Abstract
Background
Post-treatment management is essential for improving the health and quality of life of colorectal cancer (CRC) survivors. The number of cancer survivors is continually increasing, which is causing a corresponding growth in the need for effective post-treatment management programs. Current research on the topic indicates that such programs should include aspects such as physical activity and a proper diet, which would form the basis of lifestyle change among CRC survivors. Therefore, this study aimed to identify the impact of physical activity and diet on the quality of life of CRC survivors.
Methods
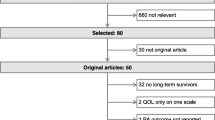
We performed a systematic literature review regarding CRC survivors. We searched the Embase, PubMed, and EBSCOhost databases, considering papers published between January 2000 and May 2017 in any language, using a combination of the following subject headings: “colorectal cancer,” “colorectal carcinoma survivor,” “survivorship plan,” “survivorship care plan,” “survivorship program,” “lifestyle,” “activities,” “exercise,” “diet program,” and “nutrition.”
Results
A total of 14,036 articles were identified, with 35 satisfying the eligibility criteria for the systematic review. These articles were grouped by the study questions into physical activity and diet: 24 articles were included in the physical activity group and 11 in the diet group.
Conclusions
The research showed that an effective survivorship program can significantly help CRC survivors maintain good health and quality of life for long periods. However, there is a lack of consensus and conclusive evidence regarding how the guidelines for such a program should be designed, in terms of both its form and content.
Similar content being viewed by others
Background
Post-treatment is a critical period for cancer survivors, mainly due to the major mental and physical health implications that accompany diagnosis and treatment. Consequently, adequate post-treatment management is essential for improving the health and quality of life of survivors.
Advances in early detection and treatment, combined with the aging and growing of the worldwide population, have resulted in a marked rise in cancer survivorship [1]. Following breast, lung, and prostate cancer, colorectal cancer (CRC) is the fourth most common source of new cases of cancer and is the second-leading cause of cancer-related deaths in the USA [2]. In 2014, Siegel et al. projected that 136,830 Americans would be diagnosed with CRC that year and that 50,310 would die as a result [3].
Because of this growing population of survivors, there is an increasing need for an effective post-treatment management program. However, while there are several examples of such programs in existence, there is still a lack of universal guidelines regarding the implementation of such programs [4]. Research indicates the efficacy of programs that are implemented at the national level, which in turn indicates the applicability of setting continued support and management as a basis for quality of care for cancer survivors [5]. Further, current research on the topic indicates a necessity to include certain important elements in such programs, particularly physical activity and proper dietary measures, which would represent a significant lifestyle change for many CRC survivors.
Objectives
Considering the above, this paper aimed to identify the impact of physical activity and diet on CRC survivors’ quality of life and to lay the groundwork for the development of guidelines for an effective survivorship program.
Rationale
Emerging evidence has indicated that lifestyle interventions that promote healthy eating, physical activity, and weight control have significant benefits to patients’ recovery. However, research on their effect following CRC treatment, particularly on quality of life, is limited. A systematic review, such as this one, can analyze available evidence to ascertain which interventions need to be made. Further, it can help identify the appropriate tools to use to attain these benefits. A systematic review can also inform survivorship care plans and facilitate the formulation of effective post-CRC care guidelines.
Methods
Search strategy and data collection
This systematic review utilized various electronic databases, namely PubMed, EMBASE, and EBSCOhost. These databases facilitated the location and identification of relevant sources for analysis in the review. The electronic records reviewed were for the past decade (2000–2019), with a specific focus on the latest publications. The main search terms included were “colorectal cancer,” “colorectal carcinoma survivor,” “survivorship plan,” “survivorship care plan,” “survivorship program,” “lifestyle,” “activities,” “exercise,” “diet program,” and “nutrition.”
With the help of two assistants and a librarian, all search terms were exploded, truncated, and adjusted to align with the specific database being used. Although we did not use randomised controlled trials (RCT), our search was aligned with findings from Cochrane Highly Sensitive Search Strategy phases I–III contained in the Cochrane Handbook for Systematic reviews of interventions
The review did not place any language restrictions on the searches, although we limited the findings to published literature. Studies that focused on types of cancer other than CRC were excluded.
A search for the title “diet physical activity and quality of life in colorectal cancer survivors” in PubMed restricted to the last 10 years returned a total of 1502 results. The phrase “effect of diet and physical activity on quality of life of colorectal cancer survivors” was used in the EBSCOhost service, in the databases of Health Source: Nursing/Academic Edition, MasterFILE Premier, MEDLINE, Academic Search Premier, AHFS Consumer Medication Information, and Health Source: Consumer Edition. The search results contained 21,874 full-text materials. The search terms were combined a number of times, and cross-referencing was used to identify any additional articles not shown in the database search.
Data extraction
The titles and abstracts of the selected studies were screened by the reviewers. Subsequently, the full texts of the identified studies were screened for eligibility. Two reviewers independently extracted the study attributes of eligible studies. These attributes included first author, sample size, year, country, journal, sampling, inclusion/exclusion criteria, study design, baseline response rate, comorbidities, type or timing of physical activities, type of diet, quality of life assessment approaches, statistical methods, and adjustments. Discrepancies were discussed between the reviewers, and if disagreements continued, a third independent review was asked to share his/her opinion.
Protocol
Methods for the inclusion criteria data analysis and the inclusion criteria themselves were specified in advance and documented in a protocol [6]. See the attached protocol.
Eligibility criteria (inclusion and exclusion)
A priori criteria were utilized for the inclusion of studies whereby we first located the abstract and subsequently proceeded to read the full-text articles if the abstracts did not offer sufficient information. In order to be included in the review, studies had to assess the quality of life of CRC survivors. Furthermore, the studies had to examine the physical activity (PA) of CRC survivors, both short term and long term, as long as specific results were provided. However, the examination of the quality of life had to exceed 2 years; otherwise, the studies were excluded. All types of colorectal cancers were eligible for the study. Since quality of life is a multidimensional concept, related studies had to conduct an assessment using more than one scale; otherwise, they were excluded. Furthermore, we included studies that investigated more than one type of cancer, although we focused on the results for colorectal cancer survivors. In all studies, PA and diet had to be independent variables and the quality of life had to be the result. All types of original quantitative studies, primarily published in English, were included. Furthermore, all studies that focused on the effect of diet and PA on the quality of life of patients with CRC, whether as individual elements or combined, were included without discrimination regarding factors such as age and language. However, the review excluded study protocols, reviews, theses, conference abstracts, qualitative studies, editorials, meta-analyses, and commentaries. The studies also had to be published between 2000 and 2019.
Type of studies
In this systematic review, we adopted a secondary research approach for data collection and analysis. The methodological procedure comprised a systematic review of the literature on the topic: “A survivorship program for CRC survivors.” The research question was formulated, based on the topic: What is the importance of physical activity (PA) and diet for CRC survivors? The data collected from the online databases (Embase, PubMed, and EBSCOhost databases) were used to answer these questions.
Types of participants
Only CRC survivors of any age were considered for this study; studies that specifically focused on other types of cancers were excluded.
Assessment of risk of bias
To confirm the validity of the studies that passed the eligibility test, a pair of reviewers worked independently, and with utmost reliability, to establish and verify the authenticity of the selected articles picked to be analyzed in this systematic review.
Assessment of risks and bias of individual studies
The two reviewers checked the quality of the methodologies for each of the studies used in the review. The items for the evaluation were adapted from a checklist formulated in Mols, et al. [6] with a particular focus on content that was essential to the specific questions in this review. Information bias was addressed through adequate assessment of study exposure, including determination of whether valid physical activity instruments were used, all aspects of physical activity, and the use of objective measures instead of self-reports. Adequate description of the data was shown, both medical and sociodemographic, such as the age of participants and their stage of cancer, including the process of data collection, whether these were self-reports or interviews.
Selection bias was addressed through the formulation of effective inclusion and exclusion criteria. Furthermore, reviewers assessed participation bias aspects, such as participant attrition, information concerning drop-outs, and non-participants, at the beginning of the review. The reviewers accommodated factors such as adequate information concerning time from diagnosis, sample size, potential study design, and correction of result measures for contradictions.
The systematic review was informed by the criteria established by the PRISMA guidelines [7].
Results
A total of 14,036 articles were identified, with 35 satisfying the eligibility criteria for the systematic review. These articles were grouped by the study questions into physical activity and diet: 24 articles were included in the physical activity group and 11 in the diet group.
Physical activity in CRC survivors
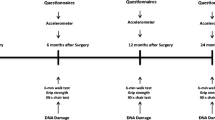
Of the 24 papers related to PA in CRC patients )Table 1), several reported health-related physical fitness to be effective for obtaining positive patient outcomes. Previously, PA has previously been determined to have a positive impact on the negative outcomes of cancer and its treatment, improving survivors’ quality of life [8]; however, very few existing programs can encourage cancer patients and survivors sufficiently to meet their PA guidelines [9]. Nevertheless, for CRC survivors, exercise is widely recommended as a means of improving fitness and enhancing patient-reported outcomes. PA can lead to a considerable reduction in the risk of cancer recurrence, and a previous study’s PA program was found to be successful in improving the quality of life of CRC survivors [10]. In particular, by implementing a 12-week supervised exercise training program, Sellar et al. reported that a PA approach is both feasible and effective for recurrence prevention, provided that there is a high level of participation and follow-up [11].
Some studies have examined how physical exercise can generate positive outcomes. Devin et al. reported that, for CRC survivors, high-intensity exercise comprises a safe, effective, and feasible intervention, because of the role it plays in improving both cardiorespiratory fitness and body composition [12]. A study by Vallance et al. showed that moderate-to-vigorous–intensity PA is critical for improving quality of life following treatment for colon cancer and that PA programs are significant in improving psychological health [13]. Moreover, Husson et al. provided further evidence that improved PA provided a positive contribution to health-related quality of life (HRQoL) [14].
Among CRC survivors, the environments within which PA interventions are implemented play a role in their efficacy and their ability to reduce detrimental sedentary behaviour [9]. One study found that, for such individuals, home-based PA interventions have a high level of efficacy in creating motivation for maintaining health-related physical fitness [15]. In accordance with the evident benefits of physical exercise, in terms of fighting and preventing cancer and its recurrence, computer-tailored interventions have been explored in relation to their potential to induce increased adherence to physical exercise; consequently, such programs have been found to show a potential to increase motivation among prostate and CRC patients and survivors [9].
A study was conducted to establish the impact of an Internet-delivered, distance-based PA program on the health and fitness of patients. It was consequently determined that motivation toward behaviour change declined when patients relied on the Internet for their physical exercise instruction. However, live PA programs delivered via the Internet are a common mode of providing self-management after successful cancer treatment. Forbes et al. studied the levels of motivation associated with such programs; they not only established that such programs have negative effects on motivation, but also that, if supervised, some programs become more effective and the rate of follow-up and participation increases [16].
However, although research findings remain inconclusive, there is evidence that information dissemination can have a positive impact on programs [17]. Brown et al. criticized the existing level of information provision concerning the onset of CRC and means of effective management following treatment [18]. Further, as mentioned, a home-care-based program has the potential for reduced efficacy as a result of reduced motivation. Considering this, Foley et al. proposed the use of a community-based multimodal exercise program [19]. Such a program can have positive impacts through its potential to improve motivation and participation. For instance, among elderly cancer survivors, along with the association between PA and improved physical health outcomes, it has been determined that such individuals’ mental health needs can be addressed through social participation. Social participation has also been revealed to promote engagement in PA [20].
One study indicated the efficacy of a combination of physical exercise and counselling in producing better outcomes in CRC survivors [21]. The nature of training programs used with cancer survivors has remained a focus of research in an effort to devise the most effective strategy for fulfilling the needs of survivors. For instance, Grote et al. investigated the efficacy of combined aerobic and resistance training for cancer survivors [22]. They found that improvement in cardiometabolic health is critical for preventing comorbidity among cancer survivors; in fact, it is as important as monitoring for the possible recurrence of cancer [22]. Further, Ligibel indicated the need to control for “energy balance factors, including diet, PA, and body weight,” in order to reduce the risk of cancer recurrence following treatment [23]. The above findings indicate the need for an effective exercise program, which utilizes PA in an appropriate manner to achieve positive results in the quality of life of cancer survivors.
In an evaluation of the Colon Health and Life-Long Exercise Change (CHALLENGE) trial, Courneya et al. confirmed the positive impact of PA on colon cancer patients [24]. Meanwhile, another study found that, in terms of CRC survivors, HRQoL is a major outcome of adherence to PA guidelines [25]. There is a lack of research on survivorship care programs for CRC survivors; hence, a more comprehensive examination of the implementation and scope of such programs, which would improve the management of care for cancer survivors, has been advocated [26]. Further, despite the limited evidence concerning the efficacy of leisure-time PA, it has been clearly determined that such interventions should be promoted among racial minorities, individuals with more than two physically limiting chronic ailments, and individuals who are currently smoking [27]. Because PA is a critical part of the post-treatment management program, factors that hinder effective PA should be identified and addressed [28]. A notable obstacle revealed in previous research is patients’ sociodemographic factors; consequently, future programs should take into consideration functioning elements, cancer symptoms, and the nature of treatment [29]. Further, inadequate information relating to treatment and management, distress from toxicities, and challenges adjusting to life and colostomy care, are other issues that should be addressed to achieve effective management of CRC survivors [30].
Nutrition in CRC survivors
Eleven papers met the inclusion criteria for diet and CRC (Table 1). Several of these studies revealed a close relationship between a poor diet and the development of different kinds of cancer, including CRC. It is well established that an unhealthy lifestyle—poor dietary and physical fitness habits—contributes to the development of cancer [31]. Based on this, Bazzan et al. highlighted the importance of investigating the ideal diet for cancer survivors in order to improve their health and quality of life [32]. Dietary factors involved in the development of cancer can be modified to achieve positive outcomes in both treatment and post-treatment management [33]. For instance, Grimmett et al. provided a summary of the effect of modifiable lifestyle factors pre- and post-diagnosis [31]. They determined that an appropriate diet, in conjunction with PA, is critical for the management of cancer throughout the continuum of the disease. This finding is indicative of the interplay between modifiable lifestyle factors and the prognosis of the disease. Their study indicates the importance that patients adopt the recommended lifestyle, which would lead to effective management and better prognosis among CRC survivors [31].
In addition to an exercise program, nutrition has been shown to have a huge impact on the health and well-being of CRC survivors. A change in lifestyle, which includes adherence to a recommended healthy diet, has been determined to have the potential for short-term benefits among CRC survivors, indicating the need for more research and a standard program to reveal the potential long-term effects [34]. Consequently, Grimmett et al. explored the role that such a change in lifestyle plays in terms of the long-term health and survival rates of cancer survivors [31], finding that a change in lifestyle is associated with longer life and better quality of life among the CRC patient population.
Among the health-related behaviours explored in Grimmett et al.’s study is consuming a diet recommended by a healthcare provider [31]. Grimmett et al. concluded that the failure to adopt healthy behaviours is a major contributor of poorer health and quality of life among cancer survivors [31]. Further, Ko et al. replicated the findings of Brown et al. by investigating the efficacy of communication strategies in improving adherence to fruit and vegetable consumption among CRC survivors [34]. Ko et al. consequently found that, similar to the fact that the involvement of a healthcare provider increases adherence to PA programs, the enhancement of communication and trust between care providers and patients mediates adherence to nutritional programs [34].
Previous evidence has indicated that, in addition to PA, a healthy diet plays an important role in reducing the risk of developing CRC [33]; thus, such an approach can be considered to contribute to reducing the risk of recurrence following successful treatment. However, despite the relatively large amount of evidence concerning the effect of diet on primary prevention, research regarding the role of diet in secondary prevention remains inadequate. Nevertheless, it can be determined from the above findings that survivors’ lifestyle behaviours are critical for successful secondary prevention and good quality of life following treatment [31]. Several of the studies examined showed that nutrition plays an important role in terms of enhancing quality of life; furthermore, a positive relationship was identified between survival/prevention of recurrence of CRC and consuming nutritious foods, PA, and physical fitness. Additionally, a study by Miller et al. [35] reported that intake of supplements among cancer survivors is a critical intervention for satisfying the body’s nutritional demands; the researchers also underlined the importance of communication between care providers and patients.
Studies have also investigated particular diets that CRC survivors should avoid in order to achieve positive outcomes in terms of health and quality of life [30]. Consequently, recommendations regarding foods that should be avoided, including red meat and low-fibre foods, have been proliferated. Such research adds to the findings of Grimmett et al., who suggested that high-fibre fruits and vegetables contribute to preventing the recurrence of CRC [31]. Thus, lifestyle modification aimed towards promoting health and good quality of life should include avoiding foods that can place a CRC survivor at risk of recurrence. According to Ho et al., the main type of diet to avoid is the Western-pattern diet, which has traditionally been associated with causing different types of cancers, including CRC [30]. Borresen et al. sought to identify specific dietary interventions suitable for inclusion in a CRC survivorship program [36]. In particular, they examined the role of dietary fibre in the prevention of cancers of the digestive system; navy beans and rice bran were the focus of their investigation, as these have previously been suggested to restrain colon carcinogenesis. Borresen et al. consequently determined that intake of whole grains and legumes is critical for survivors of CRC because this increases levels of dietary fibre, and contributes to CRC chemoprevention [36]. However, Hawkins et al. also indicated the importance for patients to possess awareness and a positive belief stance in regard to observing a healthy diet [37]. Nutritional interventions are highly recommended to include as elements of survivorship programs for CRC survivors, because of their potential to improve the general health of such individuals [38]. Nutritional interventions, as part of behaviour-modification programs, have been found to augment the health and quality of life of survivors [30]. Applying the Theory of Planned Behaviour and the Health Action Process Approach, Moug et al. indicated the positive role of adopting positive health behaviours, including consuming a healthy diet and avoiding behaviours that put the individual at risk of cancer recurrence [39]; they also recommended CRC survivors to implement dietary interventions that are based on recognizing the role that poor dietary behaviours play in CRC [39]. Additionally, Lawn et al. recommended the inclusion of nutritional interventions in self-management strategies for improving CRC survivors’ health and quality of life [38].
Winkels et al. [40] supported the findings of Hawkins et al. [37], suggesting the important role of patients’ awareness and positive belief regarding the implementing of positive dietary behaviours. They stated that patients are most likely to adhere to nutritional interventions when they understand the importance of these interventions. Winkels et al. also investigated a sample of CRC survivors’ compliance with The World Cancer Research Foundation/American Institute for Cancer Research’s (WCRF/AICR) for CRC survivors [40]. They reported that patients with knowledge of the recommendations had higher adherence rates to their diets. Considering the above, we find substantial evidence that advice on proper dietary behaviour should form a part of a survivorship program for CRC survivors. Informed individuals are more likely to have better adherence scores and, therefore, have better outcomes in terms of health and quality of life.
The role of PA and diet was tested by applying the four risk of bias items criterion; the results showed that there is an effective survivorship program that can help CRC survivors maintain good health and quality of life for long periods. A positive association emerged from outcome assessors, concealment allocation, sequence generation, and blinding of patients.
Discussion
For many CRC survivors, adherence to PA and dietary recommendations necessitates changes in their behaviours and lifestyles. Positive behaviour changes, such as adopting an appropriate diet and engaging in PA, have been shown to have a major impact on the outcomes of cancer survivors. However, it is important to note that, for successful behaviour change, the structure of a lifestyle-change program is critical. Studies have shown that a dogmatic approach may cause self-blame and stigmatization, while a more customized and evidence-based approach can have a positive impact [41].
Part of the mission of the American Cancer Society is to focus on informed decision-making for cancer survivors and their families. Critical information concerning diet and PA is important for positive outcomes [38]. A high level of adherence to the WCRF/AICR’s eight recommendations—regarding diet, PA, and body weight—has been shown to correlate with a tendency to change lifestyle and adapt positive dietary behaviours [42].
Self-care is critical for cancer survivors, but there is a need for better integration of lifestyle change into standard models of post-cancer-treatment care [43]. The benefits of conducting follow-ups and advocating lifestyle changes, as part of survivorship programs for CRC patients, have been widely highlighted in research (such benefits include identification of the potential for cancer recurrence and patients’ adoption of preventive measures) [44]. Thus, coordinated management of CRC survivors is essential for improving patient care, preventing recurrence of the disease, and improving general quality of life [45]. Coordination and communication between care providers and patients, in terms of addressing individual needs, are the most critical factors for effective post-treatment management of CRC survivors [46]. Consequently, an evidence-based coordinated program for cancer survivors, based on nutritional and PA needs, is essential. Additionally, healthcare providers should be provided with the necessary information to perform effective management of survivors [47].
Limitations of the study
This systematic review gives an integrated account of several studies, which can be used to determine an effective survivorship program to help CRC survivors maintain good health and quality of life for long periods. The most prominent limitation of this systematic review is that varieties of diet, patient populations, outcome definitions, and type and frequency of physical exercises are not the same across studies. Publication bias might also have influenced some of the results.
Conclusions
The findings of this systematic review have shown that there is a connection between effective survivorship programs for CRC survivors, and how such programs confer long-lasting benefits to this group. Conversely, the results might have been affected by reviewing imprecise studies that suggest the possibility of confounding factors other than diet and physical exercises as influencing CRC survivorship. Further research to establish if there are other factors that affect survivorship in this group is therefore warranted.
Availability of data and materials
All data analyzed during this study are included in this published article.
Abbreviations
- CRC:
-
Colorectal cancer
- HRQoL:
-
Health-related quality of life
- PA:
-
Physical activity
References
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Stein KD, Alteri R, Jemal A. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271–89. https://doi.org/10.3322/caac.21349.
National Cancer Institute (2017) Common cancer types. National Cancer Institute web site. February 26, 2018. Available at: https://www.cancer.gov/types/common-cancers. Accessed 21 Nov 2017.
Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):104–17. https://doi.org/10.3322/caac.21220.
Haggstrom D, Arora N, Helft P, Clayman ML, Oakley-Girvan I. Follow-up care delivery among colorectal cancer survivors most often seen by primary and subspecialty care physicians. J Gen Intern Med. 2009;24(Suppl 2):S472–9. https://doi.org/10.1007/s11606-009-1017-6.
Meyerhardt JA, Mangu PB, Flynn PJ, Korde L, Loprinzi CL, Minsky BD, Petrelli NJ, Ryan K, Schrag DH, Wong SL, Benson AB III. Follow-up care, surveillance protocol, and secondary prevention measures for survivors of colorectal cancer: American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol. 2013;31(35):4465–70. https://doi.org/10.1200/JCO.2013.50.7442.
Mols F, Vingerhoets AJ, Coebergh JW, van de Poll-Franse LV. Quality of life among long-term breast cancer survivors: a systematic review. Eur J Cancer. 2005;41:2613–9.
Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, Tierney JF. Preferred Reporting Items for Systematic Review and Meta-Analyses of Individual Participant Data: the PRISMA-IPD statement. Jama. 2015;313:1657–65.
Cramer H, Lauche R, Klose P, Dobos G, Langhorst J. A systematic review and meta-analysis of exercise interventions for colorectal cancer patients. Eur J Cancer Care (Engl). 2014;23(1):3–14. https://doi.org/10.1111/ecc.12093.
Golsteijn RHJ, Bolman C, Volders E, Peels DA, de Vries H, Lechner L. Development of a computer-tailored physical activity intervention for prostate and colorectal cancer patients and survivors: OncoActive. BMC Cancer. 2017;17(1):446. https://doi.org/10.1186/s12885-017-3397-z.
Lawrence L, Stone M, Rainham D, Keats MR. Environments associated with moderate-to-vigorous physical activity and sedentary behavior of colorectal cancer survivors. Int J Behav Med. 2017;24(1):120–6. https://doi.org/10.1007/s12529-016-9575-6.
Sellar C, Bell G, Haennel R, Au H-J, Chua N, Courneya KS. Feasibility and efficacy of a 12-week supervised exercise intervention for colorectal cancer survivors. Appl Physiol Nutr Metab. 2014;39(6):715–23. https://doi.org/10.1139/apnm-2013-0367.
Devin JL, Sax AT, Hughes GI, Jenkins DG, Aitken JF, Chambers SK, Dunn JC, Bolam KA, Skinner TL. The influence of high-intensity compared with moderate-intensity exercise training on cardiorespiratory fitness and body composition in colorectal cancer survivors: a randomised controlled trial. J Cancer Surviv. 2016;10(3):467–79. https://doi.org/10.1007/s11764-015-0490-7.
Vallance JK, Boyle T, Courneya KS, Lynch BM. Accelerometer-assessed physical activity and sedentary time among colon cancer survivors: associations with psychological health outcomes. J Cancer Surviv. 2015;9(3):404–11. https://doi.org/10.1007/s11764-014-0409-8.
Husson O, Mols F, Ezendam NP, Schep G, van de Poll-Franse LV. Health-related quality of life is associated with physical activity levels among colorectal cancer survivors: a longitudinal, 3-year study of the PROFILES registry. J Cancer Surviv. 2015;9(3):472–80. https://doi.org/10.1007/s11764-014-0423-x.
Pinto B, Papandonatos G, Goldstein M, Marcus BH, Farrell N. Home-based physical activity intervention for colorectal cancer survivors. Psycho-Oncology. 2013;22(1):54–64. https://doi.org/10.1002/pon.2047.
Forbes CC, Blanchard CM, Mummery WK, Courneya KS. A pilot study on the motivational effects of an internet-delivered physical activity behavior change program in Nova Scotian cancer survivors. Psychol Health. 2017;32(2):234–52. https://doi.org/10.1080/08870446.2016.1260725.
Eakin E, Hayes S, Haas M, Reeves MM, Vardy JL, Boyle F, Hiller JE, Mishra GD, Goode AD, Jefford M, Koczwara B, Saunders CM, Demark-Wahnefried W, Courneya KS, Schmitz KH, Girgis A, White K, Chapman K, Boltong AG, Lane K, McKiernan S, Millar L, O’Brien L, Sharplin G, Baldwin P, Robson EL. Healthy living after cancer: a dissemination and implementation study evaluating a telephone-delivered healthy lifestyle program for cancer survivors. BMC Cancer. 2015;15:992. https://doi.org/10.1186/s12885-015-2003-5.
Brown S, Greenfield D, Thompson J. Knowledge and awareness of long-term and late treatment consequences amongst colorectal cancer survivors: a qualitative study. Eur J Oncol Nurs. 2016;20:191–8. https://doi.org/10.1016/j.ejon.2015.08.005.
Foley M, Barnes V, Hasson S. Effects of a community-based multimodal exercise program on physical function and quality of life in cancer survivors: a pilot study. Physiother Theory Pract. 2015;31(5):303–12. https://doi.org/10.3109/09593985.2015.1004390.
Thraen-Borowski KM, Trentham-Dietz A, Edwards DF, Koltyn KF, Colbert LH. (2013) Dose-response relationships between physical activity, social participation, and health-related quality of life in colorectal cancer survivors. J Cancer Surviv. 2013;7(3):369–78. https://doi.org/10.1007/s11764-013-0277-7.
McGowan E, Speed-Andrews A, Blanchard C, Rhodes RE, Friedenreich CM, Culos-Reed SN, Courneya KS. Physical activity preferences among a population-based sample of colorectal cancer survivors. Oncol Nurs Forum. 2013;40(1):44–52. https://doi.org/10.1188/13.ONF.44-52.
Grote S, Almstedt H, Tarleton H. Cardiometabolic health among cancer survivors: a 13-week pilot study of a combined aerobic and resistance training program. Oncol Nurs Forum. 2016;43(3):306–15. https://doi.org/10.1188/16.ONF.306-315.
Ligibel J. Lifestyle factors in cancer survivorship. J Clin Oncol. 2012;30(30):3697–36704. https://doi.org/10.1200/JCO.2012.42.0638.
Courneya KS, Vardy J, Gill S, Jonker D, O’Brien P, Friedenreich CM, Dhillon H, Wong RKS, Meyer RM, Crawford JJ, Campbell KL, Prapevessis H, O'Callaghan C, Turner J, Spencer LM, van der Ploeg HP, Tu D, Booth CM. Update on the colon health and life-long exercise change trial: a phase III study of the impact of an exercise program on disease-free survival in colon cancer survivors. Curr Colorectal Cancer Rep. 2014;10:321–8. https://doi.org/10.1007/s11888-014-0231-8.
Krouse RS, Wendel CS, Garcia DO, Grant M, Temple LKF, Going SB, Hornbrook MC, Bulkley JE, McMullen CK, Herrinton LJ. Physical activity, bowel function, and quality of life among rectal cancer survivors. Qual Life Res. 2017;26(11):3131–42. https://doi.org/10.1007/s11136-017-1641-2.
D’Souza V, Daudt H, Kazanjian A. Survivorship care plans for people with colorectal cancer: do they reflect the research evidence? Curr Oncol. 2016;23(5):e488–98. https://doi.org/10.3747/co.23.3114.
D’Andrea AP, Fernandez CA, Tannenbaum SL, Clarke TC, McClure LA, LeBlanc WG, Lee DJ. Correlates of leisure time physical activity compliance in colorectal cancer survivors. Prev Med. 2014;62:78–82. https://doi.org/10.1016/j.ypmed.2014.01.032.
Fisher A, Wardle J, Beeken RJ, Croker H, Williams K, Grimmett C. Perceived barriers and benefits to physical activity in colorectal cancer patients. Support Care Cancer. 2016;24(2):903–10. https://doi.org/10.1007/s00520-015-2860-0.
Van Putten M, Husson O, Mols F, Luyer MDP, van de Poll-Franse LV, NPM E. Correlates of physical activity among colorectal cancer survivors: results from the longitudinal population-based profiles registry. Support Care Cancer. 2016;24(2):573–83. https://doi.org/10.1007/s00520-015-2816-4.
Ho MY, McBride ML, Gotay C, Grunfeld E, Earle CC, Relova S, Tsonis M, Ruan JY, Chang JT, Cheung WY. A qualitative focus group study to identify the needs of survivors of stage II and III colorectal cancer. Psychooncology. 2016;25(12):1470–6. https://doi.org/10.1002/pon.3988.
Grimmett C, Bridgewater J, Steptoe A, Wardle J. Lifestyle and quality of life in colorectal cancer survivors. Qual Life Res. 2011;20(8):1237–45. https://doi.org/10.1007/s11136-011-9855-1.
Bazzan AJ, Newberg AB, Cho WC, Monti DA. Diet and nutrition in cancer survivorship and palliative care. Evid Based Complement Alternat Med. 2013;2013:917647. https://doi.org/10.1155/2013/917647.
Soares-Miranda L, Abreu S, Silva M, Peixoto A, Ramalho R, da Silva PC, Costa C, Teixeira JP, Gonçalves C, Moreira P, Mota J, Macedo G. Cancer Survivor Study (CASUS) on colorectal patients: longitudinal study on physical activity, fitness, nutrition, and its influences on quality of life, disease recurrence, and survival. Rationale and design. Int J Colorectal Dis. 2017;32(1):75–81. https://doi.org/10.1007/s00384-016-2671-x.
Ko LK, Campbell MK, Lewis MA, Earp J, Devellis B. Mediators of fruit and vegetable consumption among colorectal cancer survivors. J Cancer Surviv. 2010;4(2):149–58. https://doi.org/10.1007/s11764-010-0116-z.
Miller P, Demark-Wahnefried W, Snyder DC, Sloane R, Morey MC, Cohen H, Kranz S, Mitchell DC, Hartman TJ. Dietary supplement use among elderly, long-term cancer survivors. J Cancer Surviv. 2008;2(3):138–48. https://doi.org/10.1007/s11764-008-0060-3.
Borresen EC, Brown DG, Harbison G, Taylor L, O’Malia J, Bazan M, Rao S, Bailey SM, Wdowik M, Weir TL, Brown RJ, Ryan EP. A randomized controlled trial to increase navy bean or rice bran consumption in colorectal cancer survivors. Nutr Cancer. 2016;68(8):1269–80. https://doi.org/10.1080/01635581.2016.1224370.
Hawkins NA, Berkowitz Z, Rodriguez JL. Awareness of dietary and alcohol guidelines among colorectal cancer survivors. Am J Prev Med. 2015;49(6 Suppl 5):S509–17. https://doi.org/10.1016/j.amepre.2015.08.012.
Lawn S, Zrim S, Leggett S, Miller M, Woodman R, Jones L, Kichenadasse G, Sukumaran S, Karapetis C, Koczwara B. Is self-management feasible and acceptable for addressing nutrition and physical activity needs of cancer survivors? Health Expect. 2015;18(6):3358–73. https://doi.org/10.1111/hex.12327.
Moug SJ, Bryce A, Mutrie N, Anderson AS. Lifestyle interventions are feasible in patients with colorectal cancer with potential short-term health benefits: a systematic review. Int J Colorectal Dis. 2017;32(6):765–75. https://doi.org/10.1007/s00384-017-2797-5.
Winkels RM, van Lee L, Beijer S, Bours MJ, van Duijnhoven FJB, Geelen A, Hoedjes M, Mols F, de Vries J, Weijenberg MP, Kampman E. Adherence to the World Cancer Research Fund/American Institute for Cancer Research lifestyle recommendations in colorectal cancer survivors: results of the PROFILES registry. Cancer Med. 2016;5(9):2587–95. https://doi.org/10.1002/cam4.791.
Anderson AS, Steele R, Coyle J. Lifestyle issues for colorectal cancer survivors—perceived needs, beliefs and opportunities. Support Care Cancer. 2013;21(1):35–42. https://doi.org/10.1007/s00520-012-1487-7.
Rock CL, Doyle C, Demark-Wahnefried W, , Meyerhardt J, Courneya KS, Schwartz AL, Bandera EV, Hamilton KK, Grant B, McCullough M, Byers T, Gansler T. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62(4):243–274. doi: https://doi.org/10.3322/caac.21142.
Davies NJ, Batehup L, Thomas R. The role of diet and physical activity in breast, colorectal, and prostate cancer survivorship: a review of the literature. Br J Cancer. 2011;105(Suppl 1):S52–73. https://doi.org/10.1038/bjc.2011.423.
Leong K, Hartley J, Karandikar S. Association of Coloproctology of Great Britain & Ireland (ACPGBI): guidelines for the management of cancer of the colon, rectum and anus (2017)—follow up, lifestyle and survivorship. Colorectal Dis. 2017;(Suppl 1):19(S1):S67–S70. doi: https://doi.org/10.1111/codi.13706.
Cercek A, Holt PR. The care of the colorectal cancer survivor. Curr Opin Gastroenterol. 2017;33(1):26–33. https://doi.org/10.1097/MOG.0000000000000321.
El-Shami K, Oeffinger KC, Erb NL, Willis A, Bretsch JK, Pratt-Chapman ML, Cannady RS, Wong SL, Rose J, Barbour AL, Stein KD, Sharpe KB, Brooks DD, Cowens-Alvarado RL. American Cancer Society colorectal cancer survivorship care guidelines. CA Cancer J Clin. 2015;65(6):428–55. https://doi.org/10.3322/caac.21286.
Doyle C, Kushi LH, Byers T, Courneya KS, Demark-Wahnefried W, Grant B, McTiernan A, Rock CL, Thompson C, Gansler T, Andrews KS. 2006 Nutrition, Physical Activity and Cancer Survivorship Advisory Committee; American Cancer Society. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin. 2006;56(6):323–53.
Acknowledgements
None
Funding
No funding
Author information
Authors and Affiliations
Contributions
AB and DM conceived the study. AB and MYD collected the data and drafted the manuscript. AB, MYD, and DM revised and finalized the manuscript. MYD contacted the authors. All authors read and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Balhareth, A., Aldossary, M.Y. & McNamara, D. Impact of physical activity and diet on colorectal cancer survivors’ quality of life: a systematic review. World J Surg Onc 17, 153 (2019). https://doi.org/10.1186/s12957-019-1697-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-019-1697-2