Abstract
Sepsis is a severe disease with a high mortality rate. Identification and treatment in the initial hours of the disease improve outcomes. Some biomarkers like procalcitonin and C-reactive protein are used for diagnosis and to access sepsis prognosis and they can help in clinical decision-making, but none has sufficient specificity or sensitivity to be routinely employed in clinical practice. This review seeks to evaluate lipid metabolism alterations in patients with sepsis and the possibility of using the respective metabolites as biomarkers of the disease. A search of the main electronic biomedical databases was conducted for the 20-year period ending in February 2020, focused on primary research articles on biomarkers in sepsis. The keywords included sepsis, septic shock, biomarker, metabolomic, lipidomic and lysophosphatidylcoline.
. It concludes that altered lipid profiles, along with the progress of the disease should provide new insights, enabling a better understanding of the pathogenic mechanisms and making it possible to design new early diagnosis and therapeutic procedures for sepsis.
Similar content being viewed by others
Background
Sepsis is a major healthcare problem and affects millions of people around the world. Patients who develop the illness have high mortality rates (at least one in four) [1, 2]. Identification and treatment in the initial hours of the disease considerably improve outcomes [3]. Sepsis is a situation in which affected individuals develop an inflammatory response to an infection that harms their own organs and culminates in organ dysfunction [4]. Patients present signs of systemic inflammatory response syndrome and sometimes it is difficult for clinicians to define whether it is due to infection or other causes [5]. In that situation, the use of biomarkers could help with early diagnosis and improved risk stratification and clinical decision making [6,7,8].
Some biomarkers have been evaluated for use in sepsis diagnosis but none have sufficient specificity or sensitivity to be routinely employed in clinical practice. Procalcitonin (PCT) and C-reactive protein (CRP) have been the most widely used, but even they have limited ability to distinguish sepsis from other inflammatory conditions or to predict outcomes [9]. Altered lipid metabolism and its pro/anti-inflammatory lipid mediators play key roles in sepsis pathophysiology.
The use of multi-'omics’ (association of at least two ‘omic’ variables: genomic, lipidomic, proteomic or metabolomic) may lead to an understanding of the pathophysiology of the disease and to the development of appropriate therapeutics. For example, in the treatment cascade of an endotoxin, the performance of a drug could alter its neutralization, influencing clearance, inflammation, bacterial load and mortality [10].
The objective of this review is to evaluate the changes of lipid metabolism in patients with sepsis and the possibility of using the respective metabolites as biomarkers of this disease. A search of the main electronic biomedical databases (PubMed, MEDLINE, Scopus, and Web of Science) was conducted for the 20-year period ending in February 2020, focused on primary research articles on biomarkers in sepsis. The keywords searched for in the abstracts and titles included “sepsis”, “septic shock”, “biomarker,” “metabolomic”, “lipidomic”, and “lysophosphatidylcoline”. The search identified 16 references with the words lipidomic x sepsis x septic shock, 34 references with the words metabolomic x sepsis x septic shock, and 13 references with the words lysophosphatidylcoline x sepsis x septic shock.
Review
Sepsis as a healthcare problem
Sepsis is a major healthcare problem and affects millions of people around the world. The mortality rate among patients that develop the illness is high (at least one in four) [1, 2]. The actual incidence of the disease in the world is uncertain. However, Fleischmann et al. made a systematic bibliographic survey and based on a statistical extrapolation of the results obtained, they suggest estimates of 31.5 million cases ofinfection, 19.4 million cases of sepsis and 5.3 million deaths per year [11].
The incidence of sepsis is increasing annually. Analyses of the occurrence of sepsis over a 22-year period (1979 to 2000), using data of a nationally representative sample of hospitals in the United States, identified more than 10 million cases in 750 million hospitalizations [1]. A large observational study in a European setting revealed an estimated mean sepsis incidence of 212.7 cases per 100,000 inhabitants with an annual incidence increase of 7.3%. In Brazil, sepsis incidence was 36.3 per 1000 patient-days and sepsis mortality was 55.7% [12].
Sepsis is a syndrome involving factors of both pathogen and host such as age, comorbidities, environment and race. It is defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection; a situation in which affected individuals develop an inflammatory response to an infection injuring their own organs and culminating in organ dysfunction. Septic shock is defined as a subset of sepsis in which underlying circulatory and cellular metabolism abnormalities are profound enough to substantially increase mortality. The patients present persistent hypotension requiring vasopressors to maintain mean arterial pressure ≥ 65 mmHg and hyperlactatemia in the absence of hypovolemia. In septic shock, mortality is more elevated (> 40%) and early identification and treatment in the initial hours of the disease improve outcomes [3].
Sepsis, similar to other systemic inflammatory response syndromes, is characterized by increased secretion of stress hormones (e.g. catecholamines and cortisol) and cytokines, complement system activation and mitochondrial dysfunction with decreased availability of ATP. Sepsis-related inflammation causes microcirculatory dysfunction, inadequate tissue oxygen supply and subcellular and cellular dysfunction [13]. Initially, in response to infection, the innate immunity is activated when microorganisms contact receptors localized in cell surfaces (toll-like receptors - TLR). Binding TLR stimulates intracellular signaling and, in turn, production of proinflammatory (TNF- α, IL-1) and anti-inflammatory molecules (IL-10) [14, 15]. There is an alteration to the pro-oxidant-antioxidant balance. Also, there is an increase in the concentration of inflammatory cytokines (TNF-α and IL-8) and a decrease in the plasma activity of superoxide dismutase (SOD) and catalase (CAT) [16]. TNF-α and IL-8 exert cardiac depression by reducing myocardial shortening [17], further jeopardizing the patient’s hemodynamics. Pro-inflammatory cytokines lead to larger adhesion molecules in neutrophils and endothelial cells. Activated neutrophils promote microorganism kill and injure endothelial cells too, increasing vascular permeability [18]. Cytokines foster coagulation, stimulating thrombin formation in the microvascular bed and contributing to organ failure. In addition, consumption of coagulation proteins promotes bleeding [15]. Organ failure may be explained by microvascular occlusion, disruption of oxygenation with tissue exudate and production of reactive oxygen types [19]. In addition, there is evidence that in sepsis, alterations occur in mitochondrial function, with a decrease in the supply of tissue oxygen thereby contributing to organic dysfunction and increased production of free radicals, impacting on cellular metabolism and inflammatory processes [20, 21]. The increase in the production of reactive oxygen species (ROS) leads to organic dysfunctions caused by cellular and endothelial lesion due to protein modification and lipid peroxidation [22].
Effects of infection and inflammation on lipid and lipoprotein metabolism
Septic patients present alterations in lipid metabolism such as hypertriglyceridemia, a decrease in HDL and LDL-cholesterol and insulin resistance [23, 24]. Lipoprotein concentration can be reduced to 50% in patients with sepsis and those reductions seem to be related to the severity of the disease [25]. The primary decline is found in HDL and slow recovery occurs in HDL and LDL fractions. The decrease of HDL is not found in patients with trauma or other critical illnesses [26]. During sepsis, HDL is elevated in the HDL-acute phase attained in the presence of serum amyloid A, one of the three major acute phase proteins [27], and in depleted cholesterol and apolipoprotein A-1 [28] conditions. Inhibition of lipoprotein lipase, upregulated hepatic triglyceride production stimulated by hyperglycemia and hyperinsulinemia, the action of cytokines and the disruption of the synthesis-utilization balance are probably responsible for those alterations [29].
The changes in lipid metabolism during sepsis serve as a protective response against infection.
Lipopolysaccharide (LPS) is a constituent of Gram-negative bacteria that is involved in the inflammatory response to sepsis [30] and the presence of LPS in patients’ blood is a clear indicator of sepsis. However, detection of LPS in aqueous blood is complicated by the molecule’s amphiphilic biochemistry, which drives it to associate with host carrier lipoproteins [31] and other molecules such as LPS-binding protein (LBP), high-density lipoprotein (HDL), low-density lipoprotein (LDL), very low-density lipoprotein (VLDL) and bactericidal/permeability-increasing protein [32]. Lipoproteins are known to be involved in the response of immunity neutralizing LPS, reducing cellular adhesion and reducing inducible nitric oxide synthase expression [33]. The structural changes in HDL may have a protective function and have metabolic consequences [34]. Chylomicron and very low-density lipoprotein neutralize the biological effects of endotoxin, and HDL particles control infection and the systemic inflammatory response [29].
Inflammation is modulated by lipid mediators derived from long chain polyunsaturated fatty acids (PUFA) with 20 or 22 carbons (n-6 or n-3 families). Those lipid mediators (eicosanoids and docosanoids) lead to metabolic changes that alter the plasma FA profile [22]. Patients with sepsis present low concentrations of n-6 and n-3 PUFAs and a high n-6/n-3 ratio and that is associated with high mortality [35,36,37,38]. An increase in oleic acid (C18:1 n-9) accompanied by a decrease in the unsaturation index as well as in the levels of n-3 PUFA was observed in erythrocyte phospholipids of septic patients as compared to healthy controls [39]. Arachidonic acid metabolism is also markedly affected in patients with sepsis. A reduced LPS-induced release of AA and the COX-associated AA metabolites, 11-HETE, PGE2, and TXB2 was apparent in septic patients [40]. Also, decreased lysophosphatidylcholine (LPC) levels and increased ceramide (Cer) species rates in plasma are commonly associated with sepsis [37,38,39,40,41]. An investigation of sepsis from peritonitis using a swine model monitored changes in hemodynamic, blood chemistry, and inflammatory markers. Mass spectrometry-based targeted quantitative analyses of blood samples were performed and found marked decreased in PC and LPC species [42]. Those results were supported by our group in a clinical study which observed important alterations in lipid metabolism in patients with sepsis, specifically including LPCs and sphingomyelin (SMs). Both LPCs and SMs were downregulated, whereas the saturated and unsaturated PCs were upregulated in the plasma and erythrocytes of septic patients [39]. Previous studies have also demonstrated an increase in circulating phospholipase A2 type II (snp-PLA2) in patients with severe infection [43, 44]. Group IIA sPLA2 is an acute-phase protein that is expressed in various tissues and cells in response to pro-inflammatory cytokines and it serves to amplify the systemic inflammatory response [45]. Members of the sPLA2 family of enzymes generate bioactive lipid mediators that include lysophosphospholipids and arachidonic acid and which can be converted to eicosanoids. Eicosanoids modulate cell growth and differentiation, inflammation, immunity, platelet aggregation and many other functions. Eicosanoids produced from arachidonic acid by COX and LOX, respectively, are 2-series PG and 4-series LT that act as mediators of inflammatory processes [46].
Biomarkers in sepsis
With the present systemic inflammatory response syndrome signals, it is sometimes difficult for clinicians to define whether it is due to infection or other causes [5]. In that situation, the use of biomarkers could help with early diagnosis, improving risk stratification and clinical decision-making [6,7,8].
Some biomarkers have been evaluated for use in sepsis. Most of them have been tested clinically, primarily as prognostic markers in sepsis. There are hundreds of biomarkers which could potentially be used for diagnosis and prognosis in septic patients [47]. They are classified as cytokine/chemokine biomarkers, cell marker biomarkers, receptor biomarkers, coagulation biomarkers, biomarkers related to vascular endothelial damage, biomarkers related to vasodilation, biomarkers of organ dysfunction and acute phase protein biomarkers [9]. Also, thirty-four biomarkers have been identified for use specifically in the diagnosis of sepsis but only five of them (CD11b, CD64, IL-12, IP-10 and PLA2-II) have reported sensitivity and specificity values greater than 90%.
A study with proteomic analysis, conducted with patients with sepsis and septic shock with a pulmonary focus, showed alterations in the proteins expressed in surviving and non-surviving sepsis patients alike. Of a total of 179, after excluding albumin and immunoglobulins, 48 were found to have been altered (16 specific proteins for survivors and 20 for non-survivors). Among the alterations in the concentrations of the proteins found were those associated to cytoskeletal organization, cell movement, energy metabolism, inflammation, coagulation and bleeding. The results also showed negative regulation of apolipoproteins like ApoA2, ApoA4, ApoC1, ApoC2, ApoC3, Apod and Pon1 [48].
So, due to their low specificity or sensitivity the use of these biomarkers is limited in routine clinical practice. Procalcitonin (PCT) and C-reactive protein (CRP) have been most widely used, but even they have limited ability to distinguish sepsis from other inflammatory conditions or to predict outcomes. Procalcitonin (PCT) is a propeptide of calcitonin produced in low concentrations by the thyroid, gastrointestinal tract and lungs in healthy individuals. In the presence of bacterial infections, pro-inflammatory mediators induce an upregulated production and, with treatment, levels decrease by 50% per day [49]. The use of PCT to guide antimicrobial therapy has low to moderate quality in minimizing endpoints like mortality, mechanical ventilation, clinical severity and reinfection [50].
Liu et al. conducted a meta-analysis with 86 articles and a total of 10,438 subjects included. They found descriptions of 60 biomarkers and the most common were procalcitonin, C-reactive protein, interleukin 6, soluble triggering receptor expressed on myeloid cells-1, presepsin, lipopolysaccharide binding protein and CD64. Plasma PCT, Strem-1 and presepsin had moderate diagnostic utility for indicating systemic response caused by infection rather than other causes [51]. C-reactive protein (CRP) and procalcitonin are the most commonly used biomarkers. However, CRP has low specificity [52]. Procalcitonin is more specific [53] than CPR, but it remains difficult for it to differentiate sepsis from other non-infection causes of inflammation [54].
A recent comprehensive review of the available experimental evidence has shown that different biomarkers have clearly been demonstrated as indicating varying injury mechanisms and can be used in early diagnosis for sepsis-induced acute kidney injury [55].
Lipid biomarker
Lipids are regulators of cellular function and their metabolism is altered in patients with sepsis. Based on that, lipidomics can be used to understand the pathophysiological mechanisms involved in the diagnosis and the response to therapeutic measures [56]. Lipidomics is the analysis of lipid metabolism and is accessed by spectrophotometric techniques [57] and chromatography [58].
LPC has been suggested to serve as a more useful prognostic marker for sepsis [37, 59, 60]. Park et al. performed a study comparing quantitative analyses of LPC 16:0 by using matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF) mass spectrometry and found a sensitivity and a selectivity of medical diagnosis of sepsis estimated to be 97.9 and 95.5% on comparing analyses of sera from patients with severe sepsis and septic shock (n = 143), pneumonia patients (n = 12), and healthy individuals (n = 31) [61]. Lysophospholipids are membrane-derived phospholipids that can arise from homeostatic lipid metabolism or as a response to stimulus-induced cellular activation. Sources of plasma LPC include hydrolysis of PC by secretory phospholipase A2 (sPLA2) or lecithin:cholesterol acyltransferase (LCAT). LPC, in turn, is hydrolyzed to LPA in the plasma by autotaxin. LPA can also be synthesized from PA by sPLA2 [62]. In the phospholipid remodeling pathway, LPC is converted to PC via reacylation by acyl-CoA:lysophosphatidylcholine acyltransferase (LPCAT) in various tissues [63]. The schematic representation of the biosynthesis of LPC is represented in Fig. 1.
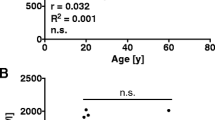
Total LPC concentration, as well as the concentration of the main LPC species, was markedly reduced in sepsis patients compared to controls and the difference in LPC-PC ratio was higher in survivors compared to non- survivors [37].
Cho et al., analyzed LPC concentration in blood samples on the first day after diagnosis of septic patients and compared them with a control group of healthy blood donors. The mean serum LPC concentration was significantly lower than in the healthy controls. No difference in serum LPC concentration was evident between survivors and non- survivors and no correlation was found with severity of the disease [59]. On the other hand a preliminary retrospective investigation of the analyses Ferrario et al. conducted of the plasma of 20 patients with septic shock found that decreases of unsaturated long-chain PC and LPC species were associated to the event at 28-days and 90-days, in combination with clinical variables such as cardiovascular SOFA score (28-day mortality model) or renal replacement therapy (90-day mortality model) [64].
In another study, authors evaluated serum LPC concentrations in patients in an emergency department with community-acquired pneumonia and correlated them to scores of clinical prediction indicators (pneumonia severity index (PSI) and CURB-65 score) and the concentration of procalcitonin. Samples of days 1 and 7 were analyzed. The mean LPC concentrations on days 1 and 7 were significantly lower in the non-survivors. Day 1 LPC concentrations were inversely correlated with the PSI and CURB- 65 scores. Day 1 LPC cut-off levels< 29.6 μmol/L were associated with the need for mechanical ventilation, vasopressors, intensive care unit admission, and hospital mortality [65]. Arshad et al. measured 105 phospholipids, 40 acylcarnitines, and 4 ceramides, as well as acid sphingomyelinase activity, in plasma from patients with community-acquired pneumonia, chronic obstructive pulmonary disease (COPD) exacerbation with infection and a control group, and found that Phospholipid concentrations were greatly decreased in community-acquired pneumonia and normalized in the course of clinical improvement. They also observed that changes in COPD were less pronounced, but also differed qualitatively [66].
The relation between serial LPC measurements with 28-day mortality was analyzed in a tertiary ICU in patients with sepsis and septic shock. Serum LPC, white blood cell, C-reactive protein and procalcitonin levels were measured at baseline (day 1 of admission) and day 7. The LPC concentration on day 7 was significantly lower in non-survivors compared to survivors and a decreased LPC concentration on day 7 and a sustained high concentration of procalcitonin on day 7 were useful for predicting the 28-day mortality. LPC concentrations increased over time in patients with appropriate antibiotics, but not in those with inappropriate antibiotics [67].
Other lipids have also been pointed out as possible sepsis markers. Ahn et al. evaluated alteration of the lipid profile of mice with sepsis induced by cecal bacterial peritonitis after ligature by cecal puncture. They observed that among 147 lipid species in the plasma, 13 subgroups (FA, LPA, LPC, LPE, PA, PC, PE, PI, MG, DG, TG, SM and Cer) had alterations in sepsis. The group also evaluated the response to administration of LPC and LPA with altered lipid profile in response [68].
Schmerler et al. demonstrate that acylcarnitines and glycerophosphatidylcholines may be helpful for differentiating infectious from non-infectious systemic inflammation due to their significantly higher concentration in sepsis patients [69]. Three lipids (PC(17:0/0:0, PE(P-19:1(12Z)/0:0), PE(22:2(13Z,16Z)/15:0),)) were selected to form a biomarker group to improve risk discrimination between the sepsis-induced lung injury patients and healthy cases [70].
Additional study design details in humans are listed in Table 1.
Conclusion
In concluding this review, we can say that altered lipid profiles, along with the progress of diseases, should provide new insights that will enable a better understanding of the physiopathology of sepsis, contributing new possibilities for effective diagnoses and therapies. The current review deals with the lipid molecules that are up-regulated or down-regulated during the early stages of sepsis, as shown in the data presented in the present review and in earlier work of our research group [39]. Based on those aspects, we suggest that replenishing the protective molecules that are down-regulated in sepsis while withdrawing the elevated deleterious factors may lead to the discovery of new therapies for improving survival in septic patients; a goal that has been elusive for decades. In view of the complexity of the sepsis response, it is unlikely that a single ideal biomarker will ever be found. A combination of several sepsis biomarkers may be more effective, but that requires further evaluation.
Availability of data and materials
Not applicable.
Abbreviations
- 11-HETE:
-
11-hydroxy-5,8,12,14-eicosatetraenoic acid
- AA:
-
Arachidonic acid
- Apo:
-
Apolipoprotein
- CAT:
-
Catalase
- Cer:
-
Ceramide
- COX:
-
Cyclooxygenase
- CRP:
-
C-reactive protein
- DG:
-
Diacylglyceride
- DHA:
-
Docosahexaenoic acid
- FA:
-
Fatty acid
- HDL:
-
High-density lipoprotein
- IL:
-
Interleukin
- IP-10:
-
Interferon gamma-induced protein 10
- LDL:
-
Low-density lipoprotein
- LPA:
-
Lysophosphate
- LPC:
-
Lysophosphatidylcholine
- LPE:
-
Lysophosphatidylethanolamine
- PCT:
-
Procalcitonin
- PGE2:
-
Prostaglandin E2
- LOX:
-
Lipoxygenase
- LPS:
-
Lipopolysaccharide
- LT:
-
Leukotriene
- MG:
-
Monoacylglyceride
- PA:
-
Phosphatidic acid
- PC:
-
Phosphatidylcholine
- PE:
-
Phosphatidiylethanolamine
- PI:
-
Phosphatidylinositol
- PLA2-II:
-
Phospholipase A2
- PSI:
-
Pneumonia severity index
- PUFA:
-
Polyunsaturated fatty acids
- ROS:
-
Reactive oxygen species
- S1P:
-
Sphingosine-1 phosphate
- SM:
-
Sphingomyelin
- Snp-PLA2:
-
Phospholipase A2 type II
- Strem-1:
-
Soluble triggering receptor expressed on myeloid cells-1
- SOD:
-
Superoxide dismutase
- TG:
-
Triacylglyceride
- TLR:
-
Toll-like receptors
- TNF-alfa:
-
Tumor necrosis factor alfa
- TXB2:
-
Thromboxane B2
- VLDL:
-
Very low-density lipoprotein
References
Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–54.
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–10.
Rhodes A, Evans LA, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis campaign: international guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304–77.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche J-D, et al. The third international consensus definitions for Sepsis and septic shock (Sepsis-3). Jama. 2016;315(8):801–10.
Winters BD, Eberlein M, Leung J, Needham DM, Pronovost PJ, Sevransky JE. Long-term mortality and quality of life in sepsis: a systematic review. Crit Care Med. 2010;38(5):1276–83.
Long B, Koyfman A. Ready for prime time? Biomarkers in Sepsis. 2017;35:109–22.
Clerico A, Plebani M. Biomarkers for sepsis: an unfinished journey. Clin Chem Lab Med. 2013;51(6):1135–8.
Marshall JC, Reinhart K. Biomarkers of sepsis. Crit Care Med. 2009;37(7):2290–8.
Pierrakos C, Vincent J-L. Sepsis biomarkers: a review. Crit Care. 2010;14(1):R15.
Russell JA, Spronk P, Walley KR. Using multiple ‘omics strategies for novel therapies in sepsis. Intensive Care Med. 2018;44(4):509–11.
Fleischmann C, Scherag A, Adhikari NKJ, Hartog CS, Tsaganos T, Schlattmann P, et al. Assessment of global incidence and mortality of hospital-treated sepsis current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–72.
Yébenes JC, Ruiz-Rodriguez JC, Ferrer R, Clèries M, Bosch A, Lorencio C, Rodriguez A, Nuvials X, Martin-Loeches I, Artigas A, SOCMIC (Catalonian Critical Care Society) Sepsis Working Group. Epidemiology of sepsis in Catalonia: analysis of incidence and outcomes in a European setting. Ann. Intensive Care. 2017;7(1):19.
Hotchkiss RS, Karl IE. The pathophysiology and treatment of Sepsis. N Engl J Med. 2003;348(2):138–50.
Brown MA, Jones WK. NF-kappaB action in sepsis: the innate immune system and the heart. Front Biosci A J Virtual Libr. 2004;9:1201–17.
Cohen J. The immunopathogenesis of sepsis. Nature. 2002;420(6917):885–91.
Kumar S, Gupta E, Kaushik S, Kumar Srivastava V, Mehta SK, Jyoti A. Evaluation of oxidative stress and antioxidant status: correlation with the severity of sepsis. Scand J Immunol. 2018;87(4):e12653.
Kumar A. Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum. J Exp Med. 1996;183(3):949–58.
Russell JA. Management of sepsis. N Engl J Med. 2006;355(16):1699–713.
Abraham E, Singer M. Mechanisms of sepsis-induced organ dysfunction. Crit Care Med. 2007;35(10):2408–16.
Englert JA, Rogers AJ. Metabolism, metabolomics, and nutritional support of patients with Sepsis. Clin Chest Med. 2016;37(2):321–31.
Mitra S, Abraham E. Participation of superoxide in neutrophil activation and cytokine production. Biochim Biophys Acta. 2006;1762(8):732–41.
Barichello T, Fortunato JJ, Vitali ÂM, Feier G, Reinke A, Moreira JCF, Quevedo J, Dal-Pizzol F. Oxidative variables in the rat brain after sepsis induced by cecal ligation and perforation. Crit Care Med. 2006;34(3):886–9.
Mesotten D, Swinnen JV, Vanderhoydonc F, Wouters PJ, Van Den Berghe G. Contribution of circulating lipids to the improved outcome of critical illness by glycemic control with intensive insulin therapy. J Clin Endocrinol Metab. 2004;89(1):219–26.
Wendel M, Paul R, Heller AR. Lipoproteins in inflammation and sepsis. II Clinical aspects Intensive Care Med. 2007;33(1):25–35.
Levels JHM, Lemaire LCJM, van den Ende AE, van Deventer SJH, van Lanschot JJB. Lipid composition and lipopolysaccharide binding capacity of lipoproteins in plasma and lymph of patients with systemic inflammatory response syndrome and multiple organ failure. Crit Care Med. 2003;31(6):1647–53.
Tanaka S, Labreuche J, Drumez E, Harrois A, Hamada S, Vigué B, Couret D, Duranteau J, Meilhac O. Low HDL levels in sepsis versus trauma patients in intensive care unit. Ann Intensive Care. 2017;7(1):4–11.
Malle E, de Beer FC. Human serum amyloid a (SAA) protein: a prominent acute-phase reactant for clinical practice. Eur J Clin Investig. 1996;26(6):427–35.
Van Leeuwen HJ, Heezius ECJM, Dallinga GM, Van JAG, Verhoef J, Van KPM. Lipoprotein metabolism in patients with severe sepsis. Crit Care Med. 2003;31(5):1359–66.
Green P, Theilla M, Singer P. Lipid metabolism in critical illness. Curr Opin Clin Nutr Metab Care. 2016;19(2):111–5.
Abraham E. Why immunomodulatory therapies have not worked in sepsis. Intensive Care Med. 1999;25(6):556–66.
Chaby R. Lipopolysaccharide-binding molecules: transporters, blockers and sensors. Cell Mol Life Sci. 2004;61(14):1697–713.
Triantafilou M, Mouratis MA, Lepper PM, Haston RM, Baldwin F, Lowes S, Elrahman Ahmed MA, Schumann C, Boyd O, Triantafilou K. Serum proteins modulate lipopolysaccharide and lipoteichoic acid-induced activation and contribute to the clinical outcome of sepsis. Virulence. 2012;3(2):136–45.
Feingold KR, Staprans I, Memom R, Moser H, Shigenaga JK, Doerrler W, Dinarello C, Grunfeld C. Endotoxin rapidly induces changes in lipid metabolism that produce hypertriglyceridemia: low doses stimulate hepatic triglyceride production while high doses inhibit clearance. J Lipid Res. 1992;33:1765–76.
Fraunberger P, Schaefer S, Werdan K, Walli AK, Seidel D. Reduction of circulating cholesterol and apolipoprotein levels during sepsis. Clin Chem Lab Med. 1999;37(3):357–62.
Rival T, Cinq-Frais C, Silva-Sinfontes S, Garcia J, Riu B, Salvayre R, Genestal M, Caspar-Bauguil S. Alteration of plasma phospholipid fatty acid profile in patients with septic shock. Biochimie. 2013;95(11):2177–81.
Serhan CN, Gotlinger K, Hong S, Arita M. Resolvins, docosatrienes, and neuroprotectins, novel omega-3-derived mediators, and their aspirin-triggered endogenous epimers: an overview of their protective roles in catabasis. Prostaglandins and Other Lipid Mediators. 2004;73(3–4):155–72.
Drobnik W, Liebisch G, Audevert F-X, Frohlich D, Gluck T, Vogel P, Rothe G, Schmitz G. Plasma ceramide and lysophosphatidylcholine inversely correlate with mortality in sepsis patients. J Lipid Res. 2003;44(4):754–61.
Barros KV, Paula A, Schalch L, Della E, Munhoz V, Antonio J, Noakes PS, Miles EA, Calder PC, Flor VL. Supplemental intravenous n-3 fatty acids and n-3 fatty acid status and outcome in critically ill elderly patients in the ICU receiving enteral nutrition. Clin Nutr. 2013;32(4):599–605.
Mecatti GC, Messias MCF, Sant’Anna Paiola R, Angolini CFF, Cunha IBS, Eberlin MN, Carvalho PO. Lipidomic profiling of plasma and erythrocytes from septic patients reveals potential biomarker candidates. Biomark Insights. 2018. https://doi.org/10.1177/1177271918765137.
Bruegel M, Ludwig U, Kleinhempel A, Petros S, Kortz L, Ceglarek U, Holdt LM, Thiery J, Fielder GM. Sepsis-associated changes of the arachidonic acid metabolism and their diagnostic potential in septic patients. Crit Care Med. 2012;40(5):1478–86.
Kamisoglu K, Sleight KE, Calvano SE, Coyle SM, Corbett SA, Androulakis IP. Temporal metabolic profiling of plasma during endotoxemia in humans. Shock. 2013;40(6):519–26.
Ferrario M, Brunelli L, Su F, Herpain A, Pastorelli R. The systemic alterations of lipids, alanine-glucose cycle and inter-organ amino acid metabolism in swine model confirms the role of liver in early phase of septic shock. Front Physiol. 2019;10:11. https://doi.org/10.3389/fphys.2019.00011.
Vadas P, Scott K, Smith G, Rjkovic I, Stefanski E, Schouten BD, Singh R, Pruzanski W. Serum phospholipase A2 enzyme activity and immunoreactivity in a prospective analysis of patients with septic shock. Life Sci. 1992;50(11):807–11.
Dinkla S, van Eijk LT, Fuchs B, Schiller J, Joosten I, Brock R, Pickkers P, et al. Inflammation-associated changes in lipid composition and the organization of the erythrocyte membrane. BBA Clin. 2016;5:186–92.
Guidet B, Piot O, Masliah J, Barakett V, Maury E, Bereziat G, Offnstadt G. Secretory non-pancreatic phopholipase A2 in severe sepsis: relation to endotoxin, cytokines and thromboxane B2. Infection. 1996;24(2):103–8.
Calder PC. Omega-3 fatty acids and inflammatory processes. Nutrients. 2010;2(3):355–74.
Prucha M, Bellingan G, Zazula R. Sepsis biomarkers. Clin Chim Acta. 2015;440:97–103.
Sharma NK, Tashima AK, Brunialti MKC, Ferreira ER, Torquato RJS, Mortara RA, Machado FR, Assuncao M, Rigato O, Salomao R. Proteomic study revealed cellular assembly and lipid metabolism dysregulation in sepsis secondary to community-acquired pneumonia. Sci Rep. 2017;7(1):1–13.
Schuetz P, Aujesky D, Mueller C, Mueller B. Biomarker-guided personalised emergency medicine for all - Hope for another hype? Swiss Med Wkly. 2015;145. https://doi.org/10.4414/smw.2015.14079.
Silva BN, Andriolo RB, Salomão R, Atallah ÁN. Effectiveness and safety of procalcitonin evaluation for reducing mortality in adult patients with sepsis, severe sepsis and septic shock. Cochrane Database Syst Rev. 2014;1. https://doi.org/10.1002/14651858.CD010959.pub2.
Liu Y, Hou J, Li Q, Chen K, Wang S-N, Wang J. Biomarkers for diagnosis of sepsis in patients with systemic inflammatory response syndrome: a systematic review and meta-analysis. Springerplus. 2016;5(1):2091.
Clyne B, Olshaker JS. The C-reactive protein. J Emerg Med. 1999;17(0736–4679):1019–25.
BalcI C, Sungurtekin H, Gürses E, Sungurtekin U, Kaptanoglu B. Usefulness of procalcitonin for diagnosis of sepsis in the intensive care unit. Crit Care. 2003;7(1):85–90.
Giamarellos-Bourboulis EJ, Giannopoulou P, Grecka P, Voros D, Mandragos K, Giamarellou H. Should procalcitonin be introduced in the diagnostic criteria for the systemic inflammatory response syndrome and sepsis? J Crit Care. 2004;19(3):152–7.
Wang K, Xie S, Xiao K, Yan P, He W, Xie L. Biomarkers of sepsis-induced acute kidney injury. Biomed Res Int. 2018. https://doi.org/10.1155/2018/6937947.
Zhao YY, Miao H, Cheng XL, Wei F. Lipidomics: novel insight into the biochemical mechanism of lipid metabolism and dysregulation-associated disease. Chem Biol Interact. 2015;240:220–38.
Cajka T, Fiehn O. Toward merging untargeted and targeted methods in mass spectrometry-based metabolomics and Lipidomics. Anal Chem. 2016;88(1):524–45.
Zhao YY, Wu SP, Liu S, Zhang Y, Lin RC. Ultra-performance liquid chromatography-mass spectrometry as a sensitive and powerful technology in lipidomic applications. Chem Biol Interact. 2014;220:181–92.
Cho WH, Park T, Park YY, Huh JW, Lim CM, Koh Y, Song DK, Hong SB. Clinical significance of enzymatic lysophosphatidylcholine (LPC) assay data in patients with sepsis. Eur J Clin Microbiol Infect Dis. 2012;31(8):1805–10.
Lee SH, Park MS, Park BH, Jung WJ, Lee IS, Kim SY, Kim EY, Jung JY, Kang YA, Ys K, Chang J, Chung KS. Prognostic implications of serum lipid metabolism over time during sepsis. Biomed Res Int. 2015. https://doi.org/10.1155/2015/789298.
Park JM, Noh JY, Kim MJ, Yun TG, Lee SG, Chung KS, Lee EH, Shin MH, Ku NS, Yoon S, Kang MJ, Park MS, Pyun JC. MALDI-TOF Mass Spectrometry Based on Parylene-Matrix Chip for the Analysis of Lysophosphatidylcholine in Sepsis Patient Sera. Anal Chem. 2019;91(22):14719–27.
Eder AM, Sasagawa T, Mao M, Aoki J, Mills GB. Constitutive and Lysophosphatidic acid ( LPA ) -induced LPA production : role of phospholipase D and phospholipase a 2. Clin Cancer Res. 2000;6:2482–91.
Sevastou I, Kaffe E, Mouratis M-A, Aidinis V. Lysoglycerophospholipids in chronic inflammatory disorders: the PLA(2)/LPC and ATX/LPA axes. Biochim Biophys Acta. 2013;1831(1):42–60.
Ferrario M, Cambiaghi A, Brunelli L, Giordano S, Caironi P, Guatteri L, Raimondi F, Gattinoni L, Latini R, Masson S, Ristagno G, Pastorelli R. Mortality prediction in patients with severe septic shock: a pilot study using a target metabolomics approach. Nat Publ. 2016. https://doi.org/10.1038/srep20391.
Cho WH, Yeo HJ, Yoon SH, Lee SE, Jeon DS, Kim YS, Lee SJ, Jo EJ, Mok LH, Kim MH, Kim KU, Lee K, Park HK, Lee MK. Lysophosphatidylcholine as a prognostic marker in community-acquired pneumonia requiring hospitalization: a pilot study. Eur J Clin Microbiol Infect Dis. 2014;34(2):309–15.
Arshad H, Alfonso JCL, Franke R, Michaelis K, Araújo L, Habid A, Zboromyrska Y, Lucke E, Strungaru E, Akmatov MK, et al. Decreased plasma phospholipid concentrations and increased acid sphingomyelinase activity are accurate biomarkers for community-acquired pneumonia. J Transl Med. 2019;17(1):365.
Park DW, Kwad DS, Park YY, Chang Y, Huh JW, Lim CM, Koh Y, Song DK, Hong SB. Impact of serial measurements of lysophosphatidylcholine on 28-day mortality prediction in patients admitted to the intensive care unit with severe sepsis or septic shock. J Crit Care. 2014;29(5):882.
Ahn W, Jung J, Song D. Lipidomic analysis of plasma lipids composition changes in septic mice. Korean J Physiol Pharmacol. 2018;22(4):399–408.
Schmerler D, Neugebauer S, Ludewig K, Bremer-Streck S, Brunkhorst FM, Kiehntopf M. Targeted metabolomics for discrimination of systemic inflammatory disorders in critically ill patients. J Lipid Res. 2012;53(7):1369–75.
Liang Q, Liu H, Jiang Y, Xing H, Zhang T, Zhang AH. Discovering lipid phenotypic changes of sepsis-induced lung injury using high-throughput lipidomic analysis. RSC Adv. 2016;6(44):38233–7.
Acknowledgments
Not applicable.
Consent to publication
Not applicable.
Author information
Authors and Affiliations
Contributions
GCM, MCFM, POC contributed to the study concept and design, GCM and POC performed in the acquisition and tabulation of data, and drafted the manuscript. All authors read and approved the final manuscript.
Author’s information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mecatti, G.C., Messias, M.C.F. & de Oliveira Carvalho, P. Lipidomic profile and candidate biomarkers in septic patients. Lipids Health Dis 19, 68 (2020). https://doi.org/10.1186/s12944-020-01246-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-020-01246-2