the staging and planning of therapy for pancreatic cancer. Am J Surg. 1986;151(1):76–80.
Gill AJ, Klimstra DS, Lam AK, Washington MK, 10 tumours of the pancreas. WHO Classification of Tumours Editorial Board: digestive system tumours. WHO Classification of Tumours. 1. 5 ed. IARC: Lyon; 2019. p. 295–372.
Fong ZV, Alvino DML, Fernandez-Del Castillo C, Mehtsun WT, Pergolini I, Warshaw AL, et al. Reappraisal of staging laparoscopy for patients with pancreatic adenocarcinoma: a contemporary analysis of 1001 patients. Ann Surg Oncol. 2017;24(11):3203–11.
Satoi S, Yanagimoto H, Yamamoto T, Toyokawa H, Hirooka S, Yamaki S, et al. A clinical role of staging laparoscopy in patients with radiographically defined locally advanced pancreatic ductal adenocarcinoma. World J Surg Oncol. 2016;14(1):14.
Ta R, O’Connor DB, Sulistijo A, Chung B, Conlon KC. The role of staging laparoscopy in resectable and borderline resectable pancreatic cancer: a systematic review and meta-analysis. Dig Surg. 2019;36(3):251–60.
Oba A, Inoue Y, Ono Y, Ishizuka N, Arakaki M, Sato T, et al. Staging laparoscopy for pancreatic cancer using intraoperative ultrasonography and fluorescence imaging: the SLING trial. Br J Surg. 2021;108(2):115–8.
Ballehaninna UK, Chamberlain RS. The clinical utility of serum CA 19–9 in the diagnosis, prognosis and management of pancreatic adenocarcinoma: an evidence based appraisal. J Gastrointest Oncol. 2012;3(2):105–19.
De Rosa A, Cameron IC, Gomez D. Indications for staging laparoscopy in pancreatic cancer. HPB (Oxford). 2016;18(1):13–20.
Ferrone CR, Haas B, Tang L, Coit DG, Fong Y, Brennan MF, et al. The influence of positive peritoneal cytology on survival in patients with pancreatic adenocarcinoma. J Gastrointest Surg. 2006;10(10):1347–53.
Aoki S, Mizuma M, Hayashi H, Yoshimachi S, Hata T, Miura T, et al. Prognostic impact of intraoperative peritoneal cytology after neoadjuvant therapy for potentially resectable pancreatic cancer. Pancreatology. 2020;20(8):1711–7.
Frampton AE, Krell J, Jamieson NB, Gall TM, Giovannetti E, Funel N, et al. microRNAs with prognostic significance in pancreatic ductal adenocarcinoma: a meta-analysis. Eur J Cancer. 2015;51(11):1389–404.
Suenaga M, Fujii T, Yamada S, Hayashi M, Shinjo K, Takami H, et al. Peritoneal lavage tumor DNA as a novel biomarker for predicting peritoneal recurrence in pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2021;28(4):2277–86.
Kubo H, Hiroshima Y, Mori R, Saigusa Y, Murakami T, Yabushita Y, et al. MiR-194-5p in pancreatic ductal adenocarcinoma peritoneal washings is associated with peritoneal recurrence and overall survival in peritoneal cytology-negative patients. Ann Surg Oncol. 2019;26(13):4506–14.
Acknowledgements
Not applicable.
Funding
There are no sources of funding to disclose.
Author information
Authors and Affiliations
Contributions
MJ and AA contributed to all aspects of this study and article. CB, AM and JS contributed to the study conception, design, data analysis and interpretation and the critical revision of the article. NP, AK, AG and GH contributed to the critical revision of the article. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval and consent were obtained from the Northern Sydney Local Health District Human Resources Ethics Council (re:HREC/16/HAWKE/105). Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jambor, M.A., Ashrafizadeh, A., Nahm, C.B. et al. The role of staging laparoscopy in pancreatic adenocarcinoma and its effect on patients’ survival. World J Surg Onc 20, 337 (2022). https://doi.org/10.1186/s12957-022-02803-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02803-y