Abstract
Background
The triglyceride-glucose (TyG) index is considered a dependable biomarker for gauging insulin resistance. The atherogenic index of plasma (AIP) represents a marker reflecting atherosclerosis. However, there is currently no study specifically exploring the associations of these two biomarkers with the severity of new-onset coronary artery disease (CAD) under different glucose metabolic states. Therefore, this study aims to evaluate the correlations of these two biomarkers with CAD severity in patients newly diagnosed with CAD under various glucose metabolism conditions.
Method
Totally 570 subjects first administered coronary angiography were enrolled, including 431 first diagnosed CAD patients and 139 non-CAD patients. CAD severity was gauged by the quantity of narrowed arteries (single-vessel and multi-vessel CAD). According to WHO diabetes guidelines, glucose metabolic states were divided into normal glucose regulation (NGR), pre-diabetes mellitus (Pre-DM), and diabetes mellitus (DM). The relationships of the TyG index and AIP with CAD severity were validated by logistic regression analysis, including adjustment for traditional cardiovascular risk elements and medical treatments. Their predictive efficacy for CAD was evaluated by receiver operating characteristic (ROC) curves.
Result
The TyG index and AIP were independently correlated with CAD in accordance with logistic regression analysis (both P < 0.05). Regardless of the glucose metabolic states, there was no statistical correlation between the TyG index and CAD severity. However, AIP in NGR patients was significantly related to CAD severity (P < 0.05). The areas under the curve of the TyG index and AIP for predicting CAD were 0.682 and 0.642 (both P < 0.001), respectively, and their optimal cut-off values were 3.210 (Youden index: 0.305) and 0.095 (Youden index:0.246), respectively.
Conclusion
The TyG index and AIP have significant associations with CAD. The TyG index had no association with CAD severity, regardless of glucose metabolic states. AIP exhibited a discernible link with CAD severity in NGR patients, but not in the pre-DM or DM populations. The TyG index and AIP have similar predictive values for new-onset CAD.
Similar content being viewed by others
Introduction
Coronary artery disease (CAD), a chronic cardiac disorder triggered by the narrowing of coronary arteries, represents the top global contributor to mortality [1]. Invasive coronary angiography (CAG), considered the ultimate tool for CAD diagnosis, effectively ascertains both the degree and number of coronary artery stenoses. According to the results of CAG, patients with ≥ 50% lumen constriction in a major coronary artery are diagnosed with CAD [2]. In addition, the quantity of stenotic vessels determines the severity of CAD. Compared with single-vessel CAD, multi-vessel CAD has a relatively lower reperfusion success rate and a higher risk of adverse prognosis in contrast with single-vessel CAD [3]. CAG is invasive and expensive, as well as having a potential risk of serious complications. Many patients refuse to receive CAG examinations during the early stages of CAD, missing timely medical evaluation and coronary revascularization treatment. Moreover, the CAD population has a high recurrence risk, especially those with Type 2 diabetes mellitus (T2DM) [4]. Therefore, timely identification and intervention in patients at high risk of CAD have an important clinical significance.
Insulin resistance (IR) is the major characteristic of T2DM and has been confirmed as a significant driver of CAD [5, 6]. Pathophysiological studies have shown that IR promotes an inflammatory state, vascular endothelial dysfunction, and dyslipidemia, which may be the main mechanisms of CAD progression [7]. The triglyceride-glucose (TyG) index, as a dependable and newfound biomarker for gauging IR, is closely related to the progression of various cardiovascular events [8]. A previous study observed the relation of the TyG index to CAD severity in the prediabetic population [2]. The TyG index is easily available and low-cost, and it is expected to provide valuable data for the clinical management of CAD.
The atherogenic index of plasma (AIP), denoting the logarithmic ratio of TG to high-density lipoprotein cholesterol (HDL-C) in molar concentration, is a parameter for evaluating plasma atherosclerosis and exhibits a profound connection to the atherosclerotic burden and cardiovascular occurrences [9,10,11]. AIP has been reported to be significantly associated with T2DM [12, 13]. A recent study demonstrated that AIP is positively correlated with the progression from prediabetes to diabetes and is negatively related to the recovery from prediabetes to normoglycemia [14]. The TyG index and AIP are both related to T2DM and cardiovascular events. However, there is currently no study specifically evaluating the role of the TyG index and AIP on new-onset CAD severity under different glucose metabolic states. Therefore, this study aims to validate the associations of the TyG index and AIP with new-onset CAD severity in different states of glucose metabolism.
Method
Ethical statements
This study was conducted at the Affiliated Qingyuan Hospital, Guangzhou Medical University (Qingyuan People’s Hospital). The study was implemented in accordance with the Declaration of Helsinki and was authorized by the Ethics Committee of the Affiliated Qingyuan Hospital, Guangzhou Medical University (Qingyuan People’s Hospital) (IRB-2023-003), which waived the requirement for informed consent due to its retrospective nature.
Study design
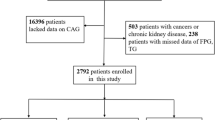
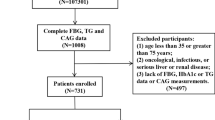
We scrutinized 1677 patients who underwent their first CAG and were admitted to Affiliated Qingyuan Hospital, Guangzhou Medical University (Qingyuan People’s Hospital) between September 1, 2019 and September 1, 2022. Exclusion conditions were: (1) age below 18 years or above 75 years; (2) previous CAG or coronary revascularization therapy; (3) malignancies, infectious diseases, severe hepatic or renal insufficiency, or impaired thyroid function; and (4) incomplete body mass index (BMI), FBG, or other measurements. Ultimately, 570 subjects were recruited, comprising 431 patients newly diagnosed with CAD and 139 patients without CAD (Fig. 1). In accordance with the established diagnostic criteria for CAD, 570 subjects were classified into the CAD (n = 431) and non-CAD (n = 139) groups. Furthermore, based on the severity of CAD, the CAD group was subdivided into the single-vessel (n = 144) and multi-vessel (n = 287) CAD groups.
Data source and collection
The data of the patients was collated from the autonomous digital medical record system, including key demographic features, clinical background, outcomes of blood analysis, and relevant medical imaging records. Demographic characteristics comprised age, gender, weight, height, blood pressure, and smoking and alcohol consumption habits. Clinical history encompassed hypertensive and diabetic medical histories as well as the states of medical treatments. Medical treatments embraced antihypertensive, antidiabetic, antilipidemic and antiplatelet drugs.
The blood specimens were acquired in the morning through the collection of fasting venous blood by skilled medical professionals. TG, total cholesterol (TC), HDL-C, low-density lipoprotein cholesterol (LDL-C), FPG, and glycosylated hemoglobin (HbA1c) were assessed on an automated hematology analyzer. Catheter-based invasive CAG was executed, utilizing percutaneous radial or femoral arteriography. The employed angiographic apparatus was furnished with ample versatility, enabling precise diagnoses of all manifestations of coronary arteries.
Definitions
CAD is characterized by a luminal constriction of ≥ 50% in one principal coronary artery [2]. The severity of CAD is contingent upon the quantity of narrowed coronary arteries. Narrowing of ≥ 50% in the left main artery is also considered multi-vessel CAD.
The AIP is derived from the formula: log10 (TG [mol/L]/HDL-C [mol/L]) [9]. The TyG index is calculated as ln (TG [mg/dL] × FPG [mg/dL]/2) [8].
According to the World Health Organization guidelines on diabetes [15], the diagnostic criteria for diabetes mellitus (DM) include FPG ≥ 7.0 mmol/L, 2-h plasma glucose level ≥ 11.1 mmol/L based on the oral glucose tolerance test, HbA1c ≥ 6.5%, or a history of T2DM. Normal glucose regulation (NGR) is defined as FPG < 6.1 mmol/L and 2-h plasma glucose level < 7.8 mmol/L. Pre-diabetes mellitus (Pre-DM) should be considered for individuals exhibiting elevated plasma glucose levels that do not meet the criteria for a T2DM diagnosis.
Statistical analysis
Continuous variates were shown as median and interquartile range (IQR), encompassing the 25th (Q25) and 75th (Q75) percentiles. Categorical variables were presented in the form of counts or percentages. In order to compare continuous variables among various groups, either a one-way analysis of variance or the Kruskal–Wallis test was deployed, while distinctions in categorical variables were compared across the groups using the chi-square test.
Logistic regression models, incorporating odds ratios (ORs) and corresponding 95% confidence intervals (CIs), were established to validate the correlations of the TyG index and AIP (independent variables) with CAD (dependent variable). Within the TyG index quartiles, three models were formulated to scrutinize the interaction of the TyG index with CAD: Model 1, an unadjusted state; Model 2, adjustment by incorporating age and sex as covariates; and Model 3, refinement by introducing the variables from Model 2, in conjunction with systolic blood pressure (SBP), BMI, smoking status, drinking status, HDL-C, LDL-C, hypertension, antihypertensive drugs, antidiabetic drugs, antilipidemic drugs and antiplatelet drugs. Similarly, based on the AIP quartiles, three distinct models were constructed to explore the relationship between AIP and CAD, considering significant covariates: Model 1, an unaltered state; Model 2, inclusion of age and sex; Model 3, further enhancement by the inclusion of variables from Model 2, along with SBP, BMI, smoking status, drinking status, LDL-C, HbA1c, DM, hypertension, antihypertensive drugs, antidiabetic drugs, antilipidemic drugs and antiplatelet drugs.
Additionally, to scrutinize the links between the TyG index or AIP (independent variables) and the severity of newly diagnosed CAD, logistic regression analysis was employed again.
Moreover, the predictive efficacy of these two indexes for CAD entailed the calculation of the area under the curve (AUC) through the receiver operating characteristic (ROC) curve and the computation of the corresponding 95% confidence interval (CI). The best cut-off values refer to the TyG index and AIP corresponding to the maximum Youden index, and the Youden index is equal to the sum of sensitivity and specificity minus 1 [16, 17]. SPSS 26.0 (IBM, USA) and GraphPad Prism 8.0 (GraphPad Software, USA; www.graphpad.com) were utilized for statistical analysis. The threshold of statistical significance was established at P < 0.05.
Results
Clinicodemographic features of the non-CAD and CAD groups
Clinicodemographic feature analysis involved 570 subjects, with 431 patients newly diagnosed with CAD and 139 individuals without CAD (Table 1). The Mean patient age was 51 years (IQR, 43–54). There were 484 men (84.9%). Within these three groups, statistically significant differences were observed in age, sex, smoking, TC, TG, HDL-C, LDL-C, HbA1c, TyG index, AIP, and glucose metabolism (P < 0.05).
Associations of the TyG index and AIP with CAD
The TyG index was distributed across four groups based on quartiles: I (0 ≤ TyG < 2.86), II (2.86 ≤ TyG < 3.29), III (3.29 ≤ TyG < 3.76), and IV (3.76 ≤ TyG ≤ 7.08). Logistic regression models unveiled a prominent linkage of the TyG index with CAD, after adjusting for traditional cardiovascular risk elements and medical treatments (P < 0.001, Table 2). With the TyG index as a continuous variate, a notable connection with CAD was demonstrated (OR = 2.317, 95%CI 1.499–3.582; P < 0.001). In addition, with the TyG index as a categorical variate, CAD risk levels were 5.196 (95%CI 2.386–11.312, P < 0.001) fold higher in patients categorized as IV cases versus category I cases after adjustment for confounders.
Likewise, AIP was stratified into four tiers based on quartiles: I (0 ≤ AIP ≤ 0.04), II (0.05 ≤ AIP ≤ 0.24), III (0.25 ≤ AIP ≤ 0.46), and IV (0.47 ≤ AIP ≤ 2.14). As shown in Table 3, the results demonstrated a notable correlation between AIP and CAD after multivariate adjustment (P < 0.05). With AIP as a continuous variable, a significant correlation with CAD was firmly established (OR = 3.897, 95%CI 1.489–10.198, P < 0.05). With AIP as a categorical variate, CAD risk was 2.425-fold higher in cases categorized as IV compared with category I cases (95%CI 1.201–4.898, P < 0.05).
Associations of the TyG index and AIP with CAD severity
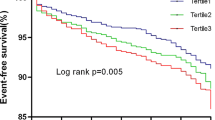
Logistic regression models revealed that the TyG index displayed no statistical significance with CAD severity (P > 0.05, Table 4). Notably, the results demonstrated a significant link between AIP and CAD severity (P < 0.05, Table 5).
Associations of the TyG index and AIP with CAD severity in different glucose metabolic states
As shown in Table 6, the TyG index exhibited no statistical significance with CAD severity irrespective of the glucose metabolism states (P > 0.05). However, AIP in NGR patients exhibited a discernible link with CAD severity (P < 0.05, Table 7).
Predictive values of the TyG index and AIP in CAD
The ROC curve analysis of the TyG index and AIP for CAD prediction is shown in Fig. 2. The AUCs of the TyG index and AIP for predicting CAD were 0.682 and 0.642 (both P < 0.001), respectively, and their optimal cut-off values were 3.210 (Youden index: 0.305) and 0.095 (Youden index: 0.246), respectively.
Discussion
The present study first assessed the associations of the TyG index and AIP with new-onset CAD severity in different states of glucose metabolism. The principal findings were: (1) The TyG index was not associated with the severity of new-onset CAD, regardless of glucose metabolic states; (2) AIP had a notable correlation with multi-vessel CAD in the NGR population; and (3) The TyG index and AIP were promising biomarkers for predicting CAD newly diagnosed, displaying similar predictive performance.
IR is a major feature of T2DM and an important risk factor for cardiovascular disease (CVD) [5, 6]. IR is susceptible to inflammation, oxidative stress, vascular endothelial dysfunction, and multiple metabolic disorders, which may be the primary mechanisms for CVD occurrence and progression [7]. IR not only promotes the occurrence of CVD in the general population and T2DM patients but also can predict the outcomes of CVD [18, 19]. In addition, IR may increase the risk of frailty, muscle loss, and cognitive impairment [20, 21].
Accurate identification of IR is expected to establish more effective cardiovascular risk stratification to improve cardiovascular primary and secondary prevention. The Hyperinsulinemic euglycemic clamp test is considered the ultimate tool for IR, but its high cost, complexity, laboriousness, and time consumption limit its application in clinical practice [22]. Homeostasis model assessment for IR (HOMA-IR) is a means for evaluating IR [21], but has limited value for subjects receiving insulin treatment or patients with severely impaired beta-cell function [23]. To address this limitation, the TyG index has been developed, which is superior to HOMA-IR in evaluating IR [24, 25]. Mounting evidence reveals that TyG-based indexes are associated with diseases related to chronic inflammation or metabolic disorders, including arterial stiffness [26], albuminuria [27], nonalcoholic fatty liver disease [28, 29], hearing impairment [30], and testosterone deficiency [31]. A recent finding reported that the TyG index had a linkage to CVD in patients with ischemic heart failure after percutaneous coronary intervention [32]. The TyG index was confirmed to be independently related to MACE in individuals with T2DM and acute coronary syndrome [18]. Moreover, a study revealed a correlation between the TyG index and the risk of prehypertension or hypertension in the Japanese population with NGR [33]. Therefore, the TyG index exhibited a substantial link with CVD risk [6, 19, 34, 35]. The adverse association was mainly mediated by the increased prevalence of T2DM, dyslipidemia and hypertension [19].
The relationship between the TyG index and CAD severity in various states of glucose metabolism has been controversial. A retrospective multi-center study encompassing 731 CAD patients reported that the TyG index exhibited an association with multi-vessel CAD in the T2DM population but not in the pre-DM or NGR groups [36]. On the contrary, another retrospective study involving 2792 CAD patients showed that the TyG index had a correlation with multi-vessel CAD in prediabetic patients, while displaying no such association in T2DM or NGR population [2]. The selection of enrolled patients may contribute to these conflicting results. In these studies, the potential effects of long-term use of secondary prevention drugs for CAD, antidiabetic drugs, and the development of healthier lifestyle habits could not be excluded. Therefore, we selected new-onset CAD patients as our study object to avoid the prevalence-incidence bias as far as possible. Consistent with the previous study [37], the present study confirmed the TyG index was a risk factor for new-onset CAD. In addition, our study demonstrated that the TyG index was not correlated with new-onset CAD severity, regardless of glucose metabolic states.
Dyslipidemia is a traditional cardiovascular risk factor as well as a key driver for the occurrence and progression of coronary atherosclerosis [38]. Considering the complex interaction of lipoprotein metabolism, compared with a single blood lipid, AIP based on the combination of TG and HDL-C is considered to be a useful marker to reflect atherosclerosis [39]. AIP has been found to exhibit a correlation with CVD risk [40]. In addition, AIP has been found to be correlated with CAD severity based on the Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score assessment [41]. Notably, the SYNTAX score cannot directly reflect the number of coronary lesions [41]. AIP has been reported to be significantly associated with T2DM [12, 13]. However, the relationship between AIP and the severity of new-onset CAD in different glucose metabolic states has not been clarified. Consistent with previous findings [42], our study confirmed that AIP was a risk element for CAD. Furthermore, our study first found that AIP in NGR patients had a notable connection with new-onset CAD severity, but there was no such correlation in pre-DM and T2DM populations. This finding suggests that IR may interfere with the relationship between AIP and CAD severity. However, more studies are needed to validate our results and explore the mechanisms in the future.
A recent finding demonstrated that the TyG index and AIP could predict subclinical CAD [43]. However, there is currently no study specifically comparing the predictive values of these two indices for newly diagnosed CAD. Our study first found that these two indexes had similar predictive performance for CAD. The TyG index and AIP are expected to serve as simple and applicable biomarkers to recognize individuals at high risk of CAD early, achieving more targeted treatment or prevention.
Strengths and limitations
The strength of this study is that it is the first study to specifically evaluate the effects of AIP and the TyG index on new-onset CAD severity under different glucose metabolic statuses. All CAD patients were those who underwent first-time CAG and were newly diagnosed with CAD, which was beneficial to avoid potential impacts of long-term use of secondary prevention drugs for CAD and healthier lifestyle habits and to avoid the prevalence-incidence bias.
There are also some limitations to this study. Firstly, the TyG index and AIP were determined based on baseline data, which could not evaluate their longitudinal associations with CVD risk over time. Having dynamic data may add value to the risk stratification of CAD. Secondly, the relatively small size of the patient cohort might reduce the statistical robustness of the findings. Thirdly, the potential impact of the long-term use of antihypertensive, antidiabetic, and antilipidemic drugs on the measurement of blood lipids and glucose levels as well as CAD occurrence cannot be excluded. Fourthly, there is a lack of data on dietary habits, as diet may be an important confounding factor. Fifthly, as a retrospective observational study, the present study was unable to establish causality and could not completely exclude residual confounding effects, such as activity habits, although many confounding factors were adjusted. Sixthly, this single-center study involving the Chinese population might lead to admission rate bias, and the findings might not apply to broader populations. Further prospective, large-scale, multi-center randomized controlled trials may make our conclusions more reliable. Future studies should consider these factors to further improve the accuracy and validity of the results.
Conclusion
The TyG index and AIP were closely related to newly diagnosed CAD as well as having similar predictive values for CAD. These two indices could be widely used in clinical practice to identify high-risk CAD populations early. The TyG index had no association with new-onset CAD severity, regardless of glucose metabolic states. AIP exhibited an independent link with the severity of new-onset CAD in NGR patients, but not in the pre-DM or T2DM populations. Monitoring AIP is expected to discover NGR individuals at high risk of severe and complex CAD early, providing novel prevention strategy for the clinical management.
Availability of data and materials
Due to privacy and ethical limitations, the data generated and analyzed in the current study are not publicly available but can be obtained from corresponding authors upon reasonable request.
Abbreviations
- TyG:
-
Triglyceride-glucose
- AIP:
-
Atherogenic index of plasma
- CAD:
-
Coronary artery disease
- NGR:
-
Normal glucose regulation
- Pre-DM:
-
Prediabetes mellitus
- DM:
-
Diabetes mellitus
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- CAG:
-
Coronary angiography
- T2DM:
-
Type 2 diabetes mellitus
- IR:
-
Insulin resistance
- FPG:
-
Fasting plasma glucose
- TG:
-
Triglyceride
- HDL-C:
-
High-density lipoprotein cholesterol
- BMI:
-
Body mass index
- TC:
-
Total cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- HbA1c:
-
Glycosylated hemoglobin
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- SBP:
-
Systolic blood pressure
- CVD:
-
Cardiovascular disease
- HOMA-IR:
-
Homeostasis model assessment for IR
- SYNTAX:
-
Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery
References
Bergmark BA, Mathenge N, Merlini PA, Lawrence-Wright MB, Giugliano RP. Acute coronary syndromes. Lancet. 2022;399(10332):1347–58.
Wang X, Xu W, Song Q, Zhao Z, Meng X, Xia C, Xie Y, Yang C, Jin P, Wang F. Association between the triglyceride-glucose index and severity of coronary artery disease. Cardiovasc Diabetol. 2022;21(1):168.
Sorajja P, Gersh BJ, Cox DA, McLaughlin MG, Zimetbaum P, Costantini C, Stuckey T, Tcheng JE, Mehran R, Lansky AJ, et al. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J. 2007;28(14):1709–16.
Zhang Y, Ding X, Hua B, Liu Q, Gao H, Chen H, Zhao XQ, Li W, Li H. Predictive effect of triglyceride-glucose index on clinical events in patients with type 2 diabetes mellitus and acute myocardial infarction: results from an observational cohort study in China. Cardiovasc Diabetol. 2021;20(1):43.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuniga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122.
Tao LC, Xu JN, Wang TT, Hua F, Li JJ. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol. 2022;21(1):68.
Li M, Chi X, Wang Y, Setrerrahmane S, Xie W, Xu H. Trends in insulin resistance: insights into mechanisms and therapeutic strategy. Signal Transduct Target Ther. 2022;7(1):216.
Khalaji A, Behnoush AH, Khanmohammadi S, Ghanbari Mardasi K, Sharifkashani S, Sahebkar A, Vinciguerra C, Cannavo A. Triglyceride-glucose index and heart failure: a systematic review and meta-analysis. Cardiovasc Diabetol. 2023;22(1):244.
Zheng X, Zhang X, Han Y, Hu H, Cao C. Nonlinear relationship between atherogenic index of plasma and the risk of prediabetes: a retrospective study based on Chinese adults. Cardiovasc Diabetol. 2023;22(1):205.
Won KB, Heo R, Park HB, Lee BK, Lin FY, Hadamitzky M, Kim YJ, Sung JM, Conte E, Andreini D, et al. Atherogenic index of plasma and the risk of rapid progression of coronary atherosclerosis beyond traditional risk factors. Atherosclerosis. 2021;324:46–51.
Dobiasova M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER(HDL)). Clin Biochem. 2001;34(7):583–8.
Yin B, Wu Z, Xia Y, Xiao S, Chen L, Li Y. Non-linear association of atherogenic index of plasma with insulin resistance and type 2 diabetes: a cross-sectional study. Cardiovasc Diabetol. 2023;22(1):157.
Qin Z, Zhou K, Li Y, Cheng W, Wang Z, Wang J, Gao F, Yang L, Xu Y, Wu Y, et al. The atherogenic index of plasma plays an important role in predicting the prognosis of type 2 diabetic subjects undergoing percutaneous coronary intervention: results from an observational cohort study in China. Cardiovasc Diabetol. 2020;19(1):23.
Yang H, Kuang M, Yang R, Xie G, Sheng G, Zou Y. Evaluation of the role of atherogenic index of plasma in the reversion from Prediabetes to normoglycemia or progression to Diabetes: a multi-center retrospective cohort study. Cardiovasc Diabetol. 2024;23(1):17.
Task Force on diabetes p-d, cardiovascular diseases of the European Society of C, European Association for the Study of D, Ryden L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, Deaton C, et al. ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD-summary. Diab Vasc Dis Res. 2014;11(3):133–73.
Hosseini Mojahed F, Aalami AH, Pouresmaeil V, Amirabadi A, Qasemi Rad M, Sahebkar A. Clinical evaluation of the diagnostic role of microRNA-155 in breast cancer. Int J Genomics. 2020;2020:9514831.
Santulli G, Pascale V, Finelli R, Visco V, Giannotti R, Massari A, Morisco C, Ciccarelli M, Illario M, Iaccarino G, et al. We are what we eat: impact of food from short supply chain on metabolic syndrome. J Clin Med. 2019;8(12):2061.
Wang L, Cong HL, Zhang JX, Hu YC, Wei A, Zhang YY, Yang H, Ren LB, Qi W, Li WY, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc Diabetol. 2020;19(1):1–11.
Che B, Zhong C, Zhang R, Pu L, Zhao T, Zhang Y, Han L. Triglyceride-glucose index and triglyceride to high-density lipoprotein cholesterol ratio as potential cardiovascular disease risk factors: an analysis of UK biobank data. Cardiovasc Diabetol. 2023;22(1):34.
Perez-Tasigchana RF, Leon-Munoz LM, Lopez-Garcia E, Gutierrez-Fisac JL, Laclaustra M, Rodriguez-Artalejo F, Guallar-Castillon P. Metabolic syndrome and insulin resistance are associated with frailty in older adults: a prospective cohort study. Age Ageing. 2017;46(5):807–12.
Mone P, De Gennaro S, Moriello D, Frullone S, D’Amelio R, Ferrante MNV, Marro A, Santulli G. Insulin resistance drives cognitive impairment in hypertensive pre-diabetic frail elders: the CENTENNIAL study. Eur J Prev Cardiol. 2023;30(12):1283–8.
Guerrero-Romero F, Simental-Mendia LE, Gonzalez-Ortiz M, Martinez-Abundis E, Ramos-Zavala MG, Hernandez-Gonzalez SO, Jacques-Camarena O, Rodriguez-Moran M. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95(7):3347–51.
Minh HV, Tien HA, Sinh CT, Thang DC, Chen CH, Tay JC, Siddique S, Wang TD, Sogunuru GP, Chia YC, et al. Assessment of preferred methods to measure insulin resistance in Asian patients with hypertension. J Clin Hypertens (Greenwich). 2021;23(3):529–37.
Simental-Mendia LE, Rodriguez-Moran M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6(4):299–304.
Lee SH, Kwon HS, Park YM, Ha HS, Jeong SH, Yang HK, Lee JH, Yim HW, Kang MI, Lee WC, et al. Predicting the development of diabetes using the product of triglycerides and glucose: the Chungju Metabolic Disease Cohort (CMC) study. PLoS ONE. 2014;9(2): e90430.
Du MF, Zhang X, Hu GL, Mu JJ, Chu C, Liao YY, Chen C, Wang D, Ma Q, Yan Y, et al. Associations of lipid accumulation product, visceral adiposity index, and triglyceride-glucose index with subclinical organ damage in healthy Chinese adults. Front Endocrinol (Lausanne). 2023;14:1164592.
Wang Z, Qian H, Zhong S, Gu T, Xu M, Yang Q. The relationship between triglyceride-glucose index and albuminuria in United States adults. Front Endocrinol (Lausanne). 2023;14:1215055.
He X, Huang X, Qian Y, Sun T. A non-linear relationship between triglyceride glucose waist circumference and nonalcoholic fatty liver disease in a Japanese population: a secondary analysis. Front Endocrinol (Lausanne). 2023;14:1188214.
Wang Y, Wang J, Liu L, Yang P, Deng S, Liu X, Zhao L, Wang C, Li Y. Baseline level and change trajectory of the triglyceride-glucose index in relation to the development of NAFLD: a large population-based cohort study. Front Endocrinol (Lausanne). 2023;14:1137098.
Liu L, Qin M, Ji J, Wang W. Correlation between hearing impairment and the Triglyceride Glucose Index: based on a national cross-sectional study. Front Endocrinol (Lausanne). 2023;14:1216718.
Wu S, Wu Y, Fang L, Zhao J, Cai Y, Xia W. A negative association between triglyceride glucose-body mass index and testosterone in adult males: a cross-sectional study. Front Endocrinol (Lausanne). 2023;14:1187212.
Sun T, Huang X, Zhang B, Ma M, Chen Z, Zhao Z, Zhou Y. Prognostic significance of the triglyceride-glucose index for patients with ischemic heart failure after percutaneous coronary intervention. Front Endocrinol (Lausanne). 2023;14:1100399.
Xu J, Xu W, Chen G, Hu Q, Jiang J. Association of TyG index with prehypertension or hypertension: a retrospective study in Japanese normoglycemia subjects. Front Endocrinol (Lausanne). 2023;14:1288693.
Haring B, Schumacher H, Mancia G, Teo KK, Lonn EM, Mahfoud F, Schmieder R, Mann JFE, Sliwa K, Yusuf S, et al. Triglyceride-Glucose Index, LDL and cardiovascular outcomes in chronic stable cardiovascular disease: results from the ONTARGET and TRANSCEND trials. Eur J Prev Cardiol. 2023. https://doi.org/10.1093/eurjpc/zwad340.
Alizargar J, Bai CH, Hsieh NC, Wu SFV. Use of the triglyceride-glucose index (TyG) in cardiovascular disease patients. Cardiovasc Diabetol. 2020;19(1):1–3.
Su J, Li Z, Huang M, Wang Y, Yang T, Ma M, Ni T, Pan G, Lai Z, Li C, et al. Triglyceride glucose index for the detection of the severity of coronary artery disease in different glucose metabolic states in patients with coronary heart disease: a RCSCD-TCM study in China. Cardiovasc Diabetol. 2022;21(1):96.
Li J, Dong Z, Wu H, Liu Y, Chen Y, Li S, Zhang Y, Qi X, Wei L. The triglyceride-glucose index is associated with atherosclerosis in patients with symptomatic coronary artery disease, regardless of diabetes mellitus and hyperlipidaemia. Cardiovasc Diabetol. 2023;22(1):224.
Wilson PWF, Polonsky TS, Miedema MD, Khera A, Kosinski AS, Kuvin JT. Systematic review for the 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):3210–27.
Quispe R, Manalac RJ, Faridi KF, Blaha MJ, Toth PP, Kulkarni KR, Nasir K, Virani SS, Banach M, Blumenthal RS, et al. Relationship of the triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio to the remainder of the lipid profile: the Very Large Database of Lipids-4 (VLDL-4) study. Atherosclerosis. 2015;242(1):243–50.
Kim SH, Cho YK, Kim YJ, Jung CH, Lee WJ, Park JY, Huh JH, Kang JG, Lee SJ, Ihm SH. Association of the atherogenic index of plasma with cardiovascular risk beyond the traditional risk factors: a nationwide population-based cohort study. Cardiovasc Diabetol. 2022;21(1):81.
Li Y, Feng Y, Li S, Ma Y, Lin J, Wan J, Zhao M. The atherogenic index of plasma (AIP) is a predictor for the severity of coronary artery disease. Front Cardiovasc Med. 2023;10:1140215.
Kurklu HA, Tan TS, Ozyuncu N, Baskovski E, Ozdol C. Atherogenic index of plasma predicts obstructive coronary artery disease in patients with stable angina pectoris. Diagnostics (Basel). 2023;13(20):3249.
Si Y, Fan W, Han C, Liu J, Sun L. Atherogenic index of plasma, triglyceride-glucose index and monocyte-to-lymphocyte ratio for predicting subclinical coronary artery disease. Am J Med Sci. 2021;362(3):285–90.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
GZ, JL and XW designed the study. XW wrote the manuscript. GZ and JL reviewed and revised the manuscript. WQ analyzed the data. HY and YC revised the important content. XW and WQ collected and checked the data.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Affiliated Qingyuan Hospital, Guangzhou Medical University (Qingyuan People’s Hospital).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, X., Qiu, W., Yang, H. et al. Associations of the triglyceride-glucose index and atherogenic index of plasma with the severity of new-onset coronary artery disease in different glucose metabolic states. Cardiovasc Diabetol 23, 76 (2024). https://doi.org/10.1186/s12933-024-02163-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02163-9