Abstract
Background
Familial hypercholesterolemia (FH) increases the risk of atherosclerosis in children and adults. Atherosclerotic cardiovascular disease in young patients FH is usually subclinical but recognition of children with more pronounced changes is crucial for adjusting effective management. Aim of this research was to use ultrasonography with two-dimensional speckle tracking (2DST) and tonometry to evaluate atherosclerotic changes in patients with FH (parents and their offspring).
Methods
Applanation tonometry and carotid arteries sonography with evaluation of the intima-media complex thickness (IMCT) and application of the 2DST were performed in 20 families with FH (20 parents and 29 children). The same size control group (age and sex matched) was included. Results were compared between peers and between generations together with the correlation analysis.
Results
Adults with FH, in comparison with healthy peers, presented significantly more atherosclerotic plaques (9 vs. 2, p = 0.0230), had significantly thicker IMC (0.84 ± 0.19 vs. 0.56 ± 0.06 mm, p < 0.0001) and had stiffer arterial wall (for stain: 6.25 ± 2.3 vs. 8.15 ± 2.46, p = 0.0103). In children from both groups there were no atherosclerotic plaques and IMCT did not differ significantly (0.42 ± 0.07 vs. 0.39 ± 0.04, p = 0.1722). However, children with FH had significantly stiffer arterial wall according to 2DST (for strain: 9.22 ± 3.4 vs. 11.93 ± 3.11, p = 0.0057) and tonometry (for the pulse wave velocity: 4.5 ± 0.64 vs.3.96 ± 0.62, p = 0.0047). These parameters correlated with atherosclerosis surrogates in their parents (p < 0.001) but were not significantly affected by presence of presumed pathogenic gene variant.
Conclusions
Children with FH presented subclinical atherosclerosis manifested as decreased arterial wall elasticity. Degree of stiffening was associated with advancement of atherosclerosis in their parents but did not present significant association with gene variants. Sonography with application of 2DST seems to be a good candidate for comprehensive evaluation of atherosclerosis in families with FH.
Similar content being viewed by others

Introduction
Familial hypercholesterolemia (FH) is an autosomal dominant hereditary disease, causing life-long elevated plasma LDL cholesterol (LDL-C) levels. The homozygous form is rare but recent study suggested that the heterozygous one might affect 1 in 200–250 individuals from the general population [1]. Both, pre-mortem [2] and post-mortem studies [3] confirmed FH association with development of premature atherosclerosis in children. Moreover, atherosclerotic cardiovascular disease (ASCVD) that usually starts in middle age or letter was also reported to progresses rapidly at an age of around 10 years in patients with FH. Hence, guidelines for Europe and America highlight that early diagnosis of FH and statin treatment from childhood are necessary for preventing the early-onset ASCVD [4, 5].
Since atherosclerosis in children with FH typically presents in subclinical stage, standard diagnostic imaging methods might not be sufficient. Even discreet morphological changes (thickening of intima-media complex [IMC] evaluated with ultrasound [6, 7]), may be absent while the function of the arterial wall is impaired already. This stiffening process can be assessed with applanation tonometry, with the pulse wave velocity (PWV) and augmentation index (AI) being its two common surrogates. Although tonometry is stated to be the gold standard technique it is not routinely used in clinical practice [8].
On the other hand, a novel sonographic technique - the 2-dimensional speckle tracking (2DST) - can be an alternative that proved its usefulness in evaluation of risk groups of adults [9, 10] and children as well [11]. This method allows to assess pattern of arterial wall deformation due to the flowing pulse wave. Degree of deformation (expressed as strain in %) and its acceleration in time (expressed as strain rate in 1/s) reflect local arterial wall elasticity [9]. Thus, sonography becomes a comprehensive technique that allows for tailoring the diagnostic method for each family member. Particularly that in children discreet disturbances in arterial wall function can be recognized with 2DST, while in their parents atherosclerotic plaques, including their hemodynamic significance, can be assessed with 2D and Doppler ultrasound.
This study aims to compare morphological and functional surrogates of atherosclerosis between family members with FH and healthy peers. First hypothesis is that in families with FH both parents and their offspring will present significantly more advanced atherosclerosis than their healthy counterparts. Second one, that both diagnostic techniques (ultrasound and applanation tonometry) will allow to recognize functional abnormalities. And finally, that the degree of atherosclerotic changes in children with FH will be associated with their aggravation in parents and with type of mutation leading to FH. Confirmation of these hypotheses will enforce the usage of ultrasound with the 2DST technique as a method of choice in evaluation of atherosclerosis in children and adults with FH.
Methods
To this cross-sectional study 20 FH families were recruited from the Regional Rare Disease Center in the Polish Mother’s Memorial Hospital Research Institute (PMMHRI). They comprised 20 parents (10 males, and 10 females) and their 29 children (13 males, and 16 females). The FH was confirmed based on genetic array and/or the Dutch Lipid Clinic Network (DLCN) and Simone Broome Register. In all children the next generation sequencing was performed (MiniSeq, Illumina, Inc., San Diego, US) using custom panel of 21 genes. Obtained data were analyzed with available databases and predictive programs (sorting intolerant from tolerant [SIFT] and polymorphism phenotyping [PolyPhen]). Detected variants were confirmed with the Sanger sequencing. All further examinations were performed within 6 months from the diagnosis of FH in children. Family members not affected with FH were not included. The same number of healthy families (no significant difference in sex and age) was recruited to the control group. Lipid profile of children from the control group was within normal limits while adult Individuals did not present significant abnormalities (levels of total cholesterol (TC), low-density lipoprotein (LDL) and triglycerides (TG) were up to borderline/borderline high levels). Eight adults from the control group reported regular treatment with statins.
In both groups exclusion criteria were chronic diseases (except for hypertension) that might increase the risk of atherosclerosis (i.e.: diabetes mellitus, chronic inflammatory diseases like rheumatoid arthritis or non-specific inflammatory bowel diseases). Hypertension is a common disease, thus it was included into analysis as a risk factor instead of excluding patients from the study. If the exclusion criterion was present in one of family members to be examined the whole family was excluded from the study. No participant had former cardiovascular events (i.e.: acute coronary syndrome or stroke) that were also assumed as criteria excluding the whole family from the study. In both groups data regarding hypertension (diagnosed according to the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) guidelines as Systolic pressure > 140 mmHg and/or diastolic pressure > 90 mmHg [https://doi.org/10.1093/eurheartj/ehy339]) and lifetime tobacco exposure (pack years) were obtained as one of the main atherosclerosis risk factors.
Study protocol
In all patients blood samples were obtained up to 7 days prior to the further examinations. Lipid profile (TC, LDL, TG, high-density lipoprotein [HDL] and non-HDL cholesterol) and HbA1C % were assessed.
At appointed date family members arrived at the hospital at morning hours fasting. They were measured and weighted in light clothing and without shoes to calculate body mass index (BMI). Then the sonographic and tonometric tests were performed by two independent researches blinded to the group affiliation. Examinations techniques were standard, and the detailed description together with accuracy and reproducibility for adults and children was reported before [9,10,11].
Briefly, the sonographic examination was performed with the Samsung RS80 apparatus equipped with a high-frequency linear probe (L3-12A) and Arterial Analysis™ software. The ECG trace was obtained, and the blood pressure was measured in patients lying supine. Major atherosclerotic changes were assessed first (atherosclerotic plaques – soft or calcified, focal IMC thickenings of more than 50% of the adjacent parts of the IMC layer [9]).
Then, the B-mode cine loops of the long and short axis through the common carotid artery (CCA) (just below the bulb) were stored during three consecutive heartbeats for each cross-section. If there was no plaque IMCT was assessed (semi-automatically, during end diastole, at the distance of 150–250 points, with the quality index > 0.9). To evaluate strain and strain rate in short axis cine loop the circular region of interest (ROI) was pointed along the border between the wall and arterial lumen. Parameters were assessed automatically and mean results from 6 heartbeats (three for each side) were included into the analysis.
The PWV and AI were evaluated by another researcher (9 years of experience in tonometric studies) using a SphygmoCor applanation tonometer (SphygmoCor, AtCor Medical, New South Wales, Australia). The AI was assessed based on two measurements of the brachial artery pressure. Then, in patients laying supine, the PWV was measured by recording the arterial pressure waveform at the carotid and femoral artery sampling sites. If the operator index was lower that 75% measurements were repeated.
Statistical analysis
Categorical variables were presented as number and percentages, while continuous variables as mean and standard deviation (SD). In comparison of nominal data between groups the Chi2 test was applied. Normality of continues variables distribution was evaluated with the Shapiro-Wilk test. Due to distribution other than normal comparisons of means between two independent subgroups (adults with FH vs. healthy adults and children with FH vs. healthy children) were performed with the Mann-Whitney test. When subgroups were related (adults with FH vs. children with FH and healthy adults vs. healthy children) the Wilcoxon signed rank test was applied. Associations between continuous variables were evaluated with the Spearman’s rank correlation test. The analysis was performed with Statistica 12 software (StatSoft Poland, Cracow, Poland). In general a p-value lower than 0.05 was considered significant, however for multiple comparisons the Bonferroni correction was applied.
Results
Comparison of demographic data and laboratory tests are presented in Table 1. Individuals with FH did not differ significantly according to determined additional risk factors of atherosclerosis (BMI, hypertension, tobacco exposure, increased concentration of HbA1C). However, both parents and children with FH presented significantly higher values of TC, LDL-C, non-HDL-C and TG in comparison to their healthy counterparts, despite the fact that all adults were treated with statins.
Morphological features of atherosclerosis
Adults with FH had significantly more atherosclerotic plaques (total number of 7, mean thickness 4 mm ± 1,2 mm) than parents from the control group (total number of 2, thickness of 1,8 mm and 2,3 mm). In analysis of IMCT adults with FH presented significantly thicker layer than observed in healthy adults (Table 2). Moreover, in both groups parents had significantly thicker IMC than their children (Table 2). In children there were no atherosclerotic plaques and the IMCT did not differ significantly between individuals with FH and healthy one.
Functional features of atherosclerosis
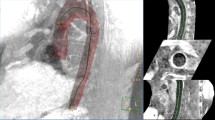
Both, parents and children with FH, presented significantly increased arterial stiffness in comparison with their healthy counterparts (Table 2). It was confirmed with tonometry as well as with the 2DST (Fig. 1). Stiffness parameters differed also between parents and children from the same group (adults with FH vs. children with FH and healthy adults vs. healthy children, Table 2).
Association of atherosclerosis markers with gens
In 5 children we found only single, likely pathogenic, gene variant, 14 children had 2 gene variants, 8 children had 3 variant gens, 3 children had 4 gene variants and in two children we did not find any variant from the analyzed panel. Sequencing identified LDLR mutations as the most common cause of FH in the tested group. In 17 patients 15 substitutions, one intragenic deletion and one intragenic duplication of LDLR were found. Variants were also revealed in APOE (6 children), PCSK9 (4 children), LCAT (4 children), ABCG5 (4 children), ABCA1 (3 children), GPIHBP1 (2 children), SCAP (2 children) and APOA (1 child).
We compared atherosclerosis markers between individuals in whom variants were presumed pathogenic according to prognostic programs or literature. There was only a trend towards more advanced atherosclerotic changes in children with these variants but the difference was not significant (Table 3).
Parameters correlations
In both groups and for both generations there was a significant correlation between IMCT and parameters derived from tonometry and those from 2DST. Only in adults stiffness parameters correlated with IMCT. On the contrary, only in adults with FHs there was a significant correlation between IMCT and stiffness parameters with stiffness parameters in their children (Table 4). In all subgroups, there was no significant association between concentrations of lipid profile components and analyzed surrogates of atherosclerosis.
Discussion
In this study family members with FH, parents as well as their offspring, presented more advanced atherosclerosis than their healthy peers. Adults with FH had both morphological and functional changes while in children with FH only arterial function was impaired (decreased elasticity). Moreover, in patients with FH there was a correlation of atherosclerosis surrogates between adults and their children. On the other hand, presence of presumed pathogenic gene variant in children did not result in significantly aggravated markers of atherosclerosis. Finally, disturbances of arterial wall elasticity were recognized in ultrasound and applanation tonometry and they correlated with each other. However, sonography allows for more comprehensive evaluation of atherosclerosis aggravation.
FH increases the risk of atherosclerosis and predispose to cardiovascular events in younger age than in healthy population [12, 13]. Although monozygotic form is rare, as many as 1 per 250 people from general population is a heterozygote [14]. It gives approximately 4.5 million individuals in Europe, of whom 20–25% are children and adolescents [15]. Despite analyses proofing cost effectiveness of FH screening [16] and treatment standards, which are developed (diet, controlling risk factors, statins [5]) or developing (gene- and cell-based therapies [17]), under-diagnosing of the disease is a major problem [18]. This work provides another argument for introducing screening programs because, even in children with no significant morphological changes, arterial wall function can be already impaired. Diagnosis of subclinical arterial wall stiffening might improve risk stratification and clinical management in FH patients [13, 19].
Many researchers have already confirmed increased risk of atherosclerosis (also subclinical [20]) and subsequent cardiovascular events in adults with FH [21]. Studies concerning children with FH are not as numerous [15, 22,23,24] but it is well documented that FH children have significantly increased IMCT in carotid arteries, femoral arteries and aorta when compared with healthy children as well as healthy siblings [24, 25]. Although, there are discrepancies in age from which these differences become significant (between 10 and 12 for siblings [24, 26] and 9–11 years for nonrelated controls [22, 25]) and they can also be affected by treatment with statins. Luirink et al., in their study with 20-years long follow up, proofed that although children with FH had initially significantly thicker IMC than healthy siblings, differences become insignificant during years of treatment with statins. It is worth to notice that in aforementioned studies morphological changes were slight (fractions of millimeter). Thus, to reach the level of statistical significance study populations had to be larger than in our research. It may explain why we observed only a slight numerical trend towards thicker IMC. On the other hand, in our group we were able to detect significant deterioration of arterial wall function. It might suggest superiority of arterial wall elasticity surrogates as markers of atherosclerosis in children with FH.
Arterial wall function was reported to be impaired in children with FH, however in former researches it was proofed mainly by flow-mediated dilation (FMD) test [27, 28] and markers calculated from 2D images (e.g. young elastic modulus, beta-stiffness index) [28, 29]. Riggio at al [29]. investigating the group of 44 children with increased cholesterol levels (18 with FH) showed that arterial wall function was impaired in comparison with healthy control, while there was no significant difference in IMCT. Although, they also used echo-tracking software, it was applied to calculate arterial wall elasticity surrogates (beta-stiffness index, arterial compliance, AIx, local PWV, Young elastic modulus) and results were not confirmed by a gold standard method (tonometry). Aggoun et al. [28] using sonography and FMD test also showed that in children with FH (30 males, mean age of 11 ± 2 years old) the arterial wall function was impaired when no significant changes in IMCT were observed. Despite applying surrogates depending on blood pressure in this last study, both studies are in line with our observations, and confirm that there is a continuum of atherosclerotic changes that impairs the arterial wall function first and then affects its morphology.
To conclude the above, in our opinion application of sonography with 2DST technique is more convenient and efficient than employing other methods for evaluation of atherosclerosis. On the contrary to the FMD procedure it does not require several minutes of painful forearm compression. Currently, purchasing of 2DST software is cheaper than buying an applanation tonometer, which handling requires experience. Moreover, repeatability of the stain evaluation with 2DST is higher than reported for tonometry, while their results correlate with each other [11, 30]. Finally, sonography is the most comprehensive technique because after storing a few loops of arterial wall motion not only function surrogates can be calculated in a semiautomatic manner, but also IMCT and atherosclerotic plaques can be assessed, what would be especially important in older patients. To confirm presented opinion, with application of discussed technique it was possible to examine two generations of patients and showed not only that individuals with FH had significantly advanced atherosclerosis than their healthy peers, but also that there was a relation between degree of atherosclerotic changes between parents and their offspring. This last observation is unique for such a young group of patients. Till now, it was only reported that maternal or paternal origin of FH does not affect carotid IMCT or phenotype of plasma lipid levels, while type of transferred mutation does [31, 32]. As far as a direct relation is concerned, in study of 154 families with other cardiovascular risk factors than FH, there was a IMCT correlation between parents and children, however median of age for parents was 61 years and for children 36 years [33].
Recognition of genetic background of the FH becomes important nowadays because particular mutations were reported to affect phenotype of patients and due to new possibilities of treatment [33,34,35,36,37]. Unfortunately, no significant association between presence of presumed pathogenic gene variants and aggravation of atherosclerosis was observed. It might be due to small analyzed group of children and young age, that did not allow to develop differences in phenotype. On the other hand, even in children genetic variability may play a significant role what is suggested a significant correlations of atherosclerosis markers between parents and their offspring who share the same gene variants.
Strength and study limitation
The main strength of this study is that results obtained based on the novel sonographic technique were confirmed with a gold standard method. Moreover, due to including family members from two generations it was possible to proof comprehensiveness of sonography with 2DST in evaluation of atherosclerosis in adults and children.
Nevertheless, this study has some limitations. Healthy family members were excluded from the study. In comparison of FH children with their healthy siblings significant differences in IMCT were observed from age 7 years. It would be interesting to compare strain and strain rate between them. However, this study addressed relation between adults and children affected with FH. Furthermore, evaluated group did not allow for such an analysis due to not enough of siblings appropriate to enter the study.
Secondly, small study population did not allow to draw conclusions on association between genetic variance and aggravation of atherosclerosis. Nevertheless, our main aim was to indicate convenient and reliable technique for examining whole families with FH what gives foundation for future studies of larger population.
Conclusions
Children with FH presented subclinical atherosclerosis that manifested with arterial wall stiffening. Aggravation of changes was associated with advancement of atherosclerosis in their parents but was not significantly affected by a type of recognized gene variant. Sonography with application of 2DST seems to be the best candidate for comprehensive evaluation of atherosclerosis in families with FH.
Availability of data and materials
On request.
Abbreviations
- 2DST:
-
Two-dimensional speckle tracking
- AI:
-
Augmentation index
- ASCVD:
-
Atherosclerotic cardiovascular disease
- BMI:
-
Body mass index
- DLCN:
-
The Dutch Lipid Clinic Network
- ECG:
-
Electrocardiogram
- ESH:
-
The European Society of Hypertension
- ESC:
-
The European Society of Cardiology
- FH:
-
Familial hypercholesterolemia
- FMD:
-
Flow-mediated dilation
- HbA1C:
-
Glycated hemoglobin
- HDL:
-
High-density lipoprotein
- IMCT:
-
Intima-media complex thickness
- IMC:
-
Intima-media complex
- LDL:
-
Low-density lipoprotein
- LDL-C:
-
LDL cholesterol
- PMMHRI:
-
The Polish Mother’s Memorial Hospital Research Institute
- PolyPhen:
-
Polymorphism phenotyping
- PWV:
-
Pulse wave velocity
- ROI:
-
Region of interest
- SIFT:
-
Sorting intolerant from tolerant
- SD:
-
Standard deviation
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
References
Mabuchi H, Nohara A, Noguchi T, Kobayashi J, Kawashiri MA, et al. Molecular genetic epidemiology of homozygous familial hypercholesterolemia in the Hokuriku district of Japan. Atherosclerosis. 2011;214:404–7.
Li S, Chen W, Srinivasan SR, Bond MG, Tang R, et al. Childhood cardiovascular risk factors intima and carotid vascular changes in adulthood: the Bogalusa heart study. JAMA. 2003;290:2271–6.
Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. Natural history of aortic and coronary atherosclerotic lesions in youth. Findings from the PDAY Study. Arterioscler Thromb. 1993;13:1291–8.
Myśliwiec M, Walczak M, Małecka-Tendera E, Dobrzańska A, Cybulska B, et al. Management of familial hypercholesterolemia in children and adolescents. Position paper of the Polish Lipid Expert Forum. J Clin Lipidol. 2014;8:173–80.
Harada-Shiba M, Ohta T, Ohtake A, Ogura M, Dobashi K, et al. Guidance for pediatric Familial hypercholesterolemia 2017. J Atheroscler Thromb. 2018;25:539–53. https://doi.org/10.5551/jat.CR002.
Margeirsdottir HD, Stensaeth KH, Larsen JR, Brunborg C, Dahl-Jorgensen K. Early signs of atherosclerosis in diabetic children on intensive insulin treatment: a population-based study. Diabetes Care. 2010;33:2043–8.
Rostampour N, Fekri K, Hashemi-Dehkordi E, Obodiat M. Association between vascular endothelial markers and carotid intima-media thickness in children and adolescents with type 1 diabetes mellitus. J Clin Diagn Res. 2017;11:SC01–5.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, et al. 2007 guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2007;28:1462–536.
Podgórski M, Grzelak P, Szymczyk K, Szymczyk E, Drożdż J, et al. Peripheral vascular stiffness, assessed with two-dimensional speckle tracking versus the degree of coronary artery calcification, evaluated by tomographic coronary artery calcification index. Arch Med Sci. 2015;11:122–9.
Podgórski M, Grzelak P, Kaczmarska M, Polguj M, Łukaszewski M, et al. Feasibility of two-dimensional speckle tracking in evaluation of arterial stiffness: comparison with pulse wave velocity and conventional sonographic markers of atherosclerosis. Vascular. 2018;26:63–9.
Podgórski M, Szatko K, Stańczyk M, Pawlak-Bratkowska M, Fila M, et al. Two-Dimensional Speckle Tracking Versus Applanation Tonometry in Evaluation of Subclinical Atherosclerosis in Children with Type 1 Diabetes Mellitus. Med Sci Monit. 2019;28:7289–94. https://doi.org/10.12659/MSM.916466.
Dyrbuś K, Gąsior M, Desperak P, Osadnik T, Nowak J, Banach M. The prevalence and management of familial hypercholesterolemia in patients with acute coronary syndrome in the polish tertiary Centre: results from the TERCET registry with 19,781 individuals. Atherosclerosis. 2019;288:33–41.
Martin AC, Gidding SS, Wiegman A, Watts GF. Knowns and unknowns in the care of pediatric familial hypercholesterolemia. J Lipid Res. 2017;58:1765–76. https://doi.org/10.1194/jlr.S074039.
EAS Familial Hypercholesterolaemia Studies Collaboration, Vallejo-Vaz AJ, De Marco M, CAT S, Akram A, et al. Overview of the current status of familial hypercholesterolaemia care in over 60 countries - the EAS Familial Hypercholesterolaemia studies collaboration (FHSC). Atherosclerosis. 2018;277:234–55. https://doi.org/10.1016/j.atherosclerosis.2018.08.051.
Wiegman A, Gidding SS, Watts GF, Chapman MJ, Ginsberg HN, et al. Familial hypercholesterolaemia in children and adolescents: gaining decades of life by optimizing detection and treatment. Eur Heart J. 2015;21:2425–37. https://doi.org/10.1093/eurheartj/ehv157.
Pelczarska A, Jakubczyk M, Jakubiak-Lasocka J, Banach M, Myśliwiec M, et al. The cost-effectiveness of screening strategies for familial hypercholesterolaemia in Poland. Atherosclerosis. 2018;270:132–8. https://doi.org/10.1016/j.atherosclerosis.2018.01.036.
Hajighasemi S, Mahdavi Gorabi A, Bianconi V, Pirro M, Banach M, et al. A review of gene- and cell-based therapies for familial hypercholesterolemia. Pharmacol Res. 2019;143:119–32. https://doi.org/10.1016/j.phrs.2019.03.016.
Češka R, Freiberger T, Susekov AV, Paragh G, Reiner Ž, et al. ScreenPro FH - screening project for Familial hypercholesterolemia in central, Southern and Eastern Europe: Basic Epidemiology. Vnitr Lek Winter. 2017;63:25–30.
Braamskamp MJAM, Langslet G, McCrindle BW, Cassiman D, Francis GA, et al. Effect of Rosuvastatin on carotid intima-media thickness in children with heterozygous Familial hypercholesterolemia: the CHARON study (hypercholesterolemia in children and adolescents taking Rosuvastatin open label). Circulation. 2017;25:359–66. https://doi.org/10.1161/CIRCULATIONAHA.116.025158.
Caballero P, Alonso R, Rosado P, Mata N, Fernández-Friera L, et al. Detection of subclinical atherosclerosis in familial hypercholesterolemia using non-invasive imaging modalities. Atherosclerosis. 2012;222:468–72. https://doi.org/10.1016/j.atherosclerosis.2012.02.043.
Miname MH, Ribeiro MS 2nd, Parga Filho J, Avila LF, Bortolotto LA, et al. Evaluation of subclinical atherosclerosis by computed tomography coronary angiography and its association with risk factors in familial hypercholesterolemia. Atherosclerosis. 2010;213:486–91. https://doi.org/10.1016/j.atherosclerosis.2010.10.001.
Luirink IK, Wiegman A, Kusters DM, Hof MH, Groothoff JW, et al. 20-year follow-up of statins in children with Familial hypercholesterolemia. N Engl J Med. 2019;381(16):1547–56. https://doi.org/10.1056/NEJMoa1816454.
Narverud I, Retterstøl K, Iversen PO, Halvorsen B, Ueland T, et al. Markers of atherosclerotic development in children with familial hypercholesterolemia: a literature review. Atherosclerosis. 2014;235:299–309. https://doi.org/10.1016/j.atherosclerosis.2014.05.917.
Slyper AH. Clinical review 168: what vascular ultrasound testing has revealed about pediatric atherogenesis, and a potential clinical role for ultrasound in pediatric risk assessment. J Clin Endocrinol Metab. 2004;89:3089–95.
Guardamagna O, Restagno G, Rolfo E, Pederiva C, Martini S, et al. The type of LDLR gene mutation predicts cardiovascular risk in children with familial hypercholesterolemia. J Pediatr. 2009;155:199e204. E192.
Guardamagna O, Abello F, Saracco P, Baracco V, Rolfo E, Pirro M. Endothelial activation, inflammation and premature atherosclerosis in children with familial dyslipidemia. Atherosclerosis. 2009;207:471e5.
Wiegman A, de Groot E, Hutten BA, Rodenburg J, Gort J, et al. Arterial intima-media thickness in children heterozygous for familial hypercholesterolaemia. Lancet. 2004;363:369–70.
de Jongh S, Lilien MR, Bakker HD, Hutten BA, Kastelein JJ, et al. Family history of cardiovascular events and endothelial dysfunction in children with familial hypercholesterolemia. Atherosclerosis. 2002;163:193–7.
Aggoun Y, Bonnet D, Sidi D, Girardet JP, Brucker E, et al. Arterial mechanical changes in children with familial hypercholesterolemia. Arterioscler Thromb Vasc Biol. 2000;20:2070–5.
Riggio S, Mandraffino G, Sardo MA, Iudicello R, Camarada N, et al. Pulse wave velocity and augmentation index, but not intima-media thickness, are early indicators of vascular damage in hypercholesterolemic children. Eur J Clin Investig. 2010;40:250e7.
Lowenthal A, Evans JM, Punn R, et al. Arterial applanation tonometry: feasibility and reproducibility in children and adolescents. Am J Hypertens. 2014;27:1218–24.
Narverud I, van Lennep JR, Christensen JJ, Versmissen J, Gran JM, et al. Maternal inheritance does not predict cholesterol levels in children with familial hypercholesterolemia. Atherosclerosis. 2015;243:155–60. https://doi.org/10.1016/j.atherosclerosis.2015.09.014.
Kusters DM, Avis HJ, Braamskamp MJ, Huijgen R, Wijburg FA, et al. Inheritance pattern of familial hypercholesterolemia and markers of cardiovascular risk. J Lipid Res. 2013;54:2543–9. https://doi.org/10.1194/jlr.M034538.
Moskau S, Golla A, Grothe C, Boes M, Pohl C, et al. Heritability of carotid artery atherosclerotic lesions: an ultrasound study in 154 families. Stroke. 2005;36:5–8.
Banach M, Penson PE. Genetic testing in familial hypercholesterolaemia: what does it add? Eur J Prev Cardiol. 2019;13:2047487319870342. https://doi.org/10.1177/2047487319870342.
Banach M, Mazidi M, Mikhailidis DP, Toth PP, Jozwiak J, et al. Association between phenotypic familial hypercholesterolaemia and telomere length in US adults: results from a multi-ethnic survey. Eur Heart J. 2018;21:3635–40.
Lee S, Akioyamen LE, Aljenedil S, et al. Genetic testingfor familial hypercholesterolaemia: Impact on diagnosis,treatment and cardiovascular risk. Eur J Prev Cardiol. 2019;26:1262–70.
Funding
This work was supported by the Polish Mother’s Memorial Hospital Research Institute, Lodz, Poland (grants numbers 2016/IV/56MN and 2016/X/9SZB).
Author information
Authors and Affiliations
Contributions
MP: research concept and design, collection and assembly of data, data analysis and interpretation, writing the article, final approval of article. KS: collection and assembly of data, writing the article, final approval of article. MS: recruitment of patients, collection of data, data analysis and interpretation, writing the article, final approval of article. MP-B: recruitment of patients, assembly of data, data analysis and interpretation, writing the article, final approval of article. AK: recruitment of patients, writing the article, final approval of article. ES: research concept and design, data analysis and interpretation, critical revision of the article, final approval of article. MT: research concept and design, data analysis and interpretation, critical revision of the article, final approval of article. SG: research concept and design, data analysis and interpretation, critical revision of the article, final approval of article. LR: performing and analyzing genetic tests, writing the article, critical revision of the article, final approval of article. AG: performing and analyzing genetic tests, critical revision of the article, final approval of article. MŁ: research concept and design, assembly of data, data analysis and interpretation, writing the article, final approval of article. PG: research concept and design, critical revision of the article, final approval of article. MB: research concept and design, data analysis and interpretation, critical revision of the article, final approval of article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the local Bioethical committee (approval number 28/2016). All the participants/participants’ guardians signed informed consent.
Consent for publication
All authors of the manuscript have read and agreed to its content and are accountable for all aspects of the accuracy and integrity of the manuscript in accordance with ICMJE criteria. The article is original, has not already been published in a journal, and is not currently under consideration by another journal. We agree to the terms of the BioMed Central Copyright and License Agreement, where applicable, Open Data policy.
Competing interests
MB - speakers bureau: Abbott/Mylan, Abbott Vascular, Actavis, Akcea, Amgen, Biofarm, KRKA, MSD, Sanofi-Aventis, Servier and Valeant; consultant to Abbott Vascular, Akcea, Amgen, Daichii Sankyo, Esperion, Lilly, MSD, Resverlogix, Sanofi-Aventis; Grants from Sanofi and Valeant; all other authors have nothing to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Podgórski, M., Szatko, K., Stańczyk, M. et al. “Apple does not fall far from the tree” – subclinical atherosclerosis in children with familial hypercholesterolemia. Lipids Health Dis 19, 169 (2020). https://doi.org/10.1186/s12944-020-01335-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-020-01335-2