Abstract
Background
A comprehensive, accurate description of workforce capacity is important for health service planning, to ensure that health services meet local needs. In many low- to middle-income countries, the government’s service planning ability is barred by the lack of accurate and/or comprehensively-described workforce data. In these low-resource settings, lack of appropriate planning leads to limited or no access to rehabilitation services. Variability in the definitions and scope of rehabilitation professionals further complicates the understanding of rehabilitation services and how it should be planned and delivered. Another challenge to describing the primary rehabilitation workforce capacity, is the lack of standardised and agreed-upon global metrics. These inconsistencies highlight the need for a comprehensive understanding of current practices, which can offer guidance to countries wishing to describe their rehabilitation workforce. This study aimed to scope the range of descriptors and metrics used to describe the rehabilitation workforce and to compare the workforce across countries that used similar descriptors in published reports.
Methods
A scoping review was conducted according to the five-step framework first developed by Arksey and O’Malley. The review included a broad search of literature regarding the rehabilitation workforce and how countries quantify and describe the rehabilitation workforce.
Results
Nineteen studies on rehabilitation workforce capacity were identified. All but one (a cross-sectional study) were database reviews. The main descriptors and indicators used to describe the rehabilitation workforce capacity were profession type, age, gender, distributions between urban/rural, level of care, and private/public sectors, absolute count totals, and population-adjusted ratios.
Conclusion
This scoping review provided an overview of descriptors and indicators used to describe the rehabilitation workforce capacity internationally. The study is a first step towards developing standardised descriptors and metrics to quantify the rehabilitation workforce capacity, that will allow for comparison between different settings.
Trial registration
This scoping review protocol has been registered with the Open Science Framework (http://osf.10/7h6xz).
Similar content being viewed by others
Introduction
A comprehensive and accurate description of workforce capacity is important for health service planning to ensure that health services meet local needs [1]. Health service planning strongly hinges on the appropriate level of human resources to deliver the required health services. In many low- to middle-income countries (LMICs), the government’s ability to plan services is barred by the lack of accurate and/or comprehensively-described workforce data [2]. Although many services are sub-optimal in countries with constrained resources, services such as rehabilitation are particularly affected as it is often under-recognised and not prioritised in countries with limited resources for healthcare delivery [1]. In these low-resource settings, the lack of appropriate planning leads to limited or no access to rehabilitation services.
The limited access to rehabilitation services in LMICs is widely reported in the literature [1, 3], despite the increasing need for rehabilitation services in these settings. Of further concern is that the need for rehabilitation services is increasing at a higher rate in LMICs compared to high-income countries (HICs) [4, 5]. Therefore, ministries of health must understand the rehabilitation workforce, as it should be a fundamental component of health service planning. The importance of describing the rehabilitation workforce is also accentuated by the World Health Organisation’s (WHO) Rehabilitation 2030 initiative, which aims to strengthen rehabilitation in the health system [1]. However, strengthening of rehabilitation in the health system remains a challenge due to limited rehabilitation-related data. Rehabilitation is a complex construct, which remains poorly understood by policymakers. The variability in the definitions and scope of rehabilitation professionals further complicates the understanding of rehabilitation services and how it should be planned and delivered [5,6,7].
Definitions of the rehabilitation workforce vary across countries due to differences in the classification of rehabilitation professionals [5, 7, 8]. The WHO Rehabilitation Competency Framework highlights the diversity in the rehabilitation workforce between WHO regions [9]. WHO defines a rehabilitation worker as ‘a person delivering or supporting the delivery of rehabilitation, whether interacting directly or indirectly with a person, their family or service-user groups’ [3]. In many countries, rehabilitation professionals are also referred to as ‘allied health workers’ and could also encompass different professionals such as radiographers [8, 10]. The WHO classification of a ‘rehabilitation worker’ also includes other professionals such as nurses and psychologists who specialise in rehabilitation [3, 9]. However, the core professionals classified as rehabilitation professionals in LMICs include occupational therapists, audiologists, speech-language therapists and physiotherapists [3, 9].
Describing the primary rehabilitation workforce capacity is also challenged by a lack of standardised and agreed-upon global metrics [5, 7]. The knowledge base describing the rehabilitation workforce is arguably limited (and biased towards HICs), as there is a paucity of knowledge on workforce metrics to describe the local context, plan services and enable between-country comparisons [5, 7, 8]. Although some descriptors used to describe the rehabilitation workforce are similar in published reports, differences are also apparent [5, 7, 8, 11]. These inconsistencies highlight the need for a comprehensive understanding of current practices, which can offer guidance to countries wishing to describe their rehabilitation workforce [1, 3]. A synthesis of rehabilitation workforce descriptors will be particularly useful to LMICs, to enable the efficient selection of metrics that will suit their local contexts. In addition, it will allow countries to use rehabilitation workforce descriptors that can be used for global comparison and benchmarking [2, 5, 9].
To respond to the WHO’s recommendation for a country-specific description of the rehabilitation workforce, the selection of appropriate and commonly used metrics is an important preliminary step towards service planning [12]. Therefore, this study aimed to scope the range of descriptors and metrics used to describe the rehabilitation workforce in published reports. A secondary objective was to compare the workforce across countries that used similar descriptors in the published reports.
Methods
Study design
A scoping review was conducted according to the five-step framework first developed by Arksey and O’Malley [13]. These steps are i) identifying the research objective(s), ii) identifying relevant studies, iii) selecting the studies, iv) charting the data, and v) collating, summarising and reporting the results. The review included a broad search of literature regarding the rehabilitation workforce and how countries quantify and describe the rehabilitation workforce. Reporting followed the PRISMA Extension for Scoping Reviews checklist (see Addendum 1) [14].
Identifying the research question
The research objectives assisted in determining the eligibility criteria, guided the scope of the review, and determined an effective search strategy.
To achieve the overall study aim, the following objectives were completed:
-
1)
Understand the data collection methods or data sources used to collate rehabilitation workforce capacity information (descriptors and indicators),
-
2)
Synthesise which descriptors and indicators were used to describe (or quantify) national or regional rehabilitation workforce data (e.g., type of therapist, qualifications and work setting).
Identifying relevant studies
Search strategy
A broad and comprehensive three-step search strategy was undertaken to identify published studies in five databases (PubMed, CINAHL, Scopus, Science Direct and Web of Science). These databases were chosen in consultation with a librarian as they yielded the most relevant results. Databases such as Africa Wide and EBSCOHost were accordingly excluded. As a first step, an initial limited keyword search was conducted in PubMed, using key terms related to ‘rehabilitation workforce’, ‘physiotherapy’, ‘physical therapy’, ‘occupational therapy’, ‘speech therapy’, ‘speech-language therapy’, ‘audiology’, ‘allied health’, ‘rehabilitation workforce’, ‘human resources’, ‘human resources for health’, ‘staffing’, ‘supply’, ‘population needs’ and ‘demographics’.
This was followed by an analysis of the text words of the titles and abstracts of potentially relevant articles, and keywords used to index articles. A second search was undertaken, which incorporated the identified additional or refined index and keywords across all databases. The preliminary search string that was developed for PubMed is provided in Addendum 2. Thirdly, all the reference lists of identified literature were searched to include additional evidence that might have been missed in the electronic database searches. A librarian was consulted to ensure that these searches were methodical and transparent. The librarian conducted the searches independently to ensure that the same results were produced as those that the reviewer conducting searches (TC) found.
All database search outcomes were transferred to Rayyan V0.1.0 software (Rayyan Systems Inc., MA, USA) [15]. Deduplication of all articles was conducted using Rayyan before the screening of titles and abstracts.
Inclusion and exclusion criteria
Type of evidence sources
The scoping review included peer-reviewed primary studies, published in English, on rehabilitation workforce. We considered descriptive, cross-sectional and cohort designs. Grey literature and studies published before 2000 were excluded. Studies where the full texts were not available, were also excluded. No geographical limitations were applied.
Types of outcomes
We considered rehabilitation workforce capacity demographics (e.g., profession type, gender, age, employment in the private versus public sector, and employment in a full- versus part-time capacity), and rehabilitation workforce capacity indicators (e.g., the total number of rehabilitation workforce, the ratio per population, rural versus urban distribution or distribution between levels of care). Studies only reporting on forecasting were excluded.
Population
Only literature that included the rehabilitation workforce, or at least one of the professions that are classified as rehabilitation professionals in the relevant countries (such as physiotherapy, occupational therapy, speech-language and hearing therapy/pathology and audiology), were considered [16].
Study selection
Following deduplication, one reviewer (TC) screened all titles and abstracts retrieved and determined eligibility for inclusion. Eligible titles and abstracts were included for full-text review, which was again screened against the review eligibility criteria. If the reviewer (TC) was unsure of a study’s eligibility, a discussion with the second (QL) and third (KB) reviewers ensued for consensus. Reasons for excluding ineligible studies were discussed with the second (QL) and third (KB) reviewers and were documented.
Data charting
Based on a discussion between the reviewers (TC, QL and KB), a draft data extraction form was developed in Microsoft Excel to ensure that all relevant data about the study objectives were included in the form. The form was piloted by two reviewers (TC and QL) using five randomly-selected eligible articles. Amendments were made by incorporating additional unforeseen data arising from the articles that were deemed important in terms of contributing to the review objectives. The data from the final sample of included articles were extracted by one reviewer (TC), using the final version of the data extraction form (Addendum 3).
Data analysis
Descriptive information (including number of included studies, study designs, publication years, study countries, and professional type) was summarised quantitively. Information on data collection methods and data sources that were used to collate the rehabilitation workforce capacity information were described narratively. Demographic and work setting-related descriptions (e.g., urban, rural, private, public, age and gender) of the rehabilitation workforce data were described similarly. Metrics used to describe/quantify the national or regional rehabilitation workforce data were described and synthesised. To enable comparison and ease of interpretation of the findings regarding the workforce supply, percentages were calculated and, where data were available, ratios per 10 000 of the population were determined. Where ratios were reported per 1 000 or 100 000, the ratio was adjusted to 10 000 population. In cases where studies conducted retrospective analyses, the most recent year’s data were reported.
Results
Selection of studies
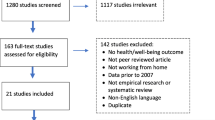
The search produced 539 initial hits. Based on title and abstract screening, 500 records were excluded (213 duplicates and 287 that did not comply with the inclusion criteria). Full texts of the remaining 39 studies were screened and four further studies were identified via PEARLing. After full-text screening, a further 24 studies were excluded, and 19 studies remained for analysis (Fig. 1).
Study characteristics
The included studies were published between 2005 and 2021. Eleven out of the 19 studies (57.9%) were published in the last five years. The total number of countries reported on the eligible studies, was 41 countries; with one study [4] reporting on 35 HICs.
Among the four LMICs included, South Africa [17, 18] and Brazil [19, 20] are classified as upper-middle-income countries [21, 22], while Pakistan [23] and Bangladesh [24] are lower-middle-income countries [25, 26]. The United States of America (USA) was included in eight (42.1%) of the studies [4, 24, 27,28,29,30,31,32], Canada in five (26.3%) [4, 28, 33,34,35] and Australia in three (15.8%) [4, 36, 37].
One of the studies compared physiotherapy between Canada and the USA [28]. The data used in that study were sourced from one of the other studies reporting on Canada only [33]. The other two studies reporting on physiotherapy in Canada were both based in Saskatchewan and published in the same year, using the same data sources [34, 35]. One of these studies reported on the distribution of rural versus urban physiotherapists [34], and the other reported on primary health care (PHC) physiotherapists [35]. The fifth study reporting on Canada was the study comparing 35 HICs [4], which is also one of the studies that included the USA and Australia. Physiotherapy was the more common profession included in the studies (n = 14, 73.7%) [4, 19, 20, 23, 24, 27, 28, 32,33,34,35,36,37,38], and in nine (64.3%) of these studies, physiotherapy was the only profession reported on [20, 24, 27, 28, 33,34,35,36, 38].
Two (10.5%) studies [35, 37] described a specific level of care. One study (5.3%) described only the PHC [35] workforce, and one study looked at the workforce providing services to adults requiring inpatient general rehabilitation [37]. Another two (10.5%) studies [29, 32] described specific population groups. One (5.3%) study included the workforce licenced to issue hearing aids and considered the population ≥ 65 years of age with hearing loss [29]. Wilson et al. (2009) only reported on the ‘underserved area’ population group, classified according to workforce shortage areas [32]. Eighteen (94.7%) of the studies were database reviews and the remaining study was a cross-sectional survey [37] (Table 1).
Rehabilitation data sources used in included studies
The data analysed by the included studies were retrieved from various publicly-accessible resources. More than half of the studies (n = 11, 57.9%)) used data from professional associations [4, 17, 18, 24, 28, 30, 31, 34,35,36, 38]. The professional associations were either regional (n = 3) [34,35,36], national (n = 7) [17, 18, 24, 28, 30, 31, 38] or international professional associations (n = 1) [3] and were either profession-specific (n = 9) [3, 24, 30, 31, 34,35,36, 38] or general health regulatory boards (n = 2) [17, 18]. Nine of the studies [17,18,19,20, 29, 32, 33, 36, 38] used general health databases and some used other government databases such as national census results or government bureau statistics. Only one [37] of the included studies conducted a cross-sectional study specifically aimed at describing rehabilitation workforce.
Workforce descriptions
Education
Two (10.5%) [34, 36] studies reported on the qualification or education of the rehabilitation workforce. One (5.3%) study reported on the number of physiotherapists with postgraduate degrees in New South Wales, Australia [36]. In 2001, 23% of physiotherapists had at least one postgraduate degree. This has increased significantly from 1975 when only 5.4% of physiotherapists had postgraduate qualifications. The second study [34] reported on three elements, namely the institution of qualification, the highest level of qualification, and whether the workforce had completed the Physiotherapy Competency Examination in Saskatchewan, Canada. Eighty-one percent of physiotherapists working in Saskatchewan qualified at the University of Saskatchewan, 13% qualified at another university in Canada and 6% qualified internationally. Most of the physiotherapists (69%) had a bachelor’s degree, 12% had a diploma or certificate and 19% had a postgraduate degree.
Age and gender
Six (31.6%) of the included studies reported on the age and/or gender of the rehabilitation workforce [17, 18, 30, 34, 36, 38]. Four of these studies examined both age and gender, one study reported on age only and the other study on gender only. Three of the studies that reported on the age of the workforce examined the number per age group [17, 18, 30]. One study reported the median age of physiotherapists working in Saskatchewan [34], and another study reported the modal age of physiotherapists per gender [36]. The remaining four studies that examined the gender of the rehabilitation workforce calculated the distribution between males and females [17, 18, 34, 38]. Table 2 shows that at least 70% of the rehabilitation workforce were female and that most of the population was < 40 years old. One study had an almost even distribution of audiologists between the age groups of 31–40, 41–50 and 51–60 years [30].
Full-time versus part-time employment
Five (26.3%) studies [30, 34, 36,37,38] reported on either the distribution of the rehabilitation workforce between full-time and part-time or on the full-time equivalent (FTE) numbers. One study reported part-time as working less than 30 h a week [36]. Another study reported part-time status as working less than 20 h a week [30]. A third study reported part-time status as less than 37 h a week [38]. One study found that 39.4% of the physiotherapists, in New South Wales, worked part-time, of which 93.2% were female and 58.7% of the physiotherapists working full-time, 59% were female [36]. The second study reported that only 25% of audiologists in the USA worked part-time [30]. Audiologists that did not have a full-time clinical role were included in the 25%. One study reported 202 FTE, allied health staff, for 466 in-patient rehabilitation beds [37]. The fourth study reported that 17% of physiotherapists in Ireland worked part-time, with the FTE number at 2617 [38]. The fifth study reported that 25% of physiotherapists in Saskatchewan worked part-time [34].
Type of rehabilitation professions
Most studies reported on physiotherapy (n = 14; 73.7%), of which nine reported on physiotherapy only [20, 24, 27, 28, 33,34,35,36, 38]. Two studies compared physiotherapy to other professions. One of these studies compared physiotherapy with family physicians [34] and the second study compared physiotherapy with occupational therapy, as well as doctors and nurses, although the primary aim was to report on physiotherapy [24]. Three studies (15.8%) reported on audiology only [29,30,31]. One (5.3%) study reported on both audiology and speech therapy [18]. Six (31.6%) studies reported on occupational therapy [4, 17, 19, 23, 32, 37], with one study that reported on occupational therapy only [17]. Three studies reported on physiotherapy, occupational therapy and speech therapy [19, 32, 37]. One of these studies also reported on other allied health staff [37]. Another two studies reported on physiotherapy and occupational therapy [4, 23].
Rehabilitation workforce distribution between public versus private sector
The distribution of the rehabilitation workforce between the public and private sectors was reported in seven (36.8%) studies [17, 18, 20, 34,35,36, 38]. Five of these studies reported on physiotherapy [20, 34,35,36, 38], one on audiology and speech therapy [18], and one on occupational therapy [17]. Two of the four studies reported on the physiotherapy workforce in Saskatchewan, Canada [34, 35]. Both studies reported similar findings, namely that the gap between private and public are almost equally distributed, with public supply being just more than 50%. One study categorised the physiotherapy workforce into ‘own’ practice, ‘private’ and ‘public’ sectors [36]. For the purposes of this study, own practice and the private sector were combined. A study conducted in Ireland reported that they had physiotherapists working in either private or public sectors and 3% worked in both the private and public sectors [38]. The previous two studies had similar findings to the two conducted in Canada, with the difference of the distribution between the public and private sectors being small. The two studies conducted in South Africa had a very different distribution, where more than 70% were working in the private sector (see Table 3 for detail) [17, 18].
Rehabilitation workforce distribution between urban versus rural settings
Four (21.1%) of the 19 studies reported on the distribution of the rehabilitation workforce in urban versus rural areas (Table 4) [29, 32, 34, 36]. Two of these studies reported on physiotherapy only, where large differences were seen between the rural and urban distribution (Table 4) [34, 36]. One study reported on the distribution of physiotherapy, occupational therapy and speech therapy per 100 000 population [32]. The fourth study reported on the distribution of audiologists who provide hearing aids between rural and urban settings [29]. Table 4 shows that most of the rehabilitation workforce was located in an urban setting. In the study reporting on the physiotherapy, occupational therapy and speech therapy workforce, the difference was not as large as in the other three studies.
Workforce distribution between levels of care
Five (26.3%) studies reported quantitative data: three studies on the distribution of the rehabilitation workforce per level of care [19, 20, 38] and the other two studies reported on data from a level of care [35, 37]. Both studies that hailed from Brazil [19, 20], reported on the level of care; however, the reports were on different levels of care. The study from 2017 [19] reported on PHC, specialised ambulatory care and hospital care. The study from 2021 [20] reported on primary, secondary and tertiary health care. The other study [38] reporting on physiotherapists per level of care, calculated the distribution between acute and non-acute care. There were 1774 physiotherapists working in non-acute care and 846 in acute care [38]. One study reported on the rehabilitation workforce capacity of general inpatient beds in Queensland, Australia (466 beds) [37]. One of the studies conducted on physiotherapists in Saskatchewan reported on the availability at PHC level [35].
Rehabilitation workforce density/supply
Supply
Most (n = 14; 73.7%) of the studies [17, 18, 20, 23, 28,29,30,31, 33,34,35,36,37,38] reported the absolute total numbers of the rehabilitation workforce. Nine of these studies provided totals at the national level [17, 18, 20, 23, 28, 30, 31, 33, 38], and the other five at the regional level [29, 34,35,36,37]. Two of these five studies reported on totals not only for a specific region but also for a specific population [29, 37]. One study reported on the number of audiologists (n = 879) who serve the population who are most likely to have hearing impairments in Arizona, USA [29]. The other study in Queensland, Australia, reported on the FTE (n = 119) of general inpatient beds [37]. Two studies reported on the total physiotherapists (n = 643) in Saskatchewan, Canada [34, 35] and the third study reported on physiotherapists (n = 6900) in New South Wales, Australia [36]. Three of the studies reporting on national totals were conducted in Canada (n = 15 772), the USA (n = 167 810) and Ireland (n = 3172) for physiotherapy [28, 33, 38]. One of the studies reported on the physiotherapy and occupational therapy workforce in Pakistan (n = 1150) [23]. Two studies reported on the occupational therapy (n = 5180) and audiology and speech therapy (n = 3266) workforce in South Africa [17, 18]. See Table 5 for the supply of professions not included in the national ratios.
Population-adjusted ratios
Thirteen (68.4%) of the studies reported on the population-adjusted ratios [4, 17,18,19,20, 24, 27, 28, 31,32,33, 35, 38].The population ratio varied from 1 000 per capita to 100 000. All four of the LMICs reported population-adjusted ratios of less than one per 10 000 capita [17,18,19,20, 24]. One of the studies compared the population-adjusted ratio of 35 HICs [4].
Figure 2 shows the ratio of physiotherapists per 10 000 population of those studies that reported ratios [19, 20, 24, 27, 28, 33, 38], as well as Rathore et al. (2011) that provided the total number [23, 39] (for the latter, the population ratio were calculated using population data from The World Bank (https://data.worldbank.org/indicator/SP.POP.TOTL)).
Figure 3 shows the ratios of occupational therapists per 10 000 population of those studies that reported ratios [17, 19, 24] and the ratio for Pakistan [23], for which the ratio was calculated as mentioned previously.
Figure 4 shows the ratios of audiologists and speech therapists reported in the study findings [18, 19, 30,31,32].
Figure 5 shows the ratios of physiotherapy and occupational therapy combined per 10 000 population of the 35 HICs [4] and for the studies that provided data to calculate the combined ratios [19, 23, 24].
Discussion
To our knowledge, this is the first scoping review that examined descriptors and indicators of the rehabilitation workforce capacity across core rehabilitation professions and on a global level. Although only four LMICs were included in the review, the main descriptors and indicators identified are arguably applicable across contexts and settings. Our findings indicated that the following descriptors and indicators were most commonly used to quantify the rehabilitation workforce across countries: profession type, density, supply, distribution between rural and urban regions, distribution between public and private sectors, and age and gender.
The most common way in which the rehabilitation workforce was indicated, related to profession type. Reporting the rehabilitation workforce by profession is important, as multidisciplinary rehabilitation is reported as being the most effective for delivering quality rehabilitation services [1, 3, 6]. In this review, physiotherapy was the dominant rehabilitation profession reported (reported in 74% [4, 19, 20, 23, 24, 27, 28, 32,33,34,35,36,37,38] of the included studies, while for example, only 25% reported on speech and language therapy [18, 19, 32, 37]). In LMICs where rehabilitation professionals are scarce, physiotherapy is often the only available rehabilitation profession [3, 5, 24], leading to sub-optimal services. Knowledge about the available rehabilitation professional types is thus also important for country-level planning of education and training opportunities for rehabilitation professionals to facilitate a multidisciplinary workforce [1]. Rathore et al. (2011) for example reported that there are only two occupational therapy training programmes in Pakistan, which contributed to the low number (n = 150) of occupational therapists [23]. Countries can therefore use information on the type of therapists to initiate new training programmes and devise interim strategies to ensure that comprehensive services are delivered.
A quarter (26%) of the included studies [17, 18, 30, 34, 36] reported on the age of the rehabilitation workforce. Many studies used publicly available datasets that did not specify data on age and gender. Anderson et al. (2005) commented that the modal age is a ‘statistic of great significance’ and that it can be a predictor of the profession’s longevity [36]. Ned et al. (2020) commented that a younger workforce can be due to poor absorption and retention rates in the public sector [17]. It may also be indicative of younger therapists working abroad. An ageing workforce implies that there is a risk that experience and skillsets are maintained to deliver quality services [17]. Therefore, it is important for countries to consider age when describing the rehabilitation workforce to ensure that human resource planning meets service demands.
In many countries, gender equity is an important goal and gender should thus be considered in the descriptors to track gender distribution. About 26% of the profession included gender in the description of the rehabilitation workforce [17, 18, 30, 36]. Since rehabilitation is still a predominantly female profession (this was the case for all studies that reported gender), it is advisable that future research and descriptions of the workforce consider gender as a descriptor. Although this trend is also notable in other healthcare professionals [40], countries should consider whether gender equity is an important consideration for the local context. In addition, operational factors such as the preference for part-time positions among females may have implications for service delivery. Therefore, local contextual factors play an important role in whether gender should be included as a descriptor of the rehabilitation workforce.
The distribution of the rehabilitation workforce between rural and urban settings was reported in about a fifth of included studies (four of the studies [29, 32, 34, 36]), while one other study only commented that there was a disparity between urban and rural settings [24]. Thus, there is sparse information on the rural or urban distribution of therapists. The studies that reported on the disparity between urban and rural rehabilitation workforce practices obtained their data from various sources, of which the credibility and comparison may be questionable. Two of the studies [34, 36] used the place of employment address requested from the professional body registration data. Other studies [29, 32] used data provided by universities or government registries. The lack of data regarding rural versus urban distribution is concerning, as it is generally known that there is a need for an increased workforce in rural areas [5, 35] and that such lacking a workforce leads to inequity in access. Bath et al. (2015) reported that rehabilitation workers in rural areas felt more isolated in terms of social and professional environments and were therefore unwilling to remain in the rural areas [34]. Without information on this vital indicator, policies and guidelines on workforce capacity cannot be changed to promote equity [3, 6]. Future studies should thus include information on the geographical (rural–urban) distribution of therapists.
Seven included studies (37%) [17, 18, 20, 34,35,36, 38] reported data on the distribution of the rehabilitation workforce between the public and private sectors. In the HICs [34,35,36, 38], there was not a large disparity between the number of therapists working in private versus public practice, but this trend is different in LMICs [17, 18] where most therapists work in private practice. In countries such as South Africa – where more than 80% of the population depends on public healthcare, which has less than 5% of the total resources for health – describing the public/private distribution of healthcare may be important. In other countries with universal healthcare coverage, this descriptor may be irrelevant. For countries where the private/public distribution of the workforce is relevant, it is important to ensure that this information is accurate and updated. National registries such as health registration bodies can be considered feasible data source options.
The included studies also reported on quantitative metrics to describe the rehabilitation workforce. These metrics included absolute values and population ratios. The population-adjusted ratio is the most general measure of workforce supply in a specific area, region or population [28]. Although population ratios provide an estimate of service coverage, additional factors – such as population needs [4] – should also be considered when describing the rehabilitation workforce using this metric. Thus, the interpretation of population ratios also requires an understanding of the local context. In addition, although these population ratios are commonly used, differences in scope of practice, type of professionals between countries and varying competencies across regions and countries may still bar accurate between-country comparisons [8]. Therefore, the between-country comparison still demands some degree of caution and trends may be more useful than absolute quantitative comparisons that consider contexts.
Our review shows that HICs could have a therapist density of up to 40 times higher than LMICs. The stark difference may be due to better financial resources and because HICs have integrated rehabilitation into their policies, which prioritise funding for rehabilitation. In many LMICs, rehabilitation remains under-recognised as an essential healthcare strategy. The triple burden of non-communicable and communicable conditions and trauma evident in LMICs, are all pressing needs, which often utilise most of the health resources and funding. Consequently, rehabilitation remains underfunded and not well integrated into service and human resource planning.
Limitations
A single reviewer performed the searching and screening of titles and abstracts, which may have introduced bias. The review included only published primary studies; this may have led to the omission of unpublished information contained in the grey literature. Only studies published in English were included, which may have led to language bias and the potential exclusion of studies from some LMICs. The included studies were limited to studies reporting on rehabilitation workforce capacity, this excluded studies that were on rehabilitation workforce but did not include the capacity thereof – however, studies that did not report on capacity descriptors/metrics fell outside of the scope of this review. In line with scoping review methodology and the purpose of providing a comprehensive summary of the descriptors and metrics (rather than a critical synthesis), no critical appraisal of the included studies was performed [41].
Recommendations
The study findings can contribute to further research on rehabilitation workforce capacity and/or inform a systematic review on rehabilitation workforce. The data and information on rehabilitation workforce capacity in LMICs are lacking, and there is therefore a need to increase reliable and accurate data in LMICs to inform policies and finances for rehabilitation workforce. Future studies should adopt a more in-depth search strategy, including grey literature, to include a broader range of data (descriptors and metrics) at regional and national levels (especially in LMICs where such data may not necessarily be published as research).
Conclusion
This study aimed to scope the range of descriptors and metrics used to describe the rehabilitation workforce and to compare the workforce across countries that used similar descriptors. Despite the lack of a common definition or scope of the rehabilitation workforce capacity across countries, this review found the six most included descriptors in the eligible studies. The descriptors were profession type, density, supply, distribution between rural and urban regions, distribution between public and private sectors, age and gender. These descriptors enabled us to compare the capacity of the rehabilitation workforce across countries, keeping in mind the local context and economic status. These comparisons show that there is a large disparity in the rehabilitation workforce capacity between HICs and LMICs. With many LMICs already having poor access to rehabilitation services, this lack of workforce capacity means that access to rehabilitation services for the most vulnerable populations will be exacerbated. There is a need for reliable and appropriate data on rehabilitation workforce capacity, especially in LMICs, to strengthen rehabilitation into policies and promote the integration of rehabilitation in the local healthcare system.
Availability of data and materials
All data generated and/or analysed during this study are included in this published article, except for the population data from relevant studies which were obtained from the World Bank repository, https://data.worldbank.org/indicator/SP.POP.TOTL.
Abbreviations
- LMICs:
-
Low- to middle-income countries
- HICs:
-
High-income countries
- WHO:
-
World Health Organisation
- USA:
-
United States of America
- PHC:
-
Primary health care
- FTE:
-
Full-time equivalent
- PT:
-
Physiotherapy/physiotherapist
- ST:
-
Speech therapy/ therapist
- OT:
-
Occupational therapy/ therapist
- AU:
-
Audiologist/ Audiology
- NSW:
-
New South Wales
- SA:
-
South Africa
References
Larsen PD. Rehabilitation 2030: A Call for Action. Rehabil Nurs. 2017;44:129. https://doi.org/10.1097/RNJ.0000000000000226.
AS N, Htwe O, AY T, W DG, BS Y, MS N. Facilitators and Barriers to the Rehabilitation Workforce Capacity Building in Low- to Middle-Income Countries. Phys Med Rehabil Clin N Am. 2019;30:867–77. https://pubmed.ncbi.nlm.nih.gov/31563176/.
World Health Organization (WHO). Rehabilitation in Health Systems. 2017.
Jesus TS, Landry MD, Hoenig H, Dussault G, Koh GC, Fronteira I. Is Physical Rehabilitation Need Associated With the Rehabilitation Workforce Supply? An Ecological Study Across 35 High-Income Countries. Int J Heal Policy Manag. 2020;2017 x:1–9.
Gupta N, Castillo-Laborde C, Landry MD. Health-related rehabilitation services: Assessing the global supply of and need for human resources. BMC Health Serv Res. 2011;11.
Naicker AS, Htwe O, Tannor AY, De Groote W, Yuliawiratman BS, Naicker MS. Facilitators and Barriers to the Rehabilitation Workforce Capacity Building in Low- to Middle-Income Countries. Phys Med Rehabil Clin N Am. 2019;30:867–77.
Spotlight. Monitoring human resources for health-related rehabilitation services. World Health. 2009.
Jesus TS, Landry MD, Dussault G, Fronteira I. Human resources for health (and rehabilitation): Six Rehab-Workforce Challenges for the century. Hum Resour Health. 2017;15:8. https://doi.org/10.1186/s12960-017-0182-7.
World Health Organization (WHO). Rehabilitation Competency Framework. 2020.
Louw Q, Grimmer K, Dizon JM, Machingaidze S, Parker H, Ernstzen D. Building capacity in primary care rehabilitation clinical practice guidelines: a South African initiative. Heal Res POLICY Syst. 2018;16.
Cartmill L, Comans TA, Clark MJ, Ash S, Sheppard L. Using staffing ratios for workforce planning: Evidence on nine allied health professions. Hum Resour Health. 2012;10:2. https://doi.org/10.1186/1478-4491-10-2.
Gilmore B, MacLachlan M, McVeigh J, McClean C, Carr S, Duttine A, et al. A study of human resource competencies required to implement community rehabilitation in less resourced settings. Human Resources for Health. 2017;15.
Arksey H, O’Malley L. SCOPING STUDIES: TOWARDS A METHODOLOGICAL FRAMEWORK. Int J Soc Res Methodol. 2005;8:19–32. https://doi.org/10.1017/S0922156508005621.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H. PRISMA Extension for Scoping Reviews (PRISMA-Scr): Checklist and Explanation. Ann Intern Med. 2018;:467–73.
Rayyan. https://rayyan.ai/reviews. Accessed 30 Jun 2021.
NDoH. Framework and Strategy for Disability and Rehabilitation. 2015.
Ned L, Tiwari R, Buchanan H, Van Niekerk L, Sherry K, Chikte U. Changing demographic trends among South African occupational therapists: 2002 to 2018. Hum Resour Health. 2020;18:22. https://doi.org/10.1186/s12960-020-0464-3.
Pillay M, Tiwari R, Kathard H, Chikte U. Sustainable workforce: South African Audiologists and Speech Therapists. Hum Resour Health. 2020;18:1–13.
Rodes CH, Kurebayashi R, Kondo VE, Dornelles Luft V, de Góes Â, Basso Schmitt AC. The access and rehabilitation working process in Primary Health Care. Fisioter e Pesqui. 2017;24:74–82. http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=125266410&site=ehost-live&scope=site.
Rodés CH, Vitor J, Daré L, Araujo BC De, Graciani L, Maria S, et al. The physiotherapy workforce in the Brazilian Unified Health Care System. 2021;:1–11.
Brazil | Data. https://data.worldbank.org/country/brazil?view=chart. Accessed 10 Jun 2022.
South Africa | Data. https://data.worldbank.org/country/south-africa?view=chart. Accessed 10 Jun 2022.
Rathore FA, New PW, Iftikhar A. A Report on Disability and Rehabilitation Medicine in Pakistan: Past, Present, and Future Directions. Arch Phys Med Rehabil. 2011;92:161–6.
Jesus TS, Koh G, Landry M, Ong PH, Lopes AMF, Green PL, et al. Finding the “right-size” physical therapy workforce: International perspective across 4 countries. Phys Ther. 2016;96:1597–609.
Pakistan | Data. https://data.worldbank.org/country/pakistan?view=chart. Accessed 10 Jun 2022.
Bangladesh | Data. https://data.worldbank.org/country/bangladesh?view=chart. Accessed 10 Jun 2022.
Zimbelman JL, Juraschek SP, Zhang X, Lin VW-H. Physical therapy workforce in the United States: forecasting nationwide shortages. PM R. 2010;2:1021–9.
Landry MD, Ricketts TC, Fraher E, Verrier MC. Physical therapy health human resource ratios: A comparative analysis of the United States and Canada. Phys Ther. 2009;89:149–61.
Coco L, Titlow KS, Marrone N. Geographic distribution of the hearing aid dispensing workforce: A teleaudiology planning assessment for Arizona. Am J Audiol. 2018;27 3 Special Issue:462–73.
Windmill IM, Freeman BA. Demand for audiology services: 30-yr projections and impact on academic programs. J Am Acad Audiol. 2013;24:407–16.
Planey AM. Audiologist availability and supply in the United States: A multi-scale spatial and political economic analysis. Soc Sci Med. 2019;222:216–24. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85060092395&doi=10.1016%2Fj.socscimed.2019.01.015&partnerID=40&md5=b728be2fb7fb37c08e82268eff07a732.
Wilson RD, Lewis SA, Murray PK. Trends in the Rehabilitation Therapist Workforce in Underserved Areas: 1980–2000. 2009.
Landry MD, Ricketts TC, Verrier MC. The precarious supply of physical therapists across Canada: exploring national trends in health human resources (1991 to 2005). Hum Resour Health. 2007;5:23.
Bath B, Gabrush J, Fritzler R, Dickson N, Bisaro D, Bryan K, et al. Mapping the physiotherapy profession in saskatchewan: Examining rural versus urban practice patterns. Physiother Canada. 2015;67:221–31.
Shah TI, Bath B, Milosavljevic S. Comparing geographical distribution of community-based physiotherapists and family physicians across Saskatchewan. Can Geogr Can. 2015;59:461–73.
Anderson G, Ellis E, Williams V, Gates C. Profile of the physiotherapy profession in New South Wales (1975–2002). Aust J Physiother. 2005;51:109–16.
Barrett C, Stephens C, Hulcombe J, McEvoy B. Profiling the allied health staffing of Queensland Health inpatient general rehabilitation units. Aust Health Rev. 2015;39:89–94.
Eighan J, Walsh B, Smith S, Wren M-A, Barron S, Morgenroth E. A profile of physiotherapy supply in Ireland. Ir J Med Sci. 2019;188:19–27.
Population, total | Data. https://data.worldbank.org/indicator/SP.POP.TOTL. Accessed 10 May 2022.
El Arnaout N, Chehab RF, Rafii B, Alameddine M. Gender equity in planning, development and management of human resources for health: A scoping review. Hum Resour Health. 2019;17:1–9.
Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18:2119–26.
Acknowledgements
N/A
Funding
This research was funded by the National Research Foundation, Ninety-One Scholarship and South African Physiotherapy Association.
Author information
Authors and Affiliations
Contributions
TC conducted the database searching and screening of eligible studies with the assistance of QL and KB. TC and QL did data extraction and analysis with input from KB. TC wrote the manuscript with major contributions from QL and KB. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
N/A
Consent for publication
N/A
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Addendum 1.
PRISMA Extension for Scoping Reviews checklist.
Additional file 2: Addendum 2.
PubMed Search String.
Additional file 3: Addendum 3.
Data extraction forms 1 and 2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Conradie, T., Berner, K. & Louw, Q. Rehabilitation workforce descriptors: a scoping review. BMC Health Serv Res 22, 1169 (2022). https://doi.org/10.1186/s12913-022-08531-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08531-z