Abstract
Background
To assess whether the Multidisciplinary Risk Assessment and Management Program for Patients with Diabetes Mellitus (RAMP-DM) led to improvements in biomedical outcomes, observed cardiovascular events and predicted cardiovascular risks after 12-month intervention in the primary care setting.
Methods
A random sample of 1,248 people with diabetes enrolled to RAMP-DM for at least 12 months was selected and 1,248 people with diabetes under the usual primary care were matched by age, sex, and HbA1c level at baseline as the usual care group. Biomedical and cardiovascular outcomes were measured at baseline and at 12-month after the enrollment. Difference-in-differences approach was employed to measure the effect of RAMP-DM on the changes in biomedical outcomes, proportion of subjects reaching treatment targets, observed and predicted cardiovascular risks.
Results
Compared to the usual care group, RAMP-DM group had lower cardiovascular events incidence (1.21% vs 2.89%, P = 0.003), and net decrease in HbA1c (−0.20%, P < 0.01), SBP (−3.62 mmHg, P < 0.01) and 10-year cardiovascular disease (CVD) risks (total CVD risk, −2.06%, P < 0.01; coronary heart disease (CHD) risk, −1.43%, P < 0.01; stroke risk, −0.71%, P < 0.01). The RAMP-DM subjects witnessed significant rises in the proportion of reaching treatment targets of HbA1c, and SBP/DBP. After adjusting for confounding variables, the significance remained for HbA1c, predicted CHD and stroke risks.
Conclusions
The RAMP-DM resulted in greater improvements in HbA1c and reduction in observed and predicted cardiovascular risks at 12 months follow-up, which indicated a risk-stratification multidisciplinary intervention was an effective strategy for managing Chinese people with diabetes in the primary care setting.
Trial registry
ClinicalTrials.gov, NCT02034695
Similar content being viewed by others
Background
Diabetes mellitus (DM) has become one of the major disease burdens in the world. It was estimated that by 2013, there were at least 382 million people with diabetes all over the world [1], and a 55% increase is anticipated by 2035 [2]. In Hong Kong, the prevalence of diagnosed diabetes reached 5% in the whole population and 20% in those aged above 65 years old. Diabetes is the leading cause of coronary heart disease, stroke, end stage renal disease, blindness and amputation [3],[4]. Early screening of the risk factors or precursory symptoms of diabetic complications is crucial, so early treatment can be given to prevent complications and mortalities. Many international guidelines have started to emphasis the comprehensive care for people with diabetes, which takes into account the integrated management of microvascular and macrovascular risk rather than only focusing on glycemic control [5]–[7].
Given the large number of people with diabetes and the huge disease burden, risk stratification based management strategy is appealing, so that resources can be allocated accordingly. Personalized treatment goals in clinical measurements and lifestyle modifications based on risk stratification are highly recommended by current guidelines [6]–[8]. Personalized diabetology is advocated by researchers as the potential solution to deal with the uncertainty in treatment and translate the evidence from randomized control trials (RCTs) to the real-world. However, studies on the effects of personalized treatment are sparse [9].
The Chronic Care Model in primary care developed by Dr. Wagner provided a multidimensional solution to achieving optimal primary care for patients with chronic diseases [10]. Among the six components identified in this model, four are usually explicitly addressed in chronic care management, which are delivery system redesign, decision support, clinical information system and self-management support. A systematic review found that to achieve positive outcomes, at least two of these components were included in interventions, and positive outcomes were found in all five studies containing four components [11], indicating that multidisciplinary approach is crucial to improve the control of diabetes.
Previously, a prospective trial of risk stratification and intervention involving 370 people with diabetes was completed in the U.S. [12]. Risk stratification was based on blood pressure, self-monitoring of blood glucose, microalbuminuria, foot examination and self-reported complications. Interventions for high-, moderate- and low-risk groups followed the American Diabetes Association Clinical Practice Recommendations. After a 12-month follow-up, this study found a considerable increase in the percentage of patients reaching HbA1C < 7% and blood pressure <130/85 mmHg. The net benefit of the intervention group compared to the control group was not reported [12]. Although the intervention in this study involves all the four components of the Chronic Care Model [10], it was conducted within staff-model primary care clinics. The generalizability of the study results to Asian populations is, however, doubtful.
In Asia, researchers of the Joint Asia Diabetes Evaluation Program (JADE) developed a web-based risk stratification and comprehensive care model for people with diabetes. This model includes a series of risk engines to stratify patients into different risk groups, and comprehensive care protocols recommended by the International Diabetes Federation. Doctors can access to this care model by an electronic portal [13]. This program addressed the decision support and clinical information system. It was reported that 3687 patients over seven Asian countries were enrolled through the electronic portal during 2007 to 2009, whereas the effectiveness of this model compared to the usual care is not clear [14].
A complex integrated care program for people with diabetes and the elderly was piloted in London. The interventions included risk stratification and a multi-disciplinary team led by general practitioners or consultants [15]. A comprehensive evaluation approach was proposed to assess the impact of the program on clinical outcomes as well as service use [16]. The results of the evaluation have not reported yet.
Up to date, evidence is lacking about the effectiveness of risk-stratification and risk-specific management programs for Chinese people with diabetes in the primary care setting. This study aimed at evaluating the effectiveness of a Multidisciplinary Risk Assessment and Management Program for Patients with Diabetes Mellitus (RAMP-DM) at 12 months follow-up in terms of biomedical outcomes, observed cardiovascular events and predicted long-term cardiovascular risks in the primary care setting. This was the first study to provide imperative translational evidence of risk-stratification and risk-specific management for diabetes in the real world primary care setting.
Methods
Study design
We conducted a longitudinal comparative study to compare the changes of biomedical measurements, observed cardiovascular events and cardiovascular risks at 12 months follow-up using a difference-in-differences approach between the RAMP-DM group and the usual care group.
Setting of RAMP-DM
The RAMP-DM is a territory-wide program which intends to cover all the people with diabetes under the care of public General Out-Patient Clinics (GOPCs) in Hong Kong. GOPCs provide primary care for about 190,000 people with diabetes, which account for about 60% of all the people with diabetes in Hong Kong. From August 2009 to June 2010, the RAMP-DM was piloted in four of the seven clusters in Hong Kong. Details of the RAMP-DM program have been reported elsewhere [17]. In brief, all people with diabetes under GOPCs care are eligible to be enrolled in the RAMP-DM. The enrolled subjects underwent a series of assessment of risk factors and potential existing diabetic complications when they entered the program, which included measurements of basic parameters (body mass index, waist circumference, blood pressure, etc.), tests of biomedical parameters (HbA1c, full lipid profile, renal function, etc.), and examinations of eyes and feet. Based on the results of these screenings and history of previous complications, RAMP-DM participants were stratified into ‘very high’, ‘high’, ‘medium’ and ‘low’ risk groups according to the JADE classification [14]. For RAMP-DM participants with different risk stratifications, different management strategies were provided by a team of multidisciplinary healthcare professionals, which includes associate consultants in family medicine, GOPCs doctors, advanced practice nurses, registered nurses, and allied health professionals (namely optometrist, dietitian, podiatrist and physiotherapist). Enrolled patients were also eligible to be invited to join the Patient Empowerment Program (PEP), which is a structured education program delivered by two non-governmental organizations to enhance patients’ knowledge and skill on diabetes self-care management. In summary, the interventions for RAMP-DM participants included nurse assessment (including risk stratification), and would be arranged in addition to care from GOPCs doctors, to have nurse intervention, associate consultant intervention, allied-health professional intervention and PEP according to risk levels and need.
Patients under usual care, on the other hand, will be continuously managed solely by GOPCs doctors without risk assessment and stratification. These patients could still be referred to allied health professionals and PEP at their doctors’ discretion.
Subjects
To detect a 5% between group difference in the proportion of achieving the clinical treatment target (HbA1c <7%), with 80% power and 95% confidence interval, 1,248 subjects were needed in each group. A sample of 1,248 RAMP-DM participants (312 from each of the 4 clusters) was randomly selected out of 18,492 subjects, who were enrolled in RAMP-DM between August 2009 and June 2010. A group of 1,248 people with diabetes who attended GOPC but were not enrolled in RAMP-DM during this period were matched by age, sex and HbA1c level as a control group. The baseline dates for RAMP-DM participants are the dates when they received nurse assessment. For usual care group, the baseline date is set as 30 June 2010. The follow-up period for both groups is 12 months since their respective baseline dates.
The ethics approval for this study was granted by the Institutional Review Board of The University of Hong Kong and relevant clusters.
Outcome measures
The primary outcomes of this study were the changes in HbA1c, observed cardiovascular events and predicted 10-year cardiovascular risks over 12 months follow-up. The secondary outcomes were changes in blood pressure, lipid profiles and BMI. We assessed the changes in biomedical outcomes by mean values as well as the proportions of subjects reaching treatment targets in HbA1c (<7%), blood pressure (<130/80 mmHg) and LDL-C (<2.6 mmol/L) recommended by Hong Kong local framework [18]. The 10-year predicted cardiovascular risks were estimated by the Framingham risk function for total cardiovascular disease (CVD) risk [19], and the UKPDS risk engines for coronary heart disease (CHD) [20] and stroke [21], respectively. Demographic data, biomedical outcomes, disease history, drug treatment and RAMP-DM intervention data were extracted from the population-based health and intervention linked database (Clinical Management System) owned by Hospital Authority. To avoid the impact of aging on CVD risks, we applied the age at baseline to calculate the CVD risks at both baseline and 12 months.
Data analysis
We used the mean and standard deviation to describe continuous variables and the categorical variables were summarized by counts and percentages. Paired t-test was employed to compare the paired differences in biomedical measurements and cardiovascular risks between baseline and 12 months for all subjects. The differences in proportions of subjects achieving treatment targets between baseline and 12 months were examined by the McNemar test. We applied the Chi-square test to investigate the between group differences in the incidences of cardiovascular events.
The difference-in-differences approach was used to test the between group differences in the changes of biomedical measurements, cardiovascular risks and target achievement rates. In other words, we calculated the within-group changes over 12 months follow-up for outcomes of interest, and compared the within-group changes between RAMP-DM and control groups by t-test in unadjusted analysis.
To adjust for potential confounders, we constructed three multiple linear regression models to adjust the baseline parameters and drug treatment. Model 1 adjusted the baseline parameters only, model 2 adjusted the baseline parameters and drug treatment at baseline, and model 3 adjusted the baseline parameters, drugs treatment at both baseline and 12 months follow-up.
To further investigate the effects of each component of the RAMP-DM interventions on the changes of biomedical outcomes and cardiovascular risks, we applied multiple linear regressions adjusting for the baseline parameters, and drug treatment among RAMP-DM participants.
We used STATA Version 12.0 (StataCorp LP. College Station, Texas, U.S.) to conduct all the data analyses, and a P-value less than 0.05 was considered as statistically significant.
Results
We excluded 80 control subjects with existing CVD at baseline and 96 control subjects who were enrolled in RAMP-DM over 12 months follow-up. The same number of case–control pairs from RAMP group were excluded as well (including 54 subjects with previous CVD). The baseline characteristics of RAMP-DM group and the usual care group are shown in Table 1.
At baseline (Table 1), the proportions of patients reaching treatment target (HbA1c < 7%) was similar between RAMP-DM group and usual care group (P = 0.079). RAMP-DM participants had significantly higher levels in TC (P < 0.001), LDL-C (P < 0.001) and blood pressure (P < 0.001), resulting in smaller proportions of patients reaching treatment targets in LDL-C (P < 0.001) and blood pressure (P < 0.001). The predicted 10-year total CVD risk by the Framingham risk function, 10-year risks of CHD and stroke by the UKPDS risk engines were similar (P = 0.088, P = 0.177 and P = 0.644, respectively).
Drug treatment and RAMP-DM interventions
Table 2 summarizes the drug treatment and RAMP-DM interventions for included subjects. At baseline, a significantly higher proportion in the usual care group were using insulin (P < 0.001), and this trend continued at 12 months. Among RAMP-DM participants, on average 39.2% and 13.3% subjects received nurse intervention and associate consultant intervention respectively. Patients under usual care were also eligible for PEP and allied health professionals consultation, but the proportions having these interventions were quite small (2.6% and 1.1%, respectively).
Observed cardiovascular events
Table 3 shows the incidences of observed cardiovascular events over 12 months follow-up. A total of 12 (1.21%) and 31 (2.89%) CVD events were observed in RAMP-DM group and control group respectively. Compared to the control subjects, RAMP-DM participants had significantly lower incidences in CHD (−1.49%, P < 0.001) and total CVD (−1.77%, P = 0.003).
Biomedical outcomes
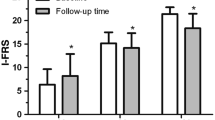
Over 12 months follow-up, RAMP-DM subjects showed significant improvements in the control of HbA1c (−0.11%, P < 0.01), lipid profiles (TC, −0.27 mmol/L, P < 0.01; LDL-C, −0.31 mmol/L, P < 0.01, HDL-C,0.04 mmol/L, P < 0.01; Triglyceride, −0.09, P < 0.05), blood pressure (SBP,-4.20 mmHg, P < 0.01; DBP,-2.53 mmHg, P < 0.01) and BMI (−0.32 kg/m2, P < 0.01) We observed increase in the proportions of reaching the treatment targets in HbA1c (4.11%, P < 0.05), LDL-C (17.52%, P < 0.01) and blood pressure (5.34%, P < 0.01) (Table 4). In the control group, a significant increase in HbA1c was observed compared to baseline (0.10%, P < 0.05). Compared to the control subjects, RAMP-DM participants showed significantly larger improvements in HbA1c (−0.20%, P < 0.01), HDL-C (0.02 mmol/L, P < 0.05) and blood pressure (SBP,-3.62 mmHg, P < 0.01; DBP,-1.73 mmHg, P < 0.01). After adjusting for baseline parameters and drug treatment, the differences in the changes of HbA1c and DBP were still significant (Table 4).
Predicted cardiovascular risks
After 12 months of follow-up, significant decreases in predicted total CVD risks and CHD risks were observed in both RAMP-DM and control groups (Table 4). The control group failed to achieve improvement in stroke risk. The unadjusted difference-in-differences of cardiovascular risks were significant in total CVD risk (−2.06%, P < 0.01), as well as the specific CHD (−1.43%, P < 0.01) and stroke risk (−0.71%, P < 0.05), and these differences remained significant after adjusting for baseline parameters. After adjusting for baseline parameters and drug treatments, the RAMP-DM participants still showed larger reductions in the risks of CHD and stroke predicted by the UKPDS risk engines.
Impact of individual RAMP-DM intervention on biomedical outcomes and predicted CVD risks
After observing improvements in biomedical outcomes and reductions in CVD risks in RAMP-DM participants, multiple linear regression analyses were conducted to further investigate the impact of each component of RAMP-DM interventions on the improvements in clinical outcomes among RAMP-participants. The results are shown in Table 5. After adjusting for baseline parameters, drug treatment at baseline and 12 months, associate consultant intervention was associated with decreases in LDL-C (P < 0.05), triglyceride (P < 0.05) and CHD risk (P < 0.01). PEP was associated with a decrease in BMI, but a paradoxical increase in DBP.
Discussion
To the best of our knowledge, this is the first study to evaluate the effectiveness of a risk-stratification management approach involving multidisciplinary interventions for people with diabetes in the real-world primary care setting. This study found that the RAMP-DM intervention led to lower incidence of cardiovascular events and significant improvements in HbA1c and predicted cardiovascular risks compared to the usual care. Further investigation of the effects of each RAMP-DM intervention component found that, after adjusting for potential confounders, associate consultant intervention was associated with improvements in lipid control and predicted CHD risk, while PEP was related to decreases in BMI.
Compared to the previous study on risk stratification and intervention in staff-model primary care clinics by Clark et al. [12], the magnitude of improvement in HbA1c in our study was smaller. In our study, there was a 0.2% net decrease of HbA1c in RAMP-DM group, while Clark’s study showed about 0.35% between group differences in the changes of HbA1c after 12-month follow-up. Our subjects were much less severe at baseline with an average HbA1c of 7.2%, whereas the mean HbA1c in Clark’s study was above 8.5%. The RAMP-DM is designed to cover all people with diabetes in the primary care in Hong Kong; therefore, we randomly selected subjects to assess the effectiveness of RAMP-DM in general instead of selecting severer cases deliberately. We observed 5.40% more subjects under RAMP-DM reaching treatment target (HbA1c < 7.0%), which addressed the clinical benefits of RAMP-DM.
RAMP group had a greater increase in the proportions of reaching HbA1c < 7%, and SBP/DBP < 130/80 mmHg compared to usual care group, but after adjusting for the baseline parameters and drug treatment, the differences became insignificant, although the results were still favoring RAMP-DM participants. Male sex and no history of myocardial infarction were found to be associated with uncontrolled blood pressure [22]. As all of our study subjects were without cardiovascular complications at baseline and gender was well matched between groups, it was likely that the baseline parameters and drug treatment affected the outcomes. Drug treatment and duration of disease were indicators of diabetes severity. Moe et.al found that compared to people with diabetes and without medication, these on medication subjects had higher risk of cardiovascular death [23]. For severer subjects at baseline, doctors might provide them with more intensive care, no matter they were enrolled in RAMP-DM or not, leading to bigger improvement. Also, regression to the mean might lead to bigger reduction for those with higher baseline HbA1c and SBP levels. In addition, subjects in control group were also eligible to be referred to some of the services in the RAMP-DM intervention package (allied health professionals and PEP) if necessary, which might bias the effects of RAMP-DM towards null.
The RAMP-DM group observed fewer coronary heart disease and total cardiovascular events compared to the control group during 12 months follow-up. This is consistent with the findings of the improvement of HbA1c and predicted cardiovascular risks in RAMP-DM group. A recent study shows that the increase in HbA1c level is significantly associated with the incidence of coronary heart disease during 6 years follow-up [24]. To validate the association in our study, longer follow-up period is needed.
We employed the Framingham cardiovascular risk function developed for primary care [19] to assess the longer term effects in total CVD risk, and applied the UKPDS risk engines [20],[21] to predict the changes in CHD and stroke risks. Although we found that RAMP-DM participants showed significantly greater improvement in the total CVD risk, the differences were not significant after adjusting for drug treatment, while the differences in CHD and stroke risk predicted by the UKPDS risk engines remained significant. Our previous study found that the UKPDS risk engine is more sensitive to detect differences in CHD risk in Chinese people with diabetes [25], as it was developed for people with diabetes specifically. Moreover, the previous study showed that the CHD risk predicted by the UKPDS risk function showed excellent convergent validity with the JADE risk function that was developed in Chinese people with diabetes [25],[26]. We could not use the JADE risk function for the estimation of CVD risk in this study because many required parameters such as estimated glomerular filtration rate and urine albumin:creatinine ratio were missing in many subjects.
Very few studies on DM management measured cardiovascular risk reduction as an outcome. Most studies only reported changes in blood pressure and lipid profiles in addition to HbA1c. Comprehensive cardiovascular risk management is getting increasing attention in diabetes care [5],[27]. The RAMP-DM provided personalized risk-stratification based care to people with diabetes by multidisciplinary health care professionals, which promoted the concept of cardiovascular risk management and facilitated the optimization of medical resources.
The RAMP-DM addressed four interralated components of the Chronic Care Model [10], with multidisciplinary management involving doctors, nurses and allied health professionals. By exploration on individual intervention components among RAMP-DM participants, we found that nurse intervention alone was not associated with any improvements in biomedical outcomes and cardiovascular risks.
Previous trials on nurses led interventions resulted in inconsistent findings in changes of HbA1c. The PEACH study in the Australia primary care setting delivering telephone coaching on medication goals by practice nurses failed to achieve improvement in HbA1c and other relevant biomedical measures [28]. A Spain based standardized language in nursing care plans [29] and a U.S. based nurse care management also showed no improvements in HbA1c [30]. However, a nurse-led telephone coaching intervention in the U.S. found significant reductions in HbA1c [31]. Lacking of prescribing rights is likely to limit the role of nurses in diabetes management, thus affect the benefits of sole nurses intervention [28].
On the other hand, most multidisciplinary interventions involving at least nurses and physicians found favoring results on blood glucose control. A multidisciplinary intervention for patients with HbA1c higher than 10% in Israel found the intervention group had significant decrease in HbA1c after six months. This multidisciplinary team contained diabetologist, the dietician and the diabetes nurse educator [32]. Positive results were also found in similar multidisciplinary interventions in Taiwan [33], the U.S. [34] and France [35]. Most of these multidisciplinary interventions included diabetic education sessions. A symposium convened by American Association of Diabetes Educators acknowledged that the most effective education programs occurred within multidisciplinary teams [36].
The PEP was associated with improvement in BMI, and had favoring effects on HbA1c, lipid profiles and SBP. The small number of subjects enrolled in PEP (7.2%) might be insufficient to detect significant changes. An independent study on the effectiveness of PEP confirmed these favoring results [37]. A RCT was designed to compare the effects of long-term (2 years) education program with initial education only in France. The results are yet to report [38].
There are several limitations of this study. First, since it is not a RCT, some unknown potential confounders might affect the results. However, a study found that the positive effects of interventions in controlled trial settings could not be replicated in real-world primary care settings [39]. Second, the lipid profiles and blood pressure between the RAMP-DM and usual care groups were not well matched at baseline, which might affect the changes over 12 months. Third, the lack of blinding of clinicians and patients is the inherent limitation of population based clinical interventions. Fourth, the Framingham risk function and the UKPDS risk engines were developed in western population, and the UKPDS risk engines were developed in subjects with type 2 diabetes. We had less than 1% subjects with type 1 diabetes, which might affect the accuracy of the predicted CHD and stroke risks. As cardiovascular events need time to develop, the follow-up period of one year was not long enough for us to validate the predicted CVD risk with observed cardiovascular events.
Conclusions
This longitudinal comparative study in a pragmatic primary care setting found that a multidisciplinary risk assessment and management program for people with diabetes (RAMP-DM) significantly reduced HbA1c, observed CVD events and predicted 10-year cardiovascular risks over 12 months follow-up. The encouraging results support the risk stratification and multidisciplinary approach for the management of diabetic patients. A further study focusing on the longer term effects of RAMP-DM in terms of the cardiovascular risk control and the effects of the frequency of interventions will be conducted at three years follow-up.
Abbreviations
- CHD:
-
Coronary heart disease
- CVD:
-
Cardiovascular Disease
- DM:
-
Diabetes mellitus
- GOPC:
-
General Out-Patient Clinics
- GP:
-
General practitioner
- JADE:
-
Joint Asia Diabetes Evaluation Program
- PEP:
-
Patient Empowerment Program
- RAMP-DM:
-
Risk Assessment and Management Program for Patients with Diabetes Mellitus
References
Diabetes atlas, 5rd ed. [http://www.idf.org/diabetesatlas/]
Guariguata L, Whiting D, Hambleton I, Beagley J, Linnenkamp U, Shaw J: Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014, 103 (2): 137-149. 10.1016/j.diabres.2013.11.002.
Kumar P, Clark M: Diabetes mellitus and other disorders of metabolism. Clin Med. 2002, 2: 1069-1071.
Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, Connolly V, King H: The Burden of Mortality Attributable to Diabetes Realistic estimates for the year 2000. Diabetes Care. 2005, 28 (9): 2130-2135. 10.2337/diacare.28.9.2130.
Standards of medical care in diabetes 2013. Diabetes Care. 2013, 36 (Supplement 1): S11-S57. 10.2337/dc13-S011.
Handelsman Y, Mechanick JI, Blonde L, Grunberger G, Bloomgarden ZT, Bray GA, Dagogo-Jack S, Davidson JA, Einhorn D, Ganda O: American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for developing a diabetes mellitus comprehensive care plan. Endocr Pract. 2011, 17: 1-53. 10.4158/EP.17.S2.1.
Type 2 Diabetes National Clinical Guideline for Management in Primary and Secondary Care (Update). Royal College of Physicians. 2008
2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2008, 32 (supplement 1): S1-S201.
Esposito K, Gentile S, Candido R, De Micheli A, Gallo M, Medea G, Ceriello A: Management of hyperglycemia in type 2 diabetes: evidence and uncertainty. Cardiovasc Diabetol. 2013, 12 (1): 81-10.1186/1475-2840-12-81.
Bodenheimer T, Wagner EH, Grumbach K: Improving primary care for patients with chronic illness. JAMA. 2002, 288 (14): 1775-1779. 10.1001/jama.288.14.1775.
Bodenheimer T, Wagner EH, Grumbach K: Improving primary care for patients with chronic illness, The Chronic Care Model, Part 2. JAMA. 2002, 288 (15): 1909-1914. 10.1001/jama.288.15.1909.
Clark CM, Snyder JW, Meek RL, Stutz LM, Parkin CG: A systematic approach to risk stratification and intervention within a managed care environment improves diabetes outcomes and patient satisfaction. Diabetes Care. 2001, 24 (6): 1079-1086. 10.2337/diacare.24.6.1079.
Chan J, So W, Ko G, Tong P, Yang X, Ma R, Kong A, Wong R, Le Coguiec F, Tamesis B: The Joint Asia Diabetes Evaluation (JADE) Program: a web‐based program to translate evidence to clinical practice in Type 2 diabetes. Diabet Med. 2009, 26 (7): 693-699. 10.1111/j.1464-5491.2009.02751.x.
So WY, Raboca J, Sobrepena L, Yoon KH, Deerochanawong C, Ho LT, Himathongkam T, Tong P, Lyubomirsky G, Ko G: Comprehensive risk assessments of diabetic patients from seven Asian countries: the Joint Asia Diabetes Evaluation (JADE) program*. J Diabetes. 2011, 3 (2): 109-118. 10.1111/j.1753-0407.2011.00115.x.
Harris M, Greaves F, Patterson S, Jones J, Pappas Y, Majeed A, Car J: The North West London Integrated Care Pilot: innovative strategies to improve care coordination for older adults and people with diabetes. J Ambul Care Manage. 2012, 35 (3): 216-225. 10.1097/JAC.0b013e31824d15c7.
Greaves F, Pappas Y, Bardsley M, Harris M, Curry N, Holder H, Blunt I, Soljak M, Gunn L, Majeed A: Evaluation of complex integrated care programmes: the approach in North West London.Int J Integr Care 2013, Jan-Mar, URN:NBN:NL:UI:10-1-114283. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3653284/]
Fung CS, Chin WY, Dai DS, Kwok RL, Tsui EL, Wan YF, Wong W, Wong C, Fong DY, Lam CL: Evaluation of the quality of care of a multi-disciplinary risk factor assessment and management programme (RAMP) for diabetic patients. BMC Fam Pract. 2012, 13: 116-10.1186/1471-2296-13-116. [http://www.biomedcentral.com/1471-2296/13/116], [http://www.biomedcentral.com/1471-2296/13/116]
Hong Kong Reference Framework for Diabetes Care for Adults in Primary Care Settings. 2010
D’Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB: General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008, 117 (6): 743-753. 10.1161/CIRCULATIONAHA.107.699579.
Stevens RJ, Kothari V, Adler AI, Stratton IM: The UKPDS risk engine: a model for the risk of coronary heart disease in Type II diabetes (UKPDS 56). Clin Sci (Lond). 2001, 101 (6): 671-679. 10.1042/CS20000335.
Kothari V, Stevens RJ, Adler AI, Stratton IM, Manley SE, Neil HA, Holman RR: UKPDS 60 risk of stroke in type 2 diabetes estimated by the UK Prospective Diabetes Study risk engine. Stroke. 2002, 33 (7): 1776-1781. 10.1161/01.STR.0000020091.07144.C7.
Rückert I-M, Maier W, Mielck A, Schipf S, Völzke H, Kluttig A, Greiser K-H, Berger K, Müller G, Ellert U: Personal attributes that influence the adequate management of hypertension and dyslipidemia in patients with type 2 diabetes. Results from the DIAB-CORE Cooperation. Cardiovasc Diabetol. 2012, 11 (1): 120-10.1186/1475-2840-11-120.
Moe B, Augestad LB, Nilsen TI: Diabetes severity and the role of leisure time physical exercise on cardiovascular mortality: the Nord-Trøndelag Health study (HUNT), Norway. Cardiovasc Diabetol. 2013, 12 (1): 83-10.1186/1475-2840-12-83.
Zhao W, Katzmarzyk PT, Horswell R, Wang Y, Johnson J, Hu G: HbA1c and coronary heart disease risk among diabetic patients. Diabetes Care. 2014, 37 (2): 428-435. 10.2337/dc13-1525.
Jiao FF, Lam CLK, Fung C, McGhee SM: Comparison of four cardiovascular risk prediction functions among Chinese patients with diabetes mellitus in the primary care setting. [http://onlinelibrary.wiley.com/doi/10.1111/jdi.12188/abstract]
Yang X, So W-Y, Kong AP, Ma RC, Ko GT, Ho C-S, Lam CW, Cockram CS, Chan JC, Tong PC: Development and validation of a total coronary heart disease risk score in type 2 diabetes mellitus. Am J Cardiol. 2008, 101 (5): 596-601. 10.1016/j.amjcard.2007.10.019.
New Zealand Primary Care Handbook. In 2012, [http://www.health.govt.nz/publication/new-zealand-primary-care-handbook-2012]
Blackberry ID, Furler JS, Best JD, Chondros P, Vale M, Walker C, Dunning T, Segal L, Dunbar J, Audehm R: Effectiveness of general practice based, practice nurse led telephone coaching on glycaemic control of type 2 diabetes: the Patient Engagement And Coaching for Health (PEACH) pragmatic cluster randomised controlled trial. BMJ. 2013, 347: f5272-10.1136/bmj.f5272. [http://dx.doi.org/10.1136/bmj.f5272], [http://dx.doi.org/10.1136/bmj.f5272]
Cárdenas-Valladolid J, Salinero-Fort MA, Gómez-Campelo P, De Burgos-Lunar C, Abánades-Herranz JC, Arnal-Selfa R, López-Andrés A: Effectiveness of standardized Nursing Care Plans in health outcomes in patients with type 2 Diabetes Mellitus: a two-year prospective follow-up study. PLoS One. 2012, 7 (8): e43870-10.1371/journal.pone.0043870.
Gabbay RA, Lendel I, Saleem TM, Shaeffer G, Adelman AM, Mauger DT, Collins M, Polomano RC: Nurse case management improves blood pressure, emotional distress and diabetes complication screening. Diabetes Res Clin Pract. 2006, 71 (1): 28-35. 10.1016/j.diabres.2005.05.002.
Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL: Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011, 34 (9): 1934-1942. 10.2337/dc11-0366.
Maislos M, Weisman D: Multidisciplinary approach to patients with poorly controlled type 2 diabetes mellitus: a prospective, randomized study. Acta Diabetol. 2004, 41 (2): 44-48. 10.1007/s00592-004-0143-1.
Chen MY, Huang WC, Peng YS, Guo JS, Chen CP, Jong MC, Lin HC: Effectiveness of a health promotion programme for farmers and fishermen with type‐2 diabetes in Taiwan. J Adv Nurs. 2011, 67 (9): 2060-2067. 10.1111/j.1365-2648.2011.05678.x.
Litaker D, MION LC, Planavsky L, Kippes C, Mehta N, Frolkis J: Physician-nurse practitioner teams in chronic disease management: the impact on costs, clinical effectiveness, and patients’ perception of care. J Interprof Care. 2003, 17 (3): 223-237. 10.1080/1356182031000122852.
Mousquès J, Bourgueil Y, Le Fur P, Yilmaz E: Effect of a French experiment of team work between general practitioners and nurses on efficacy and cost of type 2 diabetes patients care. Health Policy. 2010, 98 (2): 131-143. 10.1016/j.healthpol.2010.06.001.
Kent D, D’Eramo Melkus G, Stuart PMW, McKoy JM, Urbanski P, Boren SA, Coke L, Winters JE, Horsley NL, Sherr D: Reducing the risks of diabetes complications through diabetes self-management education and support. Popul Health Manag. 2013, 16 (2): 74-81. 10.1089/pop.2012.0020.
Wong CK, Wong WC, Lam CL, Wan Y, Wong WH, Chung K, Dai D, Tsui EL, Fong DY: Effects of Patient Empowerment Programme (PEP) on clinical outcomes and health service utilization in type 2 diabetes mellitus in primary care: an observational matched cohort study. PLoS One. 2014, 9 (5): e95328-10.1371/journal.pone.0095328.
Debussche X, Collin F, Fianu A, Balcou-Debussche M, Fouet-Rosiers I, Koleck M, Favier F: Structured self-management education maintained over two years in insufficiently controlled type 2 diabetes patients: the ERMIES randomised trial in Reunion Island. Cardiovasc Diabetol. 2012, 11: 91-10.1186/1475-2840-11-91.
Linmans JJ, Viechtbauer W, Koppenaal T, Spigt M, Knottnerus JA: Using electronic medical records analysis to investigate the effectiveness of lifestyle programs in real-world primary care is challenging: a case study in diabetes mellitus. J Clin Epidemiol. 2012, 65 (7): 785-792. 10.1016/j.jclinepi.2012.01.010.
Acknowledgements
This Commissioned Study on Enhanced Primary Care was funded by the Food and Health Bureau, the Government of the Hong Kong Special Administrative Region (EPC-HKU-2). The authors wish to acknowledge the contributions of the RAMP-DM program teams (including Ms. Dorothy Lam, Mr. Jackey Chan) and Statistics and Workforce Planning Department (including Ms. Eva Tsui, Mr. Peggo Lam, Mr. Choi-Fan Yiu) at the Hong Kong Hospital Authority. Also, we would like to thank all hospital authority cluster coordinators and clinical staff in the Chronic Disease Management Programs for working with our team in this evaluation study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
FFJ and CLKL initially conceived the concept of this study and wrote the manuscript. CF, CKHW and YFW were responsible for data collection. FFJ performed the statistical analysis. All the authors made substantial contribution to the interpretation of data and revised the manuscript for important intellectual content. All authors approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Jiao, F.F., Fung, C.S.C., Wong, C.K.H. et al. Effects of the Multidisciplinary Risk Assessment and Management Program for Patients with Diabetes Mellitus (RAMP-DM) on biomedical outcomes, observed cardiovascular events and cardiovascular risks in primary care: a longitudinal comparative study. Cardiovasc Diabetol 13, 127 (2014). https://doi.org/10.1186/s12933-014-0127-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-014-0127-6