Abstract
Background
The increased resistance of the human malaria parasite Plasmodium falciparum to currently employed drugs creates an urgent call for novel anti-malarial drugs. Particularly, efforts should be devoted to developing fast-acting anti-malarial compounds in case clinical resistance increases to the first-line artemisinin-based combination therapy. SC83288, an amicarbalide derivative, is a clinical development candidate for the treatment of severe malaria. SC83288 is fast-acting and able to clear P. falciparum parasites at low nanomolar concentrations in vitro, as well as in a humanized SCID mouse model system in vivo. In this study, the antiplasmodial activity of SC83288 against artemisinins was profiled in order to assess its potential to replace, or be combined with, artemisinin derivatives.
Results
Based on growth inhibition and ring survival assays, no cross-resistance was observed between artemisinins and SC83288, using parasite lines that were resistant to either one of these drugs. In addition, no synergistic or antagonistic interaction was observed between the two drugs. This study further confirmed that SC83288 is a fast acting drug in several independent assays. Combinations of SC83288 and artesunate maintained the rapid parasite killing activities of both components.
Conclusion
The results obtained in this study are consistent with artemisinins and SC83288 having distinct modes of action and different mechanisms of resistance. This study further supports efforts to continue the clinical development of SC83288 against severe malaria as an alternative to artemisinins in areas critically affected by artemisinin-resistance. Considering its fast antiplasmodial activity, SC83288 could be combined with a slow-acting anti-malarial drug.
Similar content being viewed by others
Background
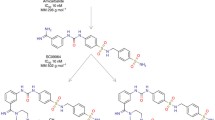
Despite a decline in global malaria mortality during the previous decade, the human malaria parasite Plasmodium falciparum continues to infect more than 200 million people annually, causing approximately 450,000 deaths per year [1]. A main factor in the relative success in decreasing malaria-related deaths was the introduction of the highly efficient chemotherapeutic agent artemisinin (Fig. 1a) and its derivatives (Fig. 1b, c). Partnered with other drugs as artemisinin-based combination therapy (ACT), artemisinins have formed the backbone of malaria treatment and control since 2006 [2]. However, P. falciparum strains displaying delayed and possibly reduced responsiveness to ACT have emerged in western Cambodia [3], and are now spreading across all of Southeast Asia [4, 5]. Accordingly, there is a need for new anti-malarial drugs with novel chemical structures that exploit distinct molecular targets to protect them from cross-resistance mechanisms. While several clinical candidates fulfilling these criteria are currently in preclinical and clinical development [6,7,8,9,10,11,12,13,14,15,16,17,18,19], more candidates are needed to build up a solid and reliable reserve library of anti-malarial drugs should the first line drugs fail. One such clinical development candidates is SC83288 (Fig. 1d), which is considered for the treatment of severe malaria [20].
SC83288, an amicarbalide derivative, is active against P. falciparum blood stages at low nanomolar concentrations in vitro, with IC50 values of 3 nM. SC83288 is able to clear a P. falciparum infection in a humanized NOD/SCID mouse model system within 48 h following intraperitoneal injections of 2.5 mg kg−1 once per day over a period of 3 days [20]. Furthermore, SC83288 is fast acting and it has favourable pharmacological and toxicological features [20]. In vitro resistance to SC83288 develops slowly and might involve mutational changes in the Ca2+ transporting PfATP6, the P. falciparum SERCA orthologue. However, PfATP6 does not seem to be the molecular target of SC83288 but rather a component of resistance [20].
PfATP6 is a validated drug target [21] and was once considered the prime molecular target of artemisinins [22,23,24,25] and a contributor to artemisinin resistance [26,27,28,29]. However, recent studies failed to detect a specific interaction between PfATP6 and artemisinins [30,31,32,33,34,35], and instead favour a pleiotropic mode of action in that many proteins are covalently modified by the alkylating property of artemisinins [36]. Moreover, resistance to artemisinins has recently been associated with polymorphisms in the kelch propeller domain protein 13 (PfK13) [37,38,39,40,41,42,43,44,45,46], a member of the kelch protein superfamily, bearing multiple protein–protein interaction sites and involved, among others, in ubiquitin-regulated protein degradation and oxidative stress responses [47].
Considering the gold standard status of artemisinin and its derivatives in the anti-malarial drug development field and taking into account that PfATP6 has repeatedly been considered a drug target of, or a contributor to drug resistance, including to SC83288, raises the possibility that SC83288 and artemisinins exert their antiplasmodial activity, or induce resistance, in P. falciparum in a similar or synergistic manner. The data presented herein suggest that these concerns are unfounded. No cross-resistance was observed between dihydroartemisinin and SC83288 in vitro. Moreover, both drugs showed neither a synergistic nor antagonistic interaction. Consistent with previous results, SC83288 was found to be a fast acting compound, although SC83288 is not as rapid regarding its in vitro speed of action as are artemisinins [20]. Furthermore, combining SC83288 with artesunate did not affect the in vitro speed of action of either drug, allowing for the possibility of a combination therapy.
Methods
Chemicals
The chemicals used in this study were obtained from the Roth, Merck, Sigma, Serva, Thermo and Applichem. SC83288 was provided by the 4SC AG, München, Germany.
Parasite culture
Plasmodium falciparum parasites were maintained in continuous in vitro culture essentially as previously described [48]. Briefly, cultures were maintained at a haematocrit of 5.0% and at a parasitaemia of not higher than 5% (if not stated otherwise) in RPMI 1640 supplemented with 2 mM l-glutamine, 25 mM HEPES, 100 µM hypoxanthine, 20 µg ml−1 gentamycin, 5% human heat-inactivated AB-positive serum and 5% Albumax. Cultures were incubated at 37 °C under controlled atmospheric conditions of 5% O2, 3% CO2, 92% N2 and 96% humidity. Synchronization of cultures at the ring stage was performed using a 5% sorbitol solution as previously described [49].
Plasmodium falciparum growth inhibition assay
Growth inhibition assays were performed according to a standardized protocol, based on the detection of parasite DNA by fluorescent SYBRGreen staining [50, 51]. Briefly, synchronized cultures of P. falciparum ring-stage parasites were incubated in the presence of increasing drug concentrations, at the following final condition: 100 µl per well, 0.5% parasitaemia, 2% haematocrit, 72 h incubation at 37 °C. After incubation, the plates were frozen at − 80 °C overnight. On the day of the measurement, plates were thawed for 1 h at room temperature. The plates were filled with 100 µl per well of a 1× SYBRGreen (ThermoFisher Scientific Inc.) solution in lysis buffer (H20, 20 mM Tris base pH 7.4, 5 mM EDTA, 0.008% (w/v) Saponin, 0.08% (w/v) Triton X-100), briefly shaken and incubated at room temperature for 1 h. Plates were protected from direct light. Fluorescence was measured in a fluorescence plate reader (FluoStar Optima, BMG Labtech GmbH) (ext/em: 485/520 nm, gain 1380, 10 flashes/well, top optic). The IC50 values were calculated using a four parameter sigmoidal function (SigmaPlot 13, Systat Software Inc.). 6–13 independent biological replicates were performed, each with technical duplicates.
Ring survival assay
The in vitro ring survival assay (RSA) rate was assessed as previously described [52]. Briefly, tightly synchronized early ring parasites (0–3 h post invasion) at a parasitaemia of 0.5–1% were exposed to various drugs at a concentration of 700 nM for 6 h. The drug was subsequently washed-out, and the parasites were returned to culture for 66 h before being collected. DNA content analysis was performed by flow cytometry on SYBRGreen-stained parasites to measure the precise parasitaemia, as previously described [53], using a BD FACS Canto. Briefly, the parasites were fixed in PBS 4% paraformaldehyde, 0.0075% glutaraldehyde for 2 h at room temperature and permeabilized in PBS 0.1% Triton-100 for 8 min. The samples were subsequently subjected to a light RNase treatment (0.3 mg/ml in PBS) for 30 min at 37 °C. DNA was stained with SYBRGreen (1:2000 dilution in PBS) for 20 min in the dark. Parasites were then transferred to tubes adapted for flow cytometry. The fluorescence signal was collected in the green channel (FITC-H) of the FACS Canto. A minimum of 2000 infected red blood cells were counted per measurement and plotted in the form of dot-plots, using the software FlowingSoftware2.5.1. Parasites survival rates [RSA score (%)] were expressed as a percentage, by comparing the parasitaemia between the drug-treated and the untreated control as followed:
3–6 independent biological replicates were performed, each with technical duplicates.
Drug interaction study
The interaction profile was assessed using the P. falciparum strain Dd2 and the fixed-ratio isobologram method [54]. This approach is based on determining the IC50 values of two individual drugs alone and in combination at different concentration ratios. In principle, the shift of a drug’s IC50 value, assessed in combination compared to the one determined for this drug alone, is indicative of the nature of the interaction between the two drugs [54]. Briefly, a synchronous culture of ring-stage P. falciparum blood-stage parasites was incubated for 72 h in the presence of increasing drug concentrations in a 96-well black microtiter plate. The final conditions of the tests were 100 µl per well, 0.5% parasitaemia, 2% final haematocrit and 72 h incubation time at 37 °C. On the day of the assay, a synchronized ring-stage culture, was established at 0.5% parasitaemia and 4% haematocrit. A solution of uninfected erythrocytes at 4% haematocrit was used as a negative control. Drugs were applied alone (A or B) and in combination at fixed concentration ratios (A:B) and analysed in threefold serial dilutions. Drug mixtures were prepared from 2x working solutions of each drug in the following fixed concentration ratios (v/v): ratio A:B = 4:1, 3:2, 2.5:2.5, 2:3, 1:4, directly in the 96-well plate. IC50 values of drugs A and B alone were determined on the same plate to ensure accurate calculation of drug interactions. After 72 h of incubation, plates were wrapped in aluminum foil and frozen at − 80 °C overnight. Parasite growth was assessed using SYBRGreen as described above. Graphical analysis was performed on isobolograms, obtained by plotting pairs of fractional IC50 (FIC50) values of drug A and drug B for each combination. The in vitro interactions were evaluated based on graphical and arithmetical analysis. It is commonly accepted that a mean sum of fractional 50% inhibitory concentrations (mean ∑FIC50) lower than 0.5 corresponds to a synergistic interaction, and higher than 1.5 to an antagonistic interaction [55]. A mean ∑FIC50 between these two cut-off values represents an indifferent interaction between the two investigated drugs. 7 independent biological replicates were performed, each with technical duplicates.
In vitro speed of action
Two independent methods were used to determine the in vitro speed of action of drugs. The relative speed of action was obtained following the approach previously described by Le Manach et al. [56]. Briefly, the growth of an asynchronous parasite blood culture in the presence of anti-malarial compounds was assessed using SYBRGreen staining and expressed as IC50 values, as described above. For each compound, three exposure times were employed 72 (standard assay time), 48 and 24 h. The IC50 ratios, normalized to the 72 h exposure were subsequently used to classify the compound as fast- or slow-acting. The absolute speed of action was obtained using the method described by Linnares et al. [57]. Briefly an asynchronous culture of P. falciparum Dd2 blood-stage parasites, at 0.5% parasitaemia and 4% haematocrit was treated with a concentration corresponding to 10 × IC50 for a duration of 8, 14, 24, 48 or 72 h, in a final volume of 100 µl per well. Drugs were refreshed every 24 h. After incubation, the parasites were washed-out in drug free medium and resuspended in 100 µl of medium. 70 µl were then transferred into a fresh plate, containing 130 µl of CFDA-stained uninfected erythrocytes at 2% haematocrit, resulting in a 1/3 dilution. After 48 h of subsequent incubation at 37 °C, the parasites were washed in PBS, and the DNA was stained using Draq5 (1:500 dilution in PBS) for 20 min at room temperature. The samples were washed once with PBS and fixed in PBS 0.05% glutaraldehyde for 1 h at room temperature. The fixed samples were kept in PBS at 4 °C until flow cytometry analysis, using a BD FACS Canto. Collecting fluorescence signals in the FITC and the PerCP-Cy5 channel allowed the proportion of the double stained infected erythrocytes to be determined, which corresponds to the new infections. Results were displayed in the form of dot-plots, using the software FlowingSoftware2.5.1. The total infections were calculated as followed:
The parasite viability was then expressed as a percentage of the untreated parasites. 4 independent biological replicates were performed, each with technical duplicates.
Results
SC83288 shows no cross-resistance with artemisinins
The matter of cross-resistance between SC83288 and artemisinins was initially addressed, using two distinct approaches. On the one hand, standard growth inhibition assays over 72 h of drug exposure were performed, and on the other hand, the susceptibility of early ring stages in a ring survival assay (RSA) was evaluated. The RSA takes into account the antiplasmodial activity of artemisinin and its derivatives against the early blood stages [36, 52]. Four different strains of P. falciparum were used in these assays: the artemisinin and SC83288 sensitive P. falciparum strains NF54 and Dd2, the genetically engineered artemisinin-resistant NF54 mutant line bearing a mutation in the kelch 13 gene (PfK13 C580Y), an established marker of artemisinin resistance [52], and a Dd2 derived SC83288 resistant line [20]. The two drug resistant clones were termed NF54ART and Dd2SC.
In the growth inhibition assay, the wild-type NF54 line and the NF54ART mutant displayed no significant difference in their dihydroartemisinin responsiveness, with IC50 value of 0.7 ± 0.1 and 0.5 ± 0.1 nM, respectively (Student’s t test, p = 0.9) (Table 1 and Fig. 2a). Both strains had also comparable susceptibilities to SC83288, with IC50 values of 5.1 ± 0.7 and 4.9 ± 0.8 nM, respectively (Student’s t test, p = 0.2) (Table 1 and Fig. 2b). In comparison, Dd2SC and the parental Dd2 strain revealed comparable IC50 values to dihydroartemisinin (0.5 ± 0.1 and 0.7 ± 0.1 nM, respectively, Student’s t test, p = 0.8) (Table 1 and Fig. 2c) but different responses to SC83288 (1.0 ± 0.2 µM and 3.1 ± 0.2 nM, respectively, Student’s t test, p < 0.001) (Table 1 and Fig. 2d).
Susceptibility of different P. falciparum strains to SC83288 and dihydroartemisinin. a and b Growth inhibition of NF54 and the artemisinin resistant derivative NF54ART carrying the PfK13 C580Y mutation by artemisinin (a) and SC83288 (b) in a standard cell proliferation assay with an exposure time of 72 h. c and d Growth inhibition of Dd2 and the SC83288 resistant derivative Dd2SC by artemisinin (c) and SC83288 (d). Mean ± SEM of 6–13 independent determinations
Artemisinins have been shown to exert part of their antiplasmodial activity against very early ring-stages parasites, just after erythrocyte invasion [58, 59]. As expected [52], the NF54ART line showed a significant difference in its RSA score to dihydroartemisinin (DHA) compared to the wild-type NF54 strain (RSA score of 11.5 ± 1.5 and 24.1 ± 1.9%, respectively, Student’s t test, p < 0.001). In comparison, Dd2 and Dd2SC had low and comparable RSA scores of 9.9 ± 2.7 and 7.7 ± 0.3%, respectively (One-Way ANOVA Holm-Sidak test, p = 0.2), indicative of artemisinin susceptibility (Fig. 3a). Importantly, none of the parasites lines showed a ring-stage susceptibility to SC83288 (RSA score of 111.0 ± 3.0, 95.7 ± 2.7, 91.4 ± 5.1 and 90.1 ± 3.3%, for Dd2, Dd2SC, NF54, and NF54ART, respectively; One-Way ANOVA Holm-Sidak test, p = 0.8) (Fig. 3b), confirming the lack of activity of SC83288 against early ring-stages [20]. Taken together, the data from these two independent assays strongly suggest against any kind of cross-resistance effects between artemisinins and SC83288 in vitro.
Ring stage susceptibility of different P. falciparum strains to dihydroartemisinin and SC83288. a Ring survival assay (RSA) scores of NF54, NF54ART, Dd2, and Dd2SC to dihydroartemisinin (DHA). b RSA scores to SC83288. Mean ± SEM of 3–6 independent determinations. Statistical significance was evaluated using the one way ANOVA Holm-Sidak test. ***p < 0.001; n.s. not significant
SC83288 and artemisinin do not interact
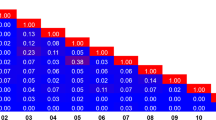
Subsequently, the question was addressed of whether artemisinin and SC83288 have an effect on one another when combined in a growth inhibition assay. To this end, the interaction profile between artemisinin and SC83288 using a fixed-ratio isobologram method [54] was investigated. A synchronous culture of Dd2 at the ring stage for 72 h was incubated in the presence of increasing drug concentrations, whereby artemisinin and SC83288 were applied alone and in combination at fixed concentration ratios. The arithmetical analysis revealed a mean sum of fractional 50% inhibitory concentrations (mean ∑FIC50) of 0.97 ± 0.06, suggestive of an indifferent interaction. The graphical analysis on the isobologram, obtained by plotting the pairs of fractional IC50 (FIC50) values of artemisinin and SC83288 for each combination, agreed with the arithmetical observation, following almost perfectly the diagonal trend line (fit to a linear polynomial curve with a R2 = 0.972) (Fig. 4), thereby corroborating the conclusion that both drugs do not interact.
Indifferent interaction between artemisinin and SC83288. The fractional half-maximal inhibitory concentrations (FIC50) of artemisinin and SC83288 in the P. falciparum strain Dd2 were displayed in an isobologram. A linear regression was fitted to the data points. Mean ± SEM of 7 independent determinations
Combining SC83288 and artesunate does not affect the in vitro speed of action
First, the in vitro killing speed of SC83288 was determined according to the method developed by Le Manach et al. [56], which classifies drugs as slow- or fast-acting based on a relative in vitro speed of action. To this end, growth inhibition assays were performed, using asynchronous cultures of Dd2, and assessed parasite growth after drug exposure of 24, 48 and 72 h. The IC50 ratios were subsequently normalized to the standard 72 h incubation assay. For comparative reasons, artemisinin and atovaquone were analysed in parallel. The IC50 ratios of SC82388 were independent of the exposure time (1.28 ± 0.08, 1.24 ± 0.05 and 1.00 ± 0.06 for 24, 48 and 72 h of drug exposure, respectively; One-way ANOVA Holm-Sidak test, p = 0.3), indicating a fast mode of action. Similarly, the exposure time did not affect the IC50 ratios of artemisinin (0.97 ± 0.07, 0.88 ± 0.01 and 1.00 ± 0.01 for 24, 48 and 72 h of treatment, respectively; One-way ANOVA Holm-Sidak test, p = 0.2). In comparison, the IC50 ratios of atovaquone were significantly different (3.4 ± 0.1, 1.35 ± 0.04 and 1.00 ± 0.04, for 24, 48 and 72 h of treatment, respectively; One-way ANOVA Holm-Sidak test, p < 0.001) (Fig. 5), consistent with atovaquone being a slow acting anti-malarial [56, 57, 60].
IC50-based relative speed of action profiles of SC83288, artemisinin, and atovaquone. The IC50 values of artemisinin, atovaquone and SC83288 were determined at exposure times of 24, 48 and 72 h in the P. falciparum Dd2 strain [56]. The data are shown normalized to the value obtained at the 72 h time point. Mean ± SEM of 6 independent determinations. Statistical significance was evaluated using the one way ANOVA Holm-Sidak test. ***p < 0.001; n.s. not significant
In order to identify possible detrimental interactions between the drugs in the prospect of a potential combination therapy, a second approach was employed to evaluate the absolute speed of action of SC83288, alone as well as in combination with artesunate or atovaquone, based on the method of Linares et al. [57]. To this end, asynchronous cultures of Dd2 were treated with 10x IC50 concentrations of SC82388, artesunate or atovaquone, alone or in combination, for a duration of 8, 14, 24, 48 or 72 h. After washing-out the drugs, the parasites were cultured with uninfected erythrocytes stained with a live cells marker, the esterase substrate carboxyfluorescein diacetate (cFDA). After 48 h of subsequent incubation, the DNA of the parasite was stained with Draq5 and the amount of cFDA and Draq5 stained cells was determined by flow cytometry. The results of this assay classified SC83288 as a fast-acting anti-malarial compound, with a 90% parasite clearance time (PCT90%) of 17 ± 3 h. In comparison, the measured PCT90% of artesunate and atovaquone were 11 ± 1 h and > 80 h, respectively (Fig. 6). Combining artesunate and SC83288 did not lead to a significant difference in the PCT90% compared with artesunate alone (9.0 ± 0.5 h, Student’s t test, p = 0.1) (Fig. 6). Similarly, combining SC83288 with atovaquone did not significantly alter the PCT90% of SC83288 alone (17 ± 6 h Student’s t test, p = 0.4) (Fig. 6).
Killing rate profile for artesunate, SC83288, atovaquone, alone and in combination. Asynchronous cultures of Dd2 were exposed to 10-times the IC50 concentration of SC82388, artesunate, or atovaquone, alone or in combination, for a duration of 8, 14, 24, 48 or 72 h before the number of re-invading parasites were determined as an indicator of parasite viability. Data were normalized to untreated controls analysed in parallel. Mean ± SEM of four independent determinations
Discussion
Understanding the mode of action and the mechanism of resistance of a therapeutic agent is not mandatory for a compound to be released on the market. However, information regarding these processes may help to predict and control interactions of the compound with the environment and with other drugs deployed in the field. To this purpose, the antiplasmodial action of SC83288 was profiled against artemisinin and artemisinin derivatives in P. falciparum.
The parasite reduction ratio after a single dose, i.e. the speed of action of the molecule, is a quality feature of an anti-malarial drug as recently emphasized by the Medicine for Malaria Venture (MMV) [61]. Particularly, drugs against severe malaria are expected to rapidly clear sequestered parasites from the patient´s microvasculature, which can make the difference between survival and death. Moreover, fast-acting anti-malarial drugs are favoured for their ability to reduce the risks of resistant parasites arising within the patient. To this day, the artemisinin derivatives remain the gold standards of a rapidly clearing anti-malarial, reducing the parasite burden within hours [2]. SC83288 has previously been characterized as a fast-acting anti-malarial compound in vitro [20] using a recrudescence assay [60]. Under these conditions, the SC83288 speed of action profile was closer to the fast-acting artemisinin than to the slow-acting atovaquone, although the SC83228 showed a slightly longer clearance time and a lower parasite reduction ratio compared to artemisinin [20]. On a direct clearance-time measurement using trophozoites, SC83288, however, revealed a higher activity than artemisinin [20], consistent with the potent antiplasmodial activity of SC83288 on trophozoites [20]. In this study, the killing speed of SC83288 was verified, using two other methods: a relative speed assay [56], and a re-invasion assay [57]. The results of these assays were consistent with previous observations, marking SC83288 as a fast-acting anti-malarial compound (Figs. 5 and 6), with an in vitro killing speed profile closer to artesunate than to atovaquone (Fig. 6). Further, combining SC83288 with artesunate did not significantly impair the speed of action (Fig. 6). The speed of action is, however, not the only crucial aspect that needs to be taken into account when developing an anti-malarial compound. As for any xenobiotic molecule, the beneficial versus adverse effects must be carefully weighed, and parameters such as safety, pharmacokinetics and drug–drug interactions need to be considered. In this regard, preliminary results on the safety and toxicology of SC83288 in mice and dogs are promising, although a full assessment would await clinical trials in humans. This study further revealed no obvious in vitro interactions between artemisinin and SC83288 in the P. falciparum strain Dd2 (Fig. 4). Both the graphical and arithmetical analysis of our isobologram method supported this observation, with the isobologram following a linear trend, and a mean sum of fractional 50% inhibitory concentration falling within the range of an indifferent interaction [55]. An isobologram may overlook possible similar modes of action, particularly if the two tested compounds are both either competitive inhibitors or mutually exclusive non-competitive inhibitors [55]. Competition of both compounds for the same binding site, independently of an interference with the binding site of the endogenous substrate, would not be noticed in an isobologram [55]. However, the chemical and structural differences between SC83288 and the artemisinins (Fig. 1) strongly argue against this possibility.
Resistance is another key aspect of the MMV’s drug candidate profile. Indeed, resistance to most marketed anti-malarial drugs, either previously or still currently used to treat a P. falciparum infection, has been identified worldwide to various degrees [62, 63]. Thus, novel drugs need to overcome existing mechanisms of resistance. A previous study has shown that SC83288 is active in vitro against various P. falciparum laboratory strains that are resistant to quinoline, quinoline-like and antifolate anti-malarials [20]. This study extends these findings to include the artemisinin resistant parasite strain NF54ART that carry the kelch 13 mutation associated with reduced artemisinin responsiveness. SC83288 was found to be active against NF54ART. Conversely, resistance to SC83288 did not affect the susceptibility of the parasite to other anti-malarial drugs, including artemisinins, chloroquine, mefloquine and the folate antagonists [20].
Conclusion
While this study does not provide molecular insights into the precise mode of action of SC83288, or into the possible mechanism of resistance, our study suggests that artemisinins and SC83288 target different molecular pathways, based on the absence of cross-reactivity in several independent assays. The absence of cross-resistance and the ability to break established resistances against several anti-malarial drugs, together with a fast in vitro parasite killing speed, are favourable features of SC83288 and would support further development of this compound, possibly as a treatment against severe malaria. Whether SC83288 can be an alternative to artesunate for the treatment of severe malaria, however, has to await clinical safety and efficacy trials in humans.
References
WHO. World malaria report 2017. Geneva: World Health Organization; 2017.
WHO. Guidelines for the treatment of malaria. Geneva: World Health Organization; 2015.
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, et al. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009;361:455–67.
Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S, et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2014;371:411–23.
Thanh NV, Thuy-Nhien N, Tuyen NTK, Tong NT, Nha-Ca NT, Dong LT, et al. Rapid decline in the susceptibility of Plasmodium falciparum to dihydroartemisinin–piperaquine in the south of Vietnam. Malar J. 2017;16:27.
Jiménez-Díaz MB, Ebert D, Salinas Y, Pradhan A, Lehane AM, Myrand-Lapierre M-E, et al. (+)-SJ733, a clinical candidate for malaria that acts through ATP4 to induce rapid host-mediated clearance of Plasmodium. Proc Natl Acad Sci USA. 2014;111:E5455–62.
Nilsen A, LaCrue AN, White KL, Forquer IP, Cross RM, Marfurt J, et al. Quinolone-3-diarylethers: a new class of antimalarial drug. Sci Transl Med. 2013;5:177ra37.
Ramachandran S, Hameed PS, Srivastava A, Shanbhag G, Morayya S, Rautela N, et al. N-aryl-2-aminobenzimidazoles: novel, efficacious, antimalarial lead compounds. J Med Chem. 2014;57:6642–52.
Hameed PS, Solapure S, Patil V, Henrich PP, Magistrado PA, Bharath S, et al. Triaminopyrimidine is a fast-killing and long-acting antimalarial clinical candidate. Nat Commun. 2015;6:6715.
Coslédan F, Fraisse L, Pellet A, Guillou F, Mordmüller B, Kremsner PG, et al. Selection of a trioxaquine as an antimalarial drug candidate. Proc Natl Acad Sci USA. 2008;105:17579–84.
Held J, Jeyaraj S, Kreidenweiss A. Antimalarial compounds in Phase II clinical development. Exp Opin Investig Drugs. 2015;24:363–82.
Vial HJ, Wein S, Farenc C, Kocken C, Nicolas O, Ancelin ML, et al. Prodrugs of bisthiazolium salts are orally potent antimalarials. Proc Natl Acad Sci USA. 2004;101:15458–63.
Charman SA, Arbe-Barnes S, Bathurst IC, Brun R, Campbell M, Charman WN, et al. Synthetic ozonide drug candidate OZ439 offers new hope for a single-dose cure of uncomplicated malaria. Proc Natl Acad Sci USA. 2011;108:4400–5.
Sonoiki E, Ng CL, Lee MCS, Guo D, Zhang Y-K, Zhou Y, et al. A potent antimalarial benzoxaborole targets a Plasmodium falciparum cleavage and polyadenylation specificity factor homologue. Nat Commun. 2017;8:14574.
Phyo AP, Jittamala P, Nosten FH, Pukrittayakamee S, Imwong M, White NJ, et al. Antimalarial activity of artefenomel (OZ439), a novel synthetic antimalarial endoperoxide, in patients with Plasmodium falciparum and Plasmodium vivax malaria: an open-label phase 2 trial. Lancet Infect Dis. 2016;16:61–9.
White NJ, Pukrittayakamee S, Phyo AP, Rueangweerayut R, Nosten F, Jittamala P, et al. Spiroindolone KAE609 for falciparum and vivax malaria. N Engl J Med. 2014;371:403–10.
Leong FJ, Zhao R, Zeng S, Magnusson B, Diagana TT, Pertel P. A first-in-human randomized, double-blind, placebo-controlled, single- and multiple-ascending oral dose study of novel Imidazolopiperazine KAF156 to assess its safety, tolerability, and pharmacokinetics in healthy adult volunteers. Antimicrob Agents Chemother. 2014;58:6437–43.
White NJ, Duong TT, Uthaisin C, Nosten F, Phyo AP, Hanboonkunupakarn B, et al. Antimalarial activity of KAF156 in falciparum and vivax malaria. N Engl J Med. 2016;375:1152–60.
Phillips MA, Lotharius J, Marsh K, White J, Dayan A, White KL, et al. A long-duration dihydroorotate dehydrogenase inhibitor (DSM265) for prevention and treatment of malaria. Sci Transl Med. 2015;7:296ra111.
Pegoraro S, Duffey M, Otto TD, Wang Y, Rösemann R, Baumgartner R, et al. SC83288 is a clinical development candidate for the treatment of severe malaria. Nat Commun. 2017;8:14193.
Arnou B, Morth JP, Nissen P, Jaxel C, Møller JV, Maire M. The Plasmodium falciparum Ca2+-ATPase PfATP6: insensitive to artemisinin, but a potential drug target. Biochem Soc Trans. 2011;39:823–31.
Meshnick SR. Artemisinin: mechanisms of action, resistance and toxicity. Int J Parasitol. 2002;32:1655–60.
O’Neill PM, Barton VE, Ward SA. The molecular mechanism of action of artemisinin—the debate continues. Molecules. 2010;15:1705–21.
Eckstein-Ludwig U, Webb RJ, Van Goethem IDA, East JM, Lee AG, Kimura M, et al. Artemisinins target the SERCA of Plasmodium falciparum. Nature. 2003;424:957–61.
Krishna S, Pulcini S, Moore CM. Teo BH-Y, Staines HM. Pumped up: reflections on PfATP6 as the target for artemisinins. Trends Pharmacol Sci. 2014;35:4–11.
Uhlemann A-C, Cameron A, Eckstein-Ludwig U, Fischbarg J, Iserovich P, Zuniga FA, et al. A single amino acid residue can determine the sensitivity of SERCAs to artemisinins. Nat Struct Mol Biol. 2005;12:628–9.
Bertaux L, Quang LH, Sinou V, Thanh NX, Parzy D. New PfATP6 mutations found in Plasmodium falciparum isolates from Vietnam. Antimicrob Agents Chemother. 2009;53:4570–1.
Pillai DR, Lau R, Khairnar K, Lepore R, Via A, Staines HM, et al. Artemether resistance in vitro is linked to mutations in PfATP6 that also interact with mutations in PfMDR1 in travellers returning with Plasmodium falciparum infections. Malar J. 2012;11:131.
Pulcini S, Staines HM, Pittman JK, Slavic K, Doerig C, Halbert J, et al. Expression in yeast links field polymorphisms in pfatp6 to in vitro artemisinin resistance and identifies new inhibitor classes. J Infect Dis. 2013;208:468–78.
Cardi D, Pozza A, Arnou B, Marchal E, Clausen JD, Andersen JP, et al. Purified E255L mutant SERCA1a and purified PfATP6 are sensitive to SERCA-type inhibitors but insensitive to artemisinins. J Biol Chem. 2010;285:26406–16.
David-Bosne S, Clausen MV, Poulsen H, Møller JV, Nissen P, le Maire M. Reappraising the effects of artemisinin on the ATPase activity of PfATP6 and SERCA1a E255L expressed in Xenopus laevis oocytes. Nat Struct Mol Biol. 2016;23:1–2.
Imwong M, Dondorp AM, Nosten F, Yi P, Mungthin M, Hanchana S, et al. Exploring the contribution of candidate genes to artemisinin resistance in Plasmodium falciparum. Antimicrob Agents Chemother. 2010;54:2886–92.
Adhin MR, Labadie-Bracho M, Vreden SG. Status of potential PfATP6 molecular markers for artemisinin resistance in Suriname. Malar J. 2012;11:322.
Cui L, Wang Z, Jiang H, Parker D, Wang H, Su X-Z, et al. Lack of association of the S769N mutation in Plasmodium falciparum SERCA (PfATP6) with resistance to artemisinins. Antimicrob Agents Chemother. 2012;56:2546–52.
Miao M, Wang Z, Yang Z, Yuan L, Parker DM, Putaporntip C, et al. Genetic diversity and lack of artemisinin selection signature on the Plasmodium falciparum ATP6 in the Greater Mekong Subregion. PLoS ONE. 2013;8:e59192.
Tilley L, Straimer J, Gnädig NF, Ralph SA, Fidock DA. Artemisinin action and resistance in Plasmodium falciparum. Trends Parasitol. 2016;32:682–96.
Witkowski B, Amaratunga C, Khim N, Sreng S, Chim P, Kim S, et al. Novel phenotypic assays for the detection of artemisinin-resistant Plasmodium falciparum malaria in Cambodia: in vitro and ex vivo drug-response studies. Lancet Infect Dis. 2013;13:1043–9.
Mok S, Ashley EA, Ferreira PE, Zhu L, Lin Z, Yeo T, et al. Drug resistance. Population transcriptomics of human malaria parasites reveals the mechanism of artemisinin resistance. Science. 2015;347:431–5.
Takala-Harrison S, Clark TG, Jacob CG, Cummings MP, Miotto O, Dondorp AM, et al. Genetic loci associated with delayed clearance of Plasmodium falciparum following artemisinin treatment in Southeast Asia. Proc Natl Acad Sci USA. 2013;110:240–5.
Cheeseman IH, Miller BA, Nair S, Nkhoma S, Tan A, Tan JC, et al. A major genome region underlying artemisinin resistance in malaria. Science. 2012;336:79–82.
Miotto O, Almagro-Garcia J, Manske M, MacInnis B, Campino S, Rockett KA, et al. Multiple populations of artemisinin-resistant Plasmodium falciparum in Cambodia. Nat Genet. 2013;45:648–55.
Ariey F, Witkowski B, Amaratunga C, Beghain J, Langlois A-C, Khim N, et al. A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature. 2014;505:50–5.
Isozumi R, Uemura H, Kimata I, Ichinose Y, Logedi J, Omar AH, et al. Novel mutations in K13 propeller gene of artemisinin-resistant Plasmodium falciparum. Emerg Infect Dis. 2015;21:490–2.
Straimer J, Gnadig NF, Witkowski B, Amaratunga C, Duru V, Ramadani AP, et al. K13-propeller mutations confer artemisinin resistance in Plasmodium falciparum clinical isolates. Science. 2015;347:428–31.
Nyunt MH, Hlaing T, Oo HW, Tin-Oo L-LK, Phway HP, Wang B, et al. Molecular assessment of artemisinin resistance markers, polymorphisms in the K13 propeller, and a multidrug-resistance gene in the eastern and western border areas of Myanmar. Clin Infect Dis. 2015;60:1208–15.
Pillai DR, Alemu A, Getie S, Bayih AG, Mohon AN, Getnet G. A unique Plasmodium falciparum K13 gene mutation in Northwest Ethiopia. Am J Trop Med Hyg. 2016;94:132–5.
Adams J, Kelso R, Cooley L. The kelch repeat superfamily of proteins: propellers of cell function. Trends Cell Biol. 2000;10:17–24.
Trager W, Jensen JB. Human malaria parasites in continuous culture. Science. 1976;193:673–5.
Lambros C, Vanderberg JP. Synchronization of Plasmodium falciparum erythrocytic stages in culture. J Parasitol. 1979;65:418–20.
Smilkstein M, Sriwilaijaroen N, Kelly JX, Wilairat P, Riscoe M. Simple and inexpensive fluorescence-based technique for high-throughput antimalarial drug screening. Antimicrob Agents Chemother. 2004;48:1803–6.
Sriwilaijaroen N, Boonma S, Attasart P, Pothikasikorn J, Panyim S, Noonpakdee W. Inhibition of Plasmodium falciparum proliferation in vitro by double-stranded RNA directed against malaria histone deacetylase. Biochem Biophys Res Commun. 2009;381:144–7.
Mbengue A, Bhattacharjee S, Pandharkar T, Liu H, Estiu G, Stahelin RV, et al. A molecular mechanism of artemisinin resistance in Plasmodium falciparum malaria. Nature. 2015;520:683–7.
Ganter M, Goldberg JM, Dvorin JD, Paulo JA, King JG, Tripathi AK, et al. Plasmodium falciparum CRK4 directs continuous rounds of DNA replication during schizogony. Nat Microbiol. 2017;2:17017.
Fivelman QL, Adagu IS, Warhurst DC. Modified fixed-ratio isobologram method for studying in vitro interactions between atovaquone and proguanil or dihydroartemisinin against drug-resistant strains of Plasmodium falciparum. Antimicrob Agents Chemother. 2004;48:4097–102.
Bell A. Antimalarial drug synergism and antagonism: mechanistic and clinical significance. FEMS Microbiol Lett. 2005;253:171–84.
Le Manach C, Scheurer C, Sax S, Schleiferböck S, Cabrera D, Younis Y, et al. Fast in vitro methods to determine the speed of action and the stage-specificity of anti-malarials in Plasmodium falciparum. Malar J. 2013;12:424.
Linares M, Viera S, Crespo B, Franco V, Gómez-Lorenzo MG, Jiménez-Díaz MB, et al. Identifying rapidly parasiticidal anti-malarial drugs using a simple and reliable in vitro parasite viability fast assay. Malar J. 2015;14:441.
Klonis N, Xie SC, McCaw JM, Crespo-Ortiz MP, Zaloumis SG, Simpson JA, et al. Altered temporal response of malaria parasites determines differential sensitivity to artemisinin. Proc Natl Acad Sci USA. 2013;110:5157–62.
Xie SC, Dogovski C, Hanssen E, Chiu F, Yang T, Crespo MP, et al. Haemoglobin degradation underpins the sensitivity of early ring stage Plasmodium falciparum to artemisinins. J Cell Sci. 2016;129:406–16.
Sanz LM, Crespo B, De-Cózar C, Ding XC, Llergo JL, Burrows JN, et al. P. falciparum in vitro killing rates allow to discriminate between different antimalarial mode-of-action. PLoS ONE. 2012;7:e30949.
Burrows JN, Duparc S, Gutteridge WE, Hooft van Huijsduijnen R, Kaszubska W, Macintyre F, et al. New developments in anti-malarial target candidate and product profiles. Malar J. 2017;16:26.
World Health Organization. Global report on antimalarial efficacy and drug resistance: 2000–2010. Geneva: World Health Organization; 2010.
Blasco B, Leroy D, Fidock DA. Antimalarial drug resistance: linking Plasmodium falciparum parasite biology to the clinic. Nat Med. 2017;23:917–28.
Authors’ contribution
MD, CPS, and ML designed this study, MD and ML analysed the data and wrote the manuscript. CPS generated the SC83288 resistant P. falciparum strain. MD performed the experimental work. All authors read and approved the final manuscript.
Acknowledgements
We thank Marina Müller and Stefan Prior for excellent technical assistance. We are grateful to Prof. Marcel Deponte for advices and guidance. We thank Prof. Alexander Dalpke for allowing us to use his group´s flow cytometer. We are thankful to Dr. Stefanie Fehler for the SC83288 supply and the coordination with the 4SC AG.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets and analysis algorithm used during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
The research leading to these results has received funding from the Bundesministerium für Bildung und Forschung under the portfolio of the German Centre for Infectious Research (DZIF) (Project TTU 03.803).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Duffey, M., Sanchez, C.P. & Lanzer, M. Profiling of the anti-malarial drug candidate SC83288 against artemisinins in Plasmodium falciparum. Malar J 17, 121 (2018). https://doi.org/10.1186/s12936-018-2279-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-018-2279-4