Abstract
Background
To maintain adequate oxygenation is of utmost importance in intraoperative care. However, clinical evidence supporting specific oxygen levels in distinct surgical settings is lacking. This study aimed to compare the effects of 30% and 80% oxygen in off-pump coronary artery bypass grafting (OPCAB).
Methods
This multicenter trial was conducted in three tertiary hospitals from August 2019 to August 2021. Patients undergoing OPCAB were cluster-randomized to receive either 30% or 80% oxygen intraoperatively, based on the month when the surgery was performed. The primary endpoint was the length of hospital stay. Intraoperative hemodynamic data were also compared.
Results
A total of 414 patients were cluster-randomized. Length of hospital stay was not different in the 30% oxygen group compared to the 80% oxygen group (median, 7.0 days vs 7.0 days; the sub-distribution hazard ratio, 0.98; 95% confidence interval [CI] 0.83–1.16; P = 0.808). The incidence of postoperative acute kidney injury was significantly higher in the 30% oxygen group than in the 80% oxygen group (30.7% vs 19.4%; odds ratio, 1.94; 95% CI 1.18–3.17; P = 0.036). Intraoperative time-weighted average mixed venous oxygen saturation was significantly higher in the 80% oxygen group (74% vs 64%; P < 0.001). The 80% oxygen group also had a significantly greater intraoperative time-weighted average cerebral regional oxygen saturation than the 30% oxygen group (56% vs 52%; P = 0.002).
Conclusions
In patients undergoing OPCAB, intraoperative administration of 80% oxygen did not decrease the length of hospital stay, compared to 30% oxygen, but may reduce postoperative acute kidney injury. Moreover, compared to 30% oxygen, intraoperative use of 80% oxygen improved oxygen delivery in patients undergoing OPCAB.
Trial registration ClinicalTrials.gov (NCT03945565; April 8, 2019).
Similar content being viewed by others
Introduction
Oxygen delivery (DO2) to peripheral tissue is frequently threatened during surgery due to various factors such as acute blood loss or large fluid shift [1]. Thus, patients undergoing surgery commonly receive a fraction of inspired oxygen (FiO2) higher than that in room air to maintain adequate oxygenation and perfusion [2, 3]. However, this conventional practice may lead to supraphysiological levels of oxygen. The resultant hyperoxia can induce oxidative stress, vasoconstriction, and microcirculatory disturbances [4,5,6,7], which may, in turn, exert unfavorable effects on postoperative outcomes. Moreover, it is generally accepted that above a certain level, manipulating FiO2 has little effect on DO2 [8]. Consequently, using high levels of supplemental oxygen during surgery is controversially discussed [9, 10]. However, evidence regarding the optimal perioperative FiO2 is insufficient and inconsistent [11].
Unlike in patients undergoing on-pump coronary artery bypass grafting, hemodynamic instability is very common in patients undergoing off-pump coronary artery bypass grafting (OPCAB) because the beating heart with considerable coronary artery disease is lifted, rotated, and fixated during surgery [12]. Oxygen therapy using a high FiO2 has certain advantages in terms of oxygenation and perfusion at the potential expense of complications related to oxygen toxicity. However, no previous study has tested the effects of a high FiO2 on clinical outcomes in patients undergoing OPCAB.
The purpose of this study was to assess the effects of intraoperative FiO2 on patients undergoing OPCAB. In this multicenter, cluster-randomized trial, we compared clinical outcomes and hemodynamic parameters between patients who received 80% and 30% oxygen during OPCAB.
Methods
Study design and outline
The CARdiac suRgery and Oxygen Therapy (CARROT) study is a multicenter, cluster-randomized trial conducted in three tertiary hospitals in Seoul, South Korea, from August 2019 to August 2021. This study was approved by the local ethics committees of the three participating hospitals (the Institutional Review Board of Seoul National University Hospital [SNUH], no. 1902-021-1008; the Institutional Review Board of Asan Medical Center [AMC], no. 2019–0818; and the Severance Hospital Institutional Review Board, no. 4-2020-0741), and the protocol was registered at ClinicalTrials.gov (identifier, NCT03945565). All patients enrolled in this study provided written informed consent. The present study was conducted in compliance with the Declaration of Helsinki and adhered to the CONSORT guidelines.
Participants and randomization
Adult patients (aged ≥ 19 years) scheduled for elective OPCAB were included in this study. Exclusion criteria comprised robot-assisted surgery, minimally invasive direct coronary artery bypass grafting, concomitant major surgery, primary pulmonary morbidity requiring oxygen therapy before surgery, mechanical ventilation (MV) prior to surgery, preoperative mechanical circulatory support (e.g., extracorporeal membrane oxygenation, intra-aortic balloon pump), and refusal to participate.
In this study, month-by-month cluster randomization was performed; participants were assigned to receive either 30% or 80% oxygen (the 30% and 80% oxygen groups, respectively) during OPCAB, based on the month in which the surgery was performed. As FiO2 levels have not been universally tested in the field of cardiac surgery and, thus, guidelines did not specify any particular levels of FiO2 [11], we hoped this study to be pragmatic and tried to compare low and high levels of FiO2 that are used in real-world clinical practice. Based on our clinical experience in the three participating hospitals and previous studies including two landmark trials performed in noncardiac surgical patients [13,14,15], we decided on 30% and 80% oxygen as the low and high FiO2 levels, respectively, for this study. Before the beginning of participant enrollment, an independent research nurse in one hospital (SNUH) performed the randomization procedure with a block size of two or four using a computer program (R version 3.4.3; R Foundation for Statistical Computing, Vienna, Austria). The random allocation table was password protected, and the monthly group allocation was communicated to each participating hospital every month. While the attending anesthetists could not be blinded to the group allocation, statisticians who assessed the collected data, as well as patients, surgeons, intensivists, and ward physicians, remained blinded.
Study protocol
In all hospitals, anesthesia was induced with intravenous administration of midazolam and sufentanil or remifentanil and maintained using a target-controlled infusion of propofol and remifentanil. The use of 100% oxygen was allowed during preoxygenation at anesthesia induction. After tracheal intubation, MV was initiated with 30% or 80% oxygen as allocated. If oxygen saturation decreased below 93–94% or arterial oxygen partial pressure (PaO2) below 60–80 mmHg, an alveolar recruitment maneuver was performed, and then a positive end-expiratory pressure of 5–10 cmH2O was applied when necessary. The FiO2 was increased if this safety goal was not achieved despite the rescue therapy or whenever deemed fatal hypoxia by the attending anesthetists. The use of 100% oxygen during transfer to the intensive care unit after the end of surgery was allowed.
Complete coronary revascularization was performed off-pump whenever feasible. Otherwise, routine anesthetic/intraoperative and postoperative care procedures in each participating hospital were not regulated by the protocol of this study, except for the above-mentioned intraoperative FiO2 setting. The routine perioperative management of OPCAB patients in each hospital is briefed in Additional file 1: Table S1.
Primary and exploratory secondary clinical outcomes
The primary clinical outcome was hospital length of stay (LOS) after OPCAB. Evidence has been inconsistent and lacking regarding the effects of the FiO2 level during OPCAB on postoperative outcomes [11]. We expected that changes of FiO2 level may affect various complications differently. For example, if a higher FiO2 may decrease surgical site infection [16], and at the same time, increase lung injury [17], the net effect on the composite complication could be negative. Thus, we decided that measures like the frequency of specific or composite complications may not be appropriate to reflect the clinical effects of different FiO2 levels. Instead, we considered hospital LOS the most appropriate clinical outcome to evaluate the clinical effects of different oxygen fractions.
The exploratory secondary clinical outcomes included length of intensive care unit stay, MV time, prolonged MV, initial postoperative PaO2/FiO2 ratio (one out of three participating hospitals), in-hospital mortality, 30-day mortality, delirium, stroke, sternal wound infection (identified by the National Healthcare Safety Network surveillance definition of the Centers for Disease Control and Prevention; see Additional file 1: Tables S2–4), acute kidney injury (AKI) developed within seven days after surgery (defined based on the serum creatinine criteria of the Kidney Disease: Improving Global Outcomes [18]), newly initiated renal replacement therapy, new-onset atrial fibrillation, type 5 myocardial infarction (diagnosed based on the Fourth Universal Definition of Myocardial Infarction [19]), conversion to on-pump surgery, and revascularization within 30 days after surgery. Definitions of the secondary clinical outcomes are provided in Additional file 1.
Biochemical outcome parameters
Biochemical outcome parameters were the maximum concentrations and areas under the curve of high-sensitivity cardiac troponin T (Severance Hospital), troponin I (SNUH and AMC), and creatine kinase MB (all three participating hospitals) measured within 72 h after surgery, and the first postoperative serum lactate concentration (all three participating hospitals). The postoperative protocols for measurements of these outcome parameters are summarized in Additional file 1: Table S1. In one hospital (SNUH), neutrophil gelatinase-associated lipocalin (NGAL) was also measured at the end of surgery.
Hemodynamic data
Data from intraoperative arterial blood gas analysis and hemodynamic monitoring were gathered as follows. From intraoperative arterial blood gas analysis, hemoglobin concentration, arterial oxygen saturation, and PaO2 were collected. Routine timing of intraoperative arterial blood gas analysis in each participating hospital is presented in Additional file 1: Table S1.
Regarding hemodynamic data, cardiac output (CO) and mixed venous oxygen saturation (SvO2) were measured via a pulmonary artery catheter (Swan-Ganz CCOmbo V 774HF75; Edwards Lifesciences, Irvine, CA, USA) being connected to a monitoring device (Vigilance II™; Edwards Lifesciences). Cerebral regional oxygen saturation was measured by near-infrared spectroscopy (INVOS™ Cerebral/Somatic Oximeter; Medtronic, Minneapolis, MN, USA). Mean arterial blood pressure data, recorded automatically every five minutes, were also collected.
Statistical analysis
We assumed a between-group median difference of 25% in hospital LOS as clinically significant. To detect this difference with a two-sided α error of < 0.05 and a β error of < 0.2 while assuming a drop-out rate due to in-hospital mortality of 2% [20] and an additional withdrawal rate of 5%, 414 participants (207 in each group) were required for this study, resulting in 385 participants discharged alive.
After checking the normality assumption for the baseline summary statistics, continuous data are presented as mean (standard deviation) or median (interquartile range) where appropriate. Categorical data are expressed as number (proportion). Then, the balance between the study groups were evaluated with the generalized estimating equations procedure accounting for intra-cluster correlation [21].
The primary clinical outcome, hospital LOS after OPCAB, was estimated using the cumulative incidence function plot and compared between the groups using the Fine and Gray model to adjust for the month-by-month clustered data and account for competing risk of in-hospital mortality.
For analyses of the exploratory secondary clinical and biochemical outcomes, the generalized estimating equations procedure was used, accounting for intra-cluster correlation [21]. The intraoperative arterial blood gas analysis data and hemodynamic variables were summarized as their time-weighted average values. To obtain reliable time-weighted average values, patients with less than three measurements were omitted. Then, an exploratory analysis was performed to compare the values between the groups using the generalized estimating equations, taking into account intra-cluster correlation. To account for the issue of multiple testing, the false discovery rate method was employed to adjust P values for all exploratory secondary outcomes.
Data were analyzed using SAS (version 9.4; SAS Institute, Cary, NC, USA) or R (version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria). A two-tailed P value < 0.05 was considered statistically significant. The results of all outcome analyses in this study were reported based on the intention-to-treat principle. Per-protocol analyses were performed separately as well.
Results
From August 2019 to August 2021, 566 patients undergoing OPCAB were screened for eligibility (Fig. 1). After excluding 152 patients, 414 patients were cluster-randomized into the 30% or 80% oxygen group (207 participants in each group; an intention-to-treat cohort). The distribution of sample size according to clusters and participating hospitals is shown in Additional file 1: Figure S1. All participants had the primary clinical outcome data available for the planned analysis without loss to follow-up. Baseline characteristics and operative profiles of the participants are provided in Table 1.
Treatment separation was well achieved between the study groups during OPCAB: the mean time-weighted average PaO2 in the 30% and 80% oxygen groups was 124 (33) mmHg and 316 (63) mmHg, respectively. The mean time-weighted average arterial oxygen saturation was 97.5% (1.5) and 99.8% (0.5), respectively. Six patients required the aforementioned rescue therapy (5 out of 207 [2.4%] in the 30% oxygen group and 1 out of 207 [0.5%] in the 80% oxygen group). Sustained hypoxia that did not improve with rescue therapy was not reported in either group. Intraoperative mechanical ventilatory profiles are shown in Additional file 1: Table S5. Nine patients underwent on-pump conversion; the remaining 405 patients were analyzed as a per-protocol cohort.
Primary and exploratory secondary clinical outcomes
The median (95% confidence interval [CI]) hospital LOS after OPCAB was 7.0 (6.5–7.5) days for the 30% oxygen group and 7.0 (6.6–7.4) days for the 80% oxygen group. There was no significant difference in hospital LOS between the two groups, in both intention-to-treat (the sub-distribution hazard ratio, 0.98; 95% CI 0.83–1.16; P = 0.808) and per-protocol analyses (the sub-distribution hazard ratio, 0.95, 95% CI 0.78–1.16, P = 0.644; Fig. 2). Data on readmission after discharge from the index hospitalization are summarized in Additional file 1: Table S6.
There was no significant difference in the exploratory secondary clinical outcomes between both groups, except for AKI (Table 2 and Fig. 3). After excluding 34 patients with preoperative end-stage renal disease or renal replacement therapy, 25.0% (95/380) of the overall intention-to-treat cohort developed AKI after OPCAB. The incidence of AKI was significantly greater in the 30% oxygen group (58/189; 30.7%) than in the 80% oxygen group (37/191; 19.4%; odds ratio, 1.94; 95% CI 1.18–3.17; adjusted P = 0.036). Only one patient in the 80% oxygen group required postoperative renal replacement therapy. Two patients in the 30% oxygen group died in hospital because of aspiration, and no additional mortality was reported within 30 days after surgery. There were two cases (one case in each group) of postoperative stroke. Similar results were found in per-protocol analyses (see Additional file 1: Table S7 and Figure S2).
Intention-to-treat analysis of the binary secondary clinical outcomes. CI, confidence interval; MV, mechanical ventilation. a18 and 16 patients with preoperative end-stage renal disease or renal replacement therapy in the 30% and 80% oxygen groups, respectively, were excluded. b7 and 10 patients with a preoperative history of atrial fibrillation in the 30% and 80% oxygen groups, respectively, were excluded. cMissing data in 47 and 31 patients in the 30% and 80% oxygen groups, respectively
Biochemical outcomes
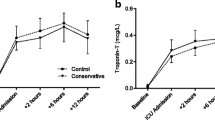
In one participating hospital (Severance Hospital, n = 68), serum cardiac troponin T levels were measured. The maximum values and areas under the curve of troponin T levels within 72 h after surgery were significantly higher in the 30% oxygen group than in the 80% oxygen group. In the other two hospitals (SNUH and AMC, n = 346), serum cardiac troponin I levels were measured, but the two groups were not significantly different. Likewise, no difference was found in creatine kinase MB levels among the two study groups (all three participating hospitals, n = 414; Table 3).
While the first postoperative serum lactate concentration was also comparable between the two groups (all three participating hospitals, n = 414; Table 3 and Additional file 1: Figure S3), serum NGAL concentrations measured at the end of surgery (SNUH, n = 197) tended to be higher in the 30% oxygen group than in the 80% oxygen group (133 [205] ng/ml vs 91 [91] ng/ml, respectively; adjusted P = 0.102).
The per-protocol analysis of these biomarkers showed similar results (see Additional file 1: Table S8).
Hemodynamic data
While time-weighted average intraoperative hemoglobin concentration and CO were similar for both groups, arterial oxygen saturation (97.9% [1.5] vs 99.8% [0.5]; adjusted P = 0.001) and PaO2 (124 [33] mmHg vs 316 [63] mmHg; adjusted P = 0.001; Table 4) were significantly lower in the 30% oxygen group than in the 80% oxygen group. There was a statistically significant but minimal difference in mean intraoperative arterial blood pressure between the 30% and 80% oxygen groups (74 [6] mmHg vs 76 [6] mmHg; adjusted P = 0.024; Table 4). The 30% oxygen group had a 10-percentage point lower time-weighted average SvO2 (63.9% [9.7]) than the 80% oxygen group (73.9% [7.3]; adjusted P = 0.001) during surgery. The 30% oxygen group also had a lower increased intraoperative cerebral regional oxygen saturation (51.7% [14.5]) compared to the 80% oxygen group (56.4% [16.1]; adjusted P = 0.001). The per-protocol analyses are summarized in Additional file 1: Table S9.
Discussion
In our study, there was no difference in hospital LOS after OPCAB between the 30% and 80% oxygen groups. However, compared to the 30% oxygen group, there was nearly a 40% reduction of the postoperative AKI incidence in the 80% oxygen group, with a lower level of serum NGAL. In addition, SvO2 and cerebral regional oxygen saturation were also significantly higher in the 80% oxygen group.
Previous studies on the effects of supplemental oxygen have been largely performed in critically ill patients [22, 23]. Although some landmark trials in patients undergoing surgery have been published [13, 14], in contrast to that in critically ill patients, the evidence on the topic is relatively insufficient and does not reflect different surgical settings [24]. Moreover, most prior studies in cardiac surgical patients enrolled only a small number of patients with cardiopulmonary bypass and had markedly heterogeneous study designs (e.g., varying FiO2 or PaO2 targets used) and primary outcomes [11]. The most recent randomized trial was performed in 330 patients undergoing cardiopulmonary bypass and failed to find any difference in clinical outcomes between the standard management (varying FiO2 to achieve PaO2 < 150 mmHg during cardiopulmonary bypass) and the intervention (FiO2 of 1.0) [25]. Consequently, there is no consensus regarding adequate oxygen therapy in cardiac surgical patients, particularly in those undergoing off-pump cardiac surgery, and thus real-world clinical practice has varied [26]. One of the main reasons for this complexity is that clinical advantages and disadvantages of a specific oxygen level can vary from organ to organ. The present CARROT trial is the first randomized clinical trial performed in patients undergoing off-pump cardiac surgery on this topic. Although no difference was found in the primary clinical endpoint, we showed that the use of 80% oxygen compared to 30% oxygen reduced postoperative AKI and improved hemodynamics without any disadvantage.
Although some cohort studies showed that increased oxygen exposure was associated with a higher risk of acute kidney injury after major surgery [27], there has been no conclusive evidence that supplemental oxygen alters renal outcome after cardiac surgery [28]. In our study, although exploratory in nature, postoperative AKI was considerably reduced in the 80% oxygen group compared to the 30% oxygen group, and this result was consistent with a lower mean serum NGAL level at the end of surgery in the 80% oxygen group (91 ng/ml vs 133 ng/ml). Furthermore, well-established risk factors for AKI, such as hemoglobin concentration (anemia) and arterial blood pressure [29, 30], were nearly identical between the two groups (see Table 4). We infer an increased DO2 as a possible mechanism underlying the beneficial effect of a higher FiO2 on postoperative AKI. In our previous substudy of this CARROT trial, we already showed that a significantly higher DO2 can be achieved by using 80% oxygen compared with 30% oxygen in OPCAB patients [31]. Likewise, in the present study, SvO2, an index of the balance between DO2 and oxygen consumption, was also higher in the 80% oxygen group, while CO and hemoglobin concentration were similar between the two groups (see Table 5). The depth of anesthetics may be an important factor that influences critical DO2 and changes the intra-organ pressure-flow relationship [32]. In our study, however, the mean time-weighted average bispectral index was nearly identical among the two groups (42.3 [4.6] and 43.2 [4.5] in the 30% and 80% oxygen groups, respectively; data not shown in the Results). Then, could the DO2 difference observed in this study reach a threshold where the incidence of postoperative AKI increases? Peritubular capillaries of the kidney are supplied by efferent glomerular arteries that carry poorly oxygenated blood [33], which is particularly prominent in the renal medulla [34]. Indeed, oxygen tension in the renal medulla is among the lowest in the body [35, 36]. Thus, it is not surprising that the kidney is vulnerable to the reduction in DO2, and conversely, increasing DO2 may ameliorate renal ischemic injury [37]. In our exploratory calculation, the mean (standard deviation) intraoperative time-weighted average indexed DO2 was 305 (63) and 289 (59) ml/min/m2 in the 80% and 30% oxygen groups, respectively. Considering that a cut-off for indexed DO2 value known to predict AKI was at approximately 270 ml/min/m2 [38, 39], more patients in the 30% oxygen group might have failed to achieve this cut-off value. As expected, in the present study, patients who developed AKI showed a lower indexed DO2 than those who did not (279 [52] ml/min/m2 vs 303 [60] ml/min/m2). The authors looked further into the data, stratifying patients by whether intraoperative time-weighted average indexed DO2 was lower than 270 ml/min/m2 (see Additional file 1: Figure S4). Interestingly, there was little difference in the incidence of postoperative AKI between the 30% and 80% oxygen groups (16.5% vs 16.8%) within the ‘high DO2’ stratum. The difference in time-weighted average CO was trivial (4.0 l/min vs 3.9 l/min). On the other hand, within the ‘low DO2’ stratum, the incidence of AKI in the 30% and 80% oxygen groups was 34.6% and 20.9%, respectively, while the time-weighted average CO was 3.1 l/min and 3.0 l/min. First, the difference in DO2 between the DO2 strata appeared to be mainly due to the difference in CO. We infer that patients with relatively high CO did not benefit from 80% oxygen because DO2 was already sufficient, whereas those with lower CO did. Taken together, it may be helpful to raise DO2 by increasing FiO2 in patients with low CO for the prevention of postoperative AKI. Based on these findings and hypothesis, the authors expect that the effects of a high FiO2 may be advantageous in specific hemodynamic environments such as OPCAB where low CO and hypotension are frequent [12], although it may not be applicable in other various surgical settings.
In general, lung injury from a high FiO2 has been acknowledged in critically ill patients [17, 40]. A prior randomized controlled trial demonstrated that targeting a higher PaO2 significantly increased mortality in critically ill patients [17]. However, a recent study found no difference in ventilator-free days between patients where a lower, intermediate, or higher oxygen saturation target was used [41]. Similarly, there have been inconsistent results in surgical patients [42]. In a previous large observational study, high intraoperative FiO2 was associated with a composite of postoperative respiratory complications (reintubation, respiratory failure, pulmonary edema, and pneumonia) in a dose-dependent manner [43]. However, a meta-analysis showed a nonsignificant association of a high intraoperative FiO2 with respiratory insufficiency after surgery [42]. In the SO-COOL trial by McGuinness et al., MV time after cardiac surgery involving cardiopulmonary bypass was comparable between the usual care and the avoidance of hyperoxemia groups [44]. In our study, we found no significant difference in MV time, incidence of prolonged MV, and initial PaO2/FiO2 ratio after OPCAB between the 30% and 80% oxygen groups. Interestingly, MV time was shorter and the incidence of prolonged MV was lower in the 80% oxygen group (see Fig. 3).
Since the World Health Organization recommended using 80% oxygen to reduce surgical site infection, the effect of perioperative FiO2 on surgical site infection has been one of the most contentious issues [45]. Despite debates and criticism [46,47,48], the World Health Organization still recommends using 80% oxygen for the prevention of surgical site infection in the updated guideline [16]. However, a recent large trial and a meta-analysis reported no or little effect of hyperoxia on surgical site infection [49, 50], and so far, evidence supporting the use of 80% oxygen to prevent surgical site infection was largely from colorectal surgery cohorts. In our study, sternal wound infection was less frequent in the 80% oxygen group than in the 30% oxygen group (see Fig. 3), although it was statistically nonsignificant. However, conclusive interpretation was not possible due to a low event rate and a different study population in our study.
There have been concerns about hyperoxia-related myocardial injury after noncardiac surgery (MINS) [51], and even myocardial infarction [52]. In the present study, there was no significant difference between the 80% and 30% oxygen groups in terms of postoperative serum troponin I and creatine kinase MB concentrations and type 5 myocardial infarction, while serum troponin T concentration measured in one participating center was rather lower in the 80% oxygen group than in the 30% oxygen group (see Table 3). In fact, previous studies also showed inconsistent results about the relationship between perioperative FiO2 and myocardial injury [28, 51, 53]. Two recent prospective controlled trials reported a nonsignificant difference in the risk for MINS between 80 and 30% oxygen [28, 53]. On the contrary, the most recent international observational study showed that an intraoperative FiO2 increment of 0.1 was associated with an increase in odds for MINS (odds ratio, 1.17; 95% CI 1.12–1.23) [51]. Further studies are required to conclude this issue, but in our study, evidence of increased myocardial injury was not observed in the 80% oxygen group compared to 30% oxygen group.
We recognize several limitations of this study. First, intraoperative FiO2 levels were randomized in this study instead of specific PaO2 targets. Even at the same FiO2, arterial blood oxygenation may vary substantially depending on the individual lung condition. Although PaO2 was not measured at prespecified time points during surgery, it is very likely that treatment separation was well achieved considering the mean difference in time-weighted average PaO2 among the two groups (124 mmHg vs 316 mmHg; see Table 4). Moreover, we expected that interventions based on FiO2 rather than PaO2 targets could be more pragmatic during clinical practice. Second, although the primary endpoint of this study was the hospital LOS, criteria for hospital discharge were not protocolized. This may have contributed to the failure to detect the difference in hospital LOS between the study groups. However, we expected that this aspect made the present study pragmatic and better reflect the real-world clinical situation. Third, the exploratory secondary clinical outcomes including postoperative AKI were not prespecified in a clinical trial registry, thereby having an exploratory nature despite the significant difference in the incidence of AKI. Fourth, we regulated intraoperative FiO2 level in the study protocol, but not postoperative supplemental oxygen therapy. Considering the importance of postoperative management, the benefits from high FiO2 might have been more evident, or even an opposite conclusion could have been reached, had the postoperative FiO2 level been also regulated. Further studies are warranted for this topic.
In conclusion, intraoperative administration of 80% oxygen or 30% oxygen did not affect hospital LOS after OPCAB. However, 80% oxygen during OPCAB may decrease the incidence of postoperative AKI and serum NGAL concentration. Furthermore, global oxygen supply and cerebral regional oxygen saturation were also superior in the 80% oxygen group to the 30% oxygen group. Although it failed to reduce hospital LOS, an intraoperative FiO2 of 0.8 provided tissue oxygenation with superior hemodynamics without any worse outcome related to hyperoxia.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding authors on reasonable request.
References
Spoelstra-de Man AM, Smit B, Oudemans-van Straaten HM, Smulders YM. Cardiovascular effects of hyperoxia during and after cardiac surgery. Anaesthesia. 2015;70:1307–19. https://doi.org/10.1111/anae.13218.
Harten JM, Anderson KJ, Kinsella J, Higgins MJ. Normobaric hyperoxia reduces cardiac index in patients after coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 2005;19:173–5. https://doi.org/10.1053/j.jvca.2004.11.053.
Martin DS, Grocott MP. Oxygen therapy and anaesthesia: Too much of a good thing? Anaesthesia. 2015;70:522–7. https://doi.org/10.1111/anae.13081.
Cornet AD, Kooter AJ, Peters MJ, Smulders YM. The potential harm of oxygen therapy in medical emergencies. Crit Care. 2013;17:313. https://doi.org/10.1186/cc12554.
Inoue T, Ku K, Kaneda T, Zang Z, Otaki M, Oku H. Cardioprotective effects of lowering oxygen tension after aortic unclamping on cardiopulmonary bypass during coronary artery bypass grafting. Circ J. 2002;66:718–22. https://doi.org/10.1253/circj.66.718.
Paparella D, Guida P, Caparrotti S, Fanelli V, Martinelli G, Mazzei V, et al. Myocardial damage influences short- and mid-term survival after valve surgery: a prospective multicenter study. J Thorac Cardiovasc Surg. 2014;148:2373-2379.e1. https://doi.org/10.1016/j.jtcvs.2013.10.061.
Sjöberg F, Singer M. The medical use of oxygen: a time for critical reappraisal. J Intern Med. 2013;274:505–28. https://doi.org/10.1111/joim.12139.
Shepherd SJ, Pearse RM. Role of central and mixed venous oxygen saturation measurement in perioperative care. Anesthesiology. 2009;111:649–56. https://doi.org/10.1097/ALN.0b013e3181af59aa.
Heinrichs J, Grocott HP. Pro: hyperoxia should be used during cardiac surgery. J Cardiothorac Vasc Anesth. 2019;33:2070–4. https://doi.org/10.1053/j.jvca.2018.02.015.
Roberts SM, Cios TJ. Con: hyperoxia should not be used routinely in the management of cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2019;33:2075–8. https://doi.org/10.1053/j.jvca.2019.02.027.
Heinrichs J, Lodewyks C, Neilson C, Abou-Setta A, Grocott HP. The impact of hyperoxia on outcomes after cardiac surgery: a systematic review and narrative synthesis. Can J Anaesth. 2018;65:923–35. https://doi.org/10.1007/s12630-018-1143-x.
Verma S, Fedak PW, Weisel RD, Szmitko PE, Badiwala MV, Bonneau D, et al. Off-pump coronary artery bypass surgery: fundamentals for the clinical cardiologist. Circulation. 2004;109:1206–11. https://doi.org/10.1161/01.CIR.0000120292.65143.F5.
Greif R, Akça O, Horn EP, Kurz A, Sessler DI, Outcomes Research Group. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med. 2000;342:161–7. https://doi.org/10.1056/NEJM200001203420303.
Meyhoff CS, Wetterslev J, Jorgensen LN, Henneberg SW, Høgdall C, Lundvall L, et al. Effect of high perioperative oxygen fraction on surgical site infection and pulmonary complications after abdominal surgery: the PROXI randomized clinical trial. JAMA. 2009;302:1543–50. https://doi.org/10.1001/jama.2009.1452.
Meyhoff CS. Perioperative hyperoxia: why guidelines, research and clinical practice collide. Br J Anaesth. 2019;122:289–91. https://doi.org/10.1016/j.bja.2018.12.016.
WHO. Global guidelines for the prevention of surgical site infection. In: Global guidelines for the prevention of surgical site infection. 2nd ed. Geneva; 2018.
Girardis M, Busani S, Damiani E, Donati A, Rinaldi L, Marudi A, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an Intensive Care Unit: the oxygen-ICU randomized clinical trial. JAMA. 2016;316:1583–9. https://doi.org/10.1001/jama.2016.11993.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179–84. https://doi.org/10.1159/000339789.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction. J Am Coll Cardiol. 2018;72:2231–64. https://doi.org/10.1016/j.jacc.2018.08.1038.
Bowdish ME, D’Agostino RS, Thourani VH, Desai N, Shahian DM, Fernandez FG, et al. The society of thoracic surgeons adult cardiac surgery database: 2020 update on outcomes and research. Ann Thorac Surg. 2020;109:1646–55. https://doi.org/10.1016/j.athoracsur.2020.03.003.
Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. https://doi.org/10.1093/biomet/73.1.13.
Gelissen H, de Grooth HJ, Smulders Y, Wils EJ, de Ruijter W, Vink R, et al. Effect of low-normal vs high-normal oxygenation targets on organ dysfunction in critically ill patients: a randomized clinical trial. JAMA. 2021;326:940–8. https://doi.org/10.1001/jama.2021.13011.
Schjørring OL, Klitgaard TL, Perner A, Wetterslev J, Lange T, Siegemund M, et al. Lower or higher oxygenation targets for acute hypoxemic respiratory failure. N Engl J Med. 2021;384:1301–11. https://doi.org/10.1056/NEJMoa2032510.
Mattishent K, Thavarajah M, Sinha A, Peel A, Egger M, Solomkin J, et al. Safety of 80% vs 30–35% fraction of inspired oxygen in patients undergoing surgery: a systematic review and meta-analysis. Br J Anaesth. 2019;122:311–24. https://doi.org/10.1016/j.bja.2018.11.026.
Abou-Arab O, Huette P, Martineau L, Beauvalot C, Beyls C, Josse E, et al. Hyperoxia during cardiopulmonary bypass does not decrease cardiovascular complications following cardiac surgery: the CARDIOX randomized clinical trial. Intensive Care Med. 2019;45:1413–21. https://doi.org/10.1007/s00134-019-05761-4.
Murphy GS, Hessel EA 2nd, Groom RC. Optimal perfusion during cardiopulmonary bypass: an evidence-based approach. Anesth Analg. 2009;108:1394–417. https://doi.org/10.1213/ane.0b013e3181875e2e.
McIlroy DR, Shotwell MS, Lopez MG, Vaughn MT, Olsen JS, Hennessy C, et al. Oxygen administration during surgery and postoperative organ injury: observational cohort study. BMJ. 2022;379:e070941. https://doi.org/10.1136/bmj-2022-070941.
Ruetzler K, Cohen B, Leung S, Mascha EJ, Knotzer J, Kurz A, et al. Supplemental intraoperative oxygen does not promote acute kidney injury or cardiovascular complications after noncardiac surgery: subanalysis of an alternating intervention trial. Anesth Analg. 2020;130:933–40. https://doi.org/10.1213/ANE.0000000000004359.
Oprea AD, Del Rio JM, Cooter M, Green CL, Karhausen JA, Nailer P, et al. Pre- and postoperative anemia, acute kidney injury, and mortality after coronary artery bypass grafting surgery: a retrospective observational study. Can J Anaesth. 2018;65:46–59. https://doi.org/10.1007/s12630-017-0991-0.
Salmasi V, Maheshwari K, Yang D, Mascha EJ, Singh A, Sessler DI, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2017;126:47–65. https://doi.org/10.1097/ALN.0000000000001432.
Nam K, Kim HB, Kwak YL, Jeong YH, Ju JW, Bae J, et al. Effect of changes in inspired oxygen fraction on oxygen delivery during cardiac surgery: a substudy of the CARROT trial. Sci Rep. 2021;11:17862. https://doi.org/10.1038/s41598-021-97555-2.
Van der Linden P, Schmartz D, Gilbart E, Engelman E, Vincent JL. Effects of propofol, etomidate, and pentobarbital on critical oxygen delivery. Crit Care Med. 2000;28:2492–9. https://doi.org/10.1097/00003246-200007000-00051.
Heyman SN, Khamaisi M, Rosen S, Rosenberger C. Renal parenchymal hypoxia, hypoxia response and the progression of chronic kidney disease. Am J Nephrol. 2008;28:998–1006. https://doi.org/10.1159/000146075.
Rosenberger C, Rosen S, Heyman SN. Renal parenchymal oxygenation and hypoxia adaptation in acute kidney injury. Clin Exp Pharmacol Physiol. 2006;33:980–8. https://doi.org/10.1111/j.1440-1681.2006.04472.x.
Brezis M, Rosen S. Hypoxia of the renal medulla–its implications for disease. N Engl J Med. 1995;332:647–55. https://doi.org/10.1056/NEJM199503093321006.
Chou SY, Porush JG, Faubert PF. Renal medullary circulation: hormonal control. Kidney Int. 1990;37:1–13. https://doi.org/10.1038/ki.1990.1.
Evans RG, Lankadeva YR, Cochrane AD, Marino B, Iguchi N, Zhu MZL, et al. Renal haemodynamics and oxygenation during and after cardiac surgery and cardiopulmonary bypass. Acta Physiol. 2018. https://doi.org/10.1111/apha.12995.
de Somer F, Mulholland JW, Bryan MR, Aloisio T, Van Nooten GJ, Ranucci M. O2 delivery and CO2 production during cardiopulmonary bypass as determinants of acute kidney injury: Time for a goal-directed perfusion management? Crit Care. 2011;15:R192. https://doi.org/10.1186/cc10349.
Ranucci M, Romitti F, Isgrò G, Cotza M, Brozzi S, Boncilli A, et al. Oxygen delivery during cardiopulmonary bypass and acute renal failure after coronary operations. Ann Thorac Surg. 2005;80:2213–20. https://doi.org/10.1016/j.athoracsur.2005.05.069.
Berger MM, Grocott MPW. Facing acute hypoxia: from the mountains to critical care medicine. Br J Anaesth. 2017;118:283–6. https://doi.org/10.1093/bja/aew407.
Semler MW, Casey JD, Lloyd BD, Hastings PG, Hays MA, Stollings JL, et al. Oxygen-saturation targets for critically ill adults receiving mechanical ventilation. N Engl J Med. 2022;387:1759–69. https://doi.org/10.1056/NEJMoa2208415.
Wetterslev J, Meyhoff CS, Jørgensen LN, Gluud C, Lindschou J, Rasmussen LS. The effects of high perioperative inspiratory oxygen fraction for adult surgical patients. Cochrane Database Syst Rev. 2015;2015:CD008884. https://doi.org/10.1002/14651858.CD008884.pub2.
Staehr-Rye AK, Meyhoff CS, Scheffenbichler FT, Vidal Melo MF, Gätke MR, Walsh JL, et al. High intraoperative inspiratory oxygen fraction and risk of major respiratory complications. Br J Anaesth. 2017;119:140–9. https://doi.org/10.1093/bja/aex128.
McGuinness SP, Parke RL, Drummond K, Willcox T, Bailey M, Kruger C, et al. A multicenter, randomized, controlled Phase IIb trial of avoidance of hyperoxemia during cardiopulmonary bypass. Anesthesiology. 2016;125:465–73. https://doi.org/10.1097/ALN.0000000000001226.
WHO. Global guidelines for the prevention of surgical site infection. In: Global guidelines for the prevention of surgical site infection. 1st ed. Geneva; 2016
Hedenstierna G, Perchiazzi G, Meyhoff CS, Larsson A. Who can make sense of the WHO guidelines to prevent surgical site infection? Anesthesiology. 2017;126:771–3. https://doi.org/10.1097/ALN.0000000000001604.
Myles PS, Kurz A. Supplemental oxygen and surgical site infection: getting to the truth. Br J Anaesth. 2017;119:13–5. https://doi.org/10.1093/bja/aex096.
Volk T, Peters J, Sessler DI. The WHO recommendation for 80% perioperative oxygen is poorly justified. Anaesthetist. 2017;66:227–9. https://doi.org/10.1007/s00101-017-0286-4.
Kurz A, Kopyeva T, Suliman I, Podolyak A, You J, Lewis B, et al. Supplemental oxygen and surgical-site infections: an alternating intervention controlled trial. Br J Anaesth. 2018;120:117–26. https://doi.org/10.1016/j.bja.2017.11.003.
Cohen B, Schacham YN, Ruetzler K, Ahuja S, Yang D, Mascha EJ, et al. Effect of intraoperative hyperoxia on the incidence of surgical site infections: a meta-analysis. Br J Anaesth. 2018;120:1176–86. https://doi.org/10.1016/j.bja.2018.02.027.
Pedersen SS, Holse C, Mathar CE, Chan MTV, Sessler DI, Liu Y, et al. Intraoperative inspiratory oxygen fraction and myocardial injury after noncardiac surgery: results from an international observational study in relation to recent controlled trials. Anesth Analg. 2022;135:1021–30. https://doi.org/10.1213/ANE.0000000000006042.
Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray JE, et al. Air versus oxygen in ST-segment-elevation myocardial infarction. Circulation. 2015;131:2143–50. https://doi.org/10.1161/CIRCULATIONAHA.114.014494.
Holse C, Aasvang EK, Vester-Andersen M, Rasmussen LS, Wetterslev J, Christensen R, et al. Hyperoxia and antioxidants for myocardial injury in noncardiac surgery: A 2 × 2 factorial, blinded, randomized clinical trial. Anesthesiology. 2022;136:408–19. https://doi.org/10.1097/ALN.0000000000004117.
Acknowledgements
The authors appreciate the comments and statistical supervision provided by the Medical Research Collaborating Center (Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea). The authors are also grateful to Prof. Sun-Young Jung (College of Pharmacy, Chung-Ang University, Seoul, Korea) for her statistical assistance and supervision.
Funding
This work was supported by the National Research Foundation (NRF) grant funded by the Ministry of Science and ICT (MSICT) of Korea (Grant No. 2020R1C1C1004516).
Author information
Authors and Affiliations
Consortia
Contributions
KN collected and analyzed the data and prepared the manuscript. JSN collected and analyzed the data and prepared the manuscript. HBK collected and analyzed the data and revised the manuscript. JC analyzed the data and revised the manuscript. IEH collected and analyzed the data regarding the microcirculatory parameters. JWJ collected and analyzed the data regarding the microcirculatory parameters. JB collected and analyzed the data regarding the microcirculatory parameters. SL collected and analyzed the data regarding the microcirculatory parameters. YJC designed the study and prepared the manuscript. JKS collected the data and revised the manuscript. YLK collected the data and revised the manuscript. JHC collected the data and revised the manuscript. ICC designed the study, interpreted the analyzed data, and revised the manuscript. EHL designed the study, analyzed the data, and revised the manuscript. YJ designed the study, analyzed the data, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the local ethics committees of the three participating hospitals: the Institutional Review Board of SNUH (no. 1902-021-1008), the Institutional Review Board of AMC (no. 2019-0818), and the Severance Hospital Institutional Review Board (no. 4-2020-0741). All patients enrolled in this study provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary materials for the CARROT study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nam, K., Nam, JS., Kim, HB. et al. Effects of intraoperative inspired oxygen fraction (FiO2 0.3 vs 0.8) on patients undergoing off-pump coronary artery bypass grafting: the CARROT multicenter, cluster-randomized trial. Crit Care 27, 286 (2023). https://doi.org/10.1186/s13054-023-04558-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04558-8