Abstract
Background
Persons with disabilities experience health inequities in terms of increased mortality, morbidity, and limitations in functioning when compared to the rest of the population. Many of the poor health outcomes experienced by persons with disabilities cannot be explained by the underlying health condition or impairment, but are health inequities driven by unfair societal and health system factors. A synthesis of the global evidence is needed to identify the factors that hinder equitable access to healthcare services for persons with disabilities, and the interventions to remove these barriers and promote disability inclusion.
Methods
We conducted a scoping review following the methodological framework proposed by Arksey and O’Malley, Int J Soc Res Methodol 8:19–32. We searched two scholarly databases, namely MEDLINE (Ovid) and Web of Science, the websites of Organizations of Persons with Disabilities and governments, and reviewed evidence shared during WHO-led consultations on the topic of health equity for persons with disabilities. We included articles published after 2011 with no restriction to geographical location, the type of underlying impairments or healthcare services. A charting form was developed and used to extract the relevant information for each included article.
Results
Of 11,884 articles identified in the search, we included 182 articles in this review. The majority of sources originated from high-income countries. Barriers were identified worldwide across different levels of the health system (such as healthcare costs, untrained healthcare workforces, issues of inclusive and coordinated services delivery), and through wider contributing factors of health inequities that expand beyond the health system (such as societal stigma or health literacy). However, the interventions to promote equitable access to healthcare services for persons with disabilities were not readily mapped onto those needs, their sources of funding and projected sustainability were often unclear, and few offered targeted approaches to address issues faced by marginalized groups of persons with disabilities with intersectional identities.
Conclusion
Persons with disabilities continue to face considerable barriers when accessing healthcare services, which negatively affects their chances of achieving their highest attainable standard of health. It is encouraging to note the increasing evidence on interventions targeting equitable access to healthcare services, but they remain too few and sparce to meet the populations’ needs. Profound systemic changes and action-oriented strategies are warranted to promote health equity for persons with disabilities, and advance global health priorities.
Similar content being viewed by others
Background
The World Health Organization estimates that approximately 1.3 billion people today have significant disability [1]. Persons with disabilities experience worse health outcomes when compared to the rest of the population in terms of premature mortality, increased morbidity, and limitations in functioning [1,2,3]. For instance, persons with disabilities are more likely to die at a younger age than the rest of the population [4,5,6,7], have a higher incidence of communicable diseases and chronic health conditions [8,9,10,11], and limitations to functioning [12,13,14]. COVID-19 further highlighted these disparities in health outcomes: during the pandemic people with disabilities were more likely to get infected by COVID-19 and, when infected, had an increased risk of severe illness and mortality compared to persons without disabilities [15,16,17].
Many of the poor health outcomes experienced by persons with disabilities cannot be explained by the underlying health condition or impairment, but are health inequities driven by unfair societal and health system factors (1). The population-wide structural and social determinants of health that generate, sustain and even widen health inequities are well-documented [18,19,20], and disproportionately impact persons with disabilities (2). For instance, persons with disabilities are significantly more likely to live in poverty [21], under precarious housing conditions [22], and have lower levels of education [23] and employment [24] than their non-disabled counterparts. The accumulation of these mutually-reinforcing determinants of health not only amplifies the health and social disadvantage experienced by persons with disabilities, but is further compounded by additional factors that are uniquely associated with disability, such as ableism [25]. Importantly, the health inequities experienced by persons with disabilities are also associated with poor access to quality healthcare. For example, a study conducted in England and Wales demonstrated that avoidable deaths from causes amenable to good quality healthcare are more common in people with intellectual disabilities (37%) than in the general population (13%) [26].
In order to address health inequities, we need to better understand the underlying factors that lead to them, and particularly those related to access to healthcare services [3, 27, 28]. Many published reviews have already synthesized the barriers of access to healthcare services for persons with disabilities, highlighting a wide range of issues such as physical inaccessibility of health facilities [29, 30], unaffordable healthcare [31], untrained healthcare workforce [32, 33], and negative attitudes of healthcare workers [34]. However, these reviews are often restricted to specific healthcare services, countries or demographics. Importantly, no published review investigated these barriers alongside the interventions to remove them and promote disability inclusion in these services, which limits the identification of solutions to promote health equity for persons with disabilities worldwide.
The present scoping review is the first to provide a comprehensive global overview of access to healthcare services for persons with disabilities as characterized by both (1) the barriers that persons with disabilities face when accessing healthcare services, and (2) the interventions that have been implemented to remove these barriers and promote equitable access to healthcare for this population. By mapping this evidence according to different components of the health system [35] and other contributing factors to health inequities, we aim to provide insights to inform the actions that governments and other key stakeholders can take to advance health equity for persons with disabilities [19, 28], and respond more efficiently to the requirements of the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD) [36].
Methods
We conducted a scoping review to identify the existing evidence on the barriers that persons with disabilities face when accessing healthcare services and the interventions to remove them and promote disability inclusion. The scoping review approach was adopted for its use for ‘reconnaissance’ to explore a large, complex, and heterogenous topic [37]. We followed the scoping review methodological framework provided by Arksey & O’Malley [38], which stipulates five steps: (1) Identifying the research questions; (2) Identifying relevant studies; (3) Study selection; (4) Charting the data; (5) Collating, summarizing, and reporting the results. We conducted this review in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews guidelines [39] (see Additional file 1) and the ‘Guidance for conducting systematic scoping reviews’ [37].
Identifying the research questions
In this scoping review, we aimed to address two research questions: (1) What are the barriers of access to healthcare services experienced by persons with disabilities worldwide?, and (2) Which interventions have been implemented to remove these barriers and promote disability inclusion in healthcare services?
Identifying relevant studies
Search strategy
Our search strategy was designed to investigate evidence from multiple and complementary sources. We searched two scientific databases, MEDLINE (Ovid) and Web of Science, which represent the highest scoring database combination accessible to the team after considerations of access and capacity constraints [40]. The search strategy was framed around the combination of three key concepts: (1) Accessibility, (2) Persons with disabilities; and (3) Healthcare services. We developed a list of key words for each concept using MeSH (Medical Subject Headings; National Library of Medicine) and other reviews on similar topics. We used Boolean, truncation, and proximity operators to construct and combine searches, and implemented adjustments as required to account for the specific functionalities of each database. The MEDLINE (Ovid) search strategy, which was run on October 13th, 2021, is provided in Additional file 2.
Additionally, we searched for evidence in websites of relevant organizations and governments using Google Search engine. We reviewed the websites of the two main global umbrella networks of Organizations of Persons with Disabilities and service providers, namely International Disability Alliance (IDA) [41] and International Disability and Development Consortium (IDDC) [42]. Since IDA and IDDC encompass a large number of local and regional organizations, we believe that this allowed us to get sufficient outreach. We also searched the Disability Evidence Portal [43]. Finally, we complemented these initial searches with a snowballing approach to review the websites of organizations mentioned in the webpages that we reviewed and included relevant information on the topic of health for persons with disabilities.
We also reviewed articles recommended by experts during consultations held by the World Health Organization for the development of the Global report on health equity for persons with disabilities [1]. Since all co-authors were involved in the planning of these consultations, and given their relevance to the objectives of the present scoping review, this provided us with a unique opportunity to identify further articles recommended by a range of stakeholders. These consultations were attended by over 1,250 experts worldwide, including persons with disabilities, representatives of Organizations for Persons with Disabilities, United Nations agencies, academics, services providers, and other experts. More details about these consultations are provided in Annex 2 of the Global report [1].
Selection criteria
We included publications from the last 11 years (2011–2022), with the meaningful threshold of 2011 being chosen due to the publication of the World Report on Disability [2] which attracted global attention to the inequities experienced by persons with disabilities. We included various publication types to capture the voices of different stakeholders and identify key themes and trends in the field of disability (qualitative, quantitative, and mixed-method peer-reviewed journal articles; systematic and scoping reviews; and reports produced by civil society organizations and governments). However, we excluded other publication types such as clinical guidelines, research protocols, commentaries, editorial comments, book chapters, conference abstracts and presentations. We included publications from any country and published in any language accessible to the research team (English, French, Italian, and Spanish). Publications were eligible if they documented the perceived or measured barriers of access to health services, and/or interventions addressing equitable access to healthcare services for persons with disabilities. We did not apply restrictions to types of underlying impairments or health services. The same selection criteria were applied for articles identified from the scientific databases, grey literature and consultations.
Study selection
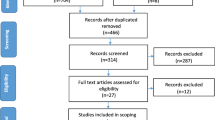
We run the search in the two scientific databases and deduplicated the articles. A single reviewer (MG) screened all titles and abstracts (n = 9,440). A second reviewer (MFM) screened a 10% random sample to determine inter-rater reliability (n = 944). A kappa score of K = 0.727 was reached, indicating substantial agreement [44]. Conflicts were resolved through discussion between three reviewers: MG, MFM, and KK. Then, the reviewers identified publications eligible for full-text review, categorizing them according to the main aim of the paper as being primarily relevant to RQ1 (barriers) or RQ2 (interventions). We used a 20% random sample of both sets of articles, weighed according to publication year, to ensure a balanced representation of studies addressing both research questions. This sampling strategy was adopted to better engage with a smaller selection of this large dataset, and completed according to considerations of content saturation. MG and MFM retrieved all articles included through this sampling strategy for full-text review. For the grey literature search, MG, MFM and AMR were assigned different sources, recorded each URL that was monitored on an Excel document with a mention ‘to be included’ or ‘to be excluded’ following assessment to the selection criteria. The additional articles suggested during the WHO-led consultations were recorded in another Excel document, and following the same selection process. The extraction of references and deduplication was conducted on the reference manager software EndNote 20.4, and screening was conducted on Rayyan [45].
Charting the data
The research team developed a data charting form for this review. The following characteristics were extracted for each included article on barriers and interventions: author(s), year of publication, study contexts (defined by country, WHO regionFootnote 1 [46], and level of income), methodology, study population, intersectionality,Footnote 2 type of healthcare service or intervention, and main outcomes. In cases where articles referred to both barriers and interventions, this was recorded as additional remarks and the data was extracted to inform both lines of enquiry. References were allocated a unique reference number.
Collating, summarizing, and reporting the results
We synthesized the barriers and interventions of access to healthcare services for persons with disabilities according to the key components of the health system [35]: (1) health and care workforce; (2) health information systems; (3) health systems financing; (4) leadership and governance; (5) service delivery; and (6) essential medicines and equipment. We used this framework because it is widely adopted in global health strategic planning. Therefore, mapping our findings to this framework can support the identification and integration of solutions to advance disability inclusion in existing universal health coverage plans. Additionally, we considered the following components that are extrinsic to the health system but nonetheless critical to healthcare access: structural barriers, social determinants of health, and risk factors related to ill-health (such as tobacco and alcohol use, or physical inactivity). We did not undertake a quality appraisal of the included papers as this is not recommended practice for scoping review designs which aim to provide an overview of the field rather than assess its evidence [38].
Results
Overview
Of 11,858 articles identified in the database search, we identified 736 and 754 articles at the title/abstract screening stage to primarily address RQ1 (barriers) and RQ2 (interventions), respectively. Following the 20% random sampling strategy in both sets of articles and full-text screening, we identified 77 and 79 articles to address RQ1 and RQ2 respectively. This indicated an inclusion rate of 52.0% and 52.3% of the samples retrieved after title-abstract screening. We included another six articles for RQ1 and 20 for RQ2 through consultations and grey literature search. In total, we included 182 articles in this review (Fig. 1). All articles were accessible in English, except for one paper written in French [49].
Barriers
The 83 included articles on the barriers of access comprised 77 articles from the database search and 6 from other sources. All 77 included articles from the database search were originally categorized for barriers (RQ1). From the articles categorized as primarily addressing RQ2 (interventions), most authors also mentioned the barriers of access to healthcare for persons with disabilities that they aimed to address (RQ1) but no novel barriers were identified that had not already been captured in the articles categorised as primarily addressing RQ1. These articles reported largely on the Americas (28.9%), European and Western Pacific regions (19.3% each), while the least represented region was Eastern Mediterranean (3.6%). Many articles were set in high-income countries (66.3%) and few in low-income countries (3.6%). About a third of the papers investigated access to general healthcare or primary care services (32.5%) while the rest focused on more targeted services. Qualitative research designs were used in half of these papers (50.6%), followed by mixed methods (25.3%), quantitative (15.7%), and review methods (8.4%). Most articles included persons with mixed types of disabilities (33.7%), followed by psychosocial disabilities (25.3%), physical (16.9%), intellectual (14.5%), and sensory disabilities (9.6%). Finally, almost half of the papers provided information about specific groups of persons with disabilities at risk of further marginalization (54.2%), with a stronger focus on women (19.3%) or children with disabilities (13.3%), but older persons (2.4%), migrants (1.2%) or persons with disabilities living in rural areas (3.6%) were less represented. Table 1 (in Additional file 3) details the characteristics of the included papers on barriers, and Fig. 2 shows the frequency of these articles based on publication year.
Interventions
The 99 included papers on the interventions comprised 79 articles from the database search and 20 from other sources. No new intervention was found in the sample of papers categorized as primarily addressing RQ1 (barriers). Similar to the articles on barriers, most articles were situated in the Americas (39.4%), Western Pacific (18.2%), and European regions (15.2%). The African (6.1%), South-East Asian (3.0%), and East-Mediterranean regions (1%) were scarcely represented. The articles reported largely on high-income countries (62.6%) and showed low representation of low-income countries (2.0%). Most articles focused on interventions for persons with psychosocial (61.6%) or mixed disabilities (20.2%), while interventions targeting persons with sensory (8.1%), intellectual (7.1%), or physical disabilities (3.0%) were few. Specific groups of persons with disabilities at risk of further marginalization were a consideration for 25.3% of papers and most particularly for children with disabilities (15.2%), but less so for women with disabilities (6.1%), those with minoritized ethnic backgrounds (2.0%), older persons or persons with disabilities living in rural areas (1.0% each). Most intervention types related to training and education (38.8%), and care coordination (28.3%). Table 2 (in Additional file 3) details the characteristics of the included papers on interventions, and Fig. 2 shows the frequency of these articles based on publication year.
Health system-related barriers and interventions
Health and care workforce
The evidence on healthcare workforce-related barriers was evenly distributed across all types of disability, and particularly well-documented for women (22.7%) and children with disabilities (18.2%) in rehabilitation services (22.7%) and maternal care (15·2%). The majority of included papers (79.5%) exposed the limited human resources, lack of training and skills, and negative attitudes of the health and care workforce that hindered access to healthcare services for persons with disabilities. Many articles showed that limited staff [50,51,52,53,54,55,56,57,58,59] and high staff turnover [60,61,62] were widespread problems that disadvantaged persons with disabilities who often needed longer or more frequent sessions so that their health needs could be met [54, 59]. Even when available, healthcare workers often lacked the knowledge, skills, experience, and confidence to care for persons with disabilities, including on providing reasonable accommodations [31, 49, 50, 52, 54,55,56, 58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96]. A large number of articles referred to issues of discriminatory attitudes and behaviours by healthcare workers towards persons with disabilities across all healthcare services, regions, and levels of income [31, 51, 53, 55, 57, 58, 61,62,63, 65, 66, 68, 70,71,72,73,74, 76,77,78,79, 81,82,83,84, 87, 88, 94, 95, 97,98,99,100,101,102,103,104,105,106]. This was illustrated by healthcare workers’ refusal to provide care for persons with disabilities or to adopt reasonable accommodations [31, 98, 106], negative assumptions around the capacity of persons with disabilities to engage in their own care [62, 70, 71, 73, 76, 94, 104, 105], or disrespect for persons with disabilities’ wishes of care [80]. Additionally, the communication challenges between healthcare workers and persons with disabilities represented critical barriers to equitable healthcare [31, 49,50,51, 55, 59, 68, 69, 71, 73, 74, 78, 82,83,84,85, 87, 90,91,92,93, 97, 99,100,101,102, 104, 107,108,109], which particularly affected persons with cognitive [85], developmental [69], or communication disabilities [51, 59].
All 19 included interventions targeting the healthcare workforce focused on the training and education of healthcare workers. These interventions largely focused on building the capacity of the healthcare workforce to care for persons with psychosocial disabilities (63.2%) and children with disabilities (15.8%), but only three were scaled up nationally (15.8%). Education programmes aimed to improve healthcare professionals’ knowledge on disability issues [110,111,112,113,114,115,116,117], inclusive communication skills [118], or to address negative attitudes [110, 111, 119,120,121,122,123]. Most interventions increased healthcare professionals’ knowledge and skills, but rigorous assessment of their application and impact in practice was often missing. Furthermore, most of these interventions were focused on the care for persons with psychosocial disabilities, which indicated gaps in healthcare workforce training for other groups of persons with disabilities with different needs. Importantly, only a few interventions incorporated a human rights-based approach to the care of persons with disabilities [111, 124] and the involvement of persons with disabilities, in line with the UNCRPD [117].
Health information systems
Few articles shed light on the barriers and interventions around the health information systems (33.7%), and largely focused on issues of care coordination. The lack of reliable disability data in healthcare services [66] and the lack of a system to record the reasonable adjustments to care for persons with disabilities [67] were reported. Care coordination was often limited due to poor referral systems [49, 52, 68] and inefficient exchange of information between healthcare providers, which would cause delays in the provision of care [61, 68, 69, 125, 126]. Most evidence documented how this issue affected children with disabilities (25.0%) and persons with psychosocial disabilities (28.6%) in general healthcare services (53.6%), but the impact on other groups and services remained largely unknown.
Only two interventions were identified on health information systems, and only one was scaled up at the regional level. Both were set in high-income countries (USA [127] and Canada [128]) and highlighted the potential of digital solutions, such as electronic patient records, to improve healthcare for persons with psychosocial or mixed disabilities.
Health systems financing
Many included articles covered the financial barriers of healthcare access for persons with disabilities (61.4%), with these barriers being disproportionately reported in low- and middle-income countries. While less than half of the articles from high income countries reported these financial issues (48.3%), almost all articles from low- and middle-income countries did (92%). The evidence focused particularly on how these barriers affected persons with psychosocial disabilities (31.4%), women (19.6%) and children with disabilities (17.6%) as they accessed general healthcare services (31.4%) and rehabilitation services (25.5%). The healthcare costs [31, 49, 50, 52, 56, 58, 60, 61, 63, 64, 76, 83, 86, 89, 91, 95, 97,98,99,100, 102, 103, 129,130,131,132,133,134,135,136,137,138], the lack or limited coverage by health insurance [31, 57, 58, 72, 82, 88, 105, 139, 140], and out-of-pocket payments [56, 57, 72, 78, 82, 131, 134, 140] often prevented persons with disabilities from accessing timely care [98, 134, 135, 140]. For example, persons with disabilities are from 4·5 to 7·2 times more likely to have unmet need for mental health due to cost [138]. There was a global lack of investment in resources to promote accessibility for persons with disabilities in health systems [49, 52, 53, 57,58,59, 62, 69, 81, 83, 86, 89, 126], such as the lack of investments in accessible equipment [52] or discriminatory decisions surrounding health insurance schemes [81]. Furthermore, persons with disabilities often faced difficulties with the administrative requirements and processes needed to obtain insurance or access disability funding [59, 101, 103, 141].
A total of seven interventions with a primary focus on inclusive health systems financing were identified, including six scaled up at the national level. All were developed in high-income countries from the Americas (USA), European (Germany) and Western Pacific regions (Australia). These interventions aimed to improve health insurance packages, mostly for persons with psychosocial disabilities (57.1%) [142,143,144,145], children with disabilities (28.6%) [146, 147], and all persons with disabilities (28.6%) [148]. However, the evidence on their impact to healthcare access was mixed. Furthermore, targeting specific groups known to be at higher risk of financial hardship, such as for women and older persons with disabilities, or persons with intellectual disabilities, was missing.
Leadership and governance
The barriers associated with this component of the health system received the least evidence globally, with 22.9% articles referring to issues of leadership and governance from countries in various regions and with different income levels. The reported lack of governmental or managerial leadership on disability inclusion highlighted prioritization issues among decision-makers in the health sector [52, 63, 83, 86]. The lack of alignment of policies between services [126] and limited awareness of healthcare workers on such policies and guidelines [53, 58, 68, 83, 89, 92, 101] emphasized implementation issues. The lack of disability guidelines and legislation enforcement [65, 66, 72, 86] and accountability mechanisms for decision-makers in the health sector [67] often led to dependence on other sources of support, such as provided by small NGOs and Organizations of Persons with Disabilities.
Among the eight interventions identified to improve issues of leadership and governance, most related to the implementation and evaluation of disability-inclusive health policies and guidelines in the health sector nationally. Interventions from Israel [149], South Africa [150], Ukraine [151] and the USA [143, 147, 148, 152] were identified, but their impact was difficult to appraise. Most of these interventions did not distinguish persons with disabilities on the basis of other individual factors (62.5%) nor the specific needs of different groups of persons with disabilities (62.5%).
Service delivery
Barriers in service delivery were identified in all types of services, with 89.2% of the included articles reporting on issues of service availability and quality. Groups of persons with disabilities at risk of further marginalization were investigated in over half of these papers, with a strong focus on the barriers experienced by women with disabilities (23.0%). Most of the articles documented the barriers found in general healthcare (29.7%), rehabilitation (21.6%), and mental healthcare services (20.3%) for people with mixed (32.4%) and psychosocial disabilities (28.4%). The lack or limited availability of healthcare services [31, 50, 52, 53, 55,56,57,58,59, 63, 72, 94, 97, 98, 101, 102, 106, 126, 129, 131, 137, 138, 140, 141, 153, 154], especially in rural areas [52, 56, 101], often segregated the most marginalized persons with disabilities [31, 50, 56, 63, 72, 98, 101, 131, 138, 154]. The lack of care coordination [57, 59, 61, 78, 79, 86, 103, 125, 126] and service fragmentation [57, 64, 71], particularly as it related to mental and physical care [49, 86, 92] and multisectoral collaboration [69, 73, 86, 92, 129], was evident on the global scene and further disadvantaged persons with disabilities who may present with more complex health needs.
The lack of accessible architectural designs often impeded access for persons with disabilities [55, 61, 63, 66, 70, 72, 76, 77, 82, 88, 95, 100, 102, 107, 125], particularly those with mobility difficulties. This was illustrated by the lack of accessible consultation rooms [61, 72], toilets or washing rooms [55, 61, 63, 70, 95, 102], ramps [95, 102], routes and parking areas [63, 72]. The sensory distractions in busy clinical environments [57, 73] could be particularly challenging for persons with communication [51] and psychosocial difficulties [57, 73]. The time constraints regulating healthcare provision, such as inflexibility of appointment times [61, 76, 82, 92, 155], long waiting to secure medical appointments [50, 69, 129], or short consultation times [49, 107, 125], hindered the opportunities to coordinate or provide timely care with needed accommodations for persons with disabilities [69, 88]. The limited or inconsistent information about health services [53, 56, 57, 63, 71, 72, 76, 78, 80, 89, 93, 94, 101, 103, 125, 134], and inaccessible medium of communication could widen this gap [72, 76, 80]. This was particularly evident in the difficulties to access any or good-quality sign language interpreters [55, 63, 72, 87, 88, 106, 109] and augmentative and alternative communication tools [51]; and negatively impacted the care of persons with sensory [72, 87, 106], cognitive [60], or communication difficulties [51].
A total of 53 interventions targeting disability-inclusive health service delivery were included, including 24.5% scaled up nationally. Most interventions aimed to promote the coordination of health service provision for persons with psychosocial disabilities (67.9%) and children with disabilities (15.1%) [156,157,158,159,160]. Programmes in the USA supporting the integration of physical and mental healthcare [143, 145, 157, 161,162,163] were evaluated, but their effects on healthcare utilization, costs and outcomes were mixed [164]. In the UK, attempts to embed routine health checks for persons with disabilities in primary care showed conflicting results [158, 165]. Beyond the health sector, multisectoral coordination was also considered, such as with non-government organizations [166], traditional and faith-based healers [167,168,169], or the police [170]. The evidence demonstrated that task-sharing approaches [166, 171, 172], mobile service delivery in the community [173], and telehealth [121, 128, 174, 175] could represent promising solutions to improve healthcare service delivery for persons with disabilities.
Essential medicines and equipment
The lack of accessible or specialized medical and rehabilitation equipment, products and devices in healthcare services were frequently mentioned as impactful barriers for persons with disabilities [52, 54, 58, 59, 61,62,63, 66, 70, 72, 76, 77, 81, 88, 94, 95, 98, 102, 129, 131, 140]. This was illustrated by the lack of adjustable examination tables [66, 70, 72, 76, 88, 94, 95, 140] or chairs [61], lifts or transfer devices [72, 140], weight scales [66, 140], delivery beds [70, 102], mobility aids [70, 102], and out-of-stock medication [63]. Even when available, this equipment could be misused [66]. These barriers were reported in countries across all world regions and with different levels of income, and particularly in rehabilitation services and general healthcare for persons with physical disabilities (30.3%).
No interventions were identified to facilitate access to medicines and accessible equipment in healthcare services for persons with disabilities, which underscores an urgent systemic gap.
Other factors
Structural factors
Beyond health systems, the impact of structural factors on access to healthcare services for persons with disabilities was evident. The negative attitudes towards persons with disabilities across all strata of society fuelled inequitable access to healthcare [55, 57, 59, 64, 79, 80, 82,83,84, 95, 98, 102, 106, 125, 130, 131, 134, 137]. Socio-cultural discriminatory beliefs about disability [59, 64, 83, 90, 102, 129, 134, 135, 153] often influenced help-seeking behaviours [64, 108, 129, 135, 137]. Family members of persons with disabilities may perpetuate these beliefs and attitudes [50, 55, 64, 68, 80, 83, 84, 95, 98, 102, 108, 129, 134, 135, 137] and hide their relatives with disabilities [98, 135], which could cause significant delays in accessing services or even prevent care [79, 98, 108, 134, 135]. Internalized stigma by persons with disabilities could also impact their access to healthcare services [31, 60, 83, 95, 105, 106, 108, 132, 133, 137, 176, 177]. This was particularly well evidenced in articles focusing on access to mental health services [83, 106, 108, 132, 133, 177] and sexual and reproductive health services [95, 176].
In total, 18 interventions targeting the negative societal attitudes towards persons with disabilities were identified [178,179,180,181,182], including 72.2% focusing specifically on persons with psychosocial disabilities and only 16.7% being scaled up at the national level. A few public campaigns targeting stigma to promote the use of mental health services were scaled up nationally in the USA [183] and UK [184]. On a global scale, the WHO QualityRights initiative aimed to improve societal attitudes towards persons with psychosocial disabilities and promote access to quality mental healthcare through a human right-based approach, with positive results [124].
Social determinants of health
The social determinants of health played a critical role in inequitable access of healthcare services for persons with disabilities. Most notably, poverty experienced by persons with disabilities [57, 86], often exacerbated by unemployment [56, 95, 131] or homelessness [73], could limit care-seeking behaviours. This was particularly relevant for persons with psychosocial disabilities. Persons with disabilities were often dependent on the benevolence of their caregivers to access health services, which resulted in issues of autonomy and confidentiality that were well evidenced for children, girls and women with disabilities [81, 99, 130, 137]. Additionally, persons with disabilities and their caregivers rarely benefited from educational opportunities to develop their health literacy [31, 52, 53, 57, 59, 62, 64, 73, 74, 76, 79, 80, 83, 87, 106, 108, 129, 134, 137], hence lacked the knowledge to identify their health needs [31, 177] and services that can help [31, 66, 82, 131, 177].
Persons with disabilities frequently faced issues related to the lack or limited availability of accessible transportation to reach healthcare services [31, 50, 54, 60, 76, 82, 89, 98, 101, 102, 138,139,140, 176, 185, 186], which could be further prohibited by transportation costs [31, 56, 60, 81, 89, 98, 101, 102, 131, 134, 135, 186], the lack of accommodations for physical [81] or psychosocial needs [62], and the risk of violence [186] in public services.
Importantly, intersectional issues leading to inequitable access of healthcare services for persons with disabilities were reported. Those living in rural areas [52, 86] were further disadvantaged due to the lack of community healthcare, which also resulted in additional travel costs [56]. Women and girls with disabilities faced additional challenges, such as dependence on male family members around health-seeking decisions which could be highly problematic in the context of domestic abuse [80] and access to sexual and reproductive healthcare services. Specific barriers faced by persons with disabilities from minority ethnic groups [57, 60, 91] were highlighted, including language barriers [91, 92], the lack of culturally appropriate information or dependence on personal networks to arrange care [60]. Lastly, immigrants and refugees with disabilities [90, 108, 153] experienced additional issues of trust with services in a ‘foreign system’ [90, 153], the fear of the consequences on their right to stay in the country if they access services [90], and language and cultural barriers [90, 108, 153].
Among the 29 interventions identified to improve access of healthcare services for persons with disabilities through the social determinants of health, almost half of these interventions focused on persons with psychosocial disabilities, and only 20.7% were scaled up nationally. The majority targeted the education of caregivers [156, 187,188,189] and persons with disabilities [187, 189,190,191,192,193,194], mostly addressing issues of stigma [178, 195], self-stigma [178, 196,197,198,199], social support [200, 201], and developing the skills and knowledge of persons with disabilities [187, 189,190,191,192,193,194]. Other education programmes targeted the health advocacy and empowerment of persons with disabilities [190, 191, 193, 202] with a component of peer-support [203]. For example, the W-DARE project in the Philippines aimed to increase access to sexual and reproductive health information and services for women with disabilities through participatory research [193, 202]. A few interventions supported the development of accessible health information disseminated outside of healthcare services [187, 204,205,206,207,208] and mostly included the active involvement from persons with disabilities, but there was a considerable discrepancy between the large need and the limited reach of these small-scale interventions. Additionally, a few interventions adopted a multisectoral approach to target the social determinants of health for persons with disabilities. One such example is the Housing First approach implemented in North America to support persons with psychosocial disabilities [209]. There were interventions aimed at addressing transportation barriers for persons with disabilities, such as the Journey Access Tool in Cambodia [210] and the TransportMYpatient programme in Tanzania [211]. Lastly, the development of telehealth services was highlighted as a promising solution for persons with disabilities living in rural areas [101, 131].
Risk factors
Persons with disabilities had heightened health risks such as medical complications or comorbid conditions [83, 85, 109], which could directly impact their access to healthcare services. For example, they may be feeling too unwell or sick to arrange care and access services [85, 132, 177], or prioritizing certain health needs over others [31, 60, 89, 105, 129]. Additionally, the overshadowing of symptoms by healthcare workers could lead to inefficient, even harmful, services for persons with disabilities in healthcare settings [89, 95]. The majority of this evidence explored the risk factors experienced by persons with psychosocial disabilities, but little was reported on the needs of other groups of persons with disabilities at risk of further marginalization. No interventions targeting risk factors were identified to improve access to healthcare services for persons with disabilities.
Discussion
This scoping review is the first of its kind to present a global overview of the barriers that persons with disabilities face when accessing healthcare services, as well as the interventions that are implemented to remove them and promote inclusive services. It yields critical insights for the global public health community on what is needed to improve healthcare access for the 1.3 billion people with disabilities worldwide [1], in order to advance health equity and catalyze efforts to achieve global health targets. Four key trends are highlighted below, and their implications for relevant stakeholders discussed.
Firstly, this review highlights a positive trend of increased publication rates of articles on the barriers of access to healthcare services over the past decade, which illustrates a heightened interest in factors leading to health inequities for persons with disabilities. A similar trend is observed for the articles on interventions, however these do not readily map onto the actual needs of persons with disabilities. For example, our results show that the common barriers faced by persons with disabilities are often related to issues of transportation to access healthcare services [31, 50, 60], widespread difficulties around communication [49, 51, 55], and the lack of accessible equipment in healthcare facilities [52, 70, 76]. These findings are echoed in previous reviews on the topic [212, 213], but our review also demonstrates that these barriers remain largely unaddressed by the interventions to promote disability inclusion. Additionally, interventions are often siloed small-scale projects with little indication on sustainability, scaling up or cross-sectoral engagement. The lack of investment and evaluation of larger-scale interventions comes in stark contrast with the high and increasing prevalence of persons with disabilities globally [1]. Therefore, we encourage service providers and policymakers to invest in and align their efforts in global, national and local health planning to meet the needs of persons with disabilities. Interventions that are expected to have the most impact are those that address the most pressing needs reported by persons with disabilities, strategize solutions across all components of the health system to meet these needs, and strengthen collaboration with multisectorial stakeholders to tackle the complex issues of health inequities beyond the health sector [214].
Secondly, it is encouraging to note the focus on certain groups of persons with disabilities at a higher risk of discrimination and marginalization in about half of the articles included on barriers. However, this trend is not replicated in the design of interventions to promote inclusive healthcare services. This means that the solutions that are being implemented may not reach some of the most marginalized groups of persons with disabilities, such as older persons with disabilities [215], ethnic minorities [216], women and girls or gender diverse persons [217], children [23], refugees and immigrants with disabilities [218]. While our findings provide only limited insights on how intersectionality interplays with health equity, it is essential to recognize that the health needs and priorities of different groups of persons with disabilities can differ widely and require tailored actions. For example, women with disabilities face unique challenges in sexual and reproductive healthcare services, such as the lack of accessible delivery beds [70], stigma towards their sexuality or even forced sterilization [102, 219]. Importantly, addressing the barriers faced by the most marginalized groups of persons with disabilities can foster health equity for everyone. This is because the same barriers often hinder access to healthcare services for other marginalized groups, such as older adults, people with noncommunicable diseases, or refugees [1]. We recommend service providers, policymakers, and stakeholders consult with persons with disabilities with a wide range of intersectional identities in order to better understand and address their unique health needs and intersectional mediating and risk factors to improve access to healthcare services. Special considerations should be given to the needs of women and girls, sexual and gender minority groups, children and older persons, ethnic minorities, and immigrants and refugees with disabilities to accelerate the prioritization and implementation of the most impactful strategies, and optimize resource allocation towards health equity [1]. For example, Ageing- and Disability-friendly cities are promising initiatives to identify and address the needs of older citizens with and without disabilities to inform more inclusive urban spaces, promote participation and healthy living in communities [220].
Thirdly, the lack of involvement of persons with disabilities and their representative organizations is observed in most interventions, and may well contribute to widening gaps and needs remaining unmet [193, 202]. In this review, we incorporated information that was shared during consultations organized by the World Health Organizations as part of the development process of the Global report on health equity for persons with disabilities [1]. While our results cannot claim to reflect the views and knowledge of those who participated in these consultations, this additional step was important to operationalize the principles of the UNCRPD towards more engagement with persons with disabilities and their representative organizations. In fact, these consultations, led to the increased representation of interventions promoting human right-based and consultative approaches in our results [124, 168, 191]. The meaningful engagement of persons with disabilities and their representative organizations in every effort to promote inclusive access to healthcare – and especially in leadership roles – is essential to progress this agenda [1]. Promoting innovative and empowering participatory processes can catalyze efforts to address health equity for persons with disabilities more meaningfully and efficiently [1, 221]. For example, the W-DARE programme on improving the sexual and reproductive health of women with disabilities in the Philippines successfully demonstrates the benefits of inclusion and participatory methods on care quality, impact, team capacity and commitment [193, 222]. We advise researchers, policymakers and services providers to strengthen collaboration with persons with disabilities and their representative organizations to accelerate the identification, prioritization and implementation of strategies, and promote innovation and capacity-building within and beyond the health sector [202]. We encourage governments and decision-makers in the health sector to set expectations and establish a collaboration mechanism to work efficiently with Organizations of Persons with Disabilities. The Government of Australia, through its digital transformation strategy, sets a good example by stating the inclusion of persons with disabilities and other groups in drafting policies and in the digital design process [223].
Fourthly, our review further emphasizes the uneven representation of countries in the research evidence on disability and healthcare provision. The evidence is largely skewed towards high-income countries, which comprises about two thirds of the articles included on barriers (66.3%) and interventions (62.6%). This represents a clear limitation since an estimated 80% of persons with disabilities worldwide live in low- and middle-income countries [1], and because interventions are highly sensitive to resources. Furthermore, this trend is compounded by the fact that intervention impact is inconsistently evaluated or done according to differing, incomparable criteria to measure success. For example, the profile of persons with disabilities who are eligible to benefit from the intervention may be mentioned, but it is often unclear whether the interventions reached people and improved their health and wellbeing [149]. Together, these gaps are detrimental to the identification of appropriate, wide-reaching, and impactful interventions to address health equity in least advantaged settings where the need is the highest. They expose the need to carefully consider and optimize the distribution of resources to advance health equity for persons with disabilities globally, and to put in place a systematic and transparent evaluation mechanism to assess impact. To address this, global health decision-makers and funders, in close collaboration with Organizations of Persons with Disabilities, have a key role to play in overseeing and coordinating the distribution of resources, building the capacity of country partners, prioritizing the most disadvantaged, and monitoring progress on health equity for persons with disabilities worldwide. Existing networks, such as the Global Action on Disability Network [224], that bring multiple stakeholders together can facilitate this coordination towards inclusive international development.
By uncovering these global trends around access to healthcare services for persons with disabilities in this review, we also expose the need to develop a comprehensive global research agenda to better mobilize, guide, and advance actions for health equity for persons with disabilities. The recently published WHO Global report on health equity for persons with disabilities already provides evidence-based recommendations for governments, researchers, and other key stakeholders to promote disability inclusion in the health sector [1], such as through data disaggregation [225], or the meaningful participation of persons with disabilities at all stages of the research cycle and in decision-making roles [221]. To complement these recommendations, a global research agenda is needed to articulate a clear vision and address the existing gaps in a sustainable manner.
To maximize impact, this research agenda should prioritize the generation of evidence that will most readily promote synergies with existing national and global health systems planning, and stimulate health policy and systems research impact [226]. In addition, it should concentrate on the potential of disability inclusive strategies to positively impact access to quality healthcare services for the wider population and other marginalized groups. Importantly, the development of this agenda requires the close collaboration and engagement of multisectorial partners and research networks to better address the deep and multidimensional roots of health inequities, with persons with disabilities and their representative organizations at the forefront of such endeavor [36]. Last but not least, it is essential for this research agenda to stimulate a wide ambition for health equity: one which goes beyond the scope of health systems to inspire and capture change at the societal level. For example, generating evidence on national budgeting priorities and mechanisms can allow to advocate for inclusive investments in the health sector and beyond more effectively. Creating interdisciplinary research networks can promote cross-sectoral coordination to foster impact to the health and well-being of persons with disabilities (e.g., promoting the implementation of inclusive public health interventions in schools to reach children with disabilities).
In conclusion, it needs to be mentioned that this scoping review was conducted under certain limitations. First, while the research team carefully selected two of the most prolific and relevant scientific databases in the field, it would have been desirable to run the search in more databases but this was not possible due to access and capacity constraints. Second, we used a random sample of the evidence to better engage with a selected set of articles and reflect on global trends in this field, which means that other relevant articles may have been missed. We reached a saturation point, as determined by the identification of redundant patterns in the information extracted from the included articles and through discussions with all co-authors on these trends. As such, the findings should provide an overview of the global evidence and fulfil the purpose of a scoping review approach, but more targeted lines of enquiry are warranted to complement these findings. Third, we included articles in only four languages, which may have limited the representation of evidence from certain countries. Fourth, we recognize that many of the interventions implemented to promote access to healthcare services for persons with disabilities may not have reached the scientific or grey literature. Lastly, the lens of the health system components was useful to present evidence on this topic and derive recommendations for leaders and decision-makers in the health sector. However, this framework may not capture all the perspectives, nuances and mechanisms that regulate health equity for persons with disabilities, especially as they related to the complexities of factors informing health-seeking behaviours. These aspects should be considered in further research to complement the findings of our review, and in the development of conceptual frameworks on health equity. Finally, future studies will benefit from the close collaboration with grassroot non-governmental and civil society organizations to inform contextualised situation analyses, identify unpublished initiatives, and complement the findings of this review. The influential role of these partners has been particularly well demonstrated in the responses to health emergencies and COVID-19 [15, 227], thus revealing their critical function to achieve health equity for persons with disabilities.
Conclusion
Persons with disabilities continue to face considerable barriers when accessing healthcare services, which negatively affects their chances of achieving their highest attainable standard of health [36]. It is encouraging to note the increasing evidence on interventions targeting equitable access to healthcare services, including some demonstrating strong alignment with the UNCRPD. However, they remain too few and sparse to meet the needs of over 1.3 billion people with disabilities globally [1]. This evidence calls for a radical change in the way that disability inclusion is considered, integrated, and sustained in health system planning. Beyond access to healthcare services, our findings indicate that wider structural change on how the health system and society can address health equity for persons with disabilities is needed to tackle current and anticipated global health priorities. Investigating intersectional mediating and risk factors is critical to reach a more nuanced understanding of the mechanisms that regulate the health inequities experienced by the most marginalized groups of persons with disabilities. Collaboration should be facilitated to drive innovation and impact: researchers, decision-makers in the health sector, Organizations of Persons with Disabilities, bilateral donors and other key stakeholders all have a role to play to drive the agenda of health equity for persons with disabilities.
Availability of data and materials
All relevant data are mentioned within the manuscript and supplementary materials, and the full references of the included papers in this review are provided.
Notes
The six WHO regions are (1) African Region; (2) Region of the Americas; (3) South-East Asia Region; (4) European Region; (5) Eastern Mediterranean Region; (6) Western Pacific Region.
We define intersectionality when individuals are socially situated through multiple overlapping identities that intersect with systems of oppression and marginalization (e.g., gender, race, social class, disability), which can lead to unique experiences of health and an increased risk of health disparities. With this definition, we acknowledge the mechanisms of oppression and marginalization that contribute to health inequities for persons with disabilities, and move away from reductionist and stigmatized views of persons with disabilities. To extract information on intersectionality, we consulted the UN list of vulnerable groups (e.g., women, LGBTQI + , race, or migrants) and complemented it with the multiple identities of persons with disabilities elaborated in the UNCRPD (e.g., children with disabilities).
[47] Kelly C, Dansereau L, Sebring J, Aubrecht K, FitzGerald M, Lee Y, et al. Intersectionality, health equity, and EDI: What's the difference for health researchers? International Journal for Equity in Health. 2022;21(1).
[48] United Nations. Vulnerable groups: who are they? 2023 [3 October 2023]. Available from: https://www.un.org/en/fight-racism/vulnerable-groups.
[36] United Nations. Convention on the Rights of Persons with Disabilities (UNCRPD). New York; 2006.
References
World Health Organization. Global report on health equity for persons with disabilities. Geneva: World Health Organization; 2022.
World Health Organization, World Bank. World report on disability. Geneva: World Health Organization; 2011.
The Missing Billion. The Missing Billion: Access to health services for 1 billion people with disabilities. London School of Hygiene & Tropical Medicine. London; 2022.
Landes SD. The intellectual disability mortality disadvantage: diminishing with age? Am J Intellect Dev Disabil. 2017;122(2):192–207.
Bahk J, Kang H-Y, Khang Y-H. The life expectancy gap between registered disabled and non-disabled people in Korea from 2004 to 2017. Int J Environ Res Public Health. 2019;16(14):2593.
Langballe EM, Tangen GG, Engdahl B, Strand BH. Increased mortality risk for adults aged 25–44 years with long-term disability: a prospective cohort study with a 35-year follow-up of 30,080 individuals from 1984–2019 in the population-based HUNT study. Lancet Reg Health Eur. 2022;22:100482.
O’Leary L, Hughes-McCormack L, Dunn K, Cooper SA. Early death and causes of death of people with down syndrome: a systematic review. J Appl Res Intellect Disabil. 2018;31(5):687–708.
Wang H, Lee PMY, Zhang J, Svendsen K, Li F, Li J. Association of intellectual disability with overall and type-specific cardiovascular diseases: a population-based cohort study in Denmark. BMC Med. 2023;21(1):41.
Elia M, Monga M, De S. Increased nephrolithiasis prevalence in people with disabilities: a national health and nutrition survey analysis. Urology. 2022;163:185–9.
Watt RG, Venturelli R, Daly B. Understanding and tackling oral health inequalities in vulnerable adult populations: From the margins to the mainstream. Br Dent J. 2019;227(1):49–54.
Moodley J, Ross E. Inequities in health outcomes and access to health care in South Africa: a comparison between persons with and without disabilities. Disabil Soc. 2015;30(4):630–44.
Radhakrishnan S, Kohler F, Gutenbrunner C, Jayaraman A, Li J, Pieber K, et al. The use of the international classification of functioning, disability and health to classify the factors influencing mobility reported by persons with an amputation: an international study. Prosthet Orthot Int. 2017;41(4):412–9.
Mahdi S, Viljoen M, Yee T, Selb M, Singhal N, Almodayfer O, et al. An international qualitative study of functioning in autism spectrum disorder using the World Health Organization international classification of functioning, disability and health framework. Autism Res. 2018;11(3):463–75.
Lifshitz H, Merrick J, Morad M. Health status and ADL functioning of older persons with intellectual disability: Community residence versus residential care centers. Res Dev Disabil. 2008;29(4):301–15.
Pearce E, Kamenov K, Barrett D, Cieza A. Promoting equity in health emergencies through health systems strengthening: Lessons learned from disability inclusion in the COVID-19 pandemic. Int J Equity Health. 2022;21(3):149.
Shakespeare T, Ndagire F, Seketi QE. Triple jeopardy: Disabled people and the COVID-19 pandemic. Lancet. 2021;397(10282):1331–3.
Williamson EJ, McDonald HI, Bhaskaran K, Walker AJ, Bacon S, Davy S, et al. Risks of covid-19 hospital admission and death for people with learning disability: population based cohort study using the OpenSAFELY platform. BMJ. 2021;374:n1592.
Balaj M, York HW, Sripada K, Besnier E, Vonen HD, Aravkin A, et al. Parental education and inequalities in child mortality: a global systematic review and meta-analysis. Lancet. 2021;398(10300):608–20.
Lancet. Taking urgent action on health inequities. Lancet. 2020;395(10225):659.
Mackenbach JP, Valverde JR, Bopp M, Brønnum-Hansen H, Deboosere P, Kalediene R, et al. Determinants of inequalities in life expectancy: an international comparative study of eight risk factors. Lancet Public Health. 2019;4(10):e529–37.
Frier A, Barnett F, Devine S, Barker R. Understanding disability and the “social determinants of health”: How does disability affect peoples’ social determinants of health? Disabil Rehabil. 2018;40(5):538–47.
Brown M, McCann E. Homelessness and people with intellectual disabilities: a systematic review of the international research evidence. J Appl Res Intellect Disabil. 2021;34(2):390–401.
UNICEF. Seen, counted, included: using data to shed light on the well-being of children with disabilities. UNICEF: New-York; 2022.
United Nations. Disability and development report 2018: Realizing the sustainable development goals by, for and with persons with disabilities. New York: UN Department of Economic and Social Affairs; 2019. p. 2019.
Janz HL. Ableism: the undiagnosed malady afflicting medicine. Can Med Assoc J. 2019;191(17):E478–9.
Heslop PD, Blair PSP, Fleming PP, Hoghton MM, Marriott AM, Russ LR. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet. 2014;383(9920):889–95.
Lancet. Prioritising disability in universal health coverage. Lancet. 2019;394(10194):187.
Swenor BK. Including disability in all health equity efforts: An urgent call to action. Lancet Public Health. 2021;6(6):e359–60.
Rhoads MA. Applying the ADA: Designing for The 2010 Americans with Disabilities Act Standards for accessible design in multiple building types: Wiley-Blackwell. 2013.
Nguyen TV, King J, Edwards N, Dunne MP. “Nothing suitable for us”: experiences of women with physical disabilities in accessing maternal healthcare services in Northern Vietnam. Disabil Rehabil. 2022;44(4):573–81.
Bright T, Wallace S, Kuper H. A systematic review of access to rehabilitation for people with disabilities in low- and middle-income countries. Int J Environ Res Public Health. 2018;15(10):2165.
McIlfatrick S, Taggart L, Truesdale-Kennedy M. Supporting women with intellectual disabilities to access breast cancer screening: a healthcare professional perspective. Eur J Cancer Care. 2011;20(3):412–20.
Smith SE, McCann HP, Dykens EM, Hodapp RM. The disability-training needs of healthcare professionals: scoping review and new initiatives. Int Rev Res Dev Disabil. 2020;58:219–64.
Hunt X, Carew MT, Braathen SH, Swartz L, Chiwaula M, Rohleder P. The sexual and reproductive rights and benefit derived from sexual and reproductive health services of people with physical disabilities in South Africa: Beliefs of non-disabled people. Reprod Health Matters. 2017;25(50):66–79.
World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurements strategies. Geneva, Switzerland: World Health Organization; 2010.
United Nations. Convention on the Rights of Persons with Disabilities (UNCRPD). New York: United Nations, Department of Economic and Social Affairs; 2006.
Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annuals of Internal Medicine. 2018;169(7):467–73.
Bramer WM, Rethlefsen ML, Kleijnen J, Franco Duran OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Revi. 2017;6(1):245.
International Disability Alliance. Advancing the rights of persons with disabilities 2023 [Available from: https://www.internationaldisabilityalliance.org.
International Disability and Development Consortium. Human right for all 2023 [Available from: https://www.iddcconsortium.net.
Disability Evidence Portal. A repository of solutions, evidence and tools for strengthening decision-making within Disability-Inclusive Development 2023. Available from: https://www.disabilityevidence.org.
McHugh ML. Interrater reliability: the kappa statistic. Biochemia Medica. 2012;22(3):276–82.
Rayyan. Rayyan screening web-tool 2023. Available from: https://www.rayyan.ai.
World Health Organization. WHO regional offices 2023. Available from: https://www.who.int/about/who-we-are/regional-offices.
Kelly C, Dansereau L, Sebring J, Aubrecht K, FitzGerald M, Lee Y, et al. Intersectionality, health equity, and EDI: What’s the difference for health researchers? Int J Equity Health. 2022;21(1):182.
United Nations. Vulnerable groups: who are they? 2023 [3 October 2023]. Available from: https://www.un.org/en/fight-racism/vulnerable-groups.
Tabril T, Chekira A, Touhami YOH, El Allani L, Najid I, Hammani Z, et al. The role of the general practitioner in management of psychiatric disorders. Revue d’Épidemiologie et de Santé Publique. 2020;68(3):185–92.
Silva VAd, Busnello ARR, Cavassin RC, Loureiro APC, Moser ADdL, Carvalho DR. Physiotherapy access for children and adolescents with physical disabilities in public institutions. Ciência Saude Coletiva. 2020;25(7):2859–70.
O’Halloran R, Grohn B, Worrall L. Environmental factors that influence communication for patients with a communication disability in acute hospital stroke units: a qualitative metasynthesis. Arch Phys Med Rehabil. 2012;93(1):S77-85.
Igwesi-Chidobe C. Obstacles to obtaining optimal physiotherapy services in a rural community in southeastern Nigeria. Rehabil Res Pract. 2012;2012:909675.
Jindal P, MacDermid JC, Rosenbaum P, DiRezze B, Narayan A. Perspectives on rehabilitation of children with cerebral palsy: Exploring a cross-cultural view of parents from India and Canada using the international classification of functioning, disability and health. Disabil Rehabil. 2018;40(23):2745–55.
Kumurenzi A, Goliath C, Mji G, Mlenzana N, Joseph C, Stathum S, et al. Experiences of patients and service providers with out-patient rehabilitation services in a rehabilitation centre in the Western Cape Province. Afr J Disabil. 2015;4(1):164.
Schildberger B, Zenzmaier C, Konig-Bachmann M. Experiences of Austrian mothers with mobility or sensory impairments during pregnancy, childbirth and the puerperium: a qualitative study. BMC Pregnancy Childbirth. 2017;17(1):201.
Gallego G, Dew A, Lincoln M, Bundy A, Chedid RJ, Bulkeley K, et al. Access to therapy services for people with disability in rural Australia: a carers’ perspective. Health Soc Care Community. 2017;25(3):1000–10.
Kaufman EA, McDonell MG, Cristofalo MA, Ries RK. Exploring barriers to primary care for patients with severe mental illness: frontline patient and provider accounts. Issues Ment Health Nurs. 2012;33(3):172–80.
Mitchell R, Fajardo Pulido D, Ryder T, Norton G, Brodaty H, Draper B, et al. Access to rehabilitation services for older adults living with dementia or in a residential aged care facility following a hip fracture: healthcare professionals’ views. Disabil Rehabil. 2021;43(6):834–45.
Nuri RP, Aldersey HM, Ghahari S, Huque AS. Service providers’ perspectives in providing services to children with disabilities and their families in Bangladesh. Disabil Rehabil. 2022;44(17):4700–8.
Bryant J, Noble N, Freund M, Rumbel J, Eades S, et al. How can dementia diagnosis and care for Aboriginal and Torres Strait Islander people be improved? Perspectives of healthcare providers providing care in Aboriginal community controlled health services. BMC Health Serv Res. 2021;21(1):699.
Guerin BM, Payne DA, Roy DE, McPherson KM. “It’s just so bloody hard”: Recommendations for improving health interventions and maternity support services for disabled women. Disabil Rehabil. 2017;39(23):2395–403.
Pitman AL, Osborn DPJ, Wright CA, Nazareth I, King MB. Cardiovascular screening of people with severe mental illness in England: views of service users and providers. Psychiatr Serv. 2011;62(11):1338–45.
Kenya Union of the Blind, World Blind Union. Documenting Kenya’s implementation of Sustainable Development Goals (SDGs) in compliance with the UN Convention on the Rights of Persons with Disabilities (CRPD). 2020.
UNICEF. Best of UNICEF research 2017. Innocenti, Florence: UNICEF Office of Research; 2017.
National Council on Disability. Medical futility and disability bias: Part of the bioethics and disability series. Washington, DC: National Council on Disability; 2019.
National Council on Disability. Enforceable Accessible Medical Equipment Standards: A Necessary Means to Address the Health Care Needs of People with Mobility Disabilities. Washington, CD: National Council on Disability; 2021.
Tuffrey-Wijne I, Goulding L, Giatras N, Abraham E, Gillard S, White S, et al. The barriers to and enablers of providing reasonably adjusted health services to people with intellectual disabilities in acute hospitals: evidence from a mixed-methods study. BMJ Open. 2014;4(4):1–10.
Webb CM, Collin SM, Deave T, Haig-Ferguson A, Spatz A, Crawley E. What stops children with a chronic illness accessing health care: a mixed methods study in children with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME). BMC Health Serv Res. 2011;11:308.
Voillemont C, Imbault E, Schoenberger M, Di Patrizio P. Care and management of adults with autism spectrum disorder in family practice: difficulties experienced by general practitioners. Fam Pract. 2022;39(3):464–70.
Tarasoff LA. “We don’t know. We’ve never had anybody like you before”: Barriers to perinatal care for women with physical disabilities. Disabil Health J. 2017;10(3):426–33.
Samtani G, Bassford TL, Williamson HJ, Armin JS. Are researchers addressing cancer treatment and survivorship among people with intellectual and developmental disabilities in the US? A scoping review. Intellect Dev Disabil. 2021;59(2):141–54.
Saleeby PW, Hunter-Jones J. Identifying barriers and facilitators to breast health services among women with disabilities. Social Work in Public Health. 2016;31(4):255–63.
Relyea E, MacDonald B, Cattaruzza C, Marshall D. On the margins of death: a scoping review on palliative care and schizophrenia. J Palliat Care. 2019;34(1):62–9.
Peters K, Cotton A. Barriers to breast cancer screening in Australia: experiences of women with physical disabilities. J Clin Nurs. 2015;24(3–4):563–72.
Aass LK, Moen OL, Skundberg-Kletthagen H, Lundqvist L-O, Schroder A. Family support and quality of community mental health care: perspectives from families living with mental illness. J Clin Nurs. 2021;31(7–8):935–48.
Pearson J, Payne D, Yoshida K, Garrett N. Access to and engagement with cervical and breast screening services for women with disabilities in Aotearoa New Zealand. Disabil Rehabil. 2022;44(10):1984–95.
Agaronnik ND, El-Jawahri A, Kirschner K, Iezzoni LI. Exploring cancer treatment experiences for patients with preexisting mobility disability. Am J Phys Med Rehabil. 2021;100(2):113–9.
Bernal OA, McClintock HF, Kurichi JE, Kwong PL, Xie D, Streim JE, et al. Patient satisfaction and perceived quality of care among younger medicare beneficiaries according to activity limitation stages. Arch Phys Med Rehabil. 2019;100(2):289–99.
Borade N, Ingle A, Nagarkar A. Lived experiences of people with mobility-related disability using assistive devices. Disabil Rehabil Assist Technol. 2021;16(7):730–4.
Bradbury-Jones C, Breckenridge JP, Devaney J, Kroll T, Lazenbatt A, Taylor J. Disabled women’s experiences of accessing and utilising maternity services when they are affected by domestic abuse: a critical incident technique study. BMC Pregnancy Childbirth. 2015;15:181.
Breckenridge JP, Devaney J, Kroll T, Lazenbatt A, Taylor J, Bradbury-Jones C. Access and utilisation of maternity care for disabled women who experience domestic abuse: a systematic review. BMC Pregnancy Childbirth. 2014;14:234.
Cassell CH, Mendez DD, Strauss RP. Maternal perspectives: Qualitative responses about perceived barriers to care among children with orofacial clefts in North Carolina. Cleft Palate Craniofac J. 2012;49(3):262–9.
Deng Y, Wang A-L, Frasso R, Ran M-S, Zhang T-M, Kong D, et al. Mental health-related stigma and attitudes toward patient care among providers of mental health services in a rural Chinese county. Int J Soc Psychiatry. 2021;68(3):610–8.
Ee J, Kroese BS, Lim JM, Rose J. What do specialist mental health professionals think of the mental health services for people with intellectual disabilities in Singapore? J Intellect Disabil. 2021;26(4):972–89.
Green AR, Wolff JL, Echavarria DM, Chapman M, Phung A, Smith D, et al. How clinicians discuss medications during primary care encounters among older adults with cognitive Iompairment. J Gen Intern Med. 2020;35(1):237–46.
Henderson J, Battams S. Mental health and barriers to the achievement of the “right to health.” Aust J Prim Health. 2011;17(3):220–6.
Hill C, Deville C, Alcorn S, Kiess A, Viswanathan A, Page B. Assessing and providing culturally competent care in radiation oncology for deaf cancer patients. Adv Radiat Oncol. 2020;5(3):333–44.
Horner-Johnson W, Klein KA, Campbell J, Guise J-M. Experiences of women with disabilities in accessing and receiving contraceptive care. J Obstet Gynecol Neonatal Nurs. 2021;50(6):732–41.
Lee S, Waters F, Briffa K, Fary RE. Limited interface between physiotherapy primary care and people with severe mental illness: a qualitative study. J Physiother. 2017;63(3):168–74.
Lindsay S, King G, Klassen AF, Esses V, Stachel M. Working with immigrant families raising a child with a disability: Challenges and recommendations for healthcare and community service providers. Disabil Rehabil. 2012;34(23):2007–17.
Makhoba M, Joseph N. Practices and views of audiologists regarding aural rehabilitation services for adults with acquired hearing loss. S Afr J Commun Disord. 2016;63(1):e1–10.
McBain H, Mulligan K, Lamontagne-Godwin F, Jones J, Haddad M, Flood C, et al. Implementation of recommended type 2 diabetes care for people with severe mental illness: a qualitative exploration with healthcare professionals. BMC Psychiatry. 2016;16:222.
Mimmo L, Woolfenden S, Travaglia J, Harrison R. Partnerships for safe care: a meta-narrative of the experience for the parent of a child with intellectual disability in hospital. Health Expect. 2019;22(6):1199–212.
Mitra M, Akobirshoev I, Moring NS, Long-Bellil L, Smeltzer SC, Smith LD, et al. Access to and satisfaction with prenatal care among pregnant women with physical disabilities: findings from a national survey. J Women’s Health. 2017;26(12):1356–63.
Nguyen A, Liamputtong P, Horey D. Reproductive health care experiences of people with physical disabilities in Vietnam. Sex Disabil. 2019;37(3):383–400.
O’Halloran R, Worrall L, Hickson L. Environmental factors that influence communication between patients and their healthcare providers in acute hospital stroke units: an observational study. Int J Lang Commun Disord. 2011;46(1):30–47.
Wheeler AC, Wylie A, Villagomez A, Bishop E, Raspa M. Health care for individuals with fragile X Syndrome: understanding access and quality. Disabil Health J. 2019;12(2):269–77.
Aenishänslin J, Amara A, Magnusson L. Experiences accessing and using rehabilitation services for people with physical disabilities in Sierra Leone. Disabil Rehabil. 2020;9207179:1–10.
Arulogun OS, Titiloye MA, Afolabi NB, Oyewole OE, Nwaorgu OGB. Experiences of girls with hearing impairment in accessing reproductive health care services in Ibadan, Nigeria. Afr J Reprod Health. 2013;17(1):85–93.
DeBeaudrap P, Mouté C, Pasquier E, Mac-Seing M, Mukangwije PU, Beninguisse G. Disability and access to sexual and reproductive health services in Cameroon: a mediation analysis of the role of socioeconomic factors. Int J Environ Res Public Health. 2019;16(3):4–10.
Elpers J, Lester C, Shinn JB, Bush ML. Rural family perspectives and experiences with early infant hearing detection and intervention: a qualitative study. J Community Health. 2016;41(2):226–33.
Ganle JK, Otupiri E, Obeng B, Edusie AK, Ankomah A, Adanu R. Challenges women with disability face in accessing and using maternal healthcare services in Ghana: a qualitative study. PLOS One. 2016;11(6):e0158361.
Gibbons HM, Owen R, Heller T. Perceptions of health and healthcare of people with intellectual and developmental disabilities in Medicaid managed care. Intellect Dev Disabil. 2016;54(2):94–105.
Morris MA, Yorkston K, Clayman ML. Improving communication in the primary care setting: perspectives of patients with speech disabilities. Patient. 2014;7(4):397–401.
Murphy KA, Stone EM, Presskreischer R, McGinty EE, Daumit GL, Pollack CE. Cancer screening among adults with and without serious mental illness: a mixed methods study. Med Care. 2021;59(4):327–33.
Cabral L, Muhr K, Savageau J. Perspectives of people who are deaf and hard of hearing on mental health, recovery, and peer support. Community Ment Health J. 2013;49(6):649–57.
Alduhaim A, Purcell A, Cumming S, Doble M. Parents’ views about factors facilitating their involvement in the oral early intervention services provided for their children with hearing loss in Kuwait. Int J Pediatr Otorhinolaryngol. 2020;128:109717.
Poon WC, Joubert L, Harvey C. Experiences of Chinese migrants caring for family members with schizophrenia in Australia. Soc Work Health Care. 2013;52(2–3):144–65.
Adigun OT, Akinrinoye O, Obilor HN. Including the excluded in antenatal care: a systematic review of concerns for D/deaf pregnant women. Behav Sci. 2021;11(5):67.
Rotenberg S, Rodríguez Gatta D, Wahedi A, Loo R, McFadden E, Ryan S. Disability training for health workers: a global evidence synthesis. Disabil Health J. 2022;15(2):101260.
Moxham L, Patterson C, Taylor E, Perlman D, Sumskis S, Brighton R. A multidisciplinary learning experience contributing to mental health rehabilitation. Disabil Rehabil. 2017;39(1):98–103.
O'Donovan J, Nam, a AS, Hamala R, Winters N, Bhutta MF. Exploring perceptions, barriers, and enablers for delivery of primary ear and hearing care by community health workers: a photovoice study in Mukono District, Uganda. Int J Equity Health. 2020;19(1):62–80.
Dagnan D, Masson J, Thwaites R, James A, Hatton C. Training therapists to work with people with intellectual disability in Improving Access to Psychological Therapies (IAPT) services. J Appl Res Intellect Disabil. 2018;31(5):760–7.
Martin-Prudent A, Lartz M, Borders C, Meehan T. Early intervention practices for children with hearing loss: Impact of professional development. Commun Disord Q. 2016;38(1):13–23.
Kilbourne AM, Goodrich DE, Lai Z, Almirall D, Nord KM, Bowersox NW, et al. Reengaging veterans with serious mental illness into care: preliminary results from a national randomized trial. Psychiatr Serv. 2015;66(1):90–3.
Morriss R, Vinjamuri I, Faizal MA, Bolton CA, McCarthy JP. Training to recognise the early signs of recurrence in schizophrenia. Cochrane Database Syst Rev. 2013;28(2):CD005147.
Happell B, Byrne L, McAllister M, Lampshire D, Roper C, Gaskin CJ, et al. Consumer involvement in the tertiary-level education of mental health professionals: a systematic review. Int J Ment Health Nurs. 2014;23(1):3–16.
Alduhaim A, Purcell A, Cumming S, Doble M. A new training package (3Cs: Connect, Communicate and Collaborate) for improving family responsive service delivery in early intervention for children with hearing loss: a proof of concept study. Int J Pediatr Otorhinolaryngol. 2021;140:110484.
Li J, Fan Y, Zhong HQ, Duan XL, Chen W, Evans-Lacko S, et al. Effectiveness of an anti-stigma training on improving attitudes and decreasing discrimination towards people with mental disorders among care assistant workers in Guangzhou, China. Int J Ment Health Syst. 2019;13(1):1.
Rai S, Gurung D, Kaiser BN, Sikkema KJ, Dhakal M, Bhardwaj A, et al. A service user co-facilitated intervention to reduce mental illness stigma among primary healthcare workers: utilizing perspectives of family members and caregivers. Fam Syst Health. 2018;36(2):198–209.
Giesbrecht EM, Miller WC, Mitchell IM, Woodgate RL. Development of a wheelchair skills home program for older adults using a participatory action design approach. BioMed Res Int. 2014;2014:172434.
Malik NN, Kannusamy P, Klanin-Yobas P. The effectiveness of mental health-related theoretical education and clinical placement in mental health settings in changing the attitudes of health care students towards mental illness: a systematic review. JBI Libr Syst Rev. 2012;10(58):4019–76.
Henderson C, Noblett J, Parke H, Clement S, Caffrey A, Gale-Grant O, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. 2014;1(6):467–82.
Pathare S, Funk M, Drew Bold N, Chauhan A, Kalha J, Krishnamoorthy S, et al. Systematic evaluation of the QualityRights programme in public mental health facilities in Gujarat, India. Br J Psychiatry. 2021;218(4):196–203.
Smeltzer SC, Mitra M, Long-Bellil L, Iezzoni LI, Smith LD. Obstetric clinicians’ experiences and educational preparation for caring for pregnant women with physical disabilities: a qualitative study. Disabil Health J. 2018;11(1):8–13.
Redfern H, Burton J, Lonne B, Seiffert H. Social work and complex care systems: the case of people hospitalised with a disability. Aust Soc Work. 2016;69(1):27–38.
Mudrick NR, Breslin ML, Nielsen KA, Swager LC. Can disability accommodation needs stored in electronic health records help providers prepare for patient visits? A qualitative study. BMC Health Serv Res. 2020;20(1):958.
Archibald D, Stratton J, Liddy C, Grant RE, Green D, Keely EJ. Evaluation of an electronic consultation service in psychiatry for primary care providers. BMC Psychiatry. 2018;18(1):119.
Zuurmond M, Mactaggart I, Kannuri N, Murthy G, Oye JE, Polack S. Barriers and facilitators to accessing health services: a qualitative study amongst people with disabilities in Cameroon and India. Int J Environ Res Public Health. 2019;16(7):1126.
Sightsavers. Knowledge, attitudes and practices in eye health and disability in Sierra Leone: Study Report 2014. 2014 2014.
Allen APT, Bolton WS, Jalloh MB, Halpin SJ, Jayne DG, Scott JDA. Barriers to accessing and providing rehabilitation after a lower limb amputation in Sierra Leone - A multidisciplinary patient and service provider perspective. Disabil Rehabil. 2020;44(11):1–8. https://pubmed.ncbi.nlm.nih.gov/33261506/#:~:text=Barriers%20to%20accessing%20services%20included,barriers%20to%20providing%20rehabilitation%20services.
Dockery L, Jeffery D, Schauman O, Williams P, Ly SF, Bonnington O, et al. Stigma- and non-stigma-related treatment barriers to mental healthcare reported by service users and caregivers. Psychiatry Res. 2015;228(3):612–9.
Harris MG, Baxter AJ, Reavley N, Diminic S, Pirkis J, Whiteford HA. Gender-related patterns and determinants of recent help-seeking for past-year affective, anxiety and substance use disorders: findings from a national epidemiological survey. Epidemiol Psychiatr Sci. 2016;25(6):548–61.
Hasan AA, Musleh M. Barriers to seeking early psychiatric treatment amongst first-episode psychosis patients: a qualitative study. Issues Ment Health Nurs. 2017;38(8):669–77.
Marthoenis M, Aichberger MC, Schouler-Ocak M. Patterns and determinants of treatment seeking among previously untreated psychotic patients in Aceh Province, Indonesia: a qualitative study. Scientifica. 2016;2016:9136079.
Novak P, Feder KA, Ali MM, Chen J. Behavioral health treatment utilization among individuals with co-occurring opioid use disorder and mental illness: Evidence from a national survey. J Subst Abuse Treat. 2019;98:47–52.
Oyelade OO, Nkosi-Mafutha NG. Living beyond the limitation: Rehabilitation, life and productivity of individuals with schizophrenia in South-West Nigeria. Health Expect. 2021;24(2):198–208.
Sakellariou D, Rotarou ES. Access to healthcare for men and women with disabilities in the UK: secondary analysis of cross-sectional data. BMJ Open. 2017;7(8):e016614-e.
Man J, Kangas M. Service satisfaction and helpfulness ratings, mental health literacy and help seeking barriers of carers of individuals with dual disabilities. J Appl Res Intellect Disabil. 2019;32(1):184–93.
Wong JL, Alschuler KN, Mroz TM, Hreha KP, Molton IR. Identification of targets for improving access to care in persons with long term physical disabilities. Disabil Health J. 2019;12(3):366–74.
Roux-Levy P-H, Sanlaville D, De Freminville B, Touraine R, Masurel A, Gueneau I, et al. Care management in a French cohort with Down syndrome from the AnDDI-Rares/CNSA study. Eur J Med Genet. 2021;64(10):104290.
Hensley MA. Case managers and the use of medicare: part D. Prof Case Manag. 2011;16(6):301–8.
McClellan C, Maclean JC, Saloner B, McGinty EE, Pesko MF. Integrated care models and behavioral health care utilization: quasi-experimental evidence from Medicaid health homes. Health Econ. 2020;29(9):1086–97.
Mueller-Stierlin AS, Helmbrecht MJ, Herder K, Prinz S, Rosenfeld N, et al. Does one size really fit all? The effectiveness of a non-diagnosis-specific integrated mental health care program in Germany in a prospective, parallel-group controlled multi-centre trial. BMC Psychiatry. 2017;17(1):283.
Romaire M, Alterbaum R, Collins A. Medicaid Behavioral Health Homes: lessons learned and early findings from Maine. Psychiatr Serv. 2020;71(11):1179–87.
Barr M, Duncan J, Dally K. Parent experience of the national disability insurance scheme (NDIS) for children with hearing loss in Australia. Disabil Soc. 2021;36(10):1663–87.
Parish SL, Rose RA, Yoo J, Swaine JG. State Medicaid policies and the health care access of low-income children with special health care needs living in the American South. N C Med J. 2012;73(1):15–23.
Kennedy J, Wood EG, Frieden L. Disparities in insurance coverage, health services use, and access following implementation of the Affordable Care Act: a comparison of disabled and nondisabled working-age adults. Inquiry J. 2017;54:46958017734031.
Aviram U, Ginath Y, Roe D. Mental health reforms in Europe: Israel’s rehabilitation in the community of persons with mental disabilities law: challenges and ppportunities. Psychiatr Serv. 2012;63(2):110–2.
Lovero KL, Lammie SL, van Zyl A, Paul SN, Ngwepe P, Mootz JJ, et al. Mixed-methods evaluation of mental healthcare integration into tuberculosis and maternal-child healthcare services of four South African districts. BMC Health Serv Res. 2019;19(1):83.
Golyk V, Syvak O, Grabljevec K, Tederko P, Gutenbrunner C, Nugraha B. Five years after development of the national disability, health and rehabilitation plan for Ukraine: achievements and challenges. J Rehabil Med. 2021;53(3):jrm00160.
Kranz AM, Ross R, Sorbero M, Kofner A, Stein BD, Dick AW. Impact of a Medicaid policy on preventive oral health services for children with intellectual disabilities, developmental disabilities, or both. J Am Dent Assoc. 2020;151(4):255–64.
Guzder J, Yohannes S, Zelkowitz P. Helpseeking of immigrant and native born parents: a qualitative study from a Montreal child day hospital. J Can Acad Child Adolesc Psychiatry. 2013;22(4):275–81.
Bryant J, Noble N, Freund M, Rumbel J, Eades S, Sanson-Fisher R, et al. How can dementia diagnosis and care for Aboriginal and Torres Strait Islander people be improved? Perspectives of healthcare providers providing care in Aboriginal community controlled health services. BMC Health Serv Res. 2021;21(1):699.
Lewis N, Lewis K, Davies B. ‘I don’t feel trapped anymore…I feel like a bird’: People with learning disabilities’ experience of psychological therapy. J Appl Res Intellect Disabil. 2016;29(5):445–54.
Brown CM, Beck AF, Steuerwald W, Alexder E, Samaan ZM, et al. Narrowing care gaps for early language delay: a quality improvement study. Clin Pediatr. 2016;55(2):137–44.
Irwin KE, Park ER, Fields LE, Corveleyn AE, Greer JA, Perez GK, et al. Bridge: Person-centered collaborative care for patients with serious mental illness and cancer. Oncologist. 2019;24(7):901–10.
Buszewicz M, Welch C, Horsfall L, Nazareth I, Osborn D, Hassiotis A, et al. Assessment of an incentivised scheme to provide annual health checks in primary care for adults with intellectual disability: a longitudinal cohort study. Lancet Psychiatry. 2014;1(7):522–30.
Isaacs AN, Sutton K, Dalziel K, Maybery D. Outcomes of a care coordinated service model for persons with severe and persistent mental illness: a qualitative study. Int J Soc Psychiatry. 2017;63(1):40–7.
Owen R, Crabb C, Stober K, Mitchell D, Yamaki K, Heller T. Utilization of and relationships with primary care providers during the transition to Medicaid managed care. J Disabil Policy Stud. 2020;31(2):67–76.
Johnson K, Tepper M, Leff HS, Mullin BO, Cook BL, Progovac AM. Assessing the long-term effectiveness of a Behavioral Health Home for adults with bipolar and psychotic disorders. Psychiatr Serv. 2021;73(2):172–9.
Highland J, Nikolajski C, Kogan J, Ji Y, Kukla M, Schuster J. Impact of Behavioral Health Homes on cost and utilization outcomes. Psychiatr Serv. 2020;71(8):796–802.
Xiong GL, Iosif A-M, Suo S, McCarron RM, Koike A, Onate J, et al. Understanding preventive health screening services use in persons with serious mental illness: How does integrated behavioral health primary care compare? Int J Psychiatry Med. 2015;48(4):279–98.
Murphy KA, Daumit GL, Stone E, McGinty EE. Physical health outcomes and implementation of behavioural health homes: a comprehensive review. Int Rev Psychiatry. 2018;30(6):224–41.
Macdonald S, Morrison J, Melville CA, Baltzer M, MacArthur L, Cooper SA. Embedding routine health checks for adults with intellectual disabilities in primary care: practice nurse perceptions. J Intellect Disabil Res. 2018;62(4):349–57.
Jones M, Kruger M, Walsh SM. Preparing non-government organization workers to conduct health checks for people with serious mental illness in regional Australia. J Psychiatr Ment Health Nurs. 2016;23(5):247–54.
Poltorak M. Anthropology, brokerage, and collaboration in the development of a Tongan public psychiatry: local lessons for global mental health. Transcult Psychiatry. 2016;53(6):743–65.
Gureje O, Appiah-Poku J, Bello T, Kola L, Araya R, Chisholm D, et al. Effect of collaborative care between traditional and faith healers and primary health-care workers on psychosis outcomes in Nigeria and Ghana (COSIMPO): a cluster randomised controlled trial. Lancet. 2020;396(10251):612–22.
Pennybaker S, Hemming P, Roy D, Anton B, Chisolm MS. Risks, benefits, and recommendations for pastoral care on inpatient psychiatric units: a systematic review. J Psychiatr Pract. 2016;22(5):363–81.
Morabito MS, Savage J, Sneider L, Wallace K. Police response to people with mental illnesses in a major U.S. city: the Boston experience with the co-responder model. Victims Offenders. 2018;13(8):1093–105.
Willems A, Iyamuremye JD, Misage CN, Smith-Swintosky V, Kayiteshonga Y. Co-creation and evaluation of nationwide remote training service for mental health education of community health workers in Rwanda. Front Public Health. 2021;9:632793.
Harney BL, Brereton R, Whitton B, Pietrzak D, Paige E, Roberts SK, et al. Hepatitis C treatment in a co-located mental health and alcohol and drug service using a nurse-led model of care. J Viral Hepatitis. 2021;28(5):771–8.
Battistella LR, Juca SSH, Tateishi M, Oshiro MS, Yamanaka EI, Lima E, et al. Lucy montoro rehabilitation network mobile unit: an alternative public healthcare policy. Disabil Rehabil Assist Technol. 2015;10(4):309–15.
Trondsen MV, Tjora A, Broom A, Scambler G. The symbolic affordances of a video-mediated gaze in emergency psychiatry. Soc Sci Med. 2018;197:87–94.
Röhricht F, Padmanabhan R, Binfield P, Mavji D, Barlow S. Simple mobile technology health management tool for people with severe mental illness: a randomised controlled feasibility trial. BMC Psychiatry. 2021;21(1):357.
Porat O, Heruti R, Navon-Porat H, Hardoff D. Counseling young people with physical disabilities regarding relationships and sexuality issues: utilization of a novel service. Sex Disabil. 2012;30(3):311–7.
Bay N, Bjørnestad J, Johannessen JO, Larsen TK, Joa I. Obstacles to care in first-episode psychosis patients with a long duration of untreated psychosis. Early Interv Psychiatry. 2016;10(1):71–6.
Smythe T, Adelson JD, Polack S. Systematic review of interventions for reducing stigma experienced by children with disabilities and their families in low- and middle-income countries: state of the evidence. Tropical Med Int Health. 2020;25(5):508–24.
Armstrong M, Morris C, Abraham C, Tarrant M. Interventions utilising contact with people with disabilities to improve children’s attitudes towards disability: a systematic review and meta-analysis. Disabil Health J. 2016;10(1):11–22.
Mehta N, Clement S, Marcus E, Stona AC, Bezborodovs N, Evans-Lacko S, et al. Evidence for effective interventions to reduce mental health-related stigma and discrimination in the medium and long term: systematic review. Br J Psychiatry. 2015;207(5):377–84.
Thornicroft GP, Mehta NM, Clement SP, Evans-Lacko SP, Doherty MM, Rose DP, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2015;387(10023):1123–32.
Mathias K, Mathias J, Goicolea I, Kermode M. Strengthening community mental health competence: a realist informed case study from Dehradun, North India. Health Soc Care Community. 2018;26(1):E179–90.
Collins RL, Wong EC, Breslau J, Burnam MA, Cefalu M, Roth E. Social marketing of mental health treatment: California’s mental illness stigma reduction campaign. Am J Public Health. 2019;109:S228–35.
Evans-Lacko S, Henderson C, Thornicroft G, McCrone P. Economic evaluation of the anti-stigma social marketing campaign in England 2009–2011. Br J Psychiatry. 2013;202(s55):s95–101.
Gormez A, Kurtulmus A, Ince Z, Torun P, Uysal O, Citak S. Psychiatric symptoms, challenging behaviour and utilization of psychiatric services among adults with intellectual disabilities in Turkey. J Appl Res Intellect Disabil. 2020;33(5):1038–48.
Mkabile S, Swartz L. Putting cultural difference in its place: barriers to access to health services for parents of children with intellectual disability in an urban African setting. Int J Soc Psychiatry. 2021;68(8):1614–22.
Tran N, Castle D. Outcomes from a regular medication information programme for consumers with a mental illness. Australas Psychiatry. 2012;20(2):143–7.
Rico-Blázquez M, García-Sanz P, Martín-Martín M, Lopez-Rodríguez JA, Morey-Montalvo M, Sanz-Cuesta T, et al. Effectiveness of a home-based nursing support and cognitive restructuring intervention on the quality of life of family caregivers in primary care: a pragmatic cluster-randomized controlled trial. Int J Nurs Stud. 2021;120:103955.
Jokel R, Meltzer J, et al. Group intervention for individuals with primary progressive aphasia and their spouses: who comes first? J Commun Disord. 2017;66:51–64.
Feldman MA, Owen F, Andrews A, Hamelin J, Barber R, Griffiths D. Health self-advocacy training for persons with intellectual disabilities: health self-advocacy training. J Intellect Disabil Res. 2012;56(11):1110–21.
Steinert C, Steinert T, Flammer E, Jaeger S. Impact of the UN convention on the rights of persons with disabilities (UN-CRPD) on mental health care research: a systematic review. BMC Psychiatry. 2016;16:166.
Chien WT, Leung SF, Chu CSK. A nurse-led, needs-based psycho-education intervention for Chinese patients with first-onset mental illness. Contemp Nurse. 2012;40(2):194–209.
Vaughan C, Gill-Atkinson L, Devine A, Zayas J, Ignacio R, Garcia J, et al. Enabling action: Reflections upon inclusive participatory research on health with women with disabilities in the Philippines. Am J Community Psychol. 2020;66(3):370–80.
Cook JA, Jonikas JA, Hamilton MM, Goldrick V, Steigman PJ, Grey DD, et al. Impact of Wellness Recovery Action Planning on service utilization and need in a randomized controlled trial. Psychiatr Rehabil J. 2013;36(4):250–7.
Neherta M, Maisa E, Sari Y. Intervention of sexual abuse prevention for mother of children with mental retardation in Payakumbuh, Indonesia, 2016. Indian J Public Health Res Dev. 2019;10(1):461–6.
Yanos PT, Lucksted A, Drapalski AL, Roe D, Lysaker P. Interventions targeting mental health self-stigma: a review and comparison. Psychiatr Rehabil J. 2015;38(2):171–8.
Hamblen JL, Grubaugh AL, Davidson TM, Borkman AL, Bunnell BE, Ruggiero KJ. An online peer educational campaign to reduce stigma and improve help seeking in veterans with posttraumatic stress disorder. Telemedicine and e-Health. 2019;25(1):41–7.
Mittal D, Sullivan G, Chekuri L, Allee E, Corrigan PW. Empirical studies of self-stigma reduction strategies: a critical review of the literature. Psychiatr Serv. 2012;63(10):974–81.
Schilling S, Bustamante JA, Sala A, Acevedo C, Tapia E, Alvarado R, et al. Development of an intervention to reduce self-stigma in outpatient mental health service users in Chile. Revista de la Facultad de Ciencias Medicas. 2015;72(4):284–94.
Hammarberg K, Sartore G, Cann W, Fisher JRW. Barriers and promoters of participation in facilitated peer support groups for carers of children with special needs. Scand J Caring Sci. 2014;28(4):775–83.
Shor R, Shalev A. The significance of services in a psychiatric hospital for family members of persons with mental illness. Fam Syst Health. 2015;33(1):68–71.
Devine A, Ignacio R, Prenter K, Temminghoff L, Gill-Atkinson L, Zayas J, et al. “Freedom to go where I want”: Improving access to sexual and reproductive health for women with disabilities in the Philippines. Reprod Health Matters. 2017;25(50):55–65.
Corrigan P, Sheehan L, Morris S, Larson JE, Torres A, Lara JL, et al. The impact of a peer navigator program in addressing the health needs of Latinos with serious mental illness. Psychiatr Serv. 2018;69(4):456–61.
Porter E, Kidd G, Murray N, Uytman C, Spink A, Anderson B. Developing the pregnancy support pack for people who have a learning disability. Br J Learn Disabil. 2012;40(4):310–7.
Oliveira GOB, Cavalcante LDW, Pagliuca LMF, Almeida PCd, Rebouças CBdA. Prevention of sexually transmitted diseases among visually impaired people: Educational text validation. Revista Latino-Americana de Enfermagem. 2016;24:1–9.
Robles-Bykbaev Y, Oyola-Flores C, Robles-Bykbaev VE, López-Nores M, Ingavélez-Guerra P, Pazos-Arias JJ, et al. A bespoke social network for deaf women in Ecuador to access information on sexual and reproductive health. Int J Environ Res Public Health. 2019;16(20):3962.
Oliveira MGd, Áfio ACE, Almeida PCd, Machado MMT, Lindsay AC, Pagliuca LMF. Teaching blind women about the anatomy and physiology of the female reproductive system through educational manual. Revista Brasileira de Saúde Materno Infantil. 2018;18(4):755–61.
Broussard B, Radkins JB, Compton MT. Developing visually based, low-literacy health education tools for African Americans with psychotic disorders and their Families. Community Ment Health J. 2014;50(6):629–36.
Mejia-Lancheros C, Lachaud J, To MJ, Lee P, Nisenbaum R, O’Campo P, et al. The long-term effects of a Housing First intervention on primary care and non-primary care physician visits among homeless adults with mental illness: a 7-Year RCT follow-up. J Prim Care Community Health. 2021;12:21501327211027104.
King JA, King MJ, Edwards N, Hair SA, Cheang S, Pearson A, et al. Addressing transport safety and accessibility for people with a disability in developing countries: a formative evaluation of the Journey Access Tool in Cambodia. Global Health Action. 2018;11(1):1538658.
Fiander AN, Vanneste T. transportMYpatient: an initiative to overcome the barrier of transport costs for patients accessing treatment for obstetric fistulae and cleft lip in Tanzania. Trop Doct. 2012;42(2):77–9.
Hashemi G, Wickenden M, Bright T, Kuper H. Barriers to accessing primary healthcare services for people with disabilities in low and middle-income countries: A meta-synthesis of qualitative studies. Disabil Rehabil. 2020;44(8):1207–20.
Gibson J, O’Connor R. Access to health care for disabled people: a systematic review. Social Care Neurodisabil. 2010;1(3):21–31.
Tangcharoensathien V, Srisookwatana O, Pinprateep P, Posayanonda T, Patcharanarumol W. Multisectoral actions for health: Challenges and opportunities in complex policy environments. Int J Health Policy Manag. 2017;6(7):359–63.
Ramirez L, Monahan C, Palacios-Espinosa X, Levy SR. Intersections of ageism toward older adults and other isms during the COVID-19 pandemic. J Soc Issues. 2022;78(4):965–90.
Gulley SP, Rasch EK, Chan L. Difference, disparity, and disability: a comparison of health, insurance coverage, and health service use on the basis of race/ethnicity among US adults with disabilities, 2006–2008. Med Care. 2014;52(10):S9–16.
Nakkeeran N, Nakkeeran B. Disability, mental health, sexual orientation and gender identity: Understanding health inequity through experience and difference. Health Research Policy and Systems. 2018;16(Suppl 1):97–108.
UNHCR. Unmet needs and diminished opportunities: Disability, displacement and humanitarian healthcare. Geneva: UNRCH: Policy Development and Evaluation Service; 2011.
Ganle JK, Baatiema L, Quansah R, Danso-Appiah A. Barriers facing persons with disability in accessing sexual and reproductive health services in sub-Saharan Africa: a systematic review. PLOS One. 2020;15(10):e0238585-e.
Yeh JC, Walsh J, Spensley C, Wallhagen M. Building inclusion: toward an aging- and disability-friendly city. Am J Public Health. 2016;106(11):1947–9.
Kuper H, Hameed S, Reichenberger V, Scherer N, Wilbur J, Zuurmond M, et al. Participatory research in disability in low-and middle-income countries: what have we learnt and what should we do? Scand J Disabil Res. 2021;23(1):328–37.
Vaughan C, Zayas J, Devine A, Gill-Atkinson L, Marella M, Garcia J, et al. W-DARE: A three-year program of participatory action research to improve the sexual and reproductive health of women with disabilities in the Philippines. BMC Public Health. 2015;15:984.
Australian Government: Digital Transformation Agency. Digital transformation strategy 2018–2025. Canberra: Commonwealth of Australia (Digital Transformation Agency); 2018.
GLAD Network. GLAD Network: Global Action on Disability Accessed 15 June 2023. Available from: https://gladnetwork.net.
Lancet Global Health. Disability: measurement matters. Lancet Global Health. 2021;9(8):e1028-e.
Cieza A, Kwamie A, Magaqa Q, Paichadze N, Sabariego C, Blanchet K, et al. Framing rehabilitation through health policy and systems research: priorities for strengthening rehabilitation. Health Res Policy Syst. 2022;20(1):101.
UNICEF. Learning about meaningful engagement with organizations of persons with disabilities in public health emergencies, including COVID-19. New York: UNICEF; 2021.
Acknowledgements
The authors gratefully acknowledge the participants of the consultations for their valuable contributions, and are particularly thankful for inputs received from persons with disabilities and their representative organizations.
Funding
MG, MFM, KK, DB and AC are in roles funded by the World Health Organization. AMR is supported by a Wellcome Trust Fellowship 219754/Z/19/Z and a Wellcome Trust Secondment Fellowship 223712/Z/21/Z. These funding bodies did not have a role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualisation of this study, and read and approved the final manuscript. In addition, MG contributed to the study design, literature search, data extraction and synthesis, figure and table production, data interpretation, review, writing and editing. MFM contributed to the study design, literature search, data extraction and synthesis, data interpretation, review, and editing. KK contributed to the study design, literature search, data interpretation, writing, review, and editing. AMR contributed to the study design, data extraction, review and editing. DB contributed to the study design and data interpretation. AC contributed to the study design, data interpretation, review and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA Extended checklist for scoping reviews.
Additional file 2.
MEDLINE (Ovid) search strategy.
Additional file 3.
Characteristics of the included studies.
Rights and permissions
Open Access This article is licensed under the terms of the Creative Commons Attribution 3.0 IGO License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the World Health Organization, provide a link to the Creative Commons licence and indicate if changes were made. The use of the World Health Organization’s name, and the use of the World Health Organization’s logo, shall be subject to a separate written licence agreement between the World Health Organization and the user and is not authorized as part of this CC-IGO licence. Note that the link provided below includes additional terms and conditions of the licence. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/3.0/igo/.
About this article
Cite this article
Gréaux, M., Moro, M.F., Kamenov, K. et al. Health equity for persons with disabilities: a global scoping review on barriers and interventions in healthcare services. Int J Equity Health 22, 236 (2023). https://doi.org/10.1186/s12939-023-02035-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-023-02035-w