Abstract
Background
Polycystic ovary syndrome (PCOS) is the most common endocrinopathy in women. This study was designed to investigate the associations of vitamin D receptor (VDR) gene variants with PCOS risk and the severity of the disease phenotype among Egyptian women.
Methods
In this study, 185 women with PCOS and 207 fertile women as controls were recruited. Cases were divided into phenotype groups based on their clinical and paraclinical features. Clinical and laboratory data were measured in the patient and control groups. All individuals were genotyped for nine single-nucleotide polymorphisms (SNPs) located across the VDR gene using TaqMan allelic discrimination real-time polymerase chain reaction.
Results
Women with PCOS were significantly (P ≤ 0.001) higher body mass index (BMI) (22.77 ± 2.5) than controls (21.68 ± 1.85 kg/m2). Women with PCOS had significantly higher anti-Mullerian hormone, prolactin, luteinizing hormone (LH), LH/follicle-stimulating hormone (FSH), free testosterone, total testosterone, and dehydroepiandrosterone sulfate levels than the control group (P ≤ 0.001). The level of FSH was significantly lower in women with PCOS than in the control group (P ≤ 0.001). Analysis of the VDR rs4516035, rs2107301, rs1544410 (BsmI), and rs731236 (TaqI) SNPs showed a significant association with PCOS phenotype A. Furthermore, rs2228570 (FokI), rs3782905, rs7975232 (ApaI), and rs739837 SNPs showed a significant association with PCOS phenotype C. Furthermore, rs11568820 SNP showed a significant association with PCOS phenotype D (P < 0.05).
Conclusions
The findings of this study indicate that variations in the VDR gene were associated with an increased risk of PCOS in Egyptian women.
Similar content being viewed by others
Introduction
Polycystic ovary syndrome (PCOS) is a prevalent endocrine disorder that affects 6-12% of women of reproductive age worldwide [1]. The syndrome is a complicated and diverse disorder with a variety of clinical symptoms, the most common of which are hyperandrogenism and/or hyperandrogenemia (HA), oligo/anovulation (OA), and polycystic ovary morphology (PCOM) [2, 3]. PCOS women are divided into four phenotypes: phenotype A (HA, OA, and PCOM), phenotype B (HA and OA), phenotype C (HA and PCOM), and phenotype D (OA and PCOM) [4].
A significant potential gene for PCOS is the vitamin D receptor (VDR) gene, also known as the calcitriol receptor or NR1I1 [5]. It is a ligand-activated transcription factor that mediates the genomic effects of vitamin D and controls a number of endocrine and cellular processes, such as bone metabolism and calcium-phosphate homeostasis [6]. Several tissues, including the skeletal, parathyroid, and reproductive systems, express it, and several target genes are modulated to induce a range of biological consequences. The VDR gene has a chromosomal location of 12q12–14 containing a promoter region that is pre-extensive and able to produce many transcripts that are tissue-specific. Research has been done on several VDR polymorphisms to determine their functional importance and possible impacts on disease susceptibility to complicated diseases such as osteoarthritis (OA), diabetes, cancer, high myopia, cardiovascular disease, and tuberculosis [7,8,9,10,11,12]. A few studies have also looked at the role of the VDR gene in endocrine diseases such as PCOS [6, 13, 14].
Approximately, 200 single-nucleotide polymorphisms (SNPs) of the VDR gene were found to be involved [15]. Vitamin D and VDR variations, including Cdx2, Fok1, Apa1, and Taq1, have been linked to the endocrine, metabolic, and genetic components of PCOS, demonstrating their critical functional involvement [6, 14, 16].
This study was designed to examine the association of the nine functionally most relevant VDR SNPs rs11568820 (C/T), rs4516035 (C/T), rs3782905 (C/G), rs2228570 (FokI) (C/T), rs2107301 (C/T), rs1544410 (BsmI) (G/A), rs7975232 (ApaI) (A/C), rs731236 (TaqI) (T/C), and rs739837 (T/G) with PCOS risk and the severity of the disease phenotype among Egyptian women.
Patient and method
Study population
This case-control study included a convenience sample of 392 women (207 healthy controls and 185 cases of PCOS) recruited at the Obstetrics and Gynecology Department, Mansoura University Hospital, Egypt. Laboratory workup was performed at the Molecular Genetic Unit in Endemic Hepatogastroenterology and Infectious Diseases, Faculty of Medicine, Mansoura University, during the period from January 2014 to November 2016.
The subjects were classified according to the Rotterdam consensus (Rotterdam ESHRE/ASRM Sponsored PCOS consensus workshop group, 2004). PCOS was diagnosed according to the Rotterdam criteria [4]. The first group consisting of 207 healthy fertile women without any PCOS features and who have regular menstrual cycles (26–35 days) was enrolled as the control group. The second group comprised 185 women with PCOS, including 88 with phenotype A PCOS (OD + HA + PCOM), 41 with phenotype C PCOS (HA + PCOM), and 56 with phenotype D PCOS (OH + PCOM).
All participants were females of reproductive age who had not been pregnant and had not received hormone treatment for at least three months prior to the study. Age and body mass index (BMI), which is determined by dividing weight (kg) by height2 (m2), were reported to exclude obese women. Follicle-stimulating hormone (FSH), luteinizing hormone (LH), total testosterone (TT), and free testosterone (FT) were detected by chemiluminescence immunization (Beckman Access Health Company, Chaska, MN, USA) with intra- and inter-assay variation coefficients of 10% during the early follicular phase of the cycle. Several recognized causes of androgen excess and ovulatory dysfunction were excluded. Serum cholesterol and triglycerides (TG) were evaluated in the fasting blood samples using precipitation and enzymatic methods.
Genomic DNA extraction from peripheral blood
All individuals had their genomic DNA extracted from peripheral blood using a commercial Qiagen DNA isolation kit (QIAmp DNA Mini kit; Qiagen, Hilden’s, Germany), following the manufacturer’s instructions. A 2% ethidium bromide-stained agarose gel was used to determine the integrity of the DNA using a NanoDrop spectrophotometer (NanoDropTM2000/2000c, Thermo-Fisher Scientific, CA, USA).
Detection of VDR polymorphisms
Nine SNPs located in the entire VDR gene were selected for the current study (Fig. 1). These SNPs include two SNPs namely, 1- rs11568820 (C/T) and 2- rs4516035 (C/T) in the promoter region flanking to transcriptional region. Six SNPs located in the transcriptional region; 3- rs2228570 (FokI) (C/T), 4- rs3782905 (C/G), 5- rs2107301 (C/T), 6- rs1544410 (BsmI) (G/A), 7- rs7975232 (ApaI) (A/C), 8- rs731236 (TaqI) (T/C), and 9- rs739837 (T/G) located in untranslated region (UTR). TaqMan allelic discrimination SNP primers were made. Fluorescent dyes were used to mark the probes that were particular to each allele (VIC and FAM). Probes are used in a real-time PCR reaction on a device (Applied Biosystems, model 7500) to type each DNA sample’s allele. Fluorescein-amidite-labeled SNP primers and probes that are already produced for use in real-time PCR (purchased from Applied Biosystems).
The following 20 µL were used for the reaction: 10.0 µL Universal Master Mix II by TaqMan (2×), 1.0 µL Assay Mix for SNP Genotyping (20×), 1.0 µL template for DNA, and 8.0 µL of RNase free water. A thermal cycler was used to carry out real-time PCR genotyping (Applied Biosystems, 7500 Real-Time PCR system). The subsequent cycles were utilized: the first step in denaturation at 95ºC for 10 min, then the denaturation stage for 40 cycles at 95ºC for 15 s, and the stage of annealing/extension at 60ºC for 1 min. TaqMan plate well fluorescence intensities were measured. Applied Biosystems, Foster City, California, USA’s automated allele-calling software (SDS 2.4) was used to evaluate the fluorescence data files from each plate [17]. To confirm the quality of the study, duplicate genotypes were performed on 10% of all samples. For statistical analysis, SPSS software was used to export all genotyping data.
Statistical analyses
Statistical analysis was performed on the data using the SPSS software program (IBM Corp. Released 2012, Version 21.0. IBM SPSS Statistics for Windows; Armonk, NY, USA). Numbers and percentages were used to convey categorical data The categorical data were compared using the chi-square or Monte Carlo test if required. The Shapiro test was used to determine whether quantitative data were normal. The mean and SD were utilized as variables with a normal distribution. More than two groups were compared using one-way ANOVA with Bonferroni post hoc multiple comparisons. The non-parametric variables were described using the median and interquartile ranges. In contrast to the Mann-Whitney test, which was used to compare just two groups, the Kruskal-Wallis test was used to compare several groups. Each allele’s total genotyping was scored and totaled in each group. Allele carriage is the proportion of people who carry at least one variation of a certain allele. A given allele’s odds ratio (OR) and 95% confidence interval (CI) were computed, compared to the case in which the target allele is not carried, using the program Med Calc (Med Calc statistical software version 16.4.3). Each SNP’s allele carriage variables were compared using chi-square and Fisher’s exact tests. The difference was thought to be significant if P < 0.05.
Results
The clinical characteristics of the PCOS and fertile groups and the PCOS phenotype groups, including PCOS phenotype, age, pre-pregnancy BMI, gravity, parity, and primary and secondary infertility data, are shown in Table 1. Women with PCOS were significantly older (24.09 ± 3.84 years vs. 21.57 ± 3.63 years) and had higher BMI (22.77 ± 2.5 kg/m2 vs. 21.68 ± 1.85 kg/m2) than the control group.
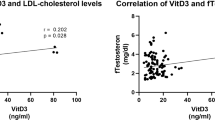
Laboratory data of the fertile and PCOS groups and the PCOS phenotype groups, including anti-Mullerian hormone (AMH), prolactin, LH, FSH, LH/FSH, FT, TT, dehydroepiandrosterone sulfate (DHEA-s), cholesterol, TG, and HbA1c levels, are shown in Table 2. Women with PCOS had significantly higher AMH, prolactin, LH, LH/FSH, FT, TT, and DHEA-s levels than the fertile group (P ≤ 0.001). Furthermore, women with PCOS had significantly higher levels of cholesterol, TG, and HbA1c than the controls (P ≤ 0.001). The level of FSH was significantly lower in women with PCOS than in the controls (P ≤ 0.001).
The different genotypes of PCOS phenotypes and the fertile group of the VDR gene SNPs are shown in Table 3. In this study, two SNPs located in the promoter region, namely, rs11568820 and rs4516035, were genotyped. The minor allele frequencies were 0.15 and 0.16 in the fertile group compared with those (0.47 and 0.28) in the PCOS group, respectively. Furthermore, six SNPs located in the transcriptional region, namely, rs2228570 (FokI), rs3782905, rs2107301, rs1544410 (BsmI), rs7975232 (ApaI), and rs731236 (TaqI), were genotyped. The minor allele frequency of rs2228570 (FokI) initial codon was 0.16 in the fertile group, whereas that in the PCOS groups was 0.28. Meanwhile, the minor allele frequencies of rs3782905 and rs2107301 in introns 3 and 4 were 0.14 and 0.11 in the fertile group, whereas those in the PCOS group were 0.29 and 0.26, respectively.
Furthermore, the minor allele frequencies of rs1544410 (BsmI) and rs7975232 (ApaI) located in intron 9 were 0.15 and 0.21 in the fertile group, whereas those in the PCOS group were 0.30 and 0.32, respectively. Meanwhile, the minor allele frequency of rs731236 (TaqI) located in exon 10 was 0.12 in the fertile group, whereas that in the PCOS group was 0.32. Finally, rs739837 SNP located in the UTR region was genotyped. The minor allele frequency was 0.13 in the fertile group, whereas that in the PCOS group was 0.28. The differences in minor allele carriage of different SNPs were analyzed in the PCOS and PCOS phenotype groups and compared with those in the fertile group using the autosomal dominant model. The total minor allele frequency ranged from 0.18 to 0.30, and the global minor allele frequency ranged from 0.18 to 0.49. The distribution of allele carriages was tested for equilibrium using the Hardy–Weinberg equation. The allele carriages of all SNPs in all groups were balanced (P > 0.05). The allele carriages and frequencies of the sub-phenotypes of PCOS are also shown in Table 3. No significant difference was observed between the allele carriage of primary infertility and that of secondary infertility.
The risk of minor allele carriage of different SNPs was compared in different phenotypes and compared with that in the fertile group using a dominant model, which means that at least one copy of a minor allele is associated with the disease (Table 4). The carriage of the T allele of rs11568820 SNP located in the promoter region had the highest association in the PCOS group compared with that of the control group (OR, 6.93; 95% CI, 4.58–10.48; P < 0.0001) (Fig. 2). The same results were obtained for the PCOS phenotype groups as a highly significant risk association was observed between phenotypes A, C, and D compared with that in the control group (P < 0.0001). The association of the T allele carriage of rs4516035 located in the promoter region was also higher among the PCOS group and phenotypes A and C than that in the control group.
Along the transcriptional region, a significant association of the T allele carriage of rs2228570 (FokI) located in the initial codon was observed among the PCOS group and phenotypes C and D compared with that in the control group. Furthermore, there was a significant association between the G allele carriage of rs3782905, which is located in intron 3, and the T allele carriage of rs2107301, which is located in intron 4, among the PCOS group and all PCOS phenotype groups. In intron 9, there was a significant association of the A allele carriage of rs1544410 (BsmI) among the PCOS group and all PCOS phenotype groups and the C allele carriage of rs7975232 (ApaI) among the PCOS group and phenotypes C and D only. Furthermore, there was a significant association between the C allele carriage of rs731236 (TaqI) located in exon 10 among the PCOS group and all PCOS phenotype groups. Finally, there was a significant association between the G allele carriage of rs739837 located in the UTR region among the PCOS group and all PCOS phenotype groups.
SNP, single-nucleotide polymorphism; PCOS, polycystic ovary syndrome; OR, odds ratio; CI, confidence interval; P, probability < 0.05. The highlighted cells indicate the highest significant risk.
Discussion
A popular genetic approach for examining relationships between candidate genes and dichotomous disease features is the unrelated case-control design. The probed SNP may be in high linkage disequilibrium with a causal variant or the SNP itself may be a common variant that significantly affects the trait if the association is significant. Population stratification within unrelated case-control populations, however, is a potential issue that should be taken into account in studies that integrate data. A family-based case-control design is an alternate strategy to prevent spurious association [18, 19]. However, the availability of a nuclear family with an index case and one fertile case is very difficult. Alternatively, genotyping adjacent markers may help eliminate spurious association in an unrelated case-control study [20]. In this study, nine markers spanning ~ 65.0 kb on the VDR gene, including promoter, exons, introns, and UTR regions, were detected.
Patients with PCOS present with alterations in sex hormone production and cholesterol and TG levels. The results showed a significant association of PCOS with BMI, AMH, prolactin, LH, FSH, FT, TT, and DHEA-s levels. When the hormone levels were compared, the level of LH was significantly higher in the PCOS group than in the control group, whereas FSH levels were significantly lower. However, the LH/FSH ratio was significantly higher in the PCOS group than in the control group. These results agree with those of many studies [21, 22].
PCOS is a multigenic disease with several causes, where several genes interact with one another as well as with environmental conditions, impacting the syndrome’s development and symptoms. Numerous biological systems rely on vitamin D and It uses VDR to moderate its activities. VDR is found in a variety of tissues, including pancreatic beta cells, skin, parathyroid, pituitary gland, or reproductive tissue, participating in the regulation of several endocrines, metabolic or reproductive functions [23]. SNPs in the VDR gene have been linked to key metabolic and endocrine parameters in PCOS, according to genetic association studies [24]. The selected SNPs were (rs11568820, rs4516035, rs2228570 (FokI), rs3782905, rs2107301, rs1544410 (BsmI), rs7975232 (ApaI), rs731236 (TaqI), and rs739837) were examined among women with PCOS and in healthy control, fertile women, the carriage of minor allele frequency of each SNP was tested for their association with the PCOS and its phenotypes compared to that of fertility group. Our interest in this research of PCOS patients arose from the fact that several studies have demonstrated the vital roles that VDR plays in the female reproductive system.
The transcription factor rs11568820 controls the transcription of the VDR gene, mRNA, and protein level [25, 26]. Yamamoto et al. [27] were the first to find an effective binding site in the 1a promoter region of the VDR gene for the intestinal-specific transcription factor rs11568820. the change from C to T, which was investigated in our study, was initially explained by Arai et al. [25] and was discovered to alter the VDR gene’s transcription in the intestine. The A-allele is more precisely bound by the CDX2 protein, which increases the transcription of the VDR gene. It should be noted that the VDR is a transcription factor and controls the transcription of genes important for glucose metabolism and other downstream genes in numerous tissues [26, 28]. Dasgupta et al. concluded that instances of the rs11568820 GA genotype and A allele were substantially more common compared to controls and seemed to provide defense against developing PCOS [29].
Statistics from a prior meta-analysis showed that VDR ApaI (rs7975232) and VDR BsmI (rs1544410) polymorphisms are linked to PCOS susceptibility in the Asian population [30]. Mahmoudi and coworkers [31] found that the ApaI (rs7975232) genotype AA might be used as a marker of reduced vulnerability to PCOS, while the CC genotype was linked to a higher incidence of PCOS. In contrast, Bagheri et al. [32] found no statistically significant correlation between that finding and PCOS risk. Iranian research found a link between the VDR TaqI (rs731236) (CC) genotype and blood LH levels [6]. This discovery was supported by Bagheri and coworkers [5]. Based on ethnic variety, only a few elevated PCOS risks were seen among Asians with the BsmI G/A polymorphism. In addition, TaqI T/C and FokI C/T polymorphisms for PCOS risk did not show any significant association, except for a few sporadic instances of elevated PCOS risk in the first in recessive models. A previous meta-analysis suggested that VDR gene polymorphisms have a role in the development of PCOS, particularly in Asian populations [33]. In the Asian population but not in the Caucasian population, VDR ApaI (rs7975232) and VDR BsmI (rs1544410) SNPs were substantially related with PCOS susceptibility, according to the analysis of subgroups by ethnicity. Genetic differences between the various ethnic groups might be the cause of this finding. Different groups may have some variances in the functional variants as a result of the process of natural selection [30].
In conclusion, this study suggests that VDR gene polymorphisms can be a good candidate for PCOS development among the Egyptian population. Further case-control studies on various ethnic populations with a larger sample size are needed to verify the current conclusions in the future.
Data availability
The datasets used and analyzed during this study are available from the corresponding author upon reasonable request.
References
Skiba MA, Islam RM, Bell RJ, Davis SR. Understanding variation in prevalence estimates of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2018;24(6):694–709.
Ramezani Tehrani F, Behboudi-Gandevani S, Bidhendi Yarandi R, Saei Ghare Naz M, Carmina E. Prevalence of acne vulgaris among women with polycystic ovary syndrome: a systemic review and meta-analysis. Gynecol Endocrinol. 2021;37(5):392–405.
Aversa A, La Vignera S, Rago R, Gambineri A, Nappi RE, Calogero AE, Ferlin A. Fundamental concepts and Novel aspects of polycystic ovarian syndrome: Expert Consensus Resolutions. Front Endocrinol (Lausanne). 2020;11:516.
Revised 2003 consensus. On diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25.
Bagheri M, Abdi Rad I, Hosseini Jazani N, Nanbakhsh F. Vitamin D receptor TaqI gene variant in exon 9 and polycystic ovary syndrome risk. Int J Fertil Steril. 2013;7(2):116–21.
Ranjzad F, Mahban A, Shemirani AI, Mahmoudi T, Vahedi M, Nikzamir A, Zali MR. Influence of gene variants related to calcium homeostasis on biochemical parameters of women with polycystic ovary syndrome. J Assist Reprod Genet. 2011;28(3):225–32.
Uitterlinden AG, Fang Y, van Meurs JB, van Leeuwen H, Pols HA. Vitamin D receptor gene polymorphisms in relation to vitamin D related disease states. J Steroid Biochem Mol Biol 2004, 89–90(1–5):187–193.
Solovieva S, Hirvonen A, Siivola P, Vehmas T, Luoma K, Riihimäki H, Leino-Arjas P. Vitamin D receptor gene polymorphisms and susceptibility of hand osteoarthritis in finnish women. Arthritis Res Ther. 2006;8(1):R20.
Köstner K, Denzer N, Müller CS, Klein R, Tilgen W, Reichrath J. The relevance of vitamin D receptor (VDR) gene polymorphisms for cancer: a review of the literature. Anticancer Res. 2009;29(9):3511–36.
Dilmec F, Uzer E, Akkafa F, Kose E, van Kuilenburg AB. Detection of VDR gene ApaI and TaqI polymorphisms in patients with type 2 diabetes mellitus using PCR-RFLP method in a turkish population. J Diabetes Complications. 2010;24(3):186–91.
Sharma PR, Singh S, Jena M, Mishra G, Prakash R, Das PK, Bamezai RN, Tiwari PK. Coding and non-coding polymorphisms in VDR gene and susceptibility to pulmonary tuberculosis in tribes, castes and Muslims of Central India. Infect Genet Evol. 2011;11(6):1456–61.
Annamaneni S, Bindu CH, Reddy KP, Vishnupriya S. Association of vitamin D receptor gene start codon (Fok1) polymorphism with high myopia. Oman J Ophthalmol. 2011;4(2):57–62.
Mahmoudi T. Genetic variation in the vitamin D receptor and polycystic ovary syndrome risk. Fertil Steril. 2009;92(4):1381–3.
Wehr E, Trummer O, Giuliani A, Gruber HJ, Pieber TR, Obermayer-Pietsch B. Vitamin D-associated polymorphisms are related to insulin resistance and vitamin D deficiency in polycystic ovary syndrome. Eur J Endocrinol. 2011;164(5):741–9.
Fuhrman BJ, Freedman DM, Bhatti P, Doody MM, Fu YP, Chang SC, Linet MS, Sigurdson AJ. Sunlight, polymorphisms of vitamin D-related genes and risk of breast cancer. Anticancer Res. 2013;33(2):543–51.
Zadeh-Vakili A, Ramezani Tehrani F, Daneshpour MS, Zarkesh M, Saadat N, Azizi F. Genetic polymorphism of vitamin D receptor gene affects the phenotype of PCOS. Gene. 2013;515(1):193–6.
Malkki M, Petersdorf EW. Genotyping of single nucleotide polymorphisms by 5’ nuclease allelic discrimination. Methods Mol Biol. 2012;882:173–82.
Spielman RS, McGinnis RE, Ewens WJ. Transmission test for linkage disequilibrium: the insulin gene region and insulin-dependent diabetes mellitus (IDDM). Am J Hum Genet. 1993;52(3):506–16.
Cardon LR, Palmer LJ. Population stratification and spurious allelic association. Lancet. 2003;361(9357):598–604.
Shin J, Lee C. Statistical power for identifying nucleotide markers associated with quantitative traits in genome-wide association analysis using a mixed model. Genomics. 2015;105(1):1–4.
Polson DW, Adams J, Wadsworth J, Franks S. Polycystic ovaries–a common finding in normal women. Lancet. 1988;1(8590):870–2.
Taylor AE, McCourt B, Martin KA, Anderson EJ, Adams JM, Schoenfeld D, Hall JE. Determinants of abnormal gonadotropin secretion in clinically defined women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1997;82(7):2248–56.
Wang Y, Zhu J, DeLuca HF. Where is the vitamin D receptor? Arch Biochem Biophys. 2012;523(1):123–33.
Jain R, von Hurst PR, Stonehouse W, Love DR, Higgins CM, Coad J. Association of vitamin D receptor gene polymorphisms with insulin resistance and response to vitamin D. Metabolism. 2012;61(3):293–301.
Arai H, Miyamoto KI, Yoshida M, Yamamoto H, Taketani Y, Morita K, Kubota M, Yoshida S, Ikeda M, Watabe F, et al. The polymorphism in the caudal-related homeodomain protein Cdx-2 binding element in the human vitamin D receptor gene. J Bone Miner Res. 2001;16(7):1256–64.
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–81.
Yamamoto H, Miyamoto K, Li B, Taketani Y, Kitano M, Inoue Y, Morita K, Pike JW, Takeda E. The caudal-related homeodomain protein Cdx-2 regulates vitamin D receptor gene expression in the small intestine. J Bone Miner Res. 1999;14(2):240–7.
Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J Clin Endocrinol Metab. 2007;92(6):2017–29.
Dasgupta S, Dutta J, Annamaneni S, Kudugunti N, Battini MR. Association of vitamin D receptor gene polymorphisms with polycystic ovary syndrome among indian women. Indian J Med Res. 2015;142(3):276–85.
Shi XY, Huang AP, Xie DW, Yu XL. Association of vitamin D receptor gene variants with polycystic ovary syndrome: a meta-analysis. BMC Med Genet. 2019;20(1):32.
Mahmoudi T, Majidzadeh AK, Farahani H, Mirakhorli M, Dabiri R, Nobakht H, Asadi A. Association of vitamin D receptor gene variants with polycystic ovary syndrome: a case control study. Int J Reprod Biomed. 2015;13(12):793–800.
Bagheri M, Rad IA, Jazani NH, Nanbakhsh F. Lack of Association of vitamin D receptor FokI (rs10735810) (C/T) and BsmI (rs1544410) (A/G) genetic variations with polycystic ovary syndrome risk: a case-control study from iranian azeri turkish women. Maedica (Bucur). 2012;7(4):303–8.
Niu YM, Wang YD, Jiang GB, Bai G, Chai HB, Li XF, Hu YY, Shen M. Association between vitamin D receptor gene polymorphisms and polycystic ovary syndrome risk: a Meta-analysis. Front Physiol. 2018;9:1902.
Acknowledgements
Not applicable.
Funding
The publication fees are covered by a transformative agreement between Springer Nature and Science, Technology, & Innovation Funding Authority (STDF) in cooperation with the Egyptian Knowledge Bank.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
M.N. took responsibility for the study concept and design. A.E. performed the statistical analyses. M.N. and O.A. wrote the first draft of the manuscript. I.A. contributed to clinical diagnosis and examination of the recruited patients. M.N., M.S., O.A., Y. A. S., N. M. A., S. A. M., M. A. and H. E. contributed to laboratory examinations and genotype distribution. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by the Institutional Review Board of the Faculty of Medicine, Mansoura University, Egypt, and all experimental procedures complied with the Declaration of Helsinki. All participants gave written informed consent to take part in the present study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Albahlol, I.A., Neamatallah, M., Serria, M.S. et al. Vitamin D receptor gene polymorphism and polycystic ovary syndrome susceptibility. BMC Med Genomics 16, 108 (2023). https://doi.org/10.1186/s12920-023-01541-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-023-01541-8