Abstract
Background
It has been shown that visceral fat accumulation is associated with autonomic dysfunction, though the precise mechanism remains unclear. A recent basic study found that leptin can directly modulate autonomic function through the dorsomedial hypothalamus in relation to obesity. Here, we investigated the mutual relationships among plasma leptin, visceral fat accumulation, and cardiac autonomic dysfunction in patients with type 2 diabetes.
Methods
This cross-sectional study included 100 diabetic patients, and 100 age- and gender-matched non-diabetic patients with cardiovascular risk factors. Plasma leptin and soluble leptin receptor levels, visceral fat area (VFA), and heart rate variability (HRV) were determined in addition to classical cardiovascular risk factors.
Results
In the type 2 diabetic patients, VFA was significantly (p < 0.05) and inversely associated with HRV parameters (SDNN: r = −0.243; SDANN5: r = −0.238), while the plasma level of leptin, but not soluble leptin receptor, was also significantly (p < 0.05) and inversely associated with HRV parameters (SDNN: r = −0.243; SDANN5: r = −0.231). Multiple regression analysis showed that plasma leptin was significantly associated with SDNN and SDANN5 independent of other factors, including age, gender, presence of hypertension and dyslipidemia, duration of diabetes, HbA1c, and eGFR. Furthermore, the relationship of leptin with SDNN and SDANN5 (β = −0.279 and −0.254, respectively) remained significant (p < 0.05) after adjustment for VFA. In patients without diabetes, no significant associations were observed between leptin and any of the HRV parameters.
Conclusions
Hyperleptinemia may be involved in cardiac autonomic dysfunction in patients with type 2 diabetes and visceral obesity.
Similar content being viewed by others
Background
The prevalence of obesity has been increasing throughout the world over the past several decades to become a global health problem [1]. Excess visceral fat accumulation accompanied by obesity contributes to development of hypertension, diabetes, dyslipidemia, and cardiovascular events [2, 3]. Adiposity and cardiac autonomic dysfunction are closely associated [4], which may be involved in a higher incidence of cardiovascular events in obese individuals [5, 6]. However, the underlying mechanisms for cardiac autonomic dysfunction related to obesity remain unclear.
Leptin, a 16-kDa peptide hormone mainly derived from adipose tissue, suppresses appetite and increases energy expenditure via hypothalamic neurons expressing the receptor for leptin (Ob-R) [7, 8]. In clinical settings, plasma leptin concentrations have found to be strongly and positively correlated to adiposity [9–11], suggesting that high leptin levels lose their ability to restrain feeding and fat accumulation in obesity. Of importance, a recent study clearly showed that hyperleptinemia, a result of obesity, directly modulated blood pressure and heart rate by acting on the dorsomedial hypothalamus expressing Ob-R in obese mice, probably via the sympathetic nervous system [12].
These basic findings led us to examine whether plasma leptin contributes to the pathophysiology of autonomic dysfunction in obesity in humans. Measuring heart rate variability (HRV) using standard electrocardiographic monitoring is a practical way to assess impaired autonomic nervous system in clinical settings [13]. Reduced HRV predicts all-cause mortality and cardiovascular events not only in community-based population [5, 6], patients with myocardial infarction [14], and in diabetic patients [15–17]. Potential mechanisms for these associations include higher corrected QT prolongation, low exercise capacity, higher levels of inflammatory biomarker, and deregulation of progenitor cells [18–20]. Thus far, no reports examining the associations among adiposity, plasma leptin, and HRV in patients with type 2 diabetes have been presented. In the present study, we examined the mutual relationships among plasma leptin, HRV, and visceral fat volume in 100 patients with diabetes, as well as 100 age- and gender-matched non-diabetic patients with cardiovascular risk factors.
Methods
Study design and participants
This cross-sectional study included 100 patients with type 2 diabetes, and 100 age- and gender-matched patients without diabetes who participated in the Hyogo Sleep Cardio-Autonomic Atherosclerosis (HSCAA) Study, which was designed to examine the impacts of sleep, cardiac autonomic dysfunction, and subclinical atherosclerosis on cardiovascular events. All patients agreed to participate in the study by providing written informed consent and the study was approved by the Ethics Committee of Hyogo College of Medicine (approval No. 948). From the cohort, initial 100 sequential diabetic patients were included, and corresponding age- and gender-matched non-diabetic patients were sequentially selected. Details of the cohort appear elsewhere [21], and classical cardiovascular risk factors and diabetes were evaluated as described in that publication. In diabetic groups, use of anti-diabetic agents included sulfonylureas (n = 30), metformin (n = 35), pioglitazone (n = 11), dipeptidyl peptidase 4 (DPP4) inhibitors (n = 33), and α-glucosidase inhibitors (n = 9), glucagon like peptide 1 (GLP1) analogues (n = 2), and insulins (n = 19). Past history of cardiovascular disease (CVD) was defined as the presence of coronary artery disease (medical history of myocardial infarction or revascularization), cerebrovascular disease, or peripheral arterial disease (PAD). Diabetic neuropathy was defined as the presence of two or more of the following: neuropathic symptoms, decreased distal sensation, and unequivocally decreased or absent ankle reflexes [22]. Serum creatinine was measured using the enzymatic method. Estimated glomerular filtration rate (eGFR) in each patient was calculated using an equation for Japanese subjects, as previously described [23]. This cross-sectional study excluded participants with chronic kidney disease (CKD), defined as eGFR less than 30 ml/min/1.73 m2. The level of urinary albumin excretion (UAE) was measured in 24-h urine specimens by immunoturbidimetry. UAE <30, 30–300, and >300 mg/day was defined as normo-, micro-, and macro-albuminuria, respectively.
Cardiac autonomic nervous function
To evaluate cardiac autonomic function, HRV was determined using an Active Tracer (AC-301A, Arm Electronics, Tokyo, Japan), as previously described [24]. According to the recommendations for clinical use of HRV [13], the standard deviation of the NN(RR) interval (SDNN) and standard deviation of the average NN(RR) intervals for each 5-min (SDANN5) period were calculated. SDNN was considered to reflect all cyclic components responsible for variability in heart rate, while SDANN5 was used to represent change in heart rate due to cycles longer than 5 min [13].
Plasma leptin and soluble leptin receptor
Blood samples were obtained essentially in the morning after an overnight fast during measurement of HRV and then quickly centrifuged to obtain plasma. Plasma leptin and soluble Ob-R (sOb-R) levels were measured using an enzyme-linked immunosorbent assay kit (R&D Systems, Inc., Minneapolis, MN, USA), as previously described [25]. The intra- and inter-assay coefficients of variation for leptin were 3.2 and 4.9 %, respectively, and those for sOb-R were 3.5 and 6.7 %, respectively.
Measurement of visceral and subcutaneous fat area
Using abdominal computed tomography (SOMATOM Definition, Siemens Medical Solutions, Forchheim, Germany), we acquired a single 10-mm slice at the level of the umbilicus. Visceral fat area (VFA) and subcutaneous fat area (SFA) values were calculated with a Ziostation workstation (Ziosoft Inc., Tokyo, Japan), as previously described [26].
Statistical analysis
For analysis, HRV parameters (SDNN, SDANN5), and plasma leptin and sOb-R levels were logarithm-transformed (log) to achieve normal distribution. To compare variables between patients with and without diabetes, a non-repeated t test (continuous variables with normal distribution) and Chi square test (for categorical variables) were utilized. We performed simple and multiple regression analyses to evaluate the relationships between HRV parameters and various clinical parameters, including plasma leptin or sOb-R, and VFA. In multiple regression analysis, HRV parameters were set as a dependent variables, and VFA and plasma leptin levels were set as independent variables after adjusting for age, gender, eGFR, HbA1c levels, duration of diabetes (in affected patients), and presence of hypertension and dyslipidemia. All statistical analyses were performed by using the Statistical Package for the Social Sciences software (PASW Statistics version 18.0). All reported p values are 2-tailed and were considered statistically significant at a level <0.05.
Results
Clinical characteristics of subjects with and without diabetes
The subject characteristics are shown in Table 1. Those with diabetes exhibited significantly higher body mass index (BMI), eGFR, fasting plasma glucose (FPG), HbA1c, VFA, and SFA values. The prevalence of hypertension and dyslipidemia tended to be higher in diabetic than non-diabetic patients, while plasma leptin and sOb-R levels, and HRV parameters were not significantly different between the groups.
Associations of VFA, SFA, plasma leptin, and sOb-R levels with HRV parameters
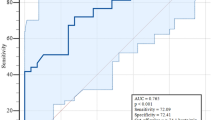
Table 2 shows the correlation coefficients between VFA, SFA, plasma leptin and sOb-R levels, and HRV parameters. VFA, but not SFA, was significantly and inversely associated with HRV parameters in patients with diabetes (Fig. 1a, b; Table 2). In contrast, such relationships were not observed in the non-diabetic patients (Table 2). Plasma leptin level was significantly and inversely associated with SDNN and SDANN5 in diabetic patients (Fig. 1c, d; Table 2), but not in the non-diabetic group (Table 2). Plasma sOb-R level was not significantly associated with HRV parameters in either group. On the other hand, plasma leptin levels were significantly and positively associated with VFA (r = 0.417, p < 0.001, r = 0.262; p = 0.008) and SFA (r = 0.732, p < 0.001, r = 0.693; p < 0.001) in both the diabetic and non-diabetic subjects. Also, plasma sOb-R level showed a tendency to be associated with VFA (r = −0.181, p = 0.072, r = −0.190; p = 0.058), but not with SFA, in both groups.
Associations of plasma leptin levels with HRV parameters in patients with or without diabetic neuropathy
Plasma leptin (0.83 ± 0.41 vs. 0.79 ± 0.42, p = 0.610), SDNN (2.00 ± 0.13 vs. 2.04 ± 0.14, p = 0.165), and SDANN5 (1.96 ± 0.13 vs. 1.99 ± 0.14, p = 0.183) were not significantly different when compared between diabetic patients with (n = 48) and without (n = 52) neuropathy. In patients with diabetic neuropathy, leptin was significantly associated with SDNN (r = −0.323, p = 0.02) or SDANN5 (r = −0.338, p = 0.014). On the other hand, in patients without diabetic neuropathy, leptin was not significantly associated with SDNN (r = −0.137, p = 0.355) or SDANN5 (r = −0.092, p = 0.534).
Plasma leptin level is associated with HRV parameters independent of clinical factors and adiposity in diabetic patients
To further examine whether the relationship of plasma leptin with cardiac autonomic dysfunction in diabetic patients was independent of the other confounding factors, multiple regression analyses were performed (Table 3). In basic model 1, which included age, male gender, eGFR, HbA1c, presence of hypertension and dyslipidemia, and duration of diabetes as covariates, duration of diabetes was the sole significant factor associated with SDNN and SDANN5. When VFA was included as an additional covariate (model 2), both duration of diabetes and VFA were significantly associated with HRV parameters. In model 3 (addition of plasma leptin to model 1 covariates), plasma leptin remained significantly associated with SDNN and SDANN5. When both VFA and plasma leptin were added to the model 1 covariates (model 4), plasma leptin, but not VFA, exhibited significant and independent associations with SDNN and SDANN5. When BMI was included as an additional covariate to model 4, plasma leptin, but neither VFA nor BMI, remained significantly associated with SDNN and SDANN5 (data no shown). When use of any of an anti-diabetic agent (sulfonylurea, metformin, pioglitazone, DPP4 inhibitor, α-glucosidase inhibitor, GLP1 analogue, or insulin) was included as an additional covariate to model 4, plasma leptin remained significantly associated with SDNN (data no shown). Among the agents, only use of insulin was independently associated with SDNN (β = −0.224, p = 0.034) together with plasma leptin (β = −0.256, p = 0.042) and duration of diabetes (β = −0.223, p = 0.041). Finally, when presence of previous CVD events was included as an additional covariate to model 4, plasma leptin remained significantly associated with SDNN (β = −0.275, p = 0.033) and tended to associated with SDANN5 (β = −0.243, p = 0.061). When multiple regression analyses were re-performed in 79 non-CVD patients (model 4), both plasma leptin and duration of diabetes showed tendency to associate with SDNN (β = −0.280, p = 0.062; β = −0.233, p = 0.051, respectively) and SDANN5 (β = −0.281, p = 0.066; β = −0.207, p = 0.087, respectively). In contrast, neither VFA nor plasma leptin was independently associated with HRV parameters in the non-diabetic patients (data not shown).
Discussion
Plasma leptin in obesity and diabetes
Plasma leptin levels are closely associated with adiposity [9–11], and its level correlated with increased metabolic syndrome components [27]. Plasma leptin level in diabetes is rather controversial; one recent study does not observe any significant difference between diabetic and non-diabetic subjects [28], others reported significant lower level in type 1 diabetic subjects [29] and type 2 diabetics with similar adiposity [30]. In our current study, plasma leptin level was comparable between diabetic and non-diabetic patients even though BMI, VFA and SFA are significant higher in diabetes. These controversial findings may be due to the status of insulin resistance and deficiency since plasma leptin level may be modified by insulin or C-peptide [29, 31].
Leptin and autonomic function
Recent study had shown that leptin may directly modulate autonomic function in obese mouse [12]. However, limited studies have shown an association of plasma leptin level with HRV in humans. In healthy subjects or police officers, short term frequency-domains of HRV are associated with plasma leptin [32, 33]. The relationships of time-domains of HRV, markers of overall autonomic function, with plasma leptin are only shown in male school teachers [34] and males with acute myocardial infarction [35]. Only a limited study showed significant association of HRV parameters with adiponectin/leptin ratio in diabetic subjects [36]. The present study is the first to show its relationship in type 2 diabetic patients, with the relationship fully adjusted for clinical parameters including quantitatively determined visceral adiposity. Its association was specific to diabetic patients since no significant associations were observed between leptin and any of the HRV parameters in non-diabetic patients.
Potential mechanisms why association between plasma leptin and HRV observed in diabetic patients only
Although it is not clear at present why the independent relationship between plasma leptin and HRV was observed in diabetic patients only, the presence of high glucose level might be a potential reason. Leptin activates proopiomelanocortin (POMC) neuron through the stimulation of the janus kinase 2-phosphoinositide 3-kinase pathway in POMC neuron and the inhibition of gamma-aminobutyric acid (GABA) release to POMC neuron in neuropeptide Y/agouti-related peptide neuron [37, 38]. Recent basic study found GABAergic synapses to POMC neurons differentially responded to leptin at different levels of glucose [39]. We found in diabetic subjects that reduced HRV was significantly association of with duration of diabetes, even though it was not significantly associated with HbA1c level.
Second, the presence of neuropathy may explain a difference in diabetic patients. Some previous studies have addressed the association between leptin and diabetic neuropathy with controversial results. Serum leptin level tended to be associated with sensory conduction velocity [40] in diabetic patients, while another study did not find any relationship [41]. In our hand, plasma leptin and HRV were not significantly different between diabetic patients with and without neuropathy. Interestingly, a significant association of leptin with HRV was seen in patients with, but not those without neuropathy. On the other hand, a recent study observed a decrease in HRV even in individuals with newly detected diabetes as well as those with impaired glucose tolerance [42]. Thus, the presence of neuropathy may not sufficiently explain why leptin is significantly associated with HRV only in diabetic patients.
Third, other comorbidities differentially distributed in the present two groups, such as hypertension, eGFR, and adiposity, may influence and modulate HRV parameters [4, 43–45]. Indeed, a study in healthy subjects showed association of leptin with HRV is dependent on BMI levels [33]. Thus, significantly higher BMI level in diabetic patients (26.1 kg/m2) than in non-diabetic patients (23.3 kg/m2) might contribute to inconsistent relation of leptin with HRV in our study. Several studies have shown that cardiac autonomic function is impaired in patients with cardiovascular diseases [5, 6, 46]. However, the association between leptin and HRV was similar even after adjusting for previous CVD events, and the association remained similar in diabetic patients without previous CVD events.
sOb-R and autonomic function
In this study, we also examined for the first time the association of plasma sOb-R with HRV. Although, plasma sOb-R tended to be inversely associated with adiposity, it was not significantly associated with any HRV parameters in our diabetic and non-diabetic patients.
Limitations
Our study design was cross-sectional, thus, even though relationships were explored in predictive terms, the results cannot be interpreted for any causal relationships. Longitudinal follow-up examinations of this cohort will clarify the role of leptin in autonomic dysfunction in patients with and without diabetes.
Conclusions
Our results showed that hyperleptinemia is associated with cardiac autonomic dysfunction in patients with diabetes, with the relationship independent of the accumulation of visceral fat.
Abbreviations
- Ob-R:
-
receptor for leptin
- HRV:
-
heart rate variability
- CVD:
-
cardiovascular disease
- DPP4:
-
dipeptidyl peptidase 4
- GLP1:
-
glucagon-like peptide 1
- PAD:
-
peripheral arterial disease
- eGFR:
-
estimated glomerular filtration rate
- CKD:
-
chronic kidney disease
- UAE:
-
urinary albumin excretion
- SDNN:
-
standard deviation of the NN(RR) interval
- SDANN5:
-
standard deviation of the average NN(RR) intervals for each 5-min
- sOb-R:
-
soluble Ob-R
- VFA:
-
visceral fat area
- SFA:
-
subcutaneous fat area
- BMI:
-
body mass index
- FPG:
-
fasting plasma glucose
- LF:
-
low frequency
- HF:
-
high frequency
- POMC:
-
proopiomelanocortin
- GABA:
-
gamma-aminobutyric acid
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. doi:10.1016/S0140-6736(14)60460-8.
Nakamura T, Tokunaga K, Shimomura I, Nishida M, Yoshida S, Kotani K, et al. Contribution of visceral fat accumulation to the development of coronary artery disease in non-obese men. Atherosclerosis. 1994;107(2):239–46.
Okauchi Y, Nishizawa H, Funahashi T, Ogawa T, Noguchi M, Ryo M, et al. Reduction of visceral fat is associated with decrease in the number of metabolic risk factors in Japanese men. Diabetes Care. 2007;30(9):2392–4. doi:10.2337/dc07-0218.
Peterson HR, Rothschild M, Weinberg CR, Fell RD, McLeish KR, Pfeifer MA. Body fat and the activity of the autonomic nervous system. N Engl J Med. 1988;318(17):1077–83. doi:10.1056/NEJM198804283181701.
Tsuji H, Larson MG, Venditti FJ Jr, Manders ES, Evans JC, Feldman CL, et al. Impact of reduced heart rate variability on risk for cardiac events. The Framingham Heart Study. Circulation. 1996;94(11):2850–5.
Liao D, Cai J, Rosamond WD, Barnes RW, Hutchinson RG, Whitsel EA, et al. Cardiac autonomic function and incident coronary heart disease: a population-based case-cohort study. The ARIC Study. Atherosclerosis Risk in Communities Study. Am J Epidemiol. 1997;145(8):696–706.
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372(6505):425–32. doi:10.1038/372425a0.
Friedman JM, Halaas JL. Leptin and the regulation of body weight in mammals. Nature. 1998;395(6704):763–70. doi:10.1038/27376.
Schwartz MW, Prigeon RL, Kahn SE, Nicolson M, Moore J, Morawiecki A, et al. Evidence that plasma leptin and insulin levels are associated with body adiposity via different mechanisms. Diabetes Care. 1997;20(9):1476–81.
Al-Daghri NM, Al-Attas OS, Al-Rubeaan K, Mohieldin M, Al-Katari M, Jones AF, et al. Serum leptin and its relation to anthropometric measures of obesity in pre-diabetic Saudis. Cardiovasc Diabetol. 2007;6:18. doi:10.1186/1475-2840-6-18.
Nishimura R, Sano H, Matsudaira T, Morimoto A, Miyashita Y, Shirasawa T, et al. Changes in body mass index, leptin and adiponectin in Japanese children during a three-year follow-up period: a population-based cohort study. Cardiovasc Diabetol. 2009;8:30. doi:10.1186/1475-2840-8-30.
Simonds SE, Pryor JT, Ravussin E, Greenway FL, Dileone R, Allen AM, et al. Leptin mediates the increase in blood pressure associated with obesity. Cell. 2014;159(6):1404–16. doi:10.1016/j.cell.2014.10.058.
Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task force of the European society of cardiology and the North American society of pacing and electrophysiology. Eur Heart J. 1996;17(3):354–81.
Katz A, Liberty IF, Porath A, Ovsyshcher I, Prystowsky EN. A simple bedside test of 1-minute heart rate variability during deep breathing as a prognostic index after myocardial infarction. Am Heart J. 1999;138(1 Pt 1):32–8.
Valensi P, Sachs RN, Harfouche B, Lormeau B, Paries J, Cosson E, et al. Predictive value of cardiac autonomic neuropathy in diabetic patients with or without silent myocardial ischemia. Diabetes Care. 2001;24(2):339–43.
Maser RE, Mitchell BD, Vinik AI, Freeman R. The association between cardiovascular autonomic neuropathy and mortality in individuals with diabetes: a meta-analysis. Diabetes Care. 2003;26(6):1895–901.
Vinik AI, Ziegler D. Diabetic cardiovascular autonomic neuropathy. Circulation. 2007;115(3):387–97. doi:10.1161/CIRCULATIONAHA.106.634949.
Veglio M, Borra M, Stevens LK, Fuller JH, Perin PC. The relation between QTc interval prolongation and diabetic complications. The EURODIAB IDDM Complication Study Group. Diabetologia. 1999;42(1):68–75.
Karjalainen JJ, Kiviniemi AM, Hautala AJ, Piira OP, Lepojarvi ES, Peltola MA, et al. Determinants and prognostic value of cardiovascular autonomic function in coronary artery disease patients with and without type 2 diabetes. Diabetes Care. 2014;37(1):286–94. doi:10.2337/dc13-1072.
Dutta P, Courties G, Wei Y, Leuschner F, Gorbatov R, Robbins CS, et al. Myocardial infarction accelerates atherosclerosis. Nature. 2012;487(7407):325–9. doi:10.1038/nature11260.
Kadoya M, Koyama H, Kurajoh M, Kanzaki A, Kakutani-Hatayama M, Okazaki H, et al. Sleep, cardiac autonomic function, and carotid atherosclerosis in patients with cardiovascular risks: HSCAA study. Atherosclerosis. 2015;238(2):409–14. doi:10.1016/j.atherosclerosis.2014.12.032.
Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33(10):2285–93. doi:10.2337/dc10-1303.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53(6):982–92. doi:10.1053/j.ajkd.2008.12.034.
Kadoya M, Koyama H, Kanzaki A, Kurajoh M, Hatayama M, Shiraishi J, et al. Plasma brain-derived neurotrophic factor and reverse dipping pattern of nocturnal blood pressure in patients with cardiovascular risk factors. PLoS One. 2014;9(8):e105977.
Morioka T, Emoto M, Yamazaki Y, Kawano N, Imamura S, Numaguchi R, et al. Leptin is associated with vascular endothelial function in overweight patients with type 2 diabetes. Cardiovasc Diabetol. 2014;13:10. doi:10.1186/1475-2840-13-10.
Sugisawa N, Tokunaga M, Tanizawa Y, Bando E, Kawamura T, Terashima M. Intra-abdominal infectious complications following gastrectomy in patients with excessive visceral fat. Gastric Cancer. 2012;15(2):206–12. doi:10.1007/s10120-011-0099-0.
Abu-Farha M, Behbehani K, Elkum N. Comprehensive analysis of circulating adipokines and hsCRP association with cardiovascular disease risk factors and metabolic syndrome in Arabs. Cardiovasc Diabetol. 2014;13:76. doi:10.1186/1475-2840-13-76.
Vinagre I, Sanchez-Quesada JL, Sanchez-Hernandez J, Santos D, Ordonez-Llanos J, De Leiva A, et al. Inflammatory biomarkers in type 2 diabetic patients: effect of glycemic control and impact of LDL subfraction phenotype. Cardiovasc Diabetol. 2014;13:34. doi:10.1186/1475-2840-13-34.
Soliman AT, Omar M, Assem HM, Nasr IS, Rizk MM, El Matary W, et al. Serum leptin concentrations in children with type 1 diabetes mellitus: relationship to body mass index, insulin dose, and glycemic control. Metabolism. 2002;51(3):292–6.
Tatti P, Masselli L, Buonanno A, Di Mauro P, Strollo F. Leptin levels in diabetic and nondiabetic subjects. Endocrine. 2001;15(3):305–8. doi:10.1385/ENDO:15:3:305.
Garcia-Serrano S, Gutierrez-Repiso C, Gonzalo M, Garcia-Arnes J, Valdes S, Soriguer F, et al. C-peptide modifies leptin and visfatin secretion in human adipose tissue. Obesity (Silver Spring). 2015;23(8):1607–15. doi:10.1002/oby.21137.
Paolisso G, Manzella D, Montano N, Gambardella A, Varricchio M. Plasma leptin concentrations and cardiac autonomic nervous system in healthy subjects with different body weights. J Clin Endocrinol Metab. 2000;85(5):1810–4. doi:10.1210/jcem.85.5.6511.
Charles LE, Burchfiel CM, Sarkisian K, Li S, Miller DB, Gu JK, et al. Leptin, adiponectin, and heart rate variability among police officers. Am J Hum Biol. 2015;27(2):184–91. doi:10.1002/ajhb.22636.
Pieterse C, Schutte R, Schutte AE. Autonomic activity and leptin in Africans and whites: the SABPA study. J Hypertens. 2014;32(4):826–33. doi:10.1097/HJH.0000000000000110.
Piestrzeniewicz K, Luczak K, Lelonek M, Wranicz JK, Goch JH. Obesity and heart rate variability in men with myocardial infarction. Cardiol J. 2008;15(1):43–9.
Lieb DC, Parson HK, Mamikunian G, Vinik AI. Cardiac autonomic imbalance in newly diagnosed and established diabetes is associated with markers of adipose tissue inflammation. Exp Diabetes Res. 2012;2012:878760. doi:10.1155/2012/878760.
Cowley MA, Smart JL, Rubinstein M, Cerdan MG, Diano S, Horvath TL, et al. Leptin activates anorexigenic POMC neurons through a neural network in the arcuate nucleus. Nature. 2001;411(6836):480–4. doi:10.1038/35078085.
Vong L, Ye C, Yang Z, Choi B, Chua S Jr, Lowell BB. Leptin action on GABAergic neurons prevents obesity and reduces inhibitory tone to POMC neurons. Neuron. 2011;71(1):142–54. doi:10.1016/j.neuron.2011.05.028.
Lee DK, Jeong JH, Chun SK, Chua S Jr, Jo YH. Interplay between glucose and leptin signalling determines the strength of GABAergic synapses at POMC neurons. Nat Commun. 2015;6:6618. doi:10.1038/ncomms7618.
Matsuda M, Kawasaki F, Inoue H, Kanda Y, Yamada K, Harada Y, et al. Possible contribution of adipocytokines on diabetic neuropathy. Diabetes Res Clin Pract. 2004;66(Suppl 1):S121–3. doi:10.1016/j.diabres.2004.05.010.
Sari R, Balci MK, Apaydin C. The relationship between plasma leptin levels and chronic complication in patients with type 2 diabetes mellitus. Metab Syndr Relat Disord. 2010;8(6):499–503. doi:10.1089/met.2009.0127.
Ziegler D, Voss A, Rathmann W, Strom A, Perz S, Roden M, et al. Increased prevalence of cardiac autonomic dysfunction at different degrees of glucose intolerance in the general population: the KORA S4 survey. Diabetologia. 2015;58(5):1118–28. doi:10.1007/s00125-015-3534-7.
Huikuri HV, Ylitalo A, Pikkujamsa SM, Ikaheimo MJ, Airaksinen KE, Rantala AO, et al. Heart rate variability in systemic hypertension. Am J Cardiol. 1996;77(12):1073–7.
Mylonopoulou M, Tentolouris N, Antonopoulos S, Mikros S, Katsaros K, Melidonis A, et al. Heart rate variability in advanced chronic kidney disease with or without diabetes: midterm effects of the initiation of chronic haemodialysis therapy. Nephrol Dial Transplant. 2010;25(11):3749–54. doi:10.1093/ndt/gfq226.
Poliakova N, Despres JP, Bergeron J, Almeras N, Tremblay A, Poirier P. Influence of obesity indices, metabolic parameters and age on cardiac autonomic function in abdominally obese men. Metabolism. 2012;61(9):1270–9. doi:10.1016/j.metabol.2012.02.006.
Ryan C, Hollenberg M, Harvey DB, Gwynn R. Impaired parasympathetic responses in patients after myocardial infarction. Am J Cardiol. 1976;37(7):1013–8.
Authors’ contributions
MK, MK, MK, MN, AM, AK, MK, HO and TS collected, analyzed and discussed data. MK and HK analyzed and wrote the manuscript. YM, TY, EM, MI and MN reviewed the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We thank the other investigators, as well as staff and participants of the Hyogo Sleep Cardio-Autonomic Atherosclerosis (HSCAA) study for their valuable contributions.
Sources of funding
This study was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (23591329 to H.K.), and unrestricted research grants from MSD and Teijin Pharmaceutical Companies.
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kurajoh, M., Koyama, H., Kadoya, M. et al. Plasma leptin level is associated with cardiac autonomic dysfunction in patients with type 2 diabetes: HSCAA study. Cardiovasc Diabetol 14, 117 (2015). https://doi.org/10.1186/s12933-015-0280-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-015-0280-6