Abstract
Background
In 2012, seasonal malaria chemoprevention (SMC) was recommended as policy for malaria control by the World Health Organization (WHO) in areas of highly seasonal malaria transmission across the Sahel sub-region in Africa along with monitoring of drug resistance. We assessed the long-term impact of SMC on Plasmodium falciparum resistance to sulfadoxine-pyrimethamine (SP) and amodiaquine (AQ) over a 3-year period of SMC implementation in the health district of Ouelessebougou, Mali.
Methods
In 8 randomly selected sub-districts of Ouelessebougou, Mali, children aged 0–5 years were randomly selected during cross-sectional surveys at baseline (August 2014) and 1, 2 and 3 years post-SMC, at the beginning and end of the malaria transmission season. Blood smears and blood spots on filter paper were obtained and frequencies of mutation in P. falciparum genes related to resistance to SP and AQ (Pfdhfr, Pfdhps, Pfmdr1, and Pfcrt) were assessed by PCR amplification on individual samples and PCR amplification followed by deep sequencing on pooled (by site and year) samples.
Results
At each survey, approximately 50–100 individual samples were analysed by PCR amplification and a total of 1,164 samples were analysed by deep sequencing with an average read depth of 18,018–36,918 after pooling by site and year. Most molecular markers of resistance did not increase in frequency over the period of study (2014–2016). After 3 years of SMC, the frequencies of Pfdhps 540E, Pfdhps 437G and Pfcrt K76T remained similar compared to baseline (4.0 vs 1.4%, p = 0.41; 74.5 vs 64.6%, p = 0.22; 71.3 vs 67.4%, p = 0.69). Nearly all samples tested carried Pfdhfr 59R, and this proportion remained similar 3 years after SMC implementation (98.8 vs 100%, p = 1). The frequency of Pfmdr1 N86Y increased significantly over time from 5.6% at baseline to 18.6% after 3 years of SMC (p = 0.016). Results of pooled analysis using deep sequencing were consistent with those by individual analysis with standard PCR, but also indicated for the first time the presence of mutations at the Pfdhps A581G allele at a frequency of 11.7% after 2 years of SMC, as well as the Pfdhps I431V allele at frequencies of 1.6–9.3% following 1 and 2 years of SMC, respectively.
Conclusion
Two and 3 years of SMC implementation were associated with increased frequency of the Pfmdr1 N86Y mutation but not Pfdhps 540E, Pfdhps 437G and Pfcrt K76T. The first-time detection of the Pfdhps haplotype bearing the I431V and A581G mutations in Mali, even at low frequency, warrants further long-term surveillance.
Similar content being viewed by others
Background
In 2020, malaria caused an estimated 241 million cases and 627,000 deaths worldwide, with most cases occurring in the WHO African Region (> 90%) [1]. Children under 5 years of age are most affected, representing 77% of all malaria deaths worldwide. In the Sahel sub-region of Africa, most childhood malaria mortality and morbidity occur during the rainy season. Administering effective malaria treatment at monthly intervals during this period has been shown to prevent illness and death from malaria in children. Seasonal malaria chemoprevention (SMC), formerly known as intermittent preventive treatment of malaria in children, is the intermittent administration of full treatment courses of an anti-malarial medicine to children during the malaria season, in areas of highly seasonal transmission. An estimated 25 million children aged 3–59 months could benefit from SMC every year [2] and 62% of eligible children benefited in 2018 [3].
Although the safety and effectiveness of SMC are well-established [4, 5], there have been concerns that long-term use of SMC will increase the spread of sulfadoxine-pyrimethamine (SP)- and amodiaquine (AQ)-resistant parasites. SP-resistant parasites can compromise the drug’s effectiveness as a preventive strategy; mutations such as the Pfdhps 540E substitution can render SP ineffective in intermittent preventive treatment in infants [6], and the Pfdhps 581G substitution (in the presence of the quintuple Pfdhfr and Pfdhps SP-resistant mutations) undermines SP use as prevention in pregnant women [7]. WHO advises that the presence of mutations at codons 437 and 540 of Pfdhps, along with the triple mutation of Pfdhfr (quintuple mutation), significantly predicts SP treatment failure; the Pfdhps 540 mutant is a useful epidemiological marker of the quintuple mutation in Africa [6]. The mutations Pfcrt 76T and Pfmdr1 86Y are associated with AQ resistance [8].
The Pfdhps A581G mutation in the gene encoding P. falciparum dihydropteroate synthetase reduces the efficacy of SP preventive therapy in Malawian pregnant women [9] and no impact of SP in intermittent preventive treatment was found in an area of Tanzania where the frequency of this mutation was high [10]. An increased prevalence of the Pfdhps I431V mutation from 0% in 2003 to 36% in 2015 was reported in Nigeria [11] suggesting that these mutations are emerging and need to be monitored in this context. Increases in prevalence of this mutation from 3 to 6% in children under 5 years of age and 2 to 8% were also reported in the ACCESS-SMC study [12] between 2016 and 2018, which covered 7 Sahelian countries, including Nigeria and Mali.
Several studies have previously evaluated the impact of SMC during one season on resistance to SP and AQ, showing no significant difference in the frequency of SP resistance markers [4, 5, 13]. Two recently published studies have shown that SMC was still effective in clearing malaria parasitaemia and preventing clinical malaria after 3 years [12, 14]. However, one of these studies was conducted in the context of a large clinical trial assessing the effect of the addition of azithromycin on hospital admissions and deaths [14], while the other study (ACCESS-SMC) was in conducted in the context of implementation through the health system [12].
It is unknown whether longer periods of SMC use will accelerate the accumulation of resistant parasites, nor the status of resistance to AQ. Most studies have assessed the effects of SMC with SP plus AQ after just one season, but continuous monitoring is required [15]. This study aimed to assess the impact of SMC on molecular markers of P. falciparum resistance to SP and AQ after implementation over three consecutive malaria transmission seasons in Ouelessebougou, Mali.
Methods
Study site and intervention
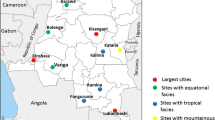
The study was conducted in children aged 3–59 months in the health district of Ouelessebougou (located 80 km south of Bamako, Mali), wherein SMC was implemented progressively across sub-districts. To assess the long-term impact of SMC on resistance to SP and AQ, 8 sub-districts were randomly selected in 2014 from the 13 sub-districts of Ouelessebougou to receive SMC over a period of 3 years: 4 sub-districts in 2014 (year 1); 2 sub-districts in 2015 (year 2); and 2 sub-districts in 2016 (year 3). The larger number of sub-districts in year 1 was justified by the need to cover a larger number of villages in year 1 to determine the optimal delivery method of the strategy [16]. SMC was implemented in the remaining sub-districts of Ouelessebougou in 2016.
Eligible children received three rounds of SMC in 2014 and four rounds in 2015 and 2016. SMC was given at monthly intervals during the peak of the malaria transmission season, starting in August. During each round, children aged 3–11 months received 75 mg of AQ given once daily for 3 days, plus a single dose of 250/12.5 mg of SP; children aged 12–59 months received 150 mg AQ base given once daily for 3 days and a single dose of 500/25 mg of SP. The single dose of SP was given only on the first day, simultaneously with the first dose of AQ. Children were observed for 30 min after drug administration, and the medicine was re-administered if vomiting occurred during this period.
Cross-sectional surveys and sample collection
From 2014 to 2016, at the beginning and the end of each malaria transmission season, a cross-sectional survey was conducted in a random sample of children to assess the prevalence of malaria infection and molecular markers of resistance to SP and AQ. In 2014, 571 and 581 samples were collected at baseline and at the end of malaria season, respectively; in 2015, 429 and 487 samples were collected at the beginning and the end of malaria transmission season, respectively; and in 2016, 747 and 952 samples, at the beginning and the end of malaria transmission season, respectively. Children were selected using simple random sampling from a census list of eligible children in the study areas, to receive SMC during that year except in December 2016 when only children aged 34–59 months were randomly selected to allow assessment of the impact of SMC on malaria immunity [17]. Selected children were examined, and a blood sample was obtained for analysis of molecular markers via blood smear microscopy and dried blood spots (DBS) on filter paper. DBS were sealed in individual plastic bags with desiccant. Baseline samples were collected at the beginning of the malaria transmission season prior the first round of SMC in 2014.
Laboratory analyses
Light microscopy
Thick blood smears were stained with 10% Giemsa for 15 min and read by certified microscopists. Asexual parasites were counted until 200 white blood cells (WBCs) were seen, and blood parasite densities were calculated assuming 8000 WBC/μL. A blood smear was considered to be negative if no parasites were identified in 100 high-power fields. Slides were read by an experienced microscopist blinded to the treatment allocation. Ten per cent of slides were re-read by a blinded expert reader for quality control.
Assessment of molecular markers of Plasmodium falciparum resistance to SP and AQ
Parasites detected by light microscopy in samples collected through the cross-sectional surveys were genotyped as markers of P. falciparum resistance to SP and AQ using two parallel approaches. The first approach used PCR-restriction fragment length polymorphism (RFLP) of specific loci in Pfdhfr 59R, Pfdhps 437G, Pfdhps 540E, Pfmdr1 86Y, and Pfcrt 76T in individual parasites, hereafter ‘individual sample analysis’, according to published methods [18, 19]. The second approach used PCR amplification and deep sequencing of gene fragments including multiple loci in the same genes plus Pfdhfr 51I, Pfdhfr 164L, Pfdhps 431 V, and Pfdhps 581G in pooled parasites, hereafter ‘pooled sample analysis’. Samples were coded and individuals involved in analysis were blinded to groups/time points of the surveys. Samples were analysed on an Ion Torrent platform as previously described [20].
Individual sample analysis
DNA was extracted from selected DBS on filter paper (3 M Whatman) as previously described [14, 18]. Assay of drug resistance markers was performed by nested PCR and/or PCR–RFLP [18, 19]. Drug resistance markers tested for this study were Pfdhfr 59R for pyrimethamine, Pfdhps 437G and Pfdhps 540E for sulfadoxine; Pfcrt 76T and Pfmdr1 86Y for amodiaquine. Results were classified as wild type, mutant or mixed (when both alleles were present).
Pooled sample analysis
gDNA extracts from microscopy-positive samples were pooled by year and by site (sub-district) with equal volumes. From these pooled gDNA extracts, relevant drug-resistance loci were amplified in Pfcrt, Pfmdr1, Pfdhfr and Pfdhps using separate reactions of a single-round of PCR (Table 1 for primers), and cleaned, pooled and sequenced libraries on an IonTorrent platform as previously described [20]. Fastq files were processed, quality-filtered, aligned to reference sequences of parasite strain 3D7 using Bowtie2, and assessed at variant loci of interest in Galaxy [21]. The output was the proportion of reads covering each locus of interest that harboured a nucleotide substitution encoding a drug-resistance mutation. The same amplification and read-processing methods were applied to the sub-set of samples that were individually deep-sequenced at Pfdhps. Two separate fragments were amplified and sequenced for both Pfdhfr and Pfdhps owing to length constraints for sequencing reads.
Data management and statistical analysis
Individual data were entered and verified using DataFax and exported to Stata (version 14, Houston, TX, USA) for analysis. Samples that were individually genotyped using PCR–RFLP with evidence of mixed infection (wild type and mutant) were categorized as mutant. At the beginning and end of the transmission season, proportions of Pfdhfr 59R, Pfdhps 437G, Pfdhps 540E, Pfmdr1 86Y, and Pfcrt K76T genotypes were determined and compared using Chi square or Fisher exact tests as appropriate.
Results
Study population
Demographic characteristics of the study population and malaria prevalence are summarized in Table 2. There was no difference in gender (p = 0.20) or age distribution (p = 0.48) of children surveyed at different time points, except at the 2016 end-of-transmission survey when older children were selected (p < 0.001). Prevalence of malaria infection was significantly higher in children surveyed at 2014 baseline and the 2016 end-of-transmission (p < 0.001).
Molecular markers of resistance to SP and AQ using individual sample analysis
The frequencies of molecular markers associated with resistance to SP and AQ at baseline and post-SMC are summarized in Table 3. The frequency of Pfdhps K540E mutation was low at baseline (4.0%) and did not vary over time with SMC implementation (p = 0.63). The frequency of Pfdhps 437G was significantly lower after 2 years of SMC at the beginning of the season compared to baseline (74.5 to 31.6%, p < 0.001), and increased to a level similar to baseline by the end-of-season survey after 3 years of SMC (74.5 vs 64.6%, p = 0.22). Nearly all samples tested carried Pfdhfr C59R (98.8%) and this proportion remained similar 2 and 3 years after SMC implementation. The frequency of Pfmdr1 N86Y increased significantly over time from 5.6% at baseline to 18.6% after 3 years of SMC (p = 0.016), while the frequency of AQ resistance marker Pfcrt K76T did not vary significantly (p = 0.27) over time after SMC implementation.
Resistance markers by deep sequencing
A total of 1,164 DBS samples from all time points were analysed by deep sequencing; after pooling by site and year; for each pool an average read depth of 18,018 at Pfdhfr, 29,789 at Pfdhps, and 36,918 at Pfmdr1 loci was obtained.
At baseline, frequencies of Pfdhfr 51I and Pfdhfr 59R were vhigh 89.1% and 99.9% respectively and remained high in sites after 1, 2 and 3 years of SMC (Fig. 1). No Pfdhfr 164L frequencies exceeding of 1% in any year or site were observed.
Change in frequency of drug resistance alleles from baseline following 1, 2 or 3 years of SMC administration in pooled parasites by study site. Allele frequencies from the same study site in successive years are presented, with frequencies indicating the proportion of sequencing reads in the year and site that harboured the indicated allele at dhfr (A), dhps (B), and pfcrt and pfmdr-1 (C). Allele frequencies at baseline were estimated from parasites collected prior to SMC implementation in 4 sites and aggregated
The baseline frequency of Pfdhps 437G (66.7%) was similar to those after 1, 2 or 3 years of SMC, which ranged from 30.1 to 86.4% without clear evidence of increases over time. Pfdhps K540E frequency was low at baseline (1.3%) and remained low following SMC, reaching a highest community frequency of 17.8% 1 year post-SMC introduction. The Pfdhps A581G mutation was observed in only two communities at frequencies of 9.6 and 11.7% both after 2 years of SMC. Similarly, the Pfdhps I431V allele was observed in only three communities at frequencies of 9.3, 7.5 and 1.6%, after 2 or 1 year of SMC.
In contrast, the low baseline frequency of Pfmdr1-86Y allele (6.1%) was exceeded by all sites in most years following SMC, with frequencies ranging from 3.8 to 54.9%. Because measurable frequencies were observed of Pfdhps mutations I431V and A581G in separate pools of 2015 and 2016, the 78 individual parasites in these two pools were deep sequenced. Genotyping at each locus was successful in 74 parasites, for which a median depth was observed of 34,796 (Pfdhps I431V) and 20,032 (Pfdhps A581G) reads. Nine of these (12%) harboured the Pfdhps I431V mutation, and 7 of these 9 (78%) also harboured the Pfdhps A581G mutation. The frequencies of each mutation were highly correlated within each infection (correlation coefficient = 0.99). Two parasites with the Pfdhps I431V mutation lacked the Pfdhps A581G allele, and there were no parasites with the Pfdhps A581G mutation that lacked the Pfdhps I431V mutation.
Discussion
An updated systematic review to map SP-resistant P. falciparum in 294 surveys of infected humans across Africa from 2004 to 2016 has implicated ongoing SP drug pressure, which may in part arise from intermittent preventive treatment of malaria in pregnancy (IPTp) and SMC programmes [22]. Whether implementing SMC over a long period of time increases the frequency of drug resistance markers, thereby decreasing the effectiveness of this strategy, has always been a concern. Several studies have shown a limited impact of SMC on the prevalence of molecular markers of resistance to SP-AQ in children before and after receiving SMC drugs during one season [4, 5, 13]. The current study evaluated the effect of three consecutive seasons of SMC implementation on molecular markers in children using PCR amplification on individual samples, as well as on pools of all samples by year with deep sequencing.
In the individual sample analysis, SMC over three consecutive malaria transmission seasons was not associated with an increase in frequency of Pfdhps 540E and Pfdhps 437G mutations, which are most commonly used for monitoring resistance of P. falciparum to sulfadoxine. The frequency of Pfdhps 540E mutation remained far below the 50% threshold recommended for SP in intermittent preventive treatment in children [6]. Nearly all samples (98.8%) carried the Pfdhfr C59R mutation at baseline, making this mutation no longer relevant in monitoring resistance to pyrimethamine. These results are consistent with those obtained at other sites in Mali and other countries in the Sahel [12, 14]. In both those studies, as in this study, the frequency of Pfdhps 540E mutation remained low in children under 5 years of age who received SMC for 3 years, as well as those in older age groups who did not receive SMC. Both studies showed that SP + AQ was highly effective against clinical malaria or asymptomatic malaria parasitaemia.
These data are consistent with those reported in previous trials in Mali and in Burkina Faso in 2008, with no significant increase in frequency of these markers versus the control group after 1 year of SMC implementation [4, 5, 13]. The data support a systematic analysis of national trends in P. falciparum resistance to SP in Africa, where the frequency of Pfdhps 540E mutation was 3.5% in 2015 in Mali [23]. In Senegal, a study indicated that the overall proportion of children carrying parasites with these mutations was lower in SMC areas than in areas where SMC had not been implemented [24].
The frequency of the Pfmdr1 86Y mutation, associated with AQ resistance in children carrying P. falciparum parasites, was low (5.6%) at baseline but increased significantly after 3 seasons of SMC implementation (to 18.6%). In a trial of SMC with azithromycin [14], the frequency of Pfmdr1 86Y increased in Bougouni, Mali from 5 to 11% between 2014 and 2016, while decreasing from 20 to 10% in Hounde, Burkina Faso. In the ACCESS-SMC study [12], the prevalence of this mutation did not increase after 3 years of SMC.
By deep sequencing, Pfdhfr mutations at codons N51I and C59R at baseline were close to 100% and remained at similarly high levels after 2 and 3 years of SMC, indicating that these mutations are no longer useful for monitoring SP resistance in the area. Similar frequencies of these mutations were also reported in the ACCESS-SMC study [12] in 7 Sahelian countries where SMC is largely deployed but also in Kenya [25] where resistance to SP was high.
As seen in the ACCESS-SMC study [12], Pfdhps I431V and A581G mutations were detected in the current study population that received SMC with SP plus AQ over 3 malaria seasons. The frequencies of mutations in codons A581G and I431V were low (0.0–4.2 for A581G and 0.2–3.2 for I431V) and consistent with reports in Niger [26] and the ACCESS-SMC study [12]. The clinical or parasitological significance of the I431V mutation is unknown, but the A581G mutation, when present along with quintuple SP-resistance mutations on the Pfdhfr and Pfdhps genes, has been associated with reduced effectiveness of SP for chemoprevention in pregnant women in East Africa, where an increase of Pfdhps S436H was reported recently [25]. Its effect in West Africa may be different, given that these data suggest it occurs on a distinct haplotype that harbours the I431V mutation but lacks the K540E mutation. The appearance of this I/K/G Pfdhps haplotype across codons I431V, K540E and A581G following SMC implementation suggests selection by SP, although the failure to detect this in any pools the following year may indicate weak selection, as has been the case for other Pfdhps resistance haplotypes. Nevertheless, the findings highlight that codons I431V and A581G should be incorporated into routine molecular surveillance of Pfdhps loci in West Africa, through which the clinical significance of these mutations can be understood. Further long-term surveillance of molecular markers should become a routine practice in Mali and other countries implementing SMC.
Limitations of this study include the relatively small number of samples analysed individually by PCR. The strengths include deep sequencing genotyping on a large number of samples, 3-year capture of children receiving SMC, and blinded analysis of the samples.
Conclusion
Two and 3 years of SMC implementation were not associated with increased frequencies of molecular markers of SP and AQ resistance. The detection of the Pfdhps haplotype bearing I431V and A581G mutations for the first time in Mali, even at a low frequency, warrants further long-term surveillance.
Availability of data and materials
The corresponding author had full access to all the data in the study and data are available at request to the corresponding author.
Abbreviations
- AQ:
-
Amodiaquine
- CRT:
-
Chloroquine resistance transporter
- DBS:
-
Dried blood spots
- DHFR:
-
Dihydrofolate reductase
- DHPS:
-
Dihydropteroate synthase
- DNA:
-
Deoxyribonucleic acid
- MDR1:
-
Multidrug resistance 1
- PCR:
-
Protein chain reaction
- RFLP:
-
Restriction fragment length polymorphism
- SMC:
-
Seasonal malaria chemoprevention
- SP:
-
Sulfadoxine-pyrimethamine
- WBC:
-
White blood cells
References
WHO. World malaria report 2021. Geneva: World Health Organization, 2021. https://www.who.int/malaria/media/world-malaria-report-2018/en/. Accessed 15 May 2021.
WHO. Seasonal malaria chemoprevention (SMC) for Plasmodium falciparum malaria control in highly seasonal transmission areas of the Sahel sub-region in Africa. Geneva: World Health Organization; 2012.
WHO. World malaria report 2019. Geneva: World Health Organization, 2019. https://www.who.int/publications/i/item/world-malaria-report-2019. Accessed 15 May 2021.
Dicko A, Diallo AI, Tembine I, Dicko Y, Dara N, Sidibe Y, et al. Intermittent preventive treatment of malaria provides substantial protection against malaria in children already protected by an insecticide-treated bednet in Mali: a randomised, double-blind, placebo-controlled trial. PLoS Med. 2011;8: e1000407.
Konate AT, Yaro JB, Ouedraogo AZ, Diarra A, Gansane A, Soulama I, et al. Intermittent preventive treatment of malaria provides substantial protection against malaria in children already protected by an insecticide-treated bednet in Burkina Faso: a randomised, double-blind, placebo-controlled trial. PLoS Med. 2011;8: e1000408.
WHO. Policy recommendation on intermittent preventive treatment during infancy with sulphadoxine-pyrimethamine (IPTi-SP) for Plasmodium falciparum malaria control in Africa. Geneva: World Health Organization; 2010. https://www.who.int/malaria/news/WHO_policy_recommendation_IPTi_032010.pdf?ua=1. Accessed 15 May 2021.
van Eijk AM, Larsen DA, Kayentao K, Koshy G, Slaughter DEC, Roper C, et al. Effect of Plasmodium falciparum sulfadoxine-pyrimethamine resistance on the effectiveness of intermittent preventive therapy for malaria in pregnancy in Africa: a systematic review and meta-analysis. Lancet Infect Dis. 2019;19:546–56.
WHO. World malaria report. Geneva: World Health Organization; 2020.
Gutman J, Kalilani L, Taylor S, Zhou Z, Wiegand RE, Thwai KL, et al. The A581G mutation in the gene encoding Plasmodium falciparum dihydropteroate synthetase reduces the effectiveness of sulfadoxine-pyrimethamine preventive therapy in Malawian pregnant women. J Infect Dis. 2015;211:1997–2005.
Roh ME, ter Kuile FO, Rerolle F, Glymour MM, Shiboski S, Gosling R, et al. Overall, anti-malarial, and non-malarial effect of intermittent preventive treatment during pregnancy with sulfadoxine-pyrimethamine on birthweight: a mediation analysis. Lancet Glob Health. 2020;8:e942–53.
Oguike MC, Falade CO, Shu E, Enato IG, Watila I, Baba ES, et al. Molecular determinants of sulfadoxine-pyrimethamine resistance in Plasmodium falciparum in Nigeria and the regional emergence of dhps 431V. Int J Parasitol Drugs Drug Resist. 2016;6:220–9.
ACCESS-SMC Partnership. Effectiveness of seasonal malaria chemoprevention at scale in west and central Africa: an observational study. Lancet. 2020;396:1829–40.
Diawara F, Steinhardt LC, Mahamar A, Traore T, Kone DT, Diawara H, et al. Measuring the impact of seasonal malaria chemoprevention as part of routine malaria control in Kita, Mali. Malar J. 2017;16:325.
Cairns ME, Sagara I, Zongo I, Kuepfer I, Thera I, Nikiema F, et al. Evaluation of seasonal malaria chemoprevention in two areas of intense seasonal malaria transmission: Secondary analysis of a household-randomised, placebo-controlled trial in Houndé district, Burkina Faso and Bougouni district, Mali. PLoS Med. 2020;17: e1003214.
McCollum AM, Schneider KA, Griffing SM, Zhou Z, Kariuki S, ter Kuile F, et al. Differences in selective pressure on dhps and dhfr drug resistant mutations in western Kenya. Malar J. 2012;11:77.
Barry A, Issiaka D, Traore T, Mahamar A, Diarra B, Sagara I, et al. Optimal mode for delivery of seasonal malaria chemoprevention in Ouelessebougou, Mali: a cluster randomized trial. PLoS ONE. 2018;13: e0193296.
Mahamar A, Issiaka D, Barry A, Attaher O, Dembele AB, Traore T, et al. Effect of seasonal malaria chemoprevention on the acquisition of antibodies to Plasmodium falciparum antigens in Ouelessebougou, Mali. Malar J. 2017;16:289.
Plowe CV, Djimde A, Bouare M, Doumbo O, Wellems TE. Pyrimethamine and proguanil resistance-conferring mutations in Plasmodium falciparum dihydrofolate reductase: polymerase chain reaction methods for surveillance in Africa. Am J Trop Med Hyg. 1995;52:565–8.
Djimde A, Doumbo OK, Cortese JF, Kayentao K, Doumbo S, Diourté Y, et al. A molecular marker for chloroquine-resistant falciparum malaria. N Engl J Med. 2001;344:257–63.
Levitt B, Obala A, Langdon S, Corcoran D, O’Meara WP, Taylor SM. Overlap extension barcoding for the next generation sequencing and genotyping of Plasmodium falciparum in individual patients in Western Kenya. Sci Rep. 2017;7:41108.
Afgan E, Baker D, Batut B, van den Beek M, Bouvier D, Cech M, et al. The Galaxy platform for accessible, reproducible and collaborative biomedical analyses: 2018 update. Nucleic Acids Res. 2018;46:W537–44.
Okell LC, Griffin JT, Roper C. Mapping sulphadoxine-pyrimethamine-resistant Plasmodium falciparum malaria in infected humans and in parasite populations in Africa. Sci Rep. 2017;7:7389.
Amimo F, Lambert B, Magit A, Sacarlal J, Hashizume M, Shibuya K. Plasmodium falciparum resistance to sulfadoxine-pyrimethamine in Africa: a systematic analysis of national trends. BMJ Global Health. 2020;5: e003217.
Cissé B, Ba EH, Sokhna C, NDiaye JL, Gomis JF, Dial Y, et al. Effectiveness of seasonal malaria chemoprevention in children under ten years of age in Senegal: a stepped-wedge cluster-randomised trial. PLoS Med. 2016;13: e1002175.
Pacheco MA, Schneider KA, Cheng Q, Munde EO, Ndege C, Onyango C, et al. Changes in the frequencies of Plasmodium falciparum dhps and dhfr drug-resistant mutations in children from Western Kenya from 2005 to 2018: the rise of Pfdhps S436H. Malar J. 2020;19:378.
Grais RF, Laminou IM, Woi-Messe L, Makarimi R, Bouriema SH, Langendorf C, et al. Molecular markers of resistance to amodiaquine plus sulfadoxine-pyrimethamine in an area with seasonal malaria chemoprevention in south central Niger. Malar J. 2018;17:98.
Acknowledgements
We are very grateful to Dr Cameron Bess (USAID, Washington office) and Dr Robert Gasior (National Academics of Sciences) and the staff at the USAID office in Bamako (Dr Jules Mihigo, Dr Boubacar Sadou, Dr Bijou Muhura) for their support to the project, to the research team, to the participants for their time, and to the National Malaria Control Programme and the health staff of the districts of Ouelessebougou for their cooperation and support. We thank the Mali Service Centre for providing administrative support to the project, Dr Richard Sakai and Souleymane Karambe for logistical support. Malaria Research and Training Centre of FAPH-FMOS/USTTB is part of the EDCTP2 programme supported by the European Union. We thank J. Patrick Gorres (LMIV, NIAID, NIH) for editing the manuscript.
Funding
The implementation of SMC was funded by the US President’s Malaria Initiative through the USAID Partnerships for Enhanced Engagement in Research programme implemented by the National Academies of Sciences, Engineering, and Medicine (Subgrant Contract # 2000004198) and the Government of Mali. Additional support came from the Intramural Research Program of NIAID-NIH. Parasite genotyping was supported by the National Institutes of Health, National Center for Advancing Translational Sciences (grant number UL1TR001117 to S. M. T.). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: AM, PED, MF, SMT, ADi. Formal analysis: AM, ADj, MF, SMT, ADi. Investigation: AM, AB, DI, ABD, MBK, OA, BND. Supervision: SMT, IS, Adj, PED, MF, ADi. Validation: AM, KMN, BL, BF, AT. Writing—original draft: AM. Writing—review, editing and approval of the manuscript: AM, KMS, BL, BF, AT, AB, DI, ABD, MBK, OA, BND, IS, ADj, PED, MF, SMT, ADi. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol (Number 2014/61/CE/FMPOS) and amendments were reviewed and approved by the Ethics Committee of the Faculty of Medicine, Pharmacy and Dentistry of the University of Bamako. Written informed consent from parents/guardians was obtained for all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mahamar, A., Sumner, K.M., Levitt, B. et al. Effect of three years’ seasonal malaria chemoprevention on molecular markers of resistance of Plasmodium falciparum to sulfadoxine-pyrimethamine and amodiaquine in Ouelessebougou, Mali. Malar J 21, 39 (2022). https://doi.org/10.1186/s12936-022-04059-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04059-z