Abstract
Background
Therapeutic efficacy studies in uncomplicated Plasmodium falciparum malaria are confounded by new infections, which constitute competing risk events since they can potentially preclude/pre-empt the detection of subsequent recrudescence of persistent, sub-microscopic primary infections.
Methods
Antimalarial studies typically report the risk of recrudescence derived using the Kaplan–Meier (K–M) method, which considers new infections acquired during the follow-up period as censored. Cumulative Incidence Function (CIF) provides an alternative approach for handling new infections, which accounts for them as a competing risk event. The complement of the estimate derived using the K–M method (1 minus K–M), and the CIF were used to derive the risk of recrudescence at the end of the follow-up period using data from studies collated in the WorldWide Antimalarial Resistance Network data repository. Absolute differences in the failure estimates derived using these two methods were quantified. In comparative studies, the equality of two K–M curves was assessed using the log-rank test, and the equality of CIFs using Gray’s k-sample test (both at 5% level of significance). Two different regression modelling strategies for recrudescence were considered: cause-specific Cox model and Fine and Gray’s sub-distributional hazard model.
Results
Data were available from 92 studies (233 treatment arms, 31,379 patients) conducted between 1996 and 2014. At the end of follow-up, the median absolute overestimation in the estimated risk of cumulative recrudescence by using 1 minus K–M approach was 0.04% (interquartile range (IQR): 0.00–0.27%, Range: 0.00–3.60%). The overestimation was correlated positively with the proportion of patients with recrudescence [Pearson’s correlation coefficient (ρ): 0.38, 95% Confidence Interval (CI) 0.30–0.46] or new infection [ρ: 0.43; 95% CI 0.35–0.54]. In three study arms, the point estimates of failure were greater than 10% (the WHO threshold for withdrawing antimalarials) when the K–M method was used, but remained below 10% when using the CIF approach, but the 95% confidence interval included this threshold.
Conclusions
The 1 minus K–M method resulted in a marginal overestimation of recrudescence that became increasingly pronounced as antimalarial efficacy declined, particularly when the observed proportion of new infection was high. The CIF approach provides an alternative approach for derivation of failure estimates in antimalarial trials, particularly in high transmission settings.
Similar content being viewed by others
Background
A competing risk is an event which precludes the occurrence of the primary event of interest [1]. The primary endpoint in therapeutic efficacy studies in uncomplicated Plasmodium falciparum malaria is recurrence of the parasite during the study follow-up which caused the original infection (recrudescence). Malaria recurrence may also be caused by a heterologous parasite, which can be either a newly acquired infection with P. falciparum, or another species of Plasmodium. In certain scenarios, such as when the parasite load of a newly acquired infection outnumbers the low level of parasitaemia of an existing infection, the recrudescent parasites may not be detected (Fig. 1a). In such a scenario, a new infection can pre-empt the patency of a recrudescent infection thereby constituting a competing risk event (Table 1).
Situational competitiveness of newly emergent infections. Adapted from White-2002 [44]. The blue line represents a hypothetical drug concentration of partner component, the green and red lines represent scenarios for parasite burden versus time profiles following treatment for an infection where all the parasites are completely killed resulting in cure (green) and an infection where parasites are initially killed by high drug levels but with drug levels below the minimum inhibitory concentration (MIC), net parasite growth results in subsequent recrudescence (red). The orange line represents parasite-time profiles for a new infection. The left y-axis is for parasite density, and the right y-axis shows drug levels at hypothetical units. The vertical dotted line is the administrative end of the study follow-up. The horizontal dotted line represents the microscopic limit of detection for parasites. a Parasite population from a new inoculation out-competes the parasite population which caused the disease thus precluding recrudescence. In this situation, new infection is a biologically competing risk event. b In this situation new infection can be thought of as biologically competing risk event which doesn’t prevent recrudescence being observed. c The parasite population which caused the disease is completely eliminated. Here, new infection is not a competing event. d In this situation, the parasite population which caused the disease and which is derived from a novel inoculation appear at the same time
The Kaplan–Meier (K–M) survival analysis is currently the approach recommended by the World Health Organization (WHO) for deriving antimalarial efficacy, where a competing risk event of a new infection is considered as a censored observation on the day of occurrence [2]. The complement of K–M estimate (1 minus K–M) is frequently reported in standalone efficacy studies as the WHO recommends replacing an existing treatment with an alternative regimen if the derived estimate of cumulative failure exceeds 10%. Several studies in clinical and statistical literature has shown that the 1 minus K–M approach provides an upwards biased estimate of the cumulative risk for the event of interest in the presence of competing risk events [1, 3,4,5,6]. In a re-analysis of an antimalarial efficacy trial from Uganda, it was demonstrated that the derived estimate of cumulative recrudescence using the 1 minus K–M approach can lead to a counter-intuitive scenario where the sum of the individual risk of recurrence for recrudescence and new infection is greater than for the composite endpoint of overall recurrence (see Figure 4 in [7]). An alternative approach for deriving failure estimate is to use the Cumulative Incidence Function (CIF) [8] (see Additional file 1: Section 1).
The presence of competing risk events can have further implications for comparative drug trials and regression modelling. First, comparative antimalarial trials utilize the widely used log-rank test to compare the efficacy between two drugs. An alternative approach, which compares the difference in cumulative risk between two groups by accounting for competing risk events, is the Gray’s k-sample test [9] (see Additional file 1: Section 2). Simulation studies have reported different performances of these two approaches depending on the underlying effect of the drug on the primary event of interest and on competing risk events [5, 10]. Second, in the presence of competing risk events, regression modelling can be carried out either using the Cox’s proportional hazard model or using the Fine and Gray’s model [11]. The former is based on modelling of the cause-specific hazard function whereas the latter is based on the modelling of sub-distribution hazard function. The differences between the cause-specific and sub-distribution hazard functions, and the underlying regression models are explained in Additional file 1: Sections 2, 3 and 4.
The application of competing risk survival analysis approach has gathered little attention in the antimalarial literature [7, 12]. This research aimed to address this research gap and there were three specific objectives:
-
i.
To investigate the influence of competing risk events on the derived estimate of polymerase chain reaction (PCR) confirmed recrudescence in a stand-alone trial;
-
ii.
To investigate the influence of competing risk events on the estimation of comparative efficacy between antimalarial drugs;
-
iii.
To demonstrate regression modelling approaches in the presence of competing risk events.
Methods
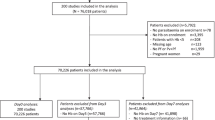
Identification of studies for potential inclusion
The WorldWide Antimalarial Resistance Network (WWARN) repository contains a large collection of standardized data on antimalarial drugs [13]. Studies in the WWARN data repository were eligible for inclusion in the current analysis, if the data were from prospective clinical efficacy studies of uncomplicated P. falciparum (alone or mixed infections with Plasmodium vivax) in which patients were treated with one of the following fixed-dose regimens: artemether–lumefantrine (AL), dihydroartemisinin–piperaquine (DP), artesunate–amodiaquine (ASAQ), or artesunate–mefloquine (ASMQ). All studies also had to have applied molecular PCR genotyping to distinguish recrudescence from new infection. Studies on prophylactic use of antimalarials, severe malaria, pregnant women, patients with hyperparasitaemia, healthy volunteers, and travellers were excluded. Treatment outcomes were generated based on the definitions outlined in the WWARN Data Management and Statistical Analysis Plan [14].
Statistical analyses
Derivation of cumulative failure estimates in standalone studies
The estimate of cumulative recrudescence at the end of study follow-up was derived using two methods: (i) the Kaplan–Meier method and (ii) the Cumulative Incidence Function (CIF) estimator (p. 255 of [15]). New infections and indeterminate outcomes were considered as censored at the time of their occurrence in the K–M approach whereas they were considered as different categories of competing events in the CIF approach. The difference in derived estimates of PCR confirmed recrudescence using these two different approaches was calculated and expressed in absolute scale. The effect of length of study follow-up, observed proportion of events and competing events per arm on the magnitude of the difference in the derived estimates between the two approaches was explored.
Impact of competing risk events in comparative efficacy studies
For comparative efficacy studies where the interest lies in establishing the difference between two drugs in terms of primary endpoint of interest (recrudescence), two different approaches were used: (i) the log-rank test to compare the equality of the K–M curves, and (ii) Gray’s k-sample test to compare the equality of the CIFs [16]. In the absence of competing risk events, the result of Gray’s k-sample test will be identical to that derived by the log-rank test [17]. In the log-rank test, new infections and indeterminate recurrence were considered as censored.
Regression models for recrudescence and new infection
In the presence of competing risk events, regression modelling can be carried out either on the cause-specific hazard function (using Cox proportional hazards model) or the sub-distribution hazard function (using Fine and Gray model) (see Additional file 1: Sections 3 and 4). A subset of data from a large multi-centre study (The 4ABC Trial [18]), which enrolled children aged less than 5 years in Africa was used to illustrate the two regression approaches in the presence of competing risk events.
The regression parameters of the Fine and Gray model were expressed as a sub-distribution hazard ratio (sdHR), and the output of the cause-specific Cox model as a cause-specific hazard ratio (csHR). Regression models were fitted without variable selection as the aim was to use the fitted model for risk prediction (rather than identification of putative factors) using the known confounders: age, baseline parasitaemia, and treatment regimen. The same set of covariates was used in models for recrudescence and new infection as recommended by Marubini and Valsechhi (p. 347) [19]. The fitted regression models were then used to estimate the predicted risk of recrudescence on day 28 (Additional file 1: Section 5).
Software
All the analyses were carried out using R software (Version 3.2.4) [20]. The log-rank test was carried out using the survdiff function in the survival package and Gray’s k-sample test was performed using the cuminc function in the cmprsk package.
Results
Characteristics of the studies and patients included
Individual patient data were available from 92 studies (31,507 patients) carried out in 169 trial sites with a total of 233 treatment arms (see Additional file 2 for details of the studies included). A total 186 arms (79.8%) were from Africa, 45 (19.3%) from Asia and 2 (0.85%) were from South America. The duration of follow-up was 28 days in 120 (51.5%) treatment arms, 42 days in 76 (32.6%) arms, and 63 days in 37 (15.9%) arms. Overall, 16,313 (51.9%) patients were treated with AL, 9064 (28.9%) with DP, 4782 (15.2%) with ASAQ and 1220 (3.9%) with ASMQ. Baseline characteristics of the patients are presented in Table 2.
Study outcomes
In Africa, a total of 4534 (18.8%) recurrent infections were documented, of which 553 (2.3%) were recrudescent infections; the proportion of recrudescent failures was 2.5% (356/14,027) for AL, 2.3% (112/4862) for DP, 1.6% (70/4482) for ASAQ and 1.9% (15/810) for ASMQ (Additional file 3: Section 1). In Asia, 8.5% (579/6787) of patients had recurrent infection, of which 126 (21.8%) were recrudescences. The proportion of patients with recrudescences in Asia was 2.7% (58/2127) for AL, 5.3% (16/300) for ASAQ, 3.2% (13/410) for ASMQ and 1.0% for DP (39/3950). In South America, there were 3 recrudescences (0.7%) and 4 new infections (1.0%). Of the 233 treatment arms, 83 (35.6%) arms reported no recrudescent infections, and 199 (85.4%) arms had at least one new infection observed. The observed proportion for the different event types are presented in Fig. 2.
Standalone efficacy studies
Risk of Plasmodium falciparum recrudescence
In 91 arms (39%), there was either absence of recurrence or only recrudescence or new infections were observed. In these arms, the failure estimates derived from both methods were identical. In the remaining 142 arms (61%), the 1 minus K–M method was associated with a marginal overestimation of the risk of PCR confirmed recrudescence compared to the CIF by a median of 0.04% [IQR: 0.00–0.27%; Range: 0.00–3.60%] (Fig. 3, upper panel). The degree of overestimation was progressively larger with increasing study follow-up duration; the median overestimation being 0.006% [IQR: 0.00–0.07%; Range: 0.00–2.54%] on day 28, 0.15% [IQR: 0.00–0.57%; Range: 0.00–3.23%] on day 42, and 0.56% [IQR: 0.11–1.12%; Range: 0.00–3.60%] on day 63 (Table 3). The magnitude of overestimation also correlated with the observed proportion of new infections [Pearson’s correlation coefficient: 0.43; 95% CI 0.35–0.54] and the observed proportion of recrudescences [Pearson’s correlation coefficient: 0.38, 95% CI 0.30–0.46] (Fig. 3, Table 3).
The overestimation of derived failure by 1 minus Kaplan–Meier method compared to the Cumulative Incidence Function. The overestimation \(\left( {\hat{F}_{KM} \left( t \right) - \hat{F}_{CIF} \left( t \right)} \right)\) of cumulative recrudescence (top panel) and new infection (bottom panel) by using the Kaplan–Meier method plotted against observed proportion of recrudescence and proportion of new infections respectively. Estimates presented are at the end of the study follow-up. The grey trend line is a smoothed estimator obtained from local polynomial regression fitting, shown together with 95% confidence interval (outer dotted lines) for the overall data. AL artemether–lumefantrine, ASAQ artesunate–amodiaquine, DP dihydroartemisinin–piperaquine, ASMQ artesunate–mefloquine. Data are shown from the study arms where at least one recrudescence and at least one competing risk event were observed and from those arms where the number of patients at risk > 25 on the last day of the study follow-up
The maximum overestimation was 3.6%, which occurred in an artesunate–mefloquine arm in Balonghin site in Burkina Faso (n = 66), an area of high transmission [21]. In this arm, the day 63 failure estimate derived using the K–M method was 20.0% [95% CI 0.0–55.1] and the corresponding CIF estimate was 16.4% [95% CI 0.0–48.6]. In 9.0% (21/233) of the treatment arms, the overestimation was greater than 1%, in 4.3% (10/233) this was greater than 2%, and in 2.6% (6/233) the difference was greater than 3%. All of the 21 study sites where the overestimation exceeded 1% were from Africa except one from Papua New Guinea, where 51% of patients with parasite recurrence were due to to P. vivax.
Study sites where estimate of PCR-confirmed recrudescence exceeded 10% using complement of K–M
In three (1.3%) study arms, the estimated cumulative risk of recrudescence exceeded 10% (the WHO threshold for withdrawing first line therapy) based on the K–M method, but the CIF estimates were all less than 10% (Table 4). Similarly, in 9 (3.9%) study arms, the estimated failures were greater than 5% (the WHO threshold required to meet for introducing a regimen as a first line therapy) using the K–M method, all of which were less than 5% using the CIF.
Risk of Plasmodium falciparum new infection
The median overestimation of the cumulative risk of new P. falciparum infections during the follow-up period using the K–M method (which considered recrudescences as censored) compared to the Cumulative Incidence Function was 0.39% [IQR: 0.08–1.10%; Range: 0.00–10.60%]. The overestimation progressively increased with the follow-up duration, which was 0.10% on day 28, 0.67% on day 42, and 1.40% on day 63 (Fig. 3; lower panels). The overestimation increased with increasing proportion of patients with new infections and recrudescences observed in a study. The maximum overestimation was 10.6%, observed in a study with artemether–lumefantrine (n = 50) carried out in Tanzania. In this study arm, there were 9 (18%) recrudescences, and 29 (58%) new infections. Using the 1 minus K–M method, the risk of new infection on day 42 was 68.6% [95% CI 54.3–83.1] and this was 58.0% [95% CI 44.2–71.7] using the CIF method.
Comparative efficacy studies
The results of the comparative efficacy studies are presented in Additional file 3: Section 2. There was no difference in the overall conclusion derived (at 5% level of significance) using the two approaches for testing for equality between the drug regimens using the log-rank test and Gray’s k-sample test.
Regression models for time to recrudescence
Data from 810 children enrolled in Burkina Faso (a subset of the The 4ABC Trial [18]) treated with artemether–lumefantrine (AL) (n = 294), artesunate–amodiaquine (ASAQ) (n = 295) and dihydroartemisinin–piperaquine (DP) (n = 221) were used to illustrate the regression modelling approaches in the presence of competing risk events. The observed proportion of patients with recrudescences were 3.2% in the DP arm, 8.2% in the AL arm, and 3.1% in the ASAQ arm, while the respective proportion for new infections were 10.0%, 48.3%, and 25.1% (Table 5). In a multivariable model for recrudescence (which included age, baseline parasitaemia and treatment regimen), age and baseline parasitaemia did not reach conventional statistical significance for recrudescence, neither in the cause-specific hazard model nor in the sub-distribution hazard model (P-value > 0.05). Treatment with AL (relative to DP) was associated with increased cause-specific hazard and increased sub-distribution hazard of recrudescence (csHR = 4.02 [95% CI 1.72–9.43]; sdHR = 2.85 [95% CI 1.24–6.57]).
The regression models presented in Table 5 were used for predicting the risk of recrudescence on day 28 for a patient aged 3 years old with an initial parasite load of 100,000/µL. For the DP regimen, the predicted risk for a patient with this covariate profile was 4.3% using the cause-specific Cox proportional hazard model, and 3.9% using the sub-distribution hazard model (Fig. 4). For the AL regimen, the predicted risks were 16.2% and 10.7% using the cause-specific and sub-distribution hazard models respectively. For ASAQ, the estimates of predicted risks were 4.8% using the cause-specific Cox model and 3.9% using the Fine and Gray’s sub-distribution hazard model.
Predicted risk of recrudescence from cause-specific Cox model and sub-distribution hazard model. The graph was generated using the regression coefficients presented in Table 5 and the estimate of baseline hazard obtained from the respective sub-distribution and cause-specific hazard model (for a 3 year old child). The cumulative baseline sub-distribution hazard on day 28 from Fine and Gray’s model was 0.006; the cumulative baseline hazard on day 28 from the cause-specific Cox model was 0.003. The vertical dotted line represents the parasitaemia of 100,000/µL for the child described in the main text. On day 28, the predicted risk of recrudescence for this patient was 16.15%, 4.76% and 4.28% using the cause-specific Cox model. The corresponding figures were 10.72%, 4.76% and 4.28% with the Fine and Gray’s sub-distribution hazard model. AL artemether–lumefantrine, ASAQ artesunate–amodiaquine, DP dihydroartemisinin–piperaquine
Discussion
Recent reviews have shown that the majority of studies published in medical journals are susceptible to competing risk biases [6, 16, 22]; a concept hitherto overlooked in malaria literature. This re-analysis of individual patient data of 233 treatment arms from 92 clinical efficacy studies conducted in Asia, Africa, and South America revealed that just over a third (83/233) of the treatment arms had an observed proportion of new infection greater than 10%, a threshold considered to make studies vulnerable to competing risk bias [23]. This suggests that competing risk events are the rule rather than the exception in antimalarial trials.
This analysis allowed the exploration of the degree to which the derived estimate of failure was affected by ignoring the competing risk events in analysis of antimalarial efficacy trials. The K–M analysis which censored new infections was associated with a marginal absolute overestimation of the cumulative risk of recrudescence. In 9% (21/233) of the study arms the overestimation was greater than 1%, in 4.3% (10/233) the difference was greater than 2%, and in 2.6% (6/233) of the arms the difference was greater than 3%. All but one of the 21 study sites where the difference exceeded 1% were from Africa (areas of intense malaria transmission), the exception being a study from Papua New Guinea where a very high proportion of patients experienced recurrent parasitaemia due to P. vivax. The degree to which K–M overestimated failure in a study arm was correlated with the proportion of patients experiencing new infection or recrudescence, and the follow-up duration; these findings are consistent with the literature [1].
The current WHO guidelines recommend that when the estimates of recrudescence at the end of the follow-up exceed 10%, a series of detailed clinical, pharmacological and in vitro investigations should be undertaken to examine the possibility of parasite drug resistance. If resistance is confirmed, then treatment policy should be revised to a more effective regimen [2]. In three study arms, the estimated failure was greater than 10% (the WHO threshold for withdrawing antimalarials) when the K–M method was used, but remained below 10% when using a competing risk survival analysis method with the 95% confidence interval for the two estimates overlapping and the estimated 95% confidence interval included this threshold (Table 4). However, if the clinical decision-making was based solely on the point-estimates, then this highlights that ignoring competing risk events can result in potentially misleading conclusions being drawn from an efficacy trial, especially when the derived estimates are at the cusp of these thresholds.
The effect of competing risk events in comparative settings was then evaluated, as the partner components of the ACT are eliminated at different rates resulting in a differential fraction of new infections observed. For example, lumefantrine has a much shorter terminal elimination half-life compared to piperaquine [24]. The underlying drug pharmacokinetics will result in a lower observed proportion of new infections following DP administration compared to the AL regimen, especially in areas of intense malaria transmission [25]. This highlights the importance of taking the proportion of competing risk events into consideration when comparing drug regimens with different pharmacological properties. In order to explore whether these pharmacological differences affected the comparative analyses of these two drugs, the equality of the survival curves was compared using the log-rank test and Gray’s k-sample test using data from 27 comparative studies. There were no apparent differences in the derived conclusions using these two approaches as there were very few observed recrudescences in each of the study arms (Additional file 3: Section 2).
Finally, two different approaches to regression modelling in the presence of competing risk events were presented using data from Burkina Faso: the regression model on cause-specific hazard and on the sub-distribution hazard. The estimates of the sub-distribution hazard ratio (sdHR) were somewhat attenuated and closer to the null value compared to the cause-specific hazard ratio (csHR) (Table 5). Although the relative risk measures (cause-specific hazard ratio and sub-distribution hazard ratio) obtained from these two regression models were similar (Table 5), they are not directly comparable as they have a different interpretation [26, 27]. In the illustrated example, the csHR of 1.67 for baseline parasitaemia implies that every tenfold rise in parasite load was associated with a 1.67-fold higher risk of recrudescence, among patients who had not experienced any recurrence yet by the end of the follow-up. The sdHR of 1.44 (higher than 1) means that the cumulative incidence of recrudescence increases with every tenfold increase in parasite density and the interpretation of the numeric value of 1.44 is not straight forward [26]. This is because subjects who have experienced new infections are still maintained in the risk-set when computing a sub-distribution hazard, even though they are no longer at risk of experiencing recrudescence (Additional file 1: Section 3).
In the presence of competing risk events, researchers are faced with a choice of methods, and this has gathered considerable attention in medical and statistical literature [10, 17, 28,29,30]. In comparative studies, the log-rank test is considered appropriate when the research interest is in understanding the biological mechanism of how a treatment affects recrudescence (hazard rate). If the research interest is to answer if subjects receiving a particular drug are more likely to experience recrudescence at the end of the study follow-up, the comparison of CIF through Gray’s k-sample test is considered appropriate [1, 31, 32]. Many authors advocate presenting results of both these approaches to provide a complete biological understanding of the treatment on the different endpoints [1, 33]. For regression models, if the aim is to estimate probability and provide evidence to inform medical decision-making, the use of sub-distributional hazard model has been advocated as the method of choice [27, 34, 35], and if the aim is to explore the underlying biological effects of a covariate on the outcome, then a regression model on the cause-specific hazard has been preferred [1, 26, 27, 34].
This analysis has a number of limitations. It was assumed that the outcome of molecular genotyping reflects the true treatment outcomes. The current approach to parasite genotyping applies a conservative approach which overestimates the recrudescence particularly in areas of intense malaria transmission [36, 37]. In areas of very high transmission, such as Uganda, parasite infections are frequently polyclonal and as many as 45% of the recrudescences could be misclassified as new infections [38]. Further difficulties arise when the subsequent recrudescence is due to a minority clone which was undetected at baseline, thus leading to misclassified outcomes. This necessitates incorporating the uncertainity around the outcome classification, such as by using a Bayesian approach for classification of late treatment failures [39]. Indeterminate outcomes were censored in K–M analysis and considered as an extra category of competing risk event when generating CIF. An indeterminate outcome can only be considered as a competing risk event if the new infection and recrudescence coincide. However, an indeterminate outcome arising for other reasons, such as missing pairwise samples, or failure to amplify the parasite DNA cannot be considered as competing events in sensu stricto. In such a situation, considering them as an extra category for CIF analysis might have introduced bias. The efficacy of ACT in uncomplicated falciparum malaria remains high, with treatment failure reported in less than 5% of patients in the vast majority of ACT studies included in this analysis. Hence, the data used in this re-analysis did not allow the investigation of what would happen when the antimalarial efficacy declines. In order to quantify the magnitude of the potential biases in situations of falling antimalarial efficacy (now observed for dihydroartemisinin–piperaquine in Cambodia and Vietnam [40,41,42]), simulation studies were conducted and reported elsewhere [43]. This study did not explore the scenario of multiple-failure time (multivariate survival data), in which each patient can experience multiple events during follow-up. This scenario is of low relevance for falciparum malaria, but multiple events frequently occur in trials of vivax malaria, in which a patient may experience multiple relapses due to reactivation of hypnozoites from the liver.
Finally, it is difficult to disentangle whether a new infection is a truly competing endpoint in a biological sense. In a situation where the parasite causing the initial infection is subdued at low density and the newly emerging infection has higher density than the subdued original infection, then on a strong assumption of identical parasite multiplication rate for both infections, this constitutes a situation where the occurrence of new infection precludes recrudescence (Fig. 1a). This assumption of identical parasite multiplication rates might be plausible for rapidly eliminated drugs. For slowly eliminated drugs, the parasite growth rate for recrudescence and a new infection are likely to be different. Similarly, a recrudescent infection where the parasite numbers never go below those encountered at the beginning of a new infection cannot be pre-empted and the occurrence of recrudescence will not be affected (Fig. 1b). The only exception is if the new infection is more resistant than the primary infection. When the initial infection is completely eliminated after exposure to antimalarials, the host is no longer at a risk of subsequent recrudescence and competing risk situation does not exist (Fig. 1c). In reality it is impossible to disentangle the underlying in vivo parasitological circumstances from this dataset. Thus, new infections can be considered as a “situational competing risk event” which is primarily dependent on the inoculum density, fitness, efficiency of a newly emergent infection and of the existing recrudescent parasites, and the host immunity.
Conclusions
Censoring competing events in the Kaplan–Meier analysis led to an overestimation of the risk of recrudescence, which was of marginal clinical importance in the data included in this analysis. In the areas of high transmission where a large proportion of recurrences are attributable to new infections, the use of CIF provides an alternative approach for the derivation of failure estimates for anti-malarial treatments.
Abbreviations
- \(\hat{F}_{KM} \left( t \right)\) :
-
The complement of Kaplan–Meier estimate [1 − \(\hat{S}_{KM} \left( t \right)\)]
- \(\hat{S}_{KM} \left( t \right)\) :
-
Kaplan–Meier estimates of drug efficacy at time t
- CIF:
-
Cumulative Incidence Function
- csHR:
-
Cause-specific hazard ratio
- K–M:
-
Kaplan–Meier estimate
- NI:
-
New infection
- RC:
-
Recrudescence
- sdHR:
-
Sub-distribution hazard ratio
- WHO:
-
World Health Organization
References
Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695–706.
WHO. Methods for surveillance of antimalarial drug efficacy. Geneva: World Health Organization; 2009.
Southern DA, Faris PD, Brant R, Galbraith PD, Norris CM, Knudtson ML, et al. Kaplan–Meier methods yielded misleading results in competing risk scenarios. J Clin Epidemiol. 2006;59:1110–4.
Lacny S, Wilson T, Clement F, Roberts DJ, Faris PD, Ghali WA, et al. Kaplan–Meier survival analysis overestimates the risk of revision arthroplasty: a meta-analysis. Clin Orthop Relat Res. 2015;473:3431–42.
Varadhan R, Weiss CO, Segal JB, Wu AW, Scharfstein D, Boyd C. Evaluating health outcomes in the presence of competing risks: a review of statistical methods and clinical applications. Med Care. 2010;48(6 Suppl):S96–105.
Van Walraven C, McAlister FA. Competing risk bias was common in Kaplan–Meier risk estimates published in prominent medical journals. J Clin Epidemiol. 2016;69:170–3.
Dahal P, Simpson JA, Dorsey G, Guérin PJ, Price RN, Stepniewska K. Statistical methods to derive efficacy estimates of anti-malarials for uncomplicated Plasmodium falciparum malaria: pitfalls and challenges. Malar J. 2017;16:430.
Prentice RL, Kalbfleisch JD, Peterson AV, Flournoy N, Farewell VT, Breslow NE. The analysis of failure times in the presence of competing risks. Biometrics. 1978;34:541–54.
Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1141–54.
Williamson PR, Kolamunnage-Dona R, Tudur Smith C. The influence of competing-risks setting on the choice of hypothesis test for treatment effect. Biostatistics. 2007;8:689–94.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:196–509.
Keene CM, Dondorp A, Crawley J, Ohuma EO, Mukaka M. A competing-risk approach for modeling length of stay in severe malaria patients in South-East Asia and the implications for planning of hospital services. Clin Infect Dis. 2018;67:1053–62.
Humphreys GS, Barnes KI, Tinto H. Strength in numbers: the WWARN case study of purpose-driven data sharing. Am J Trop Med Hyg. 2018;100:13–5.
WorldWide Antimalarial Resistance Network. Data management and statistical analysis plan Version 1.2. 2012. http://www.wwarn.org/sites/default/files/ClinicalDMSAP.pdf. Accessed 24 Sept 2018.
Kalbfleisch JD, Prentice RL. Competing risks and multistate models. The statistical analysis of failure time data. 2nd ed. New York: Wiley; 2002. p. 247–77.
Austin PC, Fine JP. Accounting for competing risks in randomized controlled trials: a review and recommendations for improvement. Stat Med. 2017;36:1203–9.
Dignam JJ, Kocherginsky MN. Choice and interpretation of statistical tests used when competing risks are present. J Clin Oncol. 2008;26:4027–34.
The Four Artemisinin-Based Combinations (4ABC) Study Group. A head-to-head comparison of four artemisinin-based combinations for treating uncomplicated malaria in african children: a randomized trial. PLoS Med. 2011;8:e1001119.
Ettore M, Valsecchi MG. Competing risks. Analysing survival data from clinical trials and observational studies. Chichester: Wiley; 2004. p. 357. Accessed 3 Mar 2019.
R Foundation for Statistical Computing. R: a language and environment for statistical computing. 2017. https://www.r-project.org/.
Sirima SB, Ogutu B, Lusingu JPA, Mtoro A, Mrango Z, Ouedraogo A, et al. Comparison of artesunate–mefloquine and artemether–lumefantrine fixed-dose combinations for treatment of uncomplicated Plasmodium falciparum malaria in children younger than 5 years in sub-Saharan Africa: a randomised, multicentre, phase 4 trial. Lancet Infect Dis. 2016;16:1123–33.
Koller MT, Raatz H, Steyerberg EW, Wolbers M. Competing risks and the clinical community: irrelevance or ignorance? Stat Med. 2012;31:1089–97.
Austin PC, Lee DS, Fine JP. Introduction to the analysis of survival data in the presence of competing risks. Circulation. 2016;133:601–9.
WHO. Guidelines for the treatment of malaria. 3rd ed. Geneva: World Health Organization; 2015.
Ratcliff A, Siswantoro H, Kenangalem E, Maristela R, Wuwung R, Laihad F, et al. Two fixed-dose artemisinin combinations for drug-resistant falciparum and vivax malaria in Papua, Indonesia: an open-label randomised comparison. Lancet. 2007;369:757–65.
Wolbers M, Koller MT, Witteman JCM, Steyerberg EW. Prognostic models with competing risks. Epidemiology. 2009;20:555–61.
Wolbers M, Koller MT, Stel VS, Schaer B, Jager KJ, Leffondre K, et al. Competing risks analyses: objectives and approaches. Eur Heart J. 2014;35:2936–41.
Freidlin B, Korn EL. Testing treatment effects in the presence of competing risks. Stat Med. 2005;24:1703–12.
Rotolo F, Michiels S. Testing the treatment effect on competing causes of death in oncology clinical trials. BMC Med Res Methodol. 2014;14:72.
Bajorunaite R, Klein JP. Comparison of failure probabilities in the presence of competing risks. J Stat Comput Simul. 2008;78:951–66.
Pintilie M. Analysing and interpreting competing risk data. Stat Med. 2007;26:1360–7.
Tai B-C, Wee J, Machin D. Analysis and design of randomised clinical trials involving competing risks endpoints. Trials. 2011;12:127.
Latouche A, Allignol A, Beyersmann J, Labopin M, Fine JP. A competing risks analysis should report results on all cause-specific hazards and cumulative incidence functions. J Clin Epidemiol. 2013;66:648–53.
Lau B, Cole SR, Gange SJ. Competing risk regression models for epidemiologic data. Am J Epidemiol. 2009;170:244–56.
Andersen PK, Geskus RB, De Witte T, Putter H. Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol. 2012;41:861–70.
Collins WJ, Greenhouse B, Rosenthal PJ, Dorsey G. The use of genotyping in antimalarial clinical trials: a systematic review of published studies from 1995–2005. Malar J. 2006;5:122.
Cattamanchi A, Kyabayinze D, Hubbard A, Rosenthal PJ, Dorsey G. Distinguishing recrudescence from reinfection in a longitudinal antimalarial drug efficacy study: comparison of results based on genotyping of MSP-1, MSP-2, and GLURP. Am J Trop Med Hyg. 2003;68:133–9.
Greenhouse B, Dokomajilar C, Hubbard A, Rosenthal PJ, Dorsey G. Impact of transmission intensity on the accuracy of genotyping to distinguish recrudescence from new infection in antimalarial clinical trials. Antimicrob Agents Chemother. 2007;51:3096–103.
Plucinski MM, Morton L, Bushman M, Dimbu PR, Udhayakumar V. Robust algorithm for systematic classification of malaria late treatment failures as recrudescence or reinfection using microsatellite genotyping. Antimicrob Agents Chemother. 2015;59:6096–100.
Leang R, Barrette A, Bouth DM, Menard D, Abdur R, Duong S, et al. Efficacy of dihydroartemisinin–piperaquine for treatment of uncomplicated Plasmodium falciparum and Plasmodium vivax in Cambodia, 2008 to 2010. Antimicrob Agents Chemother. 2013;57:818–26.
Saunders DL, Vanachayangkul P, Lon C. Dihydroartemisinin–piperaquine failure in Cambodia. N Engl J Med. 2014;371:484–5.
Phuc BQ, Rasmussen C, Duong TT, Dong LT, Loi MA, Tarning J, et al. Treatment failure of dihydroartemisinin/piperaquine for Plasmodium falciparum malaria, Vietnam. Emerg Infect Dis. 2017;23:715–7.
Dahal P, Guerin PJ, Price RN, Simpson JA, Stepniewska K. Evaluating antimalarial efficacy in single-armed and comparative drug trials using competing risk survival analysis: a simulation study. BMC Med Res Methodol. 2019;19:107.
White NJ. The assessment of antimalarial drug efficacy. Trends Parasitol. 2002;18:458–64.
Yeka A, Dorsey G, Kamya MR, Talisuna A, Lugemwa M, Rwakimari JB, et al. Artemether–lumefantrine versus dihydroartemisinin–piperaquine for treating uncomplicated malaria: a randomized trial to guide policy in Uganda. PLoS ONE. 2008;3:e2390.
Schramm B, Valeh P, Baudin E, Mazinda CS, Smith R, Pinoges L, et al. Tolerability and safety of artesunate–amodiaquine and artemether–lumefantrine fixed dose combinations for the treatment of uncomplicated Plasmodium falciparum malaria: two open-label, randomized trials in Nimba County, Liberia. Malar J. 2013;12:250.
Agarwal A, McMorrow M, Onyango P, Otieno K, Odero C, Williamson J, et al. A randomized trial of artemether–lumefantrine and dihydroartemisinin–piperaquine in the treatment of uncomplicated malaria among children in western Kenya. Malar J. 2013;12:254.
Karunajeewa HA, Mueller I, Senn M, Lin E, Law I, Gomorrai PS, et al. A trial of combination antimalarial therapies in children from Papua New Guinea. N Engl J Med. 2008;359:2545–57.
Bukirwa H, Yeka A, Kamya MR, Talisuna A, Banek K, Bakyaita N, et al. Artemisinin combination therapies for treatment of uncomplicated malaria in Uganda. PLoS Clin Trials. 2006;1:e7.
WHO. Responding to antimalarial drug resistance. Geneva: World Health Organization; 2017. http://www.who.int/malaria/areas/drug_resistance/overview/en/. Accessed 5 Dec 2017.
Acknowledgements
We would like to thank the patients and all the staff who participated in these clinical trials at all the sites. We would like to thank Dr. Charlie Woodrow, Dr. Louis K Penali, Dr. Adoke Yeka, Dr. Issaka Sagara, Dr. Oumar Faye, Dr. Khadime Sylla, Dr. Roger Tine, Prof. Paul Newton, and Dr. Nathalie Strub for their kind contribution with the data. We thank Dr. Marcel Wolbers and Prof. Sir Nick White for thoroughly reviewing the manuscript and for several helpful discussions on the topic.
Study group members: The complete list of author’s contribution is listed in Additional file 2. The members of the WorldWide Antimalarial Resistance Network (WWARN) Methodology Study Group are the authors of this paper: Prabin Dahal, World Wide Antimalarial Resistance Network (WWARN), Oxford, UK; Centre for Tropical Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK (prabin.dahal@wwarn.org); Julie Anne Simpson, Centre for Epidemiology and Biostatistics, Melbourne School of Population and Global Health, University of Melbourne, Melbourne, VIC, Australia (julieas@unimelb.edu.au); Salim Abdulla, Ifakara Health Institute, Dar es Salaam, Tanzania (sabdulla@ihi.or.tz; salim.abdulla@gmail.com); Jane Achan, Medical Research Council Unit, Gambia (achanj@yahoo.co.uk; jachan@mrc.gm); Ishag Adam, Faculty of Medicine, University of Khartoum, Khartoum, Sudan (ishagadam@hotmail.com); Aarti Agarwal, Malaria Branch, Division of Parasitic Diseases and Malaria, Centers for Disease Control and Prevention, Atlanta, GA, USA (aartiagarwal@hotmail.com); Richard Allan, The Mentor Initiative (richard@mentor-initiative.net); Anupkumar R Anvikar, National Institute of Malaria Research, Sector 8, Dwarka, New Delhi 110077, India (anvikar@gmail.com); Emmanuel Arinaitwe, Infectious Diseases Research Collaboration, Kampala, Uganda (earinaitwe@idrc-uganda.org; emmy3md@yahoo.com); Elizabeth A Ashley, Myanmar Oxford Clinical Research Unit, Myanmar; Centre for Tropical Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK (liz@tropmedres.ac); Ghulam Rahim Awab, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand; Ministry of Public Health, Islamic Republic of Afghanistan, Kabul, Afghanistan (awabgr@yahoo.com); Quique Bassat, Centro de Investigação em Saúde de Manhiça (CISM), Maputo, Mozambique; ISGlobal, Hospital Clínic - Universitat de Barcelona, Barcelona, Spain; ICREA, Pg. Lluís Companys 23, 08010 Barcelona, Spain (quique.bassat@isglobal.org); Anders Björkman, Depatment Microbiology,Tumour and Cell Biology, Karolinska institutet, Stockholm Sweden (anders.bjorkman@ki.se); Francois Bompart, Sanofi Access to Medicines, Gentilly, France (francois.bompart@sanofi.com); Steffen Borrmann, Kenya Medical Research Institute/Wellcome Trust Research Programme, Kilifi, Kenya; Heidelberg University School of Medicine, Dept. of Infectious Diseases, Heidelberg, Germany (steffen.borrmann@me.com); Teun Bousema, Radboud Institute for Health Sciences, Radboudumc Nijmegen, the Netherlands; Department of Medical Microbiology, Radboud University Nijmegen Medical Centre, Njimegen, the Netherlands (Teun.Bousema@radboudumc.nl); Ingrid Broek, Epidemioloog Epidemiologie en Surveillance, RIVM - Centrum Infectieziektebestrijding, Bilthoven (ingrid.van.den.broek@rivm.nl); Hasifa Bukirwa, African Field Epidemiology Network, Kampala, Uganda (hbukirwa@hotmail.com); Verena I Carrara, Shoklo Malaria Research Unit, Mae Sot, Thailand; Mahidol Oxford University Research Unit, Bangkok, Thailand (verena@shoklo-unit.com); Marco Corsi, Private consultancy for Drug Development in Tropical Diseases, formerly Sigma Tau SpA Industrie Farmaceutiche Riunite, Pomezia (Rome) Italy (artemisinin@gmail.com); Michel Cot, MERIT, IRD, Université Paris 5, Sorbonne Paris Cité, Paris, 75006, France (Michel.Cot@ird.fr); Umberto D'Alessandro, Medical Research Council Unit, Fajara, The Gambia; London School of Hygiene and Tropical Medicine, London, UK (udalessandro@mrc.gm); Timothy ME Davis, School of Medicine and Pharmacology, University of Western Australia,Crawley, WA, Australia (tim.davis@uwa.edu.au; tdavis@cyllene.uwa.edu.au); Marit de Wit, Médecins Sans Frontières-Operational Centre Amsterdam (Marit.DE.WIT@amsterdam.msf.org); Philippe Deloron, MERIT, IRD, Université Paris 5, Sorbonne Paris Cité, Paris, 75006, France (philippe.deloron@ird.fr); Meghna Desai, Malaria Branch, Division of Parasitic Diseases and Malaria, Centers for Disease Control and Prevention, Atlanta, GA, USA (mud8@cdc.gov); Pedro Rafael Dimbu, National Malaria Control Program, Luanda, Angola (rafaeldimbu1@gmail.com); Djibrine Djalle, Institut Pasteur de Bangui, BP 923 Bangui, Central African Republic (djibrinedjalle@gmail.com; dj_djibrine@yahoo.fr); Abdoulaye Djimde, Malaria Research and Training Center, Department of Epidemiology of Parasitic Diseases, Faculty of Pharmacy, University of Science, Techniques and Technologies of Bamako, Bamako, Mali (adjimde@icermali.org); Grant Dorsey, Department of Medicine, University of California San Francisco, San Francisco, USA (gdorsey@medsfgh.ucsf.edu); Ogobara K Doumbo, Malaria Research and Training Center, Department of Epidemiology of Parasitic Diseases, Faculty of Medicine and Odonto-Stomatology, University of Science, Techniques and Technologies of Bamako, Bamako, Mali (okd@icermali.org); Chris J Drakeley, Department of Infection and Immunity, London School of Hygiene and Tropical Medicine, London, UK (chris.drakeley@lshtm.ac.uk); Stephan Duparc, Medicines for Malaria Venture, Geneva, Switzerland (duparcs@mmv.org); Michael D Edstein, Australian Army Malaria Institute, Brisbane, Qld, Australia (Mike.Edstein@defence.gov.au); Emmanuelle Espie, GSK Vaccines, R&D center, Clinical and Epidemiology department (avenue Fleming 20, 1300 Wavre); Formerly: Epicentre, 8, rue Saint Sabin, 75011, Paris, France (emmanuelle.espie@gmail.com; emmanuelle.v.espie@gsk.com); Abul Faiz, Malaria Research Group, Chittagong, Bangladesh; Dev Care Foundation, Dhaka, Bangladesh (drmafaiz@gmail.com); Catherine Falade, Department of Pharmacology & Therapeutics,College of Medicine, University of Ibadan,Ibadan, Nigeria (lillyfunke@yahoo.com); Caterina Fanello, Centre for Global Health, Nuffield Departement of Medicine, University of Oxford, UK (caterina.fanello@ndm.ox.ac.uk); Jean-Francois Faucher, Institut de Recherche pour le Developpement (IRD), Mother and Child Health in the Tropics Research Unit; Department of Infectious Diseases, Besancon University Medical Center, Besancon (caterina.fanello@ndm.ox.ac.uk); Babacar Faye, Department of Medical Parasitology, Medical Faculty, Université Cheikh Anta Diop, Dakar, Senegal (bfaye67@yahoo.fr); Filomeno de Jesus Fortes, National Malaria Control Program, Luanda, Angola (filomenofortes@gmail.com); Nahla B Gadalla, Sudanese American Medical Association, Fairfax, VA, US (nahlagadalla@gmail.com; director@sama-sd.org); Oumar Gaye, Department of Medical Parasitology, Medical Faculty, Université Cheikh Anta Diop, Dakar, Senegal (ogaye@refer.sn); J. Pedro Gil, Drug Resistance Unit, Division of Pharmacogenetics, Department of Physiology and Pharmacology, Karolinska Institutet, Stockholm, Sweden; Center for Biodiversity, Functional and Integrative Genomics, Faculdade de Ciências, Universidade de Lisboa, Portugal (Jose.pedro.gil@ki.se); Brian Greenwood, Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, UK (brian.greenwood@lshtm.ac.uk); Anastasia Grivoyannis, The Johns Hopkins Hospital, Baltimore, Maryland, USA (grivoyannis@jhmi.edu); Kamal Hamed, Basilea Pharmaceutica International Ltd., Basel, Switzerland; Formerly Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA (kamalhamed1@aol.com; kamal.hamed@basilea.com); Tran Tinh Hien, Oxford University Clinical Research Unit (OUCRU), Centre for Tropical Medicine, Wellcome Trust Major Overseas Program (MOP) (hientt@oucru.org); David Hughes, Novartis International AG, Basel, Switzerland (david.hughes@novartis.com); Georgina Humphreys, Wellcome Trust, London, UK; Formerly: World Wide Antimalarial Resistance Network (WWARN), Oxford, UK (G.Humphreys@wellcome.ac.uk); Jimee Hwang, US President’s Malaria Initiative, Malaria Branch, Division of Parasitic Diseases and Malaria, US Centers for Disease Control and Prevention, Atlanta, GA, USA; Global Health Group, University of California San Francisco, San Francisco, USA (gdq1@cdc.gov; jhwang@cdc.gov); Maman Laminou Ibrahim, Centre de Recherche Médiacle et Saniataire (CERMES), Niamey-Niger (lamine@cermes.org); Bart Janssens, Medecins Sans Frontieres, Phnom Penh, Cambodia (Bart.JANSSENS@brussels.msf.org); Vincent Jullien, Universite´ Paris Descartes, Assistance Publique-Hoˆpitaux de Paris, Service de Pharmacologie Clinique, Groupe Hospitalier Cochin—Saint-Vincent de Paul, Inserm U663, WWARN, Paris, France (vincent.jullien@egp.aphp.fr; Vincent.Jullien@univ-nantes.fr); Elizabeth Juma, Kenya Medical Research Institute, Nairobi, Kenya (jumae@who.int; jumaelizabeth@yahoo.com); Erasmus Kamugisha, Weill-Bugando University College of Health Sciences, Mwanza, Tanzania (erasmuskamugisha@yahoo.com); Corine Karema, National Malaria Control Program–TRAC Plus, Ministry of Health, Kigali, Rwanda (ckarema@gmail.com); Harin A Karunajeewa, The Walter and Eliza Hall Institute of Medical Research (karunajeewa.h@wehi.edu.au; Harin.Karunajeewa@wh.org.au); Jean R Kiechel, Drugs for Neglected Diseases initiative, Geneva, Switzerland (jean-rene.kiechel@wanadoo.fr); Fred Kironde, Habib Medical School, Islamic University in Uganda, Kampala,Uganda (faskironde@gmail.com); Poul-Erik Kofoed, Bandim Health Project, Indepth Network, Apartado 861, Bissau, Guinea-Bissau; Health Services Research Unit, Lillebaelt Hospital/IRS University of Southern Denmark, Vejle, Denmark; Department of Paediatrics, Kolding Hospital, Kolding, Denmark (pekofoed@dadlnet.dk; Poul.Erik.Kofoed@rsyd.dk); Peter G Kremsner, Institute of Tropical Medicine, University of Tübingen, Germany; Centre de Recherches Medicales de Lambarene, Gabon (peter.kremsner@uni-tuebingen.de); Valerie Lameyre, Sanofi Access to Medicines, Gentilly, France (valerie.lameyre@sanofi.com); Sue J Lee, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand; Centre for Tropical Medicine, Nuffield Department of Clinical Medicine, Churchill Hospital, Oxford, UK (sue@tropmedres.ac); Kevin Marsh, Centre for Tropical Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, United Kingdom; Kenya Medical Research Institute/Wellcome Trust Research Programme, Kilifi, Kenya (kevin.marsh@ndm.ox.ac.uk); Andreas Mårtensson, Department of Women’s and Children’s Health, International Maternal and Child Health (IMCH), Uppsala University, Uppsala, Sweden (andreas.martensson@kbh.uu.se); Mayfong Mayxay, Lao-Oxford-Mahosot Hospital-Wellcome Trust Research Unit, Microbiology Laboratory, Mahosot Hospital, Vientiane, Laos (mayfong@tropmedres.ac); Hervé Menan, Department of Parasitology, Faculty of Pharmacy, University of Cocody, Abidjan, Côte d'Ivoire; Faculty of Postgraduate Studies, University of Health Sciences, Ministry of Health, Vientiane, Laos (rvmenan@yahoo.fr); Petra Mens, Medical Microbiology, Parasitology, Academic Medical Centre, Amsterdam, The Netherlands (p.f.mens@amc.uva.nl); Theonest K Mutabingwa, Hubert Kairuki Memorial University, Dar-es-Salaam, Tanzania; Department of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, UK (tk.bingwa@yahoo.com); Jean-Louis Ndiaye, Parasitology and Mycology Laboratory, Faculty of Medecine, Université Cheikh Anta Diop, Dakar, Senegal (jlndiaye@yahoo.com); Billy E Ngasala, Department of Parasitology, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; Malaria Research, Infectious Disease Unit, Department of Medicine Solna, Karolinska Institutet, Stockholm, Sweden (bngasala70@yahoo.co.uk); Harald Noedl, Medical University of Vienna, Vienna (harald.noedl@meduniwien.ac.at); Francois Nosten, Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine Research building, University of Oxford Old Road campus, Oxford, UK; Shoklo Malaria Research Unit, Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Mae Sot, Thailand (francois@tropmedres.ac); Andre Toure Offianan, Malariology department, Institut Pasteur de Côte d'Ivoire, Abidjan, Côte d'Ivoire (andre_offianan@yahoo.fr); Mary Oguike, Dept of Immunology & Infection, London School of Hygiene & Tropical Medicine, UK (Mary.Oguike@lshtm.ac.uk); Bernhards R Ogutu, Kenya Medical Research Institute/United States Army Medical Research Unit, Kisumu, Kenya (bernhards.ogutu@usamru-k.org); Piero Olliaro, UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases (WHO/TDR), Geneva, Switzerland (olliarop@who.int); Jean Bosco Ouedraogo, Direction Re´gionale de l’Ouest, Institut de Recherche en Sciences de la Sante´, Bobo-Dioulasso, Burkina Faso; Non Transmissible disease department, Centre Muraz Bobo-Dioulasso, Bobo-Dioulasso, Burkina Faso (jbouedraogo.irssbobo@fasonet.bf; jbouedraogo@gmail.com); Patrice Piola, Institut Pasteur du Cambodge, Phnom Penh, Cambodia (ppiola@pasteur-kh.org); Christopher V Plowe, Duke Global Health Institute, Duke University, Durham, NC, USA (chris.plowe@duke.edu); Mateusz M Plucinski, US President’s Malaria Initiative, Malaria Branch, Division of Parasitic Diseases and Malaria, US Centers for Disease Control and Prevention, Atlanta, GA, USA; Epidemic Intelligence Service, Centers for Disease Control and Prevention, Atlanta, Georgia, USA (mplucinski@cdc.gov); Oliver James Pratt, National Malaria Control Program, Ministry of Health and Social Welfare, Liberia (Opratt7@gmail.com); Zulfikarali Premji, Muhimbili University College of Health Sciences, Dar es Salaam, Tanzania (premjizulfiqarali@gmail.com); Michael Ramharter, Department of Tropical Medicine, Bernhard Nocht Institute for Tropical Medicine & I. Department of Medicine University Medical Centre Hamburg-Eppendorf, Hamburg Germany (ramharter@bnitm.de); Christophe Rogier, French military health service, Central directorate, Division "Expertise and defense health strategy", Paris, France; Institut de recherche biomédicale des armées (IRBA), Brétigny-Sur-Orge, France; Unité de recherche sur les maladies infectieuses et tropicales émergentes (URMITE)-UMR 6236, Marseille, France (christophe.rogier@gmail.com; christophe.rogier@intradef.gouv.fr); Lars Rombo, Clinical research centre, sormland county council, Uppsala university, Sweden (lars.rombo@gmail.com); Philip J Rosenthal, Department of Medicine, University of California San Francisco, San Francisco, USA (prosenthal@medsfgh.ucsf.edu); Patrick Sawa, Human Health Division, International Centre for insect physiology and Ecology, Mbita, Kenya (psawa@mbita.icipe.org); Birgit Schramm, Epicentre, Paris, France (Birgit.Schramm@epicentre.msf.org); Carol Sibley, World Wide Antimalarial Resistance Network (WWARN), Oxford, UK; Department of Genome Sciences, University of Washington, Seattle, USA (carol.sibley@wwarn.org); Veronique Sinou, Aix Marseille Univ, INSERM, SSA, IRBA, MCT, Marseille, France (veronique.sinou@univ-amu.fr); Sodiomon Sirima, Groupe de Recherche Action en Santé (GRAS) 06 BP 10248, Ouagadougou 06, Burkina Faso (s.sirima.cnlp@fasonet.bf); Frank Smithuis, Myanmar Oxford Clinical Research Unit (frank.m.smithuis@gmail.com); Sarah G Staedke, Department of Clinical Research, London School of Hygiene & Tropical Medicine, London, UK; Infectious Diseases Research Collaboration, Kampala, Uganda (Sarah.Staedke@lshtm.ac.uk); Inge Sutanto, Department of Parasitology, Faculty of Medicine, University of Indonesia, 6 Salemba Raya, Jakarta 10430, Indonesia (sutanto.inge@yahoo.com); Ambrose Otau Talisuna, Regional Office for Africa, World Health Organization, Brazzaville, Congo (talisunaa@who.int); Joel Tarning, WorldWide Antimalarial Resistance Network, Oxford, United Kingdom; Mahidol Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand; Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, United Kingdom (joel@tropmedres.ac); Walter RJ Taylor, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand (Bob@tropmedres.ac); Emmanuel Temu, The MENTOR Initiative (emmanuel.temu@gmail.com); Kamala L Thriemer, Global and Tropical Health Division, Menzies School of Health Research, Charles Darwin University, Darwin, Northern Territory, Australia (Kamala.Ley-Thriemer@menzies.edu.au); Nhien Nguyen Thuy, Oxford University Clinical Research Unit (OUCRU), Centre for Tropical Medicine, Wellcome Trust Major Overseas Program (MOP) (nhienntt@oucru.org); Venkatachalam Udhayakumar, Malaria Branch and President’s Malaria Initiative, Division of Parasitic Diseases and Malaria, Center for Global Health, Centers for Disease Control and Prevention, Atlanta,Georgia, USA (vxu0@cdc.gov); Johan Ursing, Department of Microbiology, Tumor and Cell Biology (MTC), C1, Karolinska Institutet; The Department of Infectious Diseases, Danderyds Hospital, Sweden (Johan.Ursing@ki.se; johan.ursing@gmail.com); Michel van Herp, Medecins Sans Frontieres, Operational Centre Brussels, Brussels, Belgium (michel.van.herp@brussels.msf.org); Michele van Vugt, Division of Infectious Diseases, Center for Tropical Medicine & Travel Medicine, Academic medical Center, University of Amsterdam, The Netherlands (M.vanVugt@amc.uva.nl); Christopher Whitty, Malaria Partnership, Department of Infectious and Tropical Disease, London School of Hygiene and Tropical Medicine (christopher.whitty@lshtm.ac.uk; christopher.whitty@uclh.nhs.uk); Yavo William, Department of Parasitology, Faculty of Pharmacy, University of Cocody,Abidjan, Côte d’Ivoire (yavowilliam@yahoo.fr); Cornelis Winnips, Novartis International AG, Basel, Switzerland (cornelis.winnips@novartis.com); Issaka Zongo, Direction Re´gionale de l’Ouest, Institut de Recherche en Sciences de la Sante´, Bobo-Dioulasso, Burkina Faso (zongo_issaka@yahoo.fr); Philippe Guerin, World Wide Antimalarial Resistance Network (WWARN), Oxford, UK; Centre for Tropical Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK (philippe.guerin@wwarn.org); Ric N Price, Menzies School of Health Research and Charles Darwin University, Darwin, Australia; Centre for Clinical Vaccinology and Tropical Medicine, Churchill Hospital, Oxford, UK; World Wide Antimalarial Resistance Network (WWARN), Oxford, UK (ric.price@wwarn.org); Kasia Stepniewska, World Wide Antimalarial Resistance Network (WWARN), Oxford, UK; Centre for Tropical Medicine, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, UK (kasia.stepniewska@wwarn.org).
Funding
PD is funded by Tropical Network Fund, Nuffield Department of Clinical Medicine, University of Oxford. The WorldWide Antimalarial Resistance Network (PD, KS, RNP, GSH, and PJG) is funded by a Bill and Melinda Gates Foundation grant and the ExxonMobil Foundation. JAS is an Australian National Health and Medical Research Council Senior Research Fellow (1104975). RNP is a Wellcome Trust Senior Fellow in Clinical Science (200909). The funders did not participate in the study development, the writing of the paper, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
PD, PJG, RNP, JAS and KS conceived the idea and wrote the first draft of the manuscript. All authors read and approved the final manuscript. The contributors for each of the authors are presented in Additional file 2.
Ethics declarations
Availability of data and materials
The database(s) supporting the conclusions of this article are available from the WorldWide Antimalarial Resistance Network (WWARN) (http://www.wwarn.org/), a controlled open access repository of antimalarial studies on reasonable request.
Ethics approval and consent to participate
Not applicable. This study met the criteria for waiver of ethical review as defined by the Oxford Tropical Research Ethics Committee (OxTREC) as the research consists of secondary analysis of existing, anonymous data.
Consent for publication
Not applicable.
Competing interests
The findings and conclusions in this report are those of the author(s) (Jimee Hwang, Mattaeusz Plucinski, Meghna Desai) and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The rest of the authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1.
Definitions.
Additional file 2.
List of studies used.
Additional file 3
Additional results.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
The WorldWide Antimalarial Resistance Network Methodology Study Group. Competing risk events in antimalarial drug trials in uncomplicated Plasmodium falciparum malaria: a WorldWide Antimalarial Resistance Network individual participant data meta-analysis. Malar J 18, 225 (2019). https://doi.org/10.1186/s12936-019-2837-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-019-2837-4