Abstract
Background
Prediabetes has recently been associated with subclinical atheromatous disease in the middle-aged population. Our aim was to characterize atheromatous plaque burden by the number of affected territories and the total plaque area in the prediabetes stage.
Methods
Atheromatous plaque burden (quantity of plaques and total plaque area) was assessed in 12 territories from the carotid and femoral regions using ultrasonography in 6688 non-diabetic middle-aged subjects without cardiovascular disease. Prediabetes was defined by glycosylated hemoglobin (HbA1c) between 5.7 and 6.4% according to the American Diabetes Association guidelines.
Results
Prediabetes was diagnosed in 33.9% (n = 2269) of the ILERVAS participants. Subjects with prediabetes presented a higher prevalence of subclinical atheromatous disease than participants with HbA1c < 5.7% (70.4 vs. 67.5%, p = 0.017). In the population with prediabetes this was observed at the level of the carotid territory (p < 0.001), but not in the femoral arteries. Participants in the prediabetes stage also presented a significantly higher number of affected territories (2 [1;3] vs. 1 [0;3], p = 0.002), with a positive correlation between HbA1c levels and the number of affected territories (r = 0.068, p < 0.001). However, atheromatosis was only significantly (p = 0.016) magnified by prediabetes in those subjects with 3 or more cardiovascular risk factors. The multivariable logistic regression model showed that the well-established cardiovascular risk factors together with HbA1c were independently associated with the presence of atheromatous disease in participants with prediabetes. When males and females were analyzed separately, we found that only men with prediabetes presented both carotid and femoral atherosclerosis, as well as an increase of total plaque area in comparison with non-prediabetic subjects.
Conclusions
The prediabetes stage is accompanied by an increased subclinical atheromatous disease only in the presence of other cardiovascular risk factors. Prediabetes modulates the atherogenic effect of cardiovascular risk factors in terms of distribution and total plaque area in a sex-dependent manner.
Trial registration NCT03228459 (clinicaltrials.gov)
Similar content being viewed by others
Background
The International Diabetes Federation has estimated that in 2017 there were 451 million individuals with diabetes plus 374 million people with impaired glucose tolerance worldwide, with a total expenditure of USD 850 billion [1]. Cardiovascular (CV) disease is the main comorbidity of diabetes and is estimated to affect 32.2% of all subjects and is responsible for 27% of the total cost of treating diabetes [2, 3]. At diagnosis, many patients with type 2 diabetes have one or more additional classical risk factors for macrovascular disease and many have evidence of overt atherosclerosis [4]. In addition, all phases in the pathophysiology of plaque formation are enhanced in type 2 diabetes, contributing to an accelerated process [5]. However, symptoms are not always present, and the term “unrecognized diabetic cardiac impairment” has been proposed for individuals that develop CV disease without the classic angina-related or heart failure symptoms [6]. Finally, compared with subjects without diabetes, atheromatous disease in diabetes has special characteristics, such as its being more extensive, and affecting multiple and more peripheral blood vessels, that makes it more serious and aggressive [7].
The problem increases when we consider that many of the atherogenic risk factors are already present in the prediabetic stage, years before the diagnosis of type 2 diabetes [8]. The milieu that favors CV disease in the prediabetes stage is more than hyperglycemia in the nondiabetic range and the effect of insulin resistance in the vessel walls. It includes a cluster of different metabolic changes that favors the development of atheromatous disease, such as low-grade chronic inflammation, endothelial vasodilator and fibrinolytic dysfunction, and an atherogenic lipoprotein profile [9, 10]. In this way, prospective cohort studies have shown how prediabetes [defined as impaired fasting glucose, impaired glucose tolerance or raised glycated hemoglobin (HbA1c)] is associated with an increased risk of composite CV disease, coronary heart disease and stroke compared with normoglycemia [11]. Similarly, during an 8-years period and compared to individual with persistent normoglycemia, those who shifted from normoglycemia to impaired fasting glucose had a significant increased risk of all-cause mortality [12]. Remarkably, the health risk increases in subjects with values as low as 5.6 mmol/L for fasting glucose concentration or 39 mmol/mol for HbA1c. On this basis, it is of clinical relevance to evaluate the characteristics of subclinical atheromatous disease in the prediabetes stage [11].
To shed light on this issue, we performed a cross-sectional study in order to characterize atheromatous plaque burden by the number of affected territories and the total plaque area in the prediabetes stage.
Methods
Study population, metabolic status and the selection of patients
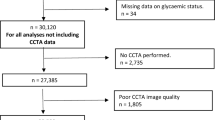
A total of 6809 subjects were enrolled between January 2015 and December 2017 from 30 primary health care centers in Lleida, Spain. The ILERVAS project is an ongoing clinical trial dealing with subclinical atheromatous disease (ClinicalTrials.gov Identifier: NCT03228459) [13]. The inclusion criteria were as follows: age 45–70 years, no history of cardiovascular disease, and at least one cardiovascular risk factor (dyslipidemia, blood hypertension, obesity, smoking habit or a first degree relative with premature (< 55 years old in men, < 65 in women) cardiovascular disease (myocardial infarction, stroke and peripheral arterial disease). The exclusion criteria were any type of diabetes, chronic kidney disease, active neoplasia, a life expectancy of less than 18 months and pregnancy.
According to the current American Diabetes Association guidelines, prediabetes was defined as an HbA1c between 39 and 47 mmol/mol (5.7 to 6.4%) and normal glucose metabolism as an HbA1c < 39 mmol/mol (< 5.7%) [14]. The HbA1c test was performed in capillary blood using a point-of-care device [Cobas B 101®, Roche Diagnostics S.L., Sant Cugat del Vallès, Spain], based on a latex agglutination inhibition immunoassay procedure that meets the generally accepted performance criteria for HbA1c [15]. A total of 121 participants with previously undiagnosed type 2 diabetes [(HbA1c ≥ 48.0 mmol/mol (≥ 6.5%)] were excluded from the investigation that was finally performed in 6688 subjects.
Clinical data regarding the cardiovascular risk factors were obtained from an electronic database (Information System for the Development of Research in Primary Care, SIDIAP) that comprises anonymized and longitudinal information from the Catalan Health Institute. The prevalence of dyslipidemia was obtained from patients who during the study period had a diagnostic code for disorders of lipoprotein metabolism according to of the International Classification of Diseases codes. The incidence of blood hypertension was obtained from subjects who had an identification code for hypertensive diseases. Obesity was defined by a body mass index (BMI) ≥ 30 kg/m2.
The prescribed antihypertensive, lipid-lowering and antithrombotic treatments were extracted from prescription- and pharmacy-invoicing databases provided by the Catalan Health Service, which are incorporated yearly into the SIDIAP database. Antihypertensive medication agents included ACE inhibitors, diuretics, ARA II, beta-blockers, calcium antagonists and other antihypertensives. Lipid-lowering drugs included statins, fibrates, ezetimibe and omega-3 fatty acids. Antithrombotic treatment consisted of the use of anticoagulant or antiplatelet agents.
Evaluation of clinical variables
Height and body weight were measured without shoes and in light clothing, and the body mass index (BMI) was obtained. A non-stretchable tape with a precision of 0.1 cm was used to assess waist circumference. According to a specified protocol, total cholesterol (mg/dl) levels were assessed in all participants from a non-fasting dried capillary blood test (fingertip puncture) using the REFLOTRON® Plus system (Roche Diagnostics, GmbH, Germany) [13]. Quantification of the entire lipid profile (HDL cholesterol, LDL cholesterol and triglycerides) was evaluated only in subjects in which total cholesterol was ≥ 200 mg/dL after fasting for 6 h or where total cholesterol ≥ 250 mg/dL regardless of fasting hours.
Blood pressure was measured in triplicate, after 5 min’ rest using an automated device [Omron M6 Comfort HEM-7221-E (Omron Healthcare, Kyoto, Japan)] at 2-min intervals, and the mean of the last 2 was calculated. The smoking habit (non-smoker, current or former smoker) was also documented. Smokers who stopped smoking ≥ 1 year prior to recruitment were considered former smokers.
Assessment of atheromatous plaque burden by ultrasound study
Bilateral carotid (common, bifurcation, internal and external arteries) and femoral (common and superficial arteries) areas were explored. The pictures were obtained by qualified sonographers using an ultrasonic Doppler Ultrasound Vivid-I (General Electric Healthcare, Waukesha, WI, USA) equipped with probe broadband linear 12L-RS that works at frequencies between 5 and 13 MHz. Standardized and validated scanning and reading protocols were used to decrease inter-operator variability and type 2 errors [16]. To measure intra and inter rater absolute agreement, Fleiss’ kappa for plaque presence and intraclass correlation coefficient for plaque area were obtained (Additional file 1: Table S1). The readers were unaware of the patients’ clinical histories.
Subclinical atheromatosis was defined as the presence of any plaque in the twelve assessed areas [17]. A plaque was well-defined as a focal intima-media thickness ≥ 1.5 mm protuberant in the lumen [18]. Subjects were categorized as having focal (1 territory), intermediate (2 to 3 territories), or generalized (4 to 12 territories) atheromatous disease. All plaques were measured, and the total plaque area (cm2) was assessed [19].
Statistical analysis
Owing the non-normal distribution of the data detected by the Shapiro–Wilk test, quantitative data was expressed as the median [interquartile range]. Comparisons between the prediabetes and non-prediabetes groups were made using the Mann–Whitney U test for quantitative variables, and the Pearson’s Chi-squared test for categorical variables. The relationship between continuous variables was assessed by the Spearman correlation test.
A multivariable logistic regression model for the presence of subclinical atheromatous disease for the development cohort was performed including the following confounding elements: sex, age, HbA1c, total cholesterol, systolic blood pressure, the BMI, waist circumference, smoking habit and medical treatments. The calibration and discrimination of the multivariable logistic regression model were evaluated using the goodness of fit Hosmer–Lemeshow test and the area under the Receiver Operating Characteristic curve, correspondingly. All “p” values were based on a two-sided test of statistical significance, and significance was accepted at the level of p < 0.050. All statistical analyses were performed using SSPS statistical package (IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY, USA).
Results
From the baseline sample of 6809 subjects, prediabetes was diagnosed in 33.3% (n = 2269) of the subjects. The main clinical and metabolic data according to the HbA1c values are displayed in Table 1. Participants with prediabetes were older and presented a higher ratio of women and classical CV risk factors such as dyslipidemia, hypertension and obesity in comparison with the control group. The prevalence of subclinical atheromatous disease in the entire population was significantly higher in subjects with prediabetes than in control participants (70.4% vs. 67.5%, p = 0.017). This difference was at the expense of carotid territory (49.3% vs. 43.5%, p < 0.001), and disappeared when only the femoral territory was evaluated (54.1% vs. 52.5%, p = 0.228). When each of the six specific territories was analyzed in the left and right side, slightly marked differences were observed in the left arteries (Table 2). In addition, when only women were analyzed, the increased prevalence of subclinical atheromatous disease detected in postmenopausal control women when compared to premenopausal control women appeared to be attenuated among those with prediabetes (Additional file 1: Table S2).
We observed a significant correlation between HbA1c levels and the number of affected territories (r = 0.068, p = 0.001), but not with the total plaque area (r = − 0.008, p = 0.609). Participants with prediabetes almost increased twice the number of affected territories with plaque [2 (1 to 3) vs. 1 (0 to 3) territories, p = 0.002) compared with control subjects and, therefore, were more likely to be classified as individuals with generalized atheromatous disease (19.5% vs. 16.3%, p < 0.001). However, the vast majority (82.6%) presented less than 4 affected territories. In addition, no differences in the carotid plaque area (0.22 [0.12;0.42] vs. 0.20 [0.11;0.41], p = 0.555), the femoral plaque area (0.68 [0.29;1.24] vs. 0.68 [0.34;1.18], p = 0.683) or the total plaque area (0.96 [0.52;1.62] vs. 0.93 [0.56;1.55], p = 0.760) were observed between groups.
When the results were assessed according to sex, the differences regarding subclinical atheromatous disease were greater among males than females (Fig. 1). Men with prediabetes presented not only a higher number of plaques in both the carotid and femoral regions but also an increase of affected territories and total plaque area in comparison with age-matched individuals without prediabetes. By contrast, women with prediabetes only presented a higher number of plaques in the carotid region and a similar number of affected territories and total plaque area to age-matched women without prediabetes.
In the entire population, the quantity of cardiovascular risk factors was correlated with the number of affected territories with atheromatous plaque (r = 0.223, p < 0.001) and with the total plaque area (r = 0.192, p < 0.001). However, the presence of prediabetes only impacted on the burden of subclinical atheromatous disease when subjects presented three or more CV risk factors (Fig. 2a). Notably, when the analysis was performed taking sex into account, we observed that men with prediabetes and two or more CV risk factors displayed a significantly higher number of affected territories with atheromatous plaque in comparison with men free of prediabetes (Fig. 2b). By contrast, we did not find any significant differences between women with prediabetes and the control group regardless of the number of CV risk factors (Fig. 2c).
Plot displaying the number of affected territories with atheromatous plaque according to the quantity of cardiovascular risk factors such as dyslipidemia, blood hypertension, obesity, smoking habit or a first degree relative with premature cardiovascular disease in the; a entire population, b men and c women
Finally, the multivariable logistic regression model showed that smoking habit, male sex, HbA1c, age, systolic blood pressure, total cholesterol, BMI and lipid-lowering and antihypertensive drugs were independently associated with the presence of atheromatous disease in participants with prediabetes (Table 3). When both sexes were assessed separately, the same parameters excluding HbA1c accounted for subclinical atherosclerosis disease in females with prediabetes (Additional file 1: Table S3), whereas only smoking status, age and systolic blood pressure were the independent variables in males (Additional file 1: Table S4).
Discussion
In the present study we provide evidence that prediabetes modulates the atherogenic effect of cardiovascular risk factors in terms of the distribution of plaques and the total atherosclerotic burden in a sex-dependent manner. In this regard, our results suggest that prediabetes and underlying insulin resistance act as an enhancer of the atherosclerotic process, but only in men with 2 or more classical CV risk factors. In addition, the distribution of plaques occurred mainly in the carotid territory in women whereas a more severe and widespread plaque burden was observed in men.
Cardiovascular disease in prediabetes
The relationship between prediabetes and subclinical CV disease has been well-documented [20, 21]. In the Heinz Nixdorf Recall Study, a population-based cohort of 2184 without overt CV disease from Germany, participants with prediabetes (fasting plasma glucose ≥ 6.1 but < 7.0 mmol/l) showed a higher prevalence of coronary artery calcification than normoglycemic participants [20]. However, the association between impaired fasting glucose and coronary artery calcification was less pronounced in women [20]. In the Multi-Ethnic Study of Atherosclerosis, a cross-sectional study among 5121 participants without type 2 diabetes or CV disease, those in the highest quartile of HbA1c showed significantly higher values for common and internal carotid intimal-medial wall thickness in both sexes, but the association between HbA1c and carotid artery calcification was only present in women [21]. On the other hand, in a recent study with 6434 asymptomatic Korean individuals who underwent a coronary computed tomographic angiography, prediabetes was not associated with an increased risk of subclinical coronary atherosclerosis [22]. Our study adds information by providing the characteristics of the atheromatous process in a population of middle-aged subjects without previous vascular disease according to the presence of prediabetes. We describe how subjects with prediabetes suffer a higher prevalence of atheromatous disease, mainly in the carotid territories, when compared with subjects with normal HbA1c. In addition, vascular disease in participants with prediabetes is characterized by the presence of plaques of a similar area in a higher number of affected territories. Overall, our data reinforce the idea that CV disease is a progressive defect associated with glucose abnormalities, appearing and increasing throughout the prediabetes stage. In fact, in the subjects with prediabetes, HbA1c positively correlates with the number of plaques. However, it should be noted that in the population included in our study the total plaque area was similar to age-matched control subjects. In addition, prediabetes was only a trigger for the number of affected territories when at least 3 classic CV risk factors were present. These findings seriously call into question the importance of insulin resistance and the prediabetes stage as primary factors of atherogenesis in the type 2 diabetes population. The lack of significance of the waist circumference in the multivariable logistic regression model in both sexes also argues against this assumption. In the Coronary Artery Risk Development in Young Adults Study, for each 5-year-long duration of prediabetes the hazard ratio for the presence of coronary artery calcified plaque was only 1.07 (1.01 to 1.13) [23]. This result also supports the modest effect of prediabetes itself as a CV risk factor.
The different impact of prediabetes on atherosclerotic processes in men and women merits some comment. First, it has been suggested that men and women may progress from normoglycemia to overt type 2 diabetes by different ways: more men than women had impaired fasting glucose, whereas women more often had impaired glucose tolerance [24]. Also, in the Framingham Heart Study, the 4-year coronary heart disease event rate among participants with prediabetes differed according to the prediabetes definition and the participants’ sex [25]. Whether or not the different transitional stage from normoglycemia to diabetes has a differential effect in the atherogenic process is an issue that remains to be elucidated. Second, the relative contribution of ageing and menopause itself in the development of CV diseases still remains uncertain [26]. It should be noted that the youngest women recruited in the LERVAS cohort were 50 years old. Therefore, the relative protection of women against prediabetes-induced plaque formation seems to be unrelated with estrogen levels. However, the inherent difference in circulating testosterone levels between men and women could not be ruled out as an underlying mechanism accounting for the widespread and significantly greater plaque detected in men [27].
The predilection of prediabetes for the carotid territory deserves attention, particularly when its impact in CV disease may be markedly different. In an autopsy study, Dalager et al. described different features in the microscopic sections of the carotid and superficial femoral arteries, probably reflecting different formation pathways [28]. Unlike the femoral arteries, the carotid bifurcation was prone to foam cell lesions and plaque formation, and lipid core plaques were more much common in the carotid territory in samples from patients who died of coronary atherosclerosis [28]. Similarly, in vivo non-invasive magnetic resonance plaque-imaging visualized significant differences in plaque composition, with larger necrotic cores as well as hemorrhaged areas in the carotid arteries compared to the femoral arteries [29]. And in clinical practice, the significant correlation found between the stenosis of coronary segments and carotid plaque occurrence disappeared when femoral plaques were evaluated [30]. Therefore, carotid territories are more prone to develop complicated plaques than femoral arteries, thus explaining different rates in the progression of atherosclerotic disease and the outcomes of CV events in subjects with prediabetes [11, 31]. In this way, results from the Emerging Risk Factors Collaboration revealed that the risk of stroke in patients with diabetes mellitus is increased twofold compared with individuals without diabetes mellitus [32]; the risk of recurrent stroke is also increased [33]. Prediabetes (defined as impaired glucose tolerance or a combination of impaired fasting glucose plus impaired glucose tolerance) has also been associated with a higher future risk of stroke (relative risk 1.20, 95% confidence interval 1.07 to 1.35) [34]. The 10-year planned follow-up of the ILERVAS Project will give us relevant clinical information on this topic [13].
Prediabetes duration has been associated with subclinical atherosclerosis, suggesting that prevention strategies to reverse cumulative exposure to this metabolic transition stage are needed [35]. From the global 374 million people with prediabetes in 2017, only 1.95% will progress to type 2 diabetes per year, suggesting that a substantial number of subjects will continue unprotected against long-term intermediate glycemic elevations [1, 36]. Our results suggest that men with at least 2 traditional risk factors represent the target prediabetes sub-population in which the efforts for testing the protective effects of anti-atherogenic therapeutic strategies should be addressed.
Potential pathogenic mechanisms
The mechanisms which explain the burden of arterial plaque associated with prediabetes, and their impact on different arterial territories, are not yet fully understood. The role of hemodynamic features and the underlying blood vessel structure warrants attention, since vascular anatomy is not uniform for the thickness of intima-media layer and the left carotid artery originates directly from the aortic arch and is therefore exposed to a constantly higher shear stress [37, 38]. In contrast to the femoral artery, a transitional zone has been described in the carotid bifurcation, an artery segment between elastic and muscular cell types where foam cell lesions and lipid core plaque develop at early ages [28, 39]. In addition, in vivo magnetic resonance imaging studies have described how the decrease of the lumen area by femoral plaque progression is compensated for by positive remodeling, creating a dissimilar rate of progression of luminal stenosis between the carotid and femoral arteries [40]. The impact of metabolic changes associated with prediabetes in these selected segments, such as insulin resistance, low-grade chronic inflammation, advanced glycation end-products (AGEs) production, dyslipidemia or fibrinolytic dysfunction, in the carotid transitional zone or in arterial remodeling is unclear [41,42,43,44]. The concentration of the endogenous secretory receptor for the AGEs receptor in 220 patients with prediabetes was significantly lower than in 99 control subjects and was one of the main determinants of the intima-media thickness of the common carotid artery [42]. Similarly, insulin resistance indices were strongly related to carotid intima-media thickness, and plaque presence and area in patients without diabetes, but were without relevance when femoral atherosclerosis was evaluated [41]. More recently, Altin et al. [43] showed how common carotid, but not femoral, intima media thickness was significantly higher in 113 patients with insulin resistance (homeostasis model assessment index > 2.5) free of CV disease compared to 112 controls. In our population without previous CV events, male participants with prediabetes exhibited a higher prevalence of atheromatous plaque both in carotid and femoral territories in comparison with the control group. However, women with prediabetes only presented a higher number of plaques in the carotid region. These findings reinforce the rationale of selecting the carotid territory for performing a screening of subclinical CV disease in those subjects with prediabetes.
Limitations and strengths
This study has some limitations that need to be considered. First, it is a cross-sectional analysis, so the nature of the study has not allowed us to establish causality. However, we will be doing a follow-up of the entire population until 2028. Second, the three accepted prediabetes definitions according to the criteria of the American Diabetes Association seem to identify different populations, as often not all the tests identify prediabetes in the same individual [14, 45, 46]. Some advantages have been linked to HbA1c, such as that fasting is not required, and the nonappearance of daily alterations in periods of illness or stress, and its higher preanalytical stability [20]. In addition, the prediabetes HbA1c-based definitions appears to be more specific and to provide modest improvements in risk discrimination for CV disease and other clinical complications than definitions based on fasting plasma glucose [47]. Third, although we have tested HbA1c using a point-of-care instrument, the large population included in our study allowed us to define two well differentiated populations, not only in their HbA1c values but also in their anthropometric and clinical characteristics. In addition, we have no available data regarding the duration of prediabetes in our population. Finally, LDL-cholesterol was assessed regardless of the fasting state when total cholesterol was ≥ 200 mg/dl or only after 6 h of fasting when ≥ 250 mg/dl, what it is not the standard recommendation. However, it is not very far from the recent new lipid guidelines that summarizes that in adults ≥ 20 years old and not on lipid-lowering therapy (the 80.7% of our population), measurement of either fasting or a non-fasting lipid profile is effective in estimating atherosclerotic cardiovascular disease risk and recording baseline LDL-cholesterol [48].
Conclusions
In summary, prediabetes is associated with a significantly increased burden of atheromatous disease in men with 2 or more CV risk factors. This finding points to this subpopulation as the main target for strategies aimed at reducing CV risk factors and HbA1c. In addition, our results suggest that the global impact of prediabetes on the atherosclerotic process in the entire population is quite limited.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to is an ongoing study but are available from the corresponding author on reasonable request.
Abbreviations
- AGEs:
-
advanced glycation end-products
- BMI:
-
body mass index
- CV:
-
cardiovascular
- HbA1c:
-
glycosylated hemoglobin
- SIDIAP:
-
Information System for the Development of Research in Primary Care
References
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, Malanda B. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
American Diabetes Association. Economic costs of diabetes in the US in 2017. Diabetes Care. 2018;41:917–28.
Einarson TR, Acs A, Ludwig C, Panton UH. Economic burden of cardiovascular disease in type 2 diabetes: a systematic review. Value Health. 2018;21:881–90.
Laakso M, Lehto S. Epidemiology of risk factors for cardiovascular disease in diabetes and impaired glucose tolerance. Atherosclerosis. 1998;137:S65–73.
Yahagi K, Kolodgie FD, Lutter C, Mori H, Romero ME, Finn AV, Virmani R. Pathology of human coronary and carotid artery atherosclerosis and vascular calcification in diabetes mellitus. Arterioscler Thromb Vasc Biol. 2017;37:191–204.
Schernthaner G, Lotan C, Baltadzhieva-Trendafilova E, Ceponis J, Clodi M, Ducena K, Goncalvesova E, Guja C, Honka M, Janež A, Lalić N, Lehmann R, Nyolczas N, Pauklin P, Rynkiewicz A, Sergienko I, Duvnjak LS. Unrecognised cardiovascular disease in type 2 diabetes: is it time to act earlier? Cardiovasc Diabetol. 2018;17:145.
Rana JS, Dunning A, Achenbach S, Al-Mallah M, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng VY, Chinnaiyan K, Chow BJ, Cury R, Delago A, Feuchtner G, Hadamitzky M, Hausleiter J, Kaufmann P, Karlsberg RP, Kim YJ, Leipsic J, Labounty TM, Lin FY, Maffei E, Raff G, Villines TC, Shaw LJ, Berman DS, Min JK. Differences in prevalence, extent, severity, and prognosis of coronary artery disease among patients with and without diabetes undergoing coronary computed tomography angiography: results from 10,110 individuals from the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes): an InteRnational Multicenter Registry. Diabetes Care. 2012;35:1787–94.
Buysschaert M, Medina JL, Bergman M, Shah A, Lonier J. Prediabetes and associated disorders. Endocrine. 2015;48:371–93.
Wasserman DH, Wang TJ, Brown NJ. The vasculature in prediabetes. Circ Res. 2018;122:1135–50.
Burns SF, Lee S, Bacha F, Tfayli H, Hannon TS, Arslanian SA. Pre-diabetes in overweight youth and early atherogenic risk. Metabolism. 2014;63:1528–35.
Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ. 2016;355:i5953.
Lee G, Kim SM, Choi S, Kim K, Jeong SM, Son JS, Yun JM, Park SM. The effect of change in fasting glucose on the risk of myocardial infarction, stroke, and all-cause mortality: a nationwide cohort study. Cardiovasc Diabetol. 2018;17:51.
Betriu À, Farràs C, Abajo M, Martinez-Alonso M, Arroyo D, Barbé F, Buti M, Lecube A, Portero M, Purroy F, Torres G, Valdivielso JM, Fernández E. Randomised intervention study to assess the prevalence of subclinical vascular disease and hidden kidney disease and its impact on morbidity and mortality: the ILERVAS project. Nefrologia. 2016;36:389–96.
American Diabetes Association. Classification and diagnosis of diabetes. Sec. 2. In standards of medical care in diabetes—2017. Diabetes Care. 2017;40:S11–24.
Lenters-Westra E, Slingerland RJ. Three of 7 hemoglobin A1c point-of-care instruments do not meet generally accepted analytical performance criteria. Clin Chem. 2014;60:1062–72.
Sabetai MM, Tegos TJ, Nicolaides AN, Dhanjil S, Pare GJ, Stevens JM. Reproducibility of computer-quantified carotid plaque echogenicity: can we overcome the subjectivity? Stroke. 2000;31:2189–96.
Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Desvarieux M, Ebrahim S, Fatar M, Hernandez Hernandez R, Kownator S, Prati P, Rundek T, Taylor A, Bornstein N, Csiba L, Vicaut E, Woo KS, Zannad F. Advisory board of the 3rd watching the risk symposium 2004, 13th European stroke conference. Mannheim intima-media thickness consensus. Cerebrovasc Dis. 2004;18:346–9.
Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, Najjar SS, Rembold CM, Post WS, American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American society of echocardiography carotid intima-media thickness task force endorsed by the society for vascular medicine. J Am Soc Echocardiogr. 2008;21:93–111.
Tiozzo E, Gardener H, Hudson BI, Dong C, Della-Morte D, Crisby M, Goldberg RB, Elkind MS, Cheung YK, Wright CB, Sacco RL, Rundek T. High-density lipoprotein subfractions and carotid plaque: the Northern Manhattan Study. Atherosclerosis. 2014;237:163–8.
Moebus S, Stang A, Möhlenkamp S, Dragano N, Schmermund A, Slomiany U, Hoffmann B, Bauer M, Broecker-Preuss M, Mann K, Siegrist J, Erbel R, Jöckel KH, Heinz Nixdorf Recall Study Group. Association of impaired fasting glucose and coronary artery calcification as a marker of subclinical atherosclerosis in a population-based cohort—results of the Heinz Nixdorf Recall Study. Diabetologia. 2009;52:81–9.
McNeely MJ, McClelland RL, Bild DE, Jacobs DR Jr, Tracy RP, Cushman M, Goff DC Jr, Astor BC, Shea S, Siscovick DS. The association between A1C and subclinical cardiovascular disease: the multi-ethnic study of atherosclerosis. Diabetes Care. 2009;32:1727–33.
Park GM, Cho YR, Lee SW, Yun SC, Won KB, Ann SH, Kim YG, Kim SJ, Roh JH, Kim YH, Yang DH, Kang JW, Lim TH, Jung CH, Koh EH, Lee WJ, Kim MS, Lee KU, Park JY, Kim HK, Choe J, Lee SG. Prediabetes is not a risk factor for subclinical coronary atherosclerosis. Int J Cardiol. 2017;243:479–84.
Reis JP, Allen NB, Bancks MP, Carr JJ, Lewis CE, Lima JA, Rana JS, Gidding SS, Schreiner PJ. Duration of diabetes and prediabetes during adulthood and subclinical atherosclerosis and cardiac dysfunction in middle age: the CARDIA study. Diabetes Care. 2018;41:731–8.
Bock G, Dalla Man C, Campioni M, Chittilapilly E, Basu R, Toffolo G, Cobelli C, Rizza R. Pathogenesis of pre-diabetes: mechanisms of fasting and postprandial hyperglycemia in people with impaired fasting glucose and/or impaired glucose tolerance. Diabetes. 2006;55:3536–49.
Levitzky YS, Pencina MJ, D’Agostino RB, Meigs JB, Murabito JM, Vasan RS, Fox CS. Impact of impaired fasting glucose on cardiovascular disease: the Framingham Heart Study. J Am Coll Cardiol. 2008;51:264–70.
Scarabin PY. Endogenous sex hormones and cardiovascular disease in postmenopausal women: new but conflicting data. Ann Transl Med. 2018;6:448.
Srinath R, Hill Golden S, Carson KA, Dobs A. Endogenous testosterone and its relationship to preclinical and clinical measures of cardiovascular disease in the atherosclerosis risk in communities study. J Clin Endocrinol Metab. 2015;100:1602–8.
Dalager S, Paaske WP, Kristensen IB, Laurberg JM, Falk E. Artery-related differences in atherosclerosis expression: implications for atherogenesis and dynamics in intima-media thickness. Stroke. 2007;38:2698–705.
Helck A, Bianda N, Canton G, Yuan C, Hippe DS, Reiser MF, Gallino A, Wyttenbach R, Saam T. Intra-individual comparison of carotid and femoral atherosclerotic plaque features with in vivo MR plaque imaging. Int J Cardiovasc Imaging. 2015;31:1611–8.
Hulthe J, Wikstrand J, Emanuelsson H, Wiklund O, de Feyter PJ, Wendelhag I. Atherosclerotic changes in the carotid artery bulb as measured by B-mode ultrasound are associated with the extent of coronary atherosclerosis. Stroke. 1997;28:1189–94.
Huang Y, Cai X, Chen P, Mai W, Tang H, Huang Y, Hu Y. Associations of prediabetes with all-cause and cardiovascular mortality: a meta-analysis. Ann Med. 2014;46:684–92.
Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, Stehouwer CD, Lewington S, Pennells L, Thompson A, Sattar N, White IR, Ray KK, Danesh J. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–22.
Callahan A, Amarenco P, Goldstein LB, Sillesen H, Messig M, Samsa GP, Altafullah I, Ledbetter LY, MacLeod MJ, Scott R, Hennerici M, Zivin JA, Welch KM, SPARCL Investigators. Risk of stroke and cardiovascular events after ischemic stroke or transient ischemic attack in patients with type 2 diabetes or metabolic syndrome: secondary analysis of the stroke prevention by aggressive reduction in cholesterol levels (SPARCL) trial. Arch Neurol. 2011;68:1245–51.
Lee M, Saver JL, Hong KS, Song S, Chang KH, Ovbiagele B. Effect of pre-diabetes on future risk of stroke: meta-analysis. Br Med J. 2012;344:e3564.
Ferrannini E. Definition of intervention points in prediabetes. Lancet Diabetes Endocrinol. 2014;2:667–75.
Nichols GA, Hillier TA, Brown JB. Progression from newly acquired impaired fasting glusose to type 2 diabetes. Diabetes Care. 2007;30:228–33.
Polak JF, Person SD, Wei GS, Godreau A, Jacobs DR Jr, Harrington A, Sidney S, O’Leary DH. Segment-specific associations of carotid intima-media thickness with cardiovascular risk factors: the coronary artery risk development in young adults (CARDIA) study. Stroke. 2010;41:9–15.
Zarins CK, Giddens DP, Bharadvaj BK, Sottiurai VS, Mabon RF, Glagov S. Carotid bifurcation atherosclerosis. Quantitative correlation of plaque localization with flow velocity profiles and wall shear stress. Circ Res. 1983;53:502–14.
Janzen J. The microscopic transitional zone between elastic and muscular arteries. Arch Mal Coeur Vaiss. 2004;97:909–14.
Bianda N, Di Valentino M, Périat D, Segatto JM, Oberson M, Moccetti M, Sudano I, Santini P, Limoni C, Froio A, Stuber M, Corti R, Gallino A, Wyttenbach R. Progression of human carotid and femoral atherosclerosis: a prospective follow-up study by magnetic resonance vessel wall imaging. Eur Heart J. 2012;33:230–7.
Panayiotou AG, Kouis P, Griffin M, Nicolaides AN. Comparison between insulin resistance indices and carotid and femoral atherosclerosis: a cross-sectional population study. Int Angiol. 2015;34:437–44.
Di Pino A, Currenti W, Urbano F, Mantegna C, Purrazzo G, Piro S, Purrello F, Rabuazzo AM. Low advanced glycation end product diet improves the lipid and inflammatory profiles of prediabetic subjects. J Clin Lipidol. 2016;10:1098–108.
Altin C, Sade LE, Gezmis E, Yilmaz M, Ozen N, Muderrisoglu H. Assessment of epicardial adipose tissue and carotid/femoral intima media thickness in insulin resistance. J Cardiol. 2017;69:843–50.
Chaubey S, Nitsch D, Altmann D, Ebrahim S. Differing effect of modifiable cardiovascular risk factors on intima-media thickening and plaque formation at different sites of the arterial vasculature. Heart. 2010;96:1579–85.
Mostafa SA, Khunti K, Srinivasan BT, Webb D, Gray LJ, Davies MJ. The potential impact and optimal cut-points of using glycated haemoglobin, HbA1c, to detect people with impaired glucose regulation in a UK multi-ethnic cohort. Diabetes Res Clin Pract. 2010;90:100–8.
Lorenzo C, Hartnett S, Hanley AJ, Rewers MJ, Wagenknecht LE, Karter AJ, Haffner SM. Impaired fasting glucose and impaired glucose tolerance have distinct lipoprotein and apolipoprotein changes: the insulin resistance atherosclerosis study. J Clin Endocrinol Metab. 2013;98:1622–30.
Warren B, Pankow JS, Matsushita K, Punjabi NM, Daya NR, Grams M, Woodward M, Selvin E. Comparative prognostic performance of definitions of prediabetes: a prospective cohort analysis of the atherosclerosis risk in communities (ARIC) study. Lancet Diabetes Endocrinol. 2017;5:34–42.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task force on clinical practice guidelines. J Am Coll Cardiol. 2019;73:e285–350.
Acknowledgements
The ILERVAS project collaborators are: Ferran Barbé, José-Manuel Valdivielso, Glòria Arqué, Jessica González, Ana Vena, Eva Miquel, Marta Ortega-Bravo, Gerard Torres, Serafín Cambray, Manuel Portero-Otin, Mariona Jové, Montserrat Martínez-Alonso, Eva Castro, Pere Godoy. The authors would like to thank The Health Bus Staff, Fundació Renal Jaume Arnó, and the Primary Care teams from Lleida for recruiting subjects and their efforts in the accurate development of the ILERVAS project.
Funding
This work was partially supported by grants from the Diputació de Lleida and the Generalitat de Catalunya (2017SGR696 and SLT0021600250) and Menarini Spain S.A. CIBER de Diabetes y Enfermedades Metabólicas Asociadas and CIBER de Enfermedades Respiratorias are initiatives of the Instituto de Salud Carlos III.
Author information
Authors and Affiliations
Consortia
Contributions
ES and ÀB recruited patients, collected and analysed data, wrote the first draft of the manuscript, and had final approval of the version for publication; CL-C, MH, supervised the research, interpreted data, and critically reviewed the draft of the article; EF, FP, MB-L, CF-S, SB, RP and FR designed the study, supervised the statistical analysis, interpreted data, critically revised draft of the article, and had final approval of the version for publication; CH and RS collected and analysed data, contributed to the discussion and had final approval of the version for publication; AL designed the study, supervised the research, analysed and interpreted data, and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from all the ILERVAS participants. The protocol was approved by the Arnau de Vilanova University Hospital ethics committee (CEIC-1410). The study was conducted according to the ethical guidelines of the Helsinki Declaration and Spanish legislation regarding the protection of personal information was also followed.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Full results and methodological details regarding intra and inter rate reliability for plaque presence and plaque area by arterial territory. Table S2. Prevalence of subclinical atheromatous disease in each of the six specific territories in women according the menopausal state. Table S3. The multivariable logistic regression model for the presence of atheromatous disease among female subjects in the prediabetes stage. Table S4. The multivariable logistic regression model for the presence of atheromatous disease among male subjects in the prediabetes stage.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sánchez, E., Betriu, À., López-Cano, C. et al. Characteristics of atheromatosis in the prediabetes stage: a cross-sectional investigation of the ILERVAS project. Cardiovasc Diabetol 18, 154 (2019). https://doi.org/10.1186/s12933-019-0962-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-019-0962-6