Abstract
Background
How much scientific evidence is there to show that stem cell therapy is sufficient in preclinical and clinical studies of spinal cord injury before it is translated into clinical practice? This is a complicated problem. A single, small-sample clinical trial is difficult to answer, and accurate insights into this question can only be given by systematically evaluating all the existing evidence.
Methods
The PubMed, Ovid-Embase, Web of Science, and Cochrane databases were searched from inception to February 10, 2022. Two independent reviewers performed the literature search, identified and screened the studies, and performed a quality assessment and data extraction.
Results
In total, 62 studies involving 2439 patients were included in the analysis. Of these, 42 were single-arm studies, and 20 were controlled studies. The meta-analysis showed that stem cells improved the ASIA impairment scale score by at least one grade in 48.9% [40.8%, 56.9%] of patients with spinal cord injury. Moreover, the rate of improvement in urinary and gastrointestinal system function was 42.1% [27.6%, 57.2%] and 52.0% [23.6%, 79.8%], respectively. However, 28 types of adverse effects were observed to occur due to stem cells and transplantation procedures. Of these, neuropathic pain, abnormal feeling, muscle spasms, vomiting, and urinary tract infection were the most common, with an incidence of > 20%. While no serious adverse effects such as tumorigenesis were reported, this could be due to the insufficient follow-up period.
Conclusions
Overall, the results demonstrated that although the efficacy of stem cell therapy is encouraging, the subsequent adverse effects remain concerning. In addition, the clinical trials had problems such as small sample sizes, poor design, and lack of prospective registration, control, and blinding. Therefore, the current evidence is not sufficiently strong to support the clinical translation of stem cell therapy for spinal cord injury, and several problems remain. Additional well-designed animal experiments and high-quality clinical studies are warranted to address these issues.
Similar content being viewed by others
Background
According to the Global Burden of Diseases report, the age-standardized rate of spinal cord injury (SCI) is 13 (11 to 16) per 100,000 people, accounting for 27,042,505 cases (24,976,608 to 30,148,230) worldwide. In 2016 alone, there were 935,000 new cases of SCI [1]. A variety of treatment strategies, such as drugs (methylprednisolone, ganglioside), surgery (decompression and fusion surgery), and rehabilitation therapy (electrical stimulation, functional exercise), have been used widely in the clinic [2]. However, their efficacy is limited due to severe pathophysiological injuries after SCI, such as neuronal necrosis and apoptosis, ischemia-reperfusion injury, and the demyelination and degeneration of spinal axons. Currently, less than 1% of patients with SCI show complete recovery of neurological function [3, 4]. Therefore, new and more effective treatments are urgently required.
Decades of research have deepened our understanding of the mechanisms underlying injury, neural repair, and regeneration in SCI [5, 6]. Studies have shown that stem cells can protect and regenerate the injured spinal cord through neuroprotection, immunomodulation, axon sprouting and/or regeneration, neuronal relay formation, and myelin regeneration, among other mechanisms [4, 7]. Therefore, stem cell therapy has attracted great attention as a treatment strategy for SCI.
Stem cell therapy has shown great progress in preclinical research. Moreover, it has shown high therapeutic efficacy in other conditions, such as hematological malignancies, burns, and corneal transplants. Thus, it has attracted the attention of countless eager patients, clinicians, pharmaceutical companies, and the media [8,9,10]. Several interested parties are eagerly calling for the clinical translation of stem cell therapy for SCI, leading to a large number of clinical trials for stem cells. To accelerate this process, findings from rodent models were directly validated in human patients instead of using a step-wise testing approach in rodent models, followed by canine and feline models, primate models, and finally humans. As a result, a vast majority of preclinical trials have been conducted in rodents, and there are fewer than 20 studies in large animal models, accounting for < 2% of all preclinical research [11]. On the contrary, the number of related clinical trials has exceeded 100. Subsequently, unproven stem cell therapies in which patients receive autologous transplants could be performed without sufficient evidence, supervision, or informed consent [12, 13].
More notably, owing to the explosive growth of basic and clinical research in the field of stem cell therapy, other important issues may be neglected in the interest of rapidly advancing the clinical translation of stem cell therapy. Of these, the first and most important issue is the safety of stem cells. Stem cell therapy can lead to tumor formation, inappropriate migration, secondary injury, infection, and other adverse effects (AEs) [14]. The second is the ethical concerns related to the source, extraction, and transformation of stem cells. For example, human embryonic stem cells (hESCs) are known to show effective outcomes. However, are these embryos a potential form of life or just cells for research? What are the legal implications of destroying embryos? Should hESCs be derived from excess gametes or blastocysts during in vitro fertilization, aborted fetuses, voluntarily donated germ cells, or embryos produced for research purposes? In addition, although umbilical cord mesenchymal stem cells (UCMSCs) can be derived from discarded neonatal umbilical cords, they are the private property of mothers and neonates and are genetic resources protected by the law. These cells may cause allergy, hemolysis, and chronic toxicity after transplantation. Furthermore, they may carry pathogens and genetic mutations. Induced pluripotent stem cells (iPSCs) have the ability of unlimited proliferation and multi-directional differentiation. However, undifferentiated iPSCs can develop teratomas due to gene insertion mutations and uncontrolled proliferation and differentiation, leading to ethics-related debates [15, 16]. Currently, one of the most pressing ethical issues is the growing number of medical institutions that offer unproven stem cell-based treatments [17]. Finally, there are regulatory controversies over stem cells, and whether these regulations should be strict or lenient is often debated. The US Food and Drug Administration (FDA) has established a strict three-level regulatory system of “regulations-regulation-guiding principles” that requires research on stem cells to be subject to FDA review. Recently, the FDA has further stepped up its regulatory and enforcement activity for stem cell therapy to ban clinics and companies that could undermine the health of the entire regenerative medicine industry. In contrast, stem cell regulation in Japan is relatively less strict. The regulation of stem cells in Japan is subject to different levels of review. There are three risk levels based on the source of cells, processing methods, and the scope of application. With regulatory reforms, stem cell products could receive conditional approval after positive clinical findings in only 10 patients [18]. Benefiting from its comprehensive legal system and special approval policies, Japan has become a global leader in technological research and the development of cell therapy products. In other countries, such as China and India, several problems surrounding the regulation of stem cells remain. The regulatory boards only propose the basic principles for the development and evaluation of cell therapy products, and there is no implementation of stratified supervision based on the characteristics and applications of stem cells [19]. In addition, the necessary issues for the successful clinical application of stem cells remain unaddressed, including the risk-benefit ratio, mode of transplant strategy, oversights, conflicts of interest, surgical innovation, informed consent, and patient vulnerability [13].
Undoubtedly, despite several challenges, the initial success of stem cells in animal experiments and patients is indeed a cause for celebration and inspiration. It has brought immense hope of recovery for countless patients with SCI. However, experts must remain aware that there is still a lot of work to be done. Although systematic reviews of stem cell therapy for SCI have been published previously, they have had certain problems and limitations [20, 21]. Most of the current studies are single-arm, early-stage clinical trials with the main purpose of evaluating the safety of stem cells. However, published systematic reviews have only included randomized controlled trials, focusing on the effectiveness of stem cells, resulting in a limited number of included studies. Therefore, such systematic reviews do not fully analyze the existing data. Furthermore, they do not address the most important aspect, i.e., the safety of stem cell therapy and the feasibility of its translation from laboratory research to clinical practice. As such, it is unclear if we now have enough evidence to support the immediate clinical translation of stem cell therapy. Therefore, we performed a single-arm meta-analysis that included all the published clinical data and did not exclude studies based on the type of clinical research. Accordingly, we systematically evaluated the benefits and risks of stem cell therapy in patients with SCI in order to examine the feasibility of its clinical translation.
Methods
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [22]. Although the study was not registered with the PROSPERO database or other comparable databases, we verified that no similar study has been registered before undertaking this study.
Inclusion and exclusion criteria
Patients and diseases (P)
Patients with SCI.
Interventions (I)
Stem cells, no source restrictions.
Control (C)
There was no restriction based on whether the study had a control group.
Outcome (O)
(1) Primary outcome measure (safety indicator): AEs involving the nervous system, musculoskeletal system, digestive system, cardiovascular system, and other systems; (2) secondary outcome measures (effectiveness indicator): American Spinal Cord Injury Association Impairment Scale (ASIA) score improvements of at least one grade and improvements in the urinary system and gastrointestinal function.
Type of study (S)
Descriptive research, analytical research, and experimental research.
Exclusion criteria
The following are the exclusion criteria:
(1) Repeatedly published research, (2) unavailablity of the full text, (3) sample size of less than 3 subjects, and (4) inclusion of patients with other serious disorders.
Data sources and searches
Candidate studies were identified through searches of the PubMed, Web of Science, Cochrane, and Embase databases from inception until February 10, 2022. The following terms were combined to generate search keywords: (Spinal cord injury OR Spinal injury OR Spinal Cord Trauma OR Spinal Cord Transection OR Spinal Cord Laceration OR Post-Traumatic Myelopathy OR Spinal Cord Contusion) AND (stem cell OR stem cells). Further details of the search strategy are shown in Additional file 1: Table S1. We also reviewed studies included in previous systematic reviews and the reference lists of the included papers to identify other relevant studies.
Literature screening and data extraction
Two trained researchers selected the papers and stringently extracted the data based on the inclusion/exclusion criteria independently, and the selections were cross-checked. Disagreements were resolved by a third researcher through a common consensus. Data were extracted according to the pre-established full-text data extraction checklist, which included (1) basic characteristics of studies such as authors, year of publication, country, and type of study; (2) patient characteristics such as gender, age, sample size, and location and duration of injury; (3) types and sources of stem cells and the dose and route of transplantation; (4) key elements of bias risk assessment; and (5) outcome measures, i.e., effectiveness and safety indicators.
Methodological quality assessment
The methodological index for non-randomized studies (MINORS) was used to evaluate the methodological quality of the included studies. The following eight items were evaluated: (1) a clearly stated aim, (2) inclusion of consecutive patients, (3) prospective collection of data, (4) endpoints appropriate to the aim of the study, (5) unbiased assessment of the study endpoint, (6) follow-up period appropriate to the aim of the study, (7) loss to follow-up less than 5%, and (8) prospective calculation of the study size. Each item was scored on a scale of 0–2, where 0 indicated unreported, 1 indicated underreported, and 2 indicated adequately reported.
Statistical analysis
STATA 16.0 (Stata Corp, College Station, TX) was used for the meta-analysis of the incidence of each outcome event. Heterogeneity among studies was estimated using the χ2 test and the I2 statistics. If p was < 0.1 and/or I2 was > 50%, there was considered to be heterogeneity among the included studies, and the random-effects model was used for combined analysis. Otherwise, the fixed-effects model was used. In addition, in order to explore the safety and efficacy of stem cells from different sources, an additional subgroup analysis was performed.
Results
Literature search
A total of 6970 related studies were obtained from the preliminary search. After removing duplicate papers, a total of 4806 unique studies remained. Based on a preliminary screening of the titles and abstracts, we excluded 2540 non-clinical studies (animal studies, cell research, and in vitro experiments, etc.), 43 studies on non-stem cell interventions (exosome derived from stem cells, etc.), and 2122 articles that were not research papers (reviews, conference abstracts, letters to editors, editorials, etc.). The full text of the remaining 102 papers was screened. Some studies were further excluded due to the non-compliance of research type, non-compliance of intervention, lack of access to data, unreported outcome indicators, and duplication. Finally, 62 studies were included. The article screening process is shown in Fig. 1.
Basic information of included studies
The 62 studies included 42 single-arm studies and 20 controlled studies. A total of 2439 patients were included, and the sample size of each study ranged from 4 to 297. The age of the patients was between 6 and 65 years. The sites of SCI included the cervical, thoracic, and lumbar spinal cord, and the injury duration ranged from 3 days to 341 months. The types of stem cells included bone marrow mesenchymal stem cells (BMSCs, 38 studies), adipose tissue-derived mesenchymal stem cells (ADMSCs, 2 studies), UCMSCs (9 studies), cord blood stem cells (CBSCs, 1 study), ESCs (3 studies), hematopoietic stem cells (HSCs, 5 studies), and neural stem cells (NSCs, 5 studies). The number of transplanted stem cells varied greatly, ranging from 5 × 104 to 1.98 × 1010. The transplantation routes included intrathecal, scaffold-loaded, intralesional, venous, arterial, and subdural administration. The follow-up period ranged from 6 to 60 months. The basic information of the included studies is shown in Additional file 1: Table S2 [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84].
Methodological quality assessment
Of the 62 studies, 57 clearly stated the purpose of the study, 48 clearly reported the criteria for the inclusion and exclusion of patients, and the endpoint indicators of 44 studies appropriately reflected the purpose of the study. However, only 28 studies developed a research protocol before the trial, and only 17 evaluated the results in a blinded manner. In addition, 22 studies had a short follow-up period (12 months), 7 studies had a high rate of loss to follow-up (> 5%), and 49 studies did not fully calculate and statistically analyze the sample size, outcome indicators, and other data. The results of the quality evaluation are shown in Fig. 2.
Meta-analysis results
Primary outcome measures
A total of 41 studies reported at least one AE. Given the large heterogeneity among the included studies, we used the random effects model for meta-analysis.
We classified the AEs based on the organ system involved and thus analyzed the AEs in each system. (1) AEs of the nervous system: This group included 11 types of AEs, with a total incidence rate of 14.9% [11.3%, 18.9%]. Among them, the incidence of neuropathic pain was the highest at 25.2% [14.2%, 37.8%]. (2) AEs of the musculoskeletal system: This group included 6 kinds of AEs, with a total incidence rate of 20.4% [9.3%, 33.9%]. Among them, the incidence of muscle spasms was the highest at 25.5% [13.2%, 39.8%]. (3) AEs of the digestive system: This group included 3 kinds of AEs, with a total incidence rate of 11.5% [3.5%, 22.5%]. Among them, the incidence of vomiting was the highest at 21.6% [8.9%, 37.2%]. (4) AEs of the cardiovascular system: This group included 4 kinds of AEs, with a total incidence rate of 7.6% [3.7%, 12.6%]. Among them, the incidence of hypertension was the highest at 12.7% [8.7%, 17.3%]. (5) Other AEs: This group included pressure ulcers, itching and rash, lung infection, and urinary tract infection. Details are provided in Table 1.
The analysis of AEs based on the source of stem cells revealed that UCMSCs were associated with the most types of AEs (15 types), followed by BMSCs (12 types), NSCs (10 types), HSCs (9 types), ESCs (5 types), ADMSCs (4 types), and CBSCs (1 type). Further details are provided in Table 1.
Secondary outcome measures
The following are the secondary outcome measures:
-
(1)
A total of 58 studies reported improvements in ASIA scores among patients. The random effects model-based meta-analysis showed that stem cells improved motor function in 48.9% [40.8%, 56.9%] of patients with SCI. Through further subgroup analysis, the therapeutic effects of different types of stem cells were examined. HSCs were found to be the most effective, followed by NSCs, UCMSCs, BMSCs, ESCs, ADMSCs, and CBSCs, as shown in Fig. 3.
-
(2)
A total of 20 studies reported urinary system function improvements. The random effects model-based meta-analysis showed that stem cells improved urinary system function in 42.1% [27.6%, 57.2%] of patients with SCI. Further details are provided in Additional file 1: Fig. S1.
-
(3)
A total of 4 studies reported gastrointestinal function improvements. The random effects model-based meta-analysis showed that stem cells improved gastrointestinal function in 52.0% [23.6%, 79.8%] of patients with SCI. Further details are provided in Additional file 1: Fig. S2.
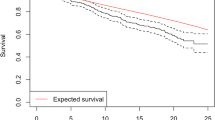
Publication bias and heterogeneity of included studies
The publication bias test of ASIA shows that the funnel chart is basically symmetrical, suggesting that the possibility of publication bias is small, as shown in Fig. 4.
After quantitative assessment of heterogeneity among included studies by I2, we found that I2 > 50%, suggesting that there is heterogeneity among included studies. Even when we performed subgroup analyses of stem cells from different sources, heterogeneity persisted. This suggests another source of heterogeneity among studies. Through a retrospective analysis of the included studies, we found that the source of stem cells, transplantation dose, transplantation route, and transplantation timing varied widely among studies, as we mentioned in the basic information of the included studies. In addition, there were differences in age, degree of injury, injury time, and follow-up time of patients. All these factors may be sources of heterogeneity. The large difference prevented us from the further subgroup analysis. Because the subgroups are subdivided again, the number of studies within each subgroup will be small, or even lack of studies. Therefore, we have clarified the source of heterogeneity as much as possible, and hope that future research will be standardized according to relevant guidelines, to reduce the heterogeneity among different studies and improve the universality of the research results.
Discussion
In recent years, the number of clinical trials based on stem cells has increased tremendously. Globally, there are now thousands of registered trials claiming to use “stem cells” in experimental treatments [85]. Thus, it appears that stem cell therapy has a well-established and strong clinical value. However, in reality, although some progress has been made, the clinical application of stem cells is still in its early stage. At present, clinical research on stem cells mainly includes phase I clinical trials, case series, and case reports. High-quality randomized controlled trials are lacking, and even simple controlled trials are few in number. Therefore, it is difficult to assess the efficacy of stem cells via head-to-head comparisons through meta-analysis [86]. In addition, although differences in cell types, sources, culture conditions, patient age, the degree of SCI, and other factors can make comparisons between studies challenging, these comparisons are still necessary [87]. Therefore, we analyzed the current evidence through a single-arm meta-analysis. Our findings showed that 48.9% of patients could benefit from stem cell therapy, i.e., 48.9% of patients showed at least one grade of improvement in the ASIA score after stem cell therapy. However, this only represents a slight improvement in sensory and motor function, far from the expected requirements for walking or daily activities. It is worth noting that the ASIA score-based assessment of sensory and motor function relies on subjective evaluation by the assessor and the patient, reducing result reliability to a certain extent [88]. Although this observed rate of 48.9% is lower than the rate of 78.57% obtained by Srivastava et al. in a randomized controlled trial with 200 patients [69] and the rate of 70% observed by Cheng et al. [31], given that small functional improvements are also extremely important for patient survival and well-being, stem cell therapy for SCI remains promising. Meanwhile, an increasing number of patients believe that the recovery of intestinal and bladder functions is as or more important than walking. Although our results show that the intestinal and bladder function improves in nearly half of all patients, these benefits only represent slight improvements in bladder fullness, urination impulse, and defecation (without sphincter control), which do not quite meet patient expectations [83].
Indeed, it is difficult to recruit enough SCI patients for clinical trials due to factors such as injury severity and patient age and physical condition. For cell-based trials, patients with SCI and grade A ASIA scores are recruited to avoid further damage. However, recovery in these patients may be low, and estimates of stem cell effectiveness may be inaccurate due to imprecisions in the measurement of subjective outcomes. Moreover, ASIA scale scores cannot fully reflect the severity of the pathology, and patients with the same ASIA grade may show a wide range of injury severity. Although the 48.8% rate of effectiveness appears encouraging, studies have shown that up to 70% of patients with complete cervical SCI can recover at least one spinal cord level within 1 year after injury [89]. Furthermore, 33% of patients with thoracic SCI have been found to show improvements of at least one grade [90]. Such spontaneous recovery in cases of SCI makes it difficult to confirm the efficacy of stem cells. Given that most trials lack a control group, it is not possible to rule out the contribution of spinal cord decompression or natural recovery to the therapeutic improvements observed after stem cell transplantation. Hence, stem cells cannot solely be credited with the therapeutic effects [90, 91]. Therefore, the actual therapeutic effects of the stem cells need to be further explored in standardized controlled trials according to the relevant guidelines.
While the extent to which stem cell therapy can benefit patients is unclear, the poor design and implementation of clinical trials also hinder the clinical applications of stem cells. Randomized controlled and double-blind human trials including placebo groups provide the most accurate and reliable data and are superior to observational studies or case reports [92]. However, most of the current studies are observational studies, case series, and so on. Small sample size and poor quality are also common problems in clinical trials [93]. Although the International Campaign for Cures of Spinal Cord Injury Paralysis (ICCP) has established a series of guidelines and standards for the design of clinical trials of SCI [92], 54.84% of the studies we examined were not registered on the clinical trial platform in advance. Hence, it was impossible to determine whether they reported all the results in accordance with the protocols and without any bias. The selective reporting of research results can lead to publication bias, thereby affecting the reliability of the conclusions garnered from a systematic review, or even leading to the opposite conclusion in some cases. Moreover, blinding is important to ensure the authenticity of clinical trial results. However, only 27.42% of studies included used blinding protocols. Failure to perform blinded evaluations may lead to the exaggeration of the actual effect and false-positive results [94]. Most of the included studies were phase I clinical trials, which are typically aimed at assessing the safety of stem cells. However, all studies explored and reported the efficacy of stem cells as the primary outcome measure, and ignored the reporting of AEs. Therefore, the safety of stem cells could be overestimated. At the same time, 35.48% of the studies followed patients for less than 1 year, which may have been insufficient to detect some AEs, such as tumor formation and inappropriate migration. Therefore, future clinical studies should extend the follow-up period as much as possible to fully explore the safety of stem cells. In addition, 79.03% of the studies did not pre-estimate the required number of patients to be enrolled in the trial or did not statistically analyze their results, reducing the likelihood of meaningful results. Most clinical trials do not have accurate and consistent inclusion and exclusion criteria for patients, leading to large differences in baseline characteristics, such as the location, type, injury duration, and severity of SCI. Moreover, the sources of stem cells and transplantation doses, timing, and routes also vary. This leads to study heterogeneity in meta-analyses and reduces the value of their findings in guiding future clinical trials. Hence, there is an urgent need to establish more stringent testing standards for stem cell therapy in SCI in order to standardize the design of clinical trials.
Patient safety should always be the top priority. The safety and AEs of stem cell therapy are mainly related to the inherent characteristics of the transplanted stem cells and the transplantation procedure. No serious AEs such as tumor formation were found in any of the studies we reviewed. Accordingly, these studies claimed that stem cell therapy was safe. However, it must be noted that the absence of serious AEs does not guarantee the safety of stem cell therapy. The 62 included studies reported a total of 28 AEs, including those affecting the nervous system, musculoskeletal system, digestive system, and cardiovascular system. Most of these AEs were mild, and the patients recovered completely after medical interventions. However, it is currently too soon to assume that stem cell therapy is safe, because this could further motivate those with blind confidence in stem cell therapy, which is not conducive to the scientific evaluation of its efficacy and safety. In addition, a study by Aspinall et al. showed that only 30% of clinical studies adequately reported various AEs during the clinical trial [95]. Hence, most studies may have ignored or even covered up AEs during the trial to “improve” the reported safety of stem cells. The meta-analysis by Zhao et al., which was based on control experiments, found a higher incidence of neuropathic pain and fever after stem cell therapy [96]. This was consistent with our findings, which indicated that the incidence of neuropathic pain, abnormal feeling, muscle spasms, vomiting, and urinary tract infection is higher than 20% in patients with SCI undergoing stem cell therapy. However, we reported a higher incidence of AEs than Zhao et al. because we enrolled more clinical trials, including single-arm studies. As a result, our sources of evidence were more comprehensive, and the results are more realistic. Although the observed AEs may not be related to the characteristics of the stem cells themselves, they could be affected by the transplantation technique, the severity of SCI, and the patients’ physical conditions. For example, neuropathic pain is mainly related to the use of large-caliber spinal needles during transplantation [97]. However, the observation of multiple AEs has greatly hindered the clinical applications of stem cells. In addition, after the subgroup analysis of stem cells from different sources, we found that mesenchymal stem cells such as BMSCs and UCMSCs—which were previously considered to have high safety—were associated with the highest rate of AEs among all the stem cells included in the current analysis [98]. This could be because the number of studies on BMSCs is the largest (61.29%, 38/62), and these studies also tend to have a large sample size. Hence, the AEs related to BMSCs are more apparent. In contrast, there was only one study on CBSCs. This study included 25 patients who were followed up for only 8 months. Hence, the AEs of CBSCs may be under-recognized. The possible AEs caused by stem cells can be explored properly only by reasonably calculating the required sample size, including patients who were clearly diagnosed with SCI, and ensuring a sufficient follow-up period. Hence, future studies should strongly focus on improving and standardizing these aspects.
Among the many safety issues surrounding stem cell transplantation, tumorigenesis is much more worrying than the fever and neuropathic pain caused by mild immune or allergic reactions [56, 79]. Stem cell products derived from hESCs and iPSCs confer the highest risk of tumorigenesis due to the presence of residual undifferentiated stem cells, malignantly transformed cells/mutations, and genetic instability. In addition, oncogenic activation due to the expression of foreign genes (e.g., various growth factors) and insertional mutagenesis of genetically modified viral vectors (e.g., retroviruses and lentiviruses) increases the risk of tumorigenicity and oncogenicity in stem cells [99]. For example, after iPSCs are treated with retroviruses, the retroviruses can get reactivated, resulting in tumor formation [100]. Although the tumorigenic potential of adult stem cells is thought to be lower than that of iPSC and hESCs, there have been reports of brain tumor formation after the injection of fetal NSCs [101]. Therefore, 71–74% of patients are “definitely” or “probably” not interested in participating in stem cell trials, and the possible risk of cancer is the greatest deterrent for these patients [46].
Currently, there is no global consensus on risk assessment strategies for the tumorigenicity and oncogenicity of stem cells. According to FDA guidelines, the risk of tumorigenesis can be decreased mainly by controlling the level of undifferentiated ESCs or other cellular impurities in hESC-derived cell products. The FDA guidelines also focus on the selection of preclinical animal species and the predictive ability of animal models to assess whether implanted cells form tumors at the transplant site and examine the malignant transformation of host cells and implanted cells in various tissues and organs. In fact, factors such as genetic and epigenetic variations in cell culture can increase the risk of tumorigenesis. Therefore, strategies to reduce the risk of tumors should be adopted during the development of high-risk stem cell products. Corresponding tumorigenicity testing methods can be established based on the quality and properties of candidate stem cells, the expected patient population, and tumorigenicity risk assessments. In preclinical studies, nude mice are usually used to study tumorigenicity in vivo, residual undifferentiated cells and transformed cells are used to study tumorigenicity in vitro, and server combined immune deficiency (SCID) mice are used to study tumorigenicity over the long term. No serious AEs like tumorigenesis have been reported in clinical trials so far, which could be due to the short follow-up period, because most of the studies (79%, 49/62) followed up patients for less than 2 years. Furthermore, the early termination of a trial is unfavorable for observing serious AEs such as tumor formation, especially because post-transplant ectopic growth can take up to 8 years [102, 103].
Although the success of stem cell therapy in preclinical studies has laid a good foundation for clinical research, its clinical translation has not been smooth. The number of new phase I and II clinical trials continued to increase from 2006 to 2012 but has since stagnated and even declined in 2018. The main reason is that the efficacy of stem cells is far less than expected [104]. First, animal studies attempt to minimize the variables in the experiment (e.g., baseline characteristics of the animals and the extent and location of lesions). However, patients with SCI show great heterogeneity (e.g., severity and location of injury, complications, age, sex, and rehabilitation training). Hence, the treatment efficacy observed in patients is often much lower than that observed in animals. Second, animal experiments often use the thoracic SCI model to study hindlimb motor recovery and related neural circuit changes. However, patients usually become quadriplegic due to cervical spine injury. In translational research, the extent and location of the lesion strongly influence the efficacy of the treatment. Some treatments yield beneficial effects only in subjects with specific lesion types [105]. Third, there are great differences in the inclusion and exclusion criteria among clinically recruited patients, and the location, severity, and timing of injury also differ. Therefore, it is difficult to include a homogenous group of patients even in high-quality randomized controlled trials, which makes the interpretation of treatment efficacy complicated and inaccurate. Fourth, the therapeutic effects observed in animal models are usually statistically significant. In clinical trials, the evaluation of functional results is more difficult because the small functional improvements generated by stem cells at the anatomical/histological level are difficult to detect. Finally, a careful investigation of the time window, dose, and route of stem cell transplantation is not a routine practice in animal studies, although these are major clinical problems that must be addressed in human studies [105].
In conclusion, the progress in clinical trials for stem cells has been exciting. However, most studies are in the early phase I/II stage, and clinical data are still being collected. It is too early to confirm that stem cells exert enormous curative effects. There are many differences and ambiguities in the selection of patients, cell types, timing of intervention, and doses and routes of stem cell transplantation in different clinical trials [75]. Therefore, close cooperation between preclinical and clinical aspects is warranted. Improving the safety, efficacy, and reproducibility of trials; identifying optimal transplantation parameters; strictly evaluating the benefits and risks of stem cell therapy; and strengthening supervision methods are urgent needs in this field [106, 107].
Strengths and limitations
We estimated the efficacy of stem cell therapy and examined the rate of associated AEs to objectively and comprehensively analyze the feasibility of clinical translation, which is key for guiding future research. To our knowledge, this study is the first to perform such an analysis.
Nevertheless, there are some undeniable limitations to this study. First, there were great differences in the baseline characteristics of patients, types of stem cells, and timing, dose, and route of transplantation among the studies. Hence, we were unable to conduct further subgroup analysis and obtain more information. Second, real stem cells show self-renewal and can differentiate into various types of cells. In practical clinical research, the definition of stem cells is not strict. Bone marrow mononuclear cells and neural progenitor cells are also sometimes used as stem cells [9, 108]. In the absence of a clear definition, we included studies that claimed to examine “stem cells,” but some of these studies may have actually used stem cell-like cells. Third, we included only studies in English and did not examine grey literature and conference abstracts. As a result, there may have been some language bias, and some important findings may have been left out. Finally, although we developed a protocol and conducted the study in strict accordance with this protocol, we did not register it in PROSPERO or other comparable databases in advance, which may have led to reporting bias.
Similarities and differences with similar studies
In order to better highlight the purpose and value of this study, we compared it with previously published studies. A total of 8 systematic reviews/meta-analyses (SR/MA) of stem cells for SCI were searched [20, 21, 109,110,111,112,113,114], as detailed in Table 2. Although safety is paramount for the clinical application of any therapy, we found that the published SR/MA focused on efficacy indicators while largely ignoring the safety outcomes of stem cell therapy. Although 7 of the 8 studies reported AEs, their reporting was not comprehensive. The AEs reported in these studies mainly included fever, headache, and neuropathic pain, but our study reported 28 kinds of AEs caused by stem cell transplantation, of which neuropathic pain, abnormal feeling, muscle spasms, vomiting, and urinary tract infections showed an incidence of > 20%. We calculated the incidence of various AEs and highlighted the common types of AEs. In addition, the types of studies we included were more extensive, the number of studies was larger, and the data extracted were richer. Therefore, our study can provide abundant data on the safety of stem cells and can guide future research.
Conclusions
To facilitate the translation of stem cell therapy from the bench to the bedside, stem cells must be fully proven to be safe and effective in animal and clinical studies. The effectiveness of stem cells is very clear in rodent models. However, our systematic review of clinical trials found that although stem cells have great potential in improving neurological function in patients with SCI, stem cell transplantation could cause 28 kinds of AEs. Some of these AEs may be potentially serious and cannot be ignored, even if they have not been detected. Current clinical trials have small samples, low quality, and lack control groups. Thus, they cannot demonstrate the safety of stem cell therapy completely. Therefore, the possible AEs caused by stem cell transplantation need to be properly explored in preclinical large animal models and early clinical studies. Furthermore, optimal transplantation conditions and parameters need to be identified to improve the therapeutic effects of stem cells. At the same time, experts in the field must pay attention to safety concerns, as the proven safety of stem cell therapy will be paramount for its clinical adoption. Our findings show that the current evidence is insufficient to advocate for the widespread use of stem cell therapy for SCI and warn against its rapid clinical translation. Until well-designed animal experiments and high-quality clinical studies are performed, the introduction of stem cell therapy into the clinic should be slow and performed with caution.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADL:
-
Activities of daily living
- ADMSCs:
-
Adipose tissue-derived mesenchymal stem cells
- AEs:
-
Adverse events
- ASIA:
-
American Spinal Cord Injury Association Impairment Scale
- BMSCs:
-
Bone marrow mesenchymal stem cells
- CBSCs:
-
Cord blood stem cells
- ESCs:
-
Embryonic stem cells
- FDA:
-
Food and Drug Administration
- hESCs:
-
Human embryonic stem cells
- HSCs:
-
Hematopoietic stem cells
- ICCP:
-
International Campaign for Cures of Spinal Cord Injury Paralysis
- iPSCs:
-
Induced pluripotent stem cells
- MINORS:
-
Methodological index for non-randomized study
- NSCs:
-
Neural stem cells
- SCI:
-
Spinal cord injury
- SCID:
-
Server combined immune-deficiency
- SR/MA:
-
Systematic review/meta-analysis
- SSEP:
-
Somatosensory evoked potential
- UCMSCs:
-
Umbilical cord mesenchymal stem cells
References
James SL, Theadom A, Ellenbogen RG, Bannick MS, Montjoy-Venning W, Lucchesi LR, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(1):56–87.
Flack JA, Sharma KD, Xie JY. Delving into the recent advancements of spinal cord injury treatment: a review of recent progress. Neural Regen Res. 2022;17(2):283.
Mansoori N, Bansil R, Sinha S. Current status of spinal cord regenerative therapies: a review. Indian J Neurosurg. 2016;5(01):003–9.
Ashammakhi N, Kim H-J, Ehsanipour A, Bierman RD, Kaarela O, Xue C, et al. Regenerative therapies for spinal cord injury. Tissue Eng Part B Rev. 2019;25(6):471–91.
Ramer LM, Ramer MS, Bradbury EJ. Restoring function after spinal cord injury: towards clinical translation of experimental strategies. Lancet Neurol. 2014;13(12):1241–56.
Courtine G, Sofroniew MV. Spinal cord repair: advances in biology and technology. Nat Med. 2019;25(6):898–908.
Assinck P, Duncan GJ, Hilton BJ, Plemel JR, Tetzlaff W. Cell transplantation therapy for spinal cord injury. Nat Neurosci. 2017;20(5):637–47.
De Luca M, Aiuti A, Cossu G, Parmar M, Pellegrini G, Robey PG. Advances in stem cell research and therapeutic development. Nat Cell Biol. 2019;21(7):801–11.
Chhabra HS, Sarda K, Jotwani G, Gourie-Devi M, Kaptanoglu E, Charlifue S, et al. Stem cell/cellular interventions in human spinal cord injury: is it time to move from guidelines to regulations and legislations? Literature review and Spinal Cord Society position statement. Eur Spine J. 2019;28(8):1837–45.
Shang Z, Wang R, Li D, Chen J, Zhang B, Wang M, et al. Spinal cord injury: a systematic review and network meta-analysis of therapeutic strategies based on 15 types of stem cells in animal models. Front Pharmacol. 2022;13:819861.
Gabel BC, Curtis EI, Marsala M, Ciacci JD. A review of stem cell therapy for spinal cord injury: large animal models and the frontier in humans. World Neurosurg. 2017;98:438–43.
Tator CH. Review of treatment trials in human spinal cord injury: issues, difficulties, and recommendations. Neurosurgery. 2006;59(5):957–87.
Cote DJ, Bredenoord AL, Smith TR, Ammirati M, Brennum J, Mendez I, et al. Ethical clinical translation of stem cell interventions for neurologic disease. Neurology. 2017;88(3):322–8.
Matsuda R, Yoshikawa M, Kimura H, Ouji Y, Nakase H, Nishimura F, et al. Cotransplantation of mouse embryonic stem cells and bone marrow stromal cells following spinal cord injury suppresses tumor development. Cell Transplant. 2009;18(1):39–54.
Wernig M, Zhao JP, Pruszak J, Hedlund E, Fu D, Soldner F, et al. Neurons derived from reprogrammed fibroblasts functionally integrate into the fetal brain and improve symptoms of rats with Parkinson’s disease. Proc Natl Acad Sci USA. 2008;105(15):5856–61.
Bock C, Kiskinis E, Verstappen G, Gu H, Boulting G, Smith ZD, et al. Reference maps of human ES and iPS cell variation enable high-throughput characterization of pluripotent cell lines. Cell. 2011;144(3):439–52.
Aly RM. Current state of stem cell-based therapies: an overview. Stem Cell Investig. 2020;7:1-10.
Cyranoski D. Japan to offer fast-track approval path for stem cell therapies. Nat Med. 2013;19(5):510.
Rosemann A, Vasen F, Bortz G. Global diversification in medicine regulation: insights from regenerative stem cell medicine. Sci Cult (Lond). 2019;28(2):223–49.
Tang QR, Xue H, Zhang Q, Guo Y, Xu H, Liu Y, et al. Evaluation of the clinical efficacy of stem cell transplantation in the treatment of spinal cord injury: a systematic review and meta-analysis. Cell Transplant. 2021;30:9636897211067804.
Liu S, Zhang H, Wang H, Huang J, Yang Y, Li G, et al. A comparative study of different stem cell transplantation for spinal cord injury: a systematic review and network meta-analysis. World Neurosurg. 2022;159:e232–e43.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Abdelaziz OS, Marie A, Abbas M, Ibrahim M, Gabr H. Feasibility, safety, and efficacy of directly transplanting autologous adult bone marrow stem cells in patients with chronic traumatic dorsal cord injury: a pilot clinical study. Neurosurg Q. 2010;20(3):216–26.
Adel N, Gabr H, Hamdy S, Afifi L, Mahmoud H. Stem cell therapy in chronic spinal cord injuries. Egypt J Neurol Psychiat Neurosurg. 2009;46(2):467–78.
Albu S, Kumru H, Coll R, Vives J, Vallés M, Benito-Penalva J, et al. Clinical effects of intrathecal administration of expanded Wharton jelly mesenchymal stromal cells in patients with chronic complete spinal cord injury: a randomized controlled study. Cytotherapy. 2021;23(2):146–56.
Al-Zoubi A, Jafar E, Jamous M, Al-Twal F, Al-Bakheet S, Zalloum M, et al. Transplantation of purified autologous leukapheresis-derived CD34+ and CD133+ stem cells for patients with chronic spinal cord injuries: long-term evaluation of safety and efficacy. Cell Transplant. 2014;23(1_suppl):25–34.
Amr SM, Gouda A, Koptan WT, Galal AA, Abdel-Fattah DS, Rashed LA, et al. Bridging defects in chronic spinal cord injury using peripheral nerve grafts combined with a chitosan-laminin scaffold and enhancing regeneration through them by co-transplantation with bone-marrow-derived mesenchymal stem cells: case series of 14 patients. J Spinal Cord Med. 2014;37(1):54–71.
Bhanot Y, Rao S, Ghosh D, Balaraju S, Radhika CR, Kumar KVS. Autologous mesenchymal stem cells in chronic spinal cord injury. Br J Neurosurg. 2011;25(4):516–22.
Bryukhovetskiy AS, Bryukhovetskiy IS. Effectiveness of repeated transplantations of hematopoietic stem cells in spinal cord injury. World J Transplant. 2015;5(3):110.
Chen W, Zhang Y, Yang S, Sun J, Qiu H, Hu X, et al. NeuroRegen scaffolds combined with autologous bone marrow mononuclear cells for the repair of acute complete spinal cord injury: a 3-year clinical study. Cell Transplant. 2020;29:0963689720950637.
Cheng H, Liu X, Hua R, Dai G, Wang X, Gao J, et al. Clinical observation of umbilical cord mesenchymal stem cell transplantation in treatment for sequelae of thoracolumbar spinal cord injury. J Transl Med. 2014;12(1):1–8.
Chernykh E, Stupak V, Muradov G, Sizikov MY, Shevela EY, Leplina OY, et al. Application of autologous bone marrow stem cells in the therapy of spinal cord injury patients. Bull Exp Biol Med. 2007;143(4):543–7.
Chhabra H, Sarda K, Arora M, Sharawat R, Singh V, Nanda A, et al. Autologous bone marrow cell transplantation in acute spinal cord injury—an Indian pilot study. Spinal cord. 2016;54(1):57–64.
Curtis E, Martin JR, Gabel B, Sidhu N, Rzesiewicz TK, Mandeville R, et al. A first-in-human, phase I study of neural stem cell transplantation for chronic spinal cord injury. Cell stem cell. 2018;22(6):941–50 e6.
Dai G, Liu X, Zhang Z, Wang X, Li M, Cheng H, et al. Comparative analysis of curative effect of CT-guided stem cell transplantation and open surgical transplantation for sequelae of spinal cord injury. J Transl Med. 2013;11(1):1–10.
Dai G, Liu X, Zhang Z, Yang Z, Dai Y, Xu R. Transplantation of autologous bone marrow mesenchymal stem cells in the treatment of complete and chronic cervical spinal cord injury. Brain Res. 2013;1533:73–9.
Deda H, Inci M, Kürekçi A, Kayıhan K, Özgün E, Üstünsoy G, et al. Treatment of chronic spinal cord injured patients with autologous bone marrow-derived hematopoietic stem cell transplantation: 1-year follow-up. Cytotherapy. 2008;10(6):565–74.
Deng W-S, Ma K, Liang B, Liu X-Y, Xu H-Y, Zhang J, et al. Collagen scaffold combined with human umbilical cord-mesenchymal stem cells transplantation for acute complete spinal cord injury. Neural Regen Res. 2020;15(9):1686.
El-Kheir WA, Gabr H, Awad MR, Ghannam O, Barakat Y, Farghali HA, et al. Autologous bone marrow-derived cell therapy combined with physical therapy induces functional improvement in chronic spinal cord injury patients. Cell Transplant. 2014;23(6):729–45.
Geffner L, Santacruz P, Izurieta M, Flor L, Maldonado B, Auad A, et al. Administration of autologous bone marrow stem cells into spinal cord injury patients via multiple routes is safe and improves their quality of life: comprehensive case studies. Cell Transplant. 2008;17(12):1277–93.
Ghobrial GM, Anderson KD, Dididze M, Martinez-Barrizonte J, Sunn GH, Gant KL, et al. Human neural stem cell transplantation in chronic cervical spinal cord injury: functional outcomes at 12 months in a phase II clinical trial. Neurosurgery. 2017;64(CN_suppl_1):87–91.
Goni VG, Chhabra R, Gupta A, Marwaha N, Dhillon MS, Pebam S, et al. Safety profile, feasibility and early clinical outcome of cotransplantation of olfactory mucosa and bone marrow stem cells in chronic spinal cord injury patients. Asian Spine J. 2014;8(4):484.
Hammadi AA, Andolina Marino SF. Clinical response of 277 patients with spinal cord injury to stem cell therapy in Iraq. Int J Stem Cells. 2012;5(1):76.
Hur JW, Cho T-H, Park D-H, Lee J-B, Park J-Y, Chung Y-G. Intrathecal transplantation of autologous adipose-derived mesenchymal stem cells for treating spinal cord injury: a human trial. J Spinal Cord Med. 2016;39(6):655–64.
Jeon SR, Park JH, Lee JH, Kim DY, Kim HS, Sung IY, et al. Treatment of spinal cord injury with bone marrow-derived, cultured autologous mesenchymal stem cells. Tissue Eng Regen Med. 2010;7(3):316–22.
Jiang P-C, Xiong W-P, Wang G, Ma C, Yao W-Q, Kendell SF, et al. A clinical trial report of autologous bone marrow-derived mesenchymal stem cell transplantation in patients with spinal cord injury. Exp Ther Med. 2013;6(1):140–6.
Kakabadze Z, Kipshidze N, Mardaleishvili K, Chutkerashvili G, Chelishvili I, Harders A, et al. Phase 1 trial of autologous bone marrow stem cell transplantation in patients with spinal cord injury. Stem Cells Int. 2016;2016:6768274.
Karamouzian S, Nematollahi-Mahani SN, Nakhaee N, Eskandary H. Clinical safety and primary efficacy of bone marrow mesenchymal cell transplantation in subacute spinal cord injured patients. Clin Neurol Neurosurg. 2012;114(7):935–9.
Kumar AA, Kumar SR, Narayanan R, Arul K, Baskaran M. Autologous bone marrow derived mononuclear cell therapy for spinal cord injury: a phase I/II clinical safety and primary efficacy data. Exp Clin Transplant. 2009;7(4):241–8.
Larocca TF, Macêdo CT, de Freitas Souza BS, Andrade-Souza YM, Villarreal CF, Matos AC, et al. Image-guided percutaneous intralesional administration of mesenchymal stromal cells in subjects with chronic complete spinal cord injury: a pilot study. Cytotherapy. 2017;19(10):1189–96.
Levi AD, Anderson KD, Okonkwo DO, Park P, Bryce TN, Kurpad SN, et al. Clinical outcomes from a multi-center study of human neural stem cell transplantation in chronic cervical spinal cord injury. J Neurotrauma. 2019;36(6):891–902.
Levi AD, Okonkwo DO, Park P, Jenkins AL III, Kurpad SN, Parr AM, et al. Emerging safety of intramedullary transplantation of human neural stem cells in chronic cervical and thoracic spinal cord injury. Neurosurgery. 2018;82(4):562–75.
Liu J, Han D, Wang Z, Xue M, Zhu L, Yan H, et al. Clinical analysis of the treatment of spinal cord injury with umbilical cord mesenchymal stem cells. Cytotherapy. 2013;15(2):185–91.
Mendonça MVP, Larocca TF, de Freitas Souza BS, Villarreal CF, Silva LFM, Matos AC, et al. Safety and neurological assessments after autologous transplantation of bone marrow mesenchymal stem cells in subjects with chronic spinal cord injury. Stem Cell Res Ther. 2014;5(6):1–11.
Oh SK, Choi KH, Yoo JY, Kim DY, Kim SJ, Jeon SR. A phase III clinical trial showing limited efficacy of autologous mesenchymal stem cell therapy for spinal cord injury. Neurosurgery. 2016;78(3):436–47.
Oraee-Yazdani S, Akhlaghpasand M, Golmohammadi M, Hafizi M, Zomorrod MS, Kabir NM, et al. Combining cell therapy with human autologous Schwann cell and bone marrow-derived mesenchymal stem cell in patients with subacute complete spinal cord injury: safety considerations and possible outcomes. Stem Cell Res Ther. 2021;12(1):1–15.
Oraee-Yazdani S, Hafizi M, Atashi A, Ashrafi F, Seddighi A, Hashemi S, et al. Co-transplantation of autologous bone marrow mesenchymal stem cells and Schwann cells through cerebral spinal fluid for the treatment of patients with chronic spinal cord injury: safety and possible outcome. Spinal cord. 2016;54(2):102–9.
Pal R, Venkataramana NK, Bansal A, Balaraju S, Jan M, Chandra R, et al. Ex vivo-expanded autologous bone marrow-derived mesenchymal stromal cells in human spinal cord injury/paraplegia: a pilot clinical study. Cytotherapy. 2009;11(7):897–911.
Park HC, Shim YS, Ha Y, Yoon SH, Park SR, Choi BH, et al. Treatment of complete spinal cord injury patients by autologous bone marrow cell transplantation and administration of granulocyte-macrophage colony stimulating factor. Tissue Eng. 2005;11(5-6):913–22.
Park JH, Kim DY, Sung IY, Choi GH, Jeon MH, Kim KK, et al. Long-term results of spinal cord injury therapy using mesenchymal stem cells derived from bone marrow in humans. Neurosurgery. 2012;70(5):1238–47.
Saito F, Nakatani T, Iwase M, Maeda Y, Murao Y, Suzuki Y, et al. Administration of cultured autologous bone marrow stromal cells into cerebrospinal fluid in spinal injury patients: a pilot study. Restor Neurol Neurosci. 2012;30(2):127–36.
Satti HS, Waheed A, Ahmed P, Ahmed K, Akram Z, Aziz T, et al. Autologous mesenchymal stromal cell transplantation for spinal cord injury: a phase I pilot study. Cytotherapy. 2016;18(4):518–22.
Sharma A, Sane H, Gokulchandran N, Kulkarni P, Jose A, Nair V, et al. Intrathecal transplantation of autologous bone marrow mononuclear cells in patients with sub-acute and chronic spinal cord injury: an open-label study. Int J Health Sci. 2020;14(2):24.
Shin JC, Kim KN, Yoo J, Kim I-S, Yun S, Lee H, et al. Clinical trial of human fetal brain-derived neural stem/progenitor cell transplantation in patients with traumatic cervical spinal cord injury. Neural Plast. 2015;2015:630932.
Shroff G. Human embryonic stem cell therapy in chronic spinal cord injury: a retrospective study. Clin Transl Sci. 2016;9(3):168–75.
Shroff G. Magnetic resonance imaging tractography as a diagnostic tool in patients with spinal cord injury treated with human embryonic stem cells. Neuroradiol J. 2017;30(1):71–9.
Shroff G, Thakur D, Dhingra V, Baroli DS, Khatri D, Gautam RD. Role of physiotherapy in the mobilization of patients with spinal cord injury undergoing human embryonic stem cells transplantation. Clin Transl Med. 2016;5(1):1–9.
Song H, Suo S, Ning C, Zhang Y, Mu W, Chen S. Bone marrow mesenchymal stem cells transplantation on acute spinal cord injury. J Hard Tissue Biol. 2020;29(2):91–8.
Srivastava RN, Agrahari AK, Singh A, Chandra T, Raj S. Effectiveness of bone marrow-derived mononuclear stem cells for neurological recovery in participants with spinal cord injury: a randomized controlled trial. Asian J Transfus Sci. 2019;13(2):120.
Suzuki Y, Ishikawa N, Omae K, Hirai T, Ohnishi K, Nakano N, et al. Bone marrow-derived mononuclear cell transplantation in spinal cord injury patients by lumbar puncture. Restor Neurol Neurosci. 2014;32(4):473–82.
Syková E, Homola A, Mazanec R, Lachmann H, Konrádová ŠL, Kobylka P, et al. Autologous bone marrow transplantation in patients with subacute and chronic spinal cord injury. Cell Transplant. 2006;15(8-9):675–87.
Tang F, Tang J, Zhao Y, Zhang J, Xiao Z, Chen B, et al. Long-term clinical observation of patients with acute and chronic complete spinal cord injury after transplantation of NeuroRegen scaffold. Sci China Life Sci. 2022;65(5):909-26.
Thakkar UG, Vanikar AV, Trivedi HL, Shah VR, Dave SD, Dixit SB, et al. Infusion of autologous adipose tissue derived neuronal differentiated mesenchymal stem cells and hematopoietic stem cells in post-traumatic paraplegia offers a viable therapeutic approach. Adv Biomed Res. 2016;5:51.
Tien NLB, Hoa ND, Van Thanh V, Van Thach N, Ngoc VTN, Dinh TC, et al. Autologous transplantation of adipose-derived stem cells to treat acute spinal cord injury: evaluation of clinical signs, mental signs, and quality of life. Open Access Maced J Med Sci. 2019;7(24):4399.
Vaquero J, Zurita M, Rico MA, Aguayo C, Bonilla C, Marin E, et al. Intrathecal administration of autologous mesenchymal stromal cells for spinal cord injury: safety and efficacy of the 100/3 guideline. Cytotherapy. 2018;20(6):806–19.
Vaquero J, Zurita M, Rico MA, Bonilla C, Aguayo C, Fernández C, et al. Repeated subarachnoid administrations of autologous mesenchymal stromal cells supported in autologous plasma improve quality of life in patients suffering incomplete spinal cord injury. Cytotherapy. 2017;19(3):349–59.
Vaquero J, Zurita M, Rico MA, Bonilla C, Aguayo C, Montilla J, et al. An approach to personalized cell therapy in chronic complete paraplegia: he Puerta de Hierro phase I/II clinical trial. Cytotherapy. 2016;18(8):1025–36.
Xiao Z, Tang F, Tang J, Yang H, Zhao Y, Chen B, et al. One-year clinical study of NeuroRegen scaffold implantation following scar resection in complete chronic spinal cord injury patients. Sci China Life Sci. 2016;59(7):647–55.
Yang Y, Pang M, Du C, Liu Z-Y, Chen Z-H, Wang N-X, et al. Repeated subarachnoid administrations of allogeneic human umbilical cord mesenchymal stem cells for spinal cord injury: a phase 1/2 pilot study. Cytotherapy. 2021;23(1):57–64.
Yao L, He C, Zhao Y, Wang J, Tang M, Li J, et al. Human umbilical cord blood stem cell transplantation for the treatment of chronic spinal cord injury: electrophysiological changes and long-term efficacy. Neural Regen Res. 2013;8(5):397.
Yazdani SO, Hafizi M, Zali A-R, Atashi A, Ashrafi F, Seddighi A-S, et al. Safety and possible outcome assessment of autologous Schwann cell and bone marrow mesenchymal stromal cell co-transplantation for treatment of patients with chronic spinal cord injury. Cytotherapy. 2013;15(7):782–91.
Yoon SH, Shim YS, Park YH, Chung JK, Nam JH, Kim MO, et al. Complete spinal cord injury treatment using autologous bone marrow cell transplantation and bone marrow stimulation with granulocyte macrophage-colony stimulating factor: phase I/II clinical trial. Stem cells. 2007;25(8):2066–73.
Zhao Y, Tang F, Xiao Z, Han G, Wang N, Yin N, et al. Clinical study of NeuroRegen scaffold combined with human mesenchymal stem cells for the repair of chronic complete spinal cord injury. Cell Transplant. 2017;26(5):891–900.
Zhao Y, Yao L, Ao L, Ou J, He Y, Shang Y. Study of the diffusion tensor imaging for preclinical therapeutic efficacy of umbilical cord mesenchymal stem cell transplantation in the treatment of spinal cord injury. Int J Gen Med. 2021;14:9721.
Chari S, Nguyen A, Saxe J. Stem cells in the clinic. Cell Stem Cell. 2018;22(6):781–2.
Chhabra HS, Sarda K. Clinical translation of stem cell based interventions for spinal cord injury—are we there yet? Adv Drug Deliv Rev. 2017;120:41–9.
Liau LL, Looi QH, Chia WC, Subramaniam T, Ng MH, Law JX. Treatment of spinal cord injury with mesenchymal stem cells. Cell Biosci. 2020;10(1):1–17.
Waring WP 3rd, Biering-Sorensen F, Burns S, Donovan W, Graves D, Jha A, et al. _ 2009 review and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med. 2010;33(4):346–52.
Steeves J, Kramer J, Fawcett J, Cragg J, Lammertse D, Blight A, et al. Extent of spontaneous motor recovery after traumatic cervical sensorimotor complete spinal cord injury. Spinal cord. 2011;49(2):257–65.
Furlan JC, Noonan V, Cadotte DW, Fehlings MG. Timing of decompressive surgery of spinal cord after traumatic spinal cord injury: an evidence-based examination of pre-clinical and clinical studies. J Neurotrauma. 2011;28(8):1371–99.
El Tecle NE, Dahdaleh NS, Bydon M, Ray WZ, Torner JC, Hitchon PW. The natural history of complete spinal cord injury: a pooled analysis of 1162 patients and a meta-analysis of modern data. J Neurosurg Spine. 2018;28(4):436–43.
Lammertse D, Tuszynski MH, Steeves JD, Curt A, Fawcett JW, Rask C, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: clinical trial design. Spinal cord. 2007;45(3):232–42.
Califf RM, Zarin DA, Kramer JM, Sherman RE, Aberle LH, Tasneem A. Characteristics of clinical trials registered in ClinicalTrials. gov, 2007-2010. JAMA. 2012;307(17):1838–47.
Vesterinen HM, Sena ES, Ffrench-Constant C, Williams A, Chandran S, Macleod MR. Improving the translational hit of experimental treatments in multiple sclerosis. Mult Scler. 2010;16(9):1044–55.
Aspinall P, Harrison L, Scheuren P, Cragg JJ, Ferguson AR, Guest JD, et al. A systematic review of safety reporting in acute spinal cord injury clinical trials: challenges and recommendations. J Neurotrauma. 2021;38(15):2047–54.
Zhao H, Sun Q-L, Duan L-J, Yang Y-D, Gao Y-S, Zhao D-Y, et al. Is cell transplantation a reliable therapeutic strategy for spinal cord injury in clinical practice? A systematic review and meta-analysis from 22 clinical controlled trials. Eur Spine J. 2019;28(5):1092–112.
Amer MH, Rose FR, Shakesheff KM, Modo M, White LJ. Translational considerations in injectable cell-based therapeutics for neurological applications: concepts, progress and challenges. NPJ Regen Med. 2017;2(1):1–13.
Vismara I, Papa S, Rossi F, Forloni G, Veglianese P. Current options for cell therapy in spinal cord injury. Trends Mol Med. 2017;23(9):831–49.
Li Y, Huo Y, Yu L, Wang J. Quality control and nonclinical research on CAR-T cell products: general principles and key issues. Engineering. 2019;5(1):122–31.
Okita K, Ichisaka T, Yamanaka S. Generation of germline-competent induced pluripotent stem cells. Nature. 2007;448(7151):313–U1.
Abbot S, Agbanyo F, Ahlfors J-E, Baghbaderani BA, Bartido S, Bharti K, et al. Report of the international conference on manufacturing and testing of pluripotent stem cells. Biologicals. 2018;56:67–83.
Dlouhy BJ, Awe O, Rao RC, Kirby PA, Hitchon PW. Autograft-derived spinal cord mass following olfactory mucosal cell transplantation in a spinal cord injury patient: case report. J Neurosurg Spine. 2014;21(4):618–22.
Woodworth CF, Jenkins G, Barron J, Hache N. Intramedullary cervical spinal mass after stem cell transplantation using an olfactory mucosal cell autograft. CMAJ. 2019;191(27):E761–E4.
Kabat M, Bobkov I, Kumar S, Grumet M. Trends in mesenchymal stem cell clinical trials 2004-2018: is efficacy optimal in a narrow dose range? Stem Cells Transl Med. 2020;9(1):17–27.
Filli L, Schwab ME. The rocky road to translation in spinal cord repair. Ann Neurol. 2012;72(4):491–501.
Nori S, Okada Y, Nishimura S, Sasaki T, Itakura G, Kobayashi Y, et al. Long-term safety issues of iPSC-based cell therapy in a spinal cord injury model: oncogenic transformation with epithelial-mesenchymal transition. Stem Cell Reports. 2015;4(3):360–73.
Campbell A, Brieva T, Raviv L, Rowley J, Niss K, Brandwein H, et al. Concise review: process development considerations for cell therapy. Stem Cells Transl Med. 2015;4(10):1155–63.
Can A. A concise review on the classification and nomenclature of stem cells. Turk J Haematol. 2008;25(2):57–9.
Xu P, Yang X. The efficacy and safety of mesenchymal stem cell transplantation for spinal cord injury patients: a meta-analysis and systematic review. Cell Transplant. 2019;28(1):36–46.
Muthu S, Jeyaraman M, Gulati A, Arora A. Current evidence on mesenchymal stem cell therapy for traumatic spinal cord injury: systematic review and meta-analysis. Cytotherapy. 2021;23(3):186–97.
Li XC, Zhong CF, Deng GB, Liang RW, Huang CM. Efficacy and safety of bone marrow-derived cell transplantation for spinal cord injury: a systematic review and meta-analysis of clinical trials. Clin Transplant. 2015;29(9):786–95.
Johnson LDV, Pickard MR, Johnson WEB. The comparative effects of mesenchymal stem cell transplantation therapy for spinal cord injury in humans and animal models: a systematic review and meta-analysis. Biology (Basel). 2021;10(3):230.
Fan X, Wang JZ, Lin XM, Zhang L. Stem cell transplantation for spinal cord injury: a meta-analysis of treatment effectiveness and safety. Neural Regen Res. 2017;12(5):815–25.
Chen WC, Liu WF, Bai YY, Zhou YY, Zhang Y, Wang CM, et al. Transplantation of mesenchymal stem cells for spinal cord injury: a systematic review and network meta-analysis. J Transl Med. 2021;19(1):178.
Acknowledgements
Not applicable.
Funding
We acknowledge the financial support from the Gansu Natural Science Foundation (No. 21JR7RA362) and The First Hospital of Lanzhou University Foundation (No. ldyyyn2021-121).
Author information
Authors and Affiliations
Contributions
XW undertook the design, guidance, and modification of the project and paper. ZS completed the implementation of the project and writing of the paper. MW, BZ, and PPWX completed the collection and collation of the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Search strategies. Table S2. Basic information of the included studies. Fig. S1. Findings from the meta-analysis of improvement in urinary system. Fig. S2. Findings from the meta-analysis of improvement in gastrointestinal function.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shang, Z., Wang, M., Zhang, B. et al. Clinical translation of stem cell therapy for spinal cord injury still premature: results from a single-arm meta-analysis based on 62 clinical trials. BMC Med 20, 284 (2022). https://doi.org/10.1186/s12916-022-02482-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-022-02482-2