Abstract
Objective
The incidence of non-virus-related hepatocellular carcinoma (NV-HCC) in hepatocellular carcinoma (HCC) is steadily increasing. The aim of this study was to establish a prognostic model to evaluate the overall survival (OS) of NV-HCC patients.
Methods
Overall, 261 patients with NV-HCC were enrolled in this study. A prognostic model was developed by using LASSO-Cox regression analysis. The prognostic power was appraised by the concordance index (C-index), and the time-dependent receiver operating characteristic curve (TD-ROC). Kaplan–Meier (K–M) survival analysis was used to evaluate the predictive ability in the respective subgroups stratified by the prognostic model risk score. A nomogram for survival prediction was established by integrating the prognostic model, TNM stage, and treatment.
Results
According to the LASSO-Cox regression results, the number of nodules, lymphocyte-to-monocyte ratio (LMR), prognostic nutritional index (PNI), alkaline phosphatase (ALP), aspartate aminotransferase (AST)/alanine aminotransferase (ALT) ratio (SLR) and C-reactive protein (CRP) were included for prognostic model construction. The C-index of the prognostic model was 0.759 (95% CI 0.723–0.797) in the development cohort and 0.796 (95% CI 0.737–0.855) in the validation cohort, and its predictive ability was better than TNM stage and treatment. The TD-ROC showed similar results. K–M survival analysis showed that NV-HCC patients with low risk scores had a better prognosis (P < 0.05). A nomogram based on the prognostic model, TNM stage, and treatment was constructed with sufficient discriminatory power with C-indexes of 0.78 and 0.85 in the development and validation cohort, respectively.
Conclusion
For NV-HCC, this prognostic model could predict an OS benefit for patients, which may assist clinicians in designing individualized therapeutic strategies.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is one of the most dominant malignant tumours in the world, and there are more than 840,000 new cases and over 780,000 deaths per year [1, 2]. Risk factors for HCC include hepatitis B virus (HBV) and hepatitis C virus (HCV), alcohol addiction, nonalcoholic fatty liver disease, obesity, diabetes mellitus, moldy food containing aflatoxin and so on [3]. Patients infected with HBV or HCV accounted for over 80% of HCC cases [4]. However, changing lifestyles and increasing HBV vaccination rates and more efficacious antiviral treatments have changed the global epidemiology of HCC [5]. The incidence of non-virus-related HCC (NV-HCC) is increasing due to fatty liver disease, obesity and insulin resistance [6]. Studies have shown that HBV deoxyribonucleic acid (DNA) may lead to worse liver function and more complications [7]. Thus, HCC patients with HBV have lower overall survival (OS) and disease-free survival (DFS) than NV-HCC patients [8, 9]. These results indicate that NV-HCC and hepatitis B-positive HCC have different clinicopathological features, prognostic factors and clinical outcomes. Thus, a distinct prognostic model for NV-HCC is needed. Recently, numerous prognostic survival models have been established for HCC patients [10, 11]. However, there are few reports on prognostic models for NV-HCC. Therefore, to facilitate clinical counseling and the individualized prediction of survival for NV-HCC, it is necessary to construct a new prognostic model to assess the specific prognosis of NV-HCC.
Numerous studies have reported that clinical characteristics and routine laboratory examinations of blood are prognostic predictors for HCC, including tumor size, HBV DNA [12], alpha-fetoprotein (AFP) [13], neutrophil/lymphocyte ratio (NLR) [14], and alkaline phosphatase (ALP) [15]. Increasing AFP levels were associated with worse survival and higher recurrence rates in patients with HCC [16]. Witjes et al. reported that high AST levels were linked to worse OS in patients with HCC [17]. The NLR is a prognostic factor affecting survival and recurrence in living-donor liver transplantation for HCC [18]. Based on ALP, tumor size, liver cirrhosis, microvascular invasion, and other factors, a nomogram was established to evaluate the prognosis of HCC [12]. However, it is a challenge to screen and combine multiple factors into a prognostic system for NV-HCC.
Materials and methods
Patients and laboratory analysis
HCC patients at Sun Yat-sen University Cancer Center from January 2013 to December 2016 were retrospectively reviewed. The inclusion criteria were as follows: (a) patients were not infected with HBV and HCV; (b) patients were diagnosed with HCC by pathology for the first time; (c) patients who had not taken antitumor therapies and anti-inflammatory medicines; (d) patients without a second malignancy in addition to HCC.
The clinical data collected included the following: gender, age, smoking, alcohol drinking history, body mass index (BMI), TNM stage, number of nodules, treatment methods, complete blood count [haemoglobin (HGB), lymphocyte, monocyte, neutrophil, platelets (PLT), red blood cell (RBC), and white blood cell (WBC) counts, neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), lymphocyte-to-monocyte ratio (LMR), prognostic nutritional index (PNI, PNI = serum ALB value (g/L) + 5 × total number of peripheral blood lymphocytes (× 109/L)], liver biochemical tests [total protein (TP), albumin (ALB), alkaline phosphatase (ALP), alanine aminotransferase (ALT), apolipoprotein B (APOB), apolipoprotein A (APOA), aspartate aminotransferase (AST), AST-to-ALT ratio (SLR), cholesterol (CHO), creatinine (CRE), C-reactive protein (CRP), cystatin C (CYSC), high-density lipoprotein (HDL), lactate dehydrogenase (LDH), and low-density lipoprotein (LDL)], coagulation function laboratory tests [activated partial thromboplastin time (APTT), fibrinogen (Fbg), prothrombin time (PT), and thrombin time (TT)], AFP, carbohydrate antigen 19-9 (CA19-9), and carcinoembryonic antigen (CEA). The AI was calculated by the following formula: (TC − HDL-C)/HDL-C [19].
Statistical analysis
The LASSO-Cox regression model (“glmnet” R package) was utilised to narrow down the candidate indexes and to develop the prognostic model. The prognostic model was calculated after centralisation and standardisation (applying the “scale” function in R) of the development cohort data. The prognostic model formula was as follows: \({\text{Risk score}} = \sum\nolimits_{i}^{{\text{n}}} {Xi \times Yi}\) (n: number of the inclusion index, X: coefficients, Y: survival-related index). The prognostic power of the prognostic risk score, TNM stage, and treatment was appraised by the concordance index (C-index), and the time-dependent receiver operating characteristic curve (TD-ROC). NV-HCC patients were divided into low-risk and high-risk groups based on the risk score’s optimal cut-off (“survminer” R package). The Kaplan–Meier method and log-rank test were used to compare the OS of two risk groups. A box plot based on the prognostic index signatures were generated to show the difference in each index between the high-risk group and the low-risk group. Sankey diagrams were generated to show the patients’ transfers among the prognostic risk score, TNM stage, treatment and survival status. A nomogram was generated with the “nomogram” function in the “nomogram” R package to predict the 1-year, 3-year, and 5-year survival rates of NV-HCC patients. The nomogram for the 1-year, 3-year, and 5-year survival rates were calibrated using calibration curves after comparing the actual survival rate with the predicted probability of survival. The differences of prognostic index signatures between the low-risk and high-risk groups were analysed by the Wilcoxon signed-rank test. All statistical analyses were performed with R software (v3.6.2) and SPSS 25.0 software. A P value less than 0.05 was considered statistically significant.
Results
Characteristics of the patients
A total of 7511 HCC samples at Sun Yat-sen University Cancer Center from January 2013 to December 2016 were initially screened, and 7250 patients with hepatitis virus infection were excluded. Overall, 261 patients were randomly divided into a development cohort (n = 183) and a validation cohort (n = 78). The clinicopathological variables of NV-HCC patients are described in Table 1. In the development cohort, there were 136 (74.32%) males and 47 (25.68%) females. The mean age of the patients was 61.55 years. In the validation cohort, 57 (73.08%) were males and 21 (26.92%) were females. The mean age of the patients was 62.71 years. The 1-, 3-, and 5-year OS rates for the development and validation cohorts were 68.85%, 49.73%, and 31.15% and 79.49%, 56.41%, and 41.03%, respectively.
Prognostic model construction and evaluation
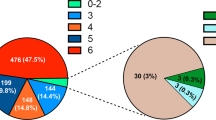
In the primary cohort, a 6-prognostic index (number of nodules, LMR, PNI, ALP, SLR and CRP) signature was constructed by performing LASSO-Cox regression analysis (Fig. 1A, B). The prognostic model was calculated as follows: Risk score = (0.4419 * number of nodules) + (− 0.0156 * LMR) + (− 0.005 * PNI) + (0.001 * ALP) + (0.1301 * SLR) + (0.0001 * CRP). The C-index was used to compare the predictive power of the prognostic model with that of TNM stage and treatment. In the development cohort, the prognostic model achieved a C-index of 0.759 (95% CI 0.723–0.797), which was higher than the C-index of TNM stage (0.708; 95% CI 0.663–0.753; P = 0.021) and treatment (0.630; 95% CI 0.582–0.677; P < 0.001). In the validation cohort, the C-index of the prognostic model, TNM stage, and treatment were 0.796 (95% CI 0.737–0.855), 0.721 (95% CI 0.647–0.795), and 0.700 (95% CI 0.630–0.770), respectively (Table 2). TD-ROC analysis was performed to evaluate the accuracy of the prognostic model, TNM stage, and treatment in the development cohort (Fig. 2A) and validation cohort (Fig. 2B). The area under the ROC curve (AUC) values of the prognostic model were higher than those of TNM stage and treatment for all cohorts (Fig. 2). For the 1-year OS, the AUCs of the prognostic model, TNM stage, and treatment were 0.849, 0.773, and 0.654, respectively (Fig. 2C). In addition, for the 3-year OS, and 5-year OS, the prognostic model also had higher AUC values than TNM stage and treatment (Fig. 2D, E).
Risk stratification of OS based on the prognostic model
Based on the optimal cut-off of the risk score, all patients were divided into a low-risk group (< 0.59) and a high-risk group (≥ 0.59). A notable difference in OS was detected between the low-risk and high-risk groups, and the high-risk group had shorter OS than the low-risk group in the development cohort (Fig. 3A) and validation cohort (Fig. 3B). Moreover, there was a significant difference between the high-risk and low-risk groups for stage I/II and stage III/IV in the development cohort (Fig. 3C, P < 0.001; Fig. 3D, P < 0.001) and in the validation cohort (Fig. 3E, P < 0.001; Fig. 3F, P = 0.004).
The differences between the high-risk and low-risk groups in the number of nodules, LMR, PNI, ALP, SLR and CRP were analysed using a boxplot (Fig. 4). The number of nodules and ALP, SLR and CRP levels in the high-risk group were significantly higher than those in the low-risk group in the development (P < 0.05; Fig. 4A, D–F) and validation cohorts (P < 0.05; Fig. 4G, J–L). In the development cohort, LMR and PNI levels in the low-risk group were significantly higher than those in the high-risk group (P < 0.05; Fig. 4B, C). However, there was no significant difference between the two groups regarding the LMR levels in the validation cohort (P = 0.092, Fig. 4H). In addition, Sankey diagrams showed that most of the low-risk group patients shifted to stage I/II, were treated with surgery, and had a higher level of survival status in the development (Fig. 5A) and validation cohorts (Fig. 5B).
The nomogram for the prediction of OS
Based on the prognostic risk score, TNM stage, and treatment, we created a prognostic nomogram for the prediction of OS in the two cohorts (Fig. 6A, B). In the development (Fig. 6C) and validation cohorts (Fig. 6D), calibration curves of 1-year, 3-year, and 5-year survival showed optimal consistency between the prediction established in the nomogram and actual observations. In the development cohort, the C-index of the prognostic model and nomogram were 0.76 and 0.78, respectively (P = 0.019) (Fig. 6E). Similarly, the nomogram model achieved a higher C-index (0.85) than the prognostic model (0.80) (P < 0.001) (Fig. 6F).
Discussion
HCC is a leading cause of cancer related death worldwide [20]. Most HCC patients have a poor prognosis, and the 5-year OS is only 12.1% [21]. HBV and HCV infection are major important risk factors for HCC. Recently, with lifestyle changes and efficient vaccination strategies, the number of HCC virus patients has decreased, and the number of NV-HCC patients is increasing [5]. In Taiwan, due to the universal newborn vaccination program, HCC incidence is significantly lower in younger persons who were vaccinated than in those who were not vaccinated at birth [22]. However, there are few studies predicting the occurrence of NV-HCC. TNM stage is commonly used to predict the prognosis for many cancers [23, 24]. However, studies reported that patients with the same TNM stage had different clinical outcomes [25]. This phenomenon indicates that the TNM stage utilized for guidance of the different treatments is insufficient. Therefore, we developed a prognostic model for NV-HCC. LASSO-Cox regression is a useful tool for feature selection and regularization to improve the accuracy of statistical models [26]. In this study, we constructed a prognostic model for NV-HCC to further guide clinical treatment by using LASSO-Cox regression analysis of the pathological results and clinical laboratory test results.
In this study, by using LASSO-Cox regression analysis, six predictive indicators (number of nodules, LMR, PNI, ALP, SLR and CRP) were selected for the prediction of NV-HCC prognosis. Then, we constructed a prognostic model based on the six factors for NV-HCC patients. The risk score was calculated as follows: Risk score = (0.4419 * number of nodules) + (− 0.0156 * LMR) + (− 0.005 * PNI) + (0.001 * ALP) + (0.1301 * SLR) + (0.0001 * CRP). Based on the risk score, the NV-HCC patients were divided into a low-risk group (risk score < 0.59) and a high-risk group (risk score ≥ 0.59). Kaplan–Meier curves revealed that the high-risk group of NV-HCC patients had a poor OS (P < 0.001). The prognostic score model achieved a higher AUC than the TNM stage and treatment for the 1-year OS, 3-year OS, and 5-year OS. Moreover, we constructed a nomogram that can help to predict OS in NV-HCC patients, which integrated the prognostic score, TNM stage and treatment. Notably, according to our study, the nomogram model was a more powerful predictive factor of OS for NV-HCC patients than the prognostic model, and the C-index of the nomogram model (0.78 and 0.85) was higher than the C-index of the prognostic risk score model (0.76 and 0.80) in the development cohort and in the validation cohort. Moreover, in the development cohort and validation cohort, the heatmaps and waterfall plots of the clinical features also indicated that patients who had shorter OS were mainly distributed in the high-risk group, TNM stage III or IV group, and treatment with chemotherapy group.
The prognosis of NV-HCC patients is closely related to the number of nodules in the liver. Mazzotta et al. reported that patients who had more than 5 HCC nodules during the waiting period had a high risk of post liver transplantation recurrence and death [27]. Markers of the inflammatory response, including LMR, SLR, lymphocytes, NLR, and CRP, play important roles in the progression of many cancers [28, 29]. Studies have revealed that LMR is associated with survival in patients with breast cancer, and a low LMR indicates poor prognosis in stage I–III breast cancer [30]. LMR markedly increased the level of tumour-infiltrating Th17 cells and promoted tumour growth in HCC [31]. Serum ALP, AST, ALT, and CRP are biomarkers of systemic inflammation and immune activation, and can be used to evaluate liver function [32]. The elevation of ALP has been demonstrated to predict poor prognosis in esophageal squamous cell carcinoma and pancreatic cancer [33, 34]. Moreover, ALP was incorporated into prognostic models for many cancers, including HCC and gastric cancer [35, 36]. Our previous study showed that the LSR is an independent prognostic factor for gastric cancer [37]. We also established a nomogram based on age, stage status, and SLR, which had a more accurate prognostic prediction for patients with gastric cancer [38]. CRP is an indicator of inflammatory response, which combined with increased cytokines, growth factors, activated stroma, and DNA damage, promotes tumour invasion, migration and metastasis [39]. Currently, a low PNI has been shown to be a significant predictor of poor postoperative outcomes and increased mortality in various malignancies, including colorectal cancer, breast cancer, and pancreatic cancer [40,41,42]. In this study, we used LASSO-Cox regression analysis to identify that the number of nodules, LMR, PNI, ALP, SLR and CRP levels can be used to predict the prognosis of NV-HCC.
There are some limitations in this study that should be noted. First, this model employed data from one medical centre. Multicentre data are needed to further verify the performance of the model. Second, this study has small sample size of NV-HCC patients in the development and validation cohorts. Therefore, a larger cohort is urgently needed to further verify the model of our study. In addition, this study only analysed the OS of NV-HCC patients, and it is uncertain whether DFS and progression-free survival (PFS) can be verified.
Conclusion
In summary, we established a prognostic model for NV-HCC based on 6 factors (number of nodules, LMR, PNI, ALP, SLR and CRP) via LASSO-Cox analysis, and found that it can be used to predict OS in NV-HCC patients. Moreover, a nomogram was constructed that integrated the prognostic model, TNM stage, and treatment. The prognostic model can provide a more precise estimation for patients with NV-HCC.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Amini M, Looha MA, Zarean E, Pourhoseingholi MA. Global pattern of trends in incidence, mortality, and mortality-to-incidence ratio rates related to liver cancer, 1990–2019: a longitudinal analysis based on the global burden of disease study. BMC Public Health. 2022;22(1):604.
Perisetti A, Goyal H, Yendala R, Thandassery RB, Giorgakis E. Non-cirrhotic hepatocellular carcinoma in chronic viral hepatitis: current insights and advancements. World J Gastroenterol. 2021;27(24):3466–82.
Bosch FX, Ribes J, Borras J. Epidemiology of primary liver cancer. Semin Liver Dis. 1999;19(3):271–85.
Wallace MC, Preen D, Jeffrey GP, Adams LA. The evolving epidemiology of hepatocellular carcinoma: a global perspective. Expert Rev Gastroenterol Hepatol. 2015;9(6):765–79.
Petrick JL, McGlynn KA. The changing epidemiology of primary liver cancer. Curr Epidemiol Rep. 2019;6(2):104–11.
Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, Huang GT, Iloeje UH, Group R-HS. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006;295(1):65–73.
Qu LS, Jin F, Huang XW, Shen XZ. High hepatitis B viral load predicts recurrence of small hepatocellular carcinoma after curative resection. J Gastrointest Surg. 2010;14(7):1111–20.
Sohn W, Paik YH, Kim JM, Kwon CH, Joh JW, Cho JY, Gwak GY, Choi MS, Lee JH, Koh KC, et al. HBV DNA and HBsAg levels as risk predictors of early and late recurrence after curative resection of HBV-related hepatocellular carcinoma. Ann Surg Oncol. 2014;21(7):2429–35.
Kadalayil L, Benini R, Pallan L, O’Beirne J, Marelli L, Yu D, Hackshaw A, Fox R, Johnson P, Burroughs AK, et al. A simple prognostic scoring system for patients receiving transarterial embolisation for hepatocellular cancer. Ann Oncol. 2013;24(10):2565–70.
Chon YE, Park H, Hyun HK, Ha Y, Kim MN, Kim BK, Lee JH, Kim SU, Kim DY, Ahn SH, et al. Development of a new nomogram including neutrophil-to-lymphocyte ratio to predict survival in patients with hepatocellular carcinoma undergoing transarterial chemoembolization. Cancers. 2019;11(4):509.
Goto T, Yoshida H, Tateishi R, Enooku K, Goto E, Sato T, Ohki T, Masuzaki R, Imamura J, Shiina S, et al. Influence of serum HBV DNA load on recurrence of hepatocellular carcinoma after treatment with percutaneous radiofrequency ablation. Hepatol Int. 2011;5(3):767–73.
Bruix J, Cheng AL, Meinhardt G, Nakajima K, De Sanctis Y, Llovet J. Prognostic factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: analysis of two phase III studies. J Hepatol. 2017;67(5):999–1008.
Harimoto N, Shirabe K, Nakagawara H, Toshima T, Yamashita Y, Ikegami T, Yoshizumi T, Soejima Y, Ikeda T, Maehara Y. Prognostic factors affecting survival at recurrence of hepatocellular carcinoma after living-donor liver transplantation: with special reference to neutrophil/lymphocyte ratio. Transplantation. 2013;96(11):1008–12.
Huang J, Liu FC, Li L, Zhou WP, Jiang BG, Pan ZY. Nomograms to predict the long-time prognosis in patients with alpha-fetoprotein negative hepatocellular carcinoma following radical resection. Cancer Med. 2020;9(8):2791–802.
Pinero F, Marciano S, Anders M, Orozco Ganem F, Zerega A, Cagliani J, Andriani O, de Santibanes E, Gil O, Podesta LG, et al. Identifying patients at higher risk of hepatocellular carcinoma recurrence after liver transplantation in a multicenter cohort study from Argentina. Eur J Gastroenterol Hepatol. 2016;28(4):421–7.
Witjes CD, IJzermans JN, van der Eijk AA, Hansen BE, Verhoef C, de Man RA. Quantitative HBV DNA and AST are strong predictors for survival after HCC detection in chronic HBV patients. Neth J Med. 2011;69(11):508–13.
Lai Q, Castro Santa E, Rico Juri JM, Pinheiro RS, Lerut J. Neutrophil and platelet-to-lymphocyte ratio as new predictors of dropout and recurrence after liver transplantation for hepatocellular cancer. Transplant Int. 2014;27(1):32–41.
Zhang M, Bi LF, Fang JH, Su XL, Da GL, Kuwamori T, Kagamimori S. Beneficial effects of taurine on serum lipids in overweight or obese non-diabetic subjects. Amino Acids. 2004;26(3):267–71.
Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16(10):589–604.
Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, Tateishi R, Han KH, Chawla YK, Shiina S, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hep Intl. 2017;11(4):317–70.
Chang MH, You SL, Chen CJ, Liu CJ, Lee CM, Lin SM, Chu HC, Wu TC, Yang SS, Kuo HS, et al. Decreased incidence of hepatocellular carcinoma in hepatitis B vaccinees: a 20-year follow-up study. J Natl Cancer Inst. 2009;101(19):1348–55.
Birim O, Kappetein AP, Waleboer M, Puvimanasinghe JP, Eijkemans MJ, Steyerberg EW, Versteegh MI, Bogers AJ. Long-term survival after non-small cell lung cancer surgery: development and validation of a prognostic model with a preoperative and postoperative mode. J Thorac Cardiovasc Surg. 2006;132(3):491–8.
Yau T, Tang VY, Yao TJ, Fan ST, Lo CM, Poon RT. Development of Hong Kong Liver Cancer staging system with treatment stratification for patients with hepatocellular carcinoma. Gastroenterology. 2014;146(7):1691.e1693-1700.
Liu MZ, Tang LL, Zong JF, Huang Y, Sun Y, Mao YP, Liu LZ, Lin AH, Ma J. Evaluation of sixth edition of AJCC staging system for nasopharyngeal carcinoma and proposed improvement. Int J Radiat Oncol Biol Phys. 2008;70(4):1115–23.
Tibshirani R. The lasso method for variable selection in the Cox model. Stat Med. 1997;16(4):385–95.
Mazzotta AD, Pascale A, Cano L, Rosmorduc O, Allard MA, Sa Cunha A, Adam R, Cherqui D, Vibert E, Golse N. Number of hepatocellular carcinoma nodules in patients listed for liver transplantation within alpha-fetoprotein score: a new prognostic risk factor. Transpl Int. 2021;34(5):954–63.
Singh J, Shukla D, Gupta S, Shrivastav BR, Tiwari PK. Clinical epidemiology of gallbladder cancer in North-Central India and association of immunological markers, NLR, MLR and PLR in the diagnostic/prognostic prediction of GBC. Cancer Treat Res Commun. 2021;28:100431.
Wang J, Li H, Xu R, Lu T, Zhao J, Zhang P, Qu L, Zhang S, Guo J, Zhang L. The MLR, NLR, PLR and D-dimer are associated with clinical outcome in lung cancer patients treated with surgery. BMC Pulm Med. 2022;22(1):104.
Zhang Z, Lin Q, Chen Y, Su C, Lin W, Wei D, Zhang L, Liu H. Prognostic evaluation of metastasis-related lymphocyte/monocyte ratio in stage—breast cancer receiving chemotherapy. Front Oncol. 2021;11:782383.
Kuang DM, Peng C, Zhao Q, Wu Y, Chen MS, Zheng L. Activated monocytes in peritumoral stroma of hepatocellular carcinoma promote expansion of memory T helper 17 cells. Hepatology. 2010;51(1):154–64.
Drotman RB, Lawhorn GT. Serum enzymes as indicators of chemically induced liver damage. Drug Chem Toxicol. 1978;1(2):163–71.
Wei XL, Zhang DS, He MM, Jin Y, Wang DS, Zhou YX, Bai L, Li ZZ, Luo HY, Wang FH, et al. The predictive value of alkaline phosphatase and lactate dehydrogenase for overall survival in patients with esophageal squamous cell carcinoma. Tumour Biol. 2016;37(2):1879–87.
Ji F, Fu SJ, Guo ZY, Pang H, Ju WQ, Wang DP, Hua YP, He XS. Prognostic value of combined preoperative lactate dehydrogenase and alkaline phosphatase levels in patients with resectable pancreatic ductal adenocarcinoma. Medicine. 2016;95(27):e4065.
Kim SY, Yoon MJ, Park YI, Kim MJ, Nam BH, Park SR. Nomograms predicting survival of patients with unresectable or metastatic gastric cancer who receive combination cytotoxic chemotherapy as first-line treatment. Gastric Cancer. 2018;21(3):453–63.
Xu XS, Wan Y, Song SD, Chen W, Miao RC, Zhou YY, Zhang LQ, Qu K, Liu SN, Zhang YL, et al. Model based on gamma-glutamyltransferase and alkaline phosphatase for hepatocellular carcinoma prognosis. World J Gastroenterol. 2014;20(31):10944–52.
Chen SL, Li JP, Li LF, Zeng T, He X. Elevated preoperative serum alanine aminotransferase/aspartate aminotransferase (ALT/AST) ratio is associated with better prognosis in patients undergoing curative treatment for gastric adenocarcinoma. Int J Mol Sci. 2016;17(6):911.
Li L, Zeng Q, Xue N, Wu M, Liang Y, Xu Q, Feng L, Xing S, Chen S. A nomogram based on aspartate aminotransferase/alanine aminotransferase (AST/ALT) ratio to predict prognosis after surgery in gastric cancer patients. Cancer Control. 2020;27(1):1073274820954458.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7.
Tokunaga R, Sakamoto Y, Nakagawa S, Miyamoto Y, Yoshida N, Oki E, Watanabe M, Baba H. Prognostic nutritional index predicts severe complications, recurrence, and poor prognosis in patients with colorectal cancer undergoing primary tumor resection. Dis Colon Rectum. 2015;58(11):1048–57.
Mohri T, Mohri Y, Shigemori T, Takeuchi K, Itoh Y, Kato T. Impact of prognostic nutritional index on long-term outcomes in patients with breast cancer. World J Surg Oncol. 2016;14(1):170.
Kanda M, Fujii T, Kodera Y, Nagai S, Takeda S, Nakao A. Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg. 2011;98(2):268–74.
Acknowledgements
None.
Funding
This work was funded by Guangdong Esophageal Cancer Institute Science and Technology Program (No. Q202001) and Nursery Fund of Henan Cancer Hospital.
Author information
Authors and Affiliations
Contributions
NX, SQD, and QXX designed this study. YJ, SLC, and YXW collected clinical data and wrote the manuscript. YYQ and LNJ performed data analysis. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Clinical Research Ethics Committee of Sun Yat-sen University Cancer Center.
Consent for publication
Not applicable.
Competing interests
The authors have declared no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, Y., Chen, S., Wu, Y. et al. Establishment and validation of a novel prognostic model for non-virus-related hepatocellular carcinoma. Cancer Cell Int 22, 300 (2022). https://doi.org/10.1186/s12935-022-02725-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-022-02725-5