Abstract
Objective
To describe how longitudinal continuity of care (COC) is measured using claims-based data and to review its association with healthcare use and costs.
Research design
Rapid review of the literature.
Methods
We searched Medline (PubMed), EMBASE and Cochrane Central, manually checked the references of included studies, and hand-searched websites for potentially additional eligible studies.
Results
We included 46 studies conducted in North America, East Asia and Europe, which used 14 COC indicators. Most reported studies (39/46) showed that higher COC was associated with lower healthcare use and costs. Most studies (37/46) adjusted for possible time bias and discussed causality between the outcomes and COC, or at least acknowledged the lack of it as a limitation.
Conclusions
Whereas a wide range of indicators is used to measure COC in claims-based data, associations between COC and healthcare use and costs were consistent, showing lower healthcare use and costs with higher COC. Results were observed in various population groups from multiple countries and settings. Further research is needed to make stronger causal claims.
Similar content being viewed by others
Introduction
Continuity of care (COC) is considered a quality indicator and a cornerstone in primary care [1,2,3]. COC is a multidimensional concept with several core elements - repeated and regular visits to a health professional sustained over time (i.e. longitudinal care); a relationship of trust and responsibility between patients and health professionals; and cooperation and communication of relevant information between providers within and between care settings [4, 5]. In practice, three broad sets of dimensions are used: informational, interpersonal, and longitudinal continuity of care [6,7,8]. Informational continuity reflects the availability (storage and access) and the way of transmission (verbal, electronic, written) and sharing of clinical information to providers involved in the patient pathway [6, 9, 10]; systems enhancing informational continuity (e.g., Electronic Medical Record, EMR) deserve more attention and may serve to counterbalance the effect of interruptions in continuity of care in some circumstances [9, 11, 12]. Interpersonal continuity reflects the quality of personal relationships between patients and providers. It often focuses on concepts such as personal trust and responsibility [6, 8, 13, 14]. Finally, longitudinal continuity - the focus of this study, is a quantitative assessment of the continuity of individual care trajectories over time. It is typically measured using indices that reflect the concentration (higher proportion of visits to a specific doctor among other doctors imply higher COC), dispersion (higher overall number of doctors visited imply lower COC), density (more frequent sharing of patients among providers implies higher COC), or sequence of doctor visits (whether the same doctor is visited from one time to the next) [15, 16]. Such indicators may reflect the fragmentation of care trajectories, which may be potentially associated with poor coordination, duplication of low-value services, or polypharmacy [17]. In fact, poor COC was found to be negatively associated with a range of patient outcomes including patient satisfaction, avoidable hospitalizations, readmissions, mortality, or increased healthcare costs [8, 18,19,20,21,22,23]. These negative outcomes affect patients, particularly those with multiple chronic diseases since several healthcare providers are usually involved in their care [18, 22, 24,25,26]. By contrast, we presume that better continuity can lead to fewer unnecessary repeated diagnostic tests and adverse drug interactions. It might also lead to higher outpatient costs (more regular doctor visits), but lower inpatient costs (fewer hospital admissions), thus resulting in lower overall costs. Consequently, focusing on the effect of COC on healthcare utilization and costs may provide important insights into the potential contribution of COC into healthcare efficiency improvement and unnecessary utilization reduction.
The measurement of COC indices requires rich longitudinal data on individual interactions with healthcare providers, which is often problematic to acquire in countries without national registries. Therefore, we considered claims-based data as a good opportunity to study longitudinal COC as they are routinely collected on a large-scale, are relatively easy to access, and provide the advantages of capturing the patient trajectories and costs across different providers over time. Such data are mainly collected for billing and reimbursement purposes with an implicit financial incentive that ensures their regular and comprehensive collection and management.
Several studies have been performed on COC, its measurement and association with health outcomes [4, 5, 7, 14, 22, 27,28,29], accounting for a single dimension of COC (e.g., longitudinal) or broader dimensions. None of these studies narrowed the focus on two important components fostering COC for health system effectiveness: the effect on healthcare utilization and costs, and the use of claims data allowing rich and long-term observations (including administrative databases that are comparable to claims data used for provider billing). Despite differences in the structure and content of administrative databases across countries, several of these databases can be used to measure aspects of COC.
The aim of this paper is to review various indicators of longitudinal COC used in claims data, and the evidence on their associations with healthcare use and costs. We will also assess methodological quality of the studies and express recommendations for future studies.
Materials and methods
We conducted a rapid review [30] of the published peer-reviewed literature, due to time and resources available considerations, knowing that systematic reviews are very resource-intensive. We adhered to PRISMA guidelines as closely as possible and consulted with other literature [31, 32] (protocol registered on PROSPERO [33]), while any derogations and potential biases are reported in the discussion section.
Literature and information search
We searched Medline (Pubmed), EMBASE, and Cochrane Central from inception up to April 1, 2019 (updated in December 2020). The search strategy (Appendix 1) comprised Medical Subject Heading Terms (MeSH) (e.g., "Continuity of Patient Care" [Mesh]), free text words (e.g., "claims data" [tiab]), Boolean terms (e.g., AND, OR) and truncations (e.g., measur*) where necessary. Beside electronic searches, we manually searched references lists of identified studies, and used the google search engine as well as the google scholar platform to identify additional eligible studies.
Eligibility of studies
First, primary studies were included if the study author(s) measured continuity of care (COC) and used claims-based data or administrative data for billing purposes. Per protocol, self-reported questionnaires and surveys as well as editorials, conference papers, letters and non-English papers, were excluded. Additionally, we excluded systematic reviews at the first stage but screened them at a later stage to identify primary studies or potential COC indicators. At the final stage, we excluded the studies not investigating associations between COC, healthcare use and/or costs.
Data items
Our review included primary studies that used COC indicators in the published literature using claims-based data. Out of various possible outcomes, including medication adherence, quality of care, disease/episode incidence, number of chronic conditions and mortality, we focused on healthcare use and costs as dependent variables. Any measure of healthcare use was accepted, such as visits to emergency departments (ED), hospital admissions and re-admissions, likelihood of hospitalization (general or disease-specific), or avoidable/preventable hospitalizations (e.g., hospitalization for ambulatory care-sensitive condition - ACSC). Any measure of healthcare costs was accepted, such as total, inpatient, outpatient care costs, or disease-specific costs. From the included studies, we extracted the following data: study identification information, study design, aim/purpose, source of claims-based data, type of population/setting, sample size, follow-up, COC indicators or indices, period of COC measurements (discrete or over the whole period of follow-up), types of outcomes associated with COC and main findings. One reviewer (MA) was involved in the search and initial selection of the included studies while three reviewers (MA, AN, CP) participated in data extraction and took final decisions on the inclusion/exclusion of eligible studies. We used https://rayyan.qcri.org website for the process of study selection [34]. Discrepancies were resolved upon discussions and consensus.
Risk of bias (quality) assessment
The quality of the studies and risk of bias were evaluated using the Newcastle-Ottawa Scale (NOS) for all included studies [35]. We used the NOS for cohort studies and the adapted version of NOS for cross-sectional studies [36]. As the issue of causality is not explicitly covered by NOS, we checked whether causality and related biases have been formally considered in the study design or acknowledged as study limitations. There is a potential risk of time bias when the COC measurement period does not precede the outcomes measurement period. In this case, it is unclear whether a change in COC changed the outcomes, or vice versa (reverse causality). In addition, attributing changes in outcomes to changes in COC is challenging due to potential omitted variable bias.
Data analysis
We reported the median of sample sizes of the included studies and reported direction and statistical significance of the associations (e.g., odds ratio (OR), hazard ratio (HR), beta-coefficients) between COC and healthcare use and costs. Additionally, we categorized the measures of COC based on the concepts they represented (e.g., density, dispersion) and on the frequency of their use in the primary studies. We also considered the timing of COC measurement, as COC measured in discrete consecutive periods (e.g., yearly) may not reflect the same type of continuity as measured over the full observation period (e.g., 2 or 4 years).
Results
Literature search yield
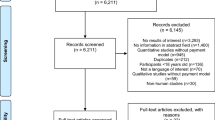
Our electronic and hand searches identified 1,593 potentially relevant studies after removal of duplicates. We excluded 1,383 records based on title/abstract screening. After that, we searched for full texts for the remaining records and manually added potentially eligible studies from the references of retrieved full texts. More studies (N = 12) were excluded due to unavailability of the full texts. Overall, 223 full-text studies were screened against our inclusion criteria, 177 of them were excluded for different reasons, finally arriving at 46 primary studies (Figure 1).
Types of study designs, populations and settings
All studies except six [20, 37,38,39,40,41] were retrospective cohorts; most were conducted in East Asia (n=23) and North America (n=20) (Table 1). The sample size of included studies ranged from 252 to 3,276,635 subjects with a median of 18,113. The vast majority of the studies targeted adults (n=39). Whereas 14 reported on patients with diabetes mellitus, 11 reported on patients with chronic obstructive pulmonary disease (COPD) or asthma, five on heart failure patients, three on hypertensive patients, and the remaining studies were conducted on other patient groups or the general population. All studies were assessed as medium to high quality with all studies showing a rating higher than 6/9 (for cohort studies) and 7/10 (for cross-sectional). Also, all studies investigated associations, adjusting for a wide range of covariates, getting at least one score (out of two maximum) for comparability. Out of 46 studies, causality issues were discussed in 18 studies, while only two studies [42, 43] made claims of a causal effect of COC on the outcomes. Furthermore, 19 studies acknowledged or accounted for time bias only (related to causality issue), which is a necessary but not sufficient condition for making claims of causality, while nine studies never addressed adjustment for time bias or discussed causality issue.
Characteristics of the COC measures
Overall, 14 different measures of COC were applied to claims data in the primary studies investigating associations between COC, healthcare use and costs. Among those, 12 were indices (i.e. composite measures accumulating information from various individual items) (Table 2), and two measures were non-index (Majority-of-Care Rule and Predominant Provider), used more as a reflection for provider attribution [20, 40, 68].
The Bice & Boxerman Continuity Of Care Index (COCI), reflecting both density and dispersion, was the most commonly applied indicator, with 35 studies out of 46 using it. Among density measures, the Usual Provider of Care (UPC) index was the most commonly used and was included in 14 studies. The Modified Modified Continuity Index (MMCI), a dispersion measure of COC, was included in five studies. The Sequential Continuity of Care index (SECON), the only sequential measure, was used in five studies. COC was measured during different measurement periods: most studies (N=19) measured COC on a single year, 13 studies measured over multiple years during follow-up, and the rest of the studies had other measurement period strategies (Table 1).
Outcomes associated with COC
Most studies reported on multiple outcomes (Table 3). Thus, out of 46 studies, the majority of studies (N=29) reported on all-cause and disease-specific hospitalizations or ED visits (N=19), and 14 studies investigated the association between COC and costs.
COC groups were determined in each individual study based on a numerical threshold of COC indices determined by the authors (e.g., 0.5, 0.75, <1) or based on the quartiles/terciles of COC measurement indices. Among the studies reporting the relationship between COC groups and odds of hospitalizations, ORs varied from 1.15 (sample of psychiatric children) [71] to 2.72 [49] (sample of children with asthma) for lower COC groups versus high COC groups, and from 0.07 [61] (sample of diabetes mellitus (DM) patients with heart failure) to 0.95 [18] (sample of COPD and DM older patients) for higher or perfect COC groups versus low COC groups. Among the studies reporting the relationship between COC and the odds of ED visits, ORs varied from 1.14 [71] (psychiatric children) to 2.25 [55] (sample of older patients with asthma) for lower COC and from 0.10 [61] (sample of DM patients with heart failure) to 0.94 [18] (sample of patients with chronic heart failure) for higher or perfect COC. Four studies out of eight focusing on avoidable hospitalization or ACSC reported the ORs, which varied from 1.12 [65] (short-term diabetes-related) to 2.29 [64] (COPD-related) for lower COC (compared to higher COC). From the studies reporting associations with costs, three reported monetary values in US dollars, whereby higher COC was associated with $1656 [77]-$4045 [43] lower total medical costs.
Whereas all studies but seven reported that higher COC was significantly associated with a reduction in healthcare use and costs, five studies found that not all tested associations were significant [42, 63, 68, 73, 75]. Specifically, the following associations did not reach significance: low COC group in short-term with risk of avoidable hospitalization (OR=1.59, CI: 0.91–2.76) [63]; high COC with all-cause hospitalizations (OR = 0.83, CI: 0.67–1.01) [68]; high COC with ED visits (OR=2.6, CI: -0.2–5.4) [73]; high COC with general practitioner (GP) measured using COCI (OR=0.953, CI: 0.884–1.029) and UPC (OR=0.940, CI: 0.849–1.040), in contrast to SECON, with risk of hospitalizations; high COC with ACSC hospitalizations (β=-0.2, CI: -2.1–1.8) [42]. Moreover, one study found unexpected direction of association for a secondary outcome [43], whereby higher COC increased costs by $402 for medical long-term care and by $764 for social long-term care. Finally, one study found mixed evidence on the associations for both tested outcomes (risk of hospitalization and costs), depending on the choice of COC index and type of consultations [44].
Due to substantial heterogeneity of COC and healthcare use measurements and statistical methods applied, it appeared infeasible to pool the studies to produce an estimate of effect size. Details of statistical metrics of individual studies are available in Table 1.
Discussion
Currently, several existing reviews focus on various aspects of COC [4, 6, 14, 78], existing COC measures [7, 8, 79, 80] and associations between COC and various health outcomes [21,22,23, 81]. Our review is the first to narrow down the focus to a specific list of longitudinal COC measures, used only with claims-based data to examine the relationship between longitudinal COC and specific outcomes: healthcare utilization and costs. We identified 46 primary studies conducted mainly in North America and East Asia that considered 14 COC indicators applied to claims-based data. Of those indicators, the COCI and UPC index, representing the concepts of dispersion and density, respectively, were the most commonly used indices. Our results also show that higher COC was frequently associated with decreased healthcare costs and utilization.
The UPC index is relatively easy to calculate and interpret, which might explain the frequency of its use. However, this measure does neither take into account the number of providers seen, nor the distribution of visits to other providers, posing a challenge for chronic patients who need specialty care from “several” providers other than the “usual” one. COCI, in contrast, considers the aforementioned aspects, but is more cumbersome to compute and overly sensitive to increasing number of providers, which leads to likely flawed conclusions about COC for patients with chronic conditions.
In fact, the main issue of currently existing COC indices applied in claims data is their inability to fully capture the multidimensional construct of COC. Longitudinal continuity is usually used in claims-based studies to exhibit interpersonal continuity, as it was assumed that recorded repeated contacts between a patient and care provider already represented a reliant and stable relationship [23]. As all the studies in the review relied on claims data, they focused on longitudinal dimension of continuity, while being unable to potentially integrate other dimensions of COC (e.g., interpersonal or informational). This leaves the gaps in assessing the effect of information or interpersonal continuity on health outcomes. It can be argued that information continuity is likely to be improved more easily than longitudinal continuity from operational perspective, by the implementation of information systems that make patient information more available to all health care providers [20]. Therefore, future studies should try find ways of incorporating broader aspects of COC, such as information exchange, management structure, or interpersonal relations. Moreover, the mentioned above indices do not capture the appropriateness of care, which is important for accurate interpretation of COC and assessment of the need for better COC, especially for patients with chronic conditions [82]. Whereas it may be appropriate to only visit a family doctor and no specialists, chronic care may often imply appropriately visiting several providers, which could result in low COC measures.
Measuring the impact of continuity on healthcare outcomes and costs is rising in the literature [83], albeit the standing aforementioned limitations. In the present review, all studies clearly defined the COC measures and used claims based administrative data to report on the associations between healthcare use and costs. Higher COC was associated with lower costs or healthcare use in any age group with a specific disease or within the general population, despite using various measures of COC and different settings in, but not limited to, countries (e.g., Korea, Taiwan, Norway, and USA) with national healthcare systems and universal coverage. Moreover, all but seven studies included in this review found this association significant for all tested outcomes. Specifically, in the five studies investigating associations with multiple outcomes, the partial results did not reach significance for distinct types of secondary outcomes [42, 63, 68, 73, 75]. One study investigating the causal effect of COC on costs found that higher COC was associated with higher non-institutional cost, but the effect was counterbalanced by lower institutional care cost, resulting in lower total cost [43]. Finally, one Swiss study investigating associations between COC, hospitalizations and costs among cancer patients found highly mixed results, whereby the type of COC index used and the type of consultation highly influenced the results [44]. It needs to be emphasized that the results of the aforementioned studies diverted only partially from the general findings, which suggested overall robust associations between COC and healthcare use and costs. Thus, our review shed light on an emerging consensus in terms of the direction of associations between COC and outcomes that were commonly identified in claims-based studies on healthcare use and cost. These findings emphasize the need to foster COC and to develop continuity-improving strategies, which may be potentially considered for future research: gatekeeping or managed care healthcare models, financing mechanisms for healthcare providers, data sharing and incentives for care coordination and professional collaboration [12, 18, 48, 72, 84,85,86].
Strengths and limitations of the present study
Our study has two main strengths. First, we focused on claims data that are relatively easily accessible and routinely collected on a large scale by public and private entities in many healthcare systems. One key advantage of claims-based data is that in most instances the unit of observation is the enrolled individual and not the provider, so they are more efficient at capturing the journey of patients across providers, whereas provider-based administrative data (e.g., Hospital Episodes Statistics in the UK) do not allow for its own the study of continuity. Second, we comprehensively presented the currently used COC indicators in the published literature, and shed light on the existing studies showing impact of COC on healthcare use and costs in various patients’ and country settings.
Nevertheless, we acknowledge two main limitations in our study. First, the fact that we performed a rapid systematic review, whereby some steps or components of systematic review may be simplified; in our case, it concerned the selection, data extraction and verification phases, which were not performed by two reviewers at all stages. For transparency of our approach, we published our protocol in PROSPERO [33]. Second, the fact that our study may be prone to biases and shortcomings of claims-based data studies. For instance, we did not have details of clinical information, diagnosis details, or use of over-the-counter medications that were not covered/collected by the insurance system, which makes the estimation of associations between COC measures and healthcare costs and use less accurate. It is important to emphasize that the way the providers are reimbursed impacts data collection: in fee-for-service systems, patient-physician interactions are observed whenever patients see their medical doctors, but in global budgets systems, we might not see these interactions, or underestimate them. Additionally, causality, associated time-bias and omitted variables bias apply to all the evidence presented in this review. Most of the studies either acknowledged inability to correct for these issues in the limitations, or adjusted their design and analysis by introducing a lag for the measurement of COC and outcomes, or including time-dependent variable in COC modeling. However, accounting for time-bias is not sufficient to make claims of causal inference, which requires dedicated study design and modeling techniques. Finally, most of the indices were measured in the short-term (1-2 years), while applying a longer observation period could be appropriate to assess whether sustained high COC is associated with health outcomes, especially since the richness of claims data allows for measurements in the long-term.
Conclusions
Despite a variety of currently used COC indicators, it remains difficult to find a measure that fully captures the multidimensionality of continuity. Although all used measures have drawbacks and challenges for estimating COC in chronic patients, our study on the association of COC with health outcomes shows that higher COC is associated with lower healthcare costs and use, which holds true for various countries with distinct healthcare systems. These results highlight the need of an effective healthcare delivery system promoting COC, as it is an important factor in managing diseases to reach more favorable health outcomes with lower healthcare expenses. As COC is a multifaceted construct, policy makers should obtain evidence not only on the longitudinal COC, covered in the current review, but also informational (e.g., electronic health records promotion and effective management) and interpersonal COC (established patient-provider relationships). Future studies should incorporate multiple aspects of COC to cover a broader picture, by making use of patient satisfaction surveys or healthcare pathways information, and cover the causality issue that was found to be problematic in many of the reviewed studies, and apply a design allowing for causal inference.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
References
Arthur KC, Mangione-Smith R, Burkhart Q, Parast L, Liu H, Elliott MN, et al. Quality of Care for Children With Medical Complexity: An Analysis of Continuity of Care as a Potential Quality Indicator. Acad pediatr. 2018;18(6):669–76. https://doi.org/10.1016/j.acap.2018.04.009 (Epub 2018/04/29. PubMed PMID: 29704650).
Yiee JH, Saigal CS, Lai J, Copp HL, Churchill BM, Litwin MS. Timing of orchiopexy in the United States: A quality-of-care indicator. Urology. 2012;80(5):1121–6 (PubMed PMID: rayyan-8871776).
Magill MK, Senf J. A new method for measuring continuity of care in family practice residencies. J Fam Pract. 1987;24(2):165–8 (Epub 1987/02/01 PubMed PMID: 3806028).
Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–21. https://doi.org/10.1136/bmj.327.7425.1219 (Epub 2003/11/25. PubMed PMID: 14630762; PubMed Central PMCID: PMCPMC274066).
Meiqari L, Al-Oudat T, Essink D, Scheele F, Wright P. How have researchers defined and used the concept of ‘continuity of care’ for chronic conditions in the context of resource-constrained settings? A scoping review of existing literature and a proposed conceptual framework. Health Res Policy Syst. 2019;17(1):27. https://doi.org/10.1186/s12961-019-0426-1 (Epub 2019/03/09. PubMed PMID: 30845968; PubMed Central PMCID: PMCPMC6407241).
Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1(3):134–43 (PubMed PMID: rayyan-8871525).
Jee SH, Cabana MD. Indices for continuity of care: a systematic review of the literature. Med Care Res Rev. 2006;63(2):158–88 (PubMed PMID: rayyan-8871054).
Bentler SE, Morgan RO, Virnig BA, Wolinsky FD. Do claims-based continuity of care measures reflect the patient perspective? Med Care Res Rev. 2014;71(2):156–73 (PubMed PMID: rayyan-8871924).
Agarwal G, Crooks VA. The nature of informational continuity of care in general practice. Brit J Gen Pract. 2008;58(556):784–9. https://doi.org/10.3399/bjgp08X342624 (PubMedPMID:WOS:000261567100009).
Hudson BF, Best S, Stone P, Noble T. Impact of informational and relational continuity for people with palliative care needs: a mixed methods rapid review. Bmj Open. 2019;9(5):e027323. https://doi.org/10.1136/bmjopen-2018-027323 (PubMed PMID: WOS:000471192800264).
Litaker D, Ritter C, Ober S, Aron D. Continuity of care and cardiovascular risk factor management: Does care by a single clinician add to informational continuity provided by electronic medical records? Ame J Manag Care. 2005;11(11):689–96 (PubMed PMID: WOS:000233132300003).
Rinner C, Sauter SK, Endel G, Heinze G, Thurner S, Klimek P, et al. Improving the informational continuity of care in diabetes mellitus treatment with a nationwide Shared EHR system: Estimates from Austrian claims data. Int J Med Inform. 2016;92:44–53. https://doi.org/10.1016/j.ijmedinf.2016.05.001 (PubMedPMID:WOS:000378050500006).
von Bultzingslowen I, Eliasson G, Sarvimaki A, Mattsson B, Hjortdahl P. Patients’ views on interpersonal continuity in primary care: a sense of security based on four core foundations. Fam Pract. 2006;23(2):210–9. https://doi.org/10.1093/fampra/cmi103 (Epub 2005/12/20. PubMed PMID: 16361395).
Saultz JW, Albedaiwi W. Interpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med. 2004;2(5):445–51 (PubMed PMID: rayyan-8871526).
Leleu H, Minvielle E. Relationship between Longitudinal Continuity of Primary Care and Likelihood of Death: Analysis of National Insurance Data. PLoS ONE. 2013;8(8):e71669 (PubMed PMID: rayyan-8871882).
Hoertel N, Limosin F, Leleu H. Poor longitudinal continuity of care is associated with an increased mortality rate among patients with mental disorders: results from the French National Health Insurance Reimbursement Database. Eur Psychiatry. 2014;29(6):358–64. https://doi.org/10.1016/j.eurpsy.2013.12.001 (Epub 2014/01/21. PubMed PMID: 24439514).
Freeman G, Hughes J. Continuity of care and the patient experience. 2010.
Hussey PS, Schneider EC, Rudin RS, Fox DS, Lai J, Pollack CE. Continuity and the costs of care for chronic disease. JAMA Intern Med. 2014;174(5):742–8 (PubMed PMID: rayyan-8871033).
Fan VS, Burman M, McDonell MB, Fihn SD. Continuity of care and other determinants of patient satisfaction with primary care. J Gen Intern Med. 2005;20(3):226–33 (PubMed PMID: rayyan-8870833).
Romaire MA, Haber SG, Wensky SG, McCall N. Primary care and specialty providers: an assessment of continuity of care, utilization, and expenditures. Med care. 2014;52(12):1042–9 (PubMed PMID: rayyan-8871490).
Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors-a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open VU. 2018;8(6):e021161. https://doi.org/10.1136/bmjopen-2017-021161 (Epub 2018/07/01. PubMed PMID: 29959146; PubMed Central PMCID: PMCPMC6042583).
Van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010;16(5):947–56 (PubMed PMID: rayyan-8871699).
Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract. 2004;53(12):974–80 (Epub 2004/12/08 PubMed PMID: 15581440).
Gruneir A, Bronskill SE, Maxwell CJ, Bai YQ, Kone AJ, Thavorn K, et al. The association between multimorbidity and hospitalization is modified by individual demographics and physician continuity of care: a retrospective cohort study. BMC Health Serv Res. 2016;16:154. https://doi.org/10.1186/s12913-016-1415-5 (Epub 2016/04/29. PubMed PMID: 27122051; PubMed Central PMCID: PMCPMC4848783).
Weir DL, McAlister FA, Majumdar SR, Eurich DT. The Interplay Between Continuity of Care, Multimorbidity, and Adverse Events in Patients With Diabetes. Med Care. 2016;54(4):386–93. https://doi.org/10.1097/MLR.0000000000000493 (PubMed PMID: 26807539 Epub 2016/01/26).
Wang C, Kuo HC, Cheng SF, Hung JL, Xiong JH, Tang PL. Continuity of care and multiple chronic conditions impact frequent use of outpatient services. Health Informatics J. 2020;26(1):318–27. https://doi.org/10.1177/1460458218824720 (PubMed PMID: 30702018 Epub 2019/02/01).
Kao YH, Lin WT, Chen WH, Wu SC, Tseng TS. Continuity of outpatient care and avoidable hospitalization: a systematic review. Am J manag Care. 2019;25(4):e126–34 (Epub 2019/04/16 PubMed PMID: 30986022).
Pollack CE, Hussey PS, Rudin RS, Fox DS, Lai J, Schneider EC. Measuring care continuity : A comparison of claims-based methods. Med Care. 2016;54(5):e30–4 (PubMed PMID: rayyan-8871432).
Yang F, Xiong ZF, Yang C, Li L, Qiao G, Wang Y, et al. Continuity of Care to Prevent Readmissions for Patients with Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis. COPD. 2017;14(2):251–61. https://doi.org/10.1080/15412555.2016.1256384 (PubMed PMID: 28326901 Epub 2017/03/23).
Schünemann HJ, Moja L. Reviews: Rapid! Rapid! Rapid! …and systematic. Syst Rev. 2015;4(1):4. https://doi.org/10.1186/2046-4053-4-4.
Kelly SE, Moher D, Clifford TJ. Quality of conduct and reporting in rapid reviews: an exploration of compliance with PRISMA and AMSTAR guidelines. Syst Rev-London. 2016;5:79. https://doi.org/10.1186/s13643-016-0258-9 (PubMed PMID: WOS:000453148200078).
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. Bmc Med. 2015;13:224. https://doi.org/10.1186/s12916-015-0465-6 (PubMed PMID: WOS:000361349600001).
Al-Gobari M, Nicolet A, Perraudin C, Wagner J, Bugnon O, Peytremann-Bridevaux I, et al. Measures of continuity of care (COC) in claims-based data: a rapid review of the literature. PROSPERO 2019 CRD42019130786 Available from:https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019130786 . 2019.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4 (PubMed PMID: 27919275; PubMed Central PMCID: PMCPMC5139140).
Wells GA SB, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [cited 2020 June 3rd].
The modified Newcastle Ottawa scale for cross sectional studies. https://doi.org/10.1371/journal.pone.0136065.s004&type=supplementary [cited 2020 June 4th ].
Bazemore A, Petterson S, Peterson LE, Bruno R, Chung Y, Phillips RL. Higher Primary Care Physician Continuity is Associated With Lower Costs and Hospitalizations. Ann Fam Med. 2018;16(6):492–7 (PubMed PMID: rayyan-8871911).
Cho KH, Lee SG, Jun B, Jung BY, Kim JH, Park EC. Effects of continuity of care on hospital admission in patients with type 2 diabetes: analysis of nationwide insurance data. BMC Health Serv Res. 2015;15:107 (PubMed PMID: rayyan-8871989).
Gill JM, Mainous AG III, Nsereko M. The effect of continuity of care on emergency department use. Arch Fam Med. 2000;9(4):333 (PubMed PMID: rayyan-8870902).
Menec VH, Sirski M, Attawar D. Does continuity of care matter in a universally insured population? Health Serv Res. 2005;40(2):389–400 (PubMed PMID: rayyan-8871281).
Pollack CE, Weissman GE, Lemke KW, Hussey PS, Weiner JP. Patient sharing among physicians and costs of care: A network analytic approach to care coordination using claims data. J Gen Intern Med. 2013;28(3):459–65.
Lei LL, Cai SB, Conwell Y, Fortinsky RH, Intrator O. Can Continuity of Care Reduce Hospitalization Among Community-dwelling Older Adult Veterans Living With Dementia? Med Care. 2020;58(11):988–95. https://doi.org/10.1097/Mlr.0000000000001386 (PubMedPMID:WOS:000578092600009).
Lei LL, Intrator O, Conwell Y, Fortinsky RH, Cai SB. Continuity of care and health care cost among community-dwelling older adult veterans living with dementia. Health Serv Res. 2020. https://doi.org/10.1111/1475-6773.13541 (PubMedPMID:WOS:000560409500001).
Blozik E, Bähler C, Näpflin M, Scherer M. Continuity of Care in Swiss Cancer Patients Using Claims Data. Patient Prefer Adherence. 2020;14:2253–62. https://doi.org/10.2147/PPA.S266381.
Chen CC, Chen SH. Better continuity of care reduces costs for diabetic patients. Am J Manag Care. 2011;17(6):420–7.
Chen YY, Hsieh CI, Chung KP. Continuity of Care, Follow-Up Care, and Outcomes among Breast Cancer Survivors. Int J Environ Res Public Health. 2019;16(17):3050.
Chen AY, Chen B, Kuo CC. Better continuity of care improves the quality of end-of-life care among elderly patients with end-stage renal disease. Sci Rep. 2020;10(1):19716.
Chen CC, Cheng SH. Care Continuity and Care Coordination: A Preliminary Examination of Their Effects on Hospitalization. Med Care Res Rev. 2020. https://doi.org/10.1177/1077558720903882 (PubMed PMID: WOS:000513319900001. Artn1077558720903882).
Cho KH, Park EC, Nam YS, Lee SH, Nam CM, Lee SG. Impact of market competition on continuity of care and hospital admissions for asthmatic children: A longitudinal analysis of nationwide health insurance data 2009–2013. PLoS ONE. 2016;11(3):e0150926.
Christakis DA, Feudtner C, Pihoker C, Connell FA. Continuity and quality of care for children with diabetes who are covered by medicaid. Ambulatory Pediatr. 2001;1(2):99–103.
Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107(3):524–9.
Christakis DA, Wright JA, Koepsell TD, et al. Is greater continuity of care associated with less emergency department utilization? Pediatrics. 1999;103(4):738–42.
Chu HY, Chen CC, Cheng SH. Continuity of care, potentially inappropriate medication, and health care outcomes among the elderly: Evidence from a longitudinal analysis in Taiwan. Medical Care. 2012;50(11):1002–9.
Hong JS, Kang HC. Continuity of ambulatory care and health outcomes in adult patients with type 2 diabetes in Korea. Health Policy. 2013;109(2):158–65.
Hong JS, Kang HC, Kim J. Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea. J Korean Med Sci. 2010;25(9):1259–71 (PubMed PMID: rayyan-8871819).
Huang ST, Wu SC, Hung YN, Lin IP. Effects of continuity of care on emergency department utilization in children with asthma. Am J Manag Care. 2016;22(1):e31–7.
Jung B, Cho KH, Lee DH, Kim S. The effects of continuity of care on hospital utilization in patients with knee osteoarthritis: analysis of Nationwide insurance data. BMC Health Serv Res. 2018;18(1):152.
Kao YH, Wu SC. Effect of continuity of care on emergency department visits in elderly patients with asthma in Taiwan. J Am Board Fam Med. 2017;30(3):384–95. https://doi.org/10.3122/jabfm.2017.03.160285.
Kim HJ, Moon K, Park TH, et al. Factors affecting treatment compliance in new hypertensive patients in Korea. Clin Exp Hypertens. 2016;38(8):701–9.
Knight JC, Dowden JJ, Worrall GJ, et al. Does higher continuity of family physician care reduce hospitalizations in elderly people with diabetes? Popul Health Manag. 2009;12(2):81–6.
Lai YR, Yang YS, Tsai ML, Lu YL, Kornelius E, Huang CN, et al. Impact of potentially inappropriate medication and continuity of care in a sample of Taiwan elderly patients with diabetes mellitus who have also experienced heart failure. Geriatr Gerontol Int. 2016;16(10):1117–26 (PubMed PMID: rayyan-8871160).
Li YC. Continuity of care for newly diagnosed diabetic patients: A population-based study. PLoS ONE. 2019;14(8):e0221327.
Lin IP, Wu SC. Effects of long-term high continuity of care on avoidable hospitalizations of chronic obstructive pulmonary disease patients. Health Policy. 2017;121(9):1001–7 (PubMed PMID: rayyan-8871206).
Lin IP, Wu SC, Huang ST. Continuity of care and avoidable hospitalizations for Chronic Obstructive Pulmonary Disease (COPD). J Am Board Fam Med. 2015;28(2):222–30 (PubMed PMID: rayyan-8871207).
Lin W, Huang IC, Wang SL, Yang MC, Yaung CL. Continuity of diabetes care is associated with avoidable hospitalizations: Evidence from Taiwan’s National Health Insurance scheme. Int J Qual Health Care. 2010;22(1):3–8 (PubMed PMID: rayyan-8871819).
Hyer JM, Paredes AZ, Tsilimigras DI, et al. Preoperative continuity of care and its relationship with cost of hepatopancreatic surgery. Surgery. 2020;168(5):809–15.
Mainous AG 3rd, Gill JM. The importance of continuity of care in the likelihood of future hospitalization: is site of care equivalent to a primary clinician? Am J Public Health. 1998;88(10):1539–41.
Menec VH, Sirski M, Attawar D, Katz A. Does continuity of care with a family physician reduce hospitalizations among older adults? J Health Serv Res Policy. 2006;11(4):196–201.
Nam YS, Cho KH, Kang HC, et al. Greater continuity of care reduces hospital admissions in patients with hypertension: An analysis of nationwide health insurance data in Korea, 2011–2013. Health Policy. 2016;120(6):604–11.
Nyweide DJ, Anthony DL, Bynum JPW, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Internl Med. 2013;173(20):1879–85.
Pennap D, Zito JM, Santosh PJ, Tom SE, Onukwugha E, Magder LS. Continuity of Care and Mental Health Service Use Among Medicaid-enrolled Youths. Med Care. 2020;58(3):199–207. https://doi.org/10.1097/Mlr.0000000000001255 (PubMedPMID:WOS:000515568500003).
Pollack CE, Lemke KW, Roberts E, Weiner JP. Patient sharing and quality of care measuring outcomes of care coordination using claims data. Medical Care. 2015;53(4):317–23 (PubMed PMID: rayyan-8871433).
Reddy A, Wong E, Canamucio A, Nelson K, Fihn SD, Yoon J, et al. Association between Continuity and Team-Based Care and Health Care Utilization: An Observational Study of Medicare-Eligible Veterans in VA Patient Aligned Care Team. Health Serv Res. 2018;53:5201–18.
Swanson JO, Vogt V, Sundmacher L, et al. Continuity of care and its effect on readmissions for COPD patients: A comparative study of Norway and Germany. Health Policy. 2018;122(7):737–45.
Vogt V, Koller D, Sundmacher L. Continuity of care in the ambulatory sector and hospital admissions among patients with heart failure in Germany. Eur J Public Health. 2016;26(4):555–61 (PubMed PMID: 26962039).
Worrall G, Knight J. Continuity of care is good for elderly people with diabetes: Retrospective cohort study of mortality and hospitalization. Can Fam Physician. 2011;57(1):e16–20.
Yang KT, Yin CH, Hung YM, Huang SJ, Lee CC, Kuo TJ. Continuity of Care Is Associated with Medical Costs and Inpatient Days in Children with Cerebral Palsy. Int J Env Res Pub He. 2020;17(8):2913. https://doi.org/10.3390/ijerph17082913 (PubMed PMID: WOS:000535744100298).
Gulliford M, Naithani S, Morgan M. What is ‘continuity of care’? J Health Serv Res Policy. 2006;11(4):248–50. https://doi.org/10.1258/135581906778476490 (PubMed PMID: 17018200 Epub 2006/10/05).
Shortell SM. Continuity of medical care: conceptualization and measurement. Med Care. 1976;14:377–91.
Smedby O, Eklund G, Eriksson EA, Smedby B. Measures of continuity of care. A register-based correlation study Med Care. 1986;24(6):511–8. https://doi.org/10.1097/00005650-198606000-00005 (PubMed PMID: 3713289 Epub 1986/06/01).
Puntis S, Rugkasa J, Forrest A, Mitchell A, Burns T. Associations between continuity of care and patient outcomes in mental health care: a systematic review. Psychiatr Serv. 2015;66(4):354–63. https://doi.org/10.1176/appi.ps.201400178 (PubMed PMID: 25828980 Epub 2015/04/02).
Lavis JN, Anderson GM. Appropriateness in health care delivery: definitions, measurement and policy implications. CMAJ. 1996;154(3):321–8 (Epub 1996/02/01. PubMed PMID: 8564901; PubMed Central PMCID: PMCPMC1487507).
Boye LK, Mogensen CB, Mechlenborg T, Waldorff FB, Andersen PT. Older multimorbid patients’ experiences on integration of services: a systematic review. BMC Health Serv Res. 2019;19(1):795. https://doi.org/10.1186/s12913-019-4644-6 (PubMed PMID: 31690308; PubMed Central PMCID: PMCPMC6833141).
Sommers AR, Wholey DR. The effect of HMO competition on gatekeeping, usual source of care, and evaluations of physician thoroughness. Am J Manag Care. 2003;9(9):618–27.
Rotar AM, Van Den Berg MJ, Schafer W, Kringos DS, Klazinga NS. Shared decision making between patient and GP about referrals from primary care: Does gatekeeping make a difference? PLoS One. 2018;13(6):e0198729. https://doi.org/10.1371/journal.pone.0198729 (PubMed PMID: 29889861; PubMed Central PMCID: PMCPMC5995363 Epub 2018/06/12).
Struckmann V, Quentin W, Busse R, van Ginneken E. In: Richardson E, Van Ginneken E, editors. How to strengthen financing mechanisms to promote care for people with multimorbidity in Europe? Copenhagen (Denmark): European Observatory Policy Briefs; 2017.
Acknowledgements
Not applicable.
Funding
This work was supported by the Swiss National Science Foundation (Award number: 407440_183447), within the National Research Programme 74 "Smarter Health Care" (NRP 74).
Author information
Authors and Affiliations
Contributions
JM obtained funding and designed the concept of the study, JM and IPB supervised the analysis and interpretation of the results, and revised the manuscript. AN and MAG were responsible for analysis and manuscript preparation. All authors contributed to the study design and development, analysis and revision of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no potential competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nicolet, A., Al-Gobari, M., Perraudin, C. et al. Association between continuity of care (COC), healthcare use and costs: what can we learn from claims data? A rapid review. BMC Health Serv Res 22, 658 (2022). https://doi.org/10.1186/s12913-022-07953-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-07953-z