Abstract
Background
Physical activity has been associated with lower cardiovascular mortality in people with diabetes, but how diabetes severity influence this association has not been extensively studied.
Methods
We prospectively examined the joint association of diabetes severity, measured as medical treatment status and disease duration, and physical exercise with cardiovascular mortality. A total of 56,170 people were followed up for 24 years through the Norwegian Cause of Death Registry. Cox proportional adjusted hazard ratios (HRs) with 95% confidence intervals (CI) were estimated.
Results
Overall, 7,723 people died from cardiovascular disease during the follow-up. Compared to the reference group of inactive people without diabetes, people with diabetes who reported no medical treatment had a hazard ratio (HR) of 1.65 (95% CI: 1.34, 2.03) if they were inactive and a HR of 0.99 (95% CI: 0.68, 1.45) if they reported ≥2.0 hours physical exercise per week. Among people who received oral hypoglycemic drugs or insulin, the corresponding comparison gave HRs of 2.46 (95% CI: 2.08-2.92) and 1.58 (95% CI: 1.21, 2.05), respectively.
Conclusions
The data suggest a more favourable effect of exercise in people with diabetes who used medication than in those who did not, suggesting that physical exercise should be encouraged as a therapeutic measure additional to medical treatment.
Similar content being viewed by others
Background
Among people with diabetes, the highest risk of death from cardiovascular disease is found in those treated with oral hypoglycemic drugs or insulin [1, 2] and in those with longer duration of diabetes [3–6]. The combination of insulin treatment and longer duration of diabetes has been associated with a particular high risk of death from cardiovascular disease [7]. These findings imply that diabetes treatment and duration are important markers for diabetes severity.
Regular physical activity may improve glycaemic control, insulin sensitivity, and cardiovascular risk factors (e.g., blood pressure, lipid profile, and body composition) in people with diabetes [8–11]. It has been reported that the most physically active people with diabetes have approximately half the risk of death from cardiovascular disease, compared to physically inactive people with diabetes, [12, 13]. In a recent study, people with diabetes who reported a moderate to high level of leisure time physical exercise had the same risk of death from cardiovascular disease as inactive people without diabetes [14]. However, if the beneficial effect of leisure time physical exercise on cardiovascular mortality among people with diabetes is modified by diabetes severity is not known.
The aim of this prospective follow-up study was therefore to assess whether diabetes severity, measured as medical treatment status and disease duration, influence the role of leisure time physical exercise on cardiovascular mortality.
Methods
Subjects
The HUNT Study is a large population-based health survey in Nord-Trøndelag County in Norway. Between 1984 and 1986, all inhabitants aged 20 years or older (85,100) were invited to participate in the first wave of the study (HUNT 1) and a total of 77,216 (90.7%) accepted the invitation, filled in a questionnaire and attended a clinical examination. The participants were given a second questionnaire at the clinical examination to complete at home and return in a pre-stamped envelope. All participants in the HUNT Study gave a written informed consent upon participation and the study was approved by the Regional Committee for Ethics in Medical Research.
For the purpose of the present study, a total of 21,046 participants were excluded at baseline; 4,413 who reported prevalent cardiovascular disease (i.e. angina, myocardial infarction, and/or stroke), 1,003 without sufficient information on diabetes (diagnosis, treatment or duration), 15,227 without information on leisure time physical exercise and 403 without information on potentially confounding factors (i.e. systolic blood pressure, body mass index). After these exclusions, 56,170 participants (27,321 men (mean age= 47.4 years old) and 28,852 women (mean age= 48.5 years old)) were available for follow up on cause of death.
Follow-up
Individual person time at risk of death was calculated from the date of participation in the HUNT 1 study (1984–86) until the date of death or until the end of follow-up 31st December 2008, whichever occurred first. The mandatory reporting of death to the Cause of Death Registry in Norway constitutes the basis for the coding of underlying cause of death. Deaths were classified according to the International Classification of Disease (ICD-9 and ICD-10). Cardiovascular disease was defined by ICD-9: 390–459 and ICD-10: I00-I99, and ischemic heart disease by ICD-9: 410–414 and ICD-10: 120–125.
Study variables
A detailed description of selection procedures, questionnaires, and measurements can be found at http://www.ntnu.edu/hunt and in a report by Holmen and colleagues [15]. Briefly, information was collected on a range of lifestyle and health related factors, including medical history, leisure time physical exercise, smoking status, alcohol consumption and education. Height was measured to the nearest centimetre and weight to the nearest half kilogram, and body mass index (BMI) was calculated as weight (kg) divided by the square value of height (m). Blood pressure was measured two times using a mercury manometer and the mean of the two measures was used.
Diabetes
Participants who answered ‘Yes’ to the question ‘Do you have or have you had diabetes?’ in the first questionnaire, were defined as having diabetes (N=1,105).
The second questionnaire included additional questions to those with known diabetes. People who responded ‘No’ to the questions ‘Do you take tablets for your diabetes?’ and ‘Do you take insulin injections?’ were categorized as people without medication, while people who responded ‘Yes’ to one of the questions were categorized as people with medication. We did not have sufficient power in the statistical analyses to assess the two questions separately. The question ‘When were you first diagnosed with diabetes?’, provided information on diabetes duration.
Leisure time physical exercise
Information on leisure-time physical exercise was obtained from the second questionnaire. The participants were asked ‘How often do you exercise (on the average)?, By exercise we mean going for walks, skiing, swimming and working out/sports’ with five mutually exclusive response options: 0, <1, 1, 2–3, ≥4 times per week. Those who reported exercising once a week or more were also asked ‘for how long do you exercise each time (average)?’, with four mutually exclusive response options: <15, 15–30, 31–60, >60 min. Based on the information of both frequency and duration of exercise we calculated ‘hours of leisure time physical exercise per week’. The frequency response option 2–3 times per week was counted as 2.5 times and ≥4 per week counted as five times, whereas the duration response options <15, 15–30, 31–60, >60 min were counted as 10, 25, 45 and 75 min, respectively. For the purpose of the statistical analysis, we categorized this variable into three groups. This resulted in 22,885 physically inactive participants, 24,140 participants performing 0.1-1.9 hours of leisure time physical exercise per week and 8,040 participants performing ≥2.0 hours of leisure time physical exercise per week.
Statistical analyses
A Cox proportional hazard model was used to estimate adjusted hazard ratios (HRs) of death from cardiovascular disease and ischemic heart disease associated with diabetes treatment (with or without oral hypoglycemic drugs or insulin) and duration, and in a separate analysis, to assess the combined association of leisure time physical exercise and diabetes treatment with risk of death. Precision of the estimated hazard ratios was assessed by a 95% confidence interval (CI). All estimated associations were adjusted for possible confounding by attained age (as the time scale) and birth cohort (five years strata). In multivariable models we adjusted for smoking status (never, former, current, unknown), alcohol consumption (0, 1–4, ≥ 5 times last 14 days, total abstainer, unknown), education (<10 years, 10–12 years, >13 years, unknown), body mass index (kg/m2) and systolic blood pressure (mmHg).
Analyses of the independent association of diabetes treatment were stratified by sex, whereas analyses of the combined association were adjusted for sex in a pooled sample to increase statistical power. The latter was justified by likelihood ratio tests of interaction with sex in the independent analyses of diabetes treatment (P = 0.11) and in the analyses combining diabetes treatment and leisure time physical exercise (P = 0.37).
Additional to the analyses combining leisure time physical exercise and diabetes treatment, we conducted analyses of physical activity stratified by diabetes treatment and tested for possible statistical interaction between the two variables in a likelihood ratio test. Moreover, a likelihood ratio test was used to assess whether the results were modified by age at baseline (< 70 years and ≥ 70 years).
We also conducted three sensitivity analyses; first, people with probable type 1 diabetes (i.e. who were diagnosed with diabetes before 40 years of age and reported insulin injections); second, we excluded the first five years of follow up to evaluate possible bias that could arise if people with the most severe diabetes were unable to be physically active; third, we excluded people who reported a moderate or high degree of movement disability.
Departure from the proportional hazards assumption was evaluated by Schoenfeld residuals and graphical procedures (log-log plots). All statistical tests were two-sided, and all analyses were conducted using Stata for Windows, version 11.2 (StataCorp LP, Texas 77845, USA).
Results
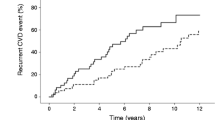
Baseline characteristics of the study population according to diabetes severity are presented in Table 1. During a median follow-up of 23.8 years (1,145,786 person-years), a total of 17,383 people died. Of these, 7,723 people died from cardiovascular disease and 3,518 from ischaemic heart disease. Compared to the 16,633 people who were excluded due to missing data on central variables, the 56,170 included study participants were similar in age (mean age, 49.7 versus 49.1 years), but were less likely to die from cardiovascular disease (age and sex adjusted HR 0.85, 95% CI: 0.81, 0.88). There was no evidence of departure from the proportional hazards assumption for any of the exposure variables under study.
Table 2 presents the independent association between diabetes treatment, measured as medical treatment status and duration, with risk of death from cardiovascular disease and ischemic heart disease. Compared to people without diabetes, the adjusted HR for cardiovascular death was 1.59 (95% CI: 1.29, 1.96) among men with diabetes who received no medical treatment, and 2.16 (95% CI: 1.80, 2.60) for men with diabetes who used medication. These associations were slightly stronger in women, although no statistical significant interaction with sex was observed (P=0.11). The adjusted HR for cardiovascular death was 1.64 (95% CI: 1.34, 2.00) in diabetic women without medication and 2.85 (95% CI: 2.43, 3.34) for those who used medication. Overall, the corresponding analyses of death from ischaemic heart disease gave slightly stronger associations in both men and women.
In a sensitivity analysis we excluded 113 participants (39 men and 74 women) with possible type 1 diabetes, but the results remained largely unchanged. The HRs for people with diabetes who used medication was 2.23 (95% CI: 1.83, 2.71) in men and and 2.82 (95% CI: 2.36, 3.37) in women (data not shown). Moreover, tests of interaction suggest a possible modifying effect of age (Pinteraction = 0.01 in men and 0.03 in women), with a slightly weaker association in the oldest age groups (≥70 years). However, stratified analyses showed that all associations between diabetes treatment status and mortality remained statistically significant in both age groups (data not shown).
The association between diabetes duration and mortality are also presented in Table 2, displaying the HRs after subdividing each of the medical treatment categories into two categories of disease duration. Overall, disease duration was not strongly related to mortality from cardiovascular disease, although the HRs were generally slightly stronger in the subgroup of longer duration (i.e. ≥5 years for persons without medical treatment, and ≥10 years for those with medical treatment). The slightly stronger associations with longer duration were somewhat more evident in the analyses of ischemic heart disease.
There was statistical evidence of interaction between diabetes treatment and hours of leisure time physical exercise per week (P <0.001), suggesting that the favorable effect of physical activity were larger in people with more severe diabetes. Table 3 shows the combined association of diabetes treatment and hours of leisure time physical exercise per week with death from cardiovascular disease and ischemic heart disease, using inactive people without diabetes as the reference group for all comparisons. In people with diabetes who did not use medication, the adjusted HR for cardiovascular death was 1.65 (95% CI: 1.34, 2.03) for inactive people and 0.99 (95% CI: 0.68, 1.45) for those who reported ≥ 2.0 hours of leisure time physical exercise per week. Among people with more severe diabetes (i.e. those who used medication), the adjusted HR for cardiovascular death was 2.46 (95% CI: 2.08, 2.92) in people who were inactive and 1.58 (95% CI: 1.21, 2.05) for those who reported ≥ 2.0 hours of leisure time physical exercise per week. People with diabetes who exercised 0.1-1.9 hours per week had approximately similar HRs as those who were inactive. A similar pattern was observed for death from ischaemic heart disease, although the difference in HRs between inactive people and the most active were somewhat larger.
These combined effects were further explored in analyses of leisure time physical exercise stratified by diabetes status and treatment. Compared to being inactive, ≥2.0 hours of physical activity per week was associated with an adjusted HR of 0.84 (0.89-0.89) in people without diabetes, a HR of 0.79 (95% CI: 0.56, 1.11) in people with diabetes who received no medical treatment, and a HR of 0.49 (95% CI: 0.56, 1.11) in people with diabetes who were medically treated (data not shown).
In sensitivity analyses, we excluded the first five years of follow up, and then also people who reported a moderate or high degree of movement disability. Both analyses gave largely similar results as those presented above (data not shown).
Discussion
In this large population based cohort study, less severe diabetes that was not medically treated was associated with a 60 per cent increased risk of death from cardiovascular disease, whereas more severe diabetes treated with oral agents or insulin was associated with a two-fold increased risk in men and a nearly three-fold higher risk in women. Within each category of treatment status, disease duration was not strongly associated with mortality. Leisure time physical exercise reduced the risk of death from cardiovascular disease in both categories of diabetes severity, but there was evidence of a stronger association in people with more severe diabetes. Corresponding analyses of death from ischaemic heart disease gave slightly stronger associations, although the precision of the estimated associations were lower.
The results of the present study are in agreement with previous prospective studies, showing that people with diabetes treated with oral hypoglycemic drugs or insulin have a higher risk of death from cardiovascular disease than those without medication [1, 2]. Several studies have reported a positive association between diabetes duration and cardiovascular mortality [3–7], but we did not find any strong effect of diabetes duration on cardiovascular mortality when diabetes treatment was taken into account. Although there was no statistically significant interaction between sex and diabetes treatment in the present study, the association between diabetes treatment and cardiovascular mortality was somewhat stronger in women than in men. Previous studies have also reported a stronger association of diabetes with cardiovascular mortality in women than in men [16, 17].
Findings from observational studies suggest that people with diabetes who are physically active have approximately half the relative risk of death from cardiovascular disease compared to inactive people with diabetes [12, 13], although different methods for measuring physical activity make comparisons between studies difficult. The results from the present study suggest a differential effect of physical exercise on cardiovascular mortality by diabetes severity, showing that the favorable effect of exercise was relatively stronger in those who reported medical treatment than in those who did not. The beneficial effect of leisure time physical exercise on cardiovascular mortality in people with diabetes may be explained by the sum of improvements in cardiovascular disease risk factors. These risk factors may be more prevalent in medically treated diabetes. Studies have reported increased cardiovascular mortality associated with hyperglycaemia, hypertension, dyslipidaemia and overweight in people with diabetes [13, 18–20], whereas regular physical exercise has been shown to improve the same risk factors [8–11, 21]. Moreover, a recent review suggests that regular physical exercise could reduce the use of anti-diabetic drugs in people with type 2 diabetes [22].
The strengths of the present study include the population-based sample, the prospective design, the large number of participants, the long follow-up period and the ascertainment of causes of death through the Cause of Death Registry at Statistics Norway.
Limitations of the study include the assessment of diabetes and leisure time physical exercise with a questionnaire at baseline. The self-reported diagnosis of diabetes in HUNT 1 was validated in a separate study [23], showing that 96.4% of the self-reported diabetes could be verified in medical files. Still, unknown diabetes could have underestimated the association between diabetes and cardiovascular mortality. It is also possible that the observed associations between diabetes treatment and cardiovascular mortality could depend on the type of diabetes. We had no information on type 1 or type 2 diabetes, but a sensitivity analysis excluding people who were diagnosed with diabetes before <40 years of age and who reported to use insulin injection suggest no large bias of the results. It should also be noted that diabetes treatment and duration is a rough estimate of diabetes severity. Unfortunately, we did not have information on glycaemic control. Nevertheless, the evidence of a dose-dependent association across diabetes treatment indicates that our classification is able to capture some of the variation in severity among people with diabetes. The physical activity questionnaire used in this study has been validated against more objective measures of fitness and activity, such as VO2max and ActiReg, in a subsample of young men [24]. The questionnaire was reported to have good repeatability and provide a useful measure of leisure time physical exercise. It is possible that the reported exercise volume may be overestimated due to subjective interpretations. However, if the reported exercise volume is overestimated, the presented associations between exercise and mortality is likely to be underestimated. Also, the effects of exercise may be different in young and elderly people. In the present study, only information on frequency and duration was used to classify participants. We acknowledge that exercise intensity could be of importance for cardiovascular health, but analyses stratified according to exercise intensity were not possible due to limited statistical power. Leisure time physical exercise was only measured at baseline, and information on prior changes due to diabetes diagnosis or subsequent changes throughout the follow-up period was not available. Such changes in physical activity could both attenuate and strengthen the estimated association. Also, new cases of diabetes and more people with diabetes receiving medical treatment could result in an underestimated association with mortality. Finally, a substantial proportion of participants were excluded due to missing information on physical exercise and possible selection bias cannot be ruled out.
Conclusions
In conclusion, the results from this prospective cohort study show a positive association between diabetes severity, measured by treatment status, and mortality from cardiovascular disease and ischemic heart disease. Leisure time physical exercise was associated with reduced mortality, and this association was especially strong among people with diabetes who reported medical treatment compared to those who did not. This suggests that physical exercise should be encouraged as a therapeutic measure additional to medical treatment.
References
de Marco R, Locatelli F, Zoppini G, Verlato G, Bonora E, Muggeo M: Cause-specific mortality in type 2 diabetes. The Verona diabetes study. Diabetes Care. 1999, 22: 756-761. 10.2337/diacare.22.5.756.
Bo S, Ciccone G, Gancia R, Rosato R, Grassi G, Merletti F, Pagano GF: Mortality within the first 10 years of the disease in type 2 diabetic patients. Nutrition, metabolism, and cardiovascular diseases: NMCD. 2006, 16: 8-12. 10.1016/j.numecd.2005.01.003.
Cho E, Rimm EB, Stampfer MJ, Willett WC, Hu FB: The impact of diabetes mellitus and prior myocardial infarction on mortality from all causes and from coronary heart disease in men. J Am Coll Cardiol. 2002, 40: 954-960. 10.1016/S0735-1097(02)02044-2.
Hu FB, Stampfer MJ, Solomon CG, Liu S, Willett WC, Speizer FE, Nathan DM, Manson JE: The impact of diabetes mellitus on mortality from all causes and coronary heart disease in women: 20 years of follow-up. Arch Intern Med. 2001, 161: 1717-1723. 10.1001/archinte.161.14.1717.
Spijkerman AM, Dekker JM, Nijpels G, Jager A, Kostense PJ, van Hinsbergh VW, Bouter LM, Heine RJ, Stehouwer CD: Impact of diabetes duration and cardiovascular risk factors on mortality in type 2 diabetes: the hoorn study. Eur J Clin Invest. 2002, 32: 924-930. 10.1046/j.1365-2362.2002.01090.x.
Fox CS, Sullivan L, D'Agostino RB, Wilson PW: The significant effect of diabetes duration on coronary heart disease mortality: the Framingham heart study. Diabetes Care. 2004, 27: 704-708. 10.2337/diacare.27.3.704.
Khalangot M, Tronko M, Kravchenko V, Kulchinska J, Hu G: The joint effects of different types of glucose-lowering treatment and duration of diabetes on total and cardiovascular mortality among subjects with type 2 diabetes. Diabetes Res Clin Pract. 2008, 82: 139-147. 10.1016/j.diabres.2008.07.002.
Sigal RJ, Kenny GP, Boule NG, Wells GA, Prud'homme D, Fortier M, Reid RD, Tulloch H, Coyle D, Phillips P, et al: Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med. 2007, 147: 357-369. 10.7326/0003-4819-147-6-200709180-00005.
Marwick TH, Hordern MD, Miller T, Chyun DA, Bertoni AG, Blumenthal RS, Philippides G, Rocchini A: Exercise training for type 2 diabetes mellitus: impact on cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009, 119: 3244-3262. 10.1161/CIRCULATIONAHA.109.192521.
Thomas DE, Elliott EJ, Naughton GA: Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2006, 3: CD002968
Hayes C, Kriska A: Role of physical activity in diabetes management and prevention. J Am Diet Assoc. 2008, 108: S19-S23.
Tanasescu M, Leitzmann MF, Rimm EB, Hu FB: Physical activity in relation to cardiovascular disease and total mortality among men with type 2 diabetes. Circulation. 2003, 107: 2435-2439. 10.1161/01.CIR.0000066906.11109.1F.
Hu G, Jousilahti P, Barengo NC, Qiao Q, Lakka TA, Tuomilehto J: Physical activity, cardiovascular risk factors, and mortality among finnish adults with diabetes. Diabetes Care. 2005, 28: 799-805. 10.2337/diacare.28.4.799.
Moe B, Eilertsen E, Nilsen TI: The combined effect of leisure-time physical activity and diabetes on cardiovascular mortality: The Nord-Trondelag Health (HUNT) cohort study, Norway. Diabetes Care. 2013, 36: 690-695. 10.2337/dc11-2472.
Holmen JMK, Krüger Ø, Langhammer A, Holmen TL, Bratsberg GH, Vatten L, Lund-Larsen PG: The Nord-Trøndelag health study 1995–97 (HUNT 2): objectives, contents, methods and participation. Nor J Epidemiol. 2003, 13: 19-32.
Dale AC, Nilsen TI, Vatten L, Midthjell K, Wiseth R: Diabetes mellitus and risk of fatal ischaemic heart disease by gender: 18 years follow-up of 74,914 individuals in the HUNT 1 Study. Eur Heart J. 2007, 28: 2924-2929. 10.1093/eurheartj/ehm447.
Huxley R, Barzi F, Woodward M: Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ. 2006, 332: 73-78. 10.1136/bmj.38678.389583.7C.
Dale AC, Midthjell K, Nilsen TI, Wiseth R, Vatten LJ: Glycaemic control in newly diagnosed diabetes patients and mortality from ischaemic heart disease: 20 years follow-up of the HUNT study in Norway. Eur Heart J. 2009, 30: 6.
Uusitupa MI, Niskanen LK, Siitonen O, Voutilainen E, Pyorala K: Ten-year cardiovascular mortality in relation to risk factors and abnormalities in lipoprotein composition in type 2 (non-insulin-dependent) diabetic and non-diabetic subjects. Diabetologia. 1993, 36: 1175-1184. 10.1007/BF00401063.
Khalangot M, Tronko M, Kravchenko V, Kulchinska J, Hu G: Body mass index and the risk of total and cardiovascular mortality among patients with type 2 diabetes: a large prospective study in Ukraine. Heart. 2009, 95: 454-460. 10.1136/hrt.2008.150524.
Boule NG, Haddad E, Kenny GP, Wells GA, Sigal RJ: Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA. 2001, 286: 1218-1227. 10.1001/jama.286.10.1218.
Teixeira-Lemos E, Nunes S, Teixeira F, Reis F: Regular physical exercise training assists in preventing type 2 diabetes development: focus on its antioxidant and anti-inflammatory properties. Cardiovasc Diabetol. 2011, 28: 10-12.
Midthjell K, Holmen J, Bjorndal A, Lund-Larsen G: Is questionnaire information valid in the study of a chronic disease such as diabetes? The Nord-Trondelag diabetes study. J Epidemiol Community Health. 1992, 46: 537-542. 10.1136/jech.46.5.537.
Kurtze N, Rangul V, Hustvedt BE, Flanders WD: Reliability and validity of self-reported physical activity in the Nord-Trondelag Health Study: HUNT 1. Scand J Public Health. 2008, 36: 52-61. 10.1177/1403494807085373.
Acknowledgements
The HUNT Study is a collaboration between the HUNT Research Centre, Faculty of Medicine, Norwegian University of Science and Technology, Verdal, Norway, The National Institute of Public Health, the National Health Screening Service of Norway, and the Nord-Trøndelag County Council.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
No potential conflicts of interest relevant to this article were reported.
Authors’ contributions
BM prepared and analyzed the data, interpreted the results, drafted the manuscript, and contributed to the final version of the manuscript. LBA interpreted the results and contributed to the final version of the manuscript. TILN initiated the study, interpreted the results, and contributed to the final version of the manuscript. TILN is guarantor of this work, and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Moe, B., Augestad, L.B. & Nilsen, T.I. Diabetes severity and the role of leisure time physical exercise on cardiovascular mortality: the Nord-Trøndelag Health study (HUNT), Norway. Cardiovasc Diabetol 12, 83 (2013). https://doi.org/10.1186/1475-2840-12-83
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2840-12-83