Abstract
Background
Previous studies have documented that visceral adipose tissue is positively associated with the risk of diabetes. However, the association of subcutaneous adipose tissue with diabetes risk is still in dispute. We aimed to assess the associations between different adipose distributions and the risk of newly diagnosed diabetes in Chinese adults.
Methods
The Shanghai Nicheng Cohort Study was conducted among Chinese adults aged 45–70 years. The baseline data of 12,137 participants were analyzed. Subcutaneous and visceral fat area (SFA and VFA) were measured by magnetic resonance imaging. Diabetes was newly diagnosed using a 75 g oral glucose tolerance test.
Results
The multivariable-adjusted odds ratios (OR) and 95% confidence intervals (CI) of newly diagnosed diabetes per 1—standard deviation increase in SFA and VFA were 1.29 (1.19–1.39) and 1.61 (1.49–1.74) in men, and 1.10 (1.03–1.18) and 1.56 (1.45–1.67) in women, respectively. However, the association between SFA and newly diagnosed diabetes disappeared in men and was reversed in women (OR 0.86 [95% CI, 0.78–0.94]) after additional adjustment for body mass index (BMI) and VFA. The positive association between VFA and newly diagnosed diabetes remained significant in both sexes after further adjustment for BMI and SFA. Areas under the receiver operating characteristic curve of newly diagnosed diabetes predicted by VFA (0.679 [95% CI, 0.659–0.699] for men and 0.707 [95% CI, 0.690–0.723] for women) were significantly larger than by the other adiposity indicators.
Conclusions
SFA was beneficial for lower risk of newly diagnosed diabetes in women but was not associated with newly diagnosed diabetes in men after taking general obesity and visceral obesity into account. VFA, however, was associated with likelihood of newly diagnosed diabetes in both Chinese men and women.
Similar content being viewed by others
Background
Diabetes, an established risk factor of cardiovascular disease (CVD), is one of the fastest growing public health problems in the world [1]. Obesity, especially abdominal obesity, is a well-known underlying risk factor for the development of diabetes [2]. Recent studies suggested that excess adiposity in specific body depots might be associated with different risks of diabetes. For example, abdominal adiposity, in particular, visceral adipose tissue, is positively associated with the risk of diabetes among whites, African Americans, and Japanese Americans [3,4,5], but the association of subcutaneous adipose tissue from the abdominal or thigh region with diabetes risk is still in dispute [6, 7]. Given the complex nature of measuring depot-specific adipose tissue in living subjects, very few large studies have measured subcutaneous adipose tissue and visceral adipose tissue using magnetic resonance imaging (MRI) or computed tomography (CT) to assess their associations with diabetes risk.
China has the world’s largest diabetes epidemic. According to the latest data, 10.9% of Chinese adults have diabetes [8]. The ranges of body mass index (BMI) of Asian population are different to those of the European or African population. According to an expert consultation from the World Health Organization (WHO), generally, the mean or median BMI is lower in Asian populations than in non-Asian populations [9]. It has been hypothesized that Asians have higher adiposity per unit BMI compared with other ethnic groups, which puts them at an increased risk of type 2 diabetes mellitus at a lower level of BMI [9]. However, very few Chinese studies have assessed the association of different depot-specific adipose tissues with the risk of diabetes. Thus, our aim were to explore the associations between different adipose distributions (subcutaneous adipose tissue and visceral adipose tissue) measured by MRI and the risk of newly diagnosed diabetes screened by an oral glucose tolerance test (OGTT) in a large-sample study of Chinese adults.
Methods
Study participants
The Shanghai Nicheng Cohort Study was designed to assess the prevalence, incidence, and related factors of cardiometabolic diseases among adults in Nicheng County, a suburb of Shanghai, China. The baseline survey was conducted between April 2013 and August 2014. The target population covered 23,375 residents aged 45–70 years who had lived in Nicheng County for at least 5 years. A total of 21,408 residents were enrolled, and 17,212 participants finished the baseline survey (mean age 56.9, proportion of Men 45.3%). We excluded the participants without data on BMI, waist circumference or body fat percentage (n = 1091), fasting or 2-h glucose (n = 75), subcutaneous fat area (SFA) and visceral fat area (VFA) (n = 2861), and the participants with a history of diabetes (n = 1048). We excluded the participants with previously diagnosed diabetes because body weight changes have been reported for diabetes treatment in patients with known diabetes. The final sample in the present cross-sectional analysis comprised 12,137 participants (mean age 56.7, proportion of Men 44.5%), the participation flowchart was shown in Additional file 1. The study was approved by the Independent Ethics Community of Shanghai Sixth People’s Hospital and written informed consent was obtained from each participant.
Baseline measurements
Information on demographics, family history of diseases, medical history, leisure-time physical activity, smoking habits, and alcohol consumption was obtained through a standard questionnaire by trained investigators at local community clinics. Based on responses, the participants were classified as never smokers, ex-smokers, and current smokers. The participants was categorized as never, past, and current drinkers according to their alcohol consumption. The participants reported their leisure-time physical activity as 0, 1–29 min/day, and ≥ 30 min/day. Education was grouped as primary school or less, middle school, and high school or more. Family history of diabetes was defined as having a first-degree relative with diabetes.
Body weight and height were measured using the standardized protocol by specially trained investigators. Height and weight were measured without shoes and with light clothing. The measurements of height were rounded to the nearest centimeter, and weight to the nearest 100 g. Blood pressure was measured twice from the right arm after 5 min of sitting using a mercury sphygmomanometer at 3-min intervals, and the mean value was calculated. Waist circumference was measured at the midpoint between the lowest rib and the iliac crest on the mid-axillary line. BMI was calculated as weight in kilograms divided by the square of height in meters. Body fat was estimated with a Tanita body composition analyzer (TBF-418, Tanita Corp., Tokyo, Japan). Blood samples were collected from participants after an overnight fast of at least 10 h. Participants without a self-reported history of diabetes were administered an OGTT of 75 g glucose. Blood samples were drawn at 0, 30, and 120 min following the OGTT test. Plasma glucose was assessed by a glucose oxidase method. Glycated hemoglobin A1c (HbA1c) values were measured by high-performance liquid chromatography (VARIANT II, Bio-Rad Laboratories, Inc., Hercules, USA).
Measurement of abdominal adipose tissue
The day after the first visit for blood sampling and other measurements mentioned above, participants underwent abdominal MRI investigations via a 3.0 T General Electric scanner (GE Healthcare, Milwaukee, WI, USA) equipped with an abdominal coil in the Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. Each participant was positioned supine in the magnet and was scanned in cross-sectional planes. T1 axial images were obtained and centered at the navel with a slice thickness of 10.0 mm for 8 slices. Based on the Framingham Heart Study, Irlbeck et al. found that SFA and VFA at the umbilical level strongly correlated to visceral and subcutaneous fat volumes after adjustment for age in both women and men (r = 0.94 for SFA and subcutaneous fat volume and r = 0.98 for VFA and visceral fat volume in men; r = 0.99 for SFA and subcutaneous fat volume and r = 0.92 for VFA and visceral fat volume in women) [10]. In the present study, SFA and VFA were obtained from the umbilical slice, based on an area of 2-D pixels meeting the adipose shading threshold from the DICOM images of each participant. Segmentation of the images into SFA and VFA was conducted by two trained investigators using sliceOmatic image analysis software (version 5; Tomovision Inc., Montreal, QC, Canada). If results differed by more than 10%, a third investigator who did not know the results reanalyzed the images.
Definition
According to the 1999 WHO criteria [11], category of glucose regulation was defined as follows using an OGTT: isolated impaired fasting glucose (6.1 mmol/L ≤ fasting plasma glucose [FPG] < 7.0 mmol/L and 2-h plasma glucose [2hPG] < 7.8 mmol/L), isolated impaired glucose tolerance (FPG < 6.1 mmol/L and 7.8 mmol/L ≤ 2hPG < 11.1 mmol/L), combined impaired fasting glucose and impaired glucose tolerance (6.1 mmol/L ≤ FPG < 7.0 mmol/L and 7.8 mmol/L ≤ 2hPG < 11.1 mmol/L), and newly diagnosed diabetes ([1] without a self-reported diagnosis of diabetes that was determined previously by a health care professional, and [2] FPG ≥ 7.0 mmol/L and/or 2hPG ≥ 11.1 mmol/L). We also used the standards of medical care in diabetes-2018 proposed by American Diabetes Association (ADA) to define newly diagnosed diabetes in a sensitivity analysis: participants without a history of diabetes who had FPG ≥ 7.0 mmol/L or 2hPG ≥ 11.1 mmol/L during the baseline OGTT or HbA1c ≥ 6.5% [12].
Statistical analysis
Sex-specific mean (SD) and frequency (proportion) were revealed by different diabetes status (Non-diabetes and newly diagnosed diabetes). Student’s t test and Chi square tests were used to assess differences between two groups for continuous and categorical variables, respectively (Table 1). Logistic regression was used to assess the associations of SFA and VFA with the risk of newly diagnosed diabetes. SFA and VFA were entered in the following two ways: (1) as quartiles, and (2) as a continuous variable. Four models were constructed: Model 1 adjusted for age; Model 2 adjusted for potential confounding factors: age, education, leisure-time physical activity, smoking habit, alcohol consumption, systolic blood pressure, and family history of diabetes; Model 3 took general obesity into account and adjusted for variables in Model 2 as well as BMI; model 4 adjusted for variables in Model 3 as well as VFA or SFA. The interaction between SFA and VFA was assessed by likelihood ratio test. The receiver operating characteristic (ROC) curve was plotted and area under the curve (AUC) was calculated to assess the ability of different adiposity indicators to discriminate newly diagnosed diabetes. Restricted cubic spline was nested in logistic models to further explore the nonlinear or dose–response association of SFA or VFA with the risk of newly diagnosed diabetes [13, 14]. In order to lessen the influence of extreme values, we included participants with SFA and VFA from the 0.5 to 99.5 percentiles (SFA [cm2] 33.0–270.1 and 47.0–352.1, VFA [cm2] 19.5–294.4 and 27.3–243.6 for men and women, respectively). Three knots were created for men (SFA [cm2] 54.5, 122.4, and 202.8; VFA [cm2] 42.4, 117.0, and 209.8) and women (SFA [cm2] 84.2, 161.3, and 268.5; VFA [cm2] 50.3, 103.5, and 179.9). All statistical analyses were performed with IBM SPSS Statistics for Windows, version 24.0 (IBM Corp, 2016) or SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). P value < 0.050 (two-tailed) was considered statistically significant.
Results
Participants characteristics
General characteristics of the study population at baseline were presented in Table 1. A total of 5401 men and 6736 women were available for analysis. Participants of both sexes who were newly diagnosed with diabetes at baseline were slightly older, their FPG, 2hPG, BMI, waist circumference, blood pressure, SFA, VFA, and VFA/SFA were higher, and they were more likely to have a family history of diabetes, as compared with those who remained free of diabetes at baseline.
Correlations between adiposity indicators
Age-adjusted partial correlations were 0.779 in men (P < 0.001) and 0.677 in women (P < 0.001) for BMI and SFA, 0.695 in men (P < 0.001) and 0.663 in women (P < 0.001) for BMI and VFA, 0.725 in men (P < 0.001) and 0.623 in women (P < 0.001) for waist circumference and SFA, and 0.696 in men (P < 0.001) and 0.624 in women (P < 0.001) for waist circumference and VFA (Additional file 2).
Associations of SFA and VFA with risk of newly diagnosed diabetes
The multivariable-adjusted (age, education, leisure-time physical activity, smoking habit, alcohol consumption, systolic blood pressure, and family history of diabetes—Model 2) odds ratios (OR) of newly diagnosed diabetes across quartiles of SFA were 1.00 (95% confidence interval [CI], 1.00–1.00), 1.52 (95% CI, 1.19–1.94), 1.75 (95% CI, 1.38–2.23), and 1.87 (95% CI, 1.48–2.38) (P for trend < 0.001) for men, and 1.00 (95% CI, 1.00–1.00), 1.06 (95% CI, 0.87–1.30), 1.07 (95% CI, 0.87–1.31), and 1.27 (95% CI, 1.05–1.55) (P for trend = 0.014) for women, respectively (Table 2). The association was non-significant (P = 0.261) in men after further adjustment for BMI (Model 3) and was reversed significantly after additional adjustment for VFA (Model 4) in men (P for trend= 0.042) and women (P for trend= 0.003). When SFA was examined as a continuous variable, the multivariable-adjusted (Model 2) ORs of newly diagnosed diabetes for each 1 SD increase in SFA were 1.29 (95% CI, 1.19–1.39) in men, and 1.10 (95% CI, 1.03–1.18) in women. When BMI, VFA and SFA were entered into the multivariable-adjusted model simultaneously (Model 4), the positive association disappeared in men and was reversed in women (OR 0.86 [95% CI, 0.78–0.94]). Restricted cubic spline models showed the positive association between SFA and the risk of newly diagnosed diabetes in multivariable-adjusted Model 2, and the inverse association between SFA and the risk of newly diagnosed diabetes in multivariable-adjusted Model 4 (Fig. 1a, c, e and g).
Odds ratios for newly diagnosed diabetes based on different levels of SFA and VFA. Solid lines are multivariable-adjusted odds ratios, and dashed lines indicate 95% confidence intervals derived from restricted cubic spline regression. Odds ratios are plotted on a log scale. Odds ratios of SFA and VFA for newly diagnosed diabetes after adjustment for age, level of education, smoking habit, alcohol consumption, leisure-time physical activity, systolic blood pressure, and family history of diabetes (Model 2) are presented in a, b for men, and e, f for women, respectively. Odds ratios of SFA and VFA for newly diagnosed diabetes after adjustment for variables in Model 2 and also for body mass index as well as VFA or SFA (Model 4) are presented in c, d for men, and g, h for women, respectively. BMI body mass index, SFA subcutaneous fat area, and VFA visceral fat area
The multivariable-adjusted (Model 2) ORs of newly diagnosed diabetes across quartiles of VFA were 1.00 (95% CI, 1.00–1.00), 1.22 (95% CI, 0.93–1.61), 2.26 (95% CI, 1.75–2.90), and 3.40 (95% CI, 2.66–4.34) (P for trend < 0.001) for men, and 1.00 (95% CI, 1.00–1.00), 1.65 (95% CI, 1.29–2.13), 2.32 (95% CI, 1.83–2.95), and 3.66 (95% CI, 2.90–4.61) (P for trend < 0.001) for women, respectively (Table 3). The positive association remained significant among men (P for trend< 0.001) and women (P for trend< 0.001) after further adjustment for BMI (Model 3) and SFA (Model 4). When VFA was examined as a continuous variable, the multivariable-adjusted (Model 4) ORs of newly diagnosed diabetes for each 1 SD increase in VFA were 1.58 (95% CI, 1.43–1.75) in men, and 1.49 (95% CI, 1.37–1.63) in women. Restricted cubic splines models showed the similar positive association between VFA as a continuous variable and the risk of newly diagnosed diabetes in multivariable-adjusted Model 2 and Model 4 in both sexes (Fig. 1b, d, f and h).
In a sensitivity analysis, the multivariable-adjusted associations of newly diagnosed diabetes (2018 ADA criteria) with SFA and VFA were presented in Additional file 3: Tables S1, S2. The odds ratios between newly diagnosed diabetes and SFA or VFA were comparable regardless of diabetes defined by ADA or WHO criteria.
Additional file 4 presented the ROC curve for predicted probability of newly diagnosed diabetes by different adiposity indicators (VFA, VFA/SFA, BMI, waist circumference, and body fat percentage) in multivariable-adjusted Model 2. The AUCs were 0.648–0.679 for men and 0.683–0.707 for women. The pairwise comparisons showed that the AUCs of newly diagnosed diabetes predicted by VFA (0.679 [95% CI, 0.659–0.699] for men and 0.707 [95% CI, 0.690–0.723] for women) were significantly larger than by the other adiposity indicators (All P values < 0.02). There were no difference among the AUCs of BMI, waist circumference, body fat percentage, and VFA/SFA.
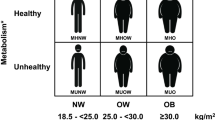
The joint associations of SFA and VFA with newly diagnosed diabetes risk in the multivariable-adjusted Model 2 were shown in Fig. 2. The positive associations between VFA and newly diagnosed diabetes risk were observed in participants with any quartile of SFA (All P for trend < 0.001). However, there were few significantly associations between SFA and newly diagnosed diabetes risk in participants with different quartiles of VFA. In women with VFA within the second quartile, SFA were negatively associated with risk of newly diagnosed diabetes (P for trend = 0.024). There were no significant interactions of VFA and SFA with the risk of newly diagnosed diabetes among both men and women (P values > 0.050).
Joint association of VFA, SFA, and newly diagnosed diabetes. Odds ratios were calculated after adjustment for age, level of education, smoking habit, alcohol consumption, leisure-time physical activity, systolic blood pressure, and family history of diabetes. Number of participants in each category and P for trend of the association of newly diagnosed diabetes with VFA and SFA were listed in table. SFA subcutaneous fat area, and VFA visceral fat area
Discussion
The present study found that SFA measured by MRI was negatively associated with risk of newly diagnosed diabetes in women (OR 0.86 [95% CI, 0.78–0.94]) but not in men (OR 0.96 [95% CI, 0.85–1.09]), after taking general obesity (assessed by BMI) and visceral obesity (assessed by VFA) into account. However, VFA was positively associated with the risk of newly diagnosed diabetes among both Chinese men and women, independent of BMI and SFA. Among the obesity indices of VFA, VFA/SFA, BMI, waist circumference, and body fat percentage, VFA had the best ability (AUC 0.679 [95% CI, 0.659–0.699] for men and 0.707 [95% CI, 0.690–0.723] for women) to discriminate newly diagnosed diabetes.
Few studies have examined the association between subcutaneous adipose tissue measured by CT or MRI and the risk of diabetes, and the results are inconsistent. Fox et al. [3] and Liu et al. [4] elucidated a positive association between subcutaneous adipose tissue and diabetes risk in white and African Americans, but they did not adjust for BMI in their analyses [3, 4, 15]. In the SABRE Study, Eastwood et al. used anthropometry-based prediction equations to estimate baseline subcutaneous adipose tissue and found a positive association of estimated subcutaneous adipose tissue with the risk of diabetes after adjustment for BMI, but only in South Asian men, not in European men and women, South Asian women, or African Caribbean men and women [16]. Other studies, however, failed to find any associations of subcutaneous adipose tissue with the risk of diabetes [5, 7]. Several studies indicated that subcutaneous adipose tissue possessed protective properties of insulin sensitivity after adjustment for BMI and visceral adipose tissue [17] or waist circumference as well as body fat [18]. However, to the best of our knowledge, no human study has provided direct evidence of a negative association between subcutaneous adipose tissue and risk of diabetes. The present study found a positive association between SFA measured by MRI and the risk of newly diagnosed diabetes after adjustment for major risk factors of diabetes. However, this positive association was non-significant in men and was reversed significantly after additional adjustment for general obesity (assessed by BMI) and visceral obesity (assessed by VFA) in women. These results first indicated that SFA was a favorable adipose depot rather than a pathogenic adipose depot for diabetes in women, and BMI and VFA confound the association between SFA and diabetes.
The exact mechanism of the favorable effects of subcutaneous adipose tissue on diabetes risk remained unclear, but several possible mechanisms have been proposed. The secretion or expression of more favorable adipokines such as leptin and adiponectin was higher in subcutaneous adipose tissue than in visceral adipose tissue [19, 20]. In addition, it is documented in animal studies that transplantation of subcutaneous adipose tissue to the visceral cavity improved glucose tolerance and insulin sensitivity [21, 22]. It was hypothesized that when subcutaneous adipose failed to store excess energy, energy can alternatively be deposited in visceral adipose, the liver, or the heart [2, 23]. Acting like a lipid-buffering tissue, subcutaneous adipose may directly or indirectly act to maintain the homeostasis of metabolism.
Compared to deposits in other fat tissues, visceral adipose tissue was more metabolically active due to different levels and affinity of receptors related to lipolysis [24, 25] and activity of enzymes related to lipolysis [26, 27]. Excess visceral adipose tissue was correlated with higher levels of free fatty acid overflow [2], inflammatory markers [28,29,30,31], and adipocytokines [32,33,34]. Kim et al. reported that fatty acid binding protein 4, S100 calcium binding protein A8/9, SH3 domain containing 1, α-2-HS-glycoprotein, and complement component 1, q subcomponent, A chain were up-regulated, while perilipin 1 and 4, carnitine palmitoyltransferase 2, acyl-CoA dehydrogenase, long chain, and acyl-CoA dehydrogenase, C-4 to C-12 straight chain were down-regulated in visceral adipose tissue of subjects with type 2 diabetes than in visceral adipose tissue of those with normal glucose tolerances. These proteins were either metabolic enzymes, adipokines, or were involved in the inflammation related process [35], which may contribute to the progress of insulin resistance or even diabetes.
Visceral adipose tissue measured by CT had a positive association with diabetes risk, even when accounting for other adiposity indicators, such as BMI, in white Americans [3], African Americans [4], and Japanese Americans [5]. Unlike white and African Americans, Asians are more likely to have abdominal adipose tissue, which leads to an increased risk of type 2 diabetes mellitus at lower BMI [9, 26]. Only one recent Chinese study demonstrated that VFA was independently associated with an increased risk of diabetes in women but not in men [36]. However, the VFA was measured by a fat area analyzer using bioelectrical impedance analysis, which is a less accurate measure of body composition than MRI and dual-energy X-ray absorptiometry. Moreover, in most of the above mentioned studies diabetes was diagnosed by fasting glucose alone, not an OGTT. Therefore, the authors could have missed some cases of diabetes [37], which usually resulted in a biased estimate of the association between different adiposity and the risk of diabetes. In the present study, we used MRI to measure body composition, and used an OGTT to diagnose diabetes among more than 12,000 Chinese participants. We first found a graded positive association between VFA and the risk of newly diagnosed diabetes among both Chinese men and women, and this association was independent of BMI, SFA and other known risk factors of diabetes. Moreover, out of the five adiposity indicators (VFA, VFA/SFA, BMI, waist circumference, and body fat percentage), VFA possessed the best ability to discriminate newly diagnosed diabetes.
As a cardiometabolic disease, diabetes is associated with 2–4 times higher risk of CVD and it double the risk of cardiovascular mortality [38,39,40,41]. Previous studies have documented that ectopic fat accumulation, mainly visceral adipose tissue, acting through the potential inflammatory response and oxidative phosphorylation pathways [42], is a risk factor of metabolic disorders, atherosclerosis, and CVD [3, 43,44,45]. The failure of visceral adipose tissue to store triglyceride could result in an increase of epicardial adipose tissue thickness [46]. Epicardial adipose tissue may turn into an adverse lopotoxic and pro-inflammatory organ, discharge fat free acid into the blood, and lead to CVD [46]. In addition, some studies showed that liver fat increased risk of impaired glucose regulation and type 2 diabetes [47], and mid-thigh lipid-rich muscle was associated with higher carotid artery intima-media thickness [48]. Although the association of abdominal subcutaneous adipose tissue with risk of atherosclerosis and CVD was in dispute [49,50,51,52], most of studies showed that thigh fat possessed favorable effect on cardiometabolic diseases. Sophie et al. found that thigh subcutaneous adipose tissue was protective for diabetes [6]. Han et al. documented that higher leg fat to total fat ratio was associated with decreased risk of CVD assessed by atherosclerotic cardiovascular disease risk equations [53]. More evidence was needed to elucidate the impact of adipose distribution on CVD.
There were several advantages of our study. Firstly, this is the first large population-based study focusing on the associations of different adipose distributions measured by MRI with the risk of newly diagnosed diabetes among Chinese adults. Secondly, diagnosis of diabetes was based on the WHO criteria [11] after a 2-h 75-g OGTT, which provided a comprehensive and accurate estimation of diabetes. Thirdly, the results of the present study were reliable, as almost all potential confounding factors had been adjusted. However, the present results were drawn from a cross-sectional study regarding the associations of SFA and VFA with the risk of diabetes, by which causal relationship cannot be inferred. A longitudinal study is still ongoing in the present study to identify the indicative power of future incident diabetes.
Conclusions
In conclusion, SFA measured by MRI was beneficial for lower risk of newly diagnosed diabetes in women but was not associated with newly diagnosed diabetes in men, while VFA was a good indicator for likelihood of newly diagnosed diabetes among Chinese adults, independently of BMI and SFA.
Abbreviations
- 2hPG:
-
2-h plasma glucose
- ADA:
-
American Diabetes Association
- AUC:
-
area under the curve
- BMI:
-
body mass index
- CVD:
-
cardiovascular disease
- FPG:
-
fasting plasma glucose
- HbA1c:
-
glycated hemoglobin A1c
- MRI:
-
magnetic resonance imaging
- OGTT:
-
oral glucose tolerance test
- OR:
-
odds ratio
- CI:
-
confidence interval
- CT:
-
computed tomography
- ROC:
-
receiver operating characteristic
- SFA:
-
subcutaneous fat area
- VFA:
-
visceral fat area
- WHO:
-
World Health Organization
References
NCD Risk Factor Collaboration. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387:1513–30.
Despres J-P, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–7.
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007;116:39–48.
Liu J, Fox CS, Hickson DA, May WD, Hairston KG, Carr JJ, et al. Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson Heart Study. J Clin Endocrinol Metab. 2010;95:5419–26.
Boyko EJ, Fujimoto WY, Leonetti DL, Newell-Morris L. Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care. 2000;23:465–71.
Eastwood SV, Tillin T, Wright A, Mayet J, Godsland I, Forouhi NG, et al. Thigh fat and muscle each contribute to excess cardiometabolic risk in South Asians, independent of visceral adipose tissue. Obesity. 2014;22:2071–9.
Bray GA, Jablonski KA, Fujimoto WY, Barrett-Connor E, Haffner S, Hanson RL, et al. Relation of central adiposity and body mass index to the development of diabetes in the Diabetes Prevention Program. Am J Clin Nutr. 2008;87:1212–8.
Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317:2515–23.
WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Irlbeck T, Massaro JM, Bamberg F, O’Donnell CJ, Hoffmann U, Fox CS. Association between single-slice measurements of visceral and abdominal subcutaneous adipose tissue with volumetric measurements: the Framingham Heart Study. Int J Obes. 2010;34:781–7.
World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO Consultation. Part 1: diagnosis and classification of diabetes mellitus. Geneva: World Health Organization; 1999.
American Diabetes Association. Classification and diagnosis of diabetes. Standards of medical care in diabetes—2018. Diabetes Care. 2018;41:S13–27.
Afzal S, Tybjærg-Hansen A, Jensen GB, Nordestgaard BG. Change in body mass index associated with lowest mortality in Denmark, 1976–2013. JAMA. 2016;315:1989–96.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61.
Liu J, Coady S, Carr JJ, Hoffmann U, Taylor HA, Fox CS. Differential associations of abdominal visceral, subcutaneous adipose tissue with cardiometabolic risk factors between African and European Americans. Obesity. 2014;22:811–8.
Eastwood SV, Tillin T, Dehbi HM, Wright A, Forouhi NG, Godsland I, et al. Ethnic differences in associations between fat deposition and incident diabetes and underlying mechanisms: the SABRE study. Obesity. 2015;23:699–706.
McLaughlin T, Lamendola C, Liu A, Abbasi F. Preferential fat deposition in subcutaneous versus visceral depots is associated with insulin sensitivity. J Clin Endocrinol Metab. 2011;96:E1756–60.
Philipsen A, Jorgensen ME, Vistisen D, Sandbaek A, Almdal TP, Christiansen JS, et al. Associations between ultrasound measures of abdominal fat distribution and indices of glucose metabolism in a population at high risk of type 2 diabetes: the ADDITION-PRO study. PLoS ONE. 2015;10:e0123062.
Lihn AS, Bruun JM, He G, Pedersen SB, Jensen PF, Richelsen B. Lower expression of adiponectin mRNA in visceral adipose tissue in lean and obese subjects. Mol Cell Endocrinol. 2004;219:9–15.
Van Harmelen V, Reynisdottir S, Eriksson P, Thorne A, Hoffstedt J, Lonnqvist F, et al. Leptin secretion from subcutaneous and visceral adipose tissue in women. Diabetes. 1998;47:913–7.
Foster MT, Shi H, Softic S, Kohli R, Seeley RJ, Woods SC. Transplantation of non-visceral fat to the visceral cavity improves glucose tolerance in mice: investigation of hepatic lipids and insulin sensitivity. Diabetologia. 2011;54:2890–9.
Tran TT, Yamamoto Y, Gesta S, Kahn CR. Beneficial effects of subcutaneous fat transplantation on metabolism. Cell Metab. 2008;7:410–20.
Heilbronn L, Smith SR, Ravussin E. Failure of fat cell proliferation, mitochondrial function and fat oxidation results in ectopic fat storage, insulin resistance and type II diabetes mellitus. Int J Obes Relat Metab Disord. 2004;28(Suppl 4):S12–21.
Bolinder J, Kager L, Ostman J, Arner P. Differences at the receptor and postreceptor levels between human omental and subcutaneous adipose tissue in the action of insulin on lipolysis. Diabetes. 1983;32:117–23.
Pedersen SB, Jonler M, Richelsen B. Characterization of regional and gender differences in glucocorticoid receptors and lipoprotein lipase activity in human adipose tissue. J Clin Endocrinol Metab. 1994;78:1354–9.
Tchernof A, Despres JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93:359–404.
Boivin A, Brochu G, Marceau S, Marceau P, Hould FS, Tchernof A. Regional differences in adipose tissue metabolism in obese men. Metabolism. 2007;56:533–40.
Sam S, Haffner S, Davidson MH, D’Agostino RB Sr, Feinstein S, Kondos G, et al. Relation of abdominal fat depots to systemic markers of inflammation in type 2 diabetes. Diabetes Care. 2009;32:932–7.
Chang EJ, Lee SK, Song YS, Jang YJ, Park HS, Hong JP, et al. IL-34 is associated with obesity, chronic inflammation, and insulin resistance. J Clin Endocrinol Metab. 2014;99:E1263–71.
Catalan V, Gomez-Ambrosi J, Rodriguez A, Ramirez B, Valenti V, Moncada R, et al. Increased IL-32 levels in obesity promote adipose tissue inflammation and extracellular matrix remodeling: effect of weight loss. Diabetes. 2016;65:3636–48.
Pou KM, Massaro JM, Hoffmann U, Vasan RS, Maurovich-Horvat P, Larson MG, et al. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation. 2007;116:1234–41.
Molica F, Morel S, Kwak BR, Rohner-Jeanrenaud F, Steffens S. Adipokines at the crossroad between obesity and cardiovascular disease. Thromb Haemost. 2015;113:553–66.
Kovacova Z, Tencerova M, Roussel B, Wedellova Z, Rossmeislova L, Langin D, et al. The impact of obesity on secretion of adiponectin multimeric isoforms differs in visceral and subcutaneous adipose tissue. Int J Obes. 2012;36:1360–5.
Hao Y, Ma X, Luo Y, Hu X, Pan X, Xiao Y, et al. Associations of serum adipocyte fatty acid binding protein with body composition and fat distribution in nondiabetic Chinese women. J Clin Endocrinol Metab. 2015;100:2055–62.
Kim SJ, Chae S, Kim H, Mun DG, Back S, Choi HY, et al. A protein profile of visceral adipose tissues linked to early pathogenesis of type 2 diabetes mellitus. Mol Cell Proteomics. 2014;13:811–22.
Lv X, Zhou W, Sun J, Lin R, Ding L, Xu M, et al. Visceral adiposity significantly associated with type 2 diabetes in middle-aged and elderly Chinese women: a cross-sectional study. J Diabetes. 2016. https://doi.org/10.1111/1753-0407.12499.
Qiao Q, Hu G, Tuomilehto J, Nakagami T, Balkau B, Borch-Johnsen K, et al. Age- and sex-specific prevalence of diabetes and impaired glucose regulation in 11 Asian cohorts. Diabetes Care. 2003;26:1770–80.
De Bacquer D, De Backer G, Ostor E, Simon J, Pyorala K. Predictive value of classical risk factors and their control in coronary patients: a follow-up of the EUROASPIRE I cohort. Eur J Cardiovasc Prev Rehabil. 2003;10:289–95.
Laakso M. Hyperglycemia and cardiovascular disease in type 2 diabetes. Diabetes. 1999;48:937–42.
Franco OH, Steyerberg EW, Hu FB, Mackenbach J, Nusselder W. Associations of diabetes mellitus with total life expectancy and life expectancy with and without cardiovascular disease. Arch Intern Med. 2007;167:1145–51.
Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–22.
Moreno-Viedma V, Amor M, Sarabi A, Bilban M, Staffler G, Zeyda M, et al. Common dysregulated pathways in obese adipose tissue and atherosclerosis. Cardiovasc Diabetol. 2016;15:120.
Bouchi R, Ohara N, Asakawa M, Nakano Y, Takeuchi T, Murakami M, et al. Is visceral adiposity a modifier for the impact of blood pressure on arterial stiffness and albuminuria in patients with type 2 diabetes? Cardiovasc Diabetol. 2016;15:10.
Fujimoto WY, Bergstrom RW, Boyko EJ, Chen KW, Leonetti DL, Newell-Morris L, et al. Visceral adiposity and incident coronary heart disease in Japanese–American men. The 10-year follow-up results of the Seattle Japanese–American Community Diabetes Study. Diabetes Care. 1999;22:1808–12.
Meijnikman AS, De Block CE, Verrijken A, Mertens I, Corthouts B, Van Gaal LF. Screening for type 2 diabetes mellitus in overweight and obese subjects made easy by the FINDRISC score. J Diabetes Complications. 2016;30:1043–9.
Gonzalez N, Moreno-Villegas Z, Gonzalez-Bris A, Egido J, Lorenzo O. Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes. Cardiovasc Diabetol. 2017;16:44.
Borel AL, Nazare JA, Smith J, Aschner P, Barter P, Van Gaal L, et al. Visceral, subcutaneous abdominal adiposity and liver fat content distribution in normal glucose tolerance, impaired fasting glucose and/or impaired glucose tolerance. Int J Obes. 2015;39:495–501.
Kim SK, Park SW, Hwang IJ, Lee YK, Cho YW. High fat stores in ectopic compartments in men with newly diagnosed type 2 diabetes: an anthropometric determinant of carotid atherosclerosis and insulin resistance. Int J Obes. 2010;34:105–10.
Abraham TM, Pedley A, Massaro JM, Hoffmann U, Fox CS. Association between visceral and subcutaneous adipose depots and incident cardiovascular disease risk factors. Circulation. 2015;132:1639–47.
Lee JJ, Pedley A, Hoffmann U, Massaro JM, Levy D, Long MT. Visceral and intrahepatic fat are associated with cardiometabolic risk factors above other ectopic fat depots: the Framingham Heart Study. Am J Med. 2018;131:684–92.
Narumi H, Yoshida K, Hashimoto N, Umehara I, Funabashi N, Yoshida S, et al. Increased subcutaneous fat accumulation has a protective role against subclinical atherosclerosis in asymptomatic subjects undergoing general health screening. Int J Cardiol. 2009;135:150–5.
Wildman RP, Janssen I, Khan UI, Thurston R, Barinas-Mitchell E, El Khoudary SR, et al. Subcutaneous adipose tissue in relation to subclinical atherosclerosis and cardiometabolic risk factors in midlife women. Am J Clin Nutr. 2011;93:719–26.
Han E, Lee YH, Lee BW, Kang ES, Lee IK, Cha BS. Anatomic fat depots and cardiovascular risk: a focus on the leg fat using nationwide surveys (KNHANES 2008–2011). Cardiovasc Diabetol. 2017;16:54.
Authors’ contributions
WJ, YB, and XH contributed to the study concept and design. WJ, PC, XH, GH analyzed the data and wrote the initial draft of the manuscript. WJ, YB, PC, XH, LW, SC, JW, LJ, HW collected and assembled the data. All authors contributed to critical revision of the manuscript. WJ is the guarantor of this work. All authors read and approved the final manuscript.
Acknowledgements
The authors thank all the investigators for their contributions (listed in Additional file 5) to this study.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The Shanghai Nicheng Cohort Study is an on-going study, and its dataset is not publicly available due to individual privacy of the participants. However, it may be available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the Independent Ethics Community of Shanghai Sixth People’s Hospital and written informed consent was obtained from each participant.
Funding
This study was supported by the Shanghai Health and Family Planning Commission (2013ZYJB1001), the Biomedical Engineering Cross Research Foundation of Shanghai Jiao Tong University (YG2015MS18), and the National Key Research and Development Program (2016YFC0903303). They have no role in study design, data collection and analysis, results interpretation or in preparation, review and approval of the manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1.
Participation flowchart.
Additional file 2.
Age-adjusted partial correlations between adiposity indicators.
Additional file 3.
Odds ratios of newly diagnosed diabetes according to the ADA criteria based on SFA or VFA as a continuous or category variable.
Additional file 4.
The receiver operating characteristic curve of adiposity indicators and newly diagnosed diabetes.
Additional file 5.
List of investigators.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chen, P., Hou, X., Hu, G. et al. Abdominal subcutaneous adipose tissue: a favorable adipose depot for diabetes?. Cardiovasc Diabetol 17, 93 (2018). https://doi.org/10.1186/s12933-018-0734-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-018-0734-8