Abstract
Background
Despite inconsistent evidence, international guidelines underline the importance of perioperative hyperoxygenation in prevention of postoperative infections. Further, data on safety and efficacy of this method in liver transplant setting are lacking. The aim was to evaluate efficacy and safety of postoperative hyperoxygenation in prophylaxis of infections after liver transplantation.
Methods
In this randomized controlled trial, patients undergoing liver transplantation were randomly assigned to either 28% or 80% fraction of inspired oxygen (FiO2) for 6 postoperative hours. Infections occurring during 30-day post-transplant period were the primary outcome measure. Secondary outcome measures included 90-day mortality, 90-day severe morbidity, 30-day pulmonary complications, durations of hospital and intensive care unit stay, and 5-day postoperative bilirubin concentration, alanine and aspartate transaminase activity, and international normalized ratio (INR) (clinicatrials.gov NCT02857855).
Results
A total of 193 patients were included and randomized to 28% (n = 99) and 80% (n = 94) FiO2. With similar patient, operative, and donor characteristics in both groups, infections occurred in 34.0% (32/94) of patients assigned to 80% FiO2 as compared to 23.2% (23/99) of patients assigned to 28% FiO2 (p = 0.112). Patients randomized to 80% FiO2 more frequently developed severe complications (p = 0.035), stayed longer in the intensive care unit (p = 0.033), and had higher bilirubin concentration over first 5 post-transplant days (p = 0.043). No significant differences were found regarding mortality, duration of hospital stay, pulmonary complications, and 5-day aspartate and alanine transaminase activity and INR.
Conclusions
Postoperative hyperoxygenation should not be used for prophylaxis of infections after liver transplantation due to the lack of efficacy.
Trial registration
ClinicalTrials.gov NCT02857855. Registered 7 July 2016.
Similar content being viewed by others
Background
Infections in patients undergoing surgery remain an important and global public health issue due to their incidence, impact on treatment outcomes, and associated costs [1, 2]. For prevention purposes, the World Health Organization (WHO) created international practice guidelines for perioperative period [3,4,5]. These include provision of 80% fraction of inspired oxygen (FiO2) for 2–6 h postoperatively to all adults. Similar recommendation was made by the Centers for Disease Control and Prevention (CDC) [6].
The rationale behind hyperoxygenation in prevention of infections is based on increased tissue oxygen tension facilitating the process of oxidative killing by neutrophils and thus augmenting immune response [7, 8]. This inexpensive and easy prophylactic measure was first found effective in reducing surgical site infections (SSIs) rate after colorectal procedures, with relative risk reduction exceeding 50% [9]. Subsequent studies, differing in details of oxygen administration and types of surgery, brought inconsistent results [10,11,12,13,14,15]. These were addressed by numerous meta-analyses pointing towards evidence for efficacy in all patients, evidence for efficacy in certain high-risk populations, or no evidence for efficacy [16,17,18,19,20,21]. This, in addition to the potential harms of hyperoxygenation, underlay the common criticism of the WHO and CDC recommendations [22,23,24].
Early postoperative infections are of particular concern in transplantation, due to the necessity of immunosuppression. Nearly half of liver transplantation (LT) recipients develop infections within 6 months after the procedure, with survival being influenced particularly by SSIs and number of infectious episodes [25]. Considering the previously reported benefits of high FiO2 in patients undergoing higher risk colorectal procedures and complete lack of data regarding patients undergoing LT, the latter seem of particular interest in evaluating the effects of perioperative hyperoxygenation. Further, increased formation of reactive oxygen species (ROS) secondary to hyperoxia may not only facilitate elimination of pathogens, but may also exacerbate the process of oxidative stress [26]. In LT, this may translate into higher degree of ischemia-reperfusion injury with potential negative effects on clinical outcomes [27, 28]. The aim of this study was to evaluate the efficacy and safety of providing high FiO2 to LT recipients in the immediate post-transplant period with respect to prevention of postoperative infections and allograft function, respectively.
Methods
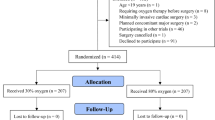
This was a randomized parallel controlled trial. Adult patients undergoing LT were screened for eligibility. Active status on the waiting list was the only inclusion criterion. Exclusion criteria comprised active infection, malignancy, cardiac arrest during transplantation, chronic obstructive pulmonary disease, and acute myocardial infarction. Recruitment took place between July 27, 2016, and March 2020 with follow-up for short-term outcomes completed on June 2020. The study protocol was approved by the institutional review board of the Medical University of Warsaw (KB/158/2016) and registered at ClinicalTrials.gov (NCT02857855) on July 7, 2016. All patients provided informed consent prior to inclusion.
Immediately after transplantation, patients were randomized by physician on duty in the department with a 1:1 allocation ratio, randomly selected blocks of 6, 8, and 10, and stratification by Child-Turcotte-Pugh class, to either 80% or 28% FiO2 for 6 postoperative hours. Random assignment was performed by drawing a sealed envelope with computer-generated code. Patients assigned to 80% FiO2 received 14 L/minute of oxygen and 2 L/minute of air through a non-rebreathing face mask with reservoir. Appropriate Venturi mask was used for patients assigned to 28% FiO2. In case of mechanical ventilation continued in the postoperative period, either 80% or 28% FiO2 was selected. Irrespective of the assignment, FiO2 could be increased in order to ensure arterial oxygen saturation > 92%. Patients and outcome assessors were unaware of the assignment.
The primary outcome measure was the occurrence of infection in the 30-day postoperative period according to CDC definitions [29]. Secondary outcome measures included 90-day postoperative mortality, 90-day severe postoperative morbidity (Clavien-Dindo grade ≥ 3), duration of postoperative hospital and intensive care unit stay, 30-day pulmonary complications, early allograft dysfunction (EAD) according to Olthoff et al., and 5-day serum bilirubin concentration, serum aspartate (AST) and alanine (ALT) transaminase activities, and international normalized ratio (INR) [30, 31]. Additionally, graft function was quantified using model for early allograft function (MEAF) and liver graft assessment following transplantation (L-GrAFT) models [32, 33]. Study on the Efficacy of Nosocomial Infection Control (SENIC) and National Nosocomial Infections Surveillance System (NNISS) risk scores were used to assess the initial SSI risk [34, 35]. This is a pre-planned analysis of the early outcomes (up to 90 days). Data on 5-year survival outcomes and biliary complications are yet to be collected.
The hypothesis was that provision of 80% FiO2 reduces the risk of postoperative infections from 40% to 24% (40% relative risk reduction, basing on Belda et al. study [10]). Sample size calculation based on thresholds for type I and type II errors of 0.05 and 0.20 with anticipated drop-out rate of 10% resulted in 296 patients (148 patients in each group). The study was prematurely terminated with the outbreak of COVID-19 pandemic in March 2020.
All patients received antibiotic prophylaxis, including intravenous piperacillin/tazobactam 4.5 g every 8 h for 3 days after first transplantations and meropenem every 8 h with vancomycin 1.0 g every 12 h adjusted for serum concentration for 7 days after re-transplantations. Antifungal prophylaxis comprised fluconazole 0.4 g every 24 h for 3 and 7 days, respectively. Hair was removed with a clipper immediately before patient transfer to the operating theater. Skin was prepared with povidone-iodine solution. Standard intraoperative FiO2 was 50%. Perioperative warming devices were used to avoid hypothermia. Continuous insulin infusion was applied in all patients for blood glucose control. Plastic adhesive drapes were routinely applied before skin incision. After fascial closure, aqueous povidone-iodine solution was used for wound irrigation. Three closed-suction drains were routinely left in the abdominal cavity and removed when clinically indicated. Skin was either stapled or closed by interrupted sutures. Conventional sterile dressing was changed and the wound examined daily. All patients were operated under laminar airflow. On first postoperative day, a routine abdominal ultrasonography was performed with additional computed tomography performed before discharge. Postoperative fluids included infusion of crystalloids at the standard rate of 1.5 ml/kg/h. All procedures were deceased donor LTs utilizing entire organs procured from donors after brain death.
Analyses were per intention-to-treat principle. Qualitative and quantitative variables were presented as n (%) and median (interquartile range [IQR]) or mean (standard error [SE]), respectively. Fisher’s exact test and Mann-Whitney U test were used for comparisons, as appropriate. Logistic regression was used for calculating odds ratios (ORs) with 95% confidence intervals (95%CIs). Mixed models were applied for longitudinal comparisons. For this purpose, natural logarithms of serum bilirubin concentration and transaminases activity were applied. Kaplan-Meier estimates were applied to estimate proportions of patients remaining in the intensive care unit (ICU) and in the hospital over time with log-rank test used for comparisons. The level of significance was set at two-tailed alpha level of 0.05. SAS/STAT version 15.2 (SAS Institute Inc., USA) was used for processing of statistical analyses.
Results
A total of 193 patients were included and randomized into 80% (n = 94) and 28% (n = 99) FiO2 group (Fig. 1). Both groups were similar regarding baseline recipient, donor, and operative characteristics (Tables 1 and 2). Postoperative tacrolimus trough levels were similar in both groups (see Additional file 1: Fig. S1). No patient was in the ICU prior to transplantation. At the end of intervention, patients assigned to 80% FiO2 had significantly higher median PaO2 (p < 0.001) and oxygen saturation (p < 0.001) with no differences in arterial pH, PaCO2, and lactate concentration as compared to those assigned to 28% FiO2. Postoperative infections occurred in 55 patients (28.5%), including 37 SSIs, 11 urinary tract infections, 9 gastrointestinal infections, 8 pneumonias, 2 bloodstream infections, and 1 vascular access infection. Most frequent SSIs were associated with prolonged ICU and hospital stay, similarly to other infections (see Additional file 2: Fig. S2). Two of patients with SSI developed sepsis (1 died) and further 3 required abscess drainage (1 percutaneous; 2 operative).
A total of 32 (34.0%) patients randomized to 80% FiO2 developed postoperative infections in the 30-day post-transplant period as compared to 23 (23.2%; p = 0.112; Table 3) patients randomized to 28% FiO2. No significant differences were observed between groups regarding the occurrence of particular types of infections. Adjusted for post-intervention oxygen saturation, assignment to 80% FiO2 was significantly associated with increased incidence of infections (p = 0.021). No other significant associations between high postoperative FiO2 and occurrence of infections were found in analyses adjusted for other covariates (see Additional file 3: Table S1). Comparisons of 30-day infection rates between patients assigned to 28% and 80% FiO2 in selected subgroups also revealed no significant differences (see Additional file 4: Table S2). Higher post-intervention oxygen saturation significantly decreased the risk of infections in patients assigned to 28% FiO2 (OR 0.79 per 1%, 95% CI 0.64–0.99; p = 0.040), contrary to those assigned to 80% FiO2 (OR 1.59 per 1%, 95% CI 0.62–4.10; p = 0.339). Arterial partial oxygen pressure was neither associated with infections in the 28% FiO2 group (OR 0.92 per 10 mmHg, 95% CI 0.78–1.08; p = 0.305) nor in 80% FiO2 group (OR 1.01 per 10 mmHg, 95% CI 0.96–1.07; p = 0.640).
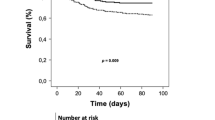
Patients receiving 80% FiO2 more frequently developed severe complications (p = 0.035; Table 3) and had longer ICU stay (p = 0.033). Particular types of severe complications in both groups are listed in Additional file 5, Table S3. The association between assignment to 80% FiO2 and higher morbidity rate was independent of the effects of patient, donor, and operative variables (see Additional file 6, Table S4). In two-factor analysis including FiO2 and post-intervention PaO2, the latter was a significant risk factor for severe morbidity (p = 0.010). No significant differences were found in patient mortality (p > 0.999), EAD rate (p = 0.288), pulmonary complication rate (p = 0.425), and duration of postoperative hospital stay (p = 0.113). Additionally, proportions of patients remaining in the ICU were significantly higher in the 80% FiO2 group (p = 0.009; Fig. 2).
Proportion of patients staying in the hospital and staying in the intensive care unit after liver transplantation depending on the assignment to either 80% or 28% FiO2 for 6 postoperative hours. Red line represents patients assigned to 80% FiO2 and blue line represents patients assigned to 28% FiO2. Colored areas represent 95% confidence intervals
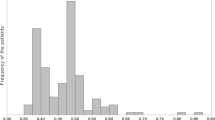
Serum bilirubin concentration during first 5 post-transplant days was significantly higher in patients assigned to 80% FiO2 (p = 0.043; Fig. 3). There were no significant differences in INR (p = 0.866) and serum activity of aspartate (p = 0.192) and alanine aminotransferase (p = 0.157). Patients in high and low FiO2 had median MEAF of 6.34 (IQR: 5.19 to 7.71) and 6.15 (IQR: 4.97 to 7.67), respectively (p = 0.247), and corresponding median L-GrAFT of − 1.39 (IQR: − 2.90 to -0.42) and − 2.34 (IQR: − 2.98 to − 0.83), respectively (p = 0.068).
Mean serum bilirubin concentration (A), serum aspartate (B) and alanine (C) transaminase activity, and international normalized ratio (D) over first 5 days after liver transplantation in patients assigned to 80% (dashed lines) and 28% (solid lines) fraction of inspired oxygen for 6 postoperative hours. Vertical lines represent standard errors of the mean
Of the 99 patients in the low oxygen group, 11 (11.1%) required FiO2 higher than 28% due to low oxygen saturation, 1 underwent re-laparotomy for bleeding after 2 h of intervention, and 1 received simple oxygen mask for organizational reasons. Of the patients requiring higher FiO2, 5 received oxygen concentration ≥ 60%. Of the 94 patients in high oxygen group, 1 required FiO2 ≥ 80%, 2 refused face mask, and 1 underwent re-laparotomy for bleeding after 4 h of intervention. Following exclusion of those patients in per-protocol analysis, infections occurred in 20 of 86 (23.3%) patients assigned to 28% FiO2 and in 30 of 90 (33.3%) patients assigned to 80% FiO2 (p = 0.181). High FiO2 remained significantly associated with severe morbidity with the corresponding rates of 25.6% (22/86) and 43.3% (39/90), respectively (p = 0.017). Proportion of patients remaining in the ICU after 7 and 14 days were 8.1% and 1.2%, respectively, in the 28% FiO2 group as compared to 20.0% and 4.4%, respectively, in the 80% FiO2 group (p = 0.032).
Discussion
The use of high postoperative FiO2 failed to prevent postoperative infections in patients undergoing LT, both in general and with respect to the most common SSIs. Further, the current study did not provide evidence for the benefits of using high FiO2 regarding any other clinical outcomes. Therefore, in contrast to WHO and CDC recommendations, the results of this study do not support hyperoxygenation in the immediate postoperative period in LT recipients [4,5,6].
This findings are in contrast to the results of early randomized trials and the corresponding meta-analyses [9, 10, 37, 38]. Nevertheless, several subsequent studies, including the largest PROXI randomized trial performed on 1400 patients and alternating intervention trial including nearly 6000 patients, did not provide evidence for efficacy of perioperative hyperoxygenation in prophylaxis of postoperative infections [11, 13, 39,40,41]. In the updated meta-analysis, the evidence for the effectiveness of high perioperative FiO2 became weaker and limited to patients undergoing surgery under general anesthesia with endotracheal intubation [16]. The results of this study provide additional data supporting the need for revision of current WHO and CDC guidelines [4,5,6].
Irrespective of the previous studies focused on SSIs, this study provides first data on postoperative hyperoxygenation in LT recipients. Considering the high risk and wide spectrum of postoperative infections in this population, all infections occurring during the 30-day postoperative period were selected as the primary end-point, rather than only SSIs. However, no significant differences between study arms were observed also for particular types of infections, including SSIs, with the actual rates being higher in the 80% FiO2 group. Interestingly, higher oxygen saturation was protective against postoperative infections; however, this effect was limited to patients assigned to 28% FiO2. Further, adjusted for the effect of oxygen saturation in two-factor analysis, assignment to 80% FiO2 significantly increased the risk of infections. This suggests that while adequate oxygen delivery is important, hyperoxygenation does not seem to be an adequate method. In fact, it may cause significant vasoconstriction and paradoxically result in decreased delivery of oxygen to various tissues [42]. Therefore, while it seems that higher oxygen saturation reflecting adequate oxygen content is associated with fewer infections, the use of high FiO2 to further increase oxygen saturation does not provide further benefits.
Hyperoxygenation was reported to aggravate oxidative stress [26, 43, 44]. This seems to be responsible for the observed clinical outcomes, such as increased long-term mortality of cancer patients, shorter cancer-free survival, and increased mortality of acutely ill patients [45,46,47]. In this study, administration of 80% FiO2 was associated with prolonged hyperbilirubinemia, pointing towards the potential negative effect of hyperoxygenation on graft function. However, there were no significant differences in the quantitative measures of graft function, namely MEAF and L-GrAFT, and remaining laboratory measures. Therefore, the clinical relevance of prolonged hyperbilirubinemia associated with hyperoxygenation should be interpreted with caution.
In addition to the lack of effectiveness with respect to prophylaxis of infections, 80% FiO2 was associated with more frequent occurrence of severe complications and lower odds of early ICU discharge. Nevertheless, there were no significant differences in overall duration of hospital stay, potentially due to higher number of factors affecting it. Given similar patient, donor, and operative characteristics in both groups, this indicates that postoperative hyperoxygenation is not only ineffective but also potentially harmful in LT. While direct information on the causative mechanism cannot be drawn from the results, patients randomized to high FiO2 had non-significantly higher rates of EAD and pulmonary complications, non-significantly higher MEAF and L-GrAFT, and non-significantly higher INR and AST and ALT levels. Notably, the results of two-factor analysis of the association between FiO2 and PaO2 and the occurrence of severe complications pointed towards the negative effect of increasing PaO2 with no significant effect of FiO2. Conversely, more detailed comparison revealed that increased severe morbidity rate in the high FiO2 group was largely due to higher number of complications potentially caused by technical reasons, such as hemorrhage, hepatic artery thrombosis, and biliary leaks. Therefore, despite that severe complications were significantly more frequent in patients assigned to 80% FiO2, the current study does not prove the direct causative effect of high FiO2 on severe morbidity.
In this study, high FiO2 was applied for 6 h postoperatively with routine use of 50% intraoperative FiO2. While different duration of hyperoxygenation were used in previous studies, all were based on a combination of intraoperative and postoperative high FiO2. The most common duration of hyperoxygenation in the postoperative period was 2 h, with 6 h being the maximum recommended period. Considering that LT duration greatly exceeds that of the standard abdominal surgeries, hyperoxygenation limited to postoperative period was chosen for safety reasons and to provide uniform timing for all patients. Importantly, despite previous results and available recommendations, intraoperative 50% FiO2 seems to be the current standard [48].
The present study is subject to several limitations. First, the planned sample size was not reached due to study termination at the national outbreak of COVID-19 with the actual power of 66.5% for detection of the hypothesized 40% relative risk reduction from 40% to 24% with 80% FiO2. Nevertheless, the 30-day rate of postoperative infections, the primary outcome measure, was nearly 1.5 fold higher for the 80% FiO2 group. Therefore, type II error secondary to inadequate power does not seem to be a realistic bias. Second, a single-center design may limit generalizability of the findings. Nevertheless, it was associated with homogeneous epidemiological, prophylactic, and organizational approach. There were deviations from the assigned FiO2 in both groups, especially for patients randomized to 28% due to inadequate oxygen saturation. This, however, represents the real-world scenario and the results of per-protocol analyses were consistent with intention-to-treat findings. Further, administration of increased FiO2 to patients assigned to low FiO2 groups due to inadequate oxygen saturation was also common in other studies [9, 40, 41]. Although not all the guidelines regarding prevention of infections were followed (i.e., hair removal, prolonged antibiotic prophylaxis, lack of goal-directed fluid therapy) due to previously established center practices, this was uniform across study cohort.
Conclusions
In conclusion, postoperative hyperoxygenation is ineffective in prevention of infections in LT recipients. Therefore, routine 80% postoperative FiO2 should be avoided in these patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 95%CI:
-
95% confidence interval
- ALT:
-
Alanine transaminase
- ASA:
-
American Society of Anesthesiologists
- AST:
-
Aspartate transaminase
- CDC:
-
Centers for Disease Control and Prevention
- EAD:
-
Early allograft dysfunction
- FFP:
-
Fresh frozen plasma
- FiO2 :
-
Fraction of inspired oxygen
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- ICU:
-
Intensive care unit
- INR:
-
International normalized ratio
- IQR:
-
Interquartile range
- L-GrAFT:
-
Liver graft assessment following transplantation
- LT:
-
Liver transplantation
- MEAF:
-
Model for early allograft function
- MELD:
-
Model for end-stage liver disease
- NNISS:
-
National Nosocomial Infections Surveillance System
- OR:
-
Odds ratio
- PaO2 :
-
Arterial partial oxygen pressure
- PaCO2 :
-
Arterial partial carbon dioxide pressure
- PRBC:
-
Packed red blood cells
- ROS:
-
Reactive oxygen species
- SE:
-
Standard error
- SENIC:
-
Study on the Efficacy of Nosocomial Infection Control
- SSI:
-
Surgical site infection
- WHO:
-
World Health Organization
References
Madrigal J, Sanaiha Y, Karunungan K, et al. National trends in postoperative infections across surgical specialties. Surgery. 2020;168:753–9.
Petrosyan Y, Thavorn K, Maclure M, et al. Long-term health outcomes and health system costs associated with surgical site infections: a retrospective cohort study. Ann Surg. 2021;273:917–23.
Allegranzi B, Bischoff P, de Jonge S, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16:e276–87.
Allegranzi B, Zayed B, Bischoff P, et al. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16:e288–303.
Global guidelines for the prevention of surgical site infection, second edition. Geneva: World Health Organization; 2018.
Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152:784–91.
Hopf HW, Hunt TK, West JM, et al. Wound tissue oxygen tension predicts the risk of wound infection in surgical patients. Arch Surg. 1997;132:997–1004.
Munoz-Price LS, Sands L, Lubarsky DA. Effect of high perioperative oxygen supplementation on surgical site infections. Clin Infect Dis. 2013;57:1465–72.
Greif R, Akça O, Horn EP, et al. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med. 2000;342:161–7.
Belda FJ, Aguilera L, García de la Asunción J, et al. Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA. 2005;294:2035–42.
Meyhoff CS, Wetterslev J, Jorgensen LN, et al. Effect of high perioperative oxygen fraction on surgical site infection and pulmonary complications after abdominal surgery: the PROXI randomized clinical trial. JAMA. 2009;302:1543–50.
Park M, Jung K, Sim WS, et al. Perioperative high inspired oxygen fraction induces atelectasis in patients undergoing abdominal surgery: a randomized controlled trial. J Clin Anesth. 2021;72:110285.
Kurz A, Kopyeva T, Suliman I, et al. Supplemental oxygen and surgical-site infections: an alternating intervention controlled trial. Br J Anaesth. 2018;120:117–26.
Yerra P, Sistla SC, Krishnaraj B, et al. Effect of peri-operative hyperoxygenation on surgical site infection in patients undergoing emergency abdominal surgery: a randomized controlled trial. Surg Infect (Larchmt). 2021;22:1052–8.
Stall A, Paryavi E, Gupta R, et al. Perioperative supplemental oxygen to reduce surgical site infection after open fixation of high-risk fractures: a randomized controlled pilot trial. J Trauma Acute Care Surg. 2013;75:657–63.
de Jonge S, Egger M, Latif A, et al. Effectiveness of 80% vs 30-35% fraction of inspired oxygen in patients undergoing surgery: an updated systematic review and meta-analysis. Br J Anaesth. 2019;122:325–34.
Cohen B, Schacham YN, Ruetzler K, et al. Effect of intraoperative hyperoxia on the incidence of surgical site infections: a meta-analysis. Br J Anaesth. 2018;120:1176–86.
Yang W, Liu Y, Zhang Y, et al. Effect of intra-operative high inspired oxygen fraction on surgical site infection: a meta-analysis of randomized controlled trials. J Hosp Infect. 2016;93:329–38.
Wetterslev J, Meyhoff CS, Jørgensen LN, et al. The effects of high perioperative inspiratory oxygen fraction for adult surgical patients. Cochrane Database Syst Rev. 2015;2015:CD008884.
Smith BK, Roberts RH, Frizelle FA. O2 No Longer the Go2: a systematic review and meta-analysis comparing the effects of giving perioperative oxygen therapy of 30% FiO2 to 80% FiO2 on surgical site infection and mortality. World J Surg. 2020;44:69–77.
Klingel ML, Patel SV. A meta-analysis of the effect of inspired oxygen concentration on the incidence of surgical site infection following cesarean section. Int J Obstet Anesth. 2013;22:104–12.
Hedenstierna G, Perchiazzi G, Meyhoff CS, et al. Who can make sense of the WHO guidelines to prevent surgical site infection? Anesthesiology. 2017;126:771–3.
Myles PS, Kurz A. Supplemental oxygen and surgical site infection: getting to the truth. Br J Anaesth. 2017;119:13–5.
Singer M, Young PJ, Laffey JG, et al. Dangers of hyperoxia. Crit Care. 2021;25:440.
Leibovici-Weissman Y, Anchel N, Nesher E, et al. Early post-liver transplantation infections and their effect on long-term survival. Transpl Infect Dis. 2021;23:e13673.
Oldman AH, Martin DS, Feelisch M, et al. Effects of perioperative oxygen concentration on oxidative stress in adult surgical patients: a systematic review. Br J Anaesth. 2021;126:622–32.
Dar WA, Sullivan E, Bynon JS, et al. Ischaemia reperfusion injury in liver transplantation: cellular and molecular mechanisms. Liver Int. 2019;39:788–801.
Grąt M, Krawczyk M, Wronka KM, et al. Ischemia-reperfusion injury and the risk of hepatocellular carcinoma recurrence after deceased donor liver transplantation. Sci Rep. 2018;8:8935.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Olthoff KM, Kulik L, Samstein B, et al. Validation of a current definition of early allograft dysfunction in liver transplant recipients and analysis of risk factors. Liver Transpl. 2010;16:943–9.
Pareja E, Cortes M, Hervás D, et al. A score model for the continuous grading of early allograft dysfunction severity. Liver Transpl. 2015;21:38–46.
Agopian VG, Harlander-Locke MP, Markovic D, et al. Evaluation of early allograft function using the liver graft assessment following transplantation risk score model. JAMA Surg. 2018;153:436–44.
Haley RW, Culver DH, Morgan WM, et al. Identifying patients at high risk of surgical wound infection. A simple multivariate index of patient susceptibility and wound contamination. Am J Epidemiol. 1985;121:206–15.
Culver DH, Horan TC, Gaynes RP, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med. 1991;91:152S–7S.
Slankamenac K, Graf R, Barkun J, et al. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258:1–7.
Kao LS, Millas SG, Pedroza C, et al. Should perioperative supplemental oxygen be routinely recommended for surgery patients? A Bayesian meta-analysis. Ann Surg. 2012;256:894–901.
Qadan M, Akça O, Mahid SS, et al. Perioperative supplemental oxygen therapy and surgical site infection: a meta-analysis of randomized controlled trials. Arch Surg. 2009;144:359–66.
Wadhwa A, Kabon B, Fleischmann E, et al. Supplemental postoperative oxygen does not reduce surgical site infection and major healing-related complications from bariatric surgery in morbidly obese patients: a randomized, blinded trial. Anesth Analg. 2014;119:357–65.
Kurz A, Fleischmann E, Sessler DI, et al. Effects of supplemental oxygen and dexamethasone on surgical site infection: a factorial randomized trial. Br J Anaesth. 2015;115:434–43.
Thibon P, Borgey F, Boutreux S, et al. Effect of perioperative oxygen supplementation on 30-day surgical site infection rate in abdominal, gynecologic, and breast surgery: the ISO2 randomized controlled trial. Anesthesiology. 2012;117:504–11.
Brugniaux JV, Coombs GB, Barak OF, et al. Highs and lows of hyperoxia: physiological, performance, and clinical aspects. Am J Physiol Regul Integr Comp Physiol. 2018;315:R1–R27.
Habre W, Peták F. Perioperative use of oxygen: variabilities across age. Br J Anaesth. 2014;113:ii26–36.
Ottolenghi S, Rubino FM, Sabbatini G, et al. Oxidative stress markers to investigate the effects of hyperoxia in anesthesia. Int J Mol Sci. 2019;20:5492.
Chu DK, Kim LH, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391:1693–705.
Meyhoff CS, Jorgensen LN, Wetterslev J, et al. Increased long-term mortality after a high perioperative inspiratory oxygen fraction during abdominal surgery: follow-up of a randomized clinical trial. Anesth Analg. 2012;115:849–54.
Meyhoff CS, Jorgensen LN, Wetterslev J, et al. Risk of new or recurrent cancer after a high perioperative inspiratory oxygen fraction during abdominal surgery. Br J Anaesth. 2014;113:i74–81.
Morkane CM, McKenna H, Cumpstey AF, et al. Intraoperative oxygenation in adult patients undergoing surgery (iOPS): a retrospective observational study across 29 UK hospitals. Perioper Med (Lond). 2018;7:17.
Funding
The study was funded by National Science Centre, Poland, grant number 2019/34/E/NZ5/00433. The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
WF—study concept, study design, performing intervention, supervision over other investigators performing intervention, interpretation of the results, literature review, manuscript drafting, approval of the final version. GN—data acquisition, interpretation of the results, literature review, revision of manuscript for important intellectual content, approval of the final version. MG—study concept, study design, preparation of study protocol, acquisition of funding, preparation of case report forms, interpretation of the results, literature review, manuscript drafting, approval of the final version. MK1—study design, interpretation of the results; revision of manuscript for important intellectual content, approval of the final version. JS—data acquisition, follow-up, revision of manuscript for important intellectual content, approval of the final version. ZL—study design, statistical analyses, revision of manuscript for important intellectual content, approval of the final version. MK2—data acquisition, follow-up, revision of manuscript for important intellectual content, approval of the final version. WP—data acquisition, interpretation of the results, revision of manuscript for important intellectual content, approval of the final version. KZ—postoperative follow-up, interpretation of the results, organizational support, revision of manuscript for important intellectual content, approval of the final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the institutional review board of the Medical University of Warsaw (KB/158/2016) and registered at ClinicalTrials.gov (NCT02857855) on July 7, 2016. All patients provided informed consent prior to inclusion.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Mean tacrolimus trough levels over 21 postoperative days in patients after liver transplantation assigned to 28% (solid line) and 80% (dashed line) fraction of inspired oxygen. Vertical lines represent standard errors of the mean.
Additional file 2: Figure S2.
Proportion of patients staying in the hospital (A) and staying in the intensive care unit (ICU) (B) after liver transplantation depending development of surgical site infections (SSIs) and other infections. Colored areas represent 95% confidence intervals.
Additional file 3: Table S1.
Effect of early postoperative fraction of inspired oxygen on infections after liver transplantation adjusted for subsequent covariates of interest in a series of two-factor analyses.
Additional file 4: Table S2.
Subgroup analyses of 30-day infection rates after liver transplantation in patients assigned to 28% and 80% FiO2.
Additional file 5: Table S3.
Severe morbidity in liver transplant recipients assigned to either 28% or 80% fraction of inspired oxygen for 6 postoperative hours.
Additional file 6: Table S4.
Effect of early postoperative fraction of inspired oxygen on severe morbidity after liver transplantation adjusted for subsequent covariates of interest in a series of two-factor analyses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Figiel, W., Niewiński, G., Grąt, M. et al. Postoperative Supplemental Oxygen in Liver Transplantation (PSOLT) does not reduce the rate of infections: results of a randomized controlled trial. BMC Med 21, 51 (2023). https://doi.org/10.1186/s12916-023-02741-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-023-02741-w